User login
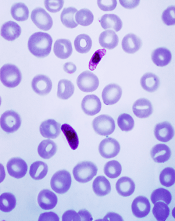
Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()
Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()
Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()