User login
Although no sonologist can make a definitive diagnosis in every case of clinically suspected ovarian pathology, hallmark characteristics of an ovarian mass contribute greatly to the clinician’s appraisal of a tumor’s malignant potential.
Ultrasound reveals details about the size and architecture of ovarian masses that are indispensable in the initial evaluation of clinically suspect ovarian pathology. Nevertheless, determining whether a mass requires surgery remains a formidable challenge, thanks to the variability in the macroscopic characteristics of benign and malignant lesions. The task is further complicated by the diversity among ovarian tumors, which can be classified into 35 subtypes.1
Here, I present a systematic approach to investigating an ovarian mass via ultrasound, focusing on 9 key questions. The morphologic criteria outlined in this article provide the basis for distinguishing between benign and potentially malignant lesions, with a high probability of success.
Keep in mind: Ultrasound cannot provide histologic information. This limitation is important because several types of ovarian masses can have a similar sonographic appearance. The endpoint should be whether or not a specific patient requires surgical intervention.
Whether a patient should be referred to a subspecialist depends on the gynecologist’s level of experience as well as the sonographic criteria.
Evaluate ovarian cancer risk
The first step in evaluating an ovarian mass, prior to ultrasound examination, is to estimate the likelihood of malignancy. In the general population, the risk of ovarian cancer is 1 in 55 (1.8%),2 but certain factors may increase this risk:
- Age. In women with adnexal masses, those 60 to 69 years of age have 12 times the malignancy risk of those aged 20 to 29.3
- Family history. Five percent of women with ovarian cancer have a family history of the disease.4 The lifetime risk of ovarian cancer based on family history alone ranges from 6.7% for 1 first-degree relative with the disease to 40% for women with hereditary syndrome (TABLE 1).5,6 Ovarian cancer risk is not increased in the relatives of women with borderline tumors.5 When ovarian cancer has an autosomal dominant inheritance pattern, the age of onset is progressively younger by 10 to 15 years in each generation.7
On the other hand, the use of oral contraceptives for 5 years has been found to reduce the lifetime risk of ovarian cancer in the general population to 0.8%.8
TABLE 1
Lifetime risk of ovarian cancer
| GROUP | RISK (%) |
|---|---|
| General population | 1.8 |
| 1 first-degree relative | 6.7 |
| 2 to 3 first-degree relatives | 8.2 |
| Hereditary syndrome | 40 |
| Data from: Schildkraut and Thompson5 and NIH Consensus Panel6 | |
Transabdominal versus transvaginal views
Transabdominal sonography provides an overview of the pelvis and permits evaluation of masses beyond the field of view of the transvaginal transducer.
In contrast, the transvaginal approach permits utilization of higher-frequency transducers, offering superior resolution.
Transvaginal sonography yields the greatest amount of information when used as an extension of a thorough pelvic examination. During real-time scanning, an examiner can optimize visualization of some adnexal masses by placing pressure on the transvaginal probe and on the patient’s abdomen with his or her free hand. Such examination may elicit pelvic tenderness and helps the examiner assess the mobility and compressibility of an ovarian mass, as well as the consistency of its internal structures.
Question 1What is the size of the lesion?
The risk of malignancy increases with size, regardless of sonomorphology. In general, ovarian tumors larger than 10 cm are unsuitable for morphologic assessment. In most cases, the clinician would proceed to surgery.
For tumors smaller than 5 cm, morphology and Doppler studies may yield relevant information.
- What is the size of the lesion?
- Is the mass solid?
- Is it a simple or complex cyst?
- Is the cyst loculated?
- Are papillary excrescences present?
- Are there echo-dense foci?
- Is there echogenicity of interior fluid?
- Is measurable fluid in the cul-de-sac?
- How does the mass change over time?
The morphologic assessment of tumors between 5 and 10 cm should be considered on an individual basis. All the criteria outlined below help determine whether observation or surgery is best in a specific case. For example, a clear 7-cm cyst in an asymptomatic 21-year-old patient might best be observed.
TABLE 2 lists the positive predictive values of size from different series. Variation among them may be explained by a different prevalence of ovarian malignancy in each series.
TABLE 2
Size as a predictor of malignancy in ovarian tumors
| AUTHOR | YEAR | POSITIVE PREDICTIVE VALUE OF TUMOR SIZE | ||
|---|---|---|---|---|
| <5 cm | 5-10 cm | >10 cm | ||
| Rulin32 | 1987 | 3.1 | 10.9 | 63.5 |
| Granberg13 | 1989 | 5.9 | 21.3 | 43.6 |
| Sassone33 | 1991 | 3.3 | 7.2 | 12.5 |
| Luxman34 | 1991 | 13.9 | 35.6 | 38.1 |
Question 2 Is the mass solid?
When a solid adnexal mass is detected, the sonologist should consider the possibility of a pedunculated leiomyoma. A stalk with vascular flow from the mass to the main body of the uterus confirms this pathology; a normal ovary on that side excludes it.
If the mass is within the ovary, a Brenner tumor, fibroma (FIGURE 1), granulosa cell tumor, or Sertoli-Leydig cell tumor should be considered. An ovarian fibroma may have significant attenuation9 and may contain calcifications.10 Solid masses are generally the smallest subset of ovarian tumors; approximately 10% are malignant.11
FIGURE 1 Fibroma
The well-demarcated hypoechoic mass in the right ovary is consistent with a fibroma.
Question 3 Is it a simple or complex cyst?
The risk that a simple, thin-walled cyst is malignant increases with patient age and the size of the cyst. Osmers et al11 found no malignancy in simple cysts removed from women 20 years of age or younger, while 3.6% of simple cysts were malignant in women over age 51.
As for size, Ekerhovd et al12 found no malignancies in simple cysts less than 2 cm in diameter, while 6.6% of simple cysts larger than 7.9 cm were found to be malignant. In general, simple ovarian cysts less than 5 cm in diameter are unlikely to be malignant.
While the risk of malignancy increases with complex ovarian cysts, these lesions are also more commonly benign. In an evaluation of 211 cystic-solid tumors, 29.4% were functional, 20.4% were retention cysts, 33.2% were benign neoplasms, and 17% were malignant.11 Color Doppler may improve diagnostic accuracy when a complex adnexal mass is detected.
Question 4Is the cyst loculated?
Although the risk of malignancy rises as loculated cysts become more complex, there is significant overlap between benign and malignant lesions.13 Mucinous cystadenomas (FIGURE 2) contain multiple septations and fluid with fine debris secondary to their thick mucinous content. A mucinous cystadenocarcinoma may contain papillary excrescences.14
FIGURE 2 Mucinous cystadenoma
Multiseptated, debris-filled mucinous cystadenoma in the left ovary of a 20-year-old patient.
Question 5 Are papillary excrescences present?
