User login
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD MAN went to his primary care physician for his annual physical. He told his physician that for the past few years, he had intermittent, painless rectal bleeding consisting of small amounts of blood on the toilet paper after defecation. He also mentioned that he often spontaneously awoke, very early in the morning. His past medical history was unremarkable.
The patient was born in Cuba but had lived in the United States for more than 30 years. He was divorced, lived alone, and had no children. He had traveled to Latin America—including Mexico, Brazil, and Cuba—off and on over the past 10 years. His last trip was approximately 2 years ago.
His physical exam was unremarkable. Rectal examination revealed no masses or external hemorrhoids; stool was brown and Hemoccult negative. Labs were remarkable for eosinophilia ranging from 10% to 24% over the past several years (the white blood cell count ranged from 5200 to 5900/mcL).
A subsequent colonoscopy revealed many white, thin, motile organisms dispersed throughout the colon (FIGURE 1). The organisms were most densely populated in the cecum. Of note, the patient also had nonbleeding internal hemorrhoids. An aspiration of the organisms was obtained and sent to the microbiology lab for further evaluation. Wet preparation microscopy is shown below (FIGURE 2).
FIGURE 1
Motile worms
Multiple motile worms were found on colonoscopy, dispersed throughout the colon. The worms were concentrated in the right colon.
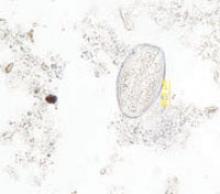
FIGURE 2
Ova
Aspiration on colonoscopy revealed football-shaped eggs that were flat on one side.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Enterobiasis
The colonoscopy and aspiration results revealed Enterobius vermicularis, or pinworm infection. E vermicularis is the most common intestinal parasite seen by primary care physicians in North America and has a wide geographic distribution.1 In the United States, more than 40 million people are estimated to be infected with pinworm, and up to 30% are children.2 Adult worms are not commonly found on colonoscopy, in part because endoscopists are not anticipating them.3
Upon further questioning after the colonoscopy, our patient reported having “worms” as a child and being treated for them. He denied recent symptoms of perianal itching. He also denied a recent history of contact with children.
Infection is via the fecal-oral route
The life cycle of E vermicularis consists of egg, larvae, and adult worm stages. Infection occurs by the fecal-oral route, with hosts including humans and cockroaches.4
The adult pinworm is very small (females average 10 mm in length; males are 4 mm in length) with a lifespan of 1 to 2 months. Infection begins with ingestion of ova, which hatch in the duodenum. The larvae mature into adult worms as they migrate through the small intestine. The adult worms then reside in the cecum, and occasionally the appendix.
The gravid female worms migrate to the perianal region at night to deposit their eggs, laying about 15,000 eggs at once. This leads to perianal itching. Reinfection occurs by hand-to-mouth transmission of the eggs from perianal scratching.1-3
Differential Dx: Roundworms, whipworms, and threadworms
Other common parasitic helminthes in the United States include Ascaris lumbricoides (roundworm) and Trichuris trichiura (whipworm). Strongyloides stercoralis (thread worm) and Necator americanus and Ancylostoma duodenale (hookworms) are less common here but should be considered in immigrants, such as our patient. Tapeworms are another parasitic helminth, but tend to be flat in appearance, unlike the worms in this case.
