User login
Implementing a critical care TEE program at your institution
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).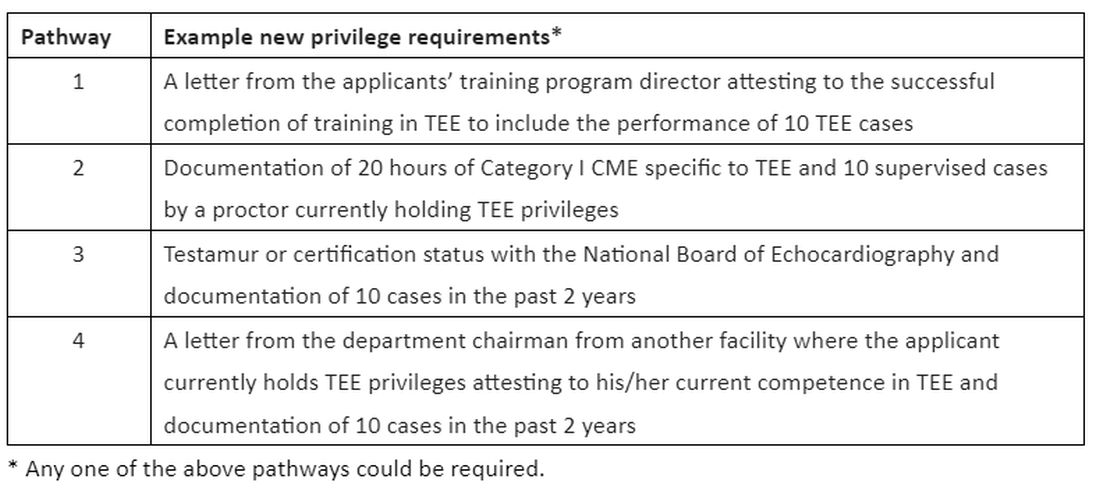
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Starting from the ground up!
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).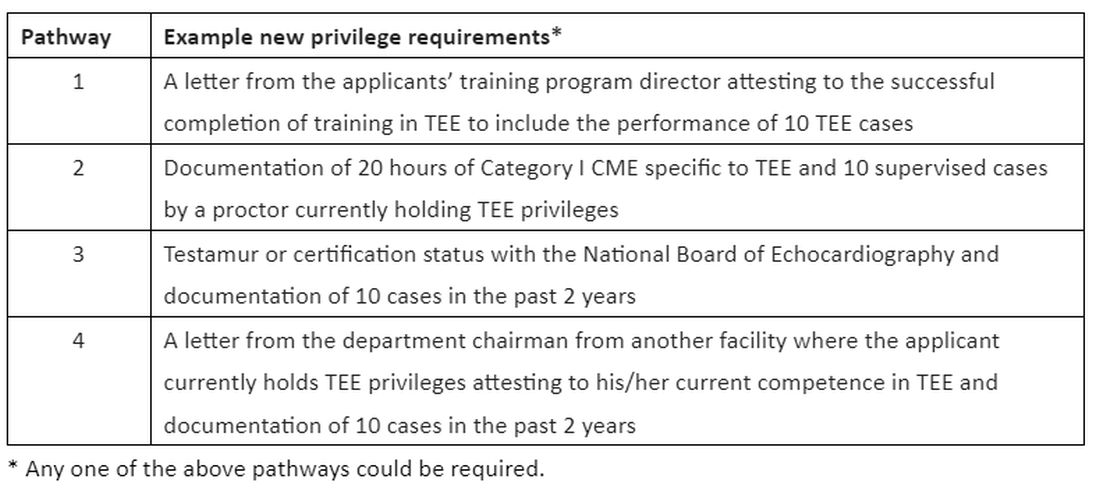
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).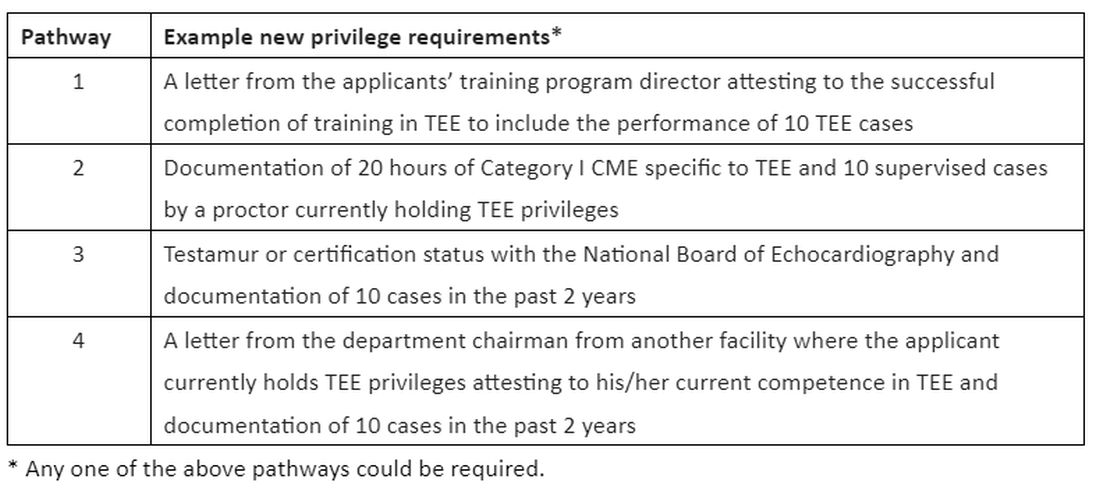
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
What do you recommend for this patient with COPD?
