User login
Psoriatic arthritis patients’ cardiovascular risks aren’t spurring increased management
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
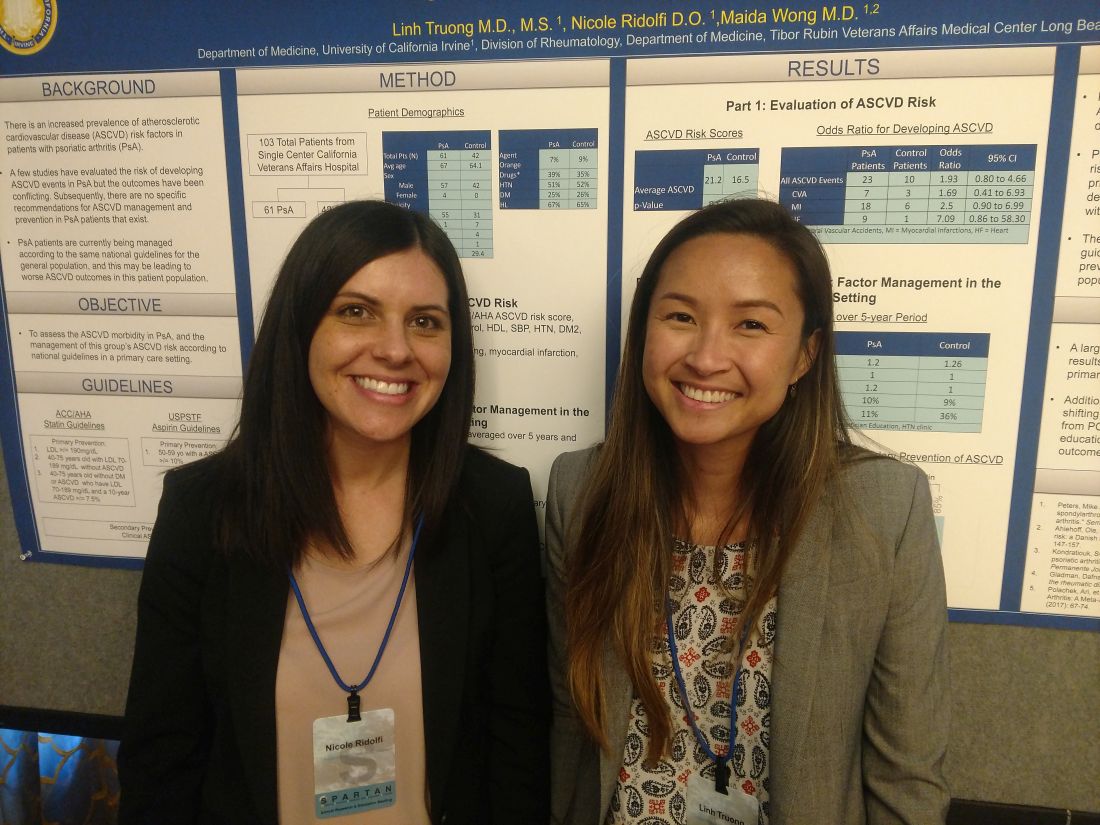
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
CAMBRIDGE, MASS. – Patients with psoriatic arthritis (PsA) receive risk factor management and follow-up for atherosclerotic cardiovascular disease (ASCVD) that is similar to the population at large, according to research presented in a poster session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
The researchers found that patients with PsA in their single-center study did not receive more intensive management and follow-up despite having a higher risk score for ASCVD. This may be caused in part by the fact that there are no specific guidelines for ASCVD management in patients with PsA, according to study authors Linh Truong, MD, and Nicole Ridolfi, DO, internal medicine residents at the University of California, Irvine.
Even though this study and others have shown that patients with psoriatic arthritis have a higher risk for ASCVD, “currently, patients with PsA are being managed exactly the same way as everyone else,” Dr. Truong said.
In addition to assessing ASCVD morbidity in patients with PsA, Dr. Truong and Dr. Ridolfi also wanted to investigate how management of the known ASCVD risk in these patients in a primary care settings compared with national guidelines. Their research came in two parts. In the first part, they calculated 10-year ASCVD risk using a risk score estimator from the American Heart Association/American College of Cardiology. They then calculated an odds ratio for relevant atherosclerotic cardiovascular disease events, such as MI, heart failure, and cerebrovascular accidents. In the second part, they evaluated how the risk factors for ASCVD in patients with PsA were managed in the primary care setting.
The researchers compared data from a single center for 103 patients – 61 with PsA and 42 matching controls. Patients in both groups had an average age in the mid-60s, an average body mass index above 29 kg/m2, and were also mostly male (four patients with PsA were female) and mostly white.
Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm (P less than .0001).
Of patients with psoriatic arthritis, 23 experienced an ASCVD event, compared with 10 patients in the control arm (OR, 1.93; 95% confidence interval, 0.80-4.66). Patients with PsA appeared to experience increased risk for MI (OR, 2.5), heart failure (OR, 7.09), and cerebrovascular accident (OR, 1.96). These increased risks had confidence intervals that approached statistical significance, but did not achieve it.
