User login
PARIS – Use of the Sapien 3 transcatheter heart valve led to similarly favorable short-term and 1-year outcomes in a propensity-matched comparison of patients with bicuspid versus tricuspid aortic stenosis, with
But the higher stroke rate isn’t necessarily a deal breaker for efforts to develop transcatheter aortic valve replacement (TAVR) as an option for patients with bicuspid aortic stenosis, according to Rajendra Makkar, MD, who presented the study results at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Dr. Makkar noted that “75% of the strokes in the bicuspid aortic stenosis group occurred in the periprocedural time period, and these are all heavily calcified valves.” “So I would make the argument that, in young bicuspid patients where you decide to treat using TAVR, the safety gain from using an embolic protection device may be even more [than in most tricuspid patients]. I say that should be the way to do it. I think carefully selected patients with bicuspid aortic stenosis can be managed with TAVR with an embolic protection device very safely.”
He presented the results of this comparison of TAVR outcomes using the Sapien 3 valve in patients with native bicuspid versus tricuspid valves; all patients had enrolled in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry between June 2015 and February 2018. The initial analysis included 1,792 Sapien 3 recipients with severely symptomatic bicuspid aortic stenosis and 55,023 with severely symptomatic tricuspid aortic stenosis.
As TAVR increasingly becomes an option for younger and healthier patients with symptomatic aortic stenosis, operators will encounter more patients with congenital bicuspid valves. Outcomes using early-generation TAVR valves in such patients were poor, so pivotal randomized trials of the Sapien 3 and other contemporary TAVR valves – including the ongoing trials of TAVR versus surgery in patients with low surgical risk – have excluded those with bicuspid aortic stenosis.
As a result, there has been little clinical data to guide interventionalists, so there was an impetus for a study like this one, explained Dr. Makkar, director of interventional cardiology and the cardiac catheterization laboratory at Cedars-Sinai Medical Center in Los Angeles.
In the registry analysis, the unadjusted 1-year all-cause mortality rate was 10.4% in the bicuspid patients and 15% in the tricuspid patients, for a significant 22% relative risk reduction. The 1-year total stroke rates were nearly identical at 3.4% in the bicuspid patients and 3.3% in the tricuspid patients. However, the two groups differed in many key ways. The bicuspid patients were on average 8 years younger, and their mean Society of Thoracic Surgeons risk score was 5.1 versus 6.7 in the tricuspid patients. The bicuspid patients also had less atrial fibrillation, peripheral artery disease, and prior revascularization.
Because of these differences, Dr. Makkar and his coinvestigators carefully propensity-matched the 1,792 bicuspid aortic stenosis who received the Sapien 3 valve at 386 U.S. sites with an equal number of tricuspid aortic stenosis patients treated at 424 sites. This yielded two populations that were virtually identical in terms of age, Society of Thoracic Surgeons score, and 22 other baseline characteristics. Of the patients in both groups, 93%had transfemoral access, 38% had conscious sedation, and the device success rate was in 97%.
Thirty-day outcomes in the two groups didn’t differ significantly except for the total stroke rate: 2.5% in the bicuspid group versus 0.9% in the tricuspid group (see graphic). The 1-year mortality rates didn’t differ significantly: 10.4% in the bicuspid group and 10.8% in the patients with tricuspid disease. However, the 1-year total stroke rate remained significantly higher in the bicuspid group by a margin of 3.4%-2.7%.
The reduction in aortic valve mean gradient and increase in aortic valve area were similar in both groups through 1 year of follow-up, as was the increase in left ventricular ejection fraction. Rates of significant paravalvular leak were similarly low in both groups.
