User login
Success in the United States in reducing morbidity caused by syphilis and gonorrhea has been offset by the rising morbidity seen with other sexually transmitted diseases (STDs), such as chlamydia and herpes. Also, recent increases in the prevalence of syphilis and human immunodeficiency virus (HIV) underscore the fact that sustaining public health successes depends on constant surveillance and a commitment to control efforts.
This Practice Alert focuses on 3 prevalent STDs: syphilis, gonorrhea, and chlamydia—those patients most likely to be infected, and specific developments in screening, diagnosis, and treatment.
Those most likely to be infected
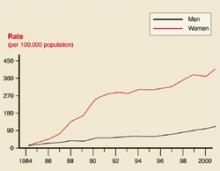
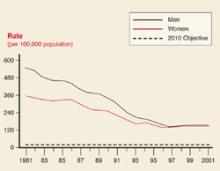
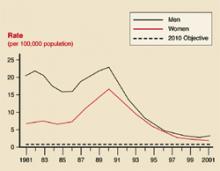
In 2001, 783,000 cases of chlamydia, 362,000 cases of gonorrhea, and 31,600 cases of syphilis were reported to the Centers for Disease Control and Prevention (CDC).1 The true incidence of each disease is unknown. Historical trends in the number of cases reported are reflected in Figures 1 ,2, and 3. In 2001, there was a slight increase in the number of syphilis cases, reversing a 10-year downward trend. The number of chlamydia cases continued to rise, which may reflect improved screening and reporting, while the number of gonorrhea cases continued downward.
FIGURE 1
Chlamydia rates
Chlamydia rates by sex: United States, 1984–2001.
FIGURE 2
Gonorrhea rates
Gonorrhea rates by sex: United States 1981–2001, and the Healthy People year 2010 objective.
FIGURE 3
Syphilis rates
Primary and secondary syphilis rates by sex: United States 1881–2001, and the Healthy People year 2010 objective.
Chlamydia
Infection with Chlamydia trachomatisis reported 4 times as often in women as in men, reflecting better screening of women in family planning programs and during prenatal care.2 The highest rates of chlamydia in women occur in the age groups 15 to 19 years (25/1000) and 20 to 25 years (24/1000). Testing in family planning clinics has yielded chlamydia infection rates of 5.6% among these women.2
Gonorrhea and syphilis
The age groups at highest risk for gonorrhea are 15 to 19 years for women (703/100,000) and 20 to 24 for men (563/100,000).3 For syphilis, the highest risk for women is age 20 to 24 years (3.8/100,000 for primary and secondary syphilis) and 35 to 39 years for men (7.2/100,000).4 There are marked geographic variations in the rates of syphilis (Figure 4). The recent increase in syphilis has been among men, largely attributed to homosexual activity.
FIGURE 4
Syphilis rates by county
Counties with primary and secondary syphilis rates above and below the Healthy People year 2010 objective: United States, 2001.
When and whom to screen
Many STDs persist asymptomatically. These silent infections can cause long-term morbidity such as infertility, pelvic inflammatory disease, ectopic pregnancies, and chronic pelvic pain. Both the United States Preventive Services Task Force and the American Academy of Family Physicians recommend that screening for STDs be performed in specific circumstances (Table 1).9,10
These recommendations should probably be considered a minimum standard, with other groups and diseases included based on the local epidemiology. The local or state health department can be a useful source of information on local epidemiologic patterns and screening and treatment recommendations. Keep in mind that the accuracy of local disease statistics depends on screening and disease reporting by local physicians.
TABLE 1
When and whom to screen for chlamydia, gonorrhea, and syphilis
| Chlamydia | Sexually active women aged 25 years should be routinely tested, and tested during pregnancy at the first prenatal care visit. |
| Other women at high risk* for chlamydia should be routinely tested, and tested during pregnancy at the first prenatal care visit. | |
| Gonorrhea | High-risk women* should be routinely tested, and tested during pregnancy at the first prenatal care visit |
| Syphilis | High-risk women should be routinely tested, and tested during pregnancy at the first prenatal care visit, again in the third trimester, and at delivery. |
| All pregnant women should be tested at the first prenatal care visit. | |
| * Definitions for high risk vary but generally include the following: those with multiple sex partners, other STDs, sexual contact to those with disease, or who exchange sex for money for drugs. | |
Urine screening tests
New nucleic acid amplification tests (NAAT) facilitate screening and diagnosis of chlamydia and gonorrhea with a urine sample. This offers the ease of urine collection in both men and women, with the added benefit of sensitivitiesand specificities equal to those obtained from urethral or endocervical samples. NAATs make possible urine screening in settings where urethral and cervical samples may not be possible because of logistics or patient nonacceptance.
