User login
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
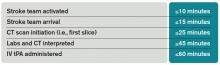
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.