User login
Compared with hemodialysis (HD), peritoneal dialysis (PD) offers comparable survival and superior patient-centered and health services outcomes.1,2 This has prompted repeated calls over the past 2 decades for policies to increase the use of home dialysis and, more specifically, for PD in the United States.3,4
Veterans comprise nearly 10% of the population with end-stage kidney disease (ESKD) burden; > 50,000 US veterans are currently on dialysis.5,6 A majority of these veterans receive their chronic kidney disease (CKD) care through their affiliated US Department of Veterans Affairs (VA) medical centers (VAMCs).
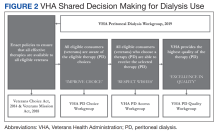
To address these needs, the VHA National Kidney Disease Program (NKDP) formed a 4-member PD workgroup in 2019. Considering the breadth of challenges involved, the PD workgroup broadly designed its approach based on the I CARE (Integrity, Commitment, Advocacy, Respect, and Excellence) VA Core Values.
This review focuses on the initial deliberations of the PD access subgroup and provides a guide to establishing a new local VA PD program.
Step 1: Prerequisites
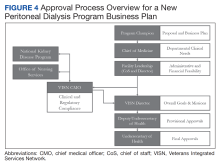
A functional nephrology service is a bedrock prerequisite for establishing a new PD program. A clinician champion capable of leading the effort is equally necessary. Occasionally, the prevalent ESKD economic and health care burden prompts local VAMC leadership to consider a new PD program to improve the quality or availability of services. More commonly, though, the nephrology section and the clinician champion are the first to recognize the need. In either scenario, the champion will require support and advocacy at multiple levels of local leadership, ie, the section or department chief, facility chief of staff, VAMC director, and the Veterans Integrated Service Network (VISN) director. The foremost task for the champion is to assess local clinical and infrastructure needs.
Goal Alignment
Any new VA nephrology program needs to be evaluated for its overall congruence with the local and national VA missions to improve the accessibility, integration, quality, and innovation of care for veterans. The following considerations are likely to apply to many VA systems.
Accessibility. A VHA directive recommends that all veterans be provided with the opportunity to choose and use any form of dialysis, especially home dialysis.9 Transitioning a veteran seamlessly from advanced CKD to PD requires the execution of multiple sequential processes in the pre-ESKD period, beginning with early identification of advanced CKD, timely referral to nephrology, education for shared dialysis decision making, coordination of care, and PD training and therapy.10 Splitting this sequence between VA and community-based care creates obstacles, including multiple approvals through VA Community Care Services that may substantially increase wait time and effort. This onerous process may be a significant deterrent against pursuing PD and increases the odds of emergency or inpatient initiation. Furthermore, the lack of PD availability limits the knowledge and experience among staff designated to assist veterans, which may result in inappropriate advocacy for HD or delay the transition to PD. Together, these processes can increase morbidity and health care use, and significantly delay or eliminate PD. Finally, many veterans reside in rural or remote areas where the expertise and the availability of PD may be unreliable. Establishing PD services within the local VAMC can improve access to PD, reduce the lead time needed to coordinate the transition to ESKD, and assist individual veterans in making an informed choice about dialysis. The program champion will need to identify and highlight all accessibility barriers within their business plan.
Integration. Many veterans receiving dialysis care at community-based facilities continue to receive nonnephrology care in the VA. This creates a parallel health care system with concerns for duplication of efforts and processes, suboptimal quality of care, and increased risk of medical errors. Establishing VA PD services increases access and integration of nephrology with other VA care.
Excellence. Studies of many chronic diseases have shown superior patient satisfaction and equal or superior quality of care delivered by the VA compared with that of non-VA facilities.11-14 Similarly, mortality rates for veterans receiving CKD and ESKD care in VA are lower compared with those at non-VA facilities.15-17 While these outcomes have not been examined for PD, integration of PD with VA care may lead to an improved overall quality of care and greater loyalty to the VA.
Innovation. Due to its integrated health care infrastructure, the VA is uniquely positioned to implement patient-centered and evidence-based pre-ESKD interventions that may improve outcomes. Prior studies have shown that pre-ESKD kidney disease education (KDE) improves pre- and post-ESKD outcomes, reduces health care costs, and leads to higher selection and use of home dialysis therapies.18-20 The VA recommends that all veterans with advanced CKD be provided access to pre-ESKD care and KDE. Unfortunately, KDE is uncommon among non-VA clinicians. A recent USRDS analysis reported that < 1% of patients with ESKD received pre-ESKD KDE.21 The ongoing Evaluate and Assess the effects of Comprehensive Pre-ESKD kidney disease Education on home dialysis in Veterans Trial (NCT04064086) should provide further evidence.
Step 2: Feasibility
A business plan requires the realistic projections of the costs and accounting for gains of the new clinical program. While there is limited guidance on personnel requirements when planning a PD program, we provide estimated resources needed to successfully establish and run a PD program (eAppendix 1, available online at doi:10.12788/fp.0356).
Clinical Considerations
Secondary or tertiary care VAMCs with multiple medical and surgical specialties routinely provide complex inpatient care. For these facilities, the lack of inpatient PD poses an obstacle to the provision of specialized nonnephrology care to veterans with ESKD, who are frequent users of such complex care. These considerations argue for the need for at least inpatient PD services at VAMCs that provide complex medical care for many veterans receiving PD in the community.
Deliberations for outpatient PD programs should be based on the clinical demands of ESKD care, the number of veterans likely to use PD, and growth projections. While there is no established minimum number that guarantees cost-effectiveness, most existing VA outpatient PD programs provide services for about 5 to 25 veterans. A local census can provide estimations of future PD needs. Travel considerations (ie, distance, terrain, traffic) may affect eligibility for purchased care and the decision where to receive PD. Many veterans may prefer PD from the local VAMC if it is convenient and allows them to maintain centralized VA care. Potential patients can be surveyed to gauge interest in receiving VA-based PD. Facilities providing structured pre-ESKD KDE may hold greater potential for PD growth, and it is important to highlight KDE infrastructure in the business plan.
Infrastructure
Spatial needs including clinic space and storage space for consumables, supplies, and equipment should be part of infrastructure requirements. The program champion may need to examine the available space for suitability and adequacy of the PD program early in the process. Ventilation renovations in the PD rooms should be incorporated into budget calculations. Water access for handwashing and PD effluent drainage should be confirmed, and if the program intends to establish home HD, additional considerations for the storage and water supply may be required. The VHA Handbook outlines the infrastructure requirements for a dialysis program.22 The VA has established national vendor contracts for dialysis equipment and consumables. However, a new PD program may need further guidance regarding the local agencies that provide administrative support and assist patients.
Telehealth technology has enabled many VAMCs to overcome geographical barriers for rural veterans.23 Ongoing expansion of community-based outpatient clinics (CBOCs) to include more rural locations is improving access to specialty care, while the launch of VA Video Connect (VVC) has further improved outreach. Investigators from Minneapolis have demonstrated the feasibility of multidisciplinary home-based telehealth management of veterans with CKD.24 Several existing nephrology sections across the VHA use a combination of VVC and CBOC-facilitated clinic visits to provide some pre-ESKD and ESKD care, including KDE, PD home visits and training, and comprehensive ESKD care visits. Recent changes in the clinical care pattern during the COVID-19 pandemic have further eased ESKD telehealth protocols. Integrating the projected use of telehealth in collaboration with existing resources available through the VHA NKDP can allow the local champion to improve the financial feasibility and long-term success of a new PD program.