These represent localized overgrowth of the epithelium. The likelihood of malignancy rises as the number of excrescences increases (FIGURE 3).15 Papillary projections into the cyst cavity of less than 3 mm are not strongly associated with malignancy.16
Because of the proportionally larger surface area that must be examined, the likelihood of missing a papillary excrescence increases with the size of the cyst.12 Ranney and Ahmad17 have reported significantly reduced survival when an ovarian neoplasm contains papillary excrescences.
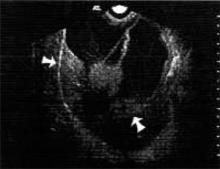
FIGURE 3 Papillary excrescences
Multiseptated 14-cm endometrioid adenocarcinoma containing several papillary excrescences (arrows).
Question 6Are there echo-dense foci?
Because fat mixed with hair produces echogenic foci with acoustic shadowing, the echo-dense foci in benign cystic teratomas are usually easily identifiable (FIGURE 4). In fact, morphologic assessment alone has a sensitivity of 93.1% for the detection of benign cystic teratomas.18 Be aware, however, that some malignant tumors may have components that cast an acoustic shadow.19
Benign cystic teratomas grow at a mean rate of 1.8 mm per year in premenopausal women,20 and 72% of cystic teratomas are avascular.18 If the solid components of an apparent benign cystic teratoma have vascular flow, a struma ovarii consisting largely of thyroid tissue should be considered.21
FIGURE 4 Benign cystic teratoma
Complex cystic/solid benign cystic teratoma. Note that part of the ovary is unaffected.
Question 7Is there echogenicity of interior fluid?
If so, it may provide a clue to diagnosis. For example, a serous cyst generally contains clear fluid, while mucinous cysts contain fine debris. An endometrioma tends to contain homogeneous debris22(FIGURE 5), while a hemorrhagic cyst may have a ground-glass appearance (FIGURE 6). Echogenic particles within a hypoechoic background are characteristic of a benign cystic teratoma.
FIGURE 5 Homogeneous debris
The homogeneous debris in this left ovarian mass is consistent with an endometrioma.
FIGURE 6 Hemorrhagic cyst
Ground-glass appearance of a hemorrhagic ovarian cyst.
Question 8Is measurable fluid in the cul-de-sac?
As the ovaries become atrophic, the production of cul-de-sac fluid declines. A post-menopausal patient has 5.5±7.8 mL of cul-de-sac fluid, depending on the degree of ovarian activity.23 Since transvaginal ultrasound can consistently detect 8 mL or more of cul-de-sac fluid, no fluid is identified in the majority of postmenopausal patients.24 Thus, a moderate amount of cul-de-sac fluid in a postmenopausal patient should raise the sonologist’s index of suspicion concerning a possible ovarian tumor.
Question 9How does the mass change over time?
The architectural pattern of ovarian masses is frequently dynamic. For example, between 53% and 89% of functional cysts spontaneously regress.11 Thus, a follow-up ultrasound examination in 6 to 8 weeks may provide additional information about a mass’s etiology. Repeat sonography is recommended in cases without obvious stigmata of malignancy or a size that would mandate surgery.
For example, a recent hemorrhagic cyst may result in an enlarged ovary with mixed echogenicity. Over 6 weeks the liquefaction of the clot within the cyst will result in either resolution of the mass or a markedly different sonographic appearance.
Other studies
Ovarian Doppler. Because of the many types of ovarian masses, sonographic morphology is usually not pathognomic and—when used alone—results in a high false-positive rate in the diagnosis of malignancy. The role of color and pulse Doppler is to reduce these false-positives. Note, however, that the positive predictive value of gray scale and color Doppler is lower in premenopausal patients than postmenopausal women because of the higher prevalence of malignancy in the latter group.
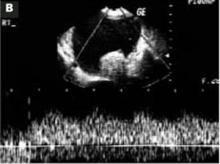
Although initial color Doppler studies of ovarian masses suggested that clinicians could use a cut-off resistance index (FIGURE 7) or pulsatility index to satisfactorily discriminate between benign and malignant lesions,25 subsequent studies demonstrated considerable overlap in the values obtained.26 As a result, evaluation of vessel distribution and architecture has taken on additional importance (FIGURE 8).
- Findings suggestive of malignancy. Malignant tumors characteristically contain dilated, saccular, and randomly dispersed vessels.27 Centrally located flow, flow along septations, and flow within papillary excrescences also suggest malignancy.
- Findings suggesting a benign mass. Peripheral flow is more consistent with a benign neoplasm. Hemorrhage in a mass is highly suggestive of a benign mass or cyst.28
Morphology scores. Almost monthly a new morphology scoring system is published that attempts to substitute objective criteria and measurements for the subjective assessment of an ovarian mass. Most morphologic scoring systems include the parameters reviewed thus far, and some include menopausal status and CA-125 values. Sensitivities and specificities as high as 95% have been reported.29
Inevitably, when these scoring systems are validated externally, both the sensitivity and specificity fall. Currently, the proposed models perform no better than an experienced clinician using the patient’s history, sonographic findings, and CA-125 measurement.30
Three-dimensional sonography. Three-dimensional power imaging may enable visualization of malignant vessel abnormalities (ie, arteriovenous shunts, tumor lakes, etc). It also may improve the evaluation of tumor architecture and tumor invasion through the ovarian capsule. To date, however, 3-dimensional imaging has not been shown to significantly affect the morphology score assigned by 2-dimensional imaging.31
Dr. Hill reports no financial relationship with any companies whose products are mentioned in this article
FIGURE 7 Malignancy
A 55-year-old patient with an 11-cm right ovarian malignancy. A) A 4.5-cm echogenic foucs within the primary systic mass.
B) Low resistance index (0.297) in a peripheral vessel.
FIGURE 8 Power Doppler
Power Doppler of abnormal vessels within an ovarian carcinoma.
1. Osmers R. Sonographic evaluation of ovarian masses and its therapeutic implications [editorial]. Ultrasound Obstet Gynecol. 1996;8:217-222.
2. Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin. 2002;52:23-47.
3. Koonings PP, Campbell K, Mishell DL, Grimes DA. Relative frequency of primary neoplasms: ten year review. Obstet Gynecol. 1989;74:921-926.
4. Randall TC, Rubin SC. Assessing a patient’s risk for hereditary ovarian cancer. OBG Manage. 1998;10:37-46.
5. Schildkraut JM, Thompson WD. Familial ovarian cancer: a population-based case-control study. Am J Epidemiol. 1988;128:456-466.
6. NIH Consensus Development Panel on Ovarian Cancer Ovarian cancer-screening, treatment and follow-up. JAMA. 1995;273:491-497.