Quality of life as measured by the Kansas City Cardiomyopathy Questionnaire showed what Dr. Makkar called “remarkable” improvement in both groups: There was an average 30-point improvement from baseline at 30 days after TAVR that was sustained through 1 year, at which point the average gain over baseline was 32 points.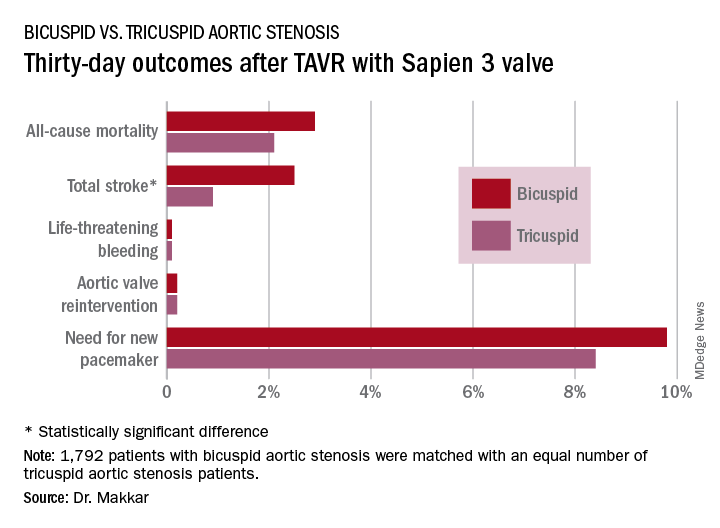
Dr. Makkar drew attention to the impressively low rates of major procedural complications in both groups: Conversion to open-heart surgery took place in 0.9% of the bicuspid and 0.4% of the tricuspid group; annulus rupture occurred in 0.3% of bicuspid TAVR patients and none of the tricuspid group; the aortic dissection rates were 0.3% and 0.1%, respectively; coronary obstruction occurred in 0.4% and 0.1%; and a second valve was needed in 0.6% of the bicuspid group and 0.1% of the tricuspid group. The fact that each of those adverse events happened in fewer than 1% of the bicuspid recipients of the Sapien 3 valve stands in striking contrast to the far higher rates when earlier-generation devices were used in TAVR for bicuspid aortic valves.
“I think our data suggest that in patients with bicuspid aortic stenosis who are at high or intermediate surgical risk, it is really reasonable to actually use TAVR as one of the treatment modalities. And I would make the argument that based on these data it is very reasonable to enroll carefully selected low–surgical risk bicuspid patients in ongoing TAVR versus surgery clinical trials,” the cardiologist said.
Session cochair Alain Cribier, MD, was put off by the higher total stroke rate in the bicuspid group.
“I think, really, that in young patients with a true congenital calcific bicuspid aortic valve, these patients should remain in the hands of the surgeons. In the future, this will be one of the remaining indications for surgery if TAVR works in low-risk patients,” predicted Dr. Cribier, professor of medicine at the University of Rouen (France) and a TAVR pioneer.
Dr. Makkar reported receiving research grants from and serving as a consultant to Edwards Lifesciences, which sponsored the study, as well as from Abbott Laboratories, Pfizer, Medtronic, and Claret Medical.
PARIS – Use of the Sapien 3 transcatheter heart valve led to similarly favorable short-term and 1-year outcomes in a propensity-matched comparison of patients with bicuspid versus tricuspid aortic stenosis, with
But the higher stroke rate isn’t necessarily a deal breaker for efforts to develop transcatheter aortic valve replacement (TAVR) as an option for patients with bicuspid aortic stenosis, according to Rajendra Makkar, MD, who presented the study results at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Dr. Makkar noted that “75% of the strokes in the bicuspid aortic stenosis group occurred in the periprocedural time period, and these are all heavily calcified valves.” “So I would make the argument that, in young bicuspid patients where you decide to treat using TAVR, the safety gain from using an embolic protection device may be even more [than in most tricuspid patients]. I say that should be the way to do it. I think carefully selected patients with bicuspid aortic stenosis can be managed with TAVR with an embolic protection device very safely.”
He presented the results of this comparison of TAVR outcomes using the Sapien 3 valve in patients with native bicuspid versus tricuspid valves; all patients had enrolled in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry between June 2015 and February 2018. The initial analysis included 1,792 Sapien 3 recipients with severely symptomatic bicuspid aortic stenosis and 55,023 with severely symptomatic tricuspid aortic stenosis.
As TAVR increasingly becomes an option for younger and healthier patients with symptomatic aortic stenosis, operators will encounter more patients with congenital bicuspid valves. Outcomes using early-generation TAVR valves in such patients were poor, so pivotal randomized trials of the Sapien 3 and other contemporary TAVR valves – including the ongoing trials of TAVR versus surgery in patients with low surgical risk – have excluded those with bicuspid aortic stenosis.