Clinicians
Experience and expertise in managing PD vary among nephrologists. A recent survey found that only 11% of second-year nephrology trainees felt fully prepared to manage PD patients and 27% felt that they were minimally prepared.25 Thus, it is important to ensure that adequately trained nephrologists are available locally before initiating a new program, and if needed, coverage across VHS or VISN can be explored. One potential method to enhance practitioner comfort in PD is the use of existing peer-to-peer education through the VA Kidney Specialty Care Access Network-Extension for Community Health care Outcomes program that links health care professionals in rural areas with specialists at a tertiary care center.23 Nurses are a primary pillar for the success of home dialysis programs and the lack of a trained nursing workforce can be a significant limitation. Similarly, while the placement and management of complications related to PD catheters are not technically challenging, the availability of interventionists (either a surgeon or trained interventional radiologist) should be part of the business plan.
Financial Considerations
The financial considerations involving a new PD program within the VHA are complex (eAppendix 2, available online at doi:10.12788/fp.0356). ESKD is one of the most complex and costly comorbidities. It is a major determinant of the expenditure and revenue generation for facilities. The Veterans Equitable Resource Allocation system classifies ESKD on repeated dialysis as price category 10, indicating high complexity and cost. The VAMC workload and facility budget allocation is assessed annually and increases as the population of price group 10 veterans increases. VHA also provides additional Veterans Equitable Resource Allocation funds to VAMCs, which can improve the bottom line for VA-based dialysis units. Providing PD facilitates outpatient and inpatient management of comorbidities, allowing for substantial cost savings while improving the quality of nonrenal care. Outsourcing dialysis care can reduce the administrative burden, although, it deprives the VAMC of all dialysis-associated revenues while bearing the cost of all nonrenal and some renal care. The net effect is reduced facility productivity. In aggregate, establishing a local dialysis program requires greater financial resources for the capital and personnel costs; however, if captured appropriately these funds can be a major source of revenue and savings for the local VAMC.
Indirect costs are important for financial projections. Most community dialysis units operate as outpatient units, whereas all but a handful of the VA dialysis units operate within or near a VAMC. As a result, the VA units providing maintenance dialysis are regularly classified as inpatient centers while providing largely outpatient services, which negatively impacts overhead cost calculations. The predominant use of in-center HD as the default modality further sets an erroneously high baseline for the indirect cost of the VA-based PD services, especially considering that the principal savings of the home dialysis are through the reduction in the labor and capital costs. A rudimentary make-buy model for the in-center HD is available through the NKDP, and establishing a similar model for PD programs may be useful.
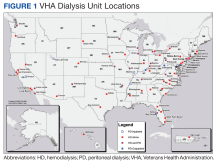
Cost considerations also may vary based on the model of ESKD care used locally. Of the 71 hospital-based and free-standing VA HD facilities, only 33 provide PD services, with 5 units providing only inpatient PD. The financial burden of establishing a fully operational outpatient PD program will be based on whether it is targeting a new unit or is expanding. The costs for equipment rental, disposables, and supplies vary based on the VA contract negotiations but are standardized across the nation with approved cost-of-living geographic adjustments. Caution needs to be exercised in employing a phased-hiring approach, as newer programs may require proportionally larger nursing resources due to greater needs for KDE, transitioning services, and training for PD. A target census-based hiring schedule should be negotiated with leadership before launch. If existing labor mapping does not allow for cross-coverage, part-time positions for physicians may be considered. Travel nurses, especially for PD training, can be considered to meet labor needs when long-term projections prohibit permanent full-time hires.
Finally, the balance sheet of a new program needs to account for different scenarios. In addition to nephrology costs, outsourcing veterans for PD services incurs multiple costs (eg, administrative, social work). Facilities with inpatient PD services alone are likely already bearing a component of the medications (including antibiotics) and/or surgical costs for their outsourced patients. These hidden costs are infrequently counted in projections. Facilities without inpatient PD cannot provide complex nonrenal care to ESKD patients on PD, even when the center is well equipped to provide it. These facilities also bear the cost of outsourcing even for complications related to PD. While a full estimation of these services varies, the hidden cost savings of many procedures or inpatient admissions, such as cardiovascular or musculoskeletal surgeries, can exceed those of dialysis in this complex population.
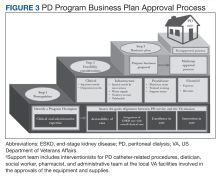
Step 3: proposal
There are no standardized formats for presenting a VHA business proposal; however, this outline provides a template. The business proposal should be designed to effectively communicate the collective data that describe the needs and requirements of a PD program to the local, regional, and national leadership. Not every rationale presented here will apply to an individual proposal and the local champion will need to tailor their rationale for their locale. A sample business plan is shown in eAppendix 3 (available online at doi:10.12788/fp.0356). VHA Handbook of dialysis requires that a PD nurse has a minimum of 12 months of nursing experience with at least 3 months of PD experience.25 Nursing training, education, and support should be discussed with nursing leadership and included in the business plan. Similarly, arrangements for laboratory, pharmacy, and prosthetics services and/or logistics to facilitate procurement of the needed devices, disposables, and supplies are essential and should be highlighted in the business plan.
Approval Process
Postapproval Process
Once approved, the champion will need to work closely with various services and managers to oversee infrastructural renovations and execute the hiring plans, establish standard operating procedures (SOPs), standardize staff proficiencies and functional statements, and finalize quality assessment parameters. Home dialysis standards have been addressed by NKDP and The Joint Commission. While PD requires home visits to assess the appropriateness of the environment, the PD program is accredited under hospital-based therapy. Standards and performance metrics should be incorporated into all the VA PD programs for standardization and assessment. Based on guidance from the VHA Handbook, quality metrics, such as dialysis adequacy, and rates of infection should be monitored and reviewed. The dialysis director may need to consider more frequent program evaluations in the first year to ensure appropriate troubleshooting. The VA infrastructure has developed the resources for a central repository for the PD SOPs and quality metrics, which can be obtained and adapted for the local program. Similarly, veteran satisfaction can be assessed through existing resources. Finally, the dialysis director can join the National VHA Dialysis Director listserv for regular updates on the existing and new VHA policies and NKDP updates.
Conclusions
Establishing a new PD program within a local federal infrastructure can appear daunting, both in terms of planning as well as approvals. However, the provision of home-based dialysis therapies may be beneficial to those in rural settings with limited access to in-center dialysis modalities as well as to those who seek autonomy and lifestyle independence in their medical care. Collaborations with the VHA NKDP or PD workgroup can help overcome many of the procedural hurdles, provide guidance about infrastructure and resource allocation and utilization, and provide easy access to established SOPs and quality parameters.
Acknowledgments
We acknowledge the late Dr. Catherine Do for her significant contribution to this manuscript. We also extend our sincere thanks to Dr. Holly Mattix-Kramer (Edward Hines Jr. Veterans Affairs Hospital and Loyola University Medical Center) for her prompt and valuable feedback on this manuscript.