NAATs do not require the presence of live organisms, and only a small number of organisms are needed for accurate test results.
One disadvantage of these tests is an inability to determine antibiotic sensitivities. Another is occasional false-positive results from dead organisms, which can occur if test of cures are performed too soon after treatment (less than 3 weeks).
NAATs can be used on urethral and endocervical swabs as well as urine samples. But they should not be used on oral or rectal samples. Some products test for both gonorrhea and chlamydia in a single specimen. A positive result could be due to either organism, however, requiring more specific testing.
The CDC believes that NAATs on urine samples are acceptable methods of screening for genital gonorrhea and chlamydia in both men and women, although for gonorrhea, cultures of urethral and endocervical swabs are preferred so that sensitivities can be obtained. Gonorrhea and chlamydia cultures are recommended for diagnosing oropharyngeal or anal infection.11
Treatment
Single-dose therapies
A variety of single-dose therapies for STDs are now available (Table 2). Single-dose therapies are convenient for patients, and they encourage quicker completion of therapy. If single-dose therapy is administered in the clinical setting, it is essentially directly observed therapy. Tests of cure can be avoided when common STDs are treated with recommended regimens and completion of treatment is assured.
A disadvantage often of single-dose therapy is its cost. However, when compared with the total costs of incomplete treatments—lower cure rates, return visits, increased infection of contacts—the price of a single-dose agent may seem more acceptable.
Many of the single-dose therapies for gonorrhea are quinolones, which should not be used to treat gonorrhea in (or acquired in) areas with high rates of quinolone resistance (Hawaii, parts of California). Consult your local or state health department to learn the local rates of resistance.
TABLE 2
Single-dose therapies available for common STDs
| Infection | Single-dose therapy |
|---|---|
| Chlamydia | Azithromycin 1 gm (oral) |
| Gonorrhea | Cefixime 400 mg (oral)*† |
| Ceftriaxone 125 mg (intramuscular) | |
| Ciprofloxacin 500 mg (oral) | |
| Ofloxacin 400 mg (oral)† | |
| Levofloxacin 250 mg (oral)† | |
| Nongonococcal urethritis | Azithromycin 1 gm (oral) |
| Syphilis (primary, secondary, early latent) | Benzathene penicillin 2.4 million units (intramuscular) |
| *Cefixime tablets are currently not being manufactured. | |
| †Not recommended for pharyngeal gonorrhea. | |
Management of sex partners
Treatment of patients with STDs is not complete until sex partners who have been exposed are also evaluated, tested, and treated. The common STDs discussed in this article are reportable to local and state health departments. However, in many jurisdictions, cost and staffing limitations prevent public health investigation and contact notification of gonorrhea or chlamydia infections. Family physicians in such locations need to advise their patients to notify sexual contacts of their exposure and recommend that they be examined and treated.
Confidentiality. When patients express concern about having their infections reported to the public health department, reassure them that these departments have a very good record of maintaining patient confidentiality and that public health information is usually afforded a greater degree of protection than information in an office medical record. When public health departments notify sexual contacts of their exposure, they do not reveal who exposed them, although in some instances the sexual contacts can figure this out.
Gonorrhea or chlamydia. The CDC recommends that when a patient is diagnosed with either gonorrhea or chlamydia, all their sex partners from the past 60 days should be evaluated and treated prophylactically.12 Patients and their sex partner(s) should avoid intercourse for 7 days after initiation of treatment and until symptoms resolve.
Syphilis. Syphilis is more complicated. Persons who were exposed to primary, secondary, and early latent syphilis within the 90 days prior to diagnosis should be treated prophylactically. Those exposed from 91 days to 6 months prior to diagnosis of secondary syphilis, or 91 days to 1 year prior to the diagnosis of early latent syphilis, should be treated prophylactically if serology testing is not available or if follow up is uncertain.
Other infections. Current sex partners of those with mucopurulent cervicitis or nongonococcal urethritis should also be evaluated and treated with the same regimen chosen for the index patient. Sex partners within the past 60 days of women with pelvic inflammatory disease should be evaluated and treated prophylactically for both gonorrhea and chlamydia while sex partners within the past 60 days of men with epididymitis should be evaluated but not necessarily treated prophylactically.
As of May 2001,169 million Americans were regular users of the Internet.5 Internet sites created for the purpose of facilitating sexual contact have proliferated and include those for heterosexuals, gay men, lesbians, swingers, and those interested in group sex.6
Use of the Internet to meet sex partners has generated concern in public health circles because of the potential for increased risk of STDs, including HIV/AIDS, from anonymous sex. One case report describes an outbreak of syphilis among gay men who were participants in an Internet chat room for sexual networking.7 Each man with syphilis who was located reported an average of 12 recent sex partners (range of 2–47); a mean of 6 partners (range of 2–15) were located and examined. Four out of the 7 with syphilis were also positive for HIV.
