User login
I devoted an entire column to the idea of a citizenship bonus in November 2011. At that time I expressed some ambivalence about its effectiveness. Since then I’ve become disenchanted and think it may do more harm than good.
SHM’s 2016 State of Hospital Medicine (SOHM) Report, based on 2015 data, shows that 46% of Hospital Medicine Groups (HMGs) connect some portion of bonus dollars to a provider’s citizenship.1 This is a relatively new phenomenon in the last 5 years or so. My anecdotal experience is that it isn’t limited to hospitalists; it is pretty common for doctors in any specialty who are employed by a hospital or other large organization.
HMGs vary in their definitions of what constitutes citizenship, but usually include things like committee participation, lectures, grand rounds presentations, community talks, research publications.
Our hospitalist group at my hospital has well-defined criteria that require attendance at more than 75% of meetings as a “light switch” (pays nothing itself, but “turns on” availability to citizenship bonus). Bonus dollars are paid for success in any one of several activities, such as making an in-person visit to two PCP offices or completing a meaningful project related to practice operations or clinical care.
I’ve been a supporter of a citizenship bonus for a long time, but two things have made me ambivalent or even opposed to it. The first is a book by Daniel Pink titled Drive: The Surprising Truth About What Motivates Us. It’s a short and very thought-provoking book summarizing research that suggests the effect of providing external rewards like compensation is to “…extinguish intrinsic motivation, diminish performance, crush creativity, and crowd out good behavior.”
The second reason for my ambivalence is my experience working with a lot of HMGs around the country. Those that have a citizenship bonus don’t seem to realize improved operations, more engaged doctors, or lower turnover, and so on. In fact, my experience is that the bonus tends to do exactly what Pink says – steer individuals and the group as a whole away from what is desired.
I’m not ready to say a citizenship bonus is always a bad idea. But it sure seems like it works out badly for many or most groups.
But if you do have a citizenship bonus, then don’t make the mistake of tying it to very basic expectations of the job, like attending group meetings or completing chart documentation on time. Doing those things should never be seen as a reason for a bonus.
Jeopardy (‘surge’) staffing: Not catching on?
As I write, influenza has swept through our region, and my hospital – like most along the west coast – is experiencing incredibly high volumes. I enter the building through a patient care unit that has been mothballed for several years, but today people from building maintenance were busy getting it ready for patients. The hospital is offering various incentives for patient care staff to work extra shifts to manage this volume surge, and our hospitalists have days with encounters near or at our highest-ever level. So surge capacity is once again on my mind.
But if every hospitalist in the group went from, say, 156 to 190 shifts annually, the practice might be able to staff every day with an additional provider without adding staff or spending more money. And a doc’s average day would be less busy, which for some people (okay, not very many) would be a worthwhile trade-off. I realize this is a tough sell and to many people it sounds crazy.
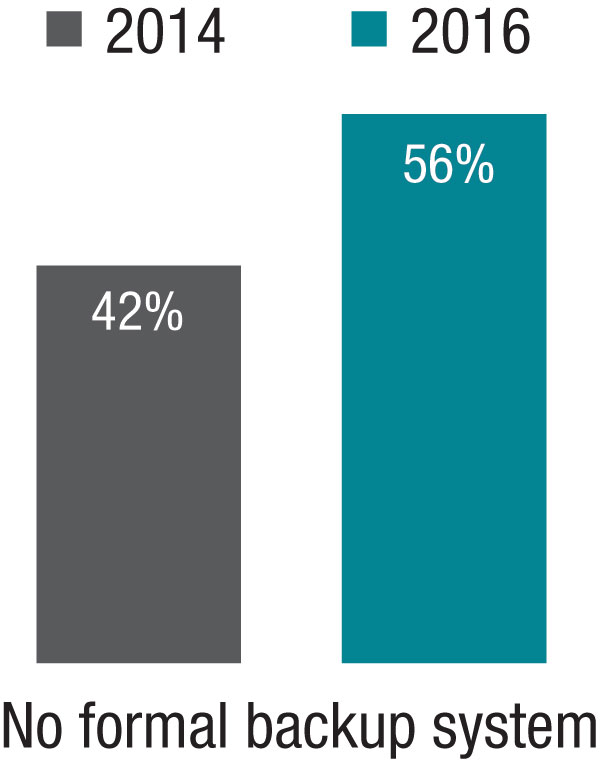
The 2014 SOHM showed 42% of HMGs had “no formal backup system,” and this had climbed to 58% in the 2016 Report. I don’t know if jeopardy or surge backup systems are really becoming less common, but it seems pretty clear they aren’t becoming more common. So it’s worth thinking about whether there is a practical way to remove inhibitors of surge capacity.