1. Jung HY, Jeon Y, Park Y, et al. Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci Rep. 2019;9(1):10266. Published 2019 Jul 16. doi:10.1038/s41598-019-46744-1
2. Wong B, Ravani P, Oliver MJ, et al. Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71(3):344-351. doi:10.1053/j.ajkd.2017.08.028
3. Chan CT, Collins K, Ditschman EP, et al. Overcoming barriers for uptake and continued use of home dialysis: an NKF-KDOQI Conference report. Am J Kidney Dis. 2020;75(6):926-934. doi:10.1053/j.ajkd.2019.11.007
4. Executive Order 13879: Advancing American kidney health. Fed Regist. 2019; 84(135):33817-33819. https://www.govinfo.gov/content/pkg/FR-2019-07-15/pdf/2019-15159.pdf
5. Patel TG, Pogach LM, Barth RH. CKD screening and management in the Veterans Health Administration: the impact of system organization and an innovative electronic record. Am J Kidney Dis. 2009;53(suppl 3):S78-S85. doi:10.1053/j.ajkd.2008.07.051
6. Saran R, Pearson A, Tilea A, et al. Burden and cost of caring for US veterans with CKD: initial findings from the VA Renal Information System (VA-REINS). Am J Kidney Dis. 2021;77(3):397-405. doi:10.1053/j.ajkd.2020.07.013
7. Sloan CE, Coffman CJ, Sanders LL, et al. Trends in peritoneal dialysis use in the United States after Medicare payment reform. Clin J Am Soc Nephrol. 2019;14(12):1763-1772. doi:10.2215/CJN.05910519
8. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. HR 5674. 115th Congress; Report No. 115-671, Part 1. May 3, 2018. Accessed February 9, 2023. https://www.congress.gov/115/bills/hr5674/BILLS-115hr5674rh.pdf
9. US Department of Veterans Affairs, Veterans Health Administration. Chronic kidney disease prevention, early recognition, and management. VHA Directive 1053. March 17, 2020. Accessed February 9, 2023. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8737
10. Blake PG, Quinn RR, Oliver MJ. Peritoneal dialysis and the process of modality selection. Perit Dial Int. 2013;33(3):233-241. doi:10.3747/pdi.2012.00119
11. Stroupe KT, Hynes DM, Giobbie-Hurder A, et al. Patient satisfaction and use of Veterans Affairs versus non-Veterans Affairs healthcare services by veterans. Med Care. 2005;43(5):453-460. doi:10.1097/01.mlr.0000160377.82164.d3
12. Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing quality of care in Veterans Affairs and non-Veterans Affairs settings. J Gen Intern Med. 2018;33(10):1631-1638. doi:10.1007/s11606-018-4433-7
13. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885. doi:10.1001/jamainternmed.2017.0605
14. Nuti SV, Qin L, Krumholz HM. Outcome after admission at Veterans Affairs vs non-Veterans Affairs hospitals--reply. JAMA. 2016;316(3):346. doi:10.1001/jama.2016.5394
15. Streja E, Kovesdy CP, Soohoo M, et al. Dialysis provider and outcomes among United States veterans who transition to dialysis. Clin J Am Soc Nephrol. 2018;13(7):1055-1062. doi:10.2215/CJN.12951117
16. Wang V, Coffman CJ, Stechuchak KM, et al. Survival among veterans obtaining dialysis in VA and non-VA settings. J Am Soc Nephrol. 2019;30(1):159-168. doi:10.1681/ASN.2018050521
17. Kurella Tamura M, Thomas IC, Montez-Rath ME, et al. Dialysis initiation and mortality among older veterans with kidney failure treated in Medicare vs the Department of Veterans Affairs. JAMA Intern Med. 2018;178(5):657-664. doi:10.1001/jamainternmed.2018.0411
18. Devins GM, Mendelssohn DC, Barré PE, Taub K, Binik YM. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46(6):1088-1098. doi:10.1053/j.ajkd.2005.08.017
19. Devoe DJ, Wong B, James MT, et al. Patient education and peritoneal dialysis modality selection: a systematic review and meta-analysis. Am J Kidney Dis. 2016;68(3):422-433. doi:10.1053/j.ajkd.2016.02.053
20. Lin E, Chertow GM, Yan B, Malcolm E, Goldhaber-Fiebert JD. Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study. PLoS Med. 2018;15(3):e1002532. Published 2018 Mar 27. doi:10.1371/journal.pmed.1002532
21. Shukla AM, Bozorgmehri S, Ruchi R, et al. Utilization of CMS pre-ESRD Kidney Disease Education services and its associations with the home dialysis therapies. Perit Dial Int. 2021;41(5):453-462. doi:10.1177/0896860820975586
22. US Dept of Veterans Affairs, Veterans Health Administration. Criteria and standards for VA dialysis programs. VHA Directive 1601. 2016. May 23, 2016. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3205
23. Crowley ST, Belcher J, Choudhury D, et al. Targeting access to kidney care via telehealth: the VA experience. Adv Chronic Kidney Dis. 2017;24(1):22-30. doi:10.1053/j.ackd.2016.11.005
24. Ishani A, Christopher J, Palmer D, et al. Telehealth by an interprofessional team in patients with CKD: a randomized controlled trial. Am J Kidney Dis. 2016;68(1):41-49. doi:10.1053/j.ajkd.2016.01.018
25. Gupta N, Taber-Hight EB, Miller BW. Perceptions of home dialysis training and experience among US nephrology fellows. Am J Kidney Dis. 2021;77(5):713-718.e1. doi:10.1053/j.ajkd.2020.09.014
Compared with hemodialysis (HD), peritoneal dialysis (PD) offers comparable survival and superior patient-centered and health services outcomes.1,2 This has prompted repeated calls over the past 2 decades for policies to increase the use of home dialysis and, more specifically, for PD in the United States.3,4
Veterans comprise nearly 10% of the population with end-stage kidney disease (ESKD) burden; > 50,000 US veterans are currently on dialysis.5,6 A majority of these veterans receive their chronic kidney disease (CKD) care through their affiliated US Department of Veterans Affairs (VA) medical centers (VAMCs).
To address these needs, the VHA National Kidney Disease Program (NKDP) formed a 4-member PD workgroup in 2019. Considering the breadth of challenges involved, the PD workgroup broadly designed its approach based on the I CARE (Integrity, Commitment, Advocacy, Respect, and Excellence) VA Core Values.
This review focuses on the initial deliberations of the PD access subgroup and provides a guide to establishing a new local VA PD program.
Step 1: Prerequisites
A functional nephrology service is a bedrock prerequisite for establishing a new PD program. A clinician champion capable of leading the effort is equally necessary. Occasionally, the prevalent ESKD economic and health care burden prompts local VAMC leadership to consider a new PD program to improve the quality or availability of services. More commonly, though, the nephrology section and the clinician champion are the first to recognize the need. In either scenario, the champion will require support and advocacy at multiple levels of local leadership, ie, the section or department chief, facility chief of staff, VAMC director, and the Veterans Integrated Service Network (VISN) director. The foremost task for the champion is to assess local clinical and infrastructure needs.
Goal Alignment
Any new VA nephrology program needs to be evaluated for its overall congruence with the local and national VA missions to improve the accessibility, integration, quality, and innovation of care for veterans. The following considerations are likely to apply to many VA systems.
