User login
- For the initial evaluation of any adult who requires routine evaluation for TB exposure, administer a second TB skin test within 1 to 3 weeks if the first test result is negative.
- The workup for active TB consists of a chest x-ray film, a human immunodeficiency virus (HIV) test, and possibly sputum collection. HIV-negative persons with a normal chest x-ray result are unlikely to have pulmonary TB, and sputum collection is unnecessary.
- Contrary to common belief, there is no age cutoff for treating latent TB.
- Treat active TB with isoniazid, rifampin, and pyrazinamide. Add ethambutol if a patient is a current or former resident of an area in which bacterial resistance to isoniazid is greater than 5%.
- Refer all suspected cases of TB to your local public health department for the purpose of tracking contacts.
With the decline of tuberculosis (TB), physician familiarity with this disease has substantially diminished. Yet TB remains common in immigrants, individuals with HIV infection, and other high-risk populations. How do we remain vigilant for TB? How do we screen? How should the physician interpret TB test results? What are the preferred options for treatment? What are the public health implications of TB? This article offers an update on this recalcitrant public health problem.
Whom, and how, to screen
Two factors are key in remaining vigilant for tuberculosis: knowing who in your patient population is most at risk for exposure, and knowing who is most likely to develop active disease if infected.
Persons at risk for exposure to TB (Table 1) or at risk for developing active disease if infected (Table 2) should receive a TB skin test regularly, although the optimal frequency has not been determined. Routine testing is not indicated for others.
Proper technique. The TB skin test should be administered with intermediate-strength purified protein derivative (PPD), 0.1 mL injected intradermally, resulting in a raised bleb. The test should be read 48 to 72 hours later and the area of induration, not erythema, measured and recorded in millimeters. With no induration, the result should be recorded as 0 mm, not as “negative.”
Interpreting test results. Interpretation of the test results depends on a person’s risk factors and age. For those listed in Table 3, a 5-mm induration is considered positive; for those listed in Tables 1 and 2 who are not in Table 3 , a 10-mm induration is positive. For everyone else, 15 mm is positive.
Caveat. Multiple puncture tests, though easier to administer, do not inject a standardized amount of tuberculin into the skin; results are more difficult to interpret and, if judged reactive, must be confirmed with a PPD test. This option is not recommended for testing.
Prior receipt of the bacillus Calmette-Guerin (BCG) vaccine does not affect the interpretation of the TB skin test, nor should it affect decisions to treat latent TB. The effectiveness of BCG vaccine in preventing TB infection in highly questionable, and the reaction to PPD caused by BCG wanes after a few years.
Two-step testing. Two-step testing means administering a second TB skin test within 1 to 3 weeks if the first test result is negative. This procedure should be used for the initial evaluation of adults who require routine testing. If the second skin test result is positive, it indicates the person was infected with TB before, and that immunity has waned and was “boosted” by the first test.
Without the 2-step process, a positive result on repeat testing would suggest recent infection rather than prior exposure. This could have implications for the decision to accept or not accept treatment for latent TB.
TABLE 1
Conditions associated with high risk of exposure to tuberculosis
| Foreign-born in area with high tuberculosis rates |
| Use of illicit drugs |
Institutionalization or work in
|
| Work in health care facilities with high-risk clients |
| Socioeconomic disadvantage |
| Children of those at high risk |
TABLE 2
Conditions associated with high risk of developing active tuberculosis
| HIV infection |
| Recent infection with Mycobacterium tuberculosis |
| Chest x-ray indicating old tuberculosis |
Immunosuppression
|
| Leukemia and other cancers of blood, lymph, and bone marrow |
| Cancer of the head and neck |
| Gastrectomy or intestinal bypass |
| Chronic malabsorption |
| End-stage renal disease |
| Diabetes |
| Silicosis |
| Illicit drug use |
TABLE 3
How to interpret a tuberculosis skin test
| 5 mm considered positive in those with: |
|
| 10 mm is considered positive in: |
Work-up for suspected tuberculosis
For those suspected of having TB because of chronic cough, night sweats, fever, and weight loss, or because of a positive TB skin test result, the workup consists of a chest x-ray film, an HIV test, and possibly sputum collection for microscopic evaluation and culture.
