User login
- Pulse palpation is a good test for ruling out atrial fibrillation (C).
- Patients with an irregular pulse should be followed up with an ECG.
- Background: Atrial fibrillation in the elderly is common and potentially life threatening. The classical sign of atrial fibrillation is an irregularly irregular pulse.
- Objective: The objective of this research was to determine the accuracy of pulse palpation to detect atrial fibrillation.
- Methods: We searched Medline, EMBASE, and the reference lists of review articles for studies that compared pulse palpation with the electrocardiogram (ECG) diagnosis of atrial fibrillation. Two reviewers independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
- Results: We identified 3 studies (2385 patients) that compared pulse palpation with ECG. The estimated sensitivity of pulse palpation ranged from 91% to 100%, while specificity ranged from 70% to 77%. Pooled sensitivity was 94% (95% confidence interval [CI], 84%–97%) and pooled specificity was 72% (95% CI, 69%–75%). The pooled positive likelihood ratio was 3.39, while the pooled negative likelihood ratio was 0.10.
- Conclusions: Pulse palpation has a high sensitivity but relatively low specificity for atrial fibrillation. It is therefore useful for ruling out atrial fibrillation. It may also be a useful screen to apply opportunistically for previously undetected atrial fibrillation. Assuming a prevalence of 3% for undetected atrial fibrillation in patients older than 65 years, and given the test’s sensitivity and specificity, opportunistic pulse palpation in this age group would detect an irregular pulse in 30% of screened patients, requiring further testing with ECG. Among screened patients, 0.2% would have atrial fibrillation undetected with pulse palpation.
The objective of this review was to determine how well pulse palpation detects the classical sign of atrial fibrillation—an irregularly irregular pulse—and to estimate the test’s false-positive and false-negative rates. You may want to consider using pulse palpation opportunistically with certain high-risk patients identified in this article.
The scope of the problem. Atrial fibrillation in the elderly is common and potentially life-threatening. Its prevalence increases from 2% in the 65- to 69-year-old age group to 8% among those older than 85 years.1
Atrial fibrillation is an independent risk factor for stroke, increasing a person’s risk 3- to 5-fold. While other major risk factors for stroke, such as hypertension, become less important with age, the risk of stroke from atrial fibrillation increases with age.
Stroke attributable to atrial fibrillation increases from 1.5% among patients 50 to 59 years to 23.5% for those aged 80 to 89.2 Furthermore, stroke in the presence of atrial fibrillation is almost twice as likely to be fatal, results in more functional impairment among survivors, and recurs frequently.3
Stroke due to atrial fibrillation results in considerable mortality and morbidity, but treatment of atrial fibrillation reduces the risk. Warfarin reduces the risk of stroke in non-rheumatic atrial fibrillation by about 70%, an annual absolute risk reduction of 3% (number needed to treat: 30), though the benefits are somewhat offset by the risk of bleeding (annual risk of 0.6%).4
Methods
Search strategy and study selection
We searched the Medline and EMBASE electronic databases from 1966 to June 2005 for all studies comparing pulse palpation with ECG diagnosis. There was no restriction on the language of publication.
The search strategy (see Search strategy and inclusion criteria) included terms for pulse, atrial fibrillation, and a search filter for studies of diagnostic accuracy developed by Van der Weijden et al5 that is highly sensitive and precise.6 We also searched the reference lists of all possibly relevant studies, including review articles. We included all studies that tested patients with both pulse palpation and ECG, and that provided data suitable for calculating sensitivity or specificity (or could be provided by the study authors).
Two reviewers (GC and JD) independently screened the electronic lists of citations. We obtained full-text documents of relevant papers and the 2 reviewers independently reviewed the full-text articles for inclusion according to predetermined criteria (see Search strategy and inclusion criteria). The reviewers agreed on all inclusions.
The authors of this study searched Medline, EMBASE, and the reference lists of review articles for studies using the following criteria.
(pulse) OR (‘Pulse’/all subheadings in MIME,MJ ME))
AND ((atrial fibrillation) OR (‘Atrial-Fibrillation’/all subheadings in MIME,MJME))
AND ((‘sensitivity-and-specificity’/all subheadings in MIME,MJME) OR (sensitivity) OR (specificity) OR (‘Diagnosis-Differential’/all subheadings in MIME,MJME) OR (‘False-Negative-Reactions’/all subheadings in MIME,MJME) OR (‘False-Positive-Reactions’/all subheadings in MIME,MJME) OR (‘Mass-Screening’/all subheadings in MIME,MJME) OR (diagnos*) OR (predictive value*) OR (reference value*) OR (ROC*) OR (Likelihood ratio) OR (monitoring) OR (‘Reference-Values’/all subheadings in MIME,MJME)) OR (atrial fibrillation and (SH=diagnosis))
Two reviewers then independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
Inclusion criteria
- Does the study compare pulse palpation to ECG diagnosis of atrial fibrillation?
- Do all the participants receive both tests?
- Are the sensitivity and specificity provided, or calculable from the data provided?
