User login
Intestinal failure, the inability of the gut to maintain nutritional homeostasis,1 is a complication of vascular thrombosis, inflammatory bowel disease, radiation enteritis, obstruction, and other conditions, and of removing segments of the small and large intestines in response to these diseases.1,2 Imbalances of fluids and electrolytes, dehydration, malabsorption, vitamin and mineral deficiencies, chronic diarrhea, and increased ostomy output contribute to a decline in the quality of life and in the survival rate in these patients.2,3
Referral to an intestinal rehabilitation program that combines gastroenterology, nutrition, pharmacy, nursing, and social work can improve nutritional status and quality of life.4 Whenever possible, the goal of rehabilitation is nutritional autonomy, helping the patient make the transition to an independent oral diet.4 In selected patients in whom rehabilitation is not effective, intestinal transplant may be an option.
In this article, we review the intestinal adaptations that follow surgical resection and provide an update on intestinal rehabilitation techniques such as dietary modification, drug therapy, and parenteral nutrition. We also review experience with intestinal transplant in patients with intestinal failure.
INTESTINAL FAILURE
Intestinal failure results from reduction in enterocyte cell mass, obstruction, dysmotility, surgical resection, congenital defects, or disease-associated loss of absorption with suboptimal nutritional autonomy.5 Patients often suffer from extensive nutrient, electrolyte, and fluid abnormalities proportional to the remnant length and part of the intestine removed.5
Epidemiologic studies have demonstrated that short-bowel syndrome is the most common cause of intestinal failure in adults and children.6,7 Short-bowel syndrome is defined as a small-bowel length less than 200 cm, most commonly from extensive resections for inflammatory bowel disease.6 In children, the syndrome is also defined by a residual small-bowel length of less than 25% expected for gestational age.7
Table 1 lists the frequencies of the underlying disorders leading to intestinal failure or short-bowel syndrome in one series.8
INTESTINAL ADAPTATION
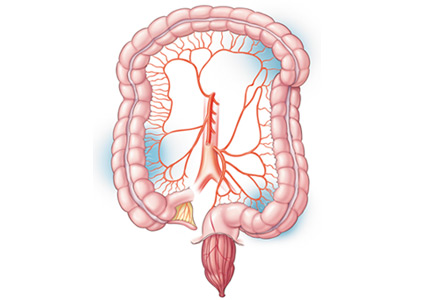
The gastrointestinal tract is the only organ for nutrient, fluid, and electrolyte absorption.9 Every day, 8 to 9 L of fluids and secretions reach the small intestine, comprising about 2 to 3 L of oral fluids, 1 L of saliva, 2 L of gastric juices, 1 L of bile, and 2 L of pancreatic juices.9 Approximately 7 to 8 L are reabsorbed by the small intestine and 1 to 2 L by the colon.9
Although carbohydrates, lipids, and proteins are absorbed through the entire small intestine and colon, site-specific digestion and absorption of different nutrients occur in different parts of the gastrointestinal tract.10 Also, certain nutrients may need site-specific receptors or transporters for their absorption,10 for example:
- Iron in the duodenum and proximal jejunum1
- Lactose in the brush border membrane of the jejunum and proximal ileum, where most of the enzyme lactase is present
- Vitamin B12 and bile salts in the distal ileum.
Hence, resection of a specific part of the intestine may predict deficiencies the patient may encounter after surgery.
The diarrhea that occurs in short-bowel syndrome may be due partly to loss of neurohumoral mediators that govern gastrointestinal transit time, most importantly cholecystokinin, peptide YY, and glucagon-like peptide 1.11 After contact with lipid- or protein-rich nutrients, cholecystokinin is released from the proximal small intestine, which decreases the gastric emptying to maximize nutrient digestion.12 Additionally, release of peptide YY and glucagon-like peptide 1 from the ileal L cells decreases gastric and intestinal motility. These mediators prolong gastrointestinal transit, increase nutrient processing time, and enhance absorption.12
After massive intestinal resection, the remnant bowel undergoes physiologic and functional adaptation to maintain nutritional homeostasis.13 Enterocytes express membrane-bound transporters and undergo accelerated cell division to enhance the absorptive surface area.13 Intestinal hypertrophy, which includes an increase in villous diameter and crypt height, continues for 2 years or more after intestinal resection, leading to greater absorptive surface area.14 It is estimated that villous height may increase by as much as 80%, illustrating a dynamic process in response to intestinal stress.15
Luminal nutrients are essential to the stimulation of enterocyte cells through paracrine mechanisms as well as through the up-regulation of colonic peptide transporter PepT1.15 Furthermore, gut motility is initially decreased in order to increase the concentration of local luminal growth factors.16
Other factors that may affect intestinal adaptation are the length of the residual colon and small intestine, enteral growth, and enterotropic factors.16 And especially in patients with short-bowel syndrome, complications such as malabsorption secondary to pancreatic insufficiency or rapid transit, excessive gastric acid secretion, bile acid wasting due to terminal ileum resection, and bacterial overgrowth in the small intestine result in worsened nutritional status and poor quality of life.16
Key factors that affect the degree of nutritional deficiencies
The degree of nutritional deficiencies and fluid and electrolyte imbalances depends on the length and location of resection and whether the colon is still continuous with the small intestine.17 Normal small-bowel length in adults is highly variable and can be up to 600 cm. Malnutrition after surgical resection usually occurs when more than three-fourths of intestinal tissue is removed.17 However, because of intestinal adaptation, patients with 50% of remnant small bowel may be able to achieve nutritional autonomy.18 Furthermore, because absorption of nutrients occurs primarily in the first 150 cm of the small intestine, resections of this anatomic region have the highest probability of resulting in malnutrition.18
After extensive intestinal resection, absorption of water and electrolytes is better and intestinal transit time is longer if the colon is still continuous with the rest of the gastrointestinal system.19 Approximately 100 cm of remnant intestinal tissue without colonic continuity or 60 cm with colonic continuity is needed to ensure the possibility of nutritional autonomy and independence from parenteral nutrition.19 Severe malnutrition and fluid and electrolyte imbalances can be prevented by appropriate and timely multidisciplinary care and early referral for intestinal rehabilitation.
INTESTINAL REHABILITATION AND NUTRITIONAL AUTONOMY
The aim of intestinal rehabilitation is to improve quality of life by reversing malnutrition and promoting nutritional autonomy, ie, independence from parenteral nutrition (Table 2).20 The complex nature of intestinal failure necessitates collaboration of multiple specialists—gastroenterologists, surgeons, dietitians, nurses, psychiatrists or psychologists, pharmacists, and social workers.20
Although most patients with intestinal failure initially require parenteral nutrition to maintain nutritional homeostasis, progressive adaptation of the remnant intestine enables a transition to enteral nutrition.21 Stimulation of the remnant intestine by enteral feeding reduces the complications of parenteral nutrition and encourages intestinal adaptation.21
Outpatient participation in an intestinal rehabilitation program can facilitate weaning from parenteral nutrition. Patients are monitored and supported during dietary modification, pharmacologic interventions, and reconstructive surgeries.21 A study of 61 patients with short-bowel syndrome undergoing a 3-week program of intestinal rehabilitation (recombinant human growth hormone, glutamine, enteral nutrition, and parenteral nutrition) reported an overall survival rate of 95% with an 85% success rate in weaning from parenteral nutrition during a mean follow-up of 50 (± 24) months.22 Permanent dependence on parenteral nutrition despite rehabilitation was predicted by length of the small bowel less than 100 cm and by the absence of terminal ileum and colon.22
Permanent intestinal failure, defined by the inability to wean from parenteral nutrition and restore nutrition autonomy, may require early referral for evaluation for intestinal and multivisceral transplant. Early referral improves survival rates, possibly because of fewer complications from parenteral nutrition.4
DIETARY MODIFICATION
Dietary modification is the single most effective means of weaning patients safely from parenteral nutrition (Table 3).23,24 Small, frequent feedings help reduce symptoms associated with rapid intestinal transit and increase the activity of luminal growth factors.23 Likewise, limits on intake of simple sugars, stimulants such as caffeine or insoluble fiber, and hypo- or hypertonic fluids decrease intestinal losses and the risk of dehydration.23 Low sugar loads also aim to reduce the occurrence of d-lactic acidosis and bacterial overgrowth in the small intestine.23 Patients who cannot maintain positive fluid balance may require standardized oral rehydration (Table 4) to improve absorption by way of the sodium-glucose coupled transporters at the brush border membrane, or they may require intravenous fluid supplementation.25
Colonic continuity
Other dietary recommendations depend on colonic continuity. In 1994, Nordgaard et al26 compared the effects of high-carbohydrate and high-fat diets in eight patients with colonic continuity and six patients with jejunostomies. The authors noted that a high-carbohydrate diet (60% carbohydrate, 20% fat) reduced fecal loss of energy and increased energy absorption in patients with colonic continuity. However, patients with an end-jejunostomy experienced equal fecal losses of carbohydrates and fat proportional to the amount consumed. The authors concluded that the presence of colonic bacteria promoted carbohydrate salvage, ie, the fermentation of malabsorbed carbohydrates to easily absorbed short-chain fatty acids.26
The colon can salvage as much as 1,000 kcal/day in patients with less than 200 cm of small bowel, and the presence of at least 50% of colon in continuity has been shown to reduce parenteral nutrition requirements by half in patients with less than 100 cm of small bowel.27 As a result, a diet high in complex carbohydrates and soluble fiber supplements is recommended in cases of preserved colon to promote adaptation and nutritional autonomy.27
Another aim of a high-carbohydrate, low- fat diet is to prevent calcium oxalate-related nephrolithiasis and choleretic diarrhea.26
In summary, patients with short-bowel syndrome with or without colonic continuity need different dietary regimens to attain nutritional autonomy.