Another study of users of HIVcounseling and testing services found that 16% had sought sex partners on the Internet and 65% of these reported having sex with someone they met on the Internet.8 Internet users reported more previous STDs,more partners, more HIV-positive partners,and more sex with gay men than did non-Internet users.
While much remains to be learned about this topic,these studies indicate that Internet-initiated sex may involve higher risk than sex initiated through other means, although anonymous sex and having multiple sex partners should be considered high-risk activities however they are initiated. Warn patients about these risks.
Collaboration is key to control
The impact of STDs on a community can be moderated when family physicians and local public health departments collaborate. The department’s role includes providing information on the local epidemiology of STDs; assistance in screening, testing, and treating; and, depending on available resources, notifying sexual partners. Many larger public health departments operate a publicly funded STD clinic for patients and sexual contacts who lack financial resources.
Family physicians can screen high-risk persons, use recommended treatment regimens, report communicable diseases as required by state statute, and assist with partner notification by urging patients to cooperate with the local health agency and, if public health partner notification is not available, urging patients to notify their sexual partners.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].
1. Centers for Disease Control and Prevention (CDC). National Center for HIV, STD and TB Prevention. Division of Sexually Transmitted Diseases. 2001 National STD Surveillance Report. Table 1: Cases of sexually transmitted diseases reported by state health departments and rates per 100,000 civilian population: United States, 1941–2001. Available at www.cdc.gov/std/stats/tables/table1.htm. Accessed on October 27, 2003.
2. CDC. Division of Sexually Transmitted Diseases. Chlamydia. Available at www.cdc.gov/std/stats/2001chlamydia.htm. Accessed on October 27, 2003.
3. CDC. Division of Sexually Transmitted Diseases. Gonorrhea. Available at www.cdc.gov/std/stats/2001gonorrhea.htm. Accessed on October 27, 2003.
4. CDC. Division of Sexually Transmitted Diseases. Syphilis. Available at www.cdc.gov/std/stats/2001syphilis.htm. Accessed on October 27, 2003.
5. Available at www.eurmktg.com/globstats.
6. Bull SS, McFarlane M. Soliciting sex on the internet. What are the risks for sexually transmitted diseases and HIV? Sex Transm Dis 2000;27:545-550.
7. Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA 2000;284:447-449.
8. McFarlane M, Bull SS, Rietmeijer CA. The internet as a newly-emerging risk environment for sexually transmitted diseases. JAMA 2000;284:443-446.
9. Agency for Healthcare Research and Quality (AHRCQ). United States Preventive Services Task Force (USPSTF). Screening: chlamydia infection. Available at www.ahcpr.gov/clinic/uspstf/uspschlm.htm. Accessed on October 27, 2003.
10. American Academy of Family Physicians. Introduction to AAFP summary of policy recommendations for periodic health examinations. Available at www.aafp.org/x10601.xml. Accessed on October 27, 2003.
11. CDC. Screening tests to detect chlamydia trachomatis and Neisseria gonorrhea infections. MMWR Recomm Rep 2002;51(RR-15):1-38.
12. CDC. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR6):1-78.
Success in the United States in reducing morbidity caused by syphilis and gonorrhea has been offset by the rising morbidity seen with other sexually transmitted diseases (STDs), such as chlamydia and herpes. Also, recent increases in the prevalence of syphilis and human immunodeficiency virus (HIV) underscore the fact that sustaining public health successes depends on constant surveillance and a commitment to control efforts.
This Practice Alert focuses on 3 prevalent STDs: syphilis, gonorrhea, and chlamydia—those patients most likely to be infected, and specific developments in screening, diagnosis, and treatment.
Those most likely to be infected
In 2001, 783,000 cases of chlamydia, 362,000 cases of gonorrhea, and 31,600 cases of syphilis were reported to the Centers for Disease Control and Prevention (CDC).1 The true incidence of each disease is unknown. Historical trends in the number of cases reported are reflected in Figures 1 ,2, and 3. In 2001, there was a slight increase in the number of syphilis cases, reversing a 10-year downward trend. The number of chlamydia cases continued to rise, which may reflect improved screening and reporting, while the number of gonorrhea cases continued downward.
FIGURE 1
Chlamydia rates
Chlamydia rates by sex: United States, 1984–2001.
