User login
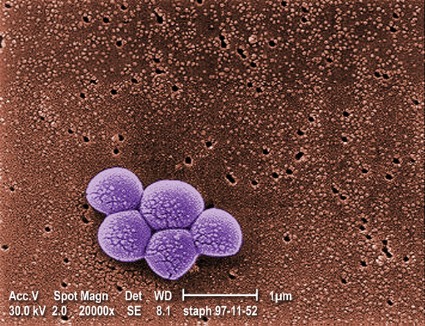
LAS VEGAS – It’s a good idea to swab both the throat and nose when looking for Staphylococcus aureus colonization; doing so picks up cases missed by swabbing the nares alone, according to researchers from the Baylor College of Medicine in Houston.
That holds true whether testing is by culture or PCR [polymerase chain reaction], said the lead investigator, Dr. Meredith Knofsky, a surgery resident there.
The team swabbed both areas preoperatively and on the day of surgery in patients undergoing operations involving hardware implants, such as new knees or hips. The 109 samples they obtained were then tested for methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) S. aureus by both MRSA select media culture and the GeneXpert PCR system.
By culture, 7 throat swabs and 18 nares swabs were positive for MRSA; 20 throat and 40 nares swabs were positive for MSSA.
By PCR, 7 throat and 21 nares samples were MRSA positive; 33 throat and 51 nares swabs were positive for MSSA.
The detection rate differences weren’t surprising; PCR is known to be more accurate and the results confirm its greater sensitivity, Dr. Knofsky said at the annual meeting of the Surgical Infection Society.
The bigger finding is that "throat screening identifies additional patients missed by screening the nares alone," she said.
Adding PCR throat testing to PCR nasal screening picked up one additional MRSA and 14 additional MSSA carriers. Similarly, the addition of throat cultures to nares cultures picked up an additional MRSA and eight additional MSSA carriers.
Not infrequently, patients were positive in one location, such as the throat, but not in the other. Although "nasal carrier status of Staphylococcus aureus is an important risk factor for surgical site infections," it’s not known at the moment if that’s also true for carriage limited to the throat, Dr. Knofsky said.
"We have plans to go back and evaluate which of these patients colonized only in the oropharynx actually developed a surgical site infection. It’s important that we invest in evaluating pharyngeal carriage," she said.
In the meantime, session moderator and surgeon Dr. E. Patchen Dellinger of the University of Washington in Seattle, noted that MSSA in the study "was two to three times more common than MRSA; an MSSA infection of implanted hardware is just as devastating to the patient as an MRSA infection. I would like to urge that we not focus on MRSA alone, but consider at least in selected surgical populations seeking and suppressing any Staph that colonizes our surgical patients."
PCR could help with that because it "has the advantage of very rapid answers. The logistics of getting [colonization] information in time to do something [before an operation] is very difficult for us. PCR could make that better, [but it] isn’t standard of care mostly because it costs a lot more" than does culture, he said.
Dr. Knofsky and Dr. Dellinger said they have no relevant disclosures.
LAS VEGAS – It’s a good idea to swab both the throat and nose when looking for Staphylococcus aureus colonization; doing so picks up cases missed by swabbing the nares alone, according to researchers from the Baylor College of Medicine in Houston.
That holds true whether testing is by culture or PCR [polymerase chain reaction], said the lead investigator, Dr. Meredith Knofsky, a surgery resident there.
The team swabbed both areas preoperatively and on the day of surgery in patients undergoing operations involving hardware implants, such as new knees or hips. The 109 samples they obtained were then tested for methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) S. aureus by both MRSA select media culture and the GeneXpert PCR system.
By culture, 7 throat swabs and 18 nares swabs were positive for MRSA; 20 throat and 40 nares swabs were positive for MSSA.
By PCR, 7 throat and 21 nares samples were MRSA positive; 33 throat and 51 nares swabs were positive for MSSA.
The detection rate differences weren’t surprising; PCR is known to be more accurate and the results confirm its greater sensitivity, Dr. Knofsky said at the annual meeting of the Surgical Infection Society.
The bigger finding is that "throat screening identifies additional patients missed by screening the nares alone," she said.