“Janice Turner” (name changed to protect confidentiality) is a 66-year-old woman with a 40-pack per year history of smoking. She is very worried about having another COPD exacerbation and wants to know if there are additional medications she could try.
Over the past 2 weeks, her respiratory symptoms have improved and returned to her baseline. She has a daily cough with white phlegm on most days and dyspnea on exertion at one-half block on level ground. She reports using her medications as prescribed and is enrolled in a pulmonary rehabilitation program, which she attends twice per week. She uses 2 to 4 inhalations of albuterol each day.
She is on the following regimen for her COPD, which is unchanged compared with what she has been prescribed for the past 12 months: 1) combination inhaled fluticasone furoate, umeclidinium, and vilanterol via the Ellipta® device, one actuation once daily and 2) inhaled albuterol, two puffs as needed every 4 hours via metered dose inhaler. She demonstrates mastery of inhaler technique for both inhaled devices. Her vaccinations are current (pneumococcus, influenza, respiratory syncytial virus, and COVID-19).
On examination, she can complete sentences without respiratory difficulty, and her vital signs are normal. She has decreased breath sounds in all lung fields, with occasional rhonchi. Heart sounds are distant, but regular, at 92 beats per minute, and she has no peripheral edema. Arterial blood gas at rest on room air indicates a pH of 7.38, PaO2 of 63 mm Hg, and PaCO2 of 42 mm Hg. An electrocardiogram shows sinus rhythm and a QTc interval of 420 milliseconds.
Three months ago, when she was clinically stable, you obtained spirometry, a complete blood count with differential, and a chest radiograph to exclude alternate diagnoses for her ongoing respiratory symptoms. She had severe airflow limitation (post-bronchodilator FEV1 = 40% predicted, FVC = 61% predicted, FEV1/FVC = 65%). At the time, she also had peripheral eosinophilia (eosinophil count of 350 cells/μL) and hyperinflation without parenchymal infiltrates.
In summary, Ms. Turner has severe smoking-associated COPD Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 3E and chronic bronchitis with two severe exacerbations in the past 12 months.1 She is currently prescribed triple inhaled maintenance therapy with corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. She has a normal QTc interval.
So what would you recommend to reduce Ms. Turner’s risk of future exacerbations?
In 2011, the US Food and Drug Administration (FDA) approved roflumilast 500 mcg by mouth per day, a selective phosphodiesterase 4 (PDE4) inhibitor, as maintenance therapy to reduce the risk of COPD exacerbations in patients with severe COPD associated with chronic bronchitis.2 The FDA approval was based on a review of the efficacy and safety of roflumilast in eight randomized, double-blind, controlled clinical trials in 9,394 adults with COPD.
Two subsequently completed randomized clinical trials in 2015 (REACT, 1,945 adults) and 2016 (RE2SPOND, 2,354 adults) also found that maintenance oral treatment escalation with roflumilast significantly reduced the risk of COPD exacerbations compared with placebo.2 The most common adverse effects reported with long-term use of roflumilast are related to the gastrointestinal tract (diarrhea, nausea, decreased appetite), weight loss, and insomnia. Four weeks of roflumilast at 250 mcg per day prior to dose escalation to 500 mcg per day reduces the risk of treatment discontinuation and improves tolerability compared with initiating treatment with the maintenance dose.
In 2022, the FDA approved a generic version of roflumilast, providing an opportunity for patients to use roflumilast at a lower cost than was previously possible. Importantly, the FDA Prescribing Information includes a warning to avoid the use of roflumilast in patients being treated with strong cytochrome P450 enzyme inducers (eg, rifampin, phenytoin). The FDA Prescribing Information also recommends weighing the risks and benefits of roflumilast in patients with a history of depression or suicidal thoughts or behavior, or patients with unexplained or clinically significant weight loss.
In 2011 (the same year as the FDA approval of roflumilast), the National Institutes of Health/National Heart, Lung, and Blood Institute-funded COPD Clinical Research Network reported that maintenance treatment with azithromycin reduced the risk of COPD exacerbations compared with placebo in a randomized clinical trial of 1,142 adults with COPD (MACRO study).3 Subgroup analyses indicated that the reduction in the risk of COPD exacerbations with azithromycin was observed in participants with or without chronic bronchitis but not in participants who currently smoked.