FIGURE 2
Gonorrhea rates
Gonorrhea rates by sex: United States 1981–2001, and the Healthy People year 2010 objective.
FIGURE 3
Syphilis rates
Primary and secondary syphilis rates by sex: United States 1881–2001, and the Healthy People year 2010 objective.
Chlamydia
Infection with Chlamydia trachomatisis reported 4 times as often in women as in men, reflecting better screening of women in family planning programs and during prenatal care.2 The highest rates of chlamydia in women occur in the age groups 15 to 19 years (25/1000) and 20 to 25 years (24/1000). Testing in family planning clinics has yielded chlamydia infection rates of 5.6% among these women.2
Gonorrhea and syphilis
The age groups at highest risk for gonorrhea are 15 to 19 years for women (703/100,000) and 20 to 24 for men (563/100,000).3 For syphilis, the highest risk for women is age 20 to 24 years (3.8/100,000 for primary and secondary syphilis) and 35 to 39 years for men (7.2/100,000).4 There are marked geographic variations in the rates of syphilis (Figure 4). The recent increase in syphilis has been among men, largely attributed to homosexual activity.
FIGURE 4
Syphilis rates by county
Counties with primary and secondary syphilis rates above and below the Healthy People year 2010 objective: United States, 2001.
When and whom to screen
Many STDs persist asymptomatically. These silent infections can cause long-term morbidity such as infertility, pelvic inflammatory disease, ectopic pregnancies, and chronic pelvic pain. Both the United States Preventive Services Task Force and the American Academy of Family Physicians recommend that screening for STDs be performed in specific circumstances (Table 1).9,10
These recommendations should probably be considered a minimum standard, with other groups and diseases included based on the local epidemiology. The local or state health department can be a useful source of information on local epidemiologic patterns and screening and treatment recommendations. Keep in mind that the accuracy of local disease statistics depends on screening and disease reporting by local physicians.
TABLE 1
When and whom to screen for chlamydia, gonorrhea, and syphilis
| Chlamydia | Sexually active women aged 25 years should be routinely tested, and tested during pregnancy at the first prenatal care visit. |
| Other women at high risk* for chlamydia should be routinely tested, and tested during pregnancy at the first prenatal care visit. | |
| Gonorrhea | High-risk women* should be routinely tested, and tested during pregnancy at the first prenatal care visit |
| Syphilis | High-risk women should be routinely tested, and tested during pregnancy at the first prenatal care visit, again in the third trimester, and at delivery. |
| All pregnant women should be tested at the first prenatal care visit. | |
| * Definitions for high risk vary but generally include the following: those with multiple sex partners, other STDs, sexual contact to those with disease, or who exchange sex for money for drugs. | |
Urine screening tests
New nucleic acid amplification tests (NAAT) facilitate screening and diagnosis of chlamydia and gonorrhea with a urine sample. This offers the ease of urine collection in both men and women, with the added benefit of sensitivitiesand specificities equal to those obtained from urethral or endocervical samples. NAATs make possible urine screening in settings where urethral and cervical samples may not be possible because of logistics or patient nonacceptance.
NAATs do not require the presence of live organisms, and only a small number of organisms are needed for accurate test results.
One disadvantage of these tests is an inability to determine antibiotic sensitivities. Another is occasional false-positive results from dead organisms, which can occur if test of cures are performed too soon after treatment (less than 3 weeks).
NAATs can be used on urethral and endocervical swabs as well as urine samples. But they should not be used on oral or rectal samples. Some products test for both gonorrhea and chlamydia in a single specimen. A positive result could be due to either organism, however, requiring more specific testing.
The CDC believes that NAATs on urine samples are acceptable methods of screening for genital gonorrhea and chlamydia in both men and women, although for gonorrhea, cultures of urethral and endocervical swabs are preferred so that sensitivities can be obtained. Gonorrhea and chlamydia cultures are recommended for diagnosing oropharyngeal or anal infection.11
Treatment
Single-dose therapies
A variety of single-dose therapies for STDs are now available (Table 2). Single-dose therapies are convenient for patients, and they encourage quicker completion of therapy. If single-dose therapy is administered in the clinical setting, it is essentially directly observed therapy. Tests of cure can be avoided when common STDs are treated with recommended regimens and completion of treatment is assured.
A disadvantage often of single-dose therapy is its cost. However, when compared with the total costs of incomplete treatments—lower cure rates, return visits, increased infection of contacts—the price of a single-dose agent may seem more acceptable.
Many of the single-dose therapies for gonorrhea are quinolones, which should not be used to treat gonorrhea in (or acquired in) areas with high rates of quinolone resistance (Hawaii, parts of California). Consult your local or state health department to learn the local rates of resistance.