Adding PCR throat testing to PCR nasal screening picked up one additional MRSA and 14 additional MSSA carriers. Similarly, the addition of throat cultures to nares cultures picked up an additional MRSA and eight additional MSSA carriers.
Not infrequently, patients were positive in one location, such as the throat, but not in the other. Although "nasal carrier status of Staphylococcus aureus is an important risk factor for surgical site infections," it’s not known at the moment if that’s also true for carriage limited to the throat, Dr. Knofsky said.
"We have plans to go back and evaluate which of these patients colonized only in the oropharynx actually developed a surgical site infection. It’s important that we invest in evaluating pharyngeal carriage," she said.
In the meantime, session moderator and surgeon Dr. E. Patchen Dellinger of the University of Washington in Seattle, noted that MSSA in the study "was two to three times more common than MRSA; an MSSA infection of implanted hardware is just as devastating to the patient as an MRSA infection. I would like to urge that we not focus on MRSA alone, but consider at least in selected surgical populations seeking and suppressing any Staph that colonizes our surgical patients."
PCR could help with that because it "has the advantage of very rapid answers. The logistics of getting [colonization] information in time to do something [before an operation] is very difficult for us. PCR could make that better, [but it] isn’t standard of care mostly because it costs a lot more" than does culture, he said.
Dr. Knofsky and Dr. Dellinger said they have no relevant disclosures.
LAS VEGAS – It’s a good idea to swab both the throat and nose when looking for Staphylococcus aureus colonization; doing so picks up cases missed by swabbing the nares alone, according to researchers from the Baylor College of Medicine in Houston.
That holds true whether testing is by culture or PCR [polymerase chain reaction], said the lead investigator, Dr. Meredith Knofsky, a surgery resident there.
The team swabbed both areas preoperatively and on the day of surgery in patients undergoing operations involving hardware implants, such as new knees or hips. The 109 samples they obtained were then tested for methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) S. aureus by both MRSA select media culture and the GeneXpert PCR system.
By culture, 7 throat swabs and 18 nares swabs were positive for MRSA; 20 throat and 40 nares swabs were positive for MSSA.
By PCR, 7 throat and 21 nares samples were MRSA positive; 33 throat and 51 nares swabs were positive for MSSA.
The detection rate differences weren’t surprising; PCR is known to be more accurate and the results confirm its greater sensitivity, Dr. Knofsky said at the annual meeting of the Surgical Infection Society.
The bigger finding is that "throat screening identifies additional patients missed by screening the nares alone," she said.
Adding PCR throat testing to PCR nasal screening picked up one additional MRSA and 14 additional MSSA carriers. Similarly, the addition of throat cultures to nares cultures picked up an additional MRSA and eight additional MSSA carriers.
Not infrequently, patients were positive in one location, such as the throat, but not in the other. Although "nasal carrier status of Staphylococcus aureus is an important risk factor for surgical site infections," it’s not known at the moment if that’s also true for carriage limited to the throat, Dr. Knofsky said.
"We have plans to go back and evaluate which of these patients colonized only in the oropharynx actually developed a surgical site infection. It’s important that we invest in evaluating pharyngeal carriage," she said.
In the meantime, session moderator and surgeon Dr. E. Patchen Dellinger of the University of Washington in Seattle, noted that MSSA in the study "was two to three times more common than MRSA; an MSSA infection of implanted hardware is just as devastating to the patient as an MRSA infection. I would like to urge that we not focus on MRSA alone, but consider at least in selected surgical populations seeking and suppressing any Staph that colonizes our surgical patients."
PCR could help with that because it "has the advantage of very rapid answers. The logistics of getting [colonization] information in time to do something [before an operation] is very difficult for us. PCR could make that better, [but it] isn’t standard of care mostly because it costs a lot more" than does culture, he said.
Dr. Knofsky and Dr. Dellinger said they have no relevant disclosures.
AT THE SIS ANNUAL MEETING
Major finding: In an analysis of 109 throat and nares swabs, the addition of PCR throat testing to PCR nasal screening picked up one additional MRSA and 14 additional MSSA carriers. Similarly, the addition of throat cultures to nares cultures picked up an additional MRSA and eight additional MSSA carriers.
Data source: Samples from presurgical patients
Disclosures: The lead investigator said she has no disclosures.