Roundworms are the largest of the parasitic helminthes listed here, and are common in the southeastern states’ rural population. Larvae penetrate the intestine, enter the lymphatics, and travel to the lungs. Here they may cause Loffler’s pneumonia, which is usually self-limited (lasting 1-2 weeks) and often goes undiagnosed. Juvenile worms are coughed up and swallowed, returning to the small intestine, where they mature and survive for 12 to 18 months.1
The whipworm is found in the southeastern states, but is more common in immigrants and migrant workers. A portion of the helminth burrows into the intestinal wall and may cause mild anemia, diarrhea, symptoms of inflammatory bowel disease, or rectal prolapse.1
Threadworms are prevalent throughout the tropical eastern hemisphere and are most commonly found in immigrants. Larvae penetrate the skin, migrate through the bloodstream to the lungs, and are coughed up and swallowed. The filariform stage penetrates the anal skin or intestinal mucosa, perpetuating infection, which may persist for 40 years—long after the patient has immigrated. Clinical presentation includes pruritus ani, pneumonia, abdominal cramping, and colitis.1
Hookworms have a similar geographic distribution to the threadworm. Necator americanus is the most prevalent hookworm in the United States, found in the southeast. Like the threadworm, larvae penetrate the skin, usually the feet, causing a rash. They migrate to the lungs, where they are coughed up and swallowed. In the intestines, they consume blood and cause iron deficiency anemia. Other symptoms include fatigue, failure to thrive, and depression. These worms may persist for 15 years.1
Some patients have itching, others are asymptomatic
The classic presentation of pinworm infection includes perianal itching that is worse at night and is associated with sleep disturbances, which our patient experienced. However, the vast majority of patients are asymptomatic, leading to underdiagnosis of the infection.2 This patient’s only complaint was intermittent rectal bleeding, which was likely due to his hemorrhoids.
More common presentations include abdominal pain, anorexia, weight loss, and diarrhea. However, case reports have described a variety of presentations, some with significant morbidity and mortality, often related to migration of the worms into the genitourinary tract and pelvic cavity.3 These include vulvovaginitis, pelvic inflammatory disease, pelvic abscesses and granulomas, urinary tract infections, prostatitis, epididymitis, appendicitis, enterocolitis, and bowel obstruction.3,5-7Physical exam findings may include perianal excoriation, with or without bacterial superinfection.
The Scotch tape test clinches the diagnosis
The “Scotch tape test” is the most commonly used diagnostic test for pinworm infection. A clinician applies a piece of clear cellulose acetate tape to the unwashed perianal skin in the morning on 3 separate occasions. He or she then applies the tape to glass slides and sends them to the lab.1
The characteristic findings are long, oval, colorless eggs, 50 to 60 micrometers in length, which are flat on one side (FIGURE 2).
The patient’s perianal area may also be examined with a flashlight late at night or early in the morning; occasionally glistening adult worms are found. Stool samples are often negative for worms and eggs; thus, stool examination is rarely helpful.
Tx: Antiparasitics for patients and others in household
Patients with pinworm infection are initially treated with 1 dose of oral mebendazole (100 mg), albendazole (400 mg), or pyrantel pamoate (11 mg/kg, maximum dose 1 g) (strength of recommendation [SOR] B).8-10 Some sources suggest pregnant patients be treated with pyrantel pamoate (a Category C drug in pregnancy), whereas others recommend deferring treatment until after delivery, as harm to the fetus by pinworm infection has not been reported in the literature (SOR C).1,3,11
Regardless of which antiparasitic is used, treatment should be repeated after 10 to 14 days, given the high relapse rate. Repeat treatment is especially important with mebendazole, which is active only against worms—not eggs.
Household members should also be treated, as the infection is readily transmitted and others may have asymptomatic infection (SOR B).1,3,12 In order to prevent reinoculation or spread of the infection, patients should practice good hand hygiene, including trimming their fingernails. The patient and family members should wash all sheets, clothes, and towels. Pets need not be treated, as they cannot serve as reservoirs.1,3
A good outcome. We treated the patient with mebendazole 100 mg once and repeated treatment 10 days later. We taught the patient how to prevent reinfection, and we asked him to follow-up at the clinic, as needed.
1. Juckett G. Common intestinal helminths. Am Fam Physician. 1995;52:2039-2041.
2. Weller PF, Nutman TB. Intestinal nematodes. In: Kasper Dl, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1259.
3. Petro M, Iavu K, Minocha A. Unusual endoscopic and microscopic view of Enterobius vermicularis: a case report with a review of the literature. South Med J. 2005;98:927-929.
4. Chan OT, Lee EK, Hardman JM, et al. The cockroach as a host for Trichinella and Enterobius vermicularis: implications for public health. Hawaii Med J. 2004;63:74-77.