DRUG THERAPY
In addition to diet therapy, most patients with intestinal failure require pharmacologic therapy.28 High stool or stoma effluent is most commonly treated with an antidiarrheal to increase transit time; diphenoxylate-atropine, loperamide, codeine sulfate, paregoric, and opium tincture are commonly prescribed (Table 5).27 In severe high-output states, a somatostatin analogue (eg, octreotide) may be added.29
Postoperative increases in gastric secretion may be countered by histamine 2 receptor antagonists and proton pump inhibitors, but long-term use of these drugs may lead to nutritional deficiencies and bacterial overgrowth in the small intestine.29 Bile acid sequestrants (in cases of distal ileal resection) and pancreatic enzymes target fat malabsorption, resultant cases of choleretic diarrhea, deficiency of essential fatty acids, kidney stones, and deficiency of fat-soluble vitamins.29 Probiotics and antibiotics can also be given for prevention and treatment of small-intestinal bacterial overgrowth.29
When traditional dietary modification and medical therapy fail to achieve nutritional homeostasis, another option to consider is a glucagon-like peptide-2 analogue to enhance intestinal adaptation.30 Produced in the native distal ileum and colon, glucagon-like peptide 2 moderates the rate of gastric emptying and small-bowel transit and enhances epithelial cell proliferation, thereby promoting intestinal adaptation.30 Further, a randomized controlled trial of 83 patients reported efficacy of these agents in reducing parenteral nutrition requirements in patients with intestinal failure.31
Hence, in patients with intestinal failure who have increased stoma effluent, drug therapy may play an important role in maintaining fluid and nutritional homeostasis.
THE ROLE OF PARENTERAL NUTRITION IN INTESTINAL FAILURE
Despite the best efforts of an intestinal rehabilitation program, not all patients gain nutritional autonomy.32 Physiologic, psychological, social, and economic factors may contribute to dependence on parenteral nutrition.32 Currently, more than 40,000 US patients depend on it for survival.33
The need for short-term or long-term parenteral nutrition is determined by the patient’s medical needs.33 Patients requiring short-term parenteral nutrition (2–6 weeks) include those whose bowel function has not returned to normal postoperatively, and those who were severely malnourished preoperatively.34 Patients needing it long-term (from months to years to lifelong) are those with gastrointestinal dysmotility and short-bowel syndrome due to extensive bowel resections.33
Complications of parenteral nutrition
Catheter-related bloodstream infection is the most common complication and cause of hospitalization. Infection can be localized to the exit site or tunnel or can be systemic (eg, line sepsis).35Staphylococcus aureus and coagulase-negative staphylococci are most often implicated in catheter infection.35 When possible, catheter salvage is desirable, but the central venous catheter must be removed in cases of tunnel infection, port abscess, septic shock, paired blood cultures positive for fungi or highly virulent bacteria, endocarditis, septic thrombosis, and other conditions.35,36
Liver disease is a serious complication of long-term parenteral nutrition and may occur in up to 55% of patients on therapy for more than 2 years; it carries a mortality rate of 15%.37
Risk factors include younger age and use of excessive carbohydrate and fat compositions, mainly soybean-oil–based lipid emulsions.37 However, fish-oil–based lipid emulsions have recently shown promise in preventing and reversing parenteral nutrition-associated liver failure and cholestasis, especially in a pediatric population.38
Catheter thrombosis may occur in up to 30% of patients on long-term parenteral nutrition.39 However, this risk is reduced with appropriate positioning of the catheter tip in the mid or lower superior vena cava.37 Treatment of thrombosis of the central access includes either anticoagulation or thrombolysis.37
Hence, appropriate and timely follow-up of patients on parenteral nutrition is essential in reducing associated complications. Monitoring weight, fluid status, serum glucose, and patency of central access are critical to ensure that the patient maintains nutritional status effectively.40 To prevent complications, a specialized nutritional support team should monitor the patient’s parenteral nutrition both in the hospital and at home.
RECONSTRUCTIVE SURGERY
Patients with intestinal failure due to short- bowel syndrome should be considered for reconstructive surgery during different phases of the adaptation process. Options include reversed-segment procedures, stricturoplasty, bowel-lengthening procedures (eg, the Bianchi procedure), and serial transverse enteroplasty.41,42 If reconstructive surgery is ineffective, referral to an intestinal transplant program should be considered.
INTESTINAL AND MULTIVISCERAL TRANSPLANT
For patients who develop permanent intestinal failure and require lifelong parenteral nutrition, and for patients who experience significant complications of parenteral nutrition, such as infections and liver disease,43 intestinal transplant has emerged as a way to restore clinical nutritional autonomy.44 In one study, the 1-year survival rate after intestinal transplant was approximately 90%.44
There are currently three transplant procedures: isolated intestine transplant, combined liver-intestine transplant, and multivisceral transplant with or without a liver, depending on the presence of parenteral nutrition-associated liver disease.42,45 Close postoperative care is required to help the patient transition from parenteral to enteral nutrition.42 An intestinal rehabilitation team is equipped to provide this level of postoperative care.42
Intestinal and multivisceral transplant gained momentum in the early 1960s in preclinical and clinical studies.46,47 Since that time, the field has experienced remarkable advances due to standardization of surgical techniques, novel immunosuppressive therapies and induction protocols, and improved postoperative care.48 With the advent of tacrolimus in 1989, the rates of allograft rejection improved significantly, and the field of transplant emerged as a potentially lifesaving therapy for patients with permanent intestinal failure.48
Since 1990, more than 2,300 intestinal transplant procedures have been performed for various etiologies of intestinal failure, with short-bowel syndrome being the most common.49
The indications for intestinal transplant approved by the US Centers for Medicare and Medicaid services are detailed in Table 6.50 Despite ongoing challenges of graft rejection and maintenance immunosuppression, posttransplant quality-of-life questionnaires have indicated a significant improvement in functional status and a decrease in depressive symptoms.51 As such, it is evident that intestinal and multivisceral transplant offers substantial promise in restoring a patient’s quality of life and nutritional status.
- Parekh NR, Steiger E. Short bowel syndrome. Curr Treat Options Gastroenterol 2007; 10:10–23.
- Williamson RC. Intestinal adaptation (first of two parts). Structural, functional and cytokinetic changes. N Engl J Med 1978; 298:1393–1402.
- Vantini I, Benini L, Bonfante F, et al. Survival rate and prognostic factors in patients with intestinal failure. Dig Liver Dis 2004; 36:46–55.
- Abu-Elmagd KM, Bond GJ, Matarese L, et al. Gut rehabilitation and intestinal transplantation. Therapy 2005; 2:853–864.
- Nightingale JMD, Lennard-Jones JE. The short bowel syndrome: what’s new and old? Dig Dis 1993; 11:12–31.
- Parekh N, Seidner D, Steiger E. Managing short bowel syndrome: making the most of what the patient still has. Cleve Clin J Med 2005; 72:833–838.
- Wales PW. Surgical therapy for short bowel syndrome. Pediatr Surg Int 2004; 20:647–657.
- Parekh NR, Steiger E, Seidner DL. Determination of residual bowel length via surgical, radiological or historical data in patients with short bowel syndrome and intestinal failure (abstract). Gastroenterology 2006; 130:A605.
- Shatnawei A, Parekh NR, Rhoda KM, et al. Intestinal failure management at the Cleveland Clinic. Arch Surg 2010; 145:521–527.
- Kelly DG, Tappenden KA, Winkler MF. Short bowel syndrome: highlights of patient management, quality of life, and survival. JPEN J Parenter Enteral Nutr 2014; 38:427–437.
- Efsen E, Jeppesen PB. Modern treatment of adult short bowel syndrome patients. Minerva Gastroenterol Dietol 2011; 57:405–417.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Dowling RH, Booth DB. Functional compensation after small bowel resection in man. Lancet 1996; 2:146–147.
- Tappenden KA. Intestinal adaptation following resection. JPEN J Parenter Enteral Nutr 2014; 38(suppl 1):23S–31S.