7. Piver MS, Recio FO. When is ovarian cancer screening helpful? Contemp Ob-Gyn. 1993;38:17-32.
8. Carlson KJ, Kates SJ, Singer DE. Screening for ovarian cancer. Ann Intern Med. 1994;121:124-132.
9. Stephenson WM, Laing FC. Sonography of ovarian fibromas. AJR Am J Roentgenol. 1985;144:1239-1240.
10. Athey PA, Malone RS. Sonography of ovarian fibromas/thecomas. J Ultrasound Med. 1987;6:431-436.
11. Osmers RGW, Osmers M, VonMaydell B, Wagner B, Kuhn W. Preoperative evaluation of ovarian tumors in the premenopause by transvaginosonography. Am J Obstet Gynecol. 1996;175:428-434.
12. Ekerhovd E, Wienerroith H, Staudach A, Granberg S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: a comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am J Obstet Gynecol. 2001;184:48-54.
13. Granberg S, Wikland M, Jansson I. Macroscopic characterization of ovarian tumors and the relation to the histologic diagnosis: criteria to be used for ultrasound evaluation. Gynecol Oncol. 1989;35:139-144.
14. Sutton CL, McKinney CD, Jones JE, et al. Ovarian masses revisited: radiologic and pathologic correlation. Radiographics. 1992;12:853-877.
15. Granberg S, Norstrom A, Wikland M. Tumors in the lower pelvis as imaged by vaginal sonography. Gynecol Oncol. 1990;37:224-229.
16. Timmerman D, Bourne TH, Tailor A, et al. A comparison of methods for preoperative discrimination between malignant and benign adnexal masses: the development of a new logistic regression model. Am J Obstet Gynecol. 1999;181:57-65.
17. Ranney B, Ahmad MI. Early identification, differentiation and treatment of ovarian neoplasia. Int J Gynaecol Obstet. 1979;17:209-218.
18. Kurjak A, Kupesic S, Babic MM, et al. Preoperative evaluation of cystic teratoma: what does color Doppler add? J Clin Ultrasound. 1997;25:309-316.
19. Lerner JP, Timor-Tritsch IE, Federman A, Abramovich G. Transvaginal ultrasonographic characterization of ovarian masses with an improved, weighted scoring system. Am J Obstet Gynecol. 1994;170:81-85.
20. Caspi B, Appelman Z, Rabinerson D, et al. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril. 1997;68:501-505.
21. Zalel Y, Caspi B, Tepper R. Doppler flow characteristics of dermoid cysts: unique appearance of struma ovary. J Ultrasound Med. 1997;16:355-358.
22. Kupfer MC, Schwimer SR, Lebovic J. Transvaginal sonographic appearance of endometriomata: spectrum of findings. J Ultrasound Med. 1992;11:129-133.
23. Donnez J, Langerock S, Thomas K. Peritoneal fluid volume and 17ß-estradiol and progesterone concentrators in ovulatory, anovulatory and postmenopausal women. Obstet Gynecol. 1982;59:687-692.
24. Khalife S, Falcone T, Hemmings R, Cohen D. Diagnostic accuracy of transvaginal ultrasound in detecting free pelvic fluid. J Reprod Med. 1998;43:795-798.
25. Kurjak A, Schulman H, Sosic A, et al. Transvaginal ultrasound, color flow, and Doppler waveform of the postmenopausal adnexal mass. Obstet Gynecol. 1992;80:917-921.
26. Hamper UM, Sheth S, Abbas FM, et al. Transvaginal color Doppler sonography of adnexal masses: differences in blood flow impedance in benign and malignant lesions. AJR Am J Roentgenol. 1993;160:1225-1228.
27. Guerriero S, Alcazar JL, Coccia ME, et al. Complex pelvic masses as a target of evaluation of vessel distribution by color Doppler sonography for the diagnosis of adnexal malignancies. Results of a multicenter European study. J Ultrasound Med. 2002;21:1105-1111.
28. Reynolds T, Hill MC, Glassman LM. Sonography of hemorrhagic ovarian cysts. J Clin Ultrasound. 1986;14:449-453.
29. Timmerman D, Verrelst H, Bourne TH, et al. Artificial neural network models for the preoperative discrimination between malignant and benign adnexal masses. Ultrasound Obstet Gynecol. 1999;13:17-25.
30. Boll D, Geomini MAJ, Brolmann HAM, et al. The pre-operative assessment of the adnexal mass: the accuracy of clinical estimates versus clinical prediction rules. Br J Obstet Gynaecol. 2003;110:519-523.
31. Cohen LS, Escobar P, Scharm C, et al. Three-dimensional ultrasound improves the diagnostic accuracy for ovarian cancer predictors. Gynecol Oncol. 2001;82:40-48.
32. Rulin MC, Preston AL. Adnexal masses in postmenopausal women. Obstet Gynecol. 1987;70:578-581.
33. Sassone AM, Timor-Tritsch IE, Artner A, et al. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol. 1991;78:70-76.
34. Luxman D, Bergman A, Sagi J, David MP. The postmenopausal adnexal mass: correlation between ultrasonic and pathologic findings. Obstet Gynecol. 1991;77:726-728.
Although no sonologist can make a definitive diagnosis in every case of clinically suspected ovarian pathology, hallmark characteristics of an ovarian mass contribute greatly to the clinician’s appraisal of a tumor’s malignant potential.
Ultrasound reveals details about the size and architecture of ovarian masses that are indispensable in the initial evaluation of clinically suspect ovarian pathology. Nevertheless, determining whether a mass requires surgery remains a formidable challenge, thanks to the variability in the macroscopic characteristics of benign and malignant lesions. The task is further complicated by the diversity among ovarian tumors, which can be classified into 35 subtypes.1
Here, I present a systematic approach to investigating an ovarian mass via ultrasound, focusing on 9 key questions. The morphologic criteria outlined in this article provide the basis for distinguishing between benign and potentially malignant lesions, with a high probability of success.
Keep in mind: Ultrasound cannot provide histologic information. This limitation is important because several types of ovarian masses can have a similar sonographic appearance. The endpoint should be whether or not a specific patient requires surgical intervention.
Whether a patient should be referred to a subspecialist depends on the gynecologist’s level of experience as well as the sonographic criteria.
Evaluate ovarian cancer risk
The first step in evaluating an ovarian mass, prior to ultrasound examination, is to estimate the likelihood of malignancy. In the general population, the risk of ovarian cancer is 1 in 55 (1.8%),2 but certain factors may increase this risk:
- Age. In women with adnexal masses, those 60 to 69 years of age have 12 times the malignancy risk of those aged 20 to 29.3
- Family history. Five percent of women with ovarian cancer have a family history of the disease.4 The lifetime risk of ovarian cancer based on family history alone ranges from 6.7% for 1 first-degree relative with the disease to 40% for women with hereditary syndrome (TABLE 1).5,6 Ovarian cancer risk is not increased in the relatives of women with borderline tumors.5 When ovarian cancer has an autosomal dominant inheritance pattern, the age of onset is progressively younger by 10 to 15 years in each generation.7
On the other hand, the use of oral contraceptives for 5 years has been found to reduce the lifetime risk of ovarian cancer in the general population to 0.8%.8
TABLE 1
Lifetime risk of ovarian cancer
| GROUP | RISK (%) |
|---|---|
| General population | 1.8 |
| 1 first-degree relative | 6.7 |
| 2 to 3 first-degree relatives | 8.2 |
| Hereditary syndrome | 40 |
| Data from: Schildkraut and Thompson5 and NIH Consensus Panel6 | |
Transabdominal versus transvaginal views
Transabdominal sonography provides an overview of the pelvis and permits evaluation of masses beyond the field of view of the transvaginal transducer.
