User login
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
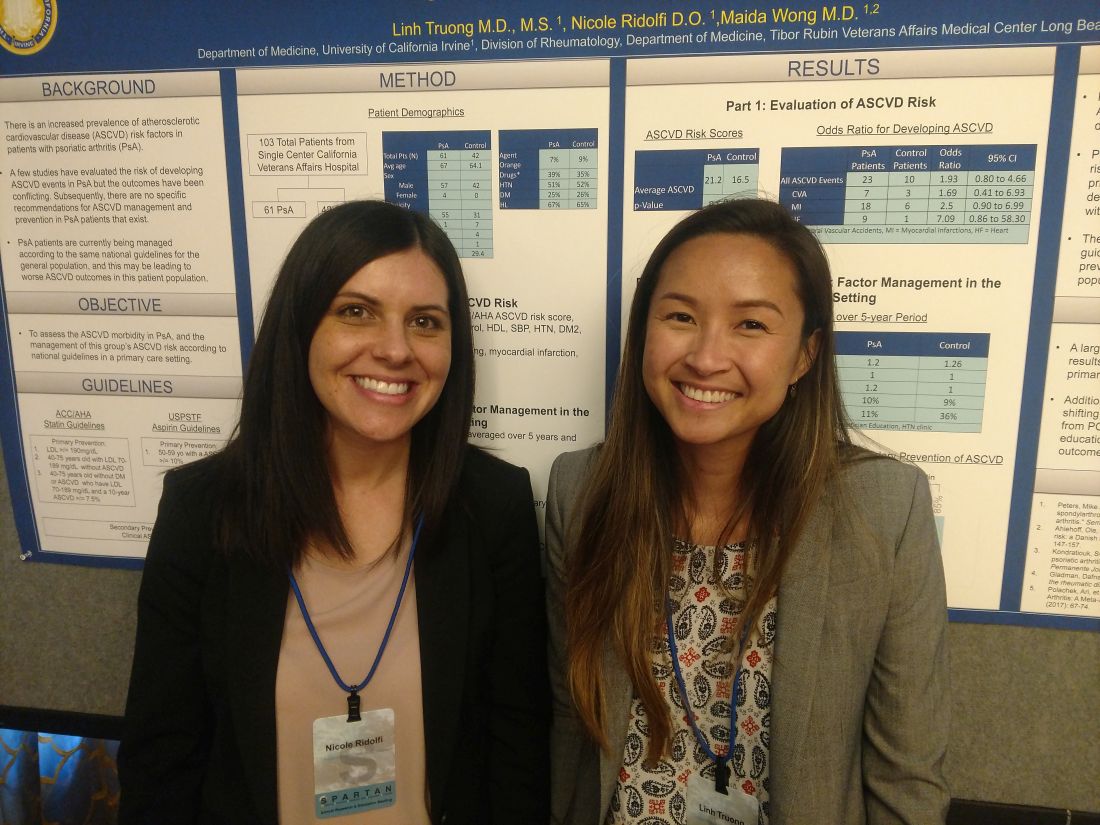
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
REPORTING FROM SPARTAN 2018
Key clinical point: PsA patients have increased risk for ASCVD but are managed with the same intensity as the general population.
Major finding: Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm.
Study details: A single-center study of 61 patients with PsA and 42 matching controls.
Disclosures: The presenters reported having no disclosures.