- Friedman HI, Chandler JG, Peck CC, Nemeth TJ, Odum SK. Alterations in intestinal structure, fat absorption and body weight after intestinal bypass for morbid obesity. Surg Gynecol Obstet 1978; 146:757–767.
- O’Keefe SJ, Buchman AL, Fishbein TM, Jeejeebhoy KN, Jeppesen PB, Shaffer J. Short bowel syndrome and intestinal failure: consensus definitions and overview. Clin Gastroenterol Hepatol 2006; 4:6–10.
- Lennard-Jones JE. Review article: practical management of the short bowel. Aliment Pharmacol Ther 1994; 8:563–577.
- Goulet O, Colomb-Jung V, Joly F. Role of the colon in short bowel syndrome and intestinal transplantation. J Pediatr Gastroenterol Nutr 2009; 48(suppl 2):S66–S71.
- Jeppesen PB, Mortensen PB. Colonic digestion and absorption of energy from carbohydrates and medium-chain fat in small bowel failure. JPEN J Parenter Enteral Nutr 1999; 23(suppl 5):S101–S105.
- Buchman AL. Etiology and initial management of short bowel syndrome. Gastroenterology 2006; 130(suppl 1):S5–S15.
- Donohoe CL, Reynolds JV. Short bowel syndrome. Surgeon 2010; 8:270–279.
- Gong JF, Zhu WM, Yu WK, Li N, Li JS. Role of enteral nutrition in adult short bowel syndrome undergoing intestinal rehabilitation: the long-term outcome. Asia Pac J Clin Nutr 2009; 18:155–163.
- Sundaram A, Koutkia P, Apovian CM. Nutritional management of short bowel syndrome in adults. J Clin Gastroenterol 2002; 34:207–220.
- Byrne TA, Wilmore DW, Iyer K, et al. Growth hormone, glutamine, and an optimal diet reduces parenteral nutrition in patients with short bowel syndrome: a prospective, randomized, placebo-controlled, double-blind clinical trial. Ann Surg 2005; 242:655–661.
- Matarese LE, Steiger E. Dietary and medical management of short bowel syndrome in adult patients. J Clin Gastroenterol 2006; 40(suppl 2):S85–S93.
- Nordgaard I, Hansen BS, Mortensen PB. Colon as a digestive organ in patients with short bowel. Lancet 1994; 343:373–376.
- Ukleja A, Scolapio JS, Buchman AL. Nutritional management of short bowel syndrome. Semin Gastrointest Dis 2002; 13:161–168.
- Jeejeebhoy KN. Short bowel syndrome: a nutritional and medical approach. CMAJ 2002; 166:1297–1302.
- Seetharam P, Rodrigues G. Short bowel syndrome: a review of management options. Saudi J Gastroenterol 2011; 17:229–235.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B, O’Keefe SJ. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011; 60:902–914.
- Pironi L, Joly F, Forbes A, et al; Home Artificial Nutrition & Chronic Intestinal Failure Working Group of the European Society for Clinical Nutrition and Metabolism (ESPEN). Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut 2011; 60:17–25.
- Ekema G, Milianti S, Boroni G. Total parenteral nutrition in patients with short bowel syndrome. Minerva Pediatr 2009; 61:283–291.
- Messing B, Crenn P, Beau P, Boutron-Ruault MC, Rambaud JC, Matuchansky C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999; 117:1043–1050.
- Opilla M. Epidemiology of bloodstream infection associated with parenteral nutrition. Am J Infect Control 2008; 36:S173.e5–e8.
- Ukleja A, Romano MM. Complications of parenteral nutrition. Gastroenterol Clin North Am 2007; 36:23–46.
- Buchman AI, Iyer K, Fryer J. Parenteral nutrition-associated liver disease and the role for isolated intestine and intestine/liver transplantation. Hepatology 2006; 43:9–19.
- Fürst P, Kuhn KS. Fish oil emulsions: what benefits can they bring? Clin Nutr 2000; 19:7–14.
- Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol 2003; 21:3665–3675.
- McMahon MM, Nystrom E, Braunschweig C, Miles J, Compher C; American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors; American Society for Parenteral and Enteral Nutrition. American Society of Parenteral and Enteral Nutrition (ASPEN) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition support of adult patients with hyperglycemia. JPEN J Parenter Enteral Nutr 2013; 37:23–36.
- Kim HB, Fauza D, Garza J, Oh JT, Nurko S, Jaksic T. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg 2003; 38:425–429.
- King B, Carlson G, Khalil BA, Morabito A. Intestinal bowel lengthening in children with short bowel syndrome: systematic review of the Bianchi and STEP procedures. World J Surg 2013; 37:694–704.
- Matarese LE, O’Keefe SJ, Kandil HM, Costa G, Abu-Elmagd KM. Short bowel syndrome: clinical guidelines for nutrition management. Nutr Clin Pract 2005; 20:493–502.
- Abu-Elmagd KM, Costa G, Bond GJ, et al. Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg 2009; 250:567–581.
- Abu-Elmagd K. The concept of gut rehabilitation and the future of visceral transplantation. Nat Rev Gastroenterol Hepatol 2015; 12:108–120.
- Lillehei RC, Goott B, Miller FA. The physiological response of the small bowel of the dog to ischemia including prolonged in vitro preservation of the bowel with successful replacement and survival. Ann Surg 1959; 150:543–559.
- Starzl TE, Kaupp HA. Mass homotransplantation of abdominal organs in dogs. Surg Forum 1960; 11:28–30.
- O’Keefe SJ, Matarese L. Small bowel transplantation. Curr Gastroenterol Rep 2006; 8:360–366.
- Horslen SP. Optimal management of the post-intestinal transplant patient. Gastroenterology 2006; 130(suppl 1):S163–S169.
- Buchman AL, Scolapio J, Fryer J. AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 2003; 124:1111–1134.
- DiMartini A, Rovera GM, Graham TO, et al. Quality of life after small intestinal transplantation and among home parenteral nutrition patients. JPEN J Parenter Enteral Nutr 1998; 22:357–362.
Intestinal failure, the inability of the gut to maintain nutritional homeostasis,1 is a complication of vascular thrombosis, inflammatory bowel disease, radiation enteritis, obstruction, and other conditions, and of removing segments of the small and large intestines in response to these diseases.1,2 Imbalances of fluids and electrolytes, dehydration, malabsorption, vitamin and mineral deficiencies, chronic diarrhea, and increased ostomy output contribute to a decline in the quality of life and in the survival rate in these patients.2,3
Referral to an intestinal rehabilitation program that combines gastroenterology, nutrition, pharmacy, nursing, and social work can improve nutritional status and quality of life.4 Whenever possible, the goal of rehabilitation is nutritional autonomy, helping the patient make the transition to an independent oral diet.4 In selected patients in whom rehabilitation is not effective, intestinal transplant may be an option.
In this article, we review the intestinal adaptations that follow surgical resection and provide an update on intestinal rehabilitation techniques such as dietary modification, drug therapy, and parenteral nutrition. We also review experience with intestinal transplant in patients with intestinal failure.
INTESTINAL FAILURE
Intestinal failure results from reduction in enterocyte cell mass, obstruction, dysmotility, surgical resection, congenital defects, or disease-associated loss of absorption with suboptimal nutritional autonomy.5 Patients often suffer from extensive nutrient, electrolyte, and fluid abnormalities proportional to the remnant length and part of the intestine removed.5
Epidemiologic studies have demonstrated that short-bowel syndrome is the most common cause of intestinal failure in adults and children.6,7 Short-bowel syndrome is defined as a small-bowel length less than 200 cm, most commonly from extensive resections for inflammatory bowel disease.6 In children, the syndrome is also defined by a residual small-bowel length of less than 25% expected for gestational age.7
Table 1 lists the frequencies of the underlying disorders leading to intestinal failure or short-bowel syndrome in one series.8
INTESTINAL ADAPTATION
The gastrointestinal tract is the only organ for nutrient, fluid, and electrolyte absorption.9 Every day, 8 to 9 L of fluids and secretions reach the small intestine, comprising about 2 to 3 L of oral fluids, 1 L of saliva, 2 L of gastric juices, 1 L of bile, and 2 L of pancreatic juices.9 Approximately 7 to 8 L are reabsorbed by the small intestine and 1 to 2 L by the colon.9
Although carbohydrates, lipids, and proteins are absorbed through the entire small intestine and colon, site-specific digestion and absorption of different nutrients occur in different parts of the gastrointestinal tract.10 Also, certain nutrients may need site-specific receptors or transporters for their absorption,10 for example:
- Iron in the duodenum and proximal jejunum1
- Lactose in the brush border membrane of the jejunum and proximal ileum, where most of the enzyme lactase is present
- Vitamin B12 and bile salts in the distal ileum.
Hence, resection of a specific part of the intestine may predict deficiencies the patient may encounter after surgery.