In contrast, the transvaginal approach permits utilization of higher-frequency transducers, offering superior resolution.
Transvaginal sonography yields the greatest amount of information when used as an extension of a thorough pelvic examination. During real-time scanning, an examiner can optimize visualization of some adnexal masses by placing pressure on the transvaginal probe and on the patient’s abdomen with his or her free hand. Such examination may elicit pelvic tenderness and helps the examiner assess the mobility and compressibility of an ovarian mass, as well as the consistency of its internal structures.
Question 1What is the size of the lesion?
The risk of malignancy increases with size, regardless of sonomorphology. In general, ovarian tumors larger than 10 cm are unsuitable for morphologic assessment. In most cases, the clinician would proceed to surgery.
For tumors smaller than 5 cm, morphology and Doppler studies may yield relevant information.
- What is the size of the lesion?
- Is the mass solid?
- Is it a simple or complex cyst?
- Is the cyst loculated?
- Are papillary excrescences present?
- Are there echo-dense foci?
- Is there echogenicity of interior fluid?
- Is measurable fluid in the cul-de-sac?
- How does the mass change over time?
The morphologic assessment of tumors between 5 and 10 cm should be considered on an individual basis. All the criteria outlined below help determine whether observation or surgery is best in a specific case. For example, a clear 7-cm cyst in an asymptomatic 21-year-old patient might best be observed.
TABLE 2 lists the positive predictive values of size from different series. Variation among them may be explained by a different prevalence of ovarian malignancy in each series.
TABLE 2
Size as a predictor of malignancy in ovarian tumors
| AUTHOR | YEAR | POSITIVE PREDICTIVE VALUE OF TUMOR SIZE | ||
|---|---|---|---|---|
| <5 cm | 5-10 cm | >10 cm | ||
| Rulin32 | 1987 | 3.1 | 10.9 | 63.5 |
| Granberg13 | 1989 | 5.9 | 21.3 | 43.6 |
| Sassone33 | 1991 | 3.3 | 7.2 | 12.5 |
| Luxman34 | 1991 | 13.9 | 35.6 | 38.1 |
Question 2 Is the mass solid?
When a solid adnexal mass is detected, the sonologist should consider the possibility of a pedunculated leiomyoma. A stalk with vascular flow from the mass to the main body of the uterus confirms this pathology; a normal ovary on that side excludes it.
If the mass is within the ovary, a Brenner tumor, fibroma (FIGURE 1), granulosa cell tumor, or Sertoli-Leydig cell tumor should be considered. An ovarian fibroma may have significant attenuation9 and may contain calcifications.10 Solid masses are generally the smallest subset of ovarian tumors; approximately 10% are malignant.11
FIGURE 1 Fibroma
The well-demarcated hypoechoic mass in the right ovary is consistent with a fibroma.
Question 3 Is it a simple or complex cyst?
The risk that a simple, thin-walled cyst is malignant increases with patient age and the size of the cyst. Osmers et al11 found no malignancy in simple cysts removed from women 20 years of age or younger, while 3.6% of simple cysts were malignant in women over age 51.
As for size, Ekerhovd et al12 found no malignancies in simple cysts less than 2 cm in diameter, while 6.6% of simple cysts larger than 7.9 cm were found to be malignant. In general, simple ovarian cysts less than 5 cm in diameter are unlikely to be malignant.
While the risk of malignancy increases with complex ovarian cysts, these lesions are also more commonly benign. In an evaluation of 211 cystic-solid tumors, 29.4% were functional, 20.4% were retention cysts, 33.2% were benign neoplasms, and 17% were malignant.11 Color Doppler may improve diagnostic accuracy when a complex adnexal mass is detected.
Question 4Is the cyst loculated?
Although the risk of malignancy rises as loculated cysts become more complex, there is significant overlap between benign and malignant lesions.13 Mucinous cystadenomas (FIGURE 2) contain multiple septations and fluid with fine debris secondary to their thick mucinous content. A mucinous cystadenocarcinoma may contain papillary excrescences.14
FIGURE 2 Mucinous cystadenoma
Multiseptated, debris-filled mucinous cystadenoma in the left ovary of a 20-year-old patient.
Question 5 Are papillary excrescences present?
These represent localized overgrowth of the epithelium. The likelihood of malignancy rises as the number of excrescences increases (FIGURE 3).15 Papillary projections into the cyst cavity of less than 3 mm are not strongly associated with malignancy.16
Because of the proportionally larger surface area that must be examined, the likelihood of missing a papillary excrescence increases with the size of the cyst.12 Ranney and Ahmad17 have reported significantly reduced survival when an ovarian neoplasm contains papillary excrescences.
FIGURE 3 Papillary excrescences
Multiseptated 14-cm endometrioid adenocarcinoma containing several papillary excrescences (arrows).
Question 6Are there echo-dense foci?
Because fat mixed with hair produces echogenic foci with acoustic shadowing, the echo-dense foci in benign cystic teratomas are usually easily identifiable (FIGURE 4). In fact, morphologic assessment alone has a sensitivity of 93.1% for the detection of benign cystic teratomas.18 Be aware, however, that some malignant tumors may have components that cast an acoustic shadow.19
Benign cystic teratomas grow at a mean rate of 1.8 mm per year in premenopausal women,20 and 72% of cystic teratomas are avascular.18 If the solid components of an apparent benign cystic teratoma have vascular flow, a struma ovarii consisting largely of thyroid tissue should be considered.21
FIGURE 4 Benign cystic teratoma
Complex cystic/solid benign cystic teratoma. Note that part of the ovary is unaffected.
Question 7Is there echogenicity of interior fluid?
If so, it may provide a clue to diagnosis. For example, a serous cyst generally contains clear fluid, while mucinous cysts contain fine debris. An endometrioma tends to contain homogeneous debris22(FIGURE 5), while a hemorrhagic cyst may have a ground-glass appearance (FIGURE 6). Echogenic particles within a hypoechoic background are characteristic of a benign cystic teratoma.
FIGURE 5 Homogeneous debris
The homogeneous debris in this left ovarian mass is consistent with an endometrioma.
FIGURE 6 Hemorrhagic cyst
Ground-glass appearance of a hemorrhagic ovarian cyst.
Question 8Is measurable fluid in the cul-de-sac?