“We believe that because these data approach [statistical] significance, that further studies are needed,” Dr. Ridolfi said. “Our own validation studies are currently underway.”
In part two of the study, yearly ASCVD risk outcomes were averaged over 5 years and then evaluated based on the frequency of primary care visits, lab checks for HbA1c and lipid profile, and the use of cardioprotective ancillary referrals. The researchers also investigated statin and aspirin use in primary and secondary atherosclerotic cardiovascular disease per guidelines from the American College of Cardiology/American Heart Association and the United States Preventive Services Task Force.
Patients in both groups had similar primary care visits, HbA1c and lipid profiles, and use of cardioprotective supplements (such as fish oil and niacin). However, 36% of patients in the control arm received a nonpharmacologic ancillary referral, compared with just 11% of patients with PsA. Those referrals were in regard to weight loss and diabetes and dietary education, according to the research.
Dr. Truong and Dr. Ridolfi reported that, for primary prevention of ASCVD, PsA patients received treatment less often than did the controls with aspirin (0% vs. 26%, respectively) and statins (40% vs. 50%); there was also less use of statins for secondary prevention (73% vs. 85%).
“These data show that there is an educational opportunity in the primary care setting,” Dr. Truong said. “Or that there is an argument to be made that PsA should be managed by a rheumatology specialist.”
Dr. Truong and Dr. Ridolfi reported no disclosures.
REPORTING FROM SPARTAN 2018
Key clinical point: PsA patients have increased risk for ASCVD but are managed with the same intensity as the general population.
Major finding: Patients with PsA had an average ASCVD risk score of 21.2, compared with a score of 16.5 in the control arm.
Study details: A single-center study of 61 patients with PsA and 42 matching controls.
Disclosures: The presenters reported having no disclosures.
Physical therapy, exercise still relevant for ankylosing spondylitis
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
CAMBRIDGE, MASS. – , according to Angelo Papachristos, an advanced physiotherapist at St. Michaels Hospital in Toronto.
Speaking in an education session at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Mr. Papachristos said that therapy should be introduced at diagnosis, individualized, and constantly reevaluated.
“There is no one recommendation,” he said. “Therapy should be monitored and adjusted over time depending on how the patient responds.”
Mr. Papachristos drew attention to two portions of recommendations from the American College of Sports Medicine (ACSM).
First, that scientific evidence demonstrates that the beneficial effects of exercise are indisputable and that the benefits far outweigh the risks.
Second, that a program of regular exercise that includes cardiorespiratory, resistance, flexibility, and neuromotor aspects to improve and maintain fitness and health is essential for most adults.
How much exercise to prescribe and when to introduce exercise remains a question.
The ACSM recommends moderate-intensity cardiovascular exercise for 30 minutes or more each day or 150 minutes per week, resistance training, neuromotor exercise, and flexibility training at least twice each week.
In a 2011 literature review published in Arthritis Care & Research, researchers analyzed 12 studies (826 total patients) to find out if exercise had actual potential for patients with ankylosing spondylitis. They used three criteria: whether the programs were designed using ACSM recommendations, if/how physiological responses were measured, and whether adherence to programs was monitored.
Of the 12 trials, 5 included cardiovascular exercise, 5 included strength training, 11 included flexibility, and 4 reported program adherence.
Only one trial met ACSM recommendations for intensity, duration, frequency, and length of exercise period. That trial showed the greatest improvement in aerobic capacity (Arthritis Car Res. 2011 Apr;63[4]:597-603).
“The literature isn’t impressive,” said Mr. Papachristos. “But, that’s because it isn’t uniform. No specific protocol is being followed.”
He compared what he believes is happening with what he believes to be a better alternative.
What he calls the hit-them-with-everything approach includes diagnosis, NSAIDs, biologics, smoking cessation at the same time as exercise that includes posture, swimming, strength, and aerobic conditioning. According to Mr. Papachristos, this approach can lead to patient burnout.
Indeed, research from 2010 published in the Journal of Rheumatology showed that 40% of patients with ankylosing spondylitis said that exercise takes too much time, 60% said that exercise is hard work, 60% reported being fatigued by exercise, and 20% said that their family members did not encourage exercise (J Rheumatol. 2010 Mar 1. doi: 10.3899/jrheum.090655).
To combat burnout and improve patient outcomes, Mr. Papachristos suggested an alternative approach whereby patients would begin with diagnosis and medication, but disease education and a baseline fitness assessment would also be a priority. The first 6-9 months following diagnosis would then be used to evaluate a patient’s home and work/school ergonomic situation to assess needs. During this time, the patient would be introduced to basic exercises for range of motion and flexibility. Throughout this approach, the patient would be consistently reevaluated and, if appropriate, would slowly ramp up exercise efforts. At 12 months, the patients could graduate to core cervical and lumbar strength before reaching cardiovascular and sports recreation at 12-18 months following diagnosis.
Mr. Papachristos concluded that the coordination between physical therapist, primary care provider, and rheumatologist is of the utmost importance.
“It’s just like anything else – if we’re all on the same page, it’s better for the patient,” he said. “Patients should be encouraged on lifestyle and wellness management with the goal of lifelong regular exercise.”