Those with a normal chest x-ray result who are HIV-negative are unlikely to have pulmonary TB, and sputum collection is unnecessary. For those with suspicious chest x-ray films and for those who are HIV positive with TB symptoms, sputum samples are needed for microscopic evaluation and culture (3 samples, preferably on 3 consecutive days).
Acid-fast organisms seen under the microscope may be Mycobacterium tuberculosis or mycobacteria other than tuberculosis (commonly referred to as MOTT), and the final determination must await culture confirmation, which now takes about 4 weeks. Preliminary confirmation using polymerase chain reaction can be accomplished in a few days. Treatment for active TB should be initiated, however, and the suspicion reported to the local health department as soon as TB is suspected.
Treating latent and active disease
Latent tuberculosis. Treatment for latent TB (positive TB skin test result, negative chest x-ray film, HIV-negative) should not be initiated until active TB is ruled out. This may require waiting 3 to 4 weeks for sputum culture results.
Contrary to common belief, there is no age cutoff for initiation of treatment for latent TB. Treatment requires 6 to 9 months of isoniazid or 4 months of rifampin. A shorter course with pyrazinamide and rifampin is also possible, although questions about the safety of this regimen have been raised. Patient compliance for the duration of therapy is difficult to achieve; but if accomplished, the risk of active disease decreases from 10% to less than 1%. At highest risk of developing active disease are children, and those who are HIV-positive, recently infected with TB, or whose chest films indicate old disease.
Since isoniazid is hepatotoxic, patients should be asked about symptoms of liver inflammation (abdominal pain, decline in appetite, dark urine, light-colored stools), and liver function tests should be ordered if symptoms are present. Routine monthly testing of liver function tests is not necessary and is recommended only for those who have chronic liver disease, an alcohol abuse disorder, or are pregnant.
Active tuberculosis. Always initiate treatment with at least 3 drugs (isoniazid, rifampin, and pyrazinamide). Ethambutol should be added to the regimen if patients are current or former residents of an area where resistance to isoniazid is more than 5%. If the organism proves sensitive to isoniazid and rifampin, ethambutol can be discontinued. Pyrazinamide should be continued for a full 2 months, and isoniazid and rifampin for a full 6 months. A variety of protocols for dosing and administration frequency are available to enhance convenience and patient compliance. Drug regimens may have to be adjusted based on culture results and success of therapy.
The standard of care for active TB is directly observed therapy. This means watching the patient swallow the pills. Although such care is labor intensive and implies a lack of trust in the patient, with its implementation, the successful completion of therapy rises from 50% to close to 100%. Widespread use of directly observed therapy since the late 1980s has resulted in a marked reduction of TB rates and rates of bacterial resistance.
To prevent bacterial resistance to drugs, treatment for active disease must be administered according to guidelines and be completed. One cardinal rule in the prevention of bacterial resistance is never to add just 1 drug to a failing regimen.
Any deviation from standard therapy because of bacterial resistance, patient nonadherence, or adverse drug effects is reason to consult the local public health department or state public health department TB program.
Working with the public health department
Three complementary activities are needed to control TB in the community:
- Finding and treating those with active TB
- Investigating close contacts of persons with active disease and offering them treatment of latent TB
- Screening persons at high risk, to find and treat latent TB.
The detection and management of tuberculosis offers an excellent opportunity for family physicians and health departments to work collaboratively to improve the community’s health.
Family physicians can make several contributions to reducing TB’s impact on the community:
- Screen appropriately
- Correctly apply and interpret TB skin tests
- Accurately make the diagnosis of latent and active TB
- Treat active TB according to recommended guidelines
- Encourage treatment of latent TB among those at highest risk of activation
- Promptly report to the local health department those suspected of having TB
- Collaborate with the public health department to reduce the spread of disease.
Local or state public health departments assist in several ways:
- Communicate with and investigating family and other close contacts of those with active, contagious TB, to find anyone with latent or active TB
- Offer consultation on how to diagnose and treat latent and active TB
- Assist with directly observed therapy
- Use public health authority to isolate and quarantine patients who are infectious and pose a risk to the community through non-adherence to treatment and infection control guidelines.
Many public health departments have TB programs wherein patients with active or latent TB can receive free care and medication.
State and local public health departments have the responsibility of monitoring TB care provided by physicians in the community, to insure it is applied according to guidelines and that it is completed. The intrusiveness of this can be minimized with regular communication and appreciation of the roles and responsibilities of each party.