5. Jardine M, Kokai GK, Dalzell AM. Enterobius vermicularis and colitis in children. J Pediatr Gastroenterol Nutr. 2006;43:610-612.
6. da Silva DF, da Silva RJ, da Silva MG, et al. Parasitic infection of the appendix as a cause of acute appendicitis. Parasitol Res. 2007;102:99-102.
7. Zahariou A, Karamouti M, Papaioannou P. Enterobius vermicularis in the male urinary tract: a case report. J Med Case Reports. 2007;1:137-Available at: www.jmedicalcasereports.com/content/1/1/137. Accessed July 9, 2008.
8. Horton J. Albendazole: a review of antihelmintic efficacy and safety in humans. Parasitology. 2000;121(suppl):S113-S132.
9. St Georgiev V. Chemotherapy of enterobiasis (oxyuriasis). Expert Opin Pharmacother. 2001;2:267-275.
10. Jagota SC. Albendazole, a broad-spectrum anthelmintic, in the treatment of intestinal nematode and cestode infection: a multicenter study in 480 patients. Clin Ther. 1986;8:226-231.
11. Hamblin J, Connor PD. Pinworms in pregnancy. J Am Board Fam Pract. 1995;8:321-324.
12. Yang YS, Kim SW, Jung SH, et al. Chemotherapeutic trial to control enterobiasis in schoolchildren. Korean J Parasitol. 1997;35:265-269.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD MAN went to his primary care physician for his annual physical. He told his physician that for the past few years, he had intermittent, painless rectal bleeding consisting of small amounts of blood on the toilet paper after defecation. He also mentioned that he often spontaneously awoke, very early in the morning. His past medical history was unremarkable.
The patient was born in Cuba but had lived in the United States for more than 30 years. He was divorced, lived alone, and had no children. He had traveled to Latin America—including Mexico, Brazil, and Cuba—off and on over the past 10 years. His last trip was approximately 2 years ago.
His physical exam was unremarkable. Rectal examination revealed no masses or external hemorrhoids; stool was brown and Hemoccult negative. Labs were remarkable for eosinophilia ranging from 10% to 24% over the past several years (the white blood cell count ranged from 5200 to 5900/mcL).
A subsequent colonoscopy revealed many white, thin, motile organisms dispersed throughout the colon (FIGURE 1). The organisms were most densely populated in the cecum. Of note, the patient also had nonbleeding internal hemorrhoids. An aspiration of the organisms was obtained and sent to the microbiology lab for further evaluation. Wet preparation microscopy is shown below (FIGURE 2).
FIGURE 1
Motile worms
Multiple motile worms were found on colonoscopy, dispersed throughout the colon. The worms were concentrated in the right colon.
FIGURE 2
Ova
Aspiration on colonoscopy revealed football-shaped eggs that were flat on one side.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Enterobiasis
The colonoscopy and aspiration results revealed Enterobius vermicularis, or pinworm infection. E vermicularis is the most common intestinal parasite seen by primary care physicians in North America and has a wide geographic distribution.1 In the United States, more than 40 million people are estimated to be infected with pinworm, and up to 30% are children.2 Adult worms are not commonly found on colonoscopy, in part because endoscopists are not anticipating them.3
Upon further questioning after the colonoscopy, our patient reported having “worms” as a child and being treated for them. He denied recent symptoms of perianal itching. He also denied a recent history of contact with children.
Infection is via the fecal-oral route
The life cycle of E vermicularis consists of egg, larvae, and adult worm stages. Infection occurs by the fecal-oral route, with hosts including humans and cockroaches.4
The adult pinworm is very small (females average 10 mm in length; males are 4 mm in length) with a lifespan of 1 to 2 months. Infection begins with ingestion of ova, which hatch in the duodenum. The larvae mature into adult worms as they migrate through the small intestine. The adult worms then reside in the cecum, and occasionally the appendix.