The diarrhea that occurs in short-bowel syndrome may be due partly to loss of neurohumoral mediators that govern gastrointestinal transit time, most importantly cholecystokinin, peptide YY, and glucagon-like peptide 1.11 After contact with lipid- or protein-rich nutrients, cholecystokinin is released from the proximal small intestine, which decreases the gastric emptying to maximize nutrient digestion.12 Additionally, release of peptide YY and glucagon-like peptide 1 from the ileal L cells decreases gastric and intestinal motility. These mediators prolong gastrointestinal transit, increase nutrient processing time, and enhance absorption.12
After massive intestinal resection, the remnant bowel undergoes physiologic and functional adaptation to maintain nutritional homeostasis.13 Enterocytes express membrane-bound transporters and undergo accelerated cell division to enhance the absorptive surface area.13 Intestinal hypertrophy, which includes an increase in villous diameter and crypt height, continues for 2 years or more after intestinal resection, leading to greater absorptive surface area.14 It is estimated that villous height may increase by as much as 80%, illustrating a dynamic process in response to intestinal stress.15
Luminal nutrients are essential to the stimulation of enterocyte cells through paracrine mechanisms as well as through the up-regulation of colonic peptide transporter PepT1.15 Furthermore, gut motility is initially decreased in order to increase the concentration of local luminal growth factors.16
Other factors that may affect intestinal adaptation are the length of the residual colon and small intestine, enteral growth, and enterotropic factors.16 And especially in patients with short-bowel syndrome, complications such as malabsorption secondary to pancreatic insufficiency or rapid transit, excessive gastric acid secretion, bile acid wasting due to terminal ileum resection, and bacterial overgrowth in the small intestine result in worsened nutritional status and poor quality of life.16
Key factors that affect the degree of nutritional deficiencies
The degree of nutritional deficiencies and fluid and electrolyte imbalances depends on the length and location of resection and whether the colon is still continuous with the small intestine.17 Normal small-bowel length in adults is highly variable and can be up to 600 cm. Malnutrition after surgical resection usually occurs when more than three-fourths of intestinal tissue is removed.17 However, because of intestinal adaptation, patients with 50% of remnant small bowel may be able to achieve nutritional autonomy.18 Furthermore, because absorption of nutrients occurs primarily in the first 150 cm of the small intestine, resections of this anatomic region have the highest probability of resulting in malnutrition.18
After extensive intestinal resection, absorption of water and electrolytes is better and intestinal transit time is longer if the colon is still continuous with the rest of the gastrointestinal system.19 Approximately 100 cm of remnant intestinal tissue without colonic continuity or 60 cm with colonic continuity is needed to ensure the possibility of nutritional autonomy and independence from parenteral nutrition.19 Severe malnutrition and fluid and electrolyte imbalances can be prevented by appropriate and timely multidisciplinary care and early referral for intestinal rehabilitation.
INTESTINAL REHABILITATION AND NUTRITIONAL AUTONOMY
The aim of intestinal rehabilitation is to improve quality of life by reversing malnutrition and promoting nutritional autonomy, ie, independence from parenteral nutrition (Table 2).20 The complex nature of intestinal failure necessitates collaboration of multiple specialists—gastroenterologists, surgeons, dietitians, nurses, psychiatrists or psychologists, pharmacists, and social workers.20
Although most patients with intestinal failure initially require parenteral nutrition to maintain nutritional homeostasis, progressive adaptation of the remnant intestine enables a transition to enteral nutrition.21 Stimulation of the remnant intestine by enteral feeding reduces the complications of parenteral nutrition and encourages intestinal adaptation.21
Outpatient participation in an intestinal rehabilitation program can facilitate weaning from parenteral nutrition. Patients are monitored and supported during dietary modification, pharmacologic interventions, and reconstructive surgeries.21 A study of 61 patients with short-bowel syndrome undergoing a 3-week program of intestinal rehabilitation (recombinant human growth hormone, glutamine, enteral nutrition, and parenteral nutrition) reported an overall survival rate of 95% with an 85% success rate in weaning from parenteral nutrition during a mean follow-up of 50 (± 24) months.22 Permanent dependence on parenteral nutrition despite rehabilitation was predicted by length of the small bowel less than 100 cm and by the absence of terminal ileum and colon.22
Permanent intestinal failure, defined by the inability to wean from parenteral nutrition and restore nutrition autonomy, may require early referral for evaluation for intestinal and multivisceral transplant. Early referral improves survival rates, possibly because of fewer complications from parenteral nutrition.4
DIETARY MODIFICATION
Dietary modification is the single most effective means of weaning patients safely from parenteral nutrition (Table 3).23,24 Small, frequent feedings help reduce symptoms associated with rapid intestinal transit and increase the activity of luminal growth factors.23 Likewise, limits on intake of simple sugars, stimulants such as caffeine or insoluble fiber, and hypo- or hypertonic fluids decrease intestinal losses and the risk of dehydration.23 Low sugar loads also aim to reduce the occurrence of d-lactic acidosis and bacterial overgrowth in the small intestine.23 Patients who cannot maintain positive fluid balance may require standardized oral rehydration (Table 4) to improve absorption by way of the sodium-glucose coupled transporters at the brush border membrane, or they may require intravenous fluid supplementation.25
Colonic continuity
Other dietary recommendations depend on colonic continuity. In 1994, Nordgaard et al26 compared the effects of high-carbohydrate and high-fat diets in eight patients with colonic continuity and six patients with jejunostomies. The authors noted that a high-carbohydrate diet (60% carbohydrate, 20% fat) reduced fecal loss of energy and increased energy absorption in patients with colonic continuity. However, patients with an end-jejunostomy experienced equal fecal losses of carbohydrates and fat proportional to the amount consumed. The authors concluded that the presence of colonic bacteria promoted carbohydrate salvage, ie, the fermentation of malabsorbed carbohydrates to easily absorbed short-chain fatty acids.26
The colon can salvage as much as 1,000 kcal/day in patients with less than 200 cm of small bowel, and the presence of at least 50% of colon in continuity has been shown to reduce parenteral nutrition requirements by half in patients with less than 100 cm of small bowel.27 As a result, a diet high in complex carbohydrates and soluble fiber supplements is recommended in cases of preserved colon to promote adaptation and nutritional autonomy.27
Another aim of a high-carbohydrate, low- fat diet is to prevent calcium oxalate-related nephrolithiasis and choleretic diarrhea.26
In summary, patients with short-bowel syndrome with or without colonic continuity need different dietary regimens to attain nutritional autonomy.
DRUG THERAPY
In addition to diet therapy, most patients with intestinal failure require pharmacologic therapy.28 High stool or stoma effluent is most commonly treated with an antidiarrheal to increase transit time; diphenoxylate-atropine, loperamide, codeine sulfate, paregoric, and opium tincture are commonly prescribed (Table 5).27 In severe high-output states, a somatostatin analogue (eg, octreotide) may be added.29
Postoperative increases in gastric secretion may be countered by histamine 2 receptor antagonists and proton pump inhibitors, but long-term use of these drugs may lead to nutritional deficiencies and bacterial overgrowth in the small intestine.29 Bile acid sequestrants (in cases of distal ileal resection) and pancreatic enzymes target fat malabsorption, resultant cases of choleretic diarrhea, deficiency of essential fatty acids, kidney stones, and deficiency of fat-soluble vitamins.29 Probiotics and antibiotics can also be given for prevention and treatment of small-intestinal bacterial overgrowth.29
When traditional dietary modification and medical therapy fail to achieve nutritional homeostasis, another option to consider is a glucagon-like peptide-2 analogue to enhance intestinal adaptation.30 Produced in the native distal ileum and colon, glucagon-like peptide 2 moderates the rate of gastric emptying and small-bowel transit and enhances epithelial cell proliferation, thereby promoting intestinal adaptation.30 Further, a randomized controlled trial of 83 patients reported efficacy of these agents in reducing parenteral nutrition requirements in patients with intestinal failure.31
Hence, in patients with intestinal failure who have increased stoma effluent, drug therapy may play an important role in maintaining fluid and nutritional homeostasis.