Dr. Nelson has been a practicing hospitalist since 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Endnotes
1. Note that this is down from 2014, when 64% of groups reported having a citizenship element in their bonus. But I’m skeptical this is a real trend of decreasing popularity and suspect the drop is mostly explained by a much larger portion of respondents in this particular survey coming from hospitalist management companies which I think much less often have a citizenship bonus.
I devoted an entire column to the idea of a citizenship bonus in November 2011. At that time I expressed some ambivalence about its effectiveness. Since then I’ve become disenchanted and think it may do more harm than good.
SHM’s 2016 State of Hospital Medicine (SOHM) Report, based on 2015 data, shows that 46% of Hospital Medicine Groups (HMGs) connect some portion of bonus dollars to a provider’s citizenship.1 This is a relatively new phenomenon in the last 5 years or so. My anecdotal experience is that it isn’t limited to hospitalists; it is pretty common for doctors in any specialty who are employed by a hospital or other large organization.
HMGs vary in their definitions of what constitutes citizenship, but usually include things like committee participation, lectures, grand rounds presentations, community talks, research publications.
Our hospitalist group at my hospital has well-defined criteria that require attendance at more than 75% of meetings as a “light switch” (pays nothing itself, but “turns on” availability to citizenship bonus). Bonus dollars are paid for success in any one of several activities, such as making an in-person visit to two PCP offices or completing a meaningful project related to practice operations or clinical care.
I’ve been a supporter of a citizenship bonus for a long time, but two things have made me ambivalent or even opposed to it. The first is a book by Daniel Pink titled Drive: The Surprising Truth About What Motivates Us. It’s a short and very thought-provoking book summarizing research that suggests the effect of providing external rewards like compensation is to “…extinguish intrinsic motivation, diminish performance, crush creativity, and crowd out good behavior.”
The second reason for my ambivalence is my experience working with a lot of HMGs around the country. Those that have a citizenship bonus don’t seem to realize improved operations, more engaged doctors, or lower turnover, and so on. In fact, my experience is that the bonus tends to do exactly what Pink says – steer individuals and the group as a whole away from what is desired.
I’m not ready to say a citizenship bonus is always a bad idea. But it sure seems like it works out badly for many or most groups.
But if you do have a citizenship bonus, then don’t make the mistake of tying it to very basic expectations of the job, like attending group meetings or completing chart documentation on time. Doing those things should never be seen as a reason for a bonus.
Jeopardy (‘surge’) staffing: Not catching on?
As I write, influenza has swept through our region, and my hospital – like most along the west coast – is experiencing incredibly high volumes. I enter the building through a patient care unit that has been mothballed for several years, but today people from building maintenance were busy getting it ready for patients. The hospital is offering various incentives for patient care staff to work extra shifts to manage this volume surge, and our hospitalists have days with encounters near or at our highest-ever level. So surge capacity is once again on my mind.
But if every hospitalist in the group went from, say, 156 to 190 shifts annually, the practice might be able to staff every day with an additional provider without adding staff or spending more money. And a doc’s average day would be less busy, which for some people (okay, not very many) would be a worthwhile trade-off. I realize this is a tough sell and to many people it sounds crazy.