Excellent review of the basics of TB screening, diagnosis, and treatment: Centers for Disease Control and Prevention (CDC). Core Curriculum on Tuberculosis. 4th ed. Atlanta, Ga: CDC; 2000.
Self-study modules on TB: CDC. National Center for HIV, STD, and TB Prevention, Divisionof Tuberculosis Elimination. Available at: www.phppo.cdc.gov/PHTN/tbmodules.(Accessed on September 8, 2003.)
Training modules and statistics on TB diagnosis, treatment, and epidemiology, including state-specific analyses: CDC. National Center for HIV, STD, and TB Prevention. Division of Tuberculosis Elimination. Available at: www.cdc.gov/nchstp/tb/default.htm. (Accessedon September 8, 2003.)
The most recent, comprehensive description of TB treatment recommendations: Blumberg HM, Burman WJ, Chaisson RE, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med 2003; 167:603–662.
Prospects and trends
More reliable testing. The TB skin test is an imperfect screening tool. The development of a blood test for TB antibodies has progressed and will be evaluated and standardized. It will likely be a useful clinical and epidemiological tool in the near future.
Tuberculosis secondary to HIV. By some indicators, the rate of HIV infections has recently increased. This factor, combined with the increased life span of those with HIV, has the potential for reversing some of the recent progress in slowing TB rates. The continued development of anti-HIV medications and availability of the medications through AIDS/HIV treatment programs could help make those who are HIV infected less susceptible to TB infection and disease activation.
Tuberculosis and immigration. It is likely that as endemic TB declines in the US, a higher proportion of TB infections will occur in those who are foreign born and move to this country (see “Trends reversing in tuberculosis”). This underscores the global nature of public health and the importance of international collaboration in the control of contagious diseases and other public health threats.
At the turn of the 20th century, TB was the leading cause of death in the US and much of the world. Public health efforts and improved living conditions resulted in a steady decline in TB morbidity and mortality until the mid-1980s.
At that time a combination of events—the HIV epidemic, increased immigration from countries with high TB rates, and a decline in funding for TB control programs—resulted in a reversal of this downward trend and for several years there were increases in US TB rates. Of equal concern was an increase in multidrug resistance. These worrisome trends were reversed in the early 1990s and since that time TB rates have again been declining. In 2001 there were 15,989 new cases of TB in the US for a rate of 5.6/100,000. An increasing proportion of cases have been occurring among those born in countries with high TB rates; in 2001 49% of all those with TB in the US were foreign-born.
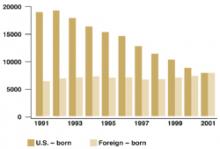
Increasing proportion of foreign-born TB cases
Number of tuberculosis cases in US-born vs foreign-born persons, United States, 1991–2001. Adapted from the Centers for Disease Control and Prevention, Atlanta, Ga.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].
- For the initial evaluation of any adult who requires routine evaluation for TB exposure, administer a second TB skin test within 1 to 3 weeks if the first test result is negative.
- The workup for active TB consists of a chest x-ray film, a human immunodeficiency virus (HIV) test, and possibly sputum collection. HIV-negative persons with a normal chest x-ray result are unlikely to have pulmonary TB, and sputum collection is unnecessary.
- Contrary to common belief, there is no age cutoff for treating latent TB.
- Treat active TB with isoniazid, rifampin, and pyrazinamide. Add ethambutol if a patient is a current or former resident of an area in which bacterial resistance to isoniazid is greater than 5%.
- Refer all suspected cases of TB to your local public health department for the purpose of tracking contacts.
With the decline of tuberculosis (TB), physician familiarity with this disease has substantially diminished. Yet TB remains common in immigrants, individuals with HIV infection, and other high-risk populations. How do we remain vigilant for TB? How do we screen? How should the physician interpret TB test results? What are the preferred options for treatment? What are the public health implications of TB? This article offers an update on this recalcitrant public health problem.
Whom, and how, to screen
Two factors are key in remaining vigilant for tuberculosis: knowing who in your patient population is most at risk for exposure, and knowing who is most likely to develop active disease if infected.
Persons at risk for exposure to TB (Table 1) or at risk for developing active disease if infected (Table 2) should receive a TB skin test regularly, although the optimal frequency has not been determined. Routine testing is not indicated for others.