THE ROLE OF PARENTERAL NUTRITION IN INTESTINAL FAILURE
Despite the best efforts of an intestinal rehabilitation program, not all patients gain nutritional autonomy.32 Physiologic, psychological, social, and economic factors may contribute to dependence on parenteral nutrition.32 Currently, more than 40,000 US patients depend on it for survival.33
The need for short-term or long-term parenteral nutrition is determined by the patient’s medical needs.33 Patients requiring short-term parenteral nutrition (2–6 weeks) include those whose bowel function has not returned to normal postoperatively, and those who were severely malnourished preoperatively.34 Patients needing it long-term (from months to years to lifelong) are those with gastrointestinal dysmotility and short-bowel syndrome due to extensive bowel resections.33
Complications of parenteral nutrition
Catheter-related bloodstream infection is the most common complication and cause of hospitalization. Infection can be localized to the exit site or tunnel or can be systemic (eg, line sepsis).35Staphylococcus aureus and coagulase-negative staphylococci are most often implicated in catheter infection.35 When possible, catheter salvage is desirable, but the central venous catheter must be removed in cases of tunnel infection, port abscess, septic shock, paired blood cultures positive for fungi or highly virulent bacteria, endocarditis, septic thrombosis, and other conditions.35,36
Liver disease is a serious complication of long-term parenteral nutrition and may occur in up to 55% of patients on therapy for more than 2 years; it carries a mortality rate of 15%.37
Risk factors include younger age and use of excessive carbohydrate and fat compositions, mainly soybean-oil–based lipid emulsions.37 However, fish-oil–based lipid emulsions have recently shown promise in preventing and reversing parenteral nutrition-associated liver failure and cholestasis, especially in a pediatric population.38
Catheter thrombosis may occur in up to 30% of patients on long-term parenteral nutrition.39 However, this risk is reduced with appropriate positioning of the catheter tip in the mid or lower superior vena cava.37 Treatment of thrombosis of the central access includes either anticoagulation or thrombolysis.37
Hence, appropriate and timely follow-up of patients on parenteral nutrition is essential in reducing associated complications. Monitoring weight, fluid status, serum glucose, and patency of central access are critical to ensure that the patient maintains nutritional status effectively.40 To prevent complications, a specialized nutritional support team should monitor the patient’s parenteral nutrition both in the hospital and at home.
RECONSTRUCTIVE SURGERY
Patients with intestinal failure due to short- bowel syndrome should be considered for reconstructive surgery during different phases of the adaptation process. Options include reversed-segment procedures, stricturoplasty, bowel-lengthening procedures (eg, the Bianchi procedure), and serial transverse enteroplasty.41,42 If reconstructive surgery is ineffective, referral to an intestinal transplant program should be considered.
INTESTINAL AND MULTIVISCERAL TRANSPLANT
For patients who develop permanent intestinal failure and require lifelong parenteral nutrition, and for patients who experience significant complications of parenteral nutrition, such as infections and liver disease,43 intestinal transplant has emerged as a way to restore clinical nutritional autonomy.44 In one study, the 1-year survival rate after intestinal transplant was approximately 90%.44
There are currently three transplant procedures: isolated intestine transplant, combined liver-intestine transplant, and multivisceral transplant with or without a liver, depending on the presence of parenteral nutrition-associated liver disease.42,45 Close postoperative care is required to help the patient transition from parenteral to enteral nutrition.42 An intestinal rehabilitation team is equipped to provide this level of postoperative care.42
Intestinal and multivisceral transplant gained momentum in the early 1960s in preclinical and clinical studies.46,47 Since that time, the field has experienced remarkable advances due to standardization of surgical techniques, novel immunosuppressive therapies and induction protocols, and improved postoperative care.48 With the advent of tacrolimus in 1989, the rates of allograft rejection improved significantly, and the field of transplant emerged as a potentially lifesaving therapy for patients with permanent intestinal failure.48
Since 1990, more than 2,300 intestinal transplant procedures have been performed for various etiologies of intestinal failure, with short-bowel syndrome being the most common.49
The indications for intestinal transplant approved by the US Centers for Medicare and Medicaid services are detailed in Table 6.50 Despite ongoing challenges of graft rejection and maintenance immunosuppression, posttransplant quality-of-life questionnaires have indicated a significant improvement in functional status and a decrease in depressive symptoms.51 As such, it is evident that intestinal and multivisceral transplant offers substantial promise in restoring a patient’s quality of life and nutritional status.
Intestinal failure, the inability of the gut to maintain nutritional homeostasis,1 is a complication of vascular thrombosis, inflammatory bowel disease, radiation enteritis, obstruction, and other conditions, and of removing segments of the small and large intestines in response to these diseases.1,2 Imbalances of fluids and electrolytes, dehydration, malabsorption, vitamin and mineral deficiencies, chronic diarrhea, and increased ostomy output contribute to a decline in the quality of life and in the survival rate in these patients.2,3
Referral to an intestinal rehabilitation program that combines gastroenterology, nutrition, pharmacy, nursing, and social work can improve nutritional status and quality of life.4 Whenever possible, the goal of rehabilitation is nutritional autonomy, helping the patient make the transition to an independent oral diet.4 In selected patients in whom rehabilitation is not effective, intestinal transplant may be an option.
In this article, we review the intestinal adaptations that follow surgical resection and provide an update on intestinal rehabilitation techniques such as dietary modification, drug therapy, and parenteral nutrition. We also review experience with intestinal transplant in patients with intestinal failure.
INTESTINAL FAILURE
Intestinal failure results from reduction in enterocyte cell mass, obstruction, dysmotility, surgical resection, congenital defects, or disease-associated loss of absorption with suboptimal nutritional autonomy.5 Patients often suffer from extensive nutrient, electrolyte, and fluid abnormalities proportional to the remnant length and part of the intestine removed.5
Epidemiologic studies have demonstrated that short-bowel syndrome is the most common cause of intestinal failure in adults and children.6,7 Short-bowel syndrome is defined as a small-bowel length less than 200 cm, most commonly from extensive resections for inflammatory bowel disease.6 In children, the syndrome is also defined by a residual small-bowel length of less than 25% expected for gestational age.7
Table 1 lists the frequencies of the underlying disorders leading to intestinal failure or short-bowel syndrome in one series.8
INTESTINAL ADAPTATION
The gastrointestinal tract is the only organ for nutrient, fluid, and electrolyte absorption.9 Every day, 8 to 9 L of fluids and secretions reach the small intestine, comprising about 2 to 3 L of oral fluids, 1 L of saliva, 2 L of gastric juices, 1 L of bile, and 2 L of pancreatic juices.9 Approximately 7 to 8 L are reabsorbed by the small intestine and 1 to 2 L by the colon.9
Although carbohydrates, lipids, and proteins are absorbed through the entire small intestine and colon, site-specific digestion and absorption of different nutrients occur in different parts of the gastrointestinal tract.10 Also, certain nutrients may need site-specific receptors or transporters for their absorption,10 for example:
- Iron in the duodenum and proximal jejunum1
- Lactose in the brush border membrane of the jejunum and proximal ileum, where most of the enzyme lactase is present
- Vitamin B12 and bile salts in the distal ileum.
Hence, resection of a specific part of the intestine may predict deficiencies the patient may encounter after surgery.
The diarrhea that occurs in short-bowel syndrome may be due partly to loss of neurohumoral mediators that govern gastrointestinal transit time, most importantly cholecystokinin, peptide YY, and glucagon-like peptide 1.11 After contact with lipid- or protein-rich nutrients, cholecystokinin is released from the proximal small intestine, which decreases the gastric emptying to maximize nutrient digestion.12 Additionally, release of peptide YY and glucagon-like peptide 1 from the ileal L cells decreases gastric and intestinal motility. These mediators prolong gastrointestinal transit, increase nutrient processing time, and enhance absorption.12
After massive intestinal resection, the remnant bowel undergoes physiologic and functional adaptation to maintain nutritional homeostasis.13 Enterocytes express membrane-bound transporters and undergo accelerated cell division to enhance the absorptive surface area.13 Intestinal hypertrophy, which includes an increase in villous diameter and crypt height, continues for 2 years or more after intestinal resection, leading to greater absorptive surface area.14 It is estimated that villous height may increase by as much as 80%, illustrating a dynamic process in response to intestinal stress.15
Luminal nutrients are essential to the stimulation of enterocyte cells through paracrine mechanisms as well as through the up-regulation of colonic peptide transporter PepT1.15 Furthermore, gut motility is initially decreased in order to increase the concentration of local luminal growth factors.16
Other factors that may affect intestinal adaptation are the length of the residual colon and small intestine, enteral growth, and enterotropic factors.16 And especially in patients with short-bowel syndrome, complications such as malabsorption secondary to pancreatic insufficiency or rapid transit, excessive gastric acid secretion, bile acid wasting due to terminal ileum resection, and bacterial overgrowth in the small intestine result in worsened nutritional status and poor quality of life.16
Key factors that affect the degree of nutritional deficiencies
The degree of nutritional deficiencies and fluid and electrolyte imbalances depends on the length and location of resection and whether the colon is still continuous with the small intestine.17 Normal small-bowel length in adults is highly variable and can be up to 600 cm. Malnutrition after surgical resection usually occurs when more than three-fourths of intestinal tissue is removed.17 However, because of intestinal adaptation, patients with 50% of remnant small bowel may be able to achieve nutritional autonomy.18 Furthermore, because absorption of nutrients occurs primarily in the first 150 cm of the small intestine, resections of this anatomic region have the highest probability of resulting in malnutrition.18
After extensive intestinal resection, absorption of water and electrolytes is better and intestinal transit time is longer if the colon is still continuous with the rest of the gastrointestinal system.19 Approximately 100 cm of remnant intestinal tissue without colonic continuity or 60 cm with colonic continuity is needed to ensure the possibility of nutritional autonomy and independence from parenteral nutrition.19 Severe malnutrition and fluid and electrolyte imbalances can be prevented by appropriate and timely multidisciplinary care and early referral for intestinal rehabilitation.
