User login
according to recent research published in Clinical Gastroenterology and Hepatology.
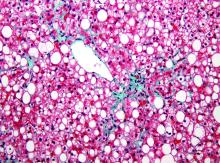
Researchers evaluated 40,700 Korean adults (minimum age, 18 years) with NAFLD who underwent health screenings during 2002-2016 with a median 6-year follow-up. Patients were categorized and placed into weight quintiles based on whether they lost weight (quintile 1, 2.3-kg or greater weight loss; quintile 2, 2.2-kg to 0.6-kg weight loss), gained weight (quintile 4, 0.7- to 2.1-kg weight gain; quintile 5, at least 2.2-kg or greater weight gain) or whether their weight remained stable (quintile 3, 0.5-kg weight loss to 0.6-kg weight gain). Researchers followed patients from baseline to fibrosis progression or last visit, calculated as person-years, and used the aspartate aminotransferase to platelet ratio index (APRI) to measure outcomes. They defined body mass index based on criteria specific to Asian populations, with underweight categorized as less than 18.5 kg/m2, normal weight as 18.5-23 kg/m2, overweight as 23-25 kg/m2, and obese as at least 25 kg/m2.
“Our findings from mostly asymptomatic, relatively young individuals with ultrasonographically detected steatosis, possibly reflecting low-risk NAFLD patients, are less likely to be affected by survivor bias and biases related to comorbidities, compared with previous findings from cohorts of high-risk groups that underwent liver biopsy,” Seungho Ryu, MD, PhD, from Kangbuk Samsung Hospital in Seoul, South Korea, and colleagues wrote in the study.
There were 5,454 participants who progressed from a low APRI to an intermediate or high APRI within 275,451.5 person-years, researchers said. Compared with the stable-weight group, hazard ratios for APRI progression in the first weight-change quintile were 0.68 (95% confidence interval, 0.62-0.74) and 0.86 in the second weight-change quintile (95% CI, 0.78-0.94). In the weight-gain groups, an increase in weight was associated with APRI progression in the fourth quintile (HR, 1.17; 95% CI, 1.07-1.28) and fifth quintile (HR, 1.71; 95% CI, 1.58-1.85) groups.
After multivariable adjustment, there was an increase in APRI progression among patients with BMIs between 23 and 24.9 kg/m2 (HR, 1.13; 95% CI, 1.02-1.26), between 25 and 29.9 kg/m2 (HR, 1.41; 95% CI, 1.28-1.55), and greater than or equal to 30 kg/m2 (HR, 2.09; 95% CI, 1.86-2.36) compared with patients with a BMI between 18.5 and 22.9 kg/m2,.
Limitations of the study included the use of ultrasonography in place of liver biopsy for diagnosing NAFLD and the use of APRI to predict fibrosis in individuals with NAFLD, researchers said.
“APRI has demonstrated a reasonable utility as a noninvasive method for the prediction of histologically confirmed advanced fibrosis,” Dr. Ryu and colleagues wrote. “Nonetheless, we acknowledge that there is no currently available longitudinal data to support the use of worsening noninvasive fibrosis markers as an indicator of histological progression of fibrosis stage over time.”
Other limitations included the study’s retrospective design, lack of availability of medication use and dietary intake, and lack of generalization based on a young, healthy population of mostly Korean employees who were employed by companies or local government. However, researchers said clinicians should encourage their patients with NAFLD to maintain a healthy weight to avoid progression of fibrosis.
The authors reported no relevant financial disclosures.
SOURCE: Kim Y et al. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.07.006.
according to recent research published in Clinical Gastroenterology and Hepatology.
Researchers evaluated 40,700 Korean adults (minimum age, 18 years) with NAFLD who underwent health screenings during 2002-2016 with a median 6-year follow-up. Patients were categorized and placed into weight quintiles based on whether they lost weight (quintile 1, 2.3-kg or greater weight loss; quintile 2, 2.2-kg to 0.6-kg weight loss), gained weight (quintile 4, 0.7- to 2.1-kg weight gain; quintile 5, at least 2.2-kg or greater weight gain) or whether their weight remained stable (quintile 3, 0.5-kg weight loss to 0.6-kg weight gain). Researchers followed patients from baseline to fibrosis progression or last visit, calculated as person-years, and used the aspartate aminotransferase to platelet ratio index (APRI) to measure outcomes. They defined body mass index based on criteria specific to Asian populations, with underweight categorized as less than 18.5 kg/m2, normal weight as 18.5-23 kg/m2, overweight as 23-25 kg/m2, and obese as at least 25 kg/m2.
“Our findings from mostly asymptomatic, relatively young individuals with ultrasonographically detected steatosis, possibly reflecting low-risk NAFLD patients, are less likely to be affected by survivor bias and biases related to comorbidities, compared with previous findings from cohorts of high-risk groups that underwent liver biopsy,” Seungho Ryu, MD, PhD, from Kangbuk Samsung Hospital in Seoul, South Korea, and colleagues wrote in the study.
There were 5,454 participants who progressed from a low APRI to an intermediate or high APRI within 275,451.5 person-years, researchers said. Compared with the stable-weight group, hazard ratios for APRI progression in the first weight-change quintile were 0.68 (95% confidence interval, 0.62-0.74) and 0.86 in the second weight-change quintile (95% CI, 0.78-0.94). In the weight-gain groups, an increase in weight was associated with APRI progression in the fourth quintile (HR, 1.17; 95% CI, 1.07-1.28) and fifth quintile (HR, 1.71; 95% CI, 1.58-1.85) groups.
