User login
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
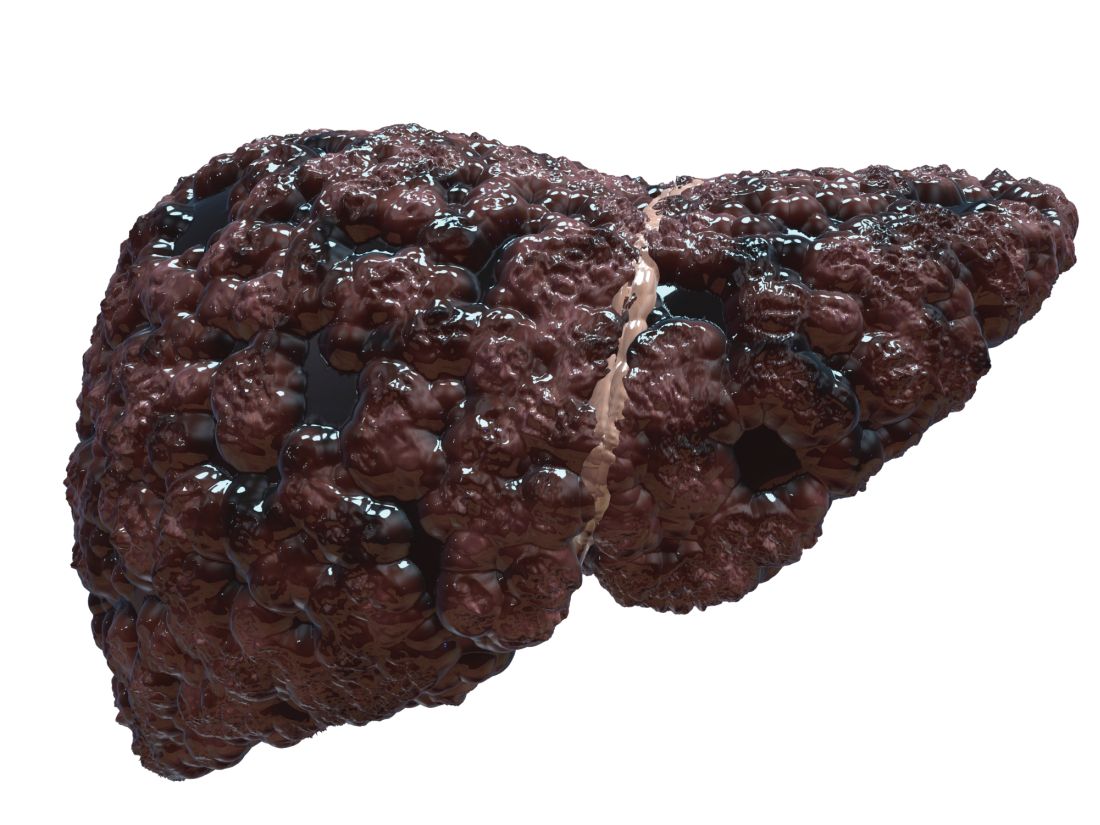
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
FROM JGH OPEN