User login
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.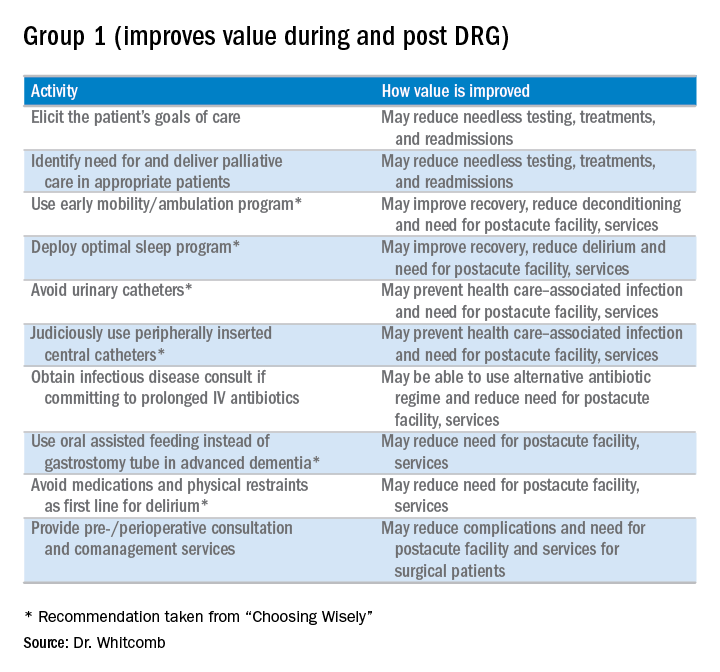
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
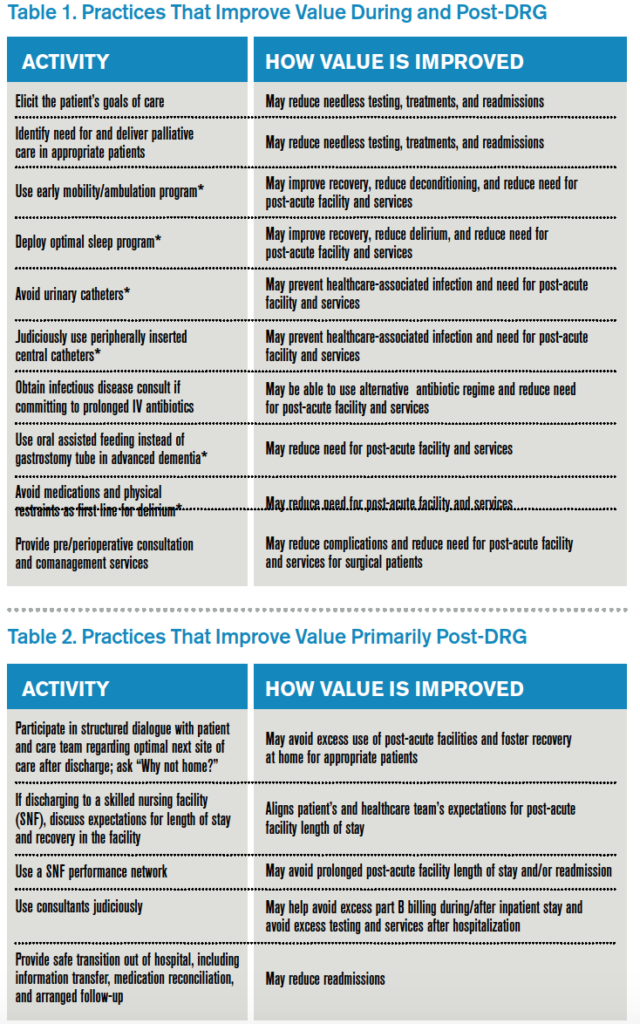
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.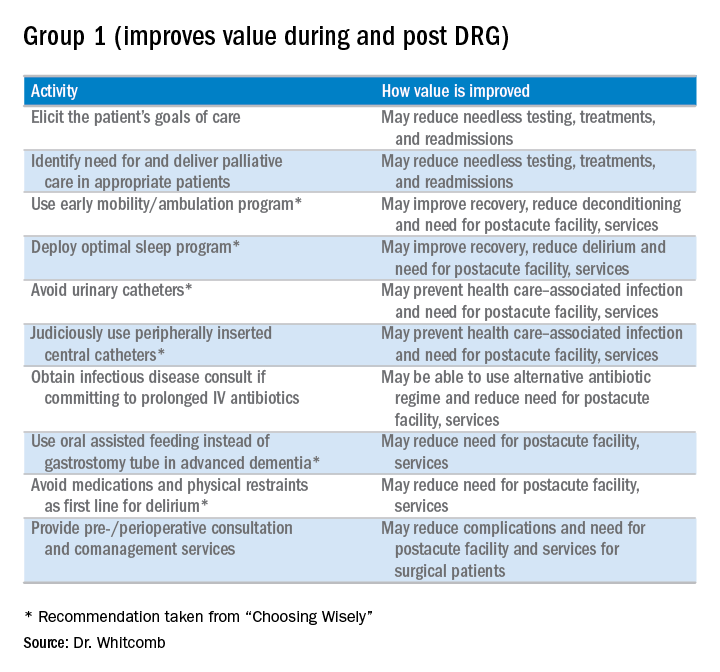
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.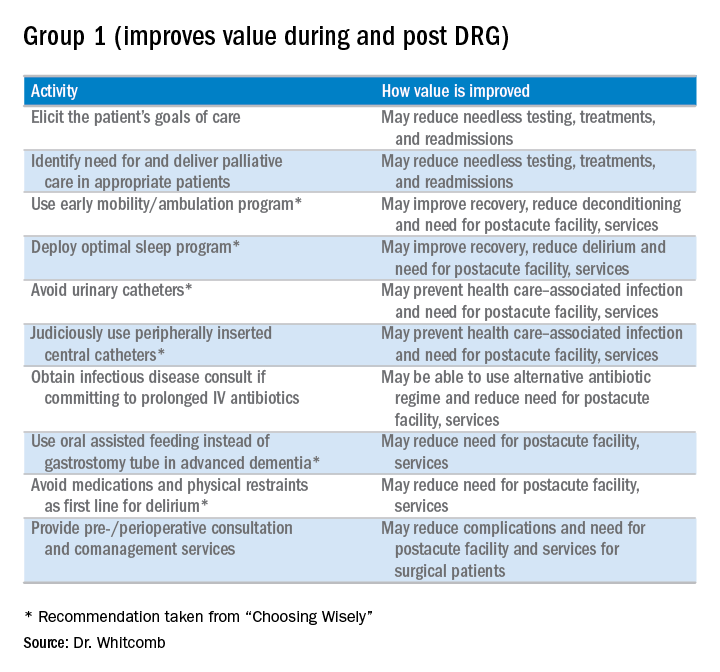
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.