User login
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
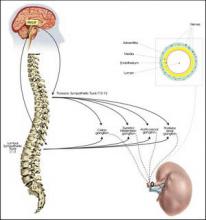
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.
CHICAGO – Deactivating the renal sympathetic nerves via a catheter-based procedure achieved impressively large and durable reductions in blood pressure in the first randomized, multicenter trial of the novel therapy in patients with resistant hypertension.
The renal sympathetic denervation procedure was straightforward and safe, and the sizeable reduction in blood pressure was maintained throughout the scheduled 6 months of follow-up. In patients treated earlier outside of the clinical trial, blood pressures have continued to drift slightly lower through 2.5 years of follow-up, raising the possibility that this procedure provides once-and-for-all treatment, Dr. Murray D. Esler said at the annual scientific sessions of the American Heart Association.
The primary endpoint in the 106-patient Symplicity HTN-2 trial was office-based blood pressure at 6 months. There was a mean 32/12 mm Hg reduction from a baseline of 178/96 mm Hg in patients in the renal denervation arm, all of whom remained on multidrug therapy. Home and ambulatory blood pressure readings followed suit, although the measured reductions were less robust.
In contrast, blood pressure was unchanged over time in patients in the control arm, even though they remained on optimally dosed multidrug antihypertensive therapy, according to Dr. Esler, associate director of the Baker IDI Heart and Diabetes Institute in Melbourne, Australia.
The encouraging results of Symplicity HTN-2 open the door to an entirely new approach to resistant hypertension, one that sidesteps the expense of lifelong therapy with multiple antihypertensive agents, the inherent limited efficacy of the drugs currently available, and compliance issues that commonly arise with multidrug therapy for a silent disease, he added.
Renal denervation therapy could be widely applicable. Roughly 15%-20% of hypertensive patients have resistant hypertension as defined by blood pressures remaining above target in spite of optimal doses of at least three antihypertensive agents, one of which should be a diuretic. This was the population enrolled in Symplicity HTN-2; in fact, nearly two-thirds of participants were on at least five antihypertensive drugs.
Future trials will evaluate renal denervation in milder forms of essential hypertension, as well as in other diseases involving activation of renal sympathetic outflow, including heart failure, cirrhosis with ascites, and chronic kidney disease.
The denervation procedure entails using standard endovascular technique to pass a proprietary radiofrequency catheter via femoral access into the renal artery lumen. The operator then delivers four to six bursts of low-power radiofrequency energy along the length of each renal artery to ablate the renal nerves, located in the adventitia of the renal artery. This results in decreased whole-body noradrenaline spillover, increased renal blood flow, and reduced plasma renin activity, the investigators noted in a published report released online simultaneously with Dr. Elser’s presentation (Lancet Nov. 17, 2010 [doi: 10.1016/S0140-6736(10)62039-9]).
No serious procedure-related complications occurred. Renal function remained unchanged during follow-up, even in patients who had mild to moderate renal impairment at baseline.
Blood pressure reductions of the magnitude achieved in Symplicity HTN-2 could, in theory, be expected to result in roughly 60% decreases in stroke and MI rates in these sorts of very-high-risk patients, according to Dr. Elser and others.
He said that the inspiration for the development of catheter-based renal denervation came from the earlier success of nonselective surgical sympathetectomy as a means of lowering blood pressure in severe hypertension in the days before modern antihypertensive drugs.
"In the current era, drugs blocking the renin-angiotensin system have moved to the fore and the sympathetic nervous system has kind of been swept into the shadows," he noted.
A U.S. clinical trial of the device therapy will begin early next year. Meanwhile, the therapy is being introduced into clinical practice in Australia and Europe. Dr. Elser said he would not be surprised to see a turf battle between interventional cardiologists and interventional radiologists over who performs the procedure.
Discussant Dr. Suzanne Oparil said, "This is an extremely important study. It has a number of great strengths and the potential to really revolutionize the way we deal with treatment-resistant hypertension."
The absence of adverse events, given the fact that 24 centers were involved in the trial, is a remarkable finding that speaks to the procedure’s safety and ease, observed Dr. Oparil, professor of medicine, physiology, and biophysics and director of the vascular biology and hypertension program at the University of Alabama, Birmingham. However, several limitations of the study were of concern, particularly the fact that only 17% of patients were being treated with aldosterone antagonists, which could be an indication that the patient population was not truly drug resistant.
Dr. Esler disclosed that he has received consulting fees and travel expenses from Ardian, which sponsored the Symplicity HTN-2 trial. Dr. Oparil is a consultant to Amylin, Boehringer-Ingelheim, Daiichi Sankyo, Forest Laboratories, Merck, NicOx, Novartis, and VIVUS.