Data extraction and analysis
We assessed study quality with the QUADAS tool.7 Two reviewers assessed study quality and extracted data independently. We calculated the pooled sensitivity and specificity using Metatest (New England Medical Center, Boston, Mass) and the pooled positive and negative likelihood ratios using the Der-Simonian and Laird random effects model of Revman 4.29 (Cochrane Collaboration), which also tests for heterogeneity.
Results
Search results and selection
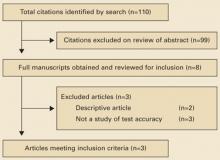
The search strategy identified 110 citations. Six studies were selected for further assessment for inclusion; 3 met the inclusion criteria and covered 2385 patients (FIGURE). All 3 studies included patients older than 65 years enrolled from general practice clinics, and in each study the pulse was taken by a nurse in the clinic. TABLE 1 summarizes the methodological quality, patient characteristics, and results of the 3 studies.
FIGURE
Studies included in this review
TABLE 1
Detecting atrial fibrillation by pulse palpation: Pertinent studies
| STUDY QUALITY CHARACTERISTICS | MORGAN AND MANT8 | SOMERVILLE ET AL10 | SUDLOW ET AL9 |
| Random or consecutive sampling | Yes | No* | Yes |
| Independent assessment | Yes | Yes | Not stated |
| Blind assessment | Yes | Yes | Not stated |
| Verification by ECG | 100% | 100% | 100% |
| Description of index and reference test | Good | Poor | Poor |
| STUDY CHARACTERISTICS | |||
| Number of patients | 1099 | 86 | 1200 |
| Age | 74.3 (65–100) | 65+ | 65+ |
| Setting | 4 GP practices | Single GP practice | Patients from 9 general practices |
| Location | Southampton, UK | Stoke-on Trent, UK | Southern Northumberland, UK |
| Index test | Radial pulse palpated by a nurse for a minimum of 20 seconds† | Pulse palpated by an experienced nurse.§ Time not specified | Pulse palpated by a nurse. Time not specified |
| Reference test | ECG read by cardiologist | 12-lead ECG read by cardiologist | Limb-lead ECG |
| RESULTS | |||
| Prevalence (%) | 6.1 | 30 | 4.6‡ |
| Sensitivity (%; 95% CI) | 91 (81–96) | 100 (87–100) | 95 (85–98)‡ |
| Specificity (%; 95% CI) | 74 (72–77) | 77 (65–86) | 70 (67–73)‡ |
| Positive likelihood ratio (95% CI) | 3.5 (3.1–4.0) | 4.1 (2.6–6.5) | 3.1 (2.8–3.5) |
| Negative likelihood ratio (95% CI) | 0.12 (0.06–0.27) | 0.024 (0.002–0.38) | 0.09 (0.03–0.25) |
| * Case-control study. | |||
| † Designated as regular or irregular. Irregular pulses were categorized into occasional ectopic, frequent ectopics, or continuously irregular. Patients with any irregularity were considered to have a positive index test. | |||
| § Experienced in community and emergency nursing, as well as taking and interpreting ECGs. | |||
| ‡ Data provided by the authors. | |||
Methodological quality of included studies
The study by Morgan and Mant8 fulfilled all the major quality criteria. The studies by Sudlow et al9 and Somerville et al10 were of moderate quality. Sudlow et al did not report an overall sensitivity or specificity, nor the data for calculating these test attributes. The authors kindly provided us the data from their study to calculate the 2×2 table of results.
Prevalence of atrial fibrillation
We calculated the pooled prevalence of atrial fibrillation, excluding data from Somerville et al, as it was a case-control study. The pooled prevalence of atrial fibrillation in the 2 remaining studies was 5.3%, consistent with previous estimates of atrial fibrillation in general practice settings and data from the Framingham cohort.1,11
Accuracy of pulse palpation for detecting atrial fibrillation
The sensitivities in the 3 studies ranged from 91% to 100% and the specificities ranged from 70% to 77%. The pooled sensitivity was 94% (95% CI, 84%–97%) and the pooled specificity was 72% (95% CI, 69%–75%). Low specificity reflects the pervasiveness of other pulse abnormalities, resulting in false-positive test results for atrial fibrillation (TABLE 2).
The pooled positive likelihood ratio was 3.4 (95% CI, 3.2–3.7), showing that pulse palpation was only moderately helpful for ruling in atrial fibrillation. The pooled negative likelihood ratio was 0.11 (95% CI, 0.06–0.20), showing that when no pulse irregularity is detected, the diagnosis of atrial fibrillation can be excluded with reasonable confidence. The chisquare test for heterogeneity for the positive likelihood ratio was 3.87 (df=2; P=.14) and for the negative likelihood ratio was 1.49 (df=2; P=.49), indicating consistency of results between the studies.