As the ovaries become atrophic, the production of cul-de-sac fluid declines. A post-menopausal patient has 5.5±7.8 mL of cul-de-sac fluid, depending on the degree of ovarian activity.23 Since transvaginal ultrasound can consistently detect 8 mL or more of cul-de-sac fluid, no fluid is identified in the majority of postmenopausal patients.24 Thus, a moderate amount of cul-de-sac fluid in a postmenopausal patient should raise the sonologist’s index of suspicion concerning a possible ovarian tumor.
Question 9How does the mass change over time?
The architectural pattern of ovarian masses is frequently dynamic. For example, between 53% and 89% of functional cysts spontaneously regress.11 Thus, a follow-up ultrasound examination in 6 to 8 weeks may provide additional information about a mass’s etiology. Repeat sonography is recommended in cases without obvious stigmata of malignancy or a size that would mandate surgery.
For example, a recent hemorrhagic cyst may result in an enlarged ovary with mixed echogenicity. Over 6 weeks the liquefaction of the clot within the cyst will result in either resolution of the mass or a markedly different sonographic appearance.
Other studies
Ovarian Doppler. Because of the many types of ovarian masses, sonographic morphology is usually not pathognomic and—when used alone—results in a high false-positive rate in the diagnosis of malignancy. The role of color and pulse Doppler is to reduce these false-positives. Note, however, that the positive predictive value of gray scale and color Doppler is lower in premenopausal patients than postmenopausal women because of the higher prevalence of malignancy in the latter group.
Although initial color Doppler studies of ovarian masses suggested that clinicians could use a cut-off resistance index (FIGURE 7) or pulsatility index to satisfactorily discriminate between benign and malignant lesions,25 subsequent studies demonstrated considerable overlap in the values obtained.26 As a result, evaluation of vessel distribution and architecture has taken on additional importance (FIGURE 8).
- Findings suggestive of malignancy. Malignant tumors characteristically contain dilated, saccular, and randomly dispersed vessels.27 Centrally located flow, flow along septations, and flow within papillary excrescences also suggest malignancy.
- Findings suggesting a benign mass. Peripheral flow is more consistent with a benign neoplasm. Hemorrhage in a mass is highly suggestive of a benign mass or cyst.28
Morphology scores. Almost monthly a new morphology scoring system is published that attempts to substitute objective criteria and measurements for the subjective assessment of an ovarian mass. Most morphologic scoring systems include the parameters reviewed thus far, and some include menopausal status and CA-125 values. Sensitivities and specificities as high as 95% have been reported.29
Inevitably, when these scoring systems are validated externally, both the sensitivity and specificity fall. Currently, the proposed models perform no better than an experienced clinician using the patient’s history, sonographic findings, and CA-125 measurement.30
Three-dimensional sonography. Three-dimensional power imaging may enable visualization of malignant vessel abnormalities (ie, arteriovenous shunts, tumor lakes, etc). It also may improve the evaluation of tumor architecture and tumor invasion through the ovarian capsule. To date, however, 3-dimensional imaging has not been shown to significantly affect the morphology score assigned by 2-dimensional imaging.31
Dr. Hill reports no financial relationship with any companies whose products are mentioned in this article
FIGURE 7 Malignancy
A 55-year-old patient with an 11-cm right ovarian malignancy. A) A 4.5-cm echogenic foucs within the primary systic mass.
B) Low resistance index (0.297) in a peripheral vessel.
FIGURE 8 Power Doppler
Power Doppler of abnormal vessels within an ovarian carcinoma.
Although no sonologist can make a definitive diagnosis in every case of clinically suspected ovarian pathology, hallmark characteristics of an ovarian mass contribute greatly to the clinician’s appraisal of a tumor’s malignant potential.
Ultrasound reveals details about the size and architecture of ovarian masses that are indispensable in the initial evaluation of clinically suspect ovarian pathology. Nevertheless, determining whether a mass requires surgery remains a formidable challenge, thanks to the variability in the macroscopic characteristics of benign and malignant lesions. The task is further complicated by the diversity among ovarian tumors, which can be classified into 35 subtypes.1
Here, I present a systematic approach to investigating an ovarian mass via ultrasound, focusing on 9 key questions. The morphologic criteria outlined in this article provide the basis for distinguishing between benign and potentially malignant lesions, with a high probability of success.
Keep in mind: Ultrasound cannot provide histologic information. This limitation is important because several types of ovarian masses can have a similar sonographic appearance. The endpoint should be whether or not a specific patient requires surgical intervention.
Whether a patient should be referred to a subspecialist depends on the gynecologist’s level of experience as well as the sonographic criteria.
Evaluate ovarian cancer risk
The first step in evaluating an ovarian mass, prior to ultrasound examination, is to estimate the likelihood of malignancy. In the general population, the risk of ovarian cancer is 1 in 55 (1.8%),2 but certain factors may increase this risk:
- Age. In women with adnexal masses, those 60 to 69 years of age have 12 times the malignancy risk of those aged 20 to 29.3
- Family history. Five percent of women with ovarian cancer have a family history of the disease.4 The lifetime risk of ovarian cancer based on family history alone ranges from 6.7% for 1 first-degree relative with the disease to 40% for women with hereditary syndrome (TABLE 1).5,6 Ovarian cancer risk is not increased in the relatives of women with borderline tumors.5 When ovarian cancer has an autosomal dominant inheritance pattern, the age of onset is progressively younger by 10 to 15 years in each generation.7
On the other hand, the use of oral contraceptives for 5 years has been found to reduce the lifetime risk of ovarian cancer in the general population to 0.8%.8
TABLE 1
Lifetime risk of ovarian cancer
| GROUP | RISK (%) |
|---|---|
| General population | 1.8 |
| 1 first-degree relative | 6.7 |
| 2 to 3 first-degree relatives | 8.2 |
| Hereditary syndrome | 40 |
| Data from: Schildkraut and Thompson5 and NIH Consensus Panel6 | |
Transabdominal versus transvaginal views
Transabdominal sonography provides an overview of the pelvis and permits evaluation of masses beyond the field of view of the transvaginal transducer.
In contrast, the transvaginal approach permits utilization of higher-frequency transducers, offering superior resolution.
Transvaginal sonography yields the greatest amount of information when used as an extension of a thorough pelvic examination. During real-time scanning, an examiner can optimize visualization of some adnexal masses by placing pressure on the transvaginal probe and on the patient’s abdomen with his or her free hand. Such examination may elicit pelvic tenderness and helps the examiner assess the mobility and compressibility of an ovarian mass, as well as the consistency of its internal structures.
Question 1What is the size of the lesion?
The risk of malignancy increases with size, regardless of sonomorphology. In general, ovarian tumors larger than 10 cm are unsuitable for morphologic assessment. In most cases, the clinician would proceed to surgery.
For tumors smaller than 5 cm, morphology and Doppler studies may yield relevant information.
- What is the size of the lesion?
- Is the mass solid?
- Is it a simple or complex cyst?
- Is the cyst loculated?
- Are papillary excrescences present?
