User login
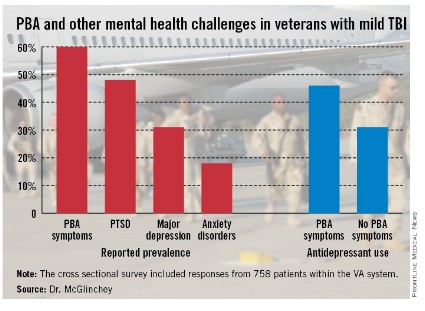
Symptoms of pseudobulbar affect were reported by 60% of veterans with mild traumatic brain injury in a survey of patients in the Veterans Affairs system.
Pseudobulbar affect (PBA) – a neurologic condition involving uncontrollable, disruptive outbursts of crying and/or laughing – was more common among 758 veterans with mild TBI than were posttraumatic stress disorder (48%), major depression (31%), and anxiety disorders (18%), according to Dr. Regina McGlinchey of the VA Boston Healthcare System and her associates, who reported their findings at the Tenth World Congress on Brain Injury in San Francisco.
Veterans with PBA symptoms were more likely to also have PTSD, a finding not previously reported, the investigators said. In the survey, 54% of patients with PBA also reported PTSD, compared with 32% of those who did not have PBA.
Veterans with PBA symptoms also were significantly more likely to be using antidepressants (46%) than were those without PBA (31%), and "those with PBA symptoms reported significantly worse health-related quality of life scores," Dr. McGlinchey said in a statement.
The survey was sponsored by Avanir, maker of Nuedexta (dextromethorphan hydrobromide/quinidine sulfate), which is indicated for treatment of pseudobulbar affect.
Symptoms of pseudobulbar affect were reported by 60% of veterans with mild traumatic brain injury in a survey of patients in the Veterans Affairs system.
Pseudobulbar affect (PBA) – a neurologic condition involving uncontrollable, disruptive outbursts of crying and/or laughing – was more common among 758 veterans with mild TBI than were posttraumatic stress disorder (48%), major depression (31%), and anxiety disorders (18%), according to Dr. Regina McGlinchey of the VA Boston Healthcare System and her associates, who reported their findings at the Tenth World Congress on Brain Injury in San Francisco.
Veterans with PBA symptoms were more likely to also have PTSD, a finding not previously reported, the investigators said. In the survey, 54% of patients with PBA also reported PTSD, compared with 32% of those who did not have PBA.
Veterans with PBA symptoms also were significantly more likely to be using antidepressants (46%) than were those without PBA (31%), and "those with PBA symptoms reported significantly worse health-related quality of life scores," Dr. McGlinchey said in a statement.
The survey was sponsored by Avanir, maker of Nuedexta (dextromethorphan hydrobromide/quinidine sulfate), which is indicated for treatment of pseudobulbar affect.
Symptoms of pseudobulbar affect were reported by 60% of veterans with mild traumatic brain injury in a survey of patients in the Veterans Affairs system.
Pseudobulbar affect (PBA) – a neurologic condition involving uncontrollable, disruptive outbursts of crying and/or laughing – was more common among 758 veterans with mild TBI than were posttraumatic stress disorder (48%), major depression (31%), and anxiety disorders (18%), according to Dr. Regina McGlinchey of the VA Boston Healthcare System and her associates, who reported their findings at the Tenth World Congress on Brain Injury in San Francisco.
Veterans with PBA symptoms were more likely to also have PTSD, a finding not previously reported, the investigators said. In the survey, 54% of patients with PBA also reported PTSD, compared with 32% of those who did not have PBA.
Veterans with PBA symptoms also were significantly more likely to be using antidepressants (46%) than were those without PBA (31%), and "those with PBA symptoms reported significantly worse health-related quality of life scores," Dr. McGlinchey said in a statement.
The survey was sponsored by Avanir, maker of Nuedexta (dextromethorphan hydrobromide/quinidine sulfate), which is indicated for treatment of pseudobulbar affect.