The gravid female worms migrate to the perianal region at night to deposit their eggs, laying about 15,000 eggs at once. This leads to perianal itching. Reinfection occurs by hand-to-mouth transmission of the eggs from perianal scratching.1-3
Differential Dx: Roundworms, whipworms, and threadworms
Other common parasitic helminthes in the United States include Ascaris lumbricoides (roundworm) and Trichuris trichiura (whipworm). Strongyloides stercoralis (thread worm) and Necator americanus and Ancylostoma duodenale (hookworms) are less common here but should be considered in immigrants, such as our patient. Tapeworms are another parasitic helminth, but tend to be flat in appearance, unlike the worms in this case.
Roundworms are the largest of the parasitic helminthes listed here, and are common in the southeastern states’ rural population. Larvae penetrate the intestine, enter the lymphatics, and travel to the lungs. Here they may cause Loffler’s pneumonia, which is usually self-limited (lasting 1-2 weeks) and often goes undiagnosed. Juvenile worms are coughed up and swallowed, returning to the small intestine, where they mature and survive for 12 to 18 months.1
The whipworm is found in the southeastern states, but is more common in immigrants and migrant workers. A portion of the helminth burrows into the intestinal wall and may cause mild anemia, diarrhea, symptoms of inflammatory bowel disease, or rectal prolapse.1
Threadworms are prevalent throughout the tropical eastern hemisphere and are most commonly found in immigrants. Larvae penetrate the skin, migrate through the bloodstream to the lungs, and are coughed up and swallowed. The filariform stage penetrates the anal skin or intestinal mucosa, perpetuating infection, which may persist for 40 years—long after the patient has immigrated. Clinical presentation includes pruritus ani, pneumonia, abdominal cramping, and colitis.1
Hookworms have a similar geographic distribution to the threadworm. Necator americanus is the most prevalent hookworm in the United States, found in the southeast. Like the threadworm, larvae penetrate the skin, usually the feet, causing a rash. They migrate to the lungs, where they are coughed up and swallowed. In the intestines, they consume blood and cause iron deficiency anemia. Other symptoms include fatigue, failure to thrive, and depression. These worms may persist for 15 years.1
Some patients have itching, others are asymptomatic
The classic presentation of pinworm infection includes perianal itching that is worse at night and is associated with sleep disturbances, which our patient experienced. However, the vast majority of patients are asymptomatic, leading to underdiagnosis of the infection.2 This patient’s only complaint was intermittent rectal bleeding, which was likely due to his hemorrhoids.
More common presentations include abdominal pain, anorexia, weight loss, and diarrhea. However, case reports have described a variety of presentations, some with significant morbidity and mortality, often related to migration of the worms into the genitourinary tract and pelvic cavity.3 These include vulvovaginitis, pelvic inflammatory disease, pelvic abscesses and granulomas, urinary tract infections, prostatitis, epididymitis, appendicitis, enterocolitis, and bowel obstruction.3,5-7Physical exam findings may include perianal excoriation, with or without bacterial superinfection.
The Scotch tape test clinches the diagnosis
The “Scotch tape test” is the most commonly used diagnostic test for pinworm infection. A clinician applies a piece of clear cellulose acetate tape to the unwashed perianal skin in the morning on 3 separate occasions. He or she then applies the tape to glass slides and sends them to the lab.1
The characteristic findings are long, oval, colorless eggs, 50 to 60 micrometers in length, which are flat on one side (FIGURE 2).
The patient’s perianal area may also be examined with a flashlight late at night or early in the morning; occasionally glistening adult worms are found. Stool samples are often negative for worms and eggs; thus, stool examination is rarely helpful.
Tx: Antiparasitics for patients and others in household
Patients with pinworm infection are initially treated with 1 dose of oral mebendazole (100 mg), albendazole (400 mg), or pyrantel pamoate (11 mg/kg, maximum dose 1 g) (strength of recommendation [SOR] B).8-10 Some sources suggest pregnant patients be treated with pyrantel pamoate (a Category C drug in pregnancy), whereas others recommend deferring treatment until after delivery, as harm to the fetus by pinworm infection has not been reported in the literature (SOR C).1,3,11
Regardless of which antiparasitic is used, treatment should be repeated after 10 to 14 days, given the high relapse rate. Repeat treatment is especially important with mebendazole, which is active only against worms—not eggs.