TABLE 2
Causes of an irregular pulse
| Sinus arrhythmia |
| Atrial extrasystoles |
| Ventricular extrasystoles |
| Atrial fibrillation |
| Atrial tachycardia with variable response |
| Second-degree heart block |
| Source: Munro and Campbell, eds, MacLeod’s Clinical Examination, 2000.14 |
Discussion
Though an irregularly irregular pulse is a classical clinical sign, we were able to find only 3 published studies evaluating its accuracy in the detection of atrial fibrillation. Study results showed a relatively high sensitivity but poor specificity.
Each study compared the diagnostic accuracy of pulse palpation by nurses in general practice against the reference test, ECG diagnosis by a cardiologist. No information was available on interobserver reliability of pulse palpation.
Working toward reliable screening. Atrial fibrillation is common, serious, and treatable. The initial clinical manifestation of undetected atrial fibrillation might be a dire consequence of the arrhythmia, such as stroke. If a suitably accurate diagnostic test or series of tests were available, it might be effective and cost-effective to screen for the disorder.12 A randomized controlled trial to evaluate such screening (including a comparison of diagnostic strategies) is currently underway.13
Whom to screen in the meantime. It may be worthwhile considering opportunistic testing for atrial fibrillation particularly in patients with ischemic heart disease or heart failure, who are at particularly high risk. Even among these patients, cases of paroxysmal atrial fibrillation may be missed, whether using pulse palpation or ECG. You may therefore want to repeat the test periodically.
CORRESPONDENCE
Jenny Doust, Level 2 Edith Cavell Building, Royal Brisbane Hospital Complex, Herston, Queensland 4029, Australia. E-mail: [email protected]. Previous presentation of work: GP and PHC RED Research Conference 2-4 June 2004, Brisbane, Australia
1. Wheeldon NM, Tayler DI, Anagnostou E, Cook D, Wales C, Oakley GD. Screening for atrial fibrillation in primary care. Heart 1998;79:50-55.
2. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983-988.
3. Lin HJ, Wolf PA, Kelly Hayes M, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke 1996;27:1760-1764.
4. Segal JB, McNamara RL, Miller MR, et al. Anticoagulants or antiplatelet therapy for non-rheumatic atrial fibrillation and flutter. Cochrane Database of Systematic Reviews 2001, Issue 1.
5. van der Weijden T, IJzermans C, Dinant G, van Duijn N, de Vet R, Buntinx F. Identifying relevant diagnostic studies in MEDLINE. The diagnostic value of the erythrocyte sedimentation rate (ESR) and dipstick as an example. Fam Pract 1997;14:204-208.
6. Doust J, Pietrzak E, Sanders S, Glasziou P. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. J Clin Epidemiol 2005;58:444-449.
7. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25.-
8. Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52:373-374,377-380.
9. Sudlow M, Rodgers H, Kenny RA, Thomson R. Identification of patients with atrial fibrillation in general practice: a study of screening methods. BMJ 1998;317:327-328.
10. Somerville S, Somerville J, Croft P, Lewis M. Atrial fibrillation: a comparison of methods to identify cases in general practice. Br J Gen Pract 2000;50:727-729.
11. Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840-844.
12. Sackett D, Haynes R, Guyatt G, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Boston: Little, Brown and Company; 1991.
13. Swancutt D, Hobbs R, Fitzmaurice D, et al. A randomised controlled trial and cost effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in the over 65s: (SAFE) [ISRCTN19633732]. BMC Cardiovasc Disord 2004;4:12.-
14. Munro JF, Campbell IW, eds. MacLeod’s Clinical Examination. 10th ed. Edinburgh: Churchill Livingston, 2000.
- Pulse palpation is a good test for ruling out atrial fibrillation (C).
- Patients with an irregular pulse should be followed up with an ECG.
- Background: Atrial fibrillation in the elderly is common and potentially life threatening. The classical sign of atrial fibrillation is an irregularly irregular pulse.
- Objective: The objective of this research was to determine the accuracy of pulse palpation to detect atrial fibrillation.
- Methods: We searched Medline, EMBASE, and the reference lists of review articles for studies that compared pulse palpation with the electrocardiogram (ECG) diagnosis of atrial fibrillation. Two reviewers independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
- Results: We identified 3 studies (2385 patients) that compared pulse palpation with ECG. The estimated sensitivity of pulse palpation ranged from 91% to 100%, while specificity ranged from 70% to 77%. Pooled sensitivity was 94% (95% confidence interval [CI], 84%–97%) and pooled specificity was 72% (95% CI, 69%–75%). The pooled positive likelihood ratio was 3.39, while the pooled negative likelihood ratio was 0.10.
- Conclusions: Pulse palpation has a high sensitivity but relatively low specificity for atrial fibrillation. It is therefore useful for ruling out atrial fibrillation. It may also be a useful screen to apply opportunistically for previously undetected atrial fibrillation. Assuming a prevalence of 3% for undetected atrial fibrillation in patients older than 65 years, and given the test’s sensitivity and specificity, opportunistic pulse palpation in this age group would detect an irregular pulse in 30% of screened patients, requiring further testing with ECG. Among screened patients, 0.2% would have atrial fibrillation undetected with pulse palpation.