Proper technique. The TB skin test should be administered with intermediate-strength purified protein derivative (PPD), 0.1 mL injected intradermally, resulting in a raised bleb. The test should be read 48 to 72 hours later and the area of induration, not erythema, measured and recorded in millimeters. With no induration, the result should be recorded as 0 mm, not as “negative.”
Interpreting test results. Interpretation of the test results depends on a person’s risk factors and age. For those listed in Table 3, a 5-mm induration is considered positive; for those listed in Tables 1 and 2 who are not in Table 3 , a 10-mm induration is positive. For everyone else, 15 mm is positive.
Caveat. Multiple puncture tests, though easier to administer, do not inject a standardized amount of tuberculin into the skin; results are more difficult to interpret and, if judged reactive, must be confirmed with a PPD test. This option is not recommended for testing.
Prior receipt of the bacillus Calmette-Guerin (BCG) vaccine does not affect the interpretation of the TB skin test, nor should it affect decisions to treat latent TB. The effectiveness of BCG vaccine in preventing TB infection in highly questionable, and the reaction to PPD caused by BCG wanes after a few years.
Two-step testing. Two-step testing means administering a second TB skin test within 1 to 3 weeks if the first test result is negative. This procedure should be used for the initial evaluation of adults who require routine testing. If the second skin test result is positive, it indicates the person was infected with TB before, and that immunity has waned and was “boosted” by the first test.
Without the 2-step process, a positive result on repeat testing would suggest recent infection rather than prior exposure. This could have implications for the decision to accept or not accept treatment for latent TB.
TABLE 1
Conditions associated with high risk of exposure to tuberculosis
| Foreign-born in area with high tuberculosis rates |
| Use of illicit drugs |
Institutionalization or work in
|
| Work in health care facilities with high-risk clients |
| Socioeconomic disadvantage |
| Children of those at high risk |
TABLE 2
Conditions associated with high risk of developing active tuberculosis
| HIV infection |
| Recent infection with Mycobacterium tuberculosis |
| Chest x-ray indicating old tuberculosis |
Immunosuppression
|
| Leukemia and other cancers of blood, lymph, and bone marrow |
| Cancer of the head and neck |
| Gastrectomy or intestinal bypass |
| Chronic malabsorption |
| End-stage renal disease |
| Diabetes |
| Silicosis |
| Illicit drug use |
TABLE 3
How to interpret a tuberculosis skin test
| 5 mm considered positive in those with: |
|
| 10 mm is considered positive in: |
Work-up for suspected tuberculosis
For those suspected of having TB because of chronic cough, night sweats, fever, and weight loss, or because of a positive TB skin test result, the workup consists of a chest x-ray film, an HIV test, and possibly sputum collection for microscopic evaluation and culture.
Those with a normal chest x-ray result who are HIV-negative are unlikely to have pulmonary TB, and sputum collection is unnecessary. For those with suspicious chest x-ray films and for those who are HIV positive with TB symptoms, sputum samples are needed for microscopic evaluation and culture (3 samples, preferably on 3 consecutive days).
Acid-fast organisms seen under the microscope may be Mycobacterium tuberculosis or mycobacteria other than tuberculosis (commonly referred to as MOTT), and the final determination must await culture confirmation, which now takes about 4 weeks. Preliminary confirmation using polymerase chain reaction can be accomplished in a few days. Treatment for active TB should be initiated, however, and the suspicion reported to the local health department as soon as TB is suspected.
Treating latent and active disease
Latent tuberculosis. Treatment for latent TB (positive TB skin test result, negative chest x-ray film, HIV-negative) should not be initiated until active TB is ruled out. This may require waiting 3 to 4 weeks for sputum culture results.
Contrary to common belief, there is no age cutoff for initiation of treatment for latent TB. Treatment requires 6 to 9 months of isoniazid or 4 months of rifampin. A shorter course with pyrazinamide and rifampin is also possible, although questions about the safety of this regimen have been raised. Patient compliance for the duration of therapy is difficult to achieve; but if accomplished, the risk of active disease decreases from 10% to less than 1%. At highest risk of developing active disease are children, and those who are HIV-positive, recently infected with TB, or whose chest films indicate old disease.