Subsequently, two other smaller randomized clinical trials in 2014 (COLUMBUS, 92 participants) and in 2019 (BACE, 301 participants) also demonstrated a reduction in the risk of COPD exacerbations with maintenance azithromycin treatment compared with placebo. Azithromycin can prolong the QT interval and, in rare cases, cause cardiac arrythmias, especially when used with other medications that can prolong the QT interval. There are also concerns that maintenance azithromycin therapy could lead to decrements in hearing or promote the development of macrolide-resistant bacteria. Maintenance treatment with azithromycin to prevent COPD exacerbations is not an FDA-approved indication.4 The FDA approval for azithromycin is currently limited to treatment of patients with mild to moderate infections caused by susceptible bacteria, but it is often prescribed off-label as maintenance treatment for COPD.
On the basis of this body of evidence from clinical trials in COPD, the 2015 CHEST and Canadian Thoracic Society (CTS) guidelines,5 the 2017 European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines,6 and the 2024 GOLD Strategy Report all include recommendations for treatment escalation with maintenance roflumilast or azithromycin to reduce the risk of COPD exacerbations. For example, the 2024 GOLD Strategy Report recommends roflumilast in patients with severe COPD and chronic bronchitis who continue to have exacerbations despite inhaled maintenance treatment with combination long-acting β2-agonist and long-acting muscarinic antagonist or with triple therapy with inhaled corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. An alternative, 2024 GOLD-recommended strategy in this population is maintenance therapy with azithromycin, “preferentially in former smokers.” GOLD’s preference for using azithromycin in patients with smoking history is based on post-hoc (ie, not part of the original study design) subgroup analyses “suggesting lesser benefit in active smokers” in the MACRO study. Results of such analyses have not been reported in other studies.
There are no results from clinical trials that have directly compared the harms and benefits of initiating maintenance therapy with roflumilast or azithromycin in patients with COPD. The roflumilast or azithromycin to prevent COPD exacerbations (RELIANCE; NCT04069312) multicenter clinical trial is addressing this evidence gap.7 The RELIANCE study is funded by the Patient-Centered Outcomes Research Institute and co-led by the COPD Foundation, a not-for-profit organization founded by John W. Walsh, a patient advocate with α1-related COPD. Also, results of two recently completed phase 3 clinical trials with nebulized ensifentrine (ENHANCE-1 and ENHANCE-2), a novel inhibitor of PDE3 and PDE4, were recently published. ENHANCE-1 and ENHANCE-2 studies indicate that twice daily nebulized ensifentrine reduces the risk of COPD exacerbations in patients with moderate or severe COPD.8 Ensifentrine is under review by the FDA, and a decision about its use in the US is expected in the summer of 2024.
Until the results from the RELIANCE clinical trial and the decision by the FDA about ensifentrine are available, we recommended a discussion with Ms. Turner about whether to initiate treatment with maintenance roflumilast or azithromycin. Both can reduce the risk of exacerbations, and the relative benefits and risks of these two evidence-based options are not yet known. Unless Ms. Turner has specific preferences (eg, concerns about specific adverse effects or differences in out-of-pocket cost) in favor of one over the other, she could flip a coin to decide between initiating maintenance roflumilast or azithromycin.
Dr. Krishnan is Professor of Medicine, Division of Pulmonary, Critical Care, Sleep & Allergy, and Professor of Public Health, Division of Epidemiology and Biostatistics, University of Illinois Chicago. Dr. Adrish is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine, Houston.
References:
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. https://goldcopd.org/2024-gold-report-2/
2. US Food and Drug Administration (Daliresp®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/022522s003lbl.pdf
3. Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromucin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689-98. PMID: 21864166. doi: 10.1056/NEJMoa1104623.
4. US Food and Drug Administration (Zithromyax®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/050710s039,050711s036,050784s023lbl.pdf
5. Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acure exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society guideline. Chest. 2015;147(4)894-942. PMID: 25321320. doi: 10.1378/chest.14-1676.
6. Wedzicha JA, Calverley PMA, Albert RK, et al. Prevention of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;50(3):1602265. PMID: 28889106. doi:10.1183/13993003.02265-2016.
7. Krishnan JA, Albert RK, Rennard SI; RELIANCE study. Waiting for actionable evidence: roflumilast or azithromycin? Chronic Obst Pulm Dis. 2022;9(1):1-3. PMID: 34783231. doi: 10.15326/jcopdf.2021.0272.
8. Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phospodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. PMID: 37364283.
“Janice Turner” (name changed to protect confidentiality) is a 66-year-old woman with a 40-pack per year history of smoking. She is very worried about having another COPD exacerbation and wants to know if there are additional medications she could try.
Over the past 2 weeks, her respiratory symptoms have improved and returned to her baseline. She has a daily cough with white phlegm on most days and dyspnea on exertion at one-half block on level ground. She reports using her medications as prescribed and is enrolled in a pulmonary rehabilitation program, which she attends twice per week. She uses 2 to 4 inhalations of albuterol each day.