Mr. Papachristos reported having no disclosures.
REPORTING FROM SPARTAN
Family history of psoriasis and PsA predicts disease phenotype
BOSTON – Family history appeared to predict disease phenotypes for patients with psoriatic arthritis, according to the results of data presented at the 2018 Spondyloarthritis Treatment and Research Network annual meeting.
“Family history of psoriatic arthritis, compared with psoriasis, had increased risk for deformities and lower risk for plaque psoriasis,” Dilek Solmaz, MD, said.
Of the 1,393 patients analyzed, 444 had a family history of either psoriasis or psoriatic arthritis. Of those, 335 had only psoriasis in their family, while 74 patients had a family history of psoriatic arthritis.
The researchers included onset age, sex, nail involvement, enthesitis, presence of deformities, and plaque type.
In a univariate analysis, psoriasis was a risk factors for younger onset, female sex, nail disease, enthesitis, plaque type psoriasis, and not achieving minimal disease activity. Family history of psoriatic arthritis appeared to be a significant risk factor for deformations (odds ratio, 2.557) and a lower risk for plaque psoriasis (OR, 0.417).
In a multivariate analysis for family history, patients who had a family history of psoriatic arthritis had an increased risk for deformities, compared with patients with family history of psoriasis (OR, 2.143). Those patients also appeared to have a decreased risk for experiencing plaque psoriasis, compared with patients with a history psoriasis (OR, 0.324). All ORs were within the 95% confidence intervals.
“The differences between family history of psoriasis and psoriatic arthritis and their relationship between pustular and plaque phenotypes could point to different genetic backgrounds, as well as pathogenic mechanisms,” Dr. Solmaz said.
BOSTON – Family history appeared to predict disease phenotypes for patients with psoriatic arthritis, according to the results of data presented at the 2018 Spondyloarthritis Treatment and Research Network annual meeting.
“Family history of psoriatic arthritis, compared with psoriasis, had increased risk for deformities and lower risk for plaque psoriasis,” Dilek Solmaz, MD, said.
Of the 1,393 patients analyzed, 444 had a family history of either psoriasis or psoriatic arthritis. Of those, 335 had only psoriasis in their family, while 74 patients had a family history of psoriatic arthritis.
The researchers included onset age, sex, nail involvement, enthesitis, presence of deformities, and plaque type.
In a univariate analysis, psoriasis was a risk factors for younger onset, female sex, nail disease, enthesitis, plaque type psoriasis, and not achieving minimal disease activity. Family history of psoriatic arthritis appeared to be a significant risk factor for deformations (odds ratio, 2.557) and a lower risk for plaque psoriasis (OR, 0.417).
In a multivariate analysis for family history, patients who had a family history of psoriatic arthritis had an increased risk for deformities, compared with patients with family history of psoriasis (OR, 2.143). Those patients also appeared to have a decreased risk for experiencing plaque psoriasis, compared with patients with a history psoriasis (OR, 0.324). All ORs were within the 95% confidence intervals.
“The differences between family history of psoriasis and psoriatic arthritis and their relationship between pustular and plaque phenotypes could point to different genetic backgrounds, as well as pathogenic mechanisms,” Dr. Solmaz said.
BOSTON – Family history appeared to predict disease phenotypes for patients with psoriatic arthritis, according to the results of data presented at the 2018 Spondyloarthritis Treatment and Research Network annual meeting.
“Family history of psoriatic arthritis, compared with psoriasis, had increased risk for deformities and lower risk for plaque psoriasis,” Dilek Solmaz, MD, said.
Of the 1,393 patients analyzed, 444 had a family history of either psoriasis or psoriatic arthritis. Of those, 335 had only psoriasis in their family, while 74 patients had a family history of psoriatic arthritis.
The researchers included onset age, sex, nail involvement, enthesitis, presence of deformities, and plaque type.
In a univariate analysis, psoriasis was a risk factors for younger onset, female sex, nail disease, enthesitis, plaque type psoriasis, and not achieving minimal disease activity. Family history of psoriatic arthritis appeared to be a significant risk factor for deformations (odds ratio, 2.557) and a lower risk for plaque psoriasis (OR, 0.417).
In a multivariate analysis for family history, patients who had a family history of psoriatic arthritis had an increased risk for deformities, compared with patients with family history of psoriasis (OR, 2.143). Those patients also appeared to have a decreased risk for experiencing plaque psoriasis, compared with patients with a history psoriasis (OR, 0.324). All ORs were within the 95% confidence intervals.
“The differences between family history of psoriasis and psoriatic arthritis and their relationship between pustular and plaque phenotypes could point to different genetic backgrounds, as well as pathogenic mechanisms,” Dr. Solmaz said.
REPORTING FROM SPARTAN 2018
Key clinical point: Family history of psoriasis and psoriatic arthritis appear linked with disease phenotypes.
Major finding: Family history of PsA, compared with that of psoriasis, had increased risk for deformities and lower risk for plaque psoriasis.
Study details: Retrospective data from the poster session of SPARTAN 18
Disclosures: The study was funded in part by the UCB Axial Fellowship Grant.