- Are there echo-dense foci?
- Is there echogenicity of interior fluid?
- Is measurable fluid in the cul-de-sac?
- How does the mass change over time?
The morphologic assessment of tumors between 5 and 10 cm should be considered on an individual basis. All the criteria outlined below help determine whether observation or surgery is best in a specific case. For example, a clear 7-cm cyst in an asymptomatic 21-year-old patient might best be observed.
TABLE 2 lists the positive predictive values of size from different series. Variation among them may be explained by a different prevalence of ovarian malignancy in each series.
TABLE 2
Size as a predictor of malignancy in ovarian tumors
| AUTHOR | YEAR | POSITIVE PREDICTIVE VALUE OF TUMOR SIZE | ||
|---|---|---|---|---|
| <5 cm | 5-10 cm | >10 cm | ||
| Rulin32 | 1987 | 3.1 | 10.9 | 63.5 |
| Granberg13 | 1989 | 5.9 | 21.3 | 43.6 |
| Sassone33 | 1991 | 3.3 | 7.2 | 12.5 |
| Luxman34 | 1991 | 13.9 | 35.6 | 38.1 |
Question 2 Is the mass solid?
When a solid adnexal mass is detected, the sonologist should consider the possibility of a pedunculated leiomyoma. A stalk with vascular flow from the mass to the main body of the uterus confirms this pathology; a normal ovary on that side excludes it.
If the mass is within the ovary, a Brenner tumor, fibroma (FIGURE 1), granulosa cell tumor, or Sertoli-Leydig cell tumor should be considered. An ovarian fibroma may have significant attenuation9 and may contain calcifications.10 Solid masses are generally the smallest subset of ovarian tumors; approximately 10% are malignant.11
FIGURE 1 Fibroma
The well-demarcated hypoechoic mass in the right ovary is consistent with a fibroma.
Question 3 Is it a simple or complex cyst?
The risk that a simple, thin-walled cyst is malignant increases with patient age and the size of the cyst. Osmers et al11 found no malignancy in simple cysts removed from women 20 years of age or younger, while 3.6% of simple cysts were malignant in women over age 51.
As for size, Ekerhovd et al12 found no malignancies in simple cysts less than 2 cm in diameter, while 6.6% of simple cysts larger than 7.9 cm were found to be malignant. In general, simple ovarian cysts less than 5 cm in diameter are unlikely to be malignant.
While the risk of malignancy increases with complex ovarian cysts, these lesions are also more commonly benign. In an evaluation of 211 cystic-solid tumors, 29.4% were functional, 20.4% were retention cysts, 33.2% were benign neoplasms, and 17% were malignant.11 Color Doppler may improve diagnostic accuracy when a complex adnexal mass is detected.
Question 4Is the cyst loculated?
Although the risk of malignancy rises as loculated cysts become more complex, there is significant overlap between benign and malignant lesions.13 Mucinous cystadenomas (FIGURE 2) contain multiple septations and fluid with fine debris secondary to their thick mucinous content. A mucinous cystadenocarcinoma may contain papillary excrescences.14
FIGURE 2 Mucinous cystadenoma
Multiseptated, debris-filled mucinous cystadenoma in the left ovary of a 20-year-old patient.
Question 5 Are papillary excrescences present?
These represent localized overgrowth of the epithelium. The likelihood of malignancy rises as the number of excrescences increases (FIGURE 3).15 Papillary projections into the cyst cavity of less than 3 mm are not strongly associated with malignancy.16
Because of the proportionally larger surface area that must be examined, the likelihood of missing a papillary excrescence increases with the size of the cyst.12 Ranney and Ahmad17 have reported significantly reduced survival when an ovarian neoplasm contains papillary excrescences.
FIGURE 3 Papillary excrescences
Multiseptated 14-cm endometrioid adenocarcinoma containing several papillary excrescences (arrows).
Question 6Are there echo-dense foci?
Because fat mixed with hair produces echogenic foci with acoustic shadowing, the echo-dense foci in benign cystic teratomas are usually easily identifiable (FIGURE 4). In fact, morphologic assessment alone has a sensitivity of 93.1% for the detection of benign cystic teratomas.18 Be aware, however, that some malignant tumors may have components that cast an acoustic shadow.19
Benign cystic teratomas grow at a mean rate of 1.8 mm per year in premenopausal women,20 and 72% of cystic teratomas are avascular.18 If the solid components of an apparent benign cystic teratoma have vascular flow, a struma ovarii consisting largely of thyroid tissue should be considered.21
FIGURE 4 Benign cystic teratoma
Complex cystic/solid benign cystic teratoma. Note that part of the ovary is unaffected.
Question 7Is there echogenicity of interior fluid?
If so, it may provide a clue to diagnosis. For example, a serous cyst generally contains clear fluid, while mucinous cysts contain fine debris. An endometrioma tends to contain homogeneous debris22(FIGURE 5), while a hemorrhagic cyst may have a ground-glass appearance (FIGURE 6). Echogenic particles within a hypoechoic background are characteristic of a benign cystic teratoma.
FIGURE 5 Homogeneous debris
The homogeneous debris in this left ovarian mass is consistent with an endometrioma.
FIGURE 6 Hemorrhagic cyst
Ground-glass appearance of a hemorrhagic ovarian cyst.
Question 8Is measurable fluid in the cul-de-sac?
As the ovaries become atrophic, the production of cul-de-sac fluid declines. A post-menopausal patient has 5.5±7.8 mL of cul-de-sac fluid, depending on the degree of ovarian activity.23 Since transvaginal ultrasound can consistently detect 8 mL or more of cul-de-sac fluid, no fluid is identified in the majority of postmenopausal patients.24 Thus, a moderate amount of cul-de-sac fluid in a postmenopausal patient should raise the sonologist’s index of suspicion concerning a possible ovarian tumor.
Question 9How does the mass change over time?
The architectural pattern of ovarian masses is frequently dynamic. For example, between 53% and 89% of functional cysts spontaneously regress.11 Thus, a follow-up ultrasound examination in 6 to 8 weeks may provide additional information about a mass’s etiology. Repeat sonography is recommended in cases without obvious stigmata of malignancy or a size that would mandate surgery.
For example, a recent hemorrhagic cyst may result in an enlarged ovary with mixed echogenicity. Over 6 weeks the liquefaction of the clot within the cyst will result in either resolution of the mass or a markedly different sonographic appearance.
Other studies
Ovarian Doppler. Because of the many types of ovarian masses, sonographic morphology is usually not pathognomic and—when used alone—results in a high false-positive rate in the diagnosis of malignancy. The role of color and pulse Doppler is to reduce these false-positives. Note, however, that the positive predictive value of gray scale and color Doppler is lower in premenopausal patients than postmenopausal women because of the higher prevalence of malignancy in the latter group.