TABLE 2
Single-dose therapies available for common STDs
| Infection | Single-dose therapy |
|---|---|
| Chlamydia | Azithromycin 1 gm (oral) |
| Gonorrhea | Cefixime 400 mg (oral)*† |
| Ceftriaxone 125 mg (intramuscular) | |
| Ciprofloxacin 500 mg (oral) | |
| Ofloxacin 400 mg (oral)† | |
| Levofloxacin 250 mg (oral)† | |
| Nongonococcal urethritis | Azithromycin 1 gm (oral) |
| Syphilis (primary, secondary, early latent) | Benzathene penicillin 2.4 million units (intramuscular) |
| *Cefixime tablets are currently not being manufactured. | |
| †Not recommended for pharyngeal gonorrhea. | |
Management of sex partners
Treatment of patients with STDs is not complete until sex partners who have been exposed are also evaluated, tested, and treated. The common STDs discussed in this article are reportable to local and state health departments. However, in many jurisdictions, cost and staffing limitations prevent public health investigation and contact notification of gonorrhea or chlamydia infections. Family physicians in such locations need to advise their patients to notify sexual contacts of their exposure and recommend that they be examined and treated.
Confidentiality. When patients express concern about having their infections reported to the public health department, reassure them that these departments have a very good record of maintaining patient confidentiality and that public health information is usually afforded a greater degree of protection than information in an office medical record. When public health departments notify sexual contacts of their exposure, they do not reveal who exposed them, although in some instances the sexual contacts can figure this out.
Gonorrhea or chlamydia. The CDC recommends that when a patient is diagnosed with either gonorrhea or chlamydia, all their sex partners from the past 60 days should be evaluated and treated prophylactically.12 Patients and their sex partner(s) should avoid intercourse for 7 days after initiation of treatment and until symptoms resolve.
Syphilis. Syphilis is more complicated. Persons who were exposed to primary, secondary, and early latent syphilis within the 90 days prior to diagnosis should be treated prophylactically. Those exposed from 91 days to 6 months prior to diagnosis of secondary syphilis, or 91 days to 1 year prior to the diagnosis of early latent syphilis, should be treated prophylactically if serology testing is not available or if follow up is uncertain.
Other infections. Current sex partners of those with mucopurulent cervicitis or nongonococcal urethritis should also be evaluated and treated with the same regimen chosen for the index patient. Sex partners within the past 60 days of women with pelvic inflammatory disease should be evaluated and treated prophylactically for both gonorrhea and chlamydia while sex partners within the past 60 days of men with epididymitis should be evaluated but not necessarily treated prophylactically.
As of May 2001,169 million Americans were regular users of the Internet.5 Internet sites created for the purpose of facilitating sexual contact have proliferated and include those for heterosexuals, gay men, lesbians, swingers, and those interested in group sex.6
Use of the Internet to meet sex partners has generated concern in public health circles because of the potential for increased risk of STDs, including HIV/AIDS, from anonymous sex. One case report describes an outbreak of syphilis among gay men who were participants in an Internet chat room for sexual networking.7 Each man with syphilis who was located reported an average of 12 recent sex partners (range of 2–47); a mean of 6 partners (range of 2–15) were located and examined. Four out of the 7 with syphilis were also positive for HIV.
Another study of users of HIVcounseling and testing services found that 16% had sought sex partners on the Internet and 65% of these reported having sex with someone they met on the Internet.8 Internet users reported more previous STDs,more partners, more HIV-positive partners,and more sex with gay men than did non-Internet users.
While much remains to be learned about this topic,these studies indicate that Internet-initiated sex may involve higher risk than sex initiated through other means, although anonymous sex and having multiple sex partners should be considered high-risk activities however they are initiated. Warn patients about these risks.
Collaboration is key to control
The impact of STDs on a community can be moderated when family physicians and local public health departments collaborate. The department’s role includes providing information on the local epidemiology of STDs; assistance in screening, testing, and treating; and, depending on available resources, notifying sexual partners. Many larger public health departments operate a publicly funded STD clinic for patients and sexual contacts who lack financial resources.
Family physicians can screen high-risk persons, use recommended treatment regimens, report communicable diseases as required by state statute, and assist with partner notification by urging patients to cooperate with the local health agency and, if public health partner notification is not available, urging patients to notify their sexual partners.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].
Success in the United States in reducing morbidity caused by syphilis and gonorrhea has been offset by the rising morbidity seen with other sexually transmitted diseases (STDs), such as chlamydia and herpes. Also, recent increases in the prevalence of syphilis and human immunodeficiency virus (HIV) underscore the fact that sustaining public health successes depends on constant surveillance and a commitment to control efforts.