The objective of this review was to determine how well pulse palpation detects the classical sign of atrial fibrillation—an irregularly irregular pulse—and to estimate the test’s false-positive and false-negative rates. You may want to consider using pulse palpation opportunistically with certain high-risk patients identified in this article.
The scope of the problem. Atrial fibrillation in the elderly is common and potentially life-threatening. Its prevalence increases from 2% in the 65- to 69-year-old age group to 8% among those older than 85 years.1
Atrial fibrillation is an independent risk factor for stroke, increasing a person’s risk 3- to 5-fold. While other major risk factors for stroke, such as hypertension, become less important with age, the risk of stroke from atrial fibrillation increases with age.
Stroke attributable to atrial fibrillation increases from 1.5% among patients 50 to 59 years to 23.5% for those aged 80 to 89.2 Furthermore, stroke in the presence of atrial fibrillation is almost twice as likely to be fatal, results in more functional impairment among survivors, and recurs frequently.3
Stroke due to atrial fibrillation results in considerable mortality and morbidity, but treatment of atrial fibrillation reduces the risk. Warfarin reduces the risk of stroke in non-rheumatic atrial fibrillation by about 70%, an annual absolute risk reduction of 3% (number needed to treat: 30), though the benefits are somewhat offset by the risk of bleeding (annual risk of 0.6%).4
Methods
Search strategy and study selection
We searched the Medline and EMBASE electronic databases from 1966 to June 2005 for all studies comparing pulse palpation with ECG diagnosis. There was no restriction on the language of publication.
The search strategy (see Search strategy and inclusion criteria) included terms for pulse, atrial fibrillation, and a search filter for studies of diagnostic accuracy developed by Van der Weijden et al5 that is highly sensitive and precise.6 We also searched the reference lists of all possibly relevant studies, including review articles. We included all studies that tested patients with both pulse palpation and ECG, and that provided data suitable for calculating sensitivity or specificity (or could be provided by the study authors).
Two reviewers (GC and JD) independently screened the electronic lists of citations. We obtained full-text documents of relevant papers and the 2 reviewers independently reviewed the full-text articles for inclusion according to predetermined criteria (see Search strategy and inclusion criteria). The reviewers agreed on all inclusions.
The authors of this study searched Medline, EMBASE, and the reference lists of review articles for studies using the following criteria.
(pulse) OR (‘Pulse’/all subheadings in MIME,MJ ME))
AND ((atrial fibrillation) OR (‘Atrial-Fibrillation’/all subheadings in MIME,MJME))
AND ((‘sensitivity-and-specificity’/all subheadings in MIME,MJME) OR (sensitivity) OR (specificity) OR (‘Diagnosis-Differential’/all subheadings in MIME,MJME) OR (‘False-Negative-Reactions’/all subheadings in MIME,MJME) OR (‘False-Positive-Reactions’/all subheadings in MIME,MJME) OR (‘Mass-Screening’/all subheadings in MIME,MJME) OR (diagnos*) OR (predictive value*) OR (reference value*) OR (ROC*) OR (Likelihood ratio) OR (monitoring) OR (‘Reference-Values’/all subheadings in MIME,MJME)) OR (atrial fibrillation and (SH=diagnosis))
Two reviewers then independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
Inclusion criteria
- Does the study compare pulse palpation to ECG diagnosis of atrial fibrillation?
- Do all the participants receive both tests?
- Are the sensitivity and specificity provided, or calculable from the data provided?
Data extraction and analysis
We assessed study quality with the QUADAS tool.7 Two reviewers assessed study quality and extracted data independently. We calculated the pooled sensitivity and specificity using Metatest (New England Medical Center, Boston, Mass) and the pooled positive and negative likelihood ratios using the Der-Simonian and Laird random effects model of Revman 4.29 (Cochrane Collaboration), which also tests for heterogeneity.
Results
Search results and selection
The search strategy identified 110 citations. Six studies were selected for further assessment for inclusion; 3 met the inclusion criteria and covered 2385 patients (FIGURE). All 3 studies included patients older than 65 years enrolled from general practice clinics, and in each study the pulse was taken by a nurse in the clinic. TABLE 1 summarizes the methodological quality, patient characteristics, and results of the 3 studies.