She is on the following regimen for her COPD, which is unchanged compared with what she has been prescribed for the past 12 months: 1) combination inhaled fluticasone furoate, umeclidinium, and vilanterol via the Ellipta® device, one actuation once daily and 2) inhaled albuterol, two puffs as needed every 4 hours via metered dose inhaler. She demonstrates mastery of inhaler technique for both inhaled devices. Her vaccinations are current (pneumococcus, influenza, respiratory syncytial virus, and COVID-19).
On examination, she can complete sentences without respiratory difficulty, and her vital signs are normal. She has decreased breath sounds in all lung fields, with occasional rhonchi. Heart sounds are distant, but regular, at 92 beats per minute, and she has no peripheral edema. Arterial blood gas at rest on room air indicates a pH of 7.38, PaO2 of 63 mm Hg, and PaCO2 of 42 mm Hg. An electrocardiogram shows sinus rhythm and a QTc interval of 420 milliseconds.
Three months ago, when she was clinically stable, you obtained spirometry, a complete blood count with differential, and a chest radiograph to exclude alternate diagnoses for her ongoing respiratory symptoms. She had severe airflow limitation (post-bronchodilator FEV1 = 40% predicted, FVC = 61% predicted, FEV1/FVC = 65%). At the time, she also had peripheral eosinophilia (eosinophil count of 350 cells/μL) and hyperinflation without parenchymal infiltrates.
In summary, Ms. Turner has severe smoking-associated COPD Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 3E and chronic bronchitis with two severe exacerbations in the past 12 months.1 She is currently prescribed triple inhaled maintenance therapy with corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. She has a normal QTc interval.
So what would you recommend to reduce Ms. Turner’s risk of future exacerbations?
In 2011, the US Food and Drug Administration (FDA) approved roflumilast 500 mcg by mouth per day, a selective phosphodiesterase 4 (PDE4) inhibitor, as maintenance therapy to reduce the risk of COPD exacerbations in patients with severe COPD associated with chronic bronchitis.2 The FDA approval was based on a review of the efficacy and safety of roflumilast in eight randomized, double-blind, controlled clinical trials in 9,394 adults with COPD.
Two subsequently completed randomized clinical trials in 2015 (REACT, 1,945 adults) and 2016 (RE2SPOND, 2,354 adults) also found that maintenance oral treatment escalation with roflumilast significantly reduced the risk of COPD exacerbations compared with placebo.2 The most common adverse effects reported with long-term use of roflumilast are related to the gastrointestinal tract (diarrhea, nausea, decreased appetite), weight loss, and insomnia. Four weeks of roflumilast at 250 mcg per day prior to dose escalation to 500 mcg per day reduces the risk of treatment discontinuation and improves tolerability compared with initiating treatment with the maintenance dose.
In 2022, the FDA approved a generic version of roflumilast, providing an opportunity for patients to use roflumilast at a lower cost than was previously possible. Importantly, the FDA Prescribing Information includes a warning to avoid the use of roflumilast in patients being treated with strong cytochrome P450 enzyme inducers (eg, rifampin, phenytoin). The FDA Prescribing Information also recommends weighing the risks and benefits of roflumilast in patients with a history of depression or suicidal thoughts or behavior, or patients with unexplained or clinically significant weight loss.
In 2011 (the same year as the FDA approval of roflumilast), the National Institutes of Health/National Heart, Lung, and Blood Institute-funded COPD Clinical Research Network reported that maintenance treatment with azithromycin reduced the risk of COPD exacerbations compared with placebo in a randomized clinical trial of 1,142 adults with COPD (MACRO study).3 Subgroup analyses indicated that the reduction in the risk of COPD exacerbations with azithromycin was observed in participants with or without chronic bronchitis but not in participants who currently smoked.
Subsequently, two other smaller randomized clinical trials in 2014 (COLUMBUS, 92 participants) and in 2019 (BACE, 301 participants) also demonstrated a reduction in the risk of COPD exacerbations with maintenance azithromycin treatment compared with placebo. Azithromycin can prolong the QT interval and, in rare cases, cause cardiac arrythmias, especially when used with other medications that can prolong the QT interval. There are also concerns that maintenance azithromycin therapy could lead to decrements in hearing or promote the development of macrolide-resistant bacteria. Maintenance treatment with azithromycin to prevent COPD exacerbations is not an FDA-approved indication.4 The FDA approval for azithromycin is currently limited to treatment of patients with mild to moderate infections caused by susceptible bacteria, but it is often prescribed off-label as maintenance treatment for COPD.