This Practice Alert focuses on 3 prevalent STDs: syphilis, gonorrhea, and chlamydia—those patients most likely to be infected, and specific developments in screening, diagnosis, and treatment.
Those most likely to be infected
In 2001, 783,000 cases of chlamydia, 362,000 cases of gonorrhea, and 31,600 cases of syphilis were reported to the Centers for Disease Control and Prevention (CDC).1 The true incidence of each disease is unknown. Historical trends in the number of cases reported are reflected in Figures 1 ,2, and 3. In 2001, there was a slight increase in the number of syphilis cases, reversing a 10-year downward trend. The number of chlamydia cases continued to rise, which may reflect improved screening and reporting, while the number of gonorrhea cases continued downward.
FIGURE 1
Chlamydia rates
Chlamydia rates by sex: United States, 1984–2001.
FIGURE 2
Gonorrhea rates
Gonorrhea rates by sex: United States 1981–2001, and the Healthy People year 2010 objective.
FIGURE 3
Syphilis rates
Primary and secondary syphilis rates by sex: United States 1881–2001, and the Healthy People year 2010 objective.
Chlamydia
Infection with Chlamydia trachomatisis reported 4 times as often in women as in men, reflecting better screening of women in family planning programs and during prenatal care.2 The highest rates of chlamydia in women occur in the age groups 15 to 19 years (25/1000) and 20 to 25 years (24/1000). Testing in family planning clinics has yielded chlamydia infection rates of 5.6% among these women.2
Gonorrhea and syphilis
The age groups at highest risk for gonorrhea are 15 to 19 years for women (703/100,000) and 20 to 24 for men (563/100,000).3 For syphilis, the highest risk for women is age 20 to 24 years (3.8/100,000 for primary and secondary syphilis) and 35 to 39 years for men (7.2/100,000).4 There are marked geographic variations in the rates of syphilis (Figure 4). The recent increase in syphilis has been among men, largely attributed to homosexual activity.
FIGURE 4
Syphilis rates by county
Counties with primary and secondary syphilis rates above and below the Healthy People year 2010 objective: United States, 2001.
When and whom to screen
Many STDs persist asymptomatically. These silent infections can cause long-term morbidity such as infertility, pelvic inflammatory disease, ectopic pregnancies, and chronic pelvic pain. Both the United States Preventive Services Task Force and the American Academy of Family Physicians recommend that screening for STDs be performed in specific circumstances (Table 1).9,10
These recommendations should probably be considered a minimum standard, with other groups and diseases included based on the local epidemiology. The local or state health department can be a useful source of information on local epidemiologic patterns and screening and treatment recommendations. Keep in mind that the accuracy of local disease statistics depends on screening and disease reporting by local physicians.
TABLE 1
When and whom to screen for chlamydia, gonorrhea, and syphilis
| Chlamydia | Sexually active women aged 25 years should be routinely tested, and tested during pregnancy at the first prenatal care visit. |
| Other women at high risk* for chlamydia should be routinely tested, and tested during pregnancy at the first prenatal care visit. | |
| Gonorrhea | High-risk women* should be routinely tested, and tested during pregnancy at the first prenatal care visit |
| Syphilis | High-risk women should be routinely tested, and tested during pregnancy at the first prenatal care visit, again in the third trimester, and at delivery. |
| All pregnant women should be tested at the first prenatal care visit. | |
| * Definitions for high risk vary but generally include the following: those with multiple sex partners, other STDs, sexual contact to those with disease, or who exchange sex for money for drugs. | |
Urine screening tests
New nucleic acid amplification tests (NAAT) facilitate screening and diagnosis of chlamydia and gonorrhea with a urine sample. This offers the ease of urine collection in both men and women, with the added benefit of sensitivitiesand specificities equal to those obtained from urethral or endocervical samples. NAATs make possible urine screening in settings where urethral and cervical samples may not be possible because of logistics or patient nonacceptance.
NAATs do not require the presence of live organisms, and only a small number of organisms are needed for accurate test results.
One disadvantage of these tests is an inability to determine antibiotic sensitivities. Another is occasional false-positive results from dead organisms, which can occur if test of cures are performed too soon after treatment (less than 3 weeks).
NAATs can be used on urethral and endocervical swabs as well as urine samples. But they should not be used on oral or rectal samples. Some products test for both gonorrhea and chlamydia in a single specimen. A positive result could be due to either organism, however, requiring more specific testing.
