User login
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
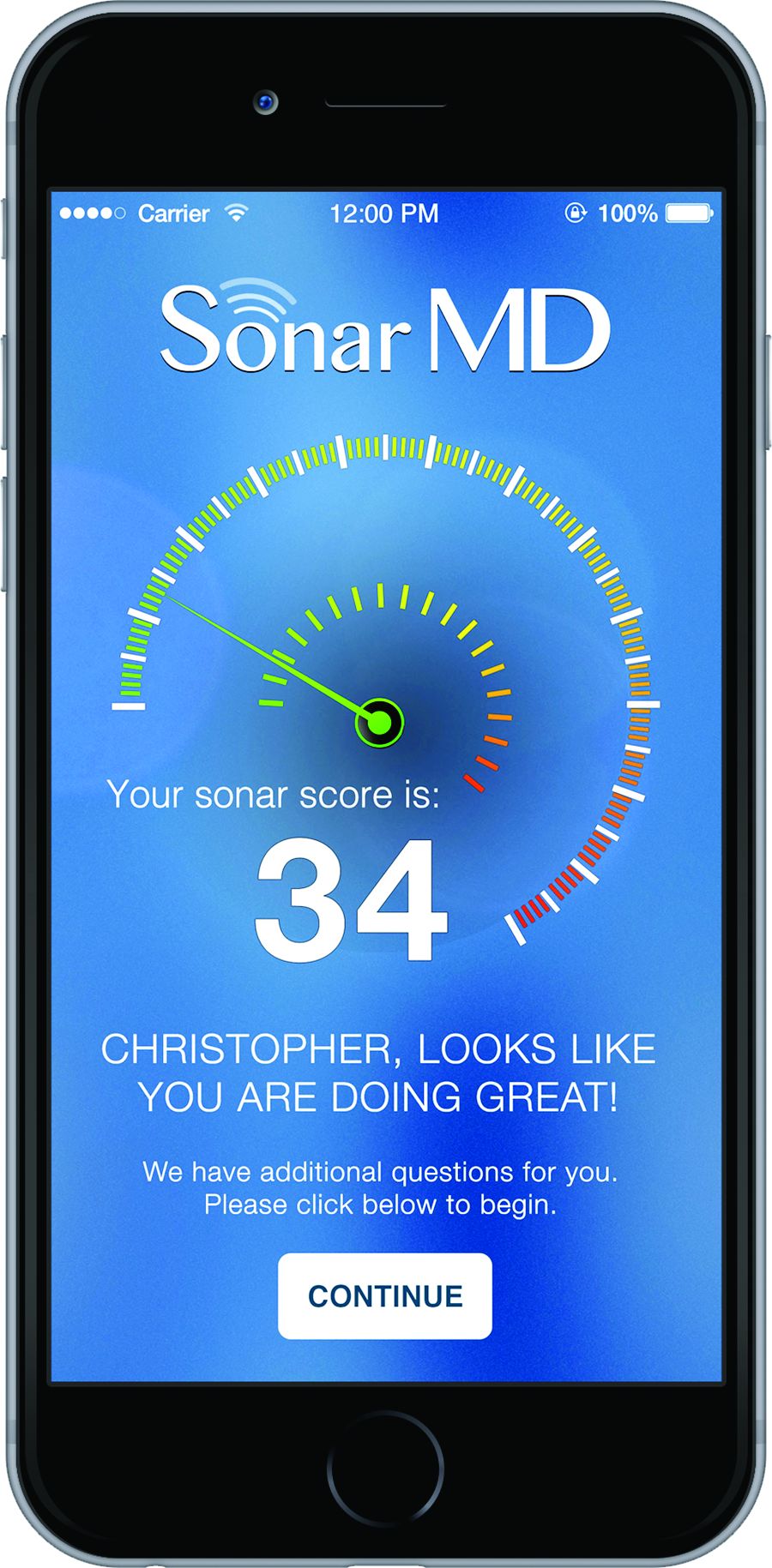
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.