As a result, there has been little clinical data to guide interventionalists, so there was an impetus for a study like this one, explained Dr. Makkar, director of interventional cardiology and the cardiac catheterization laboratory at Cedars-Sinai Medical Center in Los Angeles.
In the registry analysis, the unadjusted 1-year all-cause mortality rate was 10.4% in the bicuspid patients and 15% in the tricuspid patients, for a significant 22% relative risk reduction. The 1-year total stroke rates were nearly identical at 3.4% in the bicuspid patients and 3.3% in the tricuspid patients. However, the two groups differed in many key ways. The bicuspid patients were on average 8 years younger, and their mean Society of Thoracic Surgeons risk score was 5.1 versus 6.7 in the tricuspid patients. The bicuspid patients also had less atrial fibrillation, peripheral artery disease, and prior revascularization.
Because of these differences, Dr. Makkar and his coinvestigators carefully propensity-matched the 1,792 bicuspid aortic stenosis who received the Sapien 3 valve at 386 U.S. sites with an equal number of tricuspid aortic stenosis patients treated at 424 sites. This yielded two populations that were virtually identical in terms of age, Society of Thoracic Surgeons score, and 22 other baseline characteristics. Of the patients in both groups, 93%had transfemoral access, 38% had conscious sedation, and the device success rate was in 97%.
Thirty-day outcomes in the two groups didn’t differ significantly except for the total stroke rate: 2.5% in the bicuspid group versus 0.9% in the tricuspid group (see graphic). The 1-year mortality rates didn’t differ significantly: 10.4% in the bicuspid group and 10.8% in the patients with tricuspid disease. However, the 1-year total stroke rate remained significantly higher in the bicuspid group by a margin of 3.4%-2.7%.
The reduction in aortic valve mean gradient and increase in aortic valve area were similar in both groups through 1 year of follow-up, as was the increase in left ventricular ejection fraction. Rates of significant paravalvular leak were similarly low in both groups.
Quality of life as measured by the Kansas City Cardiomyopathy Questionnaire showed what Dr. Makkar called “remarkable” improvement in both groups: There was an average 30-point improvement from baseline at 30 days after TAVR that was sustained through 1 year, at which point the average gain over baseline was 32 points.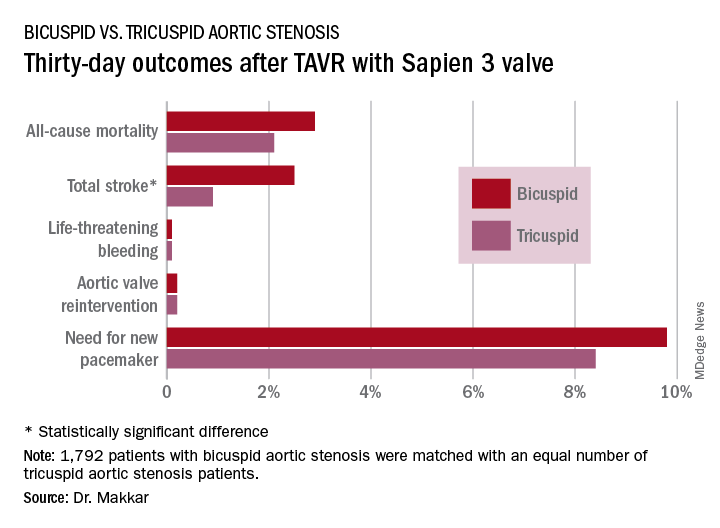
Dr. Makkar drew attention to the impressively low rates of major procedural complications in both groups: Conversion to open-heart surgery took place in 0.9% of the bicuspid and 0.4% of the tricuspid group; annulus rupture occurred in 0.3% of bicuspid TAVR patients and none of the tricuspid group; the aortic dissection rates were 0.3% and 0.1%, respectively; coronary obstruction occurred in 0.4% and 0.1%; and a second valve was needed in 0.6% of the bicuspid group and 0.1% of the tricuspid group. The fact that each of those adverse events happened in fewer than 1% of the bicuspid recipients of the Sapien 3 valve stands in striking contrast to the far higher rates when earlier-generation devices were used in TAVR for bicuspid aortic valves.
