User login
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
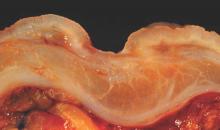
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High stress levels independently predicted peptic ulcers.
Major finding: After adjustment for other risk factors, every one-point increase on a 12-item stress questionnaire increased the odds of peptic ulcers by 12% (OR, 1.12; 95% CI, 1.01-1.23).
Data source: Prospective, population-based study of 76 patients with peptic ulcers.
Disclosures: The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.