User login
NEW YORK – Endovascular vs. open repair for ruptured aortic aneurysms has long been a source of controversy, but results of a multicenter international study indicate superior long-term survival with EVAR.
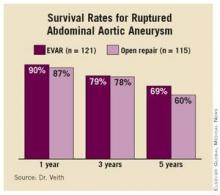
The study, which compared results from 121 patients who underwent EVAR vs. 115 who underwent open surgery, showed that the survival benefit from EVAR was maintained for 5 years, Dr. Frank Veith said at the annual meeting of the Eastern Vascular Society. “Of course, after 6 years there was catch-up because these were old, sick patients who died due to natural causes,” he added. But he emphasized that “the superiority of EVAR over open repair for ruptured abdominal aortic aneurysm is strongly supported in the long-term as well as the short-term data.” (See box.)
Dr. Veith of New York University and a visiting professor at Zurich University, presented the results on behalf of the Zurich group.
Results of other studies support the Zurich group’s conclusion that EVAR should become the standard of care for all patients with ruptured abdominal aortic aneurysm (AAA) who have suitable anatomy, Dr. Veith said. He cited a preliminary study by the Zurich group that looked at outcomes in a limited cohort at 2 years (J. Vasc. Surg. 2005;41:752-7) and another study from the Netherlands that looked at short-term outcomes in 187 patients (J. Vasc. Surg. 2008;48:1396-1400). He also noted that a U.K. study that followed 54 EVAR patients over a 10-year period found no survival advantage over open repair (Vascular 2007;15:191-6).
However, an unpublished 2009 analysis showed a 30-day mortality rate of 21% in EVAR patients, “comparing favorably with open repair,” Dr. Veith said. The “most important data” in this study were “from the 13 centers like our own that did EVAR on all anatomically suitable ruptured AAA patients,” he said. “We collected 680 ruptured AAA patients by EVAR and 763 by open repair by the same surgeons in the same institutions, and the 30-day mortality was dramatically better for EVAR” (19.7% vs. 36.3%), he said.
In the Zurich group’s study, growing numbers of suitable patients underwent EVAR for ruptured AAA between 1998 and 2009. “The increasing use of EVAR was related to increasing experience, increasing enthusiasm, and better devices,” Dr. Veith said. The average age of patients in the study was 72 years, and the investigators followed the patients with annual angiography, CT scan, and physical examination. All but two of the 103 surviving patients who had EVAR were followed long term.
The actual survival rate of all early EVAR patients was 62% in the Zurich study, Dr. Veith said. “In terms of quality of life, 86% of these patients were living at home, 78% were independent in their lifestyle, and 81% considered their quality of life to be good to excellent,” he added.
Dr. Julie Freischlag, chair of the department of surgery at Johns Hopkins Hospital, Baltimore, and coauthor of the Veterans Affairs Cooperative Study Group report comparing EVAR and open repair for ruptured AAA (JAMA 2009;302:1535-42), said she concurred with the conclusions that Dr. Veith reported. “We were real excited about that, because if you had to prove to the government why you should spend extra money to do an endovascular graft repair, one reason would be to increase survival, so we’re glad to see this,” she said.
Dr. Veith had no relevant disclosures.
NEW YORK – Endovascular vs. open repair for ruptured aortic aneurysms has long been a source of controversy, but results of a multicenter international study indicate superior long-term survival with EVAR.
The study, which compared results from 121 patients who underwent EVAR vs. 115 who underwent open surgery, showed that the survival benefit from EVAR was maintained for 5 years, Dr. Frank Veith said at the annual meeting of the Eastern Vascular Society. “Of course, after 6 years there was catch-up because these were old, sick patients who died due to natural causes,” he added. But he emphasized that “the superiority of EVAR over open repair for ruptured abdominal aortic aneurysm is strongly supported in the long-term as well as the short-term data.” (See box.)
Dr. Veith of New York University and a visiting professor at Zurich University, presented the results on behalf of the Zurich group.
Results of other studies support the Zurich group’s conclusion that EVAR should become the standard of care for all patients with ruptured abdominal aortic aneurysm (AAA) who have suitable anatomy, Dr. Veith said. He cited a preliminary study by the Zurich group that looked at outcomes in a limited cohort at 2 years (J. Vasc. Surg. 2005;41:752-7) and another study from the Netherlands that looked at short-term outcomes in 187 patients (J. Vasc. Surg. 2008;48:1396-1400). He also noted that a U.K. study that followed 54 EVAR patients over a 10-year period found no survival advantage over open repair (Vascular 2007;15:191-6).