Although initial color Doppler studies of ovarian masses suggested that clinicians could use a cut-off resistance index (FIGURE 7) or pulsatility index to satisfactorily discriminate between benign and malignant lesions,25 subsequent studies demonstrated considerable overlap in the values obtained.26 As a result, evaluation of vessel distribution and architecture has taken on additional importance (FIGURE 8).
- Findings suggestive of malignancy. Malignant tumors characteristically contain dilated, saccular, and randomly dispersed vessels.27 Centrally located flow, flow along septations, and flow within papillary excrescences also suggest malignancy.
- Findings suggesting a benign mass. Peripheral flow is more consistent with a benign neoplasm. Hemorrhage in a mass is highly suggestive of a benign mass or cyst.28
Morphology scores. Almost monthly a new morphology scoring system is published that attempts to substitute objective criteria and measurements for the subjective assessment of an ovarian mass. Most morphologic scoring systems include the parameters reviewed thus far, and some include menopausal status and CA-125 values. Sensitivities and specificities as high as 95% have been reported.29
Inevitably, when these scoring systems are validated externally, both the sensitivity and specificity fall. Currently, the proposed models perform no better than an experienced clinician using the patient’s history, sonographic findings, and CA-125 measurement.30
Three-dimensional sonography. Three-dimensional power imaging may enable visualization of malignant vessel abnormalities (ie, arteriovenous shunts, tumor lakes, etc). It also may improve the evaluation of tumor architecture and tumor invasion through the ovarian capsule. To date, however, 3-dimensional imaging has not been shown to significantly affect the morphology score assigned by 2-dimensional imaging.31
Dr. Hill reports no financial relationship with any companies whose products are mentioned in this article
FIGURE 7 Malignancy
A 55-year-old patient with an 11-cm right ovarian malignancy. A) A 4.5-cm echogenic foucs within the primary systic mass.
B) Low resistance index (0.297) in a peripheral vessel.
FIGURE 8 Power Doppler
Power Doppler of abnormal vessels within an ovarian carcinoma.
1. Osmers R. Sonographic evaluation of ovarian masses and its therapeutic implications [editorial]. Ultrasound Obstet Gynecol. 1996;8:217-222.
2. Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin. 2002;52:23-47.
3. Koonings PP, Campbell K, Mishell DL, Grimes DA. Relative frequency of primary neoplasms: ten year review. Obstet Gynecol. 1989;74:921-926.
4. Randall TC, Rubin SC. Assessing a patient’s risk for hereditary ovarian cancer. OBG Manage. 1998;10:37-46.
5. Schildkraut JM, Thompson WD. Familial ovarian cancer: a population-based case-control study. Am J Epidemiol. 1988;128:456-466.
6. NIH Consensus Development Panel on Ovarian Cancer Ovarian cancer-screening, treatment and follow-up. JAMA. 1995;273:491-497.
7. Piver MS, Recio FO. When is ovarian cancer screening helpful? Contemp Ob-Gyn. 1993;38:17-32.
8. Carlson KJ, Kates SJ, Singer DE. Screening for ovarian cancer. Ann Intern Med. 1994;121:124-132.
9. Stephenson WM, Laing FC. Sonography of ovarian fibromas. AJR Am J Roentgenol. 1985;144:1239-1240.
10. Athey PA, Malone RS. Sonography of ovarian fibromas/thecomas. J Ultrasound Med. 1987;6:431-436.
11. Osmers RGW, Osmers M, VonMaydell B, Wagner B, Kuhn W. Preoperative evaluation of ovarian tumors in the premenopause by transvaginosonography. Am J Obstet Gynecol. 1996;175:428-434.
12. Ekerhovd E, Wienerroith H, Staudach A, Granberg S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: a comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am J Obstet Gynecol. 2001;184:48-54.
13. Granberg S, Wikland M, Jansson I. Macroscopic characterization of ovarian tumors and the relation to the histologic diagnosis: criteria to be used for ultrasound evaluation. Gynecol Oncol. 1989;35:139-144.
14. Sutton CL, McKinney CD, Jones JE, et al. Ovarian masses revisited: radiologic and pathologic correlation. Radiographics. 1992;12:853-877.
15. Granberg S, Norstrom A, Wikland M. Tumors in the lower pelvis as imaged by vaginal sonography. Gynecol Oncol. 1990;37:224-229.
16. Timmerman D, Bourne TH, Tailor A, et al. A comparison of methods for preoperative discrimination between malignant and benign adnexal masses: the development of a new logistic regression model. Am J Obstet Gynecol. 1999;181:57-65.
17. Ranney B, Ahmad MI. Early identification, differentiation and treatment of ovarian neoplasia. Int J Gynaecol Obstet. 1979;17:209-218.
18. Kurjak A, Kupesic S, Babic MM, et al. Preoperative evaluation of cystic teratoma: what does color Doppler add? J Clin Ultrasound. 1997;25:309-316.
19. Lerner JP, Timor-Tritsch IE, Federman A, Abramovich G. Transvaginal ultrasonographic characterization of ovarian masses with an improved, weighted scoring system. Am J Obstet Gynecol. 1994;170:81-85.
20. Caspi B, Appelman Z, Rabinerson D, et al. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril. 1997;68:501-505.
21. Zalel Y, Caspi B, Tepper R. Doppler flow characteristics of dermoid cysts: unique appearance of struma ovary. J Ultrasound Med. 1997;16:355-358.
22. Kupfer MC, Schwimer SR, Lebovic J. Transvaginal sonographic appearance of endometriomata: spectrum of findings. J Ultrasound Med. 1992;11:129-133.
23. Donnez J, Langerock S, Thomas K. Peritoneal fluid volume and 17ß-estradiol and progesterone concentrators in ovulatory, anovulatory and postmenopausal women. Obstet Gynecol. 1982;59:687-692.
24. Khalife S, Falcone T, Hemmings R, Cohen D. Diagnostic accuracy of transvaginal ultrasound in detecting free pelvic fluid. J Reprod Med. 1998;43:795-798.
25. Kurjak A, Schulman H, Sosic A, et al. Transvaginal ultrasound, color flow, and Doppler waveform of the postmenopausal adnexal mass. Obstet Gynecol. 1992;80:917-921.
26. Hamper UM, Sheth S, Abbas FM, et al. Transvaginal color Doppler sonography of adnexal masses: differences in blood flow impedance in benign and malignant lesions. AJR Am J Roentgenol. 1993;160:1225-1228.
27. Guerriero S, Alcazar JL, Coccia ME, et al. Complex pelvic masses as a target of evaluation of vessel distribution by color Doppler sonography for the diagnosis of adnexal malignancies. Results of a multicenter European study. J Ultrasound Med. 2002;21:1105-1111.
28. Reynolds T, Hill MC, Glassman LM. Sonography of hemorrhagic ovarian cysts. J Clin Ultrasound. 1986;14:449-453.
29. Timmerman D, Verrelst H, Bourne TH, et al. Artificial neural network models for the preoperative discrimination between malignant and benign adnexal masses. Ultrasound Obstet Gynecol. 1999;13:17-25.