Since isoniazid is hepatotoxic, patients should be asked about symptoms of liver inflammation (abdominal pain, decline in appetite, dark urine, light-colored stools), and liver function tests should be ordered if symptoms are present. Routine monthly testing of liver function tests is not necessary and is recommended only for those who have chronic liver disease, an alcohol abuse disorder, or are pregnant.
Active tuberculosis. Always initiate treatment with at least 3 drugs (isoniazid, rifampin, and pyrazinamide). Ethambutol should be added to the regimen if patients are current or former residents of an area where resistance to isoniazid is more than 5%. If the organism proves sensitive to isoniazid and rifampin, ethambutol can be discontinued. Pyrazinamide should be continued for a full 2 months, and isoniazid and rifampin for a full 6 months. A variety of protocols for dosing and administration frequency are available to enhance convenience and patient compliance. Drug regimens may have to be adjusted based on culture results and success of therapy.
The standard of care for active TB is directly observed therapy. This means watching the patient swallow the pills. Although such care is labor intensive and implies a lack of trust in the patient, with its implementation, the successful completion of therapy rises from 50% to close to 100%. Widespread use of directly observed therapy since the late 1980s has resulted in a marked reduction of TB rates and rates of bacterial resistance.
To prevent bacterial resistance to drugs, treatment for active disease must be administered according to guidelines and be completed. One cardinal rule in the prevention of bacterial resistance is never to add just 1 drug to a failing regimen.
Any deviation from standard therapy because of bacterial resistance, patient nonadherence, or adverse drug effects is reason to consult the local public health department or state public health department TB program.
Working with the public health department
Three complementary activities are needed to control TB in the community:
- Finding and treating those with active TB
- Investigating close contacts of persons with active disease and offering them treatment of latent TB
- Screening persons at high risk, to find and treat latent TB.
The detection and management of tuberculosis offers an excellent opportunity for family physicians and health departments to work collaboratively to improve the community’s health.
Family physicians can make several contributions to reducing TB’s impact on the community:
- Screen appropriately
- Correctly apply and interpret TB skin tests
- Accurately make the diagnosis of latent and active TB
- Treat active TB according to recommended guidelines
- Encourage treatment of latent TB among those at highest risk of activation
- Promptly report to the local health department those suspected of having TB
- Collaborate with the public health department to reduce the spread of disease.
Local or state public health departments assist in several ways:
- Communicate with and investigating family and other close contacts of those with active, contagious TB, to find anyone with latent or active TB
- Offer consultation on how to diagnose and treat latent and active TB
- Assist with directly observed therapy
- Use public health authority to isolate and quarantine patients who are infectious and pose a risk to the community through non-adherence to treatment and infection control guidelines.
Many public health departments have TB programs wherein patients with active or latent TB can receive free care and medication.
State and local public health departments have the responsibility of monitoring TB care provided by physicians in the community, to insure it is applied according to guidelines and that it is completed. The intrusiveness of this can be minimized with regular communication and appreciation of the roles and responsibilities of each party.
Excellent review of the basics of TB screening, diagnosis, and treatment: Centers for Disease Control and Prevention (CDC). Core Curriculum on Tuberculosis. 4th ed. Atlanta, Ga: CDC; 2000.
Self-study modules on TB: CDC. National Center for HIV, STD, and TB Prevention, Divisionof Tuberculosis Elimination. Available at: www.phppo.cdc.gov/PHTN/tbmodules.(Accessed on September 8, 2003.)
Training modules and statistics on TB diagnosis, treatment, and epidemiology, including state-specific analyses: CDC. National Center for HIV, STD, and TB Prevention. Division of Tuberculosis Elimination. Available at: www.cdc.gov/nchstp/tb/default.htm. (Accessedon September 8, 2003.)
The most recent, comprehensive description of TB treatment recommendations: Blumberg HM, Burman WJ, Chaisson RE, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med 2003; 167:603–662.
Prospects and trends
More reliable testing. The TB skin test is an imperfect screening tool. The development of a blood test for TB antibodies has progressed and will be evaluated and standardized. It will likely be a useful clinical and epidemiological tool in the near future.
