User login
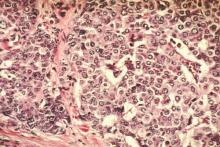
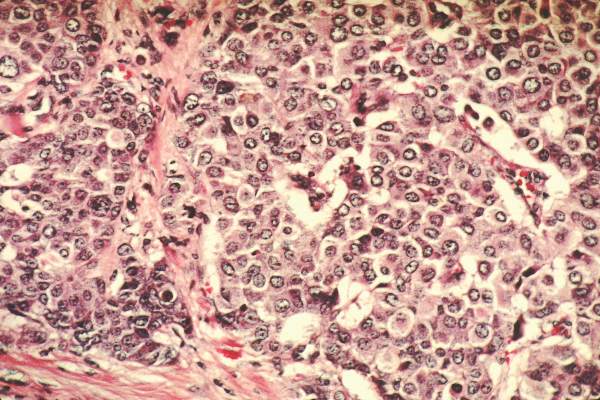
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
Chemotherapy and neoadjuvant chemotherapy are given more often to non-Hispanic black, Hispanic, and Asian women than to non-Hispanic white women with breast cancer, while black women saw a lower rate of pathological complete response (pCR), according to the results of a new study.
Dr. Brigid Killelea of Yale University, New Haven, Conn., and her colleagues looked at records from nearly 280,000 patients in the National Cancer Data Base who received treatment for stage I-III disease in 2010 and 2011.
In the cohort as a whole, 46% of women received chemotherapy, and, among the majority of patients for whom information on the timing of chemotherapy was available, 23% received neoadjuvant therapy, with non-white women receiving chemotherapy and neoadjuvant chemotherapy more frequently (P less than .001). This could mainly be explained by the advanced age, higher-grade tumors and a larger share of triple-negative and human epidermal growth factor receptor–positive tumors in the non-white women, the investigators said (J Clin Oncol. 2015 Nov. 23. doi: 10.1200/JCO.2015.63.7801).
Of about 18,000 patients in the cohort with known outcomes, 33% had a pathological complete response, Dr. Killelea and her colleagues found. Black women in the study had a lower rate of pCR, compared with white women for estrogen receptor/progesterone receptor–negative, human epidermal growth factor receptor2–positive tumors (43% vs. 54%, P = .001) and for triple-negative tumors (37% vs. 43%, P less than .001) despite adjustment for a large number of clinical and socioeconomic factors. Racial disparities in breast cancer incidence, treatment, and survival have been long reported, and racial disparities in neoadjuvant chemotherapy are important to measure, the investigators wrote, as neoadjuvant chemotherapy allows for initiation of systemic therapy before surgery in patients with locally advanced and/or node-positive disease, among other potential advantages. Meanwhile, pCR has been shown in recent years to be a key prognostic indicator for certain breast cancer subtypes and therefore is also important to measure with regard to race. Dr. Killelea and colleagues concluded that the reasons for the lower pCR rates seen among black women in the study could not be determined, and may involve differences in treatment, chemosensitivity, or socioeconomic factors that they could not control for, but that warranted investigation in future studies. “One hypothesis is that the lower pCR rate reflects undertreatment,” the investigators wrote in their analysis. “Women who were unable to complete chemotherapy or had dose reduction, treatment delays, or less-aggressive chemotherapy regimens would be less likely to have a pCR.”
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Non-white Hispanic, Asian, and black women are likelier to receive neoadjuvant chemotherapy than are white women for breast cancers, while black women had lower rates of pathological complete response, compared with white women for some types of cancers.
Major finding: Black women had a lower rate of pCR than did white women for ER/PR-negative, HER2-positive (43% vs. 54%; P = .001) and triple-negative tumors (37% vs. 43%; P less than .001).
Data source: 278,815 women identified in the National Cancer Database diagnosed with stage I-III breast cancer in 2010 and 2011, for whom ethnicity was recorded.
Disclosures: Two authors disclosed relationships with various pharma companies, while the majority reported no relationships to disclose.