INTESTINAL REHABILITATION AND NUTRITIONAL AUTONOMY
The aim of intestinal rehabilitation is to improve quality of life by reversing malnutrition and promoting nutritional autonomy, ie, independence from parenteral nutrition (Table 2).20 The complex nature of intestinal failure necessitates collaboration of multiple specialists—gastroenterologists, surgeons, dietitians, nurses, psychiatrists or psychologists, pharmacists, and social workers.20
Although most patients with intestinal failure initially require parenteral nutrition to maintain nutritional homeostasis, progressive adaptation of the remnant intestine enables a transition to enteral nutrition.21 Stimulation of the remnant intestine by enteral feeding reduces the complications of parenteral nutrition and encourages intestinal adaptation.21
Outpatient participation in an intestinal rehabilitation program can facilitate weaning from parenteral nutrition. Patients are monitored and supported during dietary modification, pharmacologic interventions, and reconstructive surgeries.21 A study of 61 patients with short-bowel syndrome undergoing a 3-week program of intestinal rehabilitation (recombinant human growth hormone, glutamine, enteral nutrition, and parenteral nutrition) reported an overall survival rate of 95% with an 85% success rate in weaning from parenteral nutrition during a mean follow-up of 50 (± 24) months.22 Permanent dependence on parenteral nutrition despite rehabilitation was predicted by length of the small bowel less than 100 cm and by the absence of terminal ileum and colon.22
Permanent intestinal failure, defined by the inability to wean from parenteral nutrition and restore nutrition autonomy, may require early referral for evaluation for intestinal and multivisceral transplant. Early referral improves survival rates, possibly because of fewer complications from parenteral nutrition.4
DIETARY MODIFICATION
Dietary modification is the single most effective means of weaning patients safely from parenteral nutrition (Table 3).23,24 Small, frequent feedings help reduce symptoms associated with rapid intestinal transit and increase the activity of luminal growth factors.23 Likewise, limits on intake of simple sugars, stimulants such as caffeine or insoluble fiber, and hypo- or hypertonic fluids decrease intestinal losses and the risk of dehydration.23 Low sugar loads also aim to reduce the occurrence of d-lactic acidosis and bacterial overgrowth in the small intestine.23 Patients who cannot maintain positive fluid balance may require standardized oral rehydration (Table 4) to improve absorption by way of the sodium-glucose coupled transporters at the brush border membrane, or they may require intravenous fluid supplementation.25
Colonic continuity
Other dietary recommendations depend on colonic continuity. In 1994, Nordgaard et al26 compared the effects of high-carbohydrate and high-fat diets in eight patients with colonic continuity and six patients with jejunostomies. The authors noted that a high-carbohydrate diet (60% carbohydrate, 20% fat) reduced fecal loss of energy and increased energy absorption in patients with colonic continuity. However, patients with an end-jejunostomy experienced equal fecal losses of carbohydrates and fat proportional to the amount consumed. The authors concluded that the presence of colonic bacteria promoted carbohydrate salvage, ie, the fermentation of malabsorbed carbohydrates to easily absorbed short-chain fatty acids.26
The colon can salvage as much as 1,000 kcal/day in patients with less than 200 cm of small bowel, and the presence of at least 50% of colon in continuity has been shown to reduce parenteral nutrition requirements by half in patients with less than 100 cm of small bowel.27 As a result, a diet high in complex carbohydrates and soluble fiber supplements is recommended in cases of preserved colon to promote adaptation and nutritional autonomy.27
Another aim of a high-carbohydrate, low- fat diet is to prevent calcium oxalate-related nephrolithiasis and choleretic diarrhea.26
In summary, patients with short-bowel syndrome with or without colonic continuity need different dietary regimens to attain nutritional autonomy.
DRUG THERAPY
In addition to diet therapy, most patients with intestinal failure require pharmacologic therapy.28 High stool or stoma effluent is most commonly treated with an antidiarrheal to increase transit time; diphenoxylate-atropine, loperamide, codeine sulfate, paregoric, and opium tincture are commonly prescribed (Table 5).27 In severe high-output states, a somatostatin analogue (eg, octreotide) may be added.29
Postoperative increases in gastric secretion may be countered by histamine 2 receptor antagonists and proton pump inhibitors, but long-term use of these drugs may lead to nutritional deficiencies and bacterial overgrowth in the small intestine.29 Bile acid sequestrants (in cases of distal ileal resection) and pancreatic enzymes target fat malabsorption, resultant cases of choleretic diarrhea, deficiency of essential fatty acids, kidney stones, and deficiency of fat-soluble vitamins.29 Probiotics and antibiotics can also be given for prevention and treatment of small-intestinal bacterial overgrowth.29
When traditional dietary modification and medical therapy fail to achieve nutritional homeostasis, another option to consider is a glucagon-like peptide-2 analogue to enhance intestinal adaptation.30 Produced in the native distal ileum and colon, glucagon-like peptide 2 moderates the rate of gastric emptying and small-bowel transit and enhances epithelial cell proliferation, thereby promoting intestinal adaptation.30 Further, a randomized controlled trial of 83 patients reported efficacy of these agents in reducing parenteral nutrition requirements in patients with intestinal failure.31
Hence, in patients with intestinal failure who have increased stoma effluent, drug therapy may play an important role in maintaining fluid and nutritional homeostasis.
THE ROLE OF PARENTERAL NUTRITION IN INTESTINAL FAILURE
Despite the best efforts of an intestinal rehabilitation program, not all patients gain nutritional autonomy.32 Physiologic, psychological, social, and economic factors may contribute to dependence on parenteral nutrition.32 Currently, more than 40,000 US patients depend on it for survival.33
The need for short-term or long-term parenteral nutrition is determined by the patient’s medical needs.33 Patients requiring short-term parenteral nutrition (2–6 weeks) include those whose bowel function has not returned to normal postoperatively, and those who were severely malnourished preoperatively.34 Patients needing it long-term (from months to years to lifelong) are those with gastrointestinal dysmotility and short-bowel syndrome due to extensive bowel resections.33
Complications of parenteral nutrition
Catheter-related bloodstream infection is the most common complication and cause of hospitalization. Infection can be localized to the exit site or tunnel or can be systemic (eg, line sepsis).35Staphylococcus aureus and coagulase-negative staphylococci are most often implicated in catheter infection.35 When possible, catheter salvage is desirable, but the central venous catheter must be removed in cases of tunnel infection, port abscess, septic shock, paired blood cultures positive for fungi or highly virulent bacteria, endocarditis, septic thrombosis, and other conditions.35,36
Liver disease is a serious complication of long-term parenteral nutrition and may occur in up to 55% of patients on therapy for more than 2 years; it carries a mortality rate of 15%.37
Risk factors include younger age and use of excessive carbohydrate and fat compositions, mainly soybean-oil–based lipid emulsions.37 However, fish-oil–based lipid emulsions have recently shown promise in preventing and reversing parenteral nutrition-associated liver failure and cholestasis, especially in a pediatric population.38
Catheter thrombosis may occur in up to 30% of patients on long-term parenteral nutrition.39 However, this risk is reduced with appropriate positioning of the catheter tip in the mid or lower superior vena cava.37 Treatment of thrombosis of the central access includes either anticoagulation or thrombolysis.37
Hence, appropriate and timely follow-up of patients on parenteral nutrition is essential in reducing associated complications. Monitoring weight, fluid status, serum glucose, and patency of central access are critical to ensure that the patient maintains nutritional status effectively.40 To prevent complications, a specialized nutritional support team should monitor the patient’s parenteral nutrition both in the hospital and at home.
RECONSTRUCTIVE SURGERY
Patients with intestinal failure due to short- bowel syndrome should be considered for reconstructive surgery during different phases of the adaptation process. Options include reversed-segment procedures, stricturoplasty, bowel-lengthening procedures (eg, the Bianchi procedure), and serial transverse enteroplasty.41,42 If reconstructive surgery is ineffective, referral to an intestinal transplant program should be considered.