However, an unpublished 2009 analysis showed a 30-day mortality rate of 21% in EVAR patients, “comparing favorably with open repair,” Dr. Veith said. The “most important data” in this study were “from the 13 centers like our own that did EVAR on all anatomically suitable ruptured AAA patients,” he said. “We collected 680 ruptured AAA patients by EVAR and 763 by open repair by the same surgeons in the same institutions, and the 30-day mortality was dramatically better for EVAR” (19.7% vs. 36.3%), he said.
In the Zurich group’s study, growing numbers of suitable patients underwent EVAR for ruptured AAA between 1998 and 2009. “The increasing use of EVAR was related to increasing experience, increasing enthusiasm, and better devices,” Dr. Veith said. The average age of patients in the study was 72 years, and the investigators followed the patients with annual angiography, CT scan, and physical examination. All but two of the 103 surviving patients who had EVAR were followed long term.
The actual survival rate of all early EVAR patients was 62% in the Zurich study, Dr. Veith said. “In terms of quality of life, 86% of these patients were living at home, 78% were independent in their lifestyle, and 81% considered their quality of life to be good to excellent,” he added.
Dr. Julie Freischlag, chair of the department of surgery at Johns Hopkins Hospital, Baltimore, and coauthor of the Veterans Affairs Cooperative Study Group report comparing EVAR and open repair for ruptured AAA (JAMA 2009;302:1535-42), said she concurred with the conclusions that Dr. Veith reported. “We were real excited about that, because if you had to prove to the government why you should spend extra money to do an endovascular graft repair, one reason would be to increase survival, so we’re glad to see this,” she said.
Dr. Veith had no relevant disclosures.
NEW YORK – Endovascular vs. open repair for ruptured aortic aneurysms has long been a source of controversy, but results of a multicenter international study indicate superior long-term survival with EVAR.
The study, which compared results from 121 patients who underwent EVAR vs. 115 who underwent open surgery, showed that the survival benefit from EVAR was maintained for 5 years, Dr. Frank Veith said at the annual meeting of the Eastern Vascular Society. “Of course, after 6 years there was catch-up because these were old, sick patients who died due to natural causes,” he added. But he emphasized that “the superiority of EVAR over open repair for ruptured abdominal aortic aneurysm is strongly supported in the long-term as well as the short-term data.” (See box.)
Dr. Veith of New York University and a visiting professor at Zurich University, presented the results on behalf of the Zurich group.
Results of other studies support the Zurich group’s conclusion that EVAR should become the standard of care for all patients with ruptured abdominal aortic aneurysm (AAA) who have suitable anatomy, Dr. Veith said. He cited a preliminary study by the Zurich group that looked at outcomes in a limited cohort at 2 years (J. Vasc. Surg. 2005;41:752-7) and another study from the Netherlands that looked at short-term outcomes in 187 patients (J. Vasc. Surg. 2008;48:1396-1400). He also noted that a U.K. study that followed 54 EVAR patients over a 10-year period found no survival advantage over open repair (Vascular 2007;15:191-6).
However, an unpublished 2009 analysis showed a 30-day mortality rate of 21% in EVAR patients, “comparing favorably with open repair,” Dr. Veith said. The “most important data” in this study were “from the 13 centers like our own that did EVAR on all anatomically suitable ruptured AAA patients,” he said. “We collected 680 ruptured AAA patients by EVAR and 763 by open repair by the same surgeons in the same institutions, and the 30-day mortality was dramatically better for EVAR” (19.7% vs. 36.3%), he said.
In the Zurich group’s study, growing numbers of suitable patients underwent EVAR for ruptured AAA between 1998 and 2009. “The increasing use of EVAR was related to increasing experience, increasing enthusiasm, and better devices,” Dr. Veith said. The average age of patients in the study was 72 years, and the investigators followed the patients with annual angiography, CT scan, and physical examination. All but two of the 103 surviving patients who had EVAR were followed long term.
The actual survival rate of all early EVAR patients was 62% in the Zurich study, Dr. Veith said. “In terms of quality of life, 86% of these patients were living at home, 78% were independent in their lifestyle, and 81% considered their quality of life to be good to excellent,” he added.
Dr. Julie Freischlag, chair of the department of surgery at Johns Hopkins Hospital, Baltimore, and coauthor of the Veterans Affairs Cooperative Study Group report comparing EVAR and open repair for ruptured AAA (JAMA 2009;302:1535-42), said she concurred with the conclusions that Dr. Veith reported. “We were real excited about that, because if you had to prove to the government why you should spend extra money to do an endovascular graft repair, one reason would be to increase survival, so we’re glad to see this,” she said.
Dr. Veith had no relevant disclosures.