30. Boll D, Geomini MAJ, Brolmann HAM, et al. The pre-operative assessment of the adnexal mass: the accuracy of clinical estimates versus clinical prediction rules. Br J Obstet Gynaecol. 2003;110:519-523.
31. Cohen LS, Escobar P, Scharm C, et al. Three-dimensional ultrasound improves the diagnostic accuracy for ovarian cancer predictors. Gynecol Oncol. 2001;82:40-48.
32. Rulin MC, Preston AL. Adnexal masses in postmenopausal women. Obstet Gynecol. 1987;70:578-581.
33. Sassone AM, Timor-Tritsch IE, Artner A, et al. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol. 1991;78:70-76.
34. Luxman D, Bergman A, Sagi J, David MP. The postmenopausal adnexal mass: correlation between ultrasonic and pathologic findings. Obstet Gynecol. 1991;77:726-728.
1. Osmers R. Sonographic evaluation of ovarian masses and its therapeutic implications [editorial]. Ultrasound Obstet Gynecol. 1996;8:217-222.
2. Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin. 2002;52:23-47.
3. Koonings PP, Campbell K, Mishell DL, Grimes DA. Relative frequency of primary neoplasms: ten year review. Obstet Gynecol. 1989;74:921-926.
4. Randall TC, Rubin SC. Assessing a patient’s risk for hereditary ovarian cancer. OBG Manage. 1998;10:37-46.
5. Schildkraut JM, Thompson WD. Familial ovarian cancer: a population-based case-control study. Am J Epidemiol. 1988;128:456-466.
6. NIH Consensus Development Panel on Ovarian Cancer Ovarian cancer-screening, treatment and follow-up. JAMA. 1995;273:491-497.
7. Piver MS, Recio FO. When is ovarian cancer screening helpful? Contemp Ob-Gyn. 1993;38:17-32.
8. Carlson KJ, Kates SJ, Singer DE. Screening for ovarian cancer. Ann Intern Med. 1994;121:124-132.
9. Stephenson WM, Laing FC. Sonography of ovarian fibromas. AJR Am J Roentgenol. 1985;144:1239-1240.
10. Athey PA, Malone RS. Sonography of ovarian fibromas/thecomas. J Ultrasound Med. 1987;6:431-436.
11. Osmers RGW, Osmers M, VonMaydell B, Wagner B, Kuhn W. Preoperative evaluation of ovarian tumors in the premenopause by transvaginosonography. Am J Obstet Gynecol. 1996;175:428-434.
12. Ekerhovd E, Wienerroith H, Staudach A, Granberg S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: a comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am J Obstet Gynecol. 2001;184:48-54.
13. Granberg S, Wikland M, Jansson I. Macroscopic characterization of ovarian tumors and the relation to the histologic diagnosis: criteria to be used for ultrasound evaluation. Gynecol Oncol. 1989;35:139-144.
14. Sutton CL, McKinney CD, Jones JE, et al. Ovarian masses revisited: radiologic and pathologic correlation. Radiographics. 1992;12:853-877.
15. Granberg S, Norstrom A, Wikland M. Tumors in the lower pelvis as imaged by vaginal sonography. Gynecol Oncol. 1990;37:224-229.
16. Timmerman D, Bourne TH, Tailor A, et al. A comparison of methods for preoperative discrimination between malignant and benign adnexal masses: the development of a new logistic regression model. Am J Obstet Gynecol. 1999;181:57-65.
17. Ranney B, Ahmad MI. Early identification, differentiation and treatment of ovarian neoplasia. Int J Gynaecol Obstet. 1979;17:209-218.
18. Kurjak A, Kupesic S, Babic MM, et al. Preoperative evaluation of cystic teratoma: what does color Doppler add? J Clin Ultrasound. 1997;25:309-316.
19. Lerner JP, Timor-Tritsch IE, Federman A, Abramovich G. Transvaginal ultrasonographic characterization of ovarian masses with an improved, weighted scoring system. Am J Obstet Gynecol. 1994;170:81-85.
20. Caspi B, Appelman Z, Rabinerson D, et al. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril. 1997;68:501-505.
21. Zalel Y, Caspi B, Tepper R. Doppler flow characteristics of dermoid cysts: unique appearance of struma ovary. J Ultrasound Med. 1997;16:355-358.
22. Kupfer MC, Schwimer SR, Lebovic J. Transvaginal sonographic appearance of endometriomata: spectrum of findings. J Ultrasound Med. 1992;11:129-133.
23. Donnez J, Langerock S, Thomas K. Peritoneal fluid volume and 17ß-estradiol and progesterone concentrators in ovulatory, anovulatory and postmenopausal women. Obstet Gynecol. 1982;59:687-692.
24. Khalife S, Falcone T, Hemmings R, Cohen D. Diagnostic accuracy of transvaginal ultrasound in detecting free pelvic fluid. J Reprod Med. 1998;43:795-798.
25. Kurjak A, Schulman H, Sosic A, et al. Transvaginal ultrasound, color flow, and Doppler waveform of the postmenopausal adnexal mass. Obstet Gynecol. 1992;80:917-921.
26. Hamper UM, Sheth S, Abbas FM, et al. Transvaginal color Doppler sonography of adnexal masses: differences in blood flow impedance in benign and malignant lesions. AJR Am J Roentgenol. 1993;160:1225-1228.
27. Guerriero S, Alcazar JL, Coccia ME, et al. Complex pelvic masses as a target of evaluation of vessel distribution by color Doppler sonography for the diagnosis of adnexal malignancies. Results of a multicenter European study. J Ultrasound Med. 2002;21:1105-1111.
28. Reynolds T, Hill MC, Glassman LM. Sonography of hemorrhagic ovarian cysts. J Clin Ultrasound. 1986;14:449-453.
29. Timmerman D, Verrelst H, Bourne TH, et al. Artificial neural network models for the preoperative discrimination between malignant and benign adnexal masses. Ultrasound Obstet Gynecol. 1999;13:17-25.
30. Boll D, Geomini MAJ, Brolmann HAM, et al. The pre-operative assessment of the adnexal mass: the accuracy of clinical estimates versus clinical prediction rules. Br J Obstet Gynaecol. 2003;110:519-523.
31. Cohen LS, Escobar P, Scharm C, et al. Three-dimensional ultrasound improves the diagnostic accuracy for ovarian cancer predictors. Gynecol Oncol. 2001;82:40-48.
32. Rulin MC, Preston AL. Adnexal masses in postmenopausal women. Obstet Gynecol. 1987;70:578-581.
33. Sassone AM, Timor-Tritsch IE, Artner A, et al. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol. 1991;78:70-76.
34. Luxman D, Bergman A, Sagi J, David MP. The postmenopausal adnexal mass: correlation between ultrasonic and pathologic findings. Obstet Gynecol. 1991;77:726-728.