Accessibility. A VHA directive recommends that all veterans be provided with the opportunity to choose and use any form of dialysis, especially home dialysis.9 Transitioning a veteran seamlessly from advanced CKD to PD requires the execution of multiple sequential processes in the pre-ESKD period, beginning with early identification of advanced CKD, timely referral to nephrology, education for shared dialysis decision making, coordination of care, and PD training and therapy.10 Splitting this sequence between VA and community-based care creates obstacles, including multiple approvals through VA Community Care Services that may substantially increase wait time and effort. This onerous process may be a significant deterrent against pursuing PD and increases the odds of emergency or inpatient initiation. Furthermore, the lack of PD availability limits the knowledge and experience among staff designated to assist veterans, which may result in inappropriate advocacy for HD or delay the transition to PD. Together, these processes can increase morbidity and health care use, and significantly delay or eliminate PD. Finally, many veterans reside in rural or remote areas where the expertise and the availability of PD may be unreliable. Establishing PD services within the local VAMC can improve access to PD, reduce the lead time needed to coordinate the transition to ESKD, and assist individual veterans in making an informed choice about dialysis. The program champion will need to identify and highlight all accessibility barriers within their business plan.
Integration. Many veterans receiving dialysis care at community-based facilities continue to receive nonnephrology care in the VA. This creates a parallel health care system with concerns for duplication of efforts and processes, suboptimal quality of care, and increased risk of medical errors. Establishing VA PD services increases access and integration of nephrology with other VA care.
Excellence. Studies of many chronic diseases have shown superior patient satisfaction and equal or superior quality of care delivered by the VA compared with that of non-VA facilities.11-14 Similarly, mortality rates for veterans receiving CKD and ESKD care in VA are lower compared with those at non-VA facilities.15-17 While these outcomes have not been examined for PD, integration of PD with VA care may lead to an improved overall quality of care and greater loyalty to the VA.
Innovation. Due to its integrated health care infrastructure, the VA is uniquely positioned to implement patient-centered and evidence-based pre-ESKD interventions that may improve outcomes. Prior studies have shown that pre-ESKD kidney disease education (KDE) improves pre- and post-ESKD outcomes, reduces health care costs, and leads to higher selection and use of home dialysis therapies.18-20 The VA recommends that all veterans with advanced CKD be provided access to pre-ESKD care and KDE. Unfortunately, KDE is uncommon among non-VA clinicians. A recent USRDS analysis reported that < 1% of patients with ESKD received pre-ESKD KDE.21 The ongoing Evaluate and Assess the effects of Comprehensive Pre-ESKD kidney disease Education on home dialysis in Veterans Trial (NCT04064086) should provide further evidence.
Step 2: Feasibility
A business plan requires the realistic projections of the costs and accounting for gains of the new clinical program. While there is limited guidance on personnel requirements when planning a PD program, we provide estimated resources needed to successfully establish and run a PD program (eAppendix 1, available online at doi:10.12788/fp.0356).
Clinical Considerations
Secondary or tertiary care VAMCs with multiple medical and surgical specialties routinely provide complex inpatient care. For these facilities, the lack of inpatient PD poses an obstacle to the provision of specialized nonnephrology care to veterans with ESKD, who are frequent users of such complex care. These considerations argue for the need for at least inpatient PD services at VAMCs that provide complex medical care for many veterans receiving PD in the community.
Deliberations for outpatient PD programs should be based on the clinical demands of ESKD care, the number of veterans likely to use PD, and growth projections. While there is no established minimum number that guarantees cost-effectiveness, most existing VA outpatient PD programs provide services for about 5 to 25 veterans. A local census can provide estimations of future PD needs. Travel considerations (ie, distance, terrain, traffic) may affect eligibility for purchased care and the decision where to receive PD. Many veterans may prefer PD from the local VAMC if it is convenient and allows them to maintain centralized VA care. Potential patients can be surveyed to gauge interest in receiving VA-based PD. Facilities providing structured pre-ESKD KDE may hold greater potential for PD growth, and it is important to highlight KDE infrastructure in the business plan.
Infrastructure
Spatial needs including clinic space and storage space for consumables, supplies, and equipment should be part of infrastructure requirements. The program champion may need to examine the available space for suitability and adequacy of the PD program early in the process. Ventilation renovations in the PD rooms should be incorporated into budget calculations. Water access for handwashing and PD effluent drainage should be confirmed, and if the program intends to establish home HD, additional considerations for the storage and water supply may be required. The VHA Handbook outlines the infrastructure requirements for a dialysis program.22 The VA has established national vendor contracts for dialysis equipment and consumables. However, a new PD program may need further guidance regarding the local agencies that provide administrative support and assist patients.
Telehealth technology has enabled many VAMCs to overcome geographical barriers for rural veterans.23 Ongoing expansion of community-based outpatient clinics (CBOCs) to include more rural locations is improving access to specialty care, while the launch of VA Video Connect (VVC) has further improved outreach. Investigators from Minneapolis have demonstrated the feasibility of multidisciplinary home-based telehealth management of veterans with CKD.24 Several existing nephrology sections across the VHA use a combination of VVC and CBOC-facilitated clinic visits to provide some pre-ESKD and ESKD care, including KDE, PD home visits and training, and comprehensive ESKD care visits. Recent changes in the clinical care pattern during the COVID-19 pandemic have further eased ESKD telehealth protocols. Integrating the projected use of telehealth in collaboration with existing resources available through the VHA NKDP can allow the local champion to improve the financial feasibility and long-term success of a new PD program.
Clinicians
Experience and expertise in managing PD vary among nephrologists. A recent survey found that only 11% of second-year nephrology trainees felt fully prepared to manage PD patients and 27% felt that they were minimally prepared.25 Thus, it is important to ensure that adequately trained nephrologists are available locally before initiating a new program, and if needed, coverage across VHS or VISN can be explored. One potential method to enhance practitioner comfort in PD is the use of existing peer-to-peer education through the VA Kidney Specialty Care Access Network-Extension for Community Health care Outcomes program that links health care professionals in rural areas with specialists at a tertiary care center.23 Nurses are a primary pillar for the success of home dialysis programs and the lack of a trained nursing workforce can be a significant limitation. Similarly, while the placement and management of complications related to PD catheters are not technically challenging, the availability of interventionists (either a surgeon or trained interventional radiologist) should be part of the business plan.
Financial Considerations
The financial considerations involving a new PD program within the VHA are complex (eAppendix 2, available online at doi:10.12788/fp.0356). ESKD is one of the most complex and costly comorbidities. It is a major determinant of the expenditure and revenue generation for facilities. The Veterans Equitable Resource Allocation system classifies ESKD on repeated dialysis as price category 10, indicating high complexity and cost. The VAMC workload and facility budget allocation is assessed annually and increases as the population of price group 10 veterans increases. VHA also provides additional Veterans Equitable Resource Allocation funds to VAMCs, which can improve the bottom line for VA-based dialysis units. Providing PD facilitates outpatient and inpatient management of comorbidities, allowing for substantial cost savings while improving the quality of nonrenal care. Outsourcing dialysis care can reduce the administrative burden, although, it deprives the VAMC of all dialysis-associated revenues while bearing the cost of all nonrenal and some renal care. The net effect is reduced facility productivity. In aggregate, establishing a local dialysis program requires greater financial resources for the capital and personnel costs; however, if captured appropriately these funds can be a major source of revenue and savings for the local VAMC.