The CDC believes that NAATs on urine samples are acceptable methods of screening for genital gonorrhea and chlamydia in both men and women, although for gonorrhea, cultures of urethral and endocervical swabs are preferred so that sensitivities can be obtained. Gonorrhea and chlamydia cultures are recommended for diagnosing oropharyngeal or anal infection.11
Treatment
Single-dose therapies
A variety of single-dose therapies for STDs are now available (Table 2). Single-dose therapies are convenient for patients, and they encourage quicker completion of therapy. If single-dose therapy is administered in the clinical setting, it is essentially directly observed therapy. Tests of cure can be avoided when common STDs are treated with recommended regimens and completion of treatment is assured.
A disadvantage often of single-dose therapy is its cost. However, when compared with the total costs of incomplete treatments—lower cure rates, return visits, increased infection of contacts—the price of a single-dose agent may seem more acceptable.
Many of the single-dose therapies for gonorrhea are quinolones, which should not be used to treat gonorrhea in (or acquired in) areas with high rates of quinolone resistance (Hawaii, parts of California). Consult your local or state health department to learn the local rates of resistance.
TABLE 2
Single-dose therapies available for common STDs
| Infection | Single-dose therapy |
|---|---|
| Chlamydia | Azithromycin 1 gm (oral) |
| Gonorrhea | Cefixime 400 mg (oral)*† |
| Ceftriaxone 125 mg (intramuscular) | |
| Ciprofloxacin 500 mg (oral) | |
| Ofloxacin 400 mg (oral)† | |
| Levofloxacin 250 mg (oral)† | |
| Nongonococcal urethritis | Azithromycin 1 gm (oral) |
| Syphilis (primary, secondary, early latent) | Benzathene penicillin 2.4 million units (intramuscular) |
| *Cefixime tablets are currently not being manufactured. | |
| †Not recommended for pharyngeal gonorrhea. | |
Management of sex partners
Treatment of patients with STDs is not complete until sex partners who have been exposed are also evaluated, tested, and treated. The common STDs discussed in this article are reportable to local and state health departments. However, in many jurisdictions, cost and staffing limitations prevent public health investigation and contact notification of gonorrhea or chlamydia infections. Family physicians in such locations need to advise their patients to notify sexual contacts of their exposure and recommend that they be examined and treated.
Confidentiality. When patients express concern about having their infections reported to the public health department, reassure them that these departments have a very good record of maintaining patient confidentiality and that public health information is usually afforded a greater degree of protection than information in an office medical record. When public health departments notify sexual contacts of their exposure, they do not reveal who exposed them, although in some instances the sexual contacts can figure this out.
Gonorrhea or chlamydia. The CDC recommends that when a patient is diagnosed with either gonorrhea or chlamydia, all their sex partners from the past 60 days should be evaluated and treated prophylactically.12 Patients and their sex partner(s) should avoid intercourse for 7 days after initiation of treatment and until symptoms resolve.
Syphilis. Syphilis is more complicated. Persons who were exposed to primary, secondary, and early latent syphilis within the 90 days prior to diagnosis should be treated prophylactically. Those exposed from 91 days to 6 months prior to diagnosis of secondary syphilis, or 91 days to 1 year prior to the diagnosis of early latent syphilis, should be treated prophylactically if serology testing is not available or if follow up is uncertain.
Other infections. Current sex partners of those with mucopurulent cervicitis or nongonococcal urethritis should also be evaluated and treated with the same regimen chosen for the index patient. Sex partners within the past 60 days of women with pelvic inflammatory disease should be evaluated and treated prophylactically for both gonorrhea and chlamydia while sex partners within the past 60 days of men with epididymitis should be evaluated but not necessarily treated prophylactically.
As of May 2001,169 million Americans were regular users of the Internet.5 Internet sites created for the purpose of facilitating sexual contact have proliferated and include those for heterosexuals, gay men, lesbians, swingers, and those interested in group sex.6
Use of the Internet to meet sex partners has generated concern in public health circles because of the potential for increased risk of STDs, including HIV/AIDS, from anonymous sex. One case report describes an outbreak of syphilis among gay men who were participants in an Internet chat room for sexual networking.7 Each man with syphilis who was located reported an average of 12 recent sex partners (range of 2–47); a mean of 6 partners (range of 2–15) were located and examined. Four out of the 7 with syphilis were also positive for HIV.
Another study of users of HIVcounseling and testing services found that 16% had sought sex partners on the Internet and 65% of these reported having sex with someone they met on the Internet.8 Internet users reported more previous STDs,more partners, more HIV-positive partners,and more sex with gay men than did non-Internet users.
While much remains to be learned about this topic,these studies indicate that Internet-initiated sex may involve higher risk than sex initiated through other means, although anonymous sex and having multiple sex partners should be considered high-risk activities however they are initiated. Warn patients about these risks.