Tuberculosis secondary to HIV. By some indicators, the rate of HIV infections has recently increased. This factor, combined with the increased life span of those with HIV, has the potential for reversing some of the recent progress in slowing TB rates. The continued development of anti-HIV medications and availability of the medications through AIDS/HIV treatment programs could help make those who are HIV infected less susceptible to TB infection and disease activation.
Tuberculosis and immigration. It is likely that as endemic TB declines in the US, a higher proportion of TB infections will occur in those who are foreign born and move to this country (see “Trends reversing in tuberculosis”). This underscores the global nature of public health and the importance of international collaboration in the control of contagious diseases and other public health threats.
At the turn of the 20th century, TB was the leading cause of death in the US and much of the world. Public health efforts and improved living conditions resulted in a steady decline in TB morbidity and mortality until the mid-1980s.
At that time a combination of events—the HIV epidemic, increased immigration from countries with high TB rates, and a decline in funding for TB control programs—resulted in a reversal of this downward trend and for several years there were increases in US TB rates. Of equal concern was an increase in multidrug resistance. These worrisome trends were reversed in the early 1990s and since that time TB rates have again been declining. In 2001 there were 15,989 new cases of TB in the US for a rate of 5.6/100,000. An increasing proportion of cases have been occurring among those born in countries with high TB rates; in 2001 49% of all those with TB in the US were foreign-born.
Increasing proportion of foreign-born TB cases
Number of tuberculosis cases in US-born vs foreign-born persons, United States, 1991–2001. Adapted from the Centers for Disease Control and Prevention, Atlanta, Ga.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].
- For the initial evaluation of any adult who requires routine evaluation for TB exposure, administer a second TB skin test within 1 to 3 weeks if the first test result is negative.
- The workup for active TB consists of a chest x-ray film, a human immunodeficiency virus (HIV) test, and possibly sputum collection. HIV-negative persons with a normal chest x-ray result are unlikely to have pulmonary TB, and sputum collection is unnecessary.
- Contrary to common belief, there is no age cutoff for treating latent TB.
- Treat active TB with isoniazid, rifampin, and pyrazinamide. Add ethambutol if a patient is a current or former resident of an area in which bacterial resistance to isoniazid is greater than 5%.
- Refer all suspected cases of TB to your local public health department for the purpose of tracking contacts.
With the decline of tuberculosis (TB), physician familiarity with this disease has substantially diminished. Yet TB remains common in immigrants, individuals with HIV infection, and other high-risk populations. How do we remain vigilant for TB? How do we screen? How should the physician interpret TB test results? What are the preferred options for treatment? What are the public health implications of TB? This article offers an update on this recalcitrant public health problem.
Whom, and how, to screen
Two factors are key in remaining vigilant for tuberculosis: knowing who in your patient population is most at risk for exposure, and knowing who is most likely to develop active disease if infected.
Persons at risk for exposure to TB (Table 1) or at risk for developing active disease if infected (Table 2) should receive a TB skin test regularly, although the optimal frequency has not been determined. Routine testing is not indicated for others.
Proper technique. The TB skin test should be administered with intermediate-strength purified protein derivative (PPD), 0.1 mL injected intradermally, resulting in a raised bleb. The test should be read 48 to 72 hours later and the area of induration, not erythema, measured and recorded in millimeters. With no induration, the result should be recorded as 0 mm, not as “negative.”
Interpreting test results. Interpretation of the test results depends on a person’s risk factors and age. For those listed in Table 3, a 5-mm induration is considered positive; for those listed in Tables 1 and 2 who are not in Table 3 , a 10-mm induration is positive. For everyone else, 15 mm is positive.
Caveat. Multiple puncture tests, though easier to administer, do not inject a standardized amount of tuberculin into the skin; results are more difficult to interpret and, if judged reactive, must be confirmed with a PPD test. This option is not recommended for testing.
Prior receipt of the bacillus Calmette-Guerin (BCG) vaccine does not affect the interpretation of the TB skin test, nor should it affect decisions to treat latent TB. The effectiveness of BCG vaccine in preventing TB infection in highly questionable, and the reaction to PPD caused by BCG wanes after a few years.
Two-step testing. Two-step testing means administering a second TB skin test within 1 to 3 weeks if the first test result is negative. This procedure should be used for the initial evaluation of adults who require routine testing. If the second skin test result is positive, it indicates the person was infected with TB before, and that immunity has waned and was “boosted” by the first test.
