User login
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
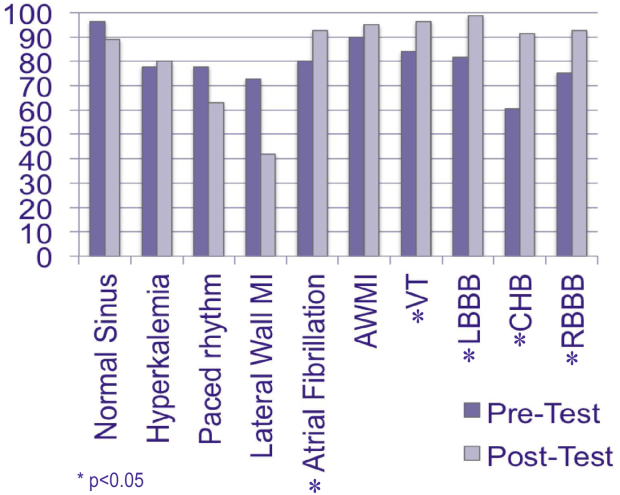
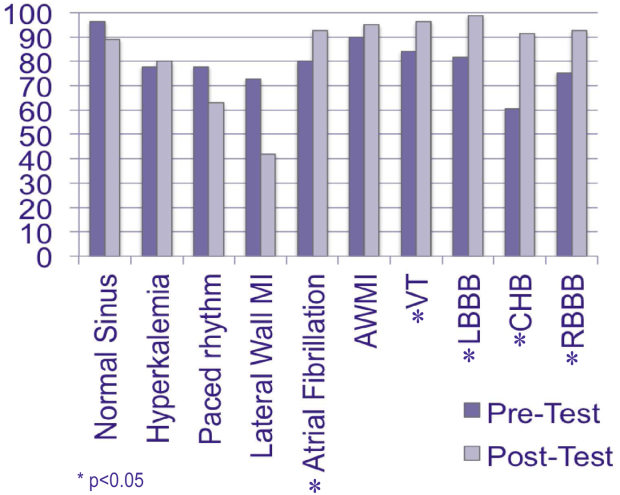
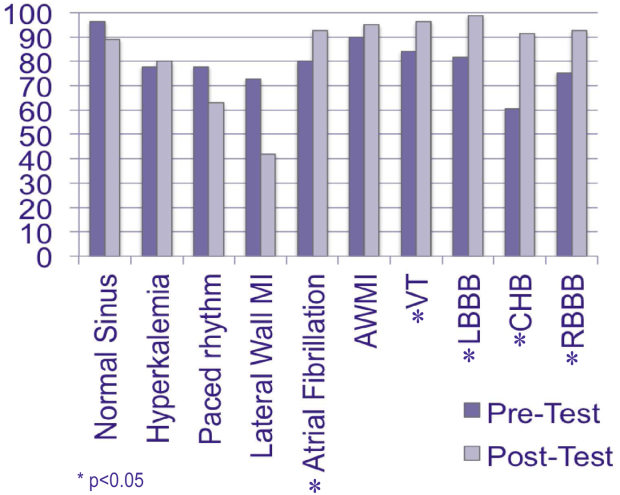
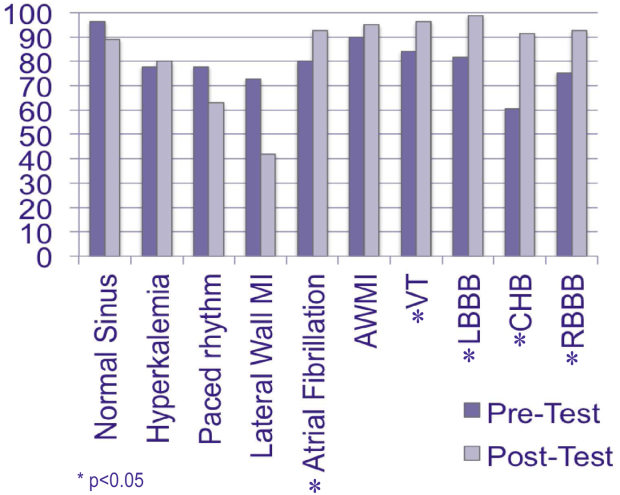
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.