Household members should also be treated, as the infection is readily transmitted and others may have asymptomatic infection (SOR B).1,3,12 In order to prevent reinoculation or spread of the infection, patients should practice good hand hygiene, including trimming their fingernails. The patient and family members should wash all sheets, clothes, and towels. Pets need not be treated, as they cannot serve as reservoirs.1,3
A good outcome. We treated the patient with mebendazole 100 mg once and repeated treatment 10 days later. We taught the patient how to prevent reinfection, and we asked him to follow-up at the clinic, as needed.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD MAN went to his primary care physician for his annual physical. He told his physician that for the past few years, he had intermittent, painless rectal bleeding consisting of small amounts of blood on the toilet paper after defecation. He also mentioned that he often spontaneously awoke, very early in the morning. His past medical history was unremarkable.
The patient was born in Cuba but had lived in the United States for more than 30 years. He was divorced, lived alone, and had no children. He had traveled to Latin America—including Mexico, Brazil, and Cuba—off and on over the past 10 years. His last trip was approximately 2 years ago.
His physical exam was unremarkable. Rectal examination revealed no masses or external hemorrhoids; stool was brown and Hemoccult negative. Labs were remarkable for eosinophilia ranging from 10% to 24% over the past several years (the white blood cell count ranged from 5200 to 5900/mcL).
A subsequent colonoscopy revealed many white, thin, motile organisms dispersed throughout the colon (FIGURE 1). The organisms were most densely populated in the cecum. Of note, the patient also had nonbleeding internal hemorrhoids. An aspiration of the organisms was obtained and sent to the microbiology lab for further evaluation. Wet preparation microscopy is shown below (FIGURE 2).
FIGURE 1
Motile worms
Multiple motile worms were found on colonoscopy, dispersed throughout the colon. The worms were concentrated in the right colon.
FIGURE 2
Ova
Aspiration on colonoscopy revealed football-shaped eggs that were flat on one side.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Enterobiasis
The colonoscopy and aspiration results revealed Enterobius vermicularis, or pinworm infection. E vermicularis is the most common intestinal parasite seen by primary care physicians in North America and has a wide geographic distribution.1 In the United States, more than 40 million people are estimated to be infected with pinworm, and up to 30% are children.2 Adult worms are not commonly found on colonoscopy, in part because endoscopists are not anticipating them.3
Upon further questioning after the colonoscopy, our patient reported having “worms” as a child and being treated for them. He denied recent symptoms of perianal itching. He also denied a recent history of contact with children.
Infection is via the fecal-oral route
The life cycle of E vermicularis consists of egg, larvae, and adult worm stages. Infection occurs by the fecal-oral route, with hosts including humans and cockroaches.4
The adult pinworm is very small (females average 10 mm in length; males are 4 mm in length) with a lifespan of 1 to 2 months. Infection begins with ingestion of ova, which hatch in the duodenum. The larvae mature into adult worms as they migrate through the small intestine. The adult worms then reside in the cecum, and occasionally the appendix.
The gravid female worms migrate to the perianal region at night to deposit their eggs, laying about 15,000 eggs at once. This leads to perianal itching. Reinfection occurs by hand-to-mouth transmission of the eggs from perianal scratching.1-3
Differential Dx: Roundworms, whipworms, and threadworms
Other common parasitic helminthes in the United States include Ascaris lumbricoides (roundworm) and Trichuris trichiura (whipworm). Strongyloides stercoralis (thread worm) and Necator americanus and Ancylostoma duodenale (hookworms) are less common here but should be considered in immigrants, such as our patient. Tapeworms are another parasitic helminth, but tend to be flat in appearance, unlike the worms in this case.