Without the 2-step process, a positive result on repeat testing would suggest recent infection rather than prior exposure. This could have implications for the decision to accept or not accept treatment for latent TB.
TABLE 1
Conditions associated with high risk of exposure to tuberculosis
| Foreign-born in area with high tuberculosis rates |
| Use of illicit drugs |
Institutionalization or work in
|
| Work in health care facilities with high-risk clients |
| Socioeconomic disadvantage |
| Children of those at high risk |
TABLE 2
Conditions associated with high risk of developing active tuberculosis
| HIV infection |
| Recent infection with Mycobacterium tuberculosis |
| Chest x-ray indicating old tuberculosis |
Immunosuppression
|
| Leukemia and other cancers of blood, lymph, and bone marrow |
| Cancer of the head and neck |
| Gastrectomy or intestinal bypass |
| Chronic malabsorption |
| End-stage renal disease |
| Diabetes |
| Silicosis |
| Illicit drug use |
TABLE 3
How to interpret a tuberculosis skin test
| 5 mm considered positive in those with: |
|
| 10 mm is considered positive in: |
Work-up for suspected tuberculosis
For those suspected of having TB because of chronic cough, night sweats, fever, and weight loss, or because of a positive TB skin test result, the workup consists of a chest x-ray film, an HIV test, and possibly sputum collection for microscopic evaluation and culture.
Those with a normal chest x-ray result who are HIV-negative are unlikely to have pulmonary TB, and sputum collection is unnecessary. For those with suspicious chest x-ray films and for those who are HIV positive with TB symptoms, sputum samples are needed for microscopic evaluation and culture (3 samples, preferably on 3 consecutive days).
Acid-fast organisms seen under the microscope may be Mycobacterium tuberculosis or mycobacteria other than tuberculosis (commonly referred to as MOTT), and the final determination must await culture confirmation, which now takes about 4 weeks. Preliminary confirmation using polymerase chain reaction can be accomplished in a few days. Treatment for active TB should be initiated, however, and the suspicion reported to the local health department as soon as TB is suspected.
Treating latent and active disease
Latent tuberculosis. Treatment for latent TB (positive TB skin test result, negative chest x-ray film, HIV-negative) should not be initiated until active TB is ruled out. This may require waiting 3 to 4 weeks for sputum culture results.
Contrary to common belief, there is no age cutoff for initiation of treatment for latent TB. Treatment requires 6 to 9 months of isoniazid or 4 months of rifampin. A shorter course with pyrazinamide and rifampin is also possible, although questions about the safety of this regimen have been raised. Patient compliance for the duration of therapy is difficult to achieve; but if accomplished, the risk of active disease decreases from 10% to less than 1%. At highest risk of developing active disease are children, and those who are HIV-positive, recently infected with TB, or whose chest films indicate old disease.
Since isoniazid is hepatotoxic, patients should be asked about symptoms of liver inflammation (abdominal pain, decline in appetite, dark urine, light-colored stools), and liver function tests should be ordered if symptoms are present. Routine monthly testing of liver function tests is not necessary and is recommended only for those who have chronic liver disease, an alcohol abuse disorder, or are pregnant.
Active tuberculosis. Always initiate treatment with at least 3 drugs (isoniazid, rifampin, and pyrazinamide). Ethambutol should be added to the regimen if patients are current or former residents of an area where resistance to isoniazid is more than 5%. If the organism proves sensitive to isoniazid and rifampin, ethambutol can be discontinued. Pyrazinamide should be continued for a full 2 months, and isoniazid and rifampin for a full 6 months. A variety of protocols for dosing and administration frequency are available to enhance convenience and patient compliance. Drug regimens may have to be adjusted based on culture results and success of therapy.
The standard of care for active TB is directly observed therapy. This means watching the patient swallow the pills. Although such care is labor intensive and implies a lack of trust in the patient, with its implementation, the successful completion of therapy rises from 50% to close to 100%. Widespread use of directly observed therapy since the late 1980s has resulted in a marked reduction of TB rates and rates of bacterial resistance.
To prevent bacterial resistance to drugs, treatment for active disease must be administered according to guidelines and be completed. One cardinal rule in the prevention of bacterial resistance is never to add just 1 drug to a failing regimen.
Any deviation from standard therapy because of bacterial resistance, patient nonadherence, or adverse drug effects is reason to consult the local public health department or state public health department TB program.
