User login
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
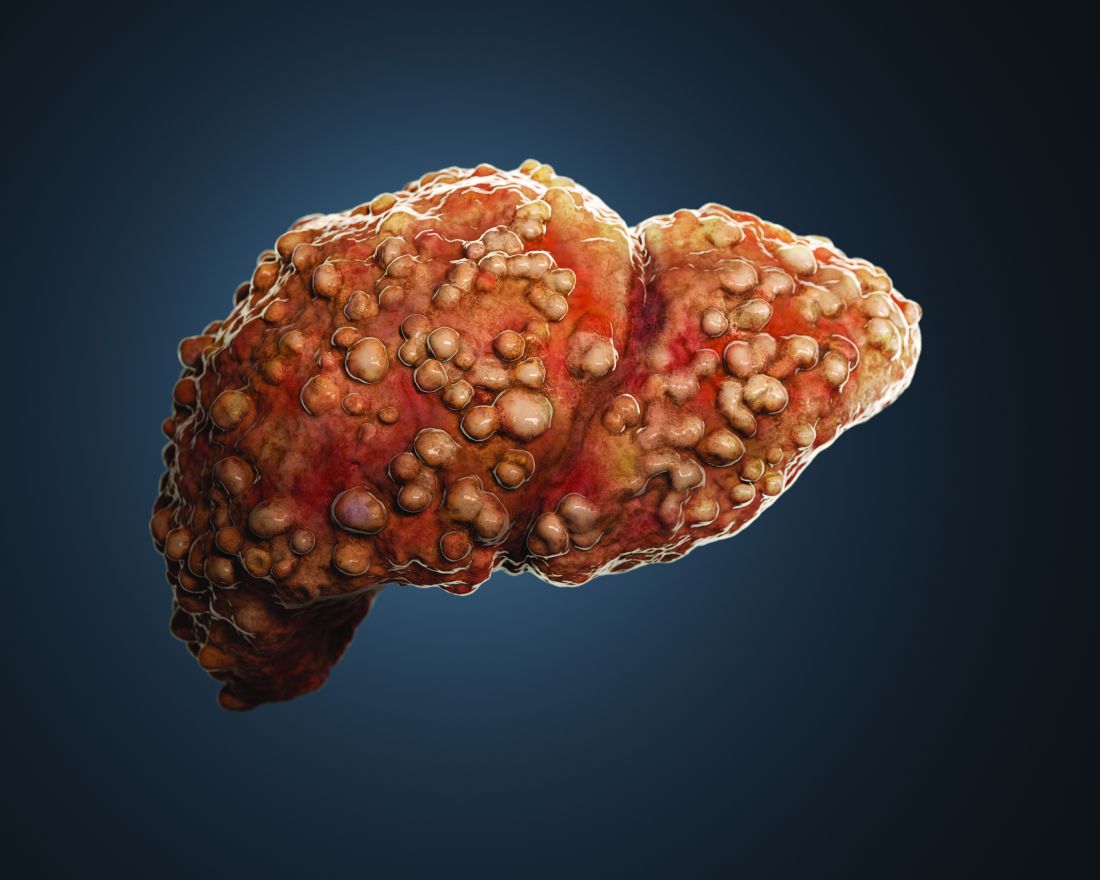
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Caution is advised in patients at risk of pulmonary edema
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.