The 2014 SOHM showed 42% of HMGs had “no formal backup system,” and this had climbed to 58% in the 2016 Report. I don’t know if jeopardy or surge backup systems are really becoming less common, but it seems pretty clear they aren’t becoming more common. So it’s worth thinking about whether there is a practical way to remove inhibitors of surge capacity.
Dr. Nelson has been a practicing hospitalist since 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Endnotes
1. Note that this is down from 2014, when 64% of groups reported having a citizenship element in their bonus. But I’m skeptical this is a real trend of decreasing popularity and suspect the drop is mostly explained by a much larger portion of respondents in this particular survey coming from hospitalist management companies which I think much less often have a citizenship bonus.
I devoted an entire column to the idea of a citizenship bonus in November 2011. At that time I expressed some ambivalence about its effectiveness. Since then I’ve become disenchanted and think it may do more harm than good.
SHM’s 2016 State of Hospital Medicine (SOHM) Report, based on 2015 data, shows that 46% of Hospital Medicine Groups (HMGs) connect some portion of bonus dollars to a provider’s citizenship.1 This is a relatively new phenomenon in the last 5 years or so. My anecdotal experience is that it isn’t limited to hospitalists; it is pretty common for doctors in any specialty who are employed by a hospital or other large organization.
HMGs vary in their definitions of what constitutes citizenship, but usually include things like committee participation, lectures, grand rounds presentations, community talks, research publications.
Our hospitalist group at my hospital has well-defined criteria that require attendance at more than 75% of meetings as a “light switch” (pays nothing itself, but “turns on” availability to citizenship bonus). Bonus dollars are paid for success in any one of several activities, such as making an in-person visit to two PCP offices or completing a meaningful project related to practice operations or clinical care.
I’ve been a supporter of a citizenship bonus for a long time, but two things have made me ambivalent or even opposed to it. The first is a book by Daniel Pink titled Drive: The Surprising Truth About What Motivates Us. It’s a short and very thought-provoking book summarizing research that suggests the effect of providing external rewards like compensation is to “…extinguish intrinsic motivation, diminish performance, crush creativity, and crowd out good behavior.”
The second reason for my ambivalence is my experience working with a lot of HMGs around the country. Those that have a citizenship bonus don’t seem to realize improved operations, more engaged doctors, or lower turnover, and so on. In fact, my experience is that the bonus tends to do exactly what Pink says – steer individuals and the group as a whole away from what is desired.
I’m not ready to say a citizenship bonus is always a bad idea. But it sure seems like it works out badly for many or most groups.
But if you do have a citizenship bonus, then don’t make the mistake of tying it to very basic expectations of the job, like attending group meetings or completing chart documentation on time. Doing those things should never be seen as a reason for a bonus.
Jeopardy (‘surge’) staffing: Not catching on?
As I write, influenza has swept through our region, and my hospital – like most along the west coast – is experiencing incredibly high volumes. I enter the building through a patient care unit that has been mothballed for several years, but today people from building maintenance were busy getting it ready for patients. The hospital is offering various incentives for patient care staff to work extra shifts to manage this volume surge, and our hospitalists have days with encounters near or at our highest-ever level. So surge capacity is once again on my mind.
But if every hospitalist in the group went from, say, 156 to 190 shifts annually, the practice might be able to staff every day with an additional provider without adding staff or spending more money. And a doc’s average day would be less busy, which for some people (okay, not very many) would be a worthwhile trade-off. I realize this is a tough sell and to many people it sounds crazy.
The 2014 SOHM showed 42% of HMGs had “no formal backup system,” and this had climbed to 58% in the 2016 Report. I don’t know if jeopardy or surge backup systems are really becoming less common, but it seems pretty clear they aren’t becoming more common. So it’s worth thinking about whether there is a practical way to remove inhibitors of surge capacity.
Dr. Nelson has been a practicing hospitalist since 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Endnotes
1. Note that this is down from 2014, when 64% of groups reported having a citizenship element in their bonus. But I’m skeptical this is a real trend of decreasing popularity and suspect the drop is mostly explained by a much larger portion of respondents in this particular survey coming from hospitalist management companies which I think much less often have a citizenship bonus.