FIGURE
Studies included in this review
TABLE 1
Detecting atrial fibrillation by pulse palpation: Pertinent studies
| STUDY QUALITY CHARACTERISTICS | MORGAN AND MANT8 | SOMERVILLE ET AL10 | SUDLOW ET AL9 |
| Random or consecutive sampling | Yes | No* | Yes |
| Independent assessment | Yes | Yes | Not stated |
| Blind assessment | Yes | Yes | Not stated |
| Verification by ECG | 100% | 100% | 100% |
| Description of index and reference test | Good | Poor | Poor |
| STUDY CHARACTERISTICS | |||
| Number of patients | 1099 | 86 | 1200 |
| Age | 74.3 (65–100) | 65+ | 65+ |
| Setting | 4 GP practices | Single GP practice | Patients from 9 general practices |
| Location | Southampton, UK | Stoke-on Trent, UK | Southern Northumberland, UK |
| Index test | Radial pulse palpated by a nurse for a minimum of 20 seconds† | Pulse palpated by an experienced nurse.§ Time not specified | Pulse palpated by a nurse. Time not specified |
| Reference test | ECG read by cardiologist | 12-lead ECG read by cardiologist | Limb-lead ECG |
| RESULTS | |||
| Prevalence (%) | 6.1 | 30 | 4.6‡ |
| Sensitivity (%; 95% CI) | 91 (81–96) | 100 (87–100) | 95 (85–98)‡ |
| Specificity (%; 95% CI) | 74 (72–77) | 77 (65–86) | 70 (67–73)‡ |
| Positive likelihood ratio (95% CI) | 3.5 (3.1–4.0) | 4.1 (2.6–6.5) | 3.1 (2.8–3.5) |
| Negative likelihood ratio (95% CI) | 0.12 (0.06–0.27) | 0.024 (0.002–0.38) | 0.09 (0.03–0.25) |
| * Case-control study. | |||
| † Designated as regular or irregular. Irregular pulses were categorized into occasional ectopic, frequent ectopics, or continuously irregular. Patients with any irregularity were considered to have a positive index test. | |||
| § Experienced in community and emergency nursing, as well as taking and interpreting ECGs. | |||
| ‡ Data provided by the authors. | |||
Methodological quality of included studies
The study by Morgan and Mant8 fulfilled all the major quality criteria. The studies by Sudlow et al9 and Somerville et al10 were of moderate quality. Sudlow et al did not report an overall sensitivity or specificity, nor the data for calculating these test attributes. The authors kindly provided us the data from their study to calculate the 2×2 table of results.
Prevalence of atrial fibrillation
We calculated the pooled prevalence of atrial fibrillation, excluding data from Somerville et al, as it was a case-control study. The pooled prevalence of atrial fibrillation in the 2 remaining studies was 5.3%, consistent with previous estimates of atrial fibrillation in general practice settings and data from the Framingham cohort.1,11
Accuracy of pulse palpation for detecting atrial fibrillation
The sensitivities in the 3 studies ranged from 91% to 100% and the specificities ranged from 70% to 77%. The pooled sensitivity was 94% (95% CI, 84%–97%) and the pooled specificity was 72% (95% CI, 69%–75%). Low specificity reflects the pervasiveness of other pulse abnormalities, resulting in false-positive test results for atrial fibrillation (TABLE 2).
The pooled positive likelihood ratio was 3.4 (95% CI, 3.2–3.7), showing that pulse palpation was only moderately helpful for ruling in atrial fibrillation. The pooled negative likelihood ratio was 0.11 (95% CI, 0.06–0.20), showing that when no pulse irregularity is detected, the diagnosis of atrial fibrillation can be excluded with reasonable confidence. The chisquare test for heterogeneity for the positive likelihood ratio was 3.87 (df=2; P=.14) and for the negative likelihood ratio was 1.49 (df=2; P=.49), indicating consistency of results between the studies.
TABLE 2
Causes of an irregular pulse
| Sinus arrhythmia |
| Atrial extrasystoles |
| Ventricular extrasystoles |
| Atrial fibrillation |
| Atrial tachycardia with variable response |
| Second-degree heart block |
| Source: Munro and Campbell, eds, MacLeod’s Clinical Examination, 2000.14 |
Discussion
Though an irregularly irregular pulse is a classical clinical sign, we were able to find only 3 published studies evaluating its accuracy in the detection of atrial fibrillation. Study results showed a relatively high sensitivity but poor specificity.
Each study compared the diagnostic accuracy of pulse palpation by nurses in general practice against the reference test, ECG diagnosis by a cardiologist. No information was available on interobserver reliability of pulse palpation.
Working toward reliable screening. Atrial fibrillation is common, serious, and treatable. The initial clinical manifestation of undetected atrial fibrillation might be a dire consequence of the arrhythmia, such as stroke. If a suitably accurate diagnostic test or series of tests were available, it might be effective and cost-effective to screen for the disorder.12 A randomized controlled trial to evaluate such screening (including a comparison of diagnostic strategies) is currently underway.13
Whom to screen in the meantime. It may be worthwhile considering opportunistic testing for atrial fibrillation particularly in patients with ischemic heart disease or heart failure, who are at particularly high risk. Even among these patients, cases of paroxysmal atrial fibrillation may be missed, whether using pulse palpation or ECG. You may therefore want to repeat the test periodically.
CORRESPONDENCE
Jenny Doust, Level 2 Edith Cavell Building, Royal Brisbane Hospital Complex, Herston, Queensland 4029, Australia. E-mail: [email protected]. Previous presentation of work: GP and PHC RED Research Conference 2-4 June 2004, Brisbane, Australia
- Pulse palpation is a good test for ruling out atrial fibrillation (C).
- Patients with an irregular pulse should be followed up with an ECG.
- Background: Atrial fibrillation in the elderly is common and potentially life threatening. The classical sign of atrial fibrillation is an irregularly irregular pulse.
