User login
The 2011 State of Hospital Medicine report offers some tantalizing insights into the operation of academic hospital medicine practices and how they compare with their nonacademic peers. Some results are not surprising, such as the fact that academic hospital medicine groups tend to be larger than nonacademic groups, and that compensation and clinical-FTE-adjusted productivity both tend to be lower for academic hospitalists. Interestingly, turnover rates were about the same in academic and nonacademic practices.
Among the more unexpected findings, however, is that academic HM practices tend to employ a higher proportion of women (44%) than nonacademic practices (35%). In addition, academic practices employed a wider range of staffing models, with only 43% of practices using shift-based staffing, compared with 78% of nonacademic respondents. Similarly, only 47% of academic groups provided on-site coverage at night, compared with 81% of nonacademic groups.
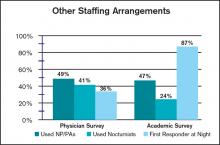
Additional differences between the way academic and nonacademic HM groups staff their programs are shown in the table, “Other Staffing Arrangements.” While the use of nurse practitioners and physician assistants (PA) was similar for academic and nonacademic practices, academic groups were much less likely to utilize nocturnists, and far more likely to have a nonphysician first responder at night (resident, nonphysician provider/PA, or other) than nonacademic groups.
It will be interesting to follow these trends over time. Because of new resident work-hour limits that went into effect in July, SHM Practice Analysis Committee (PAC) member Andrew White, MD, expects that there will be very few places that continue to use residents to cross-cover at night. “I suspect most academic centers have or will hire nocturnists,” he says, “but we’ll see.”
On the other hand, PAC member Scarlett Blue, RN, believes that continued growth in HM, coupled with a competitive job market, could result in increased use of nonphysician first responders at night—and in general. “Hospital medicine group leaders who are looking for alternative ways to meet the supply-demand conundrum may find a blended physician-NP/PA team to be one such answer,” she says.
Finally, the clinical services provided by academic HM groups vary from their nonacademic counterparts in some other important ways. Only 25% of academic practices provide care for ICU patients, compared with 78% of nonacademic practices, while 75% of academic groups perform procedures, compared with only 52% of nonacademic groups. And while the overwhelming majority of both academic and nonacademic practices provide surgical comanagement, academic practices were more than twice as likely to provide comanagement for medical subspecialty patients (45%, compared with 20% for nonacademic practices).
PAC member Troy Ahlstrom, MD, explains, tongue-in-cheek, that “academic hospitalists don’t do procedures because they have oodles of residents, fellows, and interventional radiologists to do them instead, and academics do more medical comanagement because the subspecialist who only does Waldenstrom’s macroglobulinemia probably doesn’t do diabetes.”
Whatever the reason, there are meaningful differences between academic and nonacademic HM practices that bear watching over time. You can help us identify and track these differences by ensuring that your group participates in SHM’s annual State of Hospital Medicine survey, launching this month.
The 2011 State of Hospital Medicine report offers some tantalizing insights into the operation of academic hospital medicine practices and how they compare with their nonacademic peers. Some results are not surprising, such as the fact that academic hospital medicine groups tend to be larger than nonacademic groups, and that compensation and clinical-FTE-adjusted productivity both tend to be lower for academic hospitalists. Interestingly, turnover rates were about the same in academic and nonacademic practices.
Among the more unexpected findings, however, is that academic HM practices tend to employ a higher proportion of women (44%) than nonacademic practices (35%). In addition, academic practices employed a wider range of staffing models, with only 43% of practices using shift-based staffing, compared with 78% of nonacademic respondents. Similarly, only 47% of academic groups provided on-site coverage at night, compared with 81% of nonacademic groups.
Additional differences between the way academic and nonacademic HM groups staff their programs are shown in the table, “Other Staffing Arrangements.” While the use of nurse practitioners and physician assistants (PA) was similar for academic and nonacademic practices, academic groups were much less likely to utilize nocturnists, and far more likely to have a nonphysician first responder at night (resident, nonphysician provider/PA, or other) than nonacademic groups.
It will be interesting to follow these trends over time. Because of new resident work-hour limits that went into effect in July, SHM Practice Analysis Committee (PAC) member Andrew White, MD, expects that there will be very few places that continue to use residents to cross-cover at night. “I suspect most academic centers have or will hire nocturnists,” he says, “but we’ll see.”