After multivariable adjustment, there was an increase in APRI progression among patients with BMIs between 23 and 24.9 kg/m2 (HR, 1.13; 95% CI, 1.02-1.26), between 25 and 29.9 kg/m2 (HR, 1.41; 95% CI, 1.28-1.55), and greater than or equal to 30 kg/m2 (HR, 2.09; 95% CI, 1.86-2.36) compared with patients with a BMI between 18.5 and 22.9 kg/m2,.
Limitations of the study included the use of ultrasonography in place of liver biopsy for diagnosing NAFLD and the use of APRI to predict fibrosis in individuals with NAFLD, researchers said.
“APRI has demonstrated a reasonable utility as a noninvasive method for the prediction of histologically confirmed advanced fibrosis,” Dr. Ryu and colleagues wrote. “Nonetheless, we acknowledge that there is no currently available longitudinal data to support the use of worsening noninvasive fibrosis markers as an indicator of histological progression of fibrosis stage over time.”
Other limitations included the study’s retrospective design, lack of availability of medication use and dietary intake, and lack of generalization based on a young, healthy population of mostly Korean employees who were employed by companies or local government. However, researchers said clinicians should encourage their patients with NAFLD to maintain a healthy weight to avoid progression of fibrosis.
The authors reported no relevant financial disclosures.
SOURCE: Kim Y et al. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.07.006.
according to recent research published in Clinical Gastroenterology and Hepatology.
Researchers evaluated 40,700 Korean adults (minimum age, 18 years) with NAFLD who underwent health screenings during 2002-2016 with a median 6-year follow-up. Patients were categorized and placed into weight quintiles based on whether they lost weight (quintile 1, 2.3-kg or greater weight loss; quintile 2, 2.2-kg to 0.6-kg weight loss), gained weight (quintile 4, 0.7- to 2.1-kg weight gain; quintile 5, at least 2.2-kg or greater weight gain) or whether their weight remained stable (quintile 3, 0.5-kg weight loss to 0.6-kg weight gain). Researchers followed patients from baseline to fibrosis progression or last visit, calculated as person-years, and used the aspartate aminotransferase to platelet ratio index (APRI) to measure outcomes. They defined body mass index based on criteria specific to Asian populations, with underweight categorized as less than 18.5 kg/m2, normal weight as 18.5-23 kg/m2, overweight as 23-25 kg/m2, and obese as at least 25 kg/m2.
“Our findings from mostly asymptomatic, relatively young individuals with ultrasonographically detected steatosis, possibly reflecting low-risk NAFLD patients, are less likely to be affected by survivor bias and biases related to comorbidities, compared with previous findings from cohorts of high-risk groups that underwent liver biopsy,” Seungho Ryu, MD, PhD, from Kangbuk Samsung Hospital in Seoul, South Korea, and colleagues wrote in the study.
There were 5,454 participants who progressed from a low APRI to an intermediate or high APRI within 275,451.5 person-years, researchers said. Compared with the stable-weight group, hazard ratios for APRI progression in the first weight-change quintile were 0.68 (95% confidence interval, 0.62-0.74) and 0.86 in the second weight-change quintile (95% CI, 0.78-0.94). In the weight-gain groups, an increase in weight was associated with APRI progression in the fourth quintile (HR, 1.17; 95% CI, 1.07-1.28) and fifth quintile (HR, 1.71; 95% CI, 1.58-1.85) groups.
After multivariable adjustment, there was an increase in APRI progression among patients with BMIs between 23 and 24.9 kg/m2 (HR, 1.13; 95% CI, 1.02-1.26), between 25 and 29.9 kg/m2 (HR, 1.41; 95% CI, 1.28-1.55), and greater than or equal to 30 kg/m2 (HR, 2.09; 95% CI, 1.86-2.36) compared with patients with a BMI between 18.5 and 22.9 kg/m2,.
Limitations of the study included the use of ultrasonography in place of liver biopsy for diagnosing NAFLD and the use of APRI to predict fibrosis in individuals with NAFLD, researchers said.
“APRI has demonstrated a reasonable utility as a noninvasive method for the prediction of histologically confirmed advanced fibrosis,” Dr. Ryu and colleagues wrote. “Nonetheless, we acknowledge that there is no currently available longitudinal data to support the use of worsening noninvasive fibrosis markers as an indicator of histological progression of fibrosis stage over time.”
Other limitations included the study’s retrospective design, lack of availability of medication use and dietary intake, and lack of generalization based on a young, healthy population of mostly Korean employees who were employed by companies or local government. However, researchers said clinicians should encourage their patients with NAFLD to maintain a healthy weight to avoid progression of fibrosis.
The authors reported no relevant financial disclosures.
SOURCE: Kim Y et al. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.07.006.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Obesity and weight gain were linked to progression of fibrosis in adults with NAFLD.
Major finding: Degree of weight change was associated with risk of fibrosis progression; patients who gained weight in quintile 4 and quintile 5 had hazard ratios of 1.17 and 1.71, respectively, when compared with the quintile of patients whose weight remained stable.
Data source: A retrospective study of 40,700 Korean adults with NAFLD who underwent health screenings during 2002-2016 with a median 6-year follow-up.
Disclosures: The authors reported no relevant financial disclosures.
Source: Kim Y et al. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.07.006.