- Objective: The objective of this research was to determine the accuracy of pulse palpation to detect atrial fibrillation.
- Methods: We searched Medline, EMBASE, and the reference lists of review articles for studies that compared pulse palpation with the electrocardiogram (ECG) diagnosis of atrial fibrillation. Two reviewers independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
- Results: We identified 3 studies (2385 patients) that compared pulse palpation with ECG. The estimated sensitivity of pulse palpation ranged from 91% to 100%, while specificity ranged from 70% to 77%. Pooled sensitivity was 94% (95% confidence interval [CI], 84%–97%) and pooled specificity was 72% (95% CI, 69%–75%). The pooled positive likelihood ratio was 3.39, while the pooled negative likelihood ratio was 0.10.
- Conclusions: Pulse palpation has a high sensitivity but relatively low specificity for atrial fibrillation. It is therefore useful for ruling out atrial fibrillation. It may also be a useful screen to apply opportunistically for previously undetected atrial fibrillation. Assuming a prevalence of 3% for undetected atrial fibrillation in patients older than 65 years, and given the test’s sensitivity and specificity, opportunistic pulse palpation in this age group would detect an irregular pulse in 30% of screened patients, requiring further testing with ECG. Among screened patients, 0.2% would have atrial fibrillation undetected with pulse palpation.
The objective of this review was to determine how well pulse palpation detects the classical sign of atrial fibrillation—an irregularly irregular pulse—and to estimate the test’s false-positive and false-negative rates. You may want to consider using pulse palpation opportunistically with certain high-risk patients identified in this article.
The scope of the problem. Atrial fibrillation in the elderly is common and potentially life-threatening. Its prevalence increases from 2% in the 65- to 69-year-old age group to 8% among those older than 85 years.1
Atrial fibrillation is an independent risk factor for stroke, increasing a person’s risk 3- to 5-fold. While other major risk factors for stroke, such as hypertension, become less important with age, the risk of stroke from atrial fibrillation increases with age.
Stroke attributable to atrial fibrillation increases from 1.5% among patients 50 to 59 years to 23.5% for those aged 80 to 89.2 Furthermore, stroke in the presence of atrial fibrillation is almost twice as likely to be fatal, results in more functional impairment among survivors, and recurs frequently.3
Stroke due to atrial fibrillation results in considerable mortality and morbidity, but treatment of atrial fibrillation reduces the risk. Warfarin reduces the risk of stroke in non-rheumatic atrial fibrillation by about 70%, an annual absolute risk reduction of 3% (number needed to treat: 30), though the benefits are somewhat offset by the risk of bleeding (annual risk of 0.6%).4
Methods
Search strategy and study selection
We searched the Medline and EMBASE electronic databases from 1966 to June 2005 for all studies comparing pulse palpation with ECG diagnosis. There was no restriction on the language of publication.
The search strategy (see Search strategy and inclusion criteria) included terms for pulse, atrial fibrillation, and a search filter for studies of diagnostic accuracy developed by Van der Weijden et al5 that is highly sensitive and precise.6 We also searched the reference lists of all possibly relevant studies, including review articles. We included all studies that tested patients with both pulse palpation and ECG, and that provided data suitable for calculating sensitivity or specificity (or could be provided by the study authors).
Two reviewers (GC and JD) independently screened the electronic lists of citations. We obtained full-text documents of relevant papers and the 2 reviewers independently reviewed the full-text articles for inclusion according to predetermined criteria (see Search strategy and inclusion criteria). The reviewers agreed on all inclusions.
The authors of this study searched Medline, EMBASE, and the reference lists of review articles for studies using the following criteria.
(pulse) OR (‘Pulse’/all subheadings in MIME,MJ ME))
AND ((atrial fibrillation) OR (‘Atrial-Fibrillation’/all subheadings in MIME,MJME))
AND ((‘sensitivity-and-specificity’/all subheadings in MIME,MJME) OR (sensitivity) OR (specificity) OR (‘Diagnosis-Differential’/all subheadings in MIME,MJME) OR (‘False-Negative-Reactions’/all subheadings in MIME,MJME) OR (‘False-Positive-Reactions’/all subheadings in MIME,MJME) OR (‘Mass-Screening’/all subheadings in MIME,MJME) OR (diagnos*) OR (predictive value*) OR (reference value*) OR (ROC*) OR (Likelihood ratio) OR (monitoring) OR (‘Reference-Values’/all subheadings in MIME,MJME)) OR (atrial fibrillation and (SH=diagnosis))
Two reviewers then independently assessed the search results to determine the eligibility of studies, extracted data, and assessed the quality of the studies.
Inclusion criteria
- Does the study compare pulse palpation to ECG diagnosis of atrial fibrillation?
- Do all the participants receive both tests?
- Are the sensitivity and specificity provided, or calculable from the data provided?