On the basis of this body of evidence from clinical trials in COPD, the 2015 CHEST and Canadian Thoracic Society (CTS) guidelines,5 the 2017 European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines,6 and the 2024 GOLD Strategy Report all include recommendations for treatment escalation with maintenance roflumilast or azithromycin to reduce the risk of COPD exacerbations. For example, the 2024 GOLD Strategy Report recommends roflumilast in patients with severe COPD and chronic bronchitis who continue to have exacerbations despite inhaled maintenance treatment with combination long-acting β2-agonist and long-acting muscarinic antagonist or with triple therapy with inhaled corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. An alternative, 2024 GOLD-recommended strategy in this population is maintenance therapy with azithromycin, “preferentially in former smokers.” GOLD’s preference for using azithromycin in patients with smoking history is based on post-hoc (ie, not part of the original study design) subgroup analyses “suggesting lesser benefit in active smokers” in the MACRO study. Results of such analyses have not been reported in other studies.
There are no results from clinical trials that have directly compared the harms and benefits of initiating maintenance therapy with roflumilast or azithromycin in patients with COPD. The roflumilast or azithromycin to prevent COPD exacerbations (RELIANCE; NCT04069312) multicenter clinical trial is addressing this evidence gap.7 The RELIANCE study is funded by the Patient-Centered Outcomes Research Institute and co-led by the COPD Foundation, a not-for-profit organization founded by John W. Walsh, a patient advocate with α1-related COPD. Also, results of two recently completed phase 3 clinical trials with nebulized ensifentrine (ENHANCE-1 and ENHANCE-2), a novel inhibitor of PDE3 and PDE4, were recently published. ENHANCE-1 and ENHANCE-2 studies indicate that twice daily nebulized ensifentrine reduces the risk of COPD exacerbations in patients with moderate or severe COPD.8 Ensifentrine is under review by the FDA, and a decision about its use in the US is expected in the summer of 2024.
Until the results from the RELIANCE clinical trial and the decision by the FDA about ensifentrine are available, we recommended a discussion with Ms. Turner about whether to initiate treatment with maintenance roflumilast or azithromycin. Both can reduce the risk of exacerbations, and the relative benefits and risks of these two evidence-based options are not yet known. Unless Ms. Turner has specific preferences (eg, concerns about specific adverse effects or differences in out-of-pocket cost) in favor of one over the other, she could flip a coin to decide between initiating maintenance roflumilast or azithromycin.
Dr. Krishnan is Professor of Medicine, Division of Pulmonary, Critical Care, Sleep & Allergy, and Professor of Public Health, Division of Epidemiology and Biostatistics, University of Illinois Chicago. Dr. Adrish is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine, Houston.
References:
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. https://goldcopd.org/2024-gold-report-2/
2. US Food and Drug Administration (Daliresp®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/022522s003lbl.pdf
3. Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromucin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689-98. PMID: 21864166. doi: 10.1056/NEJMoa1104623.
4. US Food and Drug Administration (Zithromyax®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/050710s039,050711s036,050784s023lbl.pdf
5. Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acure exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society guideline. Chest. 2015;147(4)894-942. PMID: 25321320. doi: 10.1378/chest.14-1676.
6. Wedzicha JA, Calverley PMA, Albert RK, et al. Prevention of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;50(3):1602265. PMID: 28889106. doi:10.1183/13993003.02265-2016.
7. Krishnan JA, Albert RK, Rennard SI; RELIANCE study. Waiting for actionable evidence: roflumilast or azithromycin? Chronic Obst Pulm Dis. 2022;9(1):1-3. PMID: 34783231. doi: 10.15326/jcopdf.2021.0272.
8. Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phospodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. PMID: 37364283.
“Janice Turner” (name changed to protect confidentiality) is a 66-year-old woman with a 40-pack per year history of smoking. She is very worried about having another COPD exacerbation and wants to know if there are additional medications she could try.
Over the past 2 weeks, her respiratory symptoms have improved and returned to her baseline. She has a daily cough with white phlegm on most days and dyspnea on exertion at one-half block on level ground. She reports using her medications as prescribed and is enrolled in a pulmonary rehabilitation program, which she attends twice per week. She uses 2 to 4 inhalations of albuterol each day.
She is on the following regimen for her COPD, which is unchanged compared with what she has been prescribed for the past 12 months: 1) combination inhaled fluticasone furoate, umeclidinium, and vilanterol via the Ellipta® device, one actuation once daily and 2) inhaled albuterol, two puffs as needed every 4 hours via metered dose inhaler. She demonstrates mastery of inhaler technique for both inhaled devices. Her vaccinations are current (pneumococcus, influenza, respiratory syncytial virus, and COVID-19).
On examination, she can complete sentences without respiratory difficulty, and her vital signs are normal. She has decreased breath sounds in all lung fields, with occasional rhonchi. Heart sounds are distant, but regular, at 92 beats per minute, and she has no peripheral edema. Arterial blood gas at rest on room air indicates a pH of 7.38, PaO2 of 63 mm Hg, and PaCO2 of 42 mm Hg. An electrocardiogram shows sinus rhythm and a QTc interval of 420 milliseconds.