INTESTINAL AND MULTIVISCERAL TRANSPLANT
For patients who develop permanent intestinal failure and require lifelong parenteral nutrition, and for patients who experience significant complications of parenteral nutrition, such as infections and liver disease,43 intestinal transplant has emerged as a way to restore clinical nutritional autonomy.44 In one study, the 1-year survival rate after intestinal transplant was approximately 90%.44
There are currently three transplant procedures: isolated intestine transplant, combined liver-intestine transplant, and multivisceral transplant with or without a liver, depending on the presence of parenteral nutrition-associated liver disease.42,45 Close postoperative care is required to help the patient transition from parenteral to enteral nutrition.42 An intestinal rehabilitation team is equipped to provide this level of postoperative care.42
Intestinal and multivisceral transplant gained momentum in the early 1960s in preclinical and clinical studies.46,47 Since that time, the field has experienced remarkable advances due to standardization of surgical techniques, novel immunosuppressive therapies and induction protocols, and improved postoperative care.48 With the advent of tacrolimus in 1989, the rates of allograft rejection improved significantly, and the field of transplant emerged as a potentially lifesaving therapy for patients with permanent intestinal failure.48
Since 1990, more than 2,300 intestinal transplant procedures have been performed for various etiologies of intestinal failure, with short-bowel syndrome being the most common.49
The indications for intestinal transplant approved by the US Centers for Medicare and Medicaid services are detailed in Table 6.50 Despite ongoing challenges of graft rejection and maintenance immunosuppression, posttransplant quality-of-life questionnaires have indicated a significant improvement in functional status and a decrease in depressive symptoms.51 As such, it is evident that intestinal and multivisceral transplant offers substantial promise in restoring a patient’s quality of life and nutritional status.
- Parekh NR, Steiger E. Short bowel syndrome. Curr Treat Options Gastroenterol 2007; 10:10–23.
- Williamson RC. Intestinal adaptation (first of two parts). Structural, functional and cytokinetic changes. N Engl J Med 1978; 298:1393–1402.
- Vantini I, Benini L, Bonfante F, et al. Survival rate and prognostic factors in patients with intestinal failure. Dig Liver Dis 2004; 36:46–55.
- Abu-Elmagd KM, Bond GJ, Matarese L, et al. Gut rehabilitation and intestinal transplantation. Therapy 2005; 2:853–864.
- Nightingale JMD, Lennard-Jones JE. The short bowel syndrome: what’s new and old? Dig Dis 1993; 11:12–31.
- Parekh N, Seidner D, Steiger E. Managing short bowel syndrome: making the most of what the patient still has. Cleve Clin J Med 2005; 72:833–838.
- Wales PW. Surgical therapy for short bowel syndrome. Pediatr Surg Int 2004; 20:647–657.
- Parekh NR, Steiger E, Seidner DL. Determination of residual bowel length via surgical, radiological or historical data in patients with short bowel syndrome and intestinal failure (abstract). Gastroenterology 2006; 130:A605.
- Shatnawei A, Parekh NR, Rhoda KM, et al. Intestinal failure management at the Cleveland Clinic. Arch Surg 2010; 145:521–527.
- Kelly DG, Tappenden KA, Winkler MF. Short bowel syndrome: highlights of patient management, quality of life, and survival. JPEN J Parenter Enteral Nutr 2014; 38:427–437.
- Efsen E, Jeppesen PB. Modern treatment of adult short bowel syndrome patients. Minerva Gastroenterol Dietol 2011; 57:405–417.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Dowling RH, Booth DB. Functional compensation after small bowel resection in man. Lancet 1996; 2:146–147.
- Tappenden KA. Intestinal adaptation following resection. JPEN J Parenter Enteral Nutr 2014; 38(suppl 1):23S–31S.
- Friedman HI, Chandler JG, Peck CC, Nemeth TJ, Odum SK. Alterations in intestinal structure, fat absorption and body weight after intestinal bypass for morbid obesity. Surg Gynecol Obstet 1978; 146:757–767.
- O’Keefe SJ, Buchman AL, Fishbein TM, Jeejeebhoy KN, Jeppesen PB, Shaffer J. Short bowel syndrome and intestinal failure: consensus definitions and overview. Clin Gastroenterol Hepatol 2006; 4:6–10.
- Lennard-Jones JE. Review article: practical management of the short bowel. Aliment Pharmacol Ther 1994; 8:563–577.
- Goulet O, Colomb-Jung V, Joly F. Role of the colon in short bowel syndrome and intestinal transplantation. J Pediatr Gastroenterol Nutr 2009; 48(suppl 2):S66–S71.
- Jeppesen PB, Mortensen PB. Colonic digestion and absorption of energy from carbohydrates and medium-chain fat in small bowel failure. JPEN J Parenter Enteral Nutr 1999; 23(suppl 5):S101–S105.
- Buchman AL. Etiology and initial management of short bowel syndrome. Gastroenterology 2006; 130(suppl 1):S5–S15.
- Donohoe CL, Reynolds JV. Short bowel syndrome. Surgeon 2010; 8:270–279.
- Gong JF, Zhu WM, Yu WK, Li N, Li JS. Role of enteral nutrition in adult short bowel syndrome undergoing intestinal rehabilitation: the long-term outcome. Asia Pac J Clin Nutr 2009; 18:155–163.
- Sundaram A, Koutkia P, Apovian CM. Nutritional management of short bowel syndrome in adults. J Clin Gastroenterol 2002; 34:207–220.
- Byrne TA, Wilmore DW, Iyer K, et al. Growth hormone, glutamine, and an optimal diet reduces parenteral nutrition in patients with short bowel syndrome: a prospective, randomized, placebo-controlled, double-blind clinical trial. Ann Surg 2005; 242:655–661.
- Matarese LE, Steiger E. Dietary and medical management of short bowel syndrome in adult patients. J Clin Gastroenterol 2006; 40(suppl 2):S85–S93.
- Nordgaard I, Hansen BS, Mortensen PB. Colon as a digestive organ in patients with short bowel. Lancet 1994; 343:373–376.
- Ukleja A, Scolapio JS, Buchman AL. Nutritional management of short bowel syndrome. Semin Gastrointest Dis 2002; 13:161–168.
- Jeejeebhoy KN. Short bowel syndrome: a nutritional and medical approach. CMAJ 2002; 166:1297–1302.
- Seetharam P, Rodrigues G. Short bowel syndrome: a review of management options. Saudi J Gastroenterol 2011; 17:229–235.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B, O’Keefe SJ. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011; 60:902–914.
- Pironi L, Joly F, Forbes A, et al; Home Artificial Nutrition & Chronic Intestinal Failure Working Group of the European Society for Clinical Nutrition and Metabolism (ESPEN). Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut 2011; 60:17–25.
- Ekema G, Milianti S, Boroni G. Total parenteral nutrition in patients with short bowel syndrome. Minerva Pediatr 2009; 61:283–291.
- Messing B, Crenn P, Beau P, Boutron-Ruault MC, Rambaud JC, Matuchansky C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999; 117:1043–1050.
- Opilla M. Epidemiology of bloodstream infection associated with parenteral nutrition. Am J Infect Control 2008; 36:S173.e5–e8.
- Ukleja A, Romano MM. Complications of parenteral nutrition. Gastroenterol Clin North Am 2007; 36:23–46.
- Buchman AI, Iyer K, Fryer J. Parenteral nutrition-associated liver disease and the role for isolated intestine and intestine/liver transplantation. Hepatology 2006; 43:9–19.
- Fürst P, Kuhn KS. Fish oil emulsions: what benefits can they bring? Clin Nutr 2000; 19:7–14.
- Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol 2003; 21:3665–3675.
- McMahon MM, Nystrom E, Braunschweig C, Miles J, Compher C; American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors; American Society for Parenteral and Enteral Nutrition. American Society of Parenteral and Enteral Nutrition (ASPEN) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition support of adult patients with hyperglycemia. JPEN J Parenter Enteral Nutr 2013; 37:23–36.
- Kim HB, Fauza D, Garza J, Oh JT, Nurko S, Jaksic T. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg 2003; 38:425–429.
- King B, Carlson G, Khalil BA, Morabito A. Intestinal bowel lengthening in children with short bowel syndrome: systematic review of the Bianchi and STEP procedures. World J Surg 2013; 37:694–704.
- Matarese LE, O’Keefe SJ, Kandil HM, Costa G, Abu-Elmagd KM. Short bowel syndrome: clinical guidelines for nutrition management. Nutr Clin Pract 2005; 20:493–502.
- Abu-Elmagd KM, Costa G, Bond GJ, et al. Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg 2009; 250:567–581.
- Abu-Elmagd K. The concept of gut rehabilitation and the future of visceral transplantation. Nat Rev Gastroenterol Hepatol 2015; 12:108–120.
- Lillehei RC, Goott B, Miller FA. The physiological response of the small bowel of the dog to ischemia including prolonged in vitro preservation of the bowel with successful replacement and survival. Ann Surg 1959; 150:543–559.
- Starzl TE, Kaupp HA. Mass homotransplantation of abdominal organs in dogs. Surg Forum 1960; 11:28–30.
- O’Keefe SJ, Matarese L. Small bowel transplantation. Curr Gastroenterol Rep 2006; 8:360–366.
- Horslen SP. Optimal management of the post-intestinal transplant patient. Gastroenterology 2006; 130(suppl 1):S163–S169.
- Buchman AL, Scolapio J, Fryer J. AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 2003; 124:1111–1134.
- DiMartini A, Rovera GM, Graham TO, et al. Quality of life after small intestinal transplantation and among home parenteral nutrition patients. JPEN J Parenter Enteral Nutr 1998; 22:357–362.