“I think our data suggest that in patients with bicuspid aortic stenosis who are at high or intermediate surgical risk, it is really reasonable to actually use TAVR as one of the treatment modalities. And I would make the argument that based on these data it is very reasonable to enroll carefully selected low–surgical risk bicuspid patients in ongoing TAVR versus surgery clinical trials,” the cardiologist said.
Session cochair Alain Cribier, MD, was put off by the higher total stroke rate in the bicuspid group.
“I think, really, that in young patients with a true congenital calcific bicuspid aortic valve, these patients should remain in the hands of the surgeons. In the future, this will be one of the remaining indications for surgery if TAVR works in low-risk patients,” predicted Dr. Cribier, professor of medicine at the University of Rouen (France) and a TAVR pioneer.
Dr. Makkar reported receiving research grants from and serving as a consultant to Edwards Lifesciences, which sponsored the study, as well as from Abbott Laboratories, Pfizer, Medtronic, and Claret Medical.
PARIS – Use of the Sapien 3 transcatheter heart valve led to similarly favorable short-term and 1-year outcomes in a propensity-matched comparison of patients with bicuspid versus tricuspid aortic stenosis, with
But the higher stroke rate isn’t necessarily a deal breaker for efforts to develop transcatheter aortic valve replacement (TAVR) as an option for patients with bicuspid aortic stenosis, according to Rajendra Makkar, MD, who presented the study results at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Dr. Makkar noted that “75% of the strokes in the bicuspid aortic stenosis group occurred in the periprocedural time period, and these are all heavily calcified valves.” “So I would make the argument that, in young bicuspid patients where you decide to treat using TAVR, the safety gain from using an embolic protection device may be even more [than in most tricuspid patients]. I say that should be the way to do it. I think carefully selected patients with bicuspid aortic stenosis can be managed with TAVR with an embolic protection device very safely.”
He presented the results of this comparison of TAVR outcomes using the Sapien 3 valve in patients with native bicuspid versus tricuspid valves; all patients had enrolled in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry between June 2015 and February 2018. The initial analysis included 1,792 Sapien 3 recipients with severely symptomatic bicuspid aortic stenosis and 55,023 with severely symptomatic tricuspid aortic stenosis.
As TAVR increasingly becomes an option for younger and healthier patients with symptomatic aortic stenosis, operators will encounter more patients with congenital bicuspid valves. Outcomes using early-generation TAVR valves in such patients were poor, so pivotal randomized trials of the Sapien 3 and other contemporary TAVR valves – including the ongoing trials of TAVR versus surgery in patients with low surgical risk – have excluded those with bicuspid aortic stenosis.
As a result, there has been little clinical data to guide interventionalists, so there was an impetus for a study like this one, explained Dr. Makkar, director of interventional cardiology and the cardiac catheterization laboratory at Cedars-Sinai Medical Center in Los Angeles.
In the registry analysis, the unadjusted 1-year all-cause mortality rate was 10.4% in the bicuspid patients and 15% in the tricuspid patients, for a significant 22% relative risk reduction. The 1-year total stroke rates were nearly identical at 3.4% in the bicuspid patients and 3.3% in the tricuspid patients. However, the two groups differed in many key ways. The bicuspid patients were on average 8 years younger, and their mean Society of Thoracic Surgeons risk score was 5.1 versus 6.7 in the tricuspid patients. The bicuspid patients also had less atrial fibrillation, peripheral artery disease, and prior revascularization.
Because of these differences, Dr. Makkar and his coinvestigators carefully propensity-matched the 1,792 bicuspid aortic stenosis who received the Sapien 3 valve at 386 U.S. sites with an equal number of tricuspid aortic stenosis patients treated at 424 sites. This yielded two populations that were virtually identical in terms of age, Society of Thoracic Surgeons score, and 22 other baseline characteristics. Of the patients in both groups, 93%had transfemoral access, 38% had conscious sedation, and the device success rate was in 97%.
Thirty-day outcomes in the two groups didn’t differ significantly except for the total stroke rate: 2.5% in the bicuspid group versus 0.9% in the tricuspid group (see graphic). The 1-year mortality rates didn’t differ significantly: 10.4% in the bicuspid group and 10.8% in the patients with tricuspid disease. However, the 1-year total stroke rate remained significantly higher in the bicuspid group by a margin of 3.4%-2.7%.