Indirect costs are important for financial projections. Most community dialysis units operate as outpatient units, whereas all but a handful of the VA dialysis units operate within or near a VAMC. As a result, the VA units providing maintenance dialysis are regularly classified as inpatient centers while providing largely outpatient services, which negatively impacts overhead cost calculations. The predominant use of in-center HD as the default modality further sets an erroneously high baseline for the indirect cost of the VA-based PD services, especially considering that the principal savings of the home dialysis are through the reduction in the labor and capital costs. A rudimentary make-buy model for the in-center HD is available through the NKDP, and establishing a similar model for PD programs may be useful.
Cost considerations also may vary based on the model of ESKD care used locally. Of the 71 hospital-based and free-standing VA HD facilities, only 33 provide PD services, with 5 units providing only inpatient PD. The financial burden of establishing a fully operational outpatient PD program will be based on whether it is targeting a new unit or is expanding. The costs for equipment rental, disposables, and supplies vary based on the VA contract negotiations but are standardized across the nation with approved cost-of-living geographic adjustments. Caution needs to be exercised in employing a phased-hiring approach, as newer programs may require proportionally larger nursing resources due to greater needs for KDE, transitioning services, and training for PD. A target census-based hiring schedule should be negotiated with leadership before launch. If existing labor mapping does not allow for cross-coverage, part-time positions for physicians may be considered. Travel nurses, especially for PD training, can be considered to meet labor needs when long-term projections prohibit permanent full-time hires.
Finally, the balance sheet of a new program needs to account for different scenarios. In addition to nephrology costs, outsourcing veterans for PD services incurs multiple costs (eg, administrative, social work). Facilities with inpatient PD services alone are likely already bearing a component of the medications (including antibiotics) and/or surgical costs for their outsourced patients. These hidden costs are infrequently counted in projections. Facilities without inpatient PD cannot provide complex nonrenal care to ESKD patients on PD, even when the center is well equipped to provide it. These facilities also bear the cost of outsourcing even for complications related to PD. While a full estimation of these services varies, the hidden cost savings of many procedures or inpatient admissions, such as cardiovascular or musculoskeletal surgeries, can exceed those of dialysis in this complex population.
Step 3: proposal
There are no standardized formats for presenting a VHA business proposal; however, this outline provides a template. The business proposal should be designed to effectively communicate the collective data that describe the needs and requirements of a PD program to the local, regional, and national leadership. Not every rationale presented here will apply to an individual proposal and the local champion will need to tailor their rationale for their locale. A sample business plan is shown in eAppendix 3 (available online at doi:10.12788/fp.0356). VHA Handbook of dialysis requires that a PD nurse has a minimum of 12 months of nursing experience with at least 3 months of PD experience.25 Nursing training, education, and support should be discussed with nursing leadership and included in the business plan. Similarly, arrangements for laboratory, pharmacy, and prosthetics services and/or logistics to facilitate procurement of the needed devices, disposables, and supplies are essential and should be highlighted in the business plan.
Approval Process
Postapproval Process
Once approved, the champion will need to work closely with various services and managers to oversee infrastructural renovations and execute the hiring plans, establish standard operating procedures (SOPs), standardize staff proficiencies and functional statements, and finalize quality assessment parameters. Home dialysis standards have been addressed by NKDP and The Joint Commission. While PD requires home visits to assess the appropriateness of the environment, the PD program is accredited under hospital-based therapy. Standards and performance metrics should be incorporated into all the VA PD programs for standardization and assessment. Based on guidance from the VHA Handbook, quality metrics, such as dialysis adequacy, and rates of infection should be monitored and reviewed. The dialysis director may need to consider more frequent program evaluations in the first year to ensure appropriate troubleshooting. The VA infrastructure has developed the resources for a central repository for the PD SOPs and quality metrics, which can be obtained and adapted for the local program. Similarly, veteran satisfaction can be assessed through existing resources. Finally, the dialysis director can join the National VHA Dialysis Director listserv for regular updates on the existing and new VHA policies and NKDP updates.
Conclusions
Establishing a new PD program within a local federal infrastructure can appear daunting, both in terms of planning as well as approvals. However, the provision of home-based dialysis therapies may be beneficial to those in rural settings with limited access to in-center dialysis modalities as well as to those who seek autonomy and lifestyle independence in their medical care. Collaborations with the VHA NKDP or PD workgroup can help overcome many of the procedural hurdles, provide guidance about infrastructure and resource allocation and utilization, and provide easy access to established SOPs and quality parameters.
Acknowledgments
We acknowledge the late Dr. Catherine Do for her significant contribution to this manuscript. We also extend our sincere thanks to Dr. Holly Mattix-Kramer (Edward Hines Jr. Veterans Affairs Hospital and Loyola University Medical Center) for her prompt and valuable feedback on this manuscript.
Compared with hemodialysis (HD), peritoneal dialysis (PD) offers comparable survival and superior patient-centered and health services outcomes.1,2 This has prompted repeated calls over the past 2 decades for policies to increase the use of home dialysis and, more specifically, for PD in the United States.3,4
Veterans comprise nearly 10% of the population with end-stage kidney disease (ESKD) burden; > 50,000 US veterans are currently on dialysis.5,6 A majority of these veterans receive their chronic kidney disease (CKD) care through their affiliated US Department of Veterans Affairs (VA) medical centers (VAMCs).
To address these needs, the VHA National Kidney Disease Program (NKDP) formed a 4-member PD workgroup in 2019. Considering the breadth of challenges involved, the PD workgroup broadly designed its approach based on the I CARE (Integrity, Commitment, Advocacy, Respect, and Excellence) VA Core Values.
This review focuses on the initial deliberations of the PD access subgroup and provides a guide to establishing a new local VA PD program.
Step 1: Prerequisites
A functional nephrology service is a bedrock prerequisite for establishing a new PD program. A clinician champion capable of leading the effort is equally necessary. Occasionally, the prevalent ESKD economic and health care burden prompts local VAMC leadership to consider a new PD program to improve the quality or availability of services. More commonly, though, the nephrology section and the clinician champion are the first to recognize the need. In either scenario, the champion will require support and advocacy at multiple levels of local leadership, ie, the section or department chief, facility chief of staff, VAMC director, and the Veterans Integrated Service Network (VISN) director. The foremost task for the champion is to assess local clinical and infrastructure needs.
Goal Alignment
Any new VA nephrology program needs to be evaluated for its overall congruence with the local and national VA missions to improve the accessibility, integration, quality, and innovation of care for veterans. The following considerations are likely to apply to many VA systems.
Accessibility. A VHA directive recommends that all veterans be provided with the opportunity to choose and use any form of dialysis, especially home dialysis.9 Transitioning a veteran seamlessly from advanced CKD to PD requires the execution of multiple sequential processes in the pre-ESKD period, beginning with early identification of advanced CKD, timely referral to nephrology, education for shared dialysis decision making, coordination of care, and PD training and therapy.10 Splitting this sequence between VA and community-based care creates obstacles, including multiple approvals through VA Community Care Services that may substantially increase wait time and effort. This onerous process may be a significant deterrent against pursuing PD and increases the odds of emergency or inpatient initiation. Furthermore, the lack of PD availability limits the knowledge and experience among staff designated to assist veterans, which may result in inappropriate advocacy for HD or delay the transition to PD. Together, these processes can increase morbidity and health care use, and significantly delay or eliminate PD. Finally, many veterans reside in rural or remote areas where the expertise and the availability of PD may be unreliable. Establishing PD services within the local VAMC can improve access to PD, reduce the lead time needed to coordinate the transition to ESKD, and assist individual veterans in making an informed choice about dialysis. The program champion will need to identify and highlight all accessibility barriers within their business plan.