Data extraction and analysis
We assessed study quality with the QUADAS tool.7 Two reviewers assessed study quality and extracted data independently. We calculated the pooled sensitivity and specificity using Metatest (New England Medical Center, Boston, Mass) and the pooled positive and negative likelihood ratios using the Der-Simonian and Laird random effects model of Revman 4.29 (Cochrane Collaboration), which also tests for heterogeneity.
Results
Search results and selection
The search strategy identified 110 citations. Six studies were selected for further assessment for inclusion; 3 met the inclusion criteria and covered 2385 patients (FIGURE). All 3 studies included patients older than 65 years enrolled from general practice clinics, and in each study the pulse was taken by a nurse in the clinic. TABLE 1 summarizes the methodological quality, patient characteristics, and results of the 3 studies.
FIGURE
Studies included in this review
TABLE 1
Detecting atrial fibrillation by pulse palpation: Pertinent studies
| STUDY QUALITY CHARACTERISTICS | MORGAN AND MANT8 | SOMERVILLE ET AL10 | SUDLOW ET AL9 |
| Random or consecutive sampling | Yes | No* | Yes |
| Independent assessment | Yes | Yes | Not stated |
| Blind assessment | Yes | Yes | Not stated |
| Verification by ECG | 100% | 100% | 100% |
| Description of index and reference test | Good | Poor | Poor |
| STUDY CHARACTERISTICS | |||
| Number of patients | 1099 | 86 | 1200 |
| Age | 74.3 (65–100) | 65+ | 65+ |
| Setting | 4 GP practices | Single GP practice | Patients from 9 general practices |
| Location | Southampton, UK | Stoke-on Trent, UK | Southern Northumberland, UK |
| Index test | Radial pulse palpated by a nurse for a minimum of 20 seconds† | Pulse palpated by an experienced nurse.§ Time not specified | Pulse palpated by a nurse. Time not specified |
| Reference test | ECG read by cardiologist | 12-lead ECG read by cardiologist | Limb-lead ECG |
| RESULTS | |||
| Prevalence (%) | 6.1 | 30 | 4.6‡ |
| Sensitivity (%; 95% CI) | 91 (81–96) | 100 (87–100) | 95 (85–98)‡ |
| Specificity (%; 95% CI) | 74 (72–77) | 77 (65–86) | 70 (67–73)‡ |
| Positive likelihood ratio (95% CI) | 3.5 (3.1–4.0) | 4.1 (2.6–6.5) | 3.1 (2.8–3.5) |
| Negative likelihood ratio (95% CI) | 0.12 (0.06–0.27) | 0.024 (0.002–0.38) | 0.09 (0.03–0.25) |
| * Case-control study. | |||
| † Designated as regular or irregular. Irregular pulses were categorized into occasional ectopic, frequent ectopics, or continuously irregular. Patients with any irregularity were considered to have a positive index test. | |||
| § Experienced in community and emergency nursing, as well as taking and interpreting ECGs. | |||
| ‡ Data provided by the authors. | |||
Methodological quality of included studies
The study by Morgan and Mant8 fulfilled all the major quality criteria. The studies by Sudlow et al9 and Somerville et al10 were of moderate quality. Sudlow et al did not report an overall sensitivity or specificity, nor the data for calculating these test attributes. The authors kindly provided us the data from their study to calculate the 2×2 table of results.
Prevalence of atrial fibrillation
We calculated the pooled prevalence of atrial fibrillation, excluding data from Somerville et al, as it was a case-control study. The pooled prevalence of atrial fibrillation in the 2 remaining studies was 5.3%, consistent with previous estimates of atrial fibrillation in general practice settings and data from the Framingham cohort.1,11
Accuracy of pulse palpation for detecting atrial fibrillation
The sensitivities in the 3 studies ranged from 91% to 100% and the specificities ranged from 70% to 77%. The pooled sensitivity was 94% (95% CI, 84%–97%) and the pooled specificity was 72% (95% CI, 69%–75%). Low specificity reflects the pervasiveness of other pulse abnormalities, resulting in false-positive test results for atrial fibrillation (TABLE 2).
The pooled positive likelihood ratio was 3.4 (95% CI, 3.2–3.7), showing that pulse palpation was only moderately helpful for ruling in atrial fibrillation. The pooled negative likelihood ratio was 0.11 (95% CI, 0.06–0.20), showing that when no pulse irregularity is detected, the diagnosis of atrial fibrillation can be excluded with reasonable confidence. The chisquare test for heterogeneity for the positive likelihood ratio was 3.87 (df=2; P=.14) and for the negative likelihood ratio was 1.49 (df=2; P=.49), indicating consistency of results between the studies.
TABLE 2
Causes of an irregular pulse
| Sinus arrhythmia |
| Atrial extrasystoles |
| Ventricular extrasystoles |
| Atrial fibrillation |
| Atrial tachycardia with variable response |
| Second-degree heart block |
| Source: Munro and Campbell, eds, MacLeod’s Clinical Examination, 2000.14 |
Discussion
Though an irregularly irregular pulse is a classical clinical sign, we were able to find only 3 published studies evaluating its accuracy in the detection of atrial fibrillation. Study results showed a relatively high sensitivity but poor specificity.