Roundworms are the largest of the parasitic helminthes listed here, and are common in the southeastern states’ rural population. Larvae penetrate the intestine, enter the lymphatics, and travel to the lungs. Here they may cause Loffler’s pneumonia, which is usually self-limited (lasting 1-2 weeks) and often goes undiagnosed. Juvenile worms are coughed up and swallowed, returning to the small intestine, where they mature and survive for 12 to 18 months.1
The whipworm is found in the southeastern states, but is more common in immigrants and migrant workers. A portion of the helminth burrows into the intestinal wall and may cause mild anemia, diarrhea, symptoms of inflammatory bowel disease, or rectal prolapse.1
Threadworms are prevalent throughout the tropical eastern hemisphere and are most commonly found in immigrants. Larvae penetrate the skin, migrate through the bloodstream to the lungs, and are coughed up and swallowed. The filariform stage penetrates the anal skin or intestinal mucosa, perpetuating infection, which may persist for 40 years—long after the patient has immigrated. Clinical presentation includes pruritus ani, pneumonia, abdominal cramping, and colitis.1
Hookworms have a similar geographic distribution to the threadworm. Necator americanus is the most prevalent hookworm in the United States, found in the southeast. Like the threadworm, larvae penetrate the skin, usually the feet, causing a rash. They migrate to the lungs, where they are coughed up and swallowed. In the intestines, they consume blood and cause iron deficiency anemia. Other symptoms include fatigue, failure to thrive, and depression. These worms may persist for 15 years.1
Some patients have itching, others are asymptomatic
The classic presentation of pinworm infection includes perianal itching that is worse at night and is associated with sleep disturbances, which our patient experienced. However, the vast majority of patients are asymptomatic, leading to underdiagnosis of the infection.2 This patient’s only complaint was intermittent rectal bleeding, which was likely due to his hemorrhoids.
More common presentations include abdominal pain, anorexia, weight loss, and diarrhea. However, case reports have described a variety of presentations, some with significant morbidity and mortality, often related to migration of the worms into the genitourinary tract and pelvic cavity.3 These include vulvovaginitis, pelvic inflammatory disease, pelvic abscesses and granulomas, urinary tract infections, prostatitis, epididymitis, appendicitis, enterocolitis, and bowel obstruction.3,5-7Physical exam findings may include perianal excoriation, with or without bacterial superinfection.
The Scotch tape test clinches the diagnosis
The “Scotch tape test” is the most commonly used diagnostic test for pinworm infection. A clinician applies a piece of clear cellulose acetate tape to the unwashed perianal skin in the morning on 3 separate occasions. He or she then applies the tape to glass slides and sends them to the lab.1
The characteristic findings are long, oval, colorless eggs, 50 to 60 micrometers in length, which are flat on one side (FIGURE 2).
The patient’s perianal area may also be examined with a flashlight late at night or early in the morning; occasionally glistening adult worms are found. Stool samples are often negative for worms and eggs; thus, stool examination is rarely helpful.
Tx: Antiparasitics for patients and others in household
Patients with pinworm infection are initially treated with 1 dose of oral mebendazole (100 mg), albendazole (400 mg), or pyrantel pamoate (11 mg/kg, maximum dose 1 g) (strength of recommendation [SOR] B).8-10 Some sources suggest pregnant patients be treated with pyrantel pamoate (a Category C drug in pregnancy), whereas others recommend deferring treatment until after delivery, as harm to the fetus by pinworm infection has not been reported in the literature (SOR C).1,3,11
Regardless of which antiparasitic is used, treatment should be repeated after 10 to 14 days, given the high relapse rate. Repeat treatment is especially important with mebendazole, which is active only against worms—not eggs.
Household members should also be treated, as the infection is readily transmitted and others may have asymptomatic infection (SOR B).1,3,12 In order to prevent reinoculation or spread of the infection, patients should practice good hand hygiene, including trimming their fingernails. The patient and family members should wash all sheets, clothes, and towels. Pets need not be treated, as they cannot serve as reservoirs.1,3
A good outcome. We treated the patient with mebendazole 100 mg once and repeated treatment 10 days later. We taught the patient how to prevent reinfection, and we asked him to follow-up at the clinic, as needed.