Working with the public health department
Three complementary activities are needed to control TB in the community:
- Finding and treating those with active TB
- Investigating close contacts of persons with active disease and offering them treatment of latent TB
- Screening persons at high risk, to find and treat latent TB.
The detection and management of tuberculosis offers an excellent opportunity for family physicians and health departments to work collaboratively to improve the community’s health.
Family physicians can make several contributions to reducing TB’s impact on the community:
- Screen appropriately
- Correctly apply and interpret TB skin tests
- Accurately make the diagnosis of latent and active TB
- Treat active TB according to recommended guidelines
- Encourage treatment of latent TB among those at highest risk of activation
- Promptly report to the local health department those suspected of having TB
- Collaborate with the public health department to reduce the spread of disease.
Local or state public health departments assist in several ways:
- Communicate with and investigating family and other close contacts of those with active, contagious TB, to find anyone with latent or active TB
- Offer consultation on how to diagnose and treat latent and active TB
- Assist with directly observed therapy
- Use public health authority to isolate and quarantine patients who are infectious and pose a risk to the community through non-adherence to treatment and infection control guidelines.
Many public health departments have TB programs wherein patients with active or latent TB can receive free care and medication.
State and local public health departments have the responsibility of monitoring TB care provided by physicians in the community, to insure it is applied according to guidelines and that it is completed. The intrusiveness of this can be minimized with regular communication and appreciation of the roles and responsibilities of each party.
Excellent review of the basics of TB screening, diagnosis, and treatment: Centers for Disease Control and Prevention (CDC). Core Curriculum on Tuberculosis. 4th ed. Atlanta, Ga: CDC; 2000.
Self-study modules on TB: CDC. National Center for HIV, STD, and TB Prevention, Divisionof Tuberculosis Elimination. Available at: www.phppo.cdc.gov/PHTN/tbmodules.(Accessed on September 8, 2003.)
Training modules and statistics on TB diagnosis, treatment, and epidemiology, including state-specific analyses: CDC. National Center for HIV, STD, and TB Prevention. Division of Tuberculosis Elimination. Available at: www.cdc.gov/nchstp/tb/default.htm. (Accessedon September 8, 2003.)
The most recent, comprehensive description of TB treatment recommendations: Blumberg HM, Burman WJ, Chaisson RE, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med 2003; 167:603–662.
Prospects and trends
More reliable testing. The TB skin test is an imperfect screening tool. The development of a blood test for TB antibodies has progressed and will be evaluated and standardized. It will likely be a useful clinical and epidemiological tool in the near future.
Tuberculosis secondary to HIV. By some indicators, the rate of HIV infections has recently increased. This factor, combined with the increased life span of those with HIV, has the potential for reversing some of the recent progress in slowing TB rates. The continued development of anti-HIV medications and availability of the medications through AIDS/HIV treatment programs could help make those who are HIV infected less susceptible to TB infection and disease activation.
Tuberculosis and immigration. It is likely that as endemic TB declines in the US, a higher proportion of TB infections will occur in those who are foreign born and move to this country (see “Trends reversing in tuberculosis”). This underscores the global nature of public health and the importance of international collaboration in the control of contagious diseases and other public health threats.
At the turn of the 20th century, TB was the leading cause of death in the US and much of the world. Public health efforts and improved living conditions resulted in a steady decline in TB morbidity and mortality until the mid-1980s.
At that time a combination of events—the HIV epidemic, increased immigration from countries with high TB rates, and a decline in funding for TB control programs—resulted in a reversal of this downward trend and for several years there were increases in US TB rates. Of equal concern was an increase in multidrug resistance. These worrisome trends were reversed in the early 1990s and since that time TB rates have again been declining. In 2001 there were 15,989 new cases of TB in the US for a rate of 5.6/100,000. An increasing proportion of cases have been occurring among those born in countries with high TB rates; in 2001 49% of all those with TB in the US were foreign-born.
Increasing proportion of foreign-born TB cases
Number of tuberculosis cases in US-born vs foreign-born persons, United States, 1991–2001. Adapted from the Centers for Disease Control and Prevention, Atlanta, Ga.
Correspondence
1825 E. Roosevelt, Phoenix, AZ 85006. E-mail: [email protected].