Three months ago, when she was clinically stable, you obtained spirometry, a complete blood count with differential, and a chest radiograph to exclude alternate diagnoses for her ongoing respiratory symptoms. She had severe airflow limitation (post-bronchodilator FEV1 = 40% predicted, FVC = 61% predicted, FEV1/FVC = 65%). At the time, she also had peripheral eosinophilia (eosinophil count of 350 cells/μL) and hyperinflation without parenchymal infiltrates.
In summary, Ms. Turner has severe smoking-associated COPD Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 3E and chronic bronchitis with two severe exacerbations in the past 12 months.1 She is currently prescribed triple inhaled maintenance therapy with corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. She has a normal QTc interval.
So what would you recommend to reduce Ms. Turner’s risk of future exacerbations?
In 2011, the US Food and Drug Administration (FDA) approved roflumilast 500 mcg by mouth per day, a selective phosphodiesterase 4 (PDE4) inhibitor, as maintenance therapy to reduce the risk of COPD exacerbations in patients with severe COPD associated with chronic bronchitis.2 The FDA approval was based on a review of the efficacy and safety of roflumilast in eight randomized, double-blind, controlled clinical trials in 9,394 adults with COPD.
Two subsequently completed randomized clinical trials in 2015 (REACT, 1,945 adults) and 2016 (RE2SPOND, 2,354 adults) also found that maintenance oral treatment escalation with roflumilast significantly reduced the risk of COPD exacerbations compared with placebo.2 The most common adverse effects reported with long-term use of roflumilast are related to the gastrointestinal tract (diarrhea, nausea, decreased appetite), weight loss, and insomnia. Four weeks of roflumilast at 250 mcg per day prior to dose escalation to 500 mcg per day reduces the risk of treatment discontinuation and improves tolerability compared with initiating treatment with the maintenance dose.
In 2022, the FDA approved a generic version of roflumilast, providing an opportunity for patients to use roflumilast at a lower cost than was previously possible. Importantly, the FDA Prescribing Information includes a warning to avoid the use of roflumilast in patients being treated with strong cytochrome P450 enzyme inducers (eg, rifampin, phenytoin). The FDA Prescribing Information also recommends weighing the risks and benefits of roflumilast in patients with a history of depression or suicidal thoughts or behavior, or patients with unexplained or clinically significant weight loss.
In 2011 (the same year as the FDA approval of roflumilast), the National Institutes of Health/National Heart, Lung, and Blood Institute-funded COPD Clinical Research Network reported that maintenance treatment with azithromycin reduced the risk of COPD exacerbations compared with placebo in a randomized clinical trial of 1,142 adults with COPD (MACRO study).3 Subgroup analyses indicated that the reduction in the risk of COPD exacerbations with azithromycin was observed in participants with or without chronic bronchitis but not in participants who currently smoked.
Subsequently, two other smaller randomized clinical trials in 2014 (COLUMBUS, 92 participants) and in 2019 (BACE, 301 participants) also demonstrated a reduction in the risk of COPD exacerbations with maintenance azithromycin treatment compared with placebo. Azithromycin can prolong the QT interval and, in rare cases, cause cardiac arrythmias, especially when used with other medications that can prolong the QT interval. There are also concerns that maintenance azithromycin therapy could lead to decrements in hearing or promote the development of macrolide-resistant bacteria. Maintenance treatment with azithromycin to prevent COPD exacerbations is not an FDA-approved indication.4 The FDA approval for azithromycin is currently limited to treatment of patients with mild to moderate infections caused by susceptible bacteria, but it is often prescribed off-label as maintenance treatment for COPD.
On the basis of this body of evidence from clinical trials in COPD, the 2015 CHEST and Canadian Thoracic Society (CTS) guidelines,5 the 2017 European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines,6 and the 2024 GOLD Strategy Report all include recommendations for treatment escalation with maintenance roflumilast or azithromycin to reduce the risk of COPD exacerbations. For example, the 2024 GOLD Strategy Report recommends roflumilast in patients with severe COPD and chronic bronchitis who continue to have exacerbations despite inhaled maintenance treatment with combination long-acting β2-agonist and long-acting muscarinic antagonist or with triple therapy with inhaled corticosteroids, long-acting β2-agonist, and long-acting muscarinic antagonist. An alternative, 2024 GOLD-recommended strategy in this population is maintenance therapy with azithromycin, “preferentially in former smokers.” GOLD’s preference for using azithromycin in patients with smoking history is based on post-hoc (ie, not part of the original study design) subgroup analyses “suggesting lesser benefit in active smokers” in the MACRO study. Results of such analyses have not been reported in other studies.