- Parekh NR, Steiger E. Short bowel syndrome. Curr Treat Options Gastroenterol 2007; 10:10–23.
- Williamson RC. Intestinal adaptation (first of two parts). Structural, functional and cytokinetic changes. N Engl J Med 1978; 298:1393–1402.
- Vantini I, Benini L, Bonfante F, et al. Survival rate and prognostic factors in patients with intestinal failure. Dig Liver Dis 2004; 36:46–55.
- Abu-Elmagd KM, Bond GJ, Matarese L, et al. Gut rehabilitation and intestinal transplantation. Therapy 2005; 2:853–864.
- Nightingale JMD, Lennard-Jones JE. The short bowel syndrome: what’s new and old? Dig Dis 1993; 11:12–31.
- Parekh N, Seidner D, Steiger E. Managing short bowel syndrome: making the most of what the patient still has. Cleve Clin J Med 2005; 72:833–838.
- Wales PW. Surgical therapy for short bowel syndrome. Pediatr Surg Int 2004; 20:647–657.
- Parekh NR, Steiger E, Seidner DL. Determination of residual bowel length via surgical, radiological or historical data in patients with short bowel syndrome and intestinal failure (abstract). Gastroenterology 2006; 130:A605.
- Shatnawei A, Parekh NR, Rhoda KM, et al. Intestinal failure management at the Cleveland Clinic. Arch Surg 2010; 145:521–527.
- Kelly DG, Tappenden KA, Winkler MF. Short bowel syndrome: highlights of patient management, quality of life, and survival. JPEN J Parenter Enteral Nutr 2014; 38:427–437.
- Efsen E, Jeppesen PB. Modern treatment of adult short bowel syndrome patients. Minerva Gastroenterol Dietol 2011; 57:405–417.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Dowling RH, Booth DB. Functional compensation after small bowel resection in man. Lancet 1996; 2:146–147.
- Tappenden KA. Intestinal adaptation following resection. JPEN J Parenter Enteral Nutr 2014; 38(suppl 1):23S–31S.
- Friedman HI, Chandler JG, Peck CC, Nemeth TJ, Odum SK. Alterations in intestinal structure, fat absorption and body weight after intestinal bypass for morbid obesity. Surg Gynecol Obstet 1978; 146:757–767.
- O’Keefe SJ, Buchman AL, Fishbein TM, Jeejeebhoy KN, Jeppesen PB, Shaffer J. Short bowel syndrome and intestinal failure: consensus definitions and overview. Clin Gastroenterol Hepatol 2006; 4:6–10.
- Lennard-Jones JE. Review article: practical management of the short bowel. Aliment Pharmacol Ther 1994; 8:563–577.
- Goulet O, Colomb-Jung V, Joly F. Role of the colon in short bowel syndrome and intestinal transplantation. J Pediatr Gastroenterol Nutr 2009; 48(suppl 2):S66–S71.
- Jeppesen PB, Mortensen PB. Colonic digestion and absorption of energy from carbohydrates and medium-chain fat in small bowel failure. JPEN J Parenter Enteral Nutr 1999; 23(suppl 5):S101–S105.
- Buchman AL. Etiology and initial management of short bowel syndrome. Gastroenterology 2006; 130(suppl 1):S5–S15.
- Donohoe CL, Reynolds JV. Short bowel syndrome. Surgeon 2010; 8:270–279.
- Gong JF, Zhu WM, Yu WK, Li N, Li JS. Role of enteral nutrition in adult short bowel syndrome undergoing intestinal rehabilitation: the long-term outcome. Asia Pac J Clin Nutr 2009; 18:155–163.
- Sundaram A, Koutkia P, Apovian CM. Nutritional management of short bowel syndrome in adults. J Clin Gastroenterol 2002; 34:207–220.
- Byrne TA, Wilmore DW, Iyer K, et al. Growth hormone, glutamine, and an optimal diet reduces parenteral nutrition in patients with short bowel syndrome: a prospective, randomized, placebo-controlled, double-blind clinical trial. Ann Surg 2005; 242:655–661.
- Matarese LE, Steiger E. Dietary and medical management of short bowel syndrome in adult patients. J Clin Gastroenterol 2006; 40(suppl 2):S85–S93.
- Nordgaard I, Hansen BS, Mortensen PB. Colon as a digestive organ in patients with short bowel. Lancet 1994; 343:373–376.
- Ukleja A, Scolapio JS, Buchman AL. Nutritional management of short bowel syndrome. Semin Gastrointest Dis 2002; 13:161–168.
- Jeejeebhoy KN. Short bowel syndrome: a nutritional and medical approach. CMAJ 2002; 166:1297–1302.
- Seetharam P, Rodrigues G. Short bowel syndrome: a review of management options. Saudi J Gastroenterol 2011; 17:229–235.
- Wallis K, Walters JR, Gabe S. Short bowel syndrome: the role of GLP-2 on improving outcome. Curr Opin Clin Nutr Metab Care 2009; 12:526–532.
- Jeppesen PB, Gilroy R, Pertkiewicz M, Allard JP, Messing B, O’Keefe SJ. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011; 60:902–914.
- Pironi L, Joly F, Forbes A, et al; Home Artificial Nutrition & Chronic Intestinal Failure Working Group of the European Society for Clinical Nutrition and Metabolism (ESPEN). Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut 2011; 60:17–25.
- Ekema G, Milianti S, Boroni G. Total parenteral nutrition in patients with short bowel syndrome. Minerva Pediatr 2009; 61:283–291.
- Messing B, Crenn P, Beau P, Boutron-Ruault MC, Rambaud JC, Matuchansky C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999; 117:1043–1050.
- Opilla M. Epidemiology of bloodstream infection associated with parenteral nutrition. Am J Infect Control 2008; 36:S173.e5–e8.
- Ukleja A, Romano MM. Complications of parenteral nutrition. Gastroenterol Clin North Am 2007; 36:23–46.
- Buchman AI, Iyer K, Fryer J. Parenteral nutrition-associated liver disease and the role for isolated intestine and intestine/liver transplantation. Hepatology 2006; 43:9–19.
- Fürst P, Kuhn KS. Fish oil emulsions: what benefits can they bring? Clin Nutr 2000; 19:7–14.
- Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol 2003; 21:3665–3675.
- McMahon MM, Nystrom E, Braunschweig C, Miles J, Compher C; American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors; American Society for Parenteral and Enteral Nutrition. American Society of Parenteral and Enteral Nutrition (ASPEN) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition support of adult patients with hyperglycemia. JPEN J Parenter Enteral Nutr 2013; 37:23–36.
- Kim HB, Fauza D, Garza J, Oh JT, Nurko S, Jaksic T. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg 2003; 38:425–429.
- King B, Carlson G, Khalil BA, Morabito A. Intestinal bowel lengthening in children with short bowel syndrome: systematic review of the Bianchi and STEP procedures. World J Surg 2013; 37:694–704.
- Matarese LE, O’Keefe SJ, Kandil HM, Costa G, Abu-Elmagd KM. Short bowel syndrome: clinical guidelines for nutrition management. Nutr Clin Pract 2005; 20:493–502.
- Abu-Elmagd KM, Costa G, Bond GJ, et al. Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg 2009; 250:567–581.
- Abu-Elmagd K. The concept of gut rehabilitation and the future of visceral transplantation. Nat Rev Gastroenterol Hepatol 2015; 12:108–120.
- Lillehei RC, Goott B, Miller FA. The physiological response of the small bowel of the dog to ischemia including prolonged in vitro preservation of the bowel with successful replacement and survival. Ann Surg 1959; 150:543–559.
- Starzl TE, Kaupp HA. Mass homotransplantation of abdominal organs in dogs. Surg Forum 1960; 11:28–30.
- O’Keefe SJ, Matarese L. Small bowel transplantation. Curr Gastroenterol Rep 2006; 8:360–366.
- Horslen SP. Optimal management of the post-intestinal transplant patient. Gastroenterology 2006; 130(suppl 1):S163–S169.
- Buchman AL, Scolapio J, Fryer J. AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 2003; 124:1111–1134.
- DiMartini A, Rovera GM, Graham TO, et al. Quality of life after small intestinal transplantation and among home parenteral nutrition patients. JPEN J Parenter Enteral Nutr 1998; 22:357–362.
KEY POINTS
- Some patients with intestinal failure require lifelong parenteral nutrition, which increases the risk of complications such as infection and liver disease. For these patients, intestinal transplant has emerged as a therapeutic option toward the goal of restoring nutritional autonomy.
- The complexities of intestinal failure require collaboration of multiple specialists—gastroenterologists, surgeons, dietitians, nurses, psychiatrists or psychologists, pharmacists, and social workers. This multidisciplinary team is essential to intestinal rehabilitation.
- Dietary modification is the single most effective means of weaning patients safely from parenteral nutrition.