On the other hand, PAC member Scarlett Blue, RN, believes that continued growth in HM, coupled with a competitive job market, could result in increased use of nonphysician first responders at night—and in general. “Hospital medicine group leaders who are looking for alternative ways to meet the supply-demand conundrum may find a blended physician-NP/PA team to be one such answer,” she says.
Finally, the clinical services provided by academic HM groups vary from their nonacademic counterparts in some other important ways. Only 25% of academic practices provide care for ICU patients, compared with 78% of nonacademic practices, while 75% of academic groups perform procedures, compared with only 52% of nonacademic groups. And while the overwhelming majority of both academic and nonacademic practices provide surgical comanagement, academic practices were more than twice as likely to provide comanagement for medical subspecialty patients (45%, compared with 20% for nonacademic practices).
PAC member Troy Ahlstrom, MD, explains, tongue-in-cheek, that “academic hospitalists don’t do procedures because they have oodles of residents, fellows, and interventional radiologists to do them instead, and academics do more medical comanagement because the subspecialist who only does Waldenstrom’s macroglobulinemia probably doesn’t do diabetes.”
Whatever the reason, there are meaningful differences between academic and nonacademic HM practices that bear watching over time. You can help us identify and track these differences by ensuring that your group participates in SHM’s annual State of Hospital Medicine survey, launching this month.
The 2011 State of Hospital Medicine report offers some tantalizing insights into the operation of academic hospital medicine practices and how they compare with their nonacademic peers. Some results are not surprising, such as the fact that academic hospital medicine groups tend to be larger than nonacademic groups, and that compensation and clinical-FTE-adjusted productivity both tend to be lower for academic hospitalists. Interestingly, turnover rates were about the same in academic and nonacademic practices.
Among the more unexpected findings, however, is that academic HM practices tend to employ a higher proportion of women (44%) than nonacademic practices (35%). In addition, academic practices employed a wider range of staffing models, with only 43% of practices using shift-based staffing, compared with 78% of nonacademic respondents. Similarly, only 47% of academic groups provided on-site coverage at night, compared with 81% of nonacademic groups.
Additional differences between the way academic and nonacademic HM groups staff their programs are shown in the table, “Other Staffing Arrangements.” While the use of nurse practitioners and physician assistants (PA) was similar for academic and nonacademic practices, academic groups were much less likely to utilize nocturnists, and far more likely to have a nonphysician first responder at night (resident, nonphysician provider/PA, or other) than nonacademic groups.
It will be interesting to follow these trends over time. Because of new resident work-hour limits that went into effect in July, SHM Practice Analysis Committee (PAC) member Andrew White, MD, expects that there will be very few places that continue to use residents to cross-cover at night. “I suspect most academic centers have or will hire nocturnists,” he says, “but we’ll see.”
On the other hand, PAC member Scarlett Blue, RN, believes that continued growth in HM, coupled with a competitive job market, could result in increased use of nonphysician first responders at night—and in general. “Hospital medicine group leaders who are looking for alternative ways to meet the supply-demand conundrum may find a blended physician-NP/PA team to be one such answer,” she says.
Finally, the clinical services provided by academic HM groups vary from their nonacademic counterparts in some other important ways. Only 25% of academic practices provide care for ICU patients, compared with 78% of nonacademic practices, while 75% of academic groups perform procedures, compared with only 52% of nonacademic groups. And while the overwhelming majority of both academic and nonacademic practices provide surgical comanagement, academic practices were more than twice as likely to provide comanagement for medical subspecialty patients (45%, compared with 20% for nonacademic practices).
PAC member Troy Ahlstrom, MD, explains, tongue-in-cheek, that “academic hospitalists don’t do procedures because they have oodles of residents, fellows, and interventional radiologists to do them instead, and academics do more medical comanagement because the subspecialist who only does Waldenstrom’s macroglobulinemia probably doesn’t do diabetes.”
Whatever the reason, there are meaningful differences between academic and nonacademic HM practices that bear watching over time. You can help us identify and track these differences by ensuring that your group participates in SHM’s annual State of Hospital Medicine survey, launching this month.