Integration. Many veterans receiving dialysis care at community-based facilities continue to receive nonnephrology care in the VA. This creates a parallel health care system with concerns for duplication of efforts and processes, suboptimal quality of care, and increased risk of medical errors. Establishing VA PD services increases access and integration of nephrology with other VA care.
Excellence. Studies of many chronic diseases have shown superior patient satisfaction and equal or superior quality of care delivered by the VA compared with that of non-VA facilities.11-14 Similarly, mortality rates for veterans receiving CKD and ESKD care in VA are lower compared with those at non-VA facilities.15-17 While these outcomes have not been examined for PD, integration of PD with VA care may lead to an improved overall quality of care and greater loyalty to the VA.
Innovation. Due to its integrated health care infrastructure, the VA is uniquely positioned to implement patient-centered and evidence-based pre-ESKD interventions that may improve outcomes. Prior studies have shown that pre-ESKD kidney disease education (KDE) improves pre- and post-ESKD outcomes, reduces health care costs, and leads to higher selection and use of home dialysis therapies.18-20 The VA recommends that all veterans with advanced CKD be provided access to pre-ESKD care and KDE. Unfortunately, KDE is uncommon among non-VA clinicians. A recent USRDS analysis reported that < 1% of patients with ESKD received pre-ESKD KDE.21 The ongoing Evaluate and Assess the effects of Comprehensive Pre-ESKD kidney disease Education on home dialysis in Veterans Trial (NCT04064086) should provide further evidence.
Step 2: Feasibility
A business plan requires the realistic projections of the costs and accounting for gains of the new clinical program. While there is limited guidance on personnel requirements when planning a PD program, we provide estimated resources needed to successfully establish and run a PD program (eAppendix 1, available online at doi:10.12788/fp.0356).
Clinical Considerations
Secondary or tertiary care VAMCs with multiple medical and surgical specialties routinely provide complex inpatient care. For these facilities, the lack of inpatient PD poses an obstacle to the provision of specialized nonnephrology care to veterans with ESKD, who are frequent users of such complex care. These considerations argue for the need for at least inpatient PD services at VAMCs that provide complex medical care for many veterans receiving PD in the community.
Deliberations for outpatient PD programs should be based on the clinical demands of ESKD care, the number of veterans likely to use PD, and growth projections. While there is no established minimum number that guarantees cost-effectiveness, most existing VA outpatient PD programs provide services for about 5 to 25 veterans. A local census can provide estimations of future PD needs. Travel considerations (ie, distance, terrain, traffic) may affect eligibility for purchased care and the decision where to receive PD. Many veterans may prefer PD from the local VAMC if it is convenient and allows them to maintain centralized VA care. Potential patients can be surveyed to gauge interest in receiving VA-based PD. Facilities providing structured pre-ESKD KDE may hold greater potential for PD growth, and it is important to highlight KDE infrastructure in the business plan.
Infrastructure
Spatial needs including clinic space and storage space for consumables, supplies, and equipment should be part of infrastructure requirements. The program champion may need to examine the available space for suitability and adequacy of the PD program early in the process. Ventilation renovations in the PD rooms should be incorporated into budget calculations. Water access for handwashing and PD effluent drainage should be confirmed, and if the program intends to establish home HD, additional considerations for the storage and water supply may be required. The VHA Handbook outlines the infrastructure requirements for a dialysis program.22 The VA has established national vendor contracts for dialysis equipment and consumables. However, a new PD program may need further guidance regarding the local agencies that provide administrative support and assist patients.
Telehealth technology has enabled many VAMCs to overcome geographical barriers for rural veterans.23 Ongoing expansion of community-based outpatient clinics (CBOCs) to include more rural locations is improving access to specialty care, while the launch of VA Video Connect (VVC) has further improved outreach. Investigators from Minneapolis have demonstrated the feasibility of multidisciplinary home-based telehealth management of veterans with CKD.24 Several existing nephrology sections across the VHA use a combination of VVC and CBOC-facilitated clinic visits to provide some pre-ESKD and ESKD care, including KDE, PD home visits and training, and comprehensive ESKD care visits. Recent changes in the clinical care pattern during the COVID-19 pandemic have further eased ESKD telehealth protocols. Integrating the projected use of telehealth in collaboration with existing resources available through the VHA NKDP can allow the local champion to improve the financial feasibility and long-term success of a new PD program.
Clinicians
Experience and expertise in managing PD vary among nephrologists. A recent survey found that only 11% of second-year nephrology trainees felt fully prepared to manage PD patients and 27% felt that they were minimally prepared.25 Thus, it is important to ensure that adequately trained nephrologists are available locally before initiating a new program, and if needed, coverage across VHS or VISN can be explored. One potential method to enhance practitioner comfort in PD is the use of existing peer-to-peer education through the VA Kidney Specialty Care Access Network-Extension for Community Health care Outcomes program that links health care professionals in rural areas with specialists at a tertiary care center.23 Nurses are a primary pillar for the success of home dialysis programs and the lack of a trained nursing workforce can be a significant limitation. Similarly, while the placement and management of complications related to PD catheters are not technically challenging, the availability of interventionists (either a surgeon or trained interventional radiologist) should be part of the business plan.
Financial Considerations
The financial considerations involving a new PD program within the VHA are complex (eAppendix 2, available online at doi:10.12788/fp.0356). ESKD is one of the most complex and costly comorbidities. It is a major determinant of the expenditure and revenue generation for facilities. The Veterans Equitable Resource Allocation system classifies ESKD on repeated dialysis as price category 10, indicating high complexity and cost. The VAMC workload and facility budget allocation is assessed annually and increases as the population of price group 10 veterans increases. VHA also provides additional Veterans Equitable Resource Allocation funds to VAMCs, which can improve the bottom line for VA-based dialysis units. Providing PD facilitates outpatient and inpatient management of comorbidities, allowing for substantial cost savings while improving the quality of nonrenal care. Outsourcing dialysis care can reduce the administrative burden, although, it deprives the VAMC of all dialysis-associated revenues while bearing the cost of all nonrenal and some renal care. The net effect is reduced facility productivity. In aggregate, establishing a local dialysis program requires greater financial resources for the capital and personnel costs; however, if captured appropriately these funds can be a major source of revenue and savings for the local VAMC.
Indirect costs are important for financial projections. Most community dialysis units operate as outpatient units, whereas all but a handful of the VA dialysis units operate within or near a VAMC. As a result, the VA units providing maintenance dialysis are regularly classified as inpatient centers while providing largely outpatient services, which negatively impacts overhead cost calculations. The predominant use of in-center HD as the default modality further sets an erroneously high baseline for the indirect cost of the VA-based PD services, especially considering that the principal savings of the home dialysis are through the reduction in the labor and capital costs. A rudimentary make-buy model for the in-center HD is available through the NKDP, and establishing a similar model for PD programs may be useful.
Cost considerations also may vary based on the model of ESKD care used locally. Of the 71 hospital-based and free-standing VA HD facilities, only 33 provide PD services, with 5 units providing only inpatient PD. The financial burden of establishing a fully operational outpatient PD program will be based on whether it is targeting a new unit or is expanding. The costs for equipment rental, disposables, and supplies vary based on the VA contract negotiations but are standardized across the nation with approved cost-of-living geographic adjustments. Caution needs to be exercised in employing a phased-hiring approach, as newer programs may require proportionally larger nursing resources due to greater needs for KDE, transitioning services, and training for PD. A target census-based hiring schedule should be negotiated with leadership before launch. If existing labor mapping does not allow for cross-coverage, part-time positions for physicians may be considered. Travel nurses, especially for PD training, can be considered to meet labor needs when long-term projections prohibit permanent full-time hires.
Finally, the balance sheet of a new program needs to account for different scenarios. In addition to nephrology costs, outsourcing veterans for PD services incurs multiple costs (eg, administrative, social work). Facilities with inpatient PD services alone are likely already bearing a component of the medications (including antibiotics) and/or surgical costs for their outsourced patients. These hidden costs are infrequently counted in projections. Facilities without inpatient PD cannot provide complex nonrenal care to ESKD patients on PD, even when the center is well equipped to provide it. These facilities also bear the cost of outsourcing even for complications related to PD. While a full estimation of these services varies, the hidden cost savings of many procedures or inpatient admissions, such as cardiovascular or musculoskeletal surgeries, can exceed those of dialysis in this complex population.
Step 3: proposal
There are no standardized formats for presenting a VHA business proposal; however, this outline provides a template. The business proposal should be designed to effectively communicate the collective data that describe the needs and requirements of a PD program to the local, regional, and national leadership. Not every rationale presented here will apply to an individual proposal and the local champion will need to tailor their rationale for their locale. A sample business plan is shown in eAppendix 3 (available online at doi:10.12788/fp.0356). VHA Handbook of dialysis requires that a PD nurse has a minimum of 12 months of nursing experience with at least 3 months of PD experience.25 Nursing training, education, and support should be discussed with nursing leadership and included in the business plan. Similarly, arrangements for laboratory, pharmacy, and prosthetics services and/or logistics to facilitate procurement of the needed devices, disposables, and supplies are essential and should be highlighted in the business plan.
Approval Process
Postapproval Process
Once approved, the champion will need to work closely with various services and managers to oversee infrastructural renovations and execute the hiring plans, establish standard operating procedures (SOPs), standardize staff proficiencies and functional statements, and finalize quality assessment parameters. Home dialysis standards have been addressed by NKDP and The Joint Commission. While PD requires home visits to assess the appropriateness of the environment, the PD program is accredited under hospital-based therapy. Standards and performance metrics should be incorporated into all the VA PD programs for standardization and assessment. Based on guidance from the VHA Handbook, quality metrics, such as dialysis adequacy, and rates of infection should be monitored and reviewed. The dialysis director may need to consider more frequent program evaluations in the first year to ensure appropriate troubleshooting. The VA infrastructure has developed the resources for a central repository for the PD SOPs and quality metrics, which can be obtained and adapted for the local program. Similarly, veteran satisfaction can be assessed through existing resources. Finally, the dialysis director can join the National VHA Dialysis Director listserv for regular updates on the existing and new VHA policies and NKDP updates.
Conclusions
Establishing a new PD program within a local federal infrastructure can appear daunting, both in terms of planning as well as approvals. However, the provision of home-based dialysis therapies may be beneficial to those in rural settings with limited access to in-center dialysis modalities as well as to those who seek autonomy and lifestyle independence in their medical care. Collaborations with the VHA NKDP or PD workgroup can help overcome many of the procedural hurdles, provide guidance about infrastructure and resource allocation and utilization, and provide easy access to established SOPs and quality parameters.
Acknowledgments
We acknowledge the late Dr. Catherine Do for her significant contribution to this manuscript. We also extend our sincere thanks to Dr. Holly Mattix-Kramer (Edward Hines Jr. Veterans Affairs Hospital and Loyola University Medical Center) for her prompt and valuable feedback on this manuscript.
1. Jung HY, Jeon Y, Park Y, et al. Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci Rep. 2019;9(1):10266. Published 2019 Jul 16. doi:10.1038/s41598-019-46744-1
2. Wong B, Ravani P, Oliver MJ, et al. Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71(3):344-351. doi:10.1053/j.ajkd.2017.08.028
3. Chan CT, Collins K, Ditschman EP, et al. Overcoming barriers for uptake and continued use of home dialysis: an NKF-KDOQI Conference report. Am J Kidney Dis. 2020;75(6):926-934. doi:10.1053/j.ajkd.2019.11.007
4. Executive Order 13879: Advancing American kidney health. Fed Regist. 2019; 84(135):33817-33819. https://www.govinfo.gov/content/pkg/FR-2019-07-15/pdf/2019-15159.pdf
5. Patel TG, Pogach LM, Barth RH. CKD screening and management in the Veterans Health Administration: the impact of system organization and an innovative electronic record. Am J Kidney Dis. 2009;53(suppl 3):S78-S85. doi:10.1053/j.ajkd.2008.07.051
6. Saran R, Pearson A, Tilea A, et al. Burden and cost of caring for US veterans with CKD: initial findings from the VA Renal Information System (VA-REINS). Am J Kidney Dis. 2021;77(3):397-405. doi:10.1053/j.ajkd.2020.07.013
7. Sloan CE, Coffman CJ, Sanders LL, et al. Trends in peritoneal dialysis use in the United States after Medicare payment reform. Clin J Am Soc Nephrol. 2019;14(12):1763-1772. doi:10.2215/CJN.05910519
8. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. HR 5674. 115th Congress; Report No. 115-671, Part 1. May 3, 2018. Accessed February 9, 2023. https://www.congress.gov/115/bills/hr5674/BILLS-115hr5674rh.pdf
9. US Department of Veterans Affairs, Veterans Health Administration. Chronic kidney disease prevention, early recognition, and management. VHA Directive 1053. March 17, 2020. Accessed February 9, 2023. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8737
10. Blake PG, Quinn RR, Oliver MJ. Peritoneal dialysis and the process of modality selection. Perit Dial Int. 2013;33(3):233-241. doi:10.3747/pdi.2012.00119
11. Stroupe KT, Hynes DM, Giobbie-Hurder A, et al. Patient satisfaction and use of Veterans Affairs versus non-Veterans Affairs healthcare services by veterans. Med Care. 2005;43(5):453-460. doi:10.1097/01.mlr.0000160377.82164.d3
12. Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing quality of care in Veterans Affairs and non-Veterans Affairs settings. J Gen Intern Med. 2018;33(10):1631-1638. doi:10.1007/s11606-018-4433-7
13. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885. doi:10.1001/jamainternmed.2017.0605
14. Nuti SV, Qin L, Krumholz HM. Outcome after admission at Veterans Affairs vs non-Veterans Affairs hospitals--reply. JAMA. 2016;316(3):346. doi:10.1001/jama.2016.5394
15. Streja E, Kovesdy CP, Soohoo M, et al. Dialysis provider and outcomes among United States veterans who transition to dialysis. Clin J Am Soc Nephrol. 2018;13(7):1055-1062. doi:10.2215/CJN.12951117
16. Wang V, Coffman CJ, Stechuchak KM, et al. Survival among veterans obtaining dialysis in VA and non-VA settings. J Am Soc Nephrol. 2019;30(1):159-168. doi:10.1681/ASN.2018050521
17. Kurella Tamura M, Thomas IC, Montez-Rath ME, et al. Dialysis initiation and mortality among older veterans with kidney failure treated in Medicare vs the Department of Veterans Affairs. JAMA Intern Med. 2018;178(5):657-664. doi:10.1001/jamainternmed.2018.0411
18. Devins GM, Mendelssohn DC, Barré PE, Taub K, Binik YM. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46(6):1088-1098. doi:10.1053/j.ajkd.2005.08.017
19. Devoe DJ, Wong B, James MT, et al. Patient education and peritoneal dialysis modality selection: a systematic review and meta-analysis. Am J Kidney Dis. 2016;68(3):422-433. doi:10.1053/j.ajkd.2016.02.053
20. Lin E, Chertow GM, Yan B, Malcolm E, Goldhaber-Fiebert JD. Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study. PLoS Med. 2018;15(3):e1002532. Published 2018 Mar 27. doi:10.1371/journal.pmed.1002532
21. Shukla AM, Bozorgmehri S, Ruchi R, et al. Utilization of CMS pre-ESRD Kidney Disease Education services and its associations with the home dialysis therapies. Perit Dial Int. 2021;41(5):453-462. doi:10.1177/0896860820975586
22. US Dept of Veterans Affairs, Veterans Health Administration. Criteria and standards for VA dialysis programs. VHA Directive 1601. 2016. May 23, 2016. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3205
23. Crowley ST, Belcher J, Choudhury D, et al. Targeting access to kidney care via telehealth: the VA experience. Adv Chronic Kidney Dis. 2017;24(1):22-30. doi:10.1053/j.ackd.2016.11.005
24. Ishani A, Christopher J, Palmer D, et al. Telehealth by an interprofessional team in patients with CKD: a randomized controlled trial. Am J Kidney Dis. 2016;68(1):41-49. doi:10.1053/j.ajkd.2016.01.018
25. Gupta N, Taber-Hight EB, Miller BW. Perceptions of home dialysis training and experience among US nephrology fellows. Am J Kidney Dis. 2021;77(5):713-718.e1. doi:10.1053/j.ajkd.2020.09.014
1. Jung HY, Jeon Y, Park Y, et al. Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci Rep. 2019;9(1):10266. Published 2019 Jul 16. doi:10.1038/s41598-019-46744-1
2. Wong B, Ravani P, Oliver MJ, et al. Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71(3):344-351. doi:10.1053/j.ajkd.2017.08.028
3. Chan CT, Collins K, Ditschman EP, et al. Overcoming barriers for uptake and continued use of home dialysis: an NKF-KDOQI Conference report. Am J Kidney Dis. 2020;75(6):926-934. doi:10.1053/j.ajkd.2019.11.007
4. Executive Order 13879: Advancing American kidney health. Fed Regist. 2019; 84(135):33817-33819. https://www.govinfo.gov/content/pkg/FR-2019-07-15/pdf/2019-15159.pdf
5. Patel TG, Pogach LM, Barth RH. CKD screening and management in the Veterans Health Administration: the impact of system organization and an innovative electronic record. Am J Kidney Dis. 2009;53(suppl 3):S78-S85. doi:10.1053/j.ajkd.2008.07.051
6. Saran R, Pearson A, Tilea A, et al. Burden and cost of caring for US veterans with CKD: initial findings from the VA Renal Information System (VA-REINS). Am J Kidney Dis. 2021;77(3):397-405. doi:10.1053/j.ajkd.2020.07.013
7. Sloan CE, Coffman CJ, Sanders LL, et al. Trends in peritoneal dialysis use in the United States after Medicare payment reform. Clin J Am Soc Nephrol. 2019;14(12):1763-1772. doi:10.2215/CJN.05910519
8. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. HR 5674. 115th Congress; Report No. 115-671, Part 1. May 3, 2018. Accessed February 9, 2023. https://www.congress.gov/115/bills/hr5674/BILLS-115hr5674rh.pdf
9. US Department of Veterans Affairs, Veterans Health Administration. Chronic kidney disease prevention, early recognition, and management. VHA Directive 1053. March 17, 2020. Accessed February 9, 2023. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8737
10. Blake PG, Quinn RR, Oliver MJ. Peritoneal dialysis and the process of modality selection. Perit Dial Int. 2013;33(3):233-241. doi:10.3747/pdi.2012.00119
11. Stroupe KT, Hynes DM, Giobbie-Hurder A, et al. Patient satisfaction and use of Veterans Affairs versus non-Veterans Affairs healthcare services by veterans. Med Care. 2005;43(5):453-460. doi:10.1097/01.mlr.0000160377.82164.d3
12. Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing quality of care in Veterans Affairs and non-Veterans Affairs settings. J Gen Intern Med. 2018;33(10):1631-1638. doi:10.1007/s11606-018-4433-7
13. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885. doi:10.1001/jamainternmed.2017.0605
14. Nuti SV, Qin L, Krumholz HM. Outcome after admission at Veterans Affairs vs non-Veterans Affairs hospitals--reply. JAMA. 2016;316(3):346. doi:10.1001/jama.2016.5394
15. Streja E, Kovesdy CP, Soohoo M, et al. Dialysis provider and outcomes among United States veterans who transition to dialysis. Clin J Am Soc Nephrol. 2018;13(7):1055-1062. doi:10.2215/CJN.12951117
16. Wang V, Coffman CJ, Stechuchak KM, et al. Survival among veterans obtaining dialysis in VA and non-VA settings. J Am Soc Nephrol. 2019;30(1):159-168. doi:10.1681/ASN.2018050521
17. Kurella Tamura M, Thomas IC, Montez-Rath ME, et al. Dialysis initiation and mortality among older veterans with kidney failure treated in Medicare vs the Department of Veterans Affairs. JAMA Intern Med. 2018;178(5):657-664. doi:10.1001/jamainternmed.2018.0411
18. Devins GM, Mendelssohn DC, Barré PE, Taub K, Binik YM. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46(6):1088-1098. doi:10.1053/j.ajkd.2005.08.017
19. Devoe DJ, Wong B, James MT, et al. Patient education and peritoneal dialysis modality selection: a systematic review and meta-analysis. Am J Kidney Dis. 2016;68(3):422-433. doi:10.1053/j.ajkd.2016.02.053
20. Lin E, Chertow GM, Yan B, Malcolm E, Goldhaber-Fiebert JD. Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study. PLoS Med. 2018;15(3):e1002532. Published 2018 Mar 27. doi:10.1371/journal.pmed.1002532
21. Shukla AM, Bozorgmehri S, Ruchi R, et al. Utilization of CMS pre-ESRD Kidney Disease Education services and its associations with the home dialysis therapies. Perit Dial Int. 2021;41(5):453-462. doi:10.1177/0896860820975586
22. US Dept of Veterans Affairs, Veterans Health Administration. Criteria and standards for VA dialysis programs. VHA Directive 1601. 2016. May 23, 2016. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3205
23. Crowley ST, Belcher J, Choudhury D, et al. Targeting access to kidney care via telehealth: the VA experience. Adv Chronic Kidney Dis. 2017;24(1):22-30. doi:10.1053/j.ackd.2016.11.005
24. Ishani A, Christopher J, Palmer D, et al. Telehealth by an interprofessional team in patients with CKD: a randomized controlled trial. Am J Kidney Dis. 2016;68(1):41-49. doi:10.1053/j.ajkd.2016.01.018
25. Gupta N, Taber-Hight EB, Miller BW. Perceptions of home dialysis training and experience among US nephrology fellows. Am J Kidney Dis. 2021;77(5):713-718.e1. doi:10.1053/j.ajkd.2020.09.014