There are no results from clinical trials that have directly compared the harms and benefits of initiating maintenance therapy with roflumilast or azithromycin in patients with COPD. The roflumilast or azithromycin to prevent COPD exacerbations (RELIANCE; NCT04069312) multicenter clinical trial is addressing this evidence gap.7 The RELIANCE study is funded by the Patient-Centered Outcomes Research Institute and co-led by the COPD Foundation, a not-for-profit organization founded by John W. Walsh, a patient advocate with α1-related COPD. Also, results of two recently completed phase 3 clinical trials with nebulized ensifentrine (ENHANCE-1 and ENHANCE-2), a novel inhibitor of PDE3 and PDE4, were recently published. ENHANCE-1 and ENHANCE-2 studies indicate that twice daily nebulized ensifentrine reduces the risk of COPD exacerbations in patients with moderate or severe COPD.8 Ensifentrine is under review by the FDA, and a decision about its use in the US is expected in the summer of 2024.
Until the results from the RELIANCE clinical trial and the decision by the FDA about ensifentrine are available, we recommended a discussion with Ms. Turner about whether to initiate treatment with maintenance roflumilast or azithromycin. Both can reduce the risk of exacerbations, and the relative benefits and risks of these two evidence-based options are not yet known. Unless Ms. Turner has specific preferences (eg, concerns about specific adverse effects or differences in out-of-pocket cost) in favor of one over the other, she could flip a coin to decide between initiating maintenance roflumilast or azithromycin.
Dr. Krishnan is Professor of Medicine, Division of Pulmonary, Critical Care, Sleep & Allergy, and Professor of Public Health, Division of Epidemiology and Biostatistics, University of Illinois Chicago. Dr. Adrish is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine, Houston.
References:
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. https://goldcopd.org/2024-gold-report-2/
2. US Food and Drug Administration (Daliresp®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/022522s003lbl.pdf
3. Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromucin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689-98. PMID: 21864166. doi: 10.1056/NEJMoa1104623.
4. US Food and Drug Administration (Zithromyax®). https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/050710s039,050711s036,050784s023lbl.pdf
5. Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acure exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society guideline. Chest. 2015;147(4)894-942. PMID: 25321320. doi: 10.1378/chest.14-1676.
6. Wedzicha JA, Calverley PMA, Albert RK, et al. Prevention of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;50(3):1602265. PMID: 28889106. doi:10.1183/13993003.02265-2016.
7. Krishnan JA, Albert RK, Rennard SI; RELIANCE study. Waiting for actionable evidence: roflumilast or azithromycin? Chronic Obst Pulm Dis. 2022;9(1):1-3. PMID: 34783231. doi: 10.15326/jcopdf.2021.0272.
8. Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phospodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. PMID: 37364283.
Daylight Saving Time: Saving light but endangering health
The American Academy of Sleep Medicine recently published its position statement reaffirming its support of utilizing permanent Standard Time (ST) as opposed to Daylight Saving Time (DST).1 DST usually occurs on the second Sunday in March when we “spring forward” by advancing the clock by 1 hour. The analogous “fall back” on the first Sunday in November refers to reversion back to the original ST, which is more synchronous with the sun’s natural pattern of rise and fall.
The earliest argument for DST practice dates back to the 1700s when Benjamin Franklin wrote a satirical piece in the Journal of Paris suggesting that advancing the clock to rise earlier in the summer would lead to economization in candle usage and save significant resources for Parisians. The modern version of this assertion infers that increased daylight in the evening will lead to increased consumer activity and work productivity with consequent economic benefits. Interestingly, the adoption of DST has demonstrated the opposite—a reduction in work productivity and economic losses.2 Another often-cited claim is that increased daylight in the evening could lead to fewer motor vehicle accidents. However, the reality is that DST is associated with more frequent car accidents in the morning.
The greatest drawback of DST is that, initially, it leads to sleep deprivation and chronically drives asynchronization between the circadian clock and the social clock. Humans synchronize their internal clock based on several factors, including light, temperature, feeding, and social habits. However, light is the strongest exogenous factor that regulates the internal clock. Light inhibits secretion of melatonin, an endogenous hormone that promotes sleep onset. While there is some individual variation in circadian patterns, exposure to bright light in the morning leads to increased physical, mental, and goal-directed activity.
Conversely, darkness or reduced light exposure in the evening hours promotes decreased activity and sleep onset via melatonin release. DST disrupts this natural process by promoting increased light exposure in the evening. This desynchronizes solar light from our internal clocks, causing a relative phase delay. Acutely, patients experience a form of imposed social jet lag. They lose an hour of sleep due to diminished sleep opportunity, as work and social obligations are typically not altered to allow for a later awakening. With recurrent delays, this lends to a pattern of chronic sleep deprivation which has significant health consequences.
