User login
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
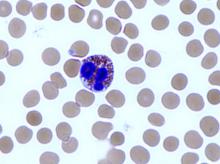
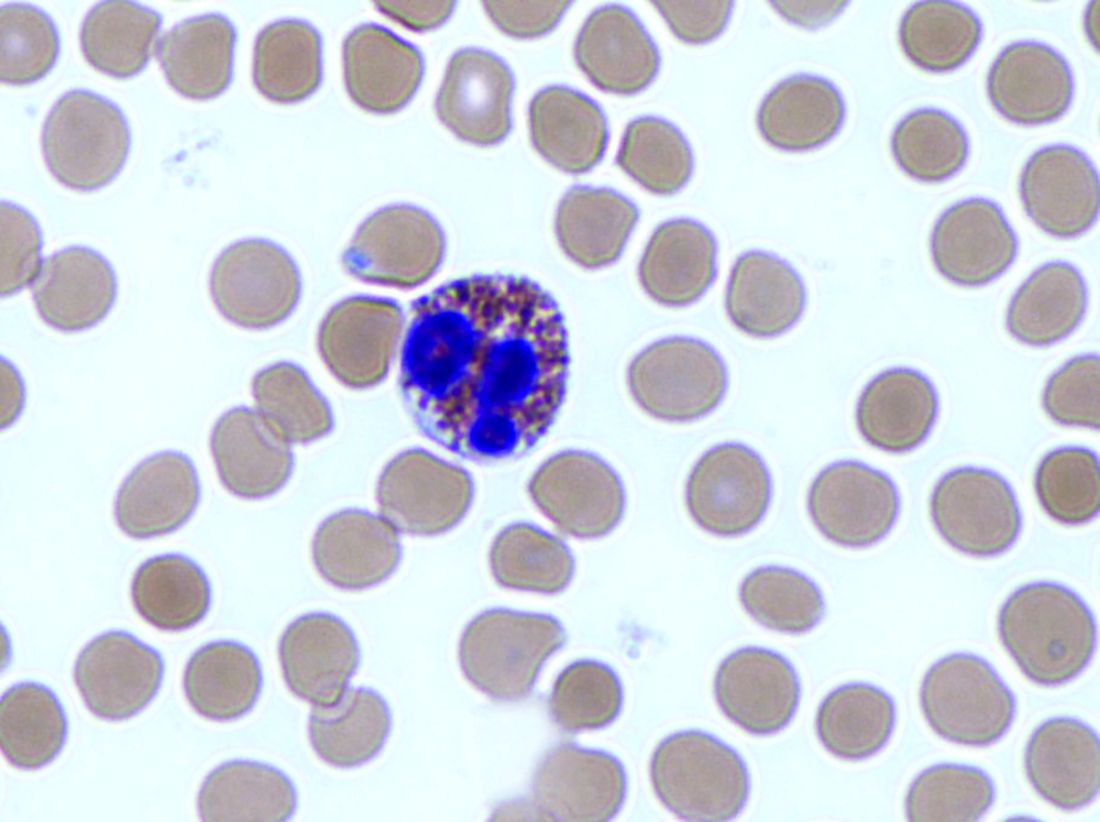
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Persistent eosinophilic inflammation is present in about half of patients with severe asthma, and the studies by Corren and Bjermer represent important advances in learning how to target this inflammatory pathway, Richard Russell, MBBS, MRCP, and Christopher Brightling, PhD, FCCP, wrote in an accompanying editorial (Chest. 2016;150:766-8).
“The most advanced therapeutic target is IL-5, which is an attractive target because it is an obligate cytokine for eosinophil maturation and survival. Its inhibition is thus predicted to reduce bone marrow production of eosinophils and promote apoptosis,” wrote Dr. Russell, a clinical research fellow, and Dr. Brightling, a professor, both at the University of Leicester (England).
“These findings support the view that an elevated blood eosinophil count is associated with a good clinical response [to the antibody reslizumab] but [the studies] did not find a clear correlation between the intensity of the baseline eosinophil count and response,” the colleagues wrote. “Thus, the best cut-off for the blood eosinophil count to apply clinically remains uncertain.”
Clinicians and patients may find a different answer to this riddle than do payers.
“From a patient perspective there is an argument to select a low or no cut-off as there is some benefit even with low baseline eosinophil counts, whereas from a payer’s perspective the health economic benefit is better with a higher cut-off.”
As is often the case, more study will help clarify these new concerns.
“We are moving into a new era of Type-2 immunity-mediated therapies that will bring new opportunities for clinicians and our patients, but with this opportunity comes new challenges. Biomarkers will increase in importance to help drive precision medicine, but we need to understand how to use them, and, in particular, what cut-points to apply. For anti-IL-5 approaches, we probably need to look towards elevated blood eosinophil counts, as aiming for a high cut-off is most likely the best way we shall achieve success.”
Dr. Russell had no financial disclosures. Mr. Brightling reported financial relationships with several pharmaceutical companies, but not with Teva.
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
Reslizumab was most effective in patients with high baseline eosinophil counts, two randomized, placebo-controlled studies have determined. The companion studies were simultaneously published in the October issue of Chest.
The drug reslizumab, an anti–interleukin-5 monoclonal antibody, is made by Teva Branded Pharmaceutical Products R&D, who sponsored both studies.
The larger study, comprising 492 patients, found no significant benefit of reslizumab over placebo, Jonathan Corren, MD, and his colleagues wrote (Chest. 2016;150:799-810). But this study didn’t stratify patients by baseline eosinophil levels; a post-hoc subanalysis found a significant benefit in forced expiratory volume in 69 of the patients who had at least 400 eosinophils/microliter (mcL) when treatment began.
In these patients, the drug significantly improved not only lung function, but asthma symptoms and asthma-related quality of life scores.
“These efficacy findings are consistent with results from other reslizumab trials and combined with the favorable safety profile observed, support the use of reslizumab in patients with asthma and elevated blood eosinophils, uncontrolled by an inhaled corticosteroid-based regimen,” Dr. Bjermer and his coauthors wrote.
The unstratified trial was conducted at 66 sites in the U.S. All of the patients had poorly controlled asthma despite using at least a medium-dosed inhaled corticosteroid. They were randomized to infusions of reslizumab 3.0 mg/kg or placebo given once every 4 weeks for 16 weeks.*
The primary endpoint was the change in forced expiratory volume in one second (FEV1); secondary endpoints included quality of life scores; the need for rescue medication; forced vital capacity; and eosinophil count.
Patients in the placebo and reslizumab groups were an average age of 45.1 years and 44.9 years, respectively. The mean disease duration of patients in both groups was 26 years.
At week 16, the mean change in FEV1 from baseline was 255 ml in the active group and 187 ml in the placebo group – not a significant difference.
The team performed a post-hoc subgroup analysis that dichotomized the cohort based on baseline eosinophil levels. For the 343 with counts of less than 400 cells/mcL, there was no difference in FEV1 at 16 weeks, between the patients who received treatment and the patients who received a placebo. The FEV1s of these two groups were separated by just 33 mL.
The story was different for the 82 patients with at least 400 cells/mcL, with 69 of such patients receiving the drug and 13 of such patients receiving the placebo. At 16 weeks, the difference in FEV1 change was 270 mL, in favor of the active group. The strength of these findings may be weakened by the large difference in size between the treatment and placebo groups and the “near complete lack of response in the small number of placebo-treated patients.”
“Interpretation of the results in the [400 or more cells/mcL] subgroup is limited as the study was not designed or statistically powered to specifically test this group of patients,” the team wrote. Nevertheless, they concluded that reslizumab is a reasonable treatment option for this group. “These findings support an acceptable benefit-risk profile for reslizumab in asthma patients with a blood eosinophil threshold” of at least 400 cells/mcL.
The stratified study examined more endpoints: pre-bronchodilator spirometry (forced expiratory volume in one second FEV1, forced vital capacity, and forced expiratory flow), asthma symptoms, quality of life, rescue inhaler use, and blood eosinophil levels.
The 315 patients in this study all had a baseline eosinophil count of at least 400 cells/mcL. They were randomized to placebo or to 0.3 or 3.0 mg/kg reslizumab dose once every 4 weeks for 16 weeks. The mean ages for the patients taking the placebo, reslizumab 0.3 mg/kg, and reslizumab 3.0 mg/kg were 44.2, 44.5, and 43.0, respectively. The range of average disease durations for patients in the placebo group and two reslizumab groups was 20 to 20.7 years.
The final FEV1 was significantly improved over placebo in both active groups, although the change was much more pronounced in those taking 3.0 mg/kg, compared with those taking 0.3 mg/kg (160 mL and 115 mL, respectively, relative to placebo). Forced vital capacity also improved significantly in the 3.0 mg/kg dose group (130 mL relative to placebo).
Reslizumab was generally well tolerated in both studies. The most frequent adverse events in the stratified study were asthma worsening, headache, nasopharyngitis, upper respiratory infections, and sinusitis.
In the unstratified study, there were two anaphylactic reactions, but only one was related to the study drug. No deaths occurred in either treatment group of this study.
Both trials were sponsored by Teva. Dr. Bjermer has served on advisory boards or provided lectures for Aerocrine, Airsonett, ALK, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Meda, Mundipharma, Nigaard, Novartis, Regeneron, Sanofi-Aventis, Takeda, and Teva. Dr. Corren has been involved in speaker bureau activities for Genentech and Merck; he has served on advisory boards for Genentech, Merck, Novartis, and Vectura.
*CORRECTION 12/9/16: An earlier version of this article misstated the infusion frequency.
[email protected]
On Twitter @Alz_Gal
FROM CHEST
Key clinical point:
Major finding: Forced expiratory volume in 1 second (FEV1) improved by 160 mL with reslizumab 3.0 mg/kg relative to placebo.
Data source: The two randomized, placebo-controlled studies comprised about 800 patients.
Disclosures: Both trials were sponsored by Teva Branded Pharmaceutical Products R&D. Dr. Bjermer has served on an advisory board or provided lectures for Teva. Dr. Corren has served on advisory boards and has been involved in speaker bureau activities for various pharmaceutical companies.