1. Juckett G. Common intestinal helminths. Am Fam Physician. 1995;52:2039-2041.
2. Weller PF, Nutman TB. Intestinal nematodes. In: Kasper Dl, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1259.
3. Petro M, Iavu K, Minocha A. Unusual endoscopic and microscopic view of Enterobius vermicularis: a case report with a review of the literature. South Med J. 2005;98:927-929.
4. Chan OT, Lee EK, Hardman JM, et al. The cockroach as a host for Trichinella and Enterobius vermicularis: implications for public health. Hawaii Med J. 2004;63:74-77.
5. Jardine M, Kokai GK, Dalzell AM. Enterobius vermicularis and colitis in children. J Pediatr Gastroenterol Nutr. 2006;43:610-612.
6. da Silva DF, da Silva RJ, da Silva MG, et al. Parasitic infection of the appendix as a cause of acute appendicitis. Parasitol Res. 2007;102:99-102.
7. Zahariou A, Karamouti M, Papaioannou P. Enterobius vermicularis in the male urinary tract: a case report. J Med Case Reports. 2007;1:137-Available at: www.jmedicalcasereports.com/content/1/1/137. Accessed July 9, 2008.
8. Horton J. Albendazole: a review of antihelmintic efficacy and safety in humans. Parasitology. 2000;121(suppl):S113-S132.
9. St Georgiev V. Chemotherapy of enterobiasis (oxyuriasis). Expert Opin Pharmacother. 2001;2:267-275.
10. Jagota SC. Albendazole, a broad-spectrum anthelmintic, in the treatment of intestinal nematode and cestode infection: a multicenter study in 480 patients. Clin Ther. 1986;8:226-231.
11. Hamblin J, Connor PD. Pinworms in pregnancy. J Am Board Fam Pract. 1995;8:321-324.
12. Yang YS, Kim SW, Jung SH, et al. Chemotherapeutic trial to control enterobiasis in schoolchildren. Korean J Parasitol. 1997;35:265-269.
1. Juckett G. Common intestinal helminths. Am Fam Physician. 1995;52:2039-2041.
2. Weller PF, Nutman TB. Intestinal nematodes. In: Kasper Dl, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1259.
3. Petro M, Iavu K, Minocha A. Unusual endoscopic and microscopic view of Enterobius vermicularis: a case report with a review of the literature. South Med J. 2005;98:927-929.
4. Chan OT, Lee EK, Hardman JM, et al. The cockroach as a host for Trichinella and Enterobius vermicularis: implications for public health. Hawaii Med J. 2004;63:74-77.
5. Jardine M, Kokai GK, Dalzell AM. Enterobius vermicularis and colitis in children. J Pediatr Gastroenterol Nutr. 2006;43:610-612.
6. da Silva DF, da Silva RJ, da Silva MG, et al. Parasitic infection of the appendix as a cause of acute appendicitis. Parasitol Res. 2007;102:99-102.
7. Zahariou A, Karamouti M, Papaioannou P. Enterobius vermicularis in the male urinary tract: a case report. J Med Case Reports. 2007;1:137-Available at: www.jmedicalcasereports.com/content/1/1/137. Accessed July 9, 2008.
8. Horton J. Albendazole: a review of antihelmintic efficacy and safety in humans. Parasitology. 2000;121(suppl):S113-S132.
9. St Georgiev V. Chemotherapy of enterobiasis (oxyuriasis). Expert Opin Pharmacother. 2001;2:267-275.
10. Jagota SC. Albendazole, a broad-spectrum anthelmintic, in the treatment of intestinal nematode and cestode infection: a multicenter study in 480 patients. Clin Ther. 1986;8:226-231.
11. Hamblin J, Connor PD. Pinworms in pregnancy. J Am Board Fam Pract. 1995;8:321-324.
12. Yang YS, Kim SW, Jung SH, et al. Chemotherapeutic trial to control enterobiasis in schoolchildren. Korean J Parasitol. 1997;35:265-269.