Losing an hour of sleep opportunity as the clock advances in spring has dire consequences. The transition to DST is associated with increased cardiovascular events, including myocardial infarction, stroke, and admissions for acute atrial fibrillation.3 4 5 A large body of work has shown that acute reduction of sleep is associated with higher sympathetic tone, compromised immunity, and increased inflammation. Further, cognitive consequences can ensue in the form of altered situational awareness, increased risky behavior, and worse reaction time—which manifest as increased motor vehicle accidents, injuries, and fatalities.6 Emergency room visits and bounce-back admissions, medical errors and injuries, and missed appointments increase following the switch to DST.7 Psychiatric outcomes, including deaths due to suicide and overdose, are worse with the spring transition.8
Is the problem with DST merely limited to springtime, when we lose an hour of sleep? Not quite. During the “fall back” period, despite theoretically gaining an hour of sleep opportunity, people exhibit evidence of sleep disruption, psychiatric issues, traffic accidents, and inflammatory bowel disease exacerbations. These consequences likely stem from a discordance between circadian and social time, which leads to an earlier awakening based on circadian physiology as opposed to the clock time.
The acute impact of changing our sleep patterns during transitions in clock time may be appreciated more readily, but the damage is much more insidious. Chronic exposure to light in the late evening creates a state of enhanced arousal when the body should be winding down. The chronic incongruency between clock and solar time leads to dyssynchrony in our usual functions, such as food intake, social and physical activity, and basal temperature. Consequently, there is an impetus to fall asleep later. This leads to an accumulation of sleep debt and its associated negative consequences in the general, already chronically sleep-deprived population. This is especially impactful to adolescents and young adults who tend to have a delay in their sleep and wake patterns and, yet, are socially bound to early morning awakenings for school or work.
The scientific evidence behind the health risk and benefit profile of DST and ST is incontrovertible and in favor of ST. The hallmark of appropriate sleep habits involves consistency and appropriate duration. Changing timing forward or backward increases the likelihood of an alteration of the baseline established sleep and circadian consistency.
Unfortunately, despite multiple polls demonstrating the populace’s dislike of DST, repeat attempts to codify DST and negate ST persist. The latest initiative, the Sunshine Protection Act, which promised permanent DST, was passed by the US Senate but was thankfully foiled by Congress in 2022. The act of setting a time is not one that should be taken lightly or in isolation because there are significant, long-lasting health, safety, and socioeconomic consequences of this decision. Practically, this entails a concerted effort from all major economies since consistency is essential for trade and geopolitical relations. China, Japan, and India don’t practice DST. The European Parliament voted successfully to abolish DST in the European Union in 2019 with a plan to implement ST in 2021. Implementation has yet to be successful due to interruptions from the COVID-19 pandemic as well as the current economic and political climate in Europe. Political or theoretical political victories should not supersede the health and safety of an elected official’s constituents. As a medical community, we should continue to use our collective voice to encourage our representatives to vote in ways that positively affect our patients’ health outcomes.
References:
1. Rishi MA, et al. JCSM. 2024;20(1):121.
2. Gibson M, et al. Rev Econ Stat. 2018;100(5):783.
3. Jansky I, et al. N Engl J Med. 2008;359(18):1966.
4. Sipilia J, et al. Sleep Med. 2016;27-28:20.
5. Chudow JJ, et al. Sleep Med. 2020;69:155.
6. Fritz J, et al. Curr Biol. 2020;30(4):729.
7. Ferrazzi E, et al. J Biol Rhythms. 2018;33(5):555-564.
8. Berk M, et al. Sleep Biol Rhythms. 2008;6(1):22.
The American Academy of Sleep Medicine recently published its position statement reaffirming its support of utilizing permanent Standard Time (ST) as opposed to Daylight Saving Time (DST).1 DST usually occurs on the second Sunday in March when we “spring forward” by advancing the clock by 1 hour. The analogous “fall back” on the first Sunday in November refers to reversion back to the original ST, which is more synchronous with the sun’s natural pattern of rise and fall.
The earliest argument for DST practice dates back to the 1700s when Benjamin Franklin wrote a satirical piece in the Journal of Paris suggesting that advancing the clock to rise earlier in the summer would lead to economization in candle usage and save significant resources for Parisians. The modern version of this assertion infers that increased daylight in the evening will lead to increased consumer activity and work productivity with consequent economic benefits. Interestingly, the adoption of DST has demonstrated the opposite—a reduction in work productivity and economic losses.2 Another often-cited claim is that increased daylight in the evening could lead to fewer motor vehicle accidents. However, the reality is that DST is associated with more frequent car accidents in the morning.
The greatest drawback of DST is that, initially, it leads to sleep deprivation and chronically drives asynchronization between the circadian clock and the social clock. Humans synchronize their internal clock based on several factors, including light, temperature, feeding, and social habits. However, light is the strongest exogenous factor that regulates the internal clock. Light inhibits secretion of melatonin, an endogenous hormone that promotes sleep onset. While there is some individual variation in circadian patterns, exposure to bright light in the morning leads to increased physical, mental, and goal-directed activity.
Conversely, darkness or reduced light exposure in the evening hours promotes decreased activity and sleep onset via melatonin release. DST disrupts this natural process by promoting increased light exposure in the evening. This desynchronizes solar light from our internal clocks, causing a relative phase delay. Acutely, patients experience a form of imposed social jet lