User login
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
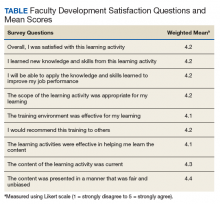
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.