The reduction in aortic valve mean gradient and increase in aortic valve area were similar in both groups through 1 year of follow-up, as was the increase in left ventricular ejection fraction. Rates of significant paravalvular leak were similarly low in both groups.
Quality of life as measured by the Kansas City Cardiomyopathy Questionnaire showed what Dr. Makkar called “remarkable” improvement in both groups: There was an average 30-point improvement from baseline at 30 days after TAVR that was sustained through 1 year, at which point the average gain over baseline was 32 points.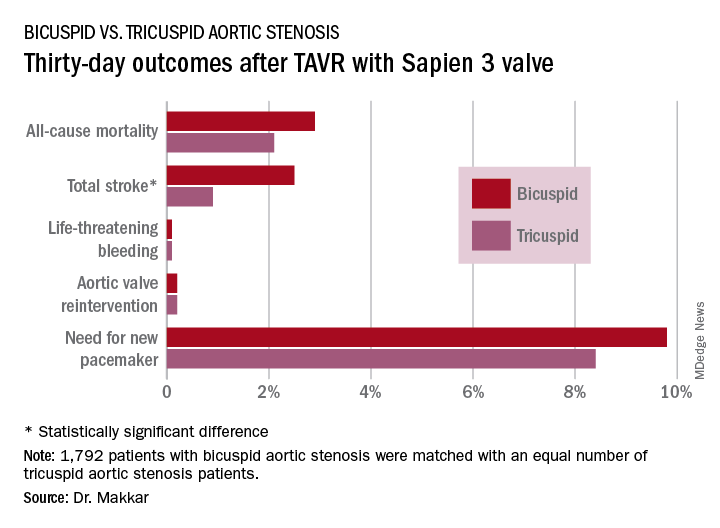
Dr. Makkar drew attention to the impressively low rates of major procedural complications in both groups: Conversion to open-heart surgery took place in 0.9% of the bicuspid and 0.4% of the tricuspid group; annulus rupture occurred in 0.3% of bicuspid TAVR patients and none of the tricuspid group; the aortic dissection rates were 0.3% and 0.1%, respectively; coronary obstruction occurred in 0.4% and 0.1%; and a second valve was needed in 0.6% of the bicuspid group and 0.1% of the tricuspid group. The fact that each of those adverse events happened in fewer than 1% of the bicuspid recipients of the Sapien 3 valve stands in striking contrast to the far higher rates when earlier-generation devices were used in TAVR for bicuspid aortic valves.
“I think our data suggest that in patients with bicuspid aortic stenosis who are at high or intermediate surgical risk, it is really reasonable to actually use TAVR as one of the treatment modalities. And I would make the argument that based on these data it is very reasonable to enroll carefully selected low–surgical risk bicuspid patients in ongoing TAVR versus surgery clinical trials,” the cardiologist said.
Session cochair Alain Cribier, MD, was put off by the higher total stroke rate in the bicuspid group.
“I think, really, that in young patients with a true congenital calcific bicuspid aortic valve, these patients should remain in the hands of the surgeons. In the future, this will be one of the remaining indications for surgery if TAVR works in low-risk patients,” predicted Dr. Cribier, professor of medicine at the University of Rouen (France) and a TAVR pioneer.
Dr. Makkar reported receiving research grants from and serving as a consultant to Edwards Lifesciences, which sponsored the study, as well as from Abbott Laboratories, Pfizer, Medtronic, and Claret Medical.
REPORTING FROM EUROPCR 2018
Key clinical point: Overall, outcomes were similarly favorable between patients with bicuspid aortic stenosis and those with tricuspid aortic stenosis.
Major finding: The 1-year all-cause mortality and total stroke rates in 1,792 TAVR patients who got the Sapien 3 valve for bicuspid aortic stenosis were 10.4% and 3.4%.
Study details: This was a propensity-matched comparison of TAVR outcomes using the Sapien 3 valve in 1,792 patients with bicuspid aortic stenosis and in an equal number with tricuspid aortic stenosis in the STS/ACC TVT Registry.
Disclosures: The study presenter reported receiving research grants from and serving as a consultant to Edwards Lifesciences, which sponsored the study, as well as from Abbott Laboratories, Pfizer, Medtronic, and Claret Medical.