Collaboration is key to control
The impact of STDs on a community can be moderated when family physicians and local public health departments collaborate. The department’s role includes providing information on the local epidemiology of STDs; assistance in screening, testing, and treating; and, depending on available resources, notifying sexual partners. Many larger public health departments operate a publicly funded STD clinic for patients and sexual contacts who lack financial resources.
Family physicians can screen high-risk persons, use recommended treatment regimens, report communicable diseases as required by state statute, and assist with partner notification by urging patients to cooperate with the local health agency and, if public health partner notification is not available, urging patients to notify their sexual partners.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].
1. Centers for Disease Control and Prevention (CDC). National Center for HIV, STD and TB Prevention. Division of Sexually Transmitted Diseases. 2001 National STD Surveillance Report. Table 1: Cases of sexually transmitted diseases reported by state health departments and rates per 100,000 civilian population: United States, 1941–2001. Available at www.cdc.gov/std/stats/tables/table1.htm. Accessed on October 27, 2003.
2. CDC. Division of Sexually Transmitted Diseases. Chlamydia. Available at www.cdc.gov/std/stats/2001chlamydia.htm. Accessed on October 27, 2003.
3. CDC. Division of Sexually Transmitted Diseases. Gonorrhea. Available at www.cdc.gov/std/stats/2001gonorrhea.htm. Accessed on October 27, 2003.
4. CDC. Division of Sexually Transmitted Diseases. Syphilis. Available at www.cdc.gov/std/stats/2001syphilis.htm. Accessed on October 27, 2003.
5. Available at www.eurmktg.com/globstats.
6. Bull SS, McFarlane M. Soliciting sex on the internet. What are the risks for sexually transmitted diseases and HIV? Sex Transm Dis 2000;27:545-550.
7. Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA 2000;284:447-449.
8. McFarlane M, Bull SS, Rietmeijer CA. The internet as a newly-emerging risk environment for sexually transmitted diseases. JAMA 2000;284:443-446.
9. Agency for Healthcare Research and Quality (AHRCQ). United States Preventive Services Task Force (USPSTF). Screening: chlamydia infection. Available at www.ahcpr.gov/clinic/uspstf/uspschlm.htm. Accessed on October 27, 2003.
10. American Academy of Family Physicians. Introduction to AAFP summary of policy recommendations for periodic health examinations. Available at www.aafp.org/x10601.xml. Accessed on October 27, 2003.
11. CDC. Screening tests to detect chlamydia trachomatis and Neisseria gonorrhea infections. MMWR Recomm Rep 2002;51(RR-15):1-38.
12. CDC. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR6):1-78.
1. Centers for Disease Control and Prevention (CDC). National Center for HIV, STD and TB Prevention. Division of Sexually Transmitted Diseases. 2001 National STD Surveillance Report. Table 1: Cases of sexually transmitted diseases reported by state health departments and rates per 100,000 civilian population: United States, 1941–2001. Available at www.cdc.gov/std/stats/tables/table1.htm. Accessed on October 27, 2003.
2. CDC. Division of Sexually Transmitted Diseases. Chlamydia. Available at www.cdc.gov/std/stats/2001chlamydia.htm. Accessed on October 27, 2003.
3. CDC. Division of Sexually Transmitted Diseases. Gonorrhea. Available at www.cdc.gov/std/stats/2001gonorrhea.htm. Accessed on October 27, 2003.
4. CDC. Division of Sexually Transmitted Diseases. Syphilis. Available at www.cdc.gov/std/stats/2001syphilis.htm. Accessed on October 27, 2003.
5. Available at www.eurmktg.com/globstats.
6. Bull SS, McFarlane M. Soliciting sex on the internet. What are the risks for sexually transmitted diseases and HIV? Sex Transm Dis 2000;27:545-550.
7. Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA 2000;284:447-449.
8. McFarlane M, Bull SS, Rietmeijer CA. The internet as a newly-emerging risk environment for sexually transmitted diseases. JAMA 2000;284:443-446.
9. Agency for Healthcare Research and Quality (AHRCQ). United States Preventive Services Task Force (USPSTF). Screening: chlamydia infection. Available at www.ahcpr.gov/clinic/uspstf/uspschlm.htm. Accessed on October 27, 2003.
10. American Academy of Family Physicians. Introduction to AAFP summary of policy recommendations for periodic health examinations. Available at www.aafp.org/x10601.xml. Accessed on October 27, 2003.
11. CDC. Screening tests to detect chlamydia trachomatis and Neisseria gonorrhea infections. MMWR Recomm Rep 2002;51(RR-15):1-38.
12. CDC. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR6):1-78.