Each study compared the diagnostic accuracy of pulse palpation by nurses in general practice against the reference test, ECG diagnosis by a cardiologist. No information was available on interobserver reliability of pulse palpation.
Working toward reliable screening. Atrial fibrillation is common, serious, and treatable. The initial clinical manifestation of undetected atrial fibrillation might be a dire consequence of the arrhythmia, such as stroke. If a suitably accurate diagnostic test or series of tests were available, it might be effective and cost-effective to screen for the disorder.12 A randomized controlled trial to evaluate such screening (including a comparison of diagnostic strategies) is currently underway.13
Whom to screen in the meantime. It may be worthwhile considering opportunistic testing for atrial fibrillation particularly in patients with ischemic heart disease or heart failure, who are at particularly high risk. Even among these patients, cases of paroxysmal atrial fibrillation may be missed, whether using pulse palpation or ECG. You may therefore want to repeat the test periodically.
CORRESPONDENCE
Jenny Doust, Level 2 Edith Cavell Building, Royal Brisbane Hospital Complex, Herston, Queensland 4029, Australia. E-mail: [email protected]. Previous presentation of work: GP and PHC RED Research Conference 2-4 June 2004, Brisbane, Australia
1. Wheeldon NM, Tayler DI, Anagnostou E, Cook D, Wales C, Oakley GD. Screening for atrial fibrillation in primary care. Heart 1998;79:50-55.
2. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983-988.
3. Lin HJ, Wolf PA, Kelly Hayes M, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke 1996;27:1760-1764.
4. Segal JB, McNamara RL, Miller MR, et al. Anticoagulants or antiplatelet therapy for non-rheumatic atrial fibrillation and flutter. Cochrane Database of Systematic Reviews 2001, Issue 1.
5. van der Weijden T, IJzermans C, Dinant G, van Duijn N, de Vet R, Buntinx F. Identifying relevant diagnostic studies in MEDLINE. The diagnostic value of the erythrocyte sedimentation rate (ESR) and dipstick as an example. Fam Pract 1997;14:204-208.
6. Doust J, Pietrzak E, Sanders S, Glasziou P. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. J Clin Epidemiol 2005;58:444-449.
7. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25.-
8. Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52:373-374,377-380.
9. Sudlow M, Rodgers H, Kenny RA, Thomson R. Identification of patients with atrial fibrillation in general practice: a study of screening methods. BMJ 1998;317:327-328.
10. Somerville S, Somerville J, Croft P, Lewis M. Atrial fibrillation: a comparison of methods to identify cases in general practice. Br J Gen Pract 2000;50:727-729.
11. Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840-844.
12. Sackett D, Haynes R, Guyatt G, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Boston: Little, Brown and Company; 1991.
13. Swancutt D, Hobbs R, Fitzmaurice D, et al. A randomised controlled trial and cost effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in the over 65s: (SAFE) [ISRCTN19633732]. BMC Cardiovasc Disord 2004;4:12.-
14. Munro JF, Campbell IW, eds. MacLeod’s Clinical Examination. 10th ed. Edinburgh: Churchill Livingston, 2000.
1. Wheeldon NM, Tayler DI, Anagnostou E, Cook D, Wales C, Oakley GD. Screening for atrial fibrillation in primary care. Heart 1998;79:50-55.
2. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983-988.
3. Lin HJ, Wolf PA, Kelly Hayes M, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke 1996;27:1760-1764.
4. Segal JB, McNamara RL, Miller MR, et al. Anticoagulants or antiplatelet therapy for non-rheumatic atrial fibrillation and flutter. Cochrane Database of Systematic Reviews 2001, Issue 1.
5. van der Weijden T, IJzermans C, Dinant G, van Duijn N, de Vet R, Buntinx F. Identifying relevant diagnostic studies in MEDLINE. The diagnostic value of the erythrocyte sedimentation rate (ESR) and dipstick as an example. Fam Pract 1997;14:204-208.
6. Doust J, Pietrzak E, Sanders S, Glasziou P. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. J Clin Epidemiol 2005;58:444-449.
7. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25.-
8. Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52:373-374,377-380.
9. Sudlow M, Rodgers H, Kenny RA, Thomson R. Identification of patients with atrial fibrillation in general practice: a study of screening methods. BMJ 1998;317:327-328.
10. Somerville S, Somerville J, Croft P, Lewis M. Atrial fibrillation: a comparison of methods to identify cases in general practice. Br J Gen Pract 2000;50:727-729.
11. Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840-844.
12. Sackett D, Haynes R, Guyatt G, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Boston: Little, Brown and Company; 1991.
13. Swancutt D, Hobbs R, Fitzmaurice D, et al. A randomised controlled trial and cost effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in the over 65s: (SAFE) [ISRCTN19633732]. BMC Cardiovasc Disord 2004;4:12.-
14. Munro JF, Campbell IW, eds. MacLeod’s Clinical Examination. 10th ed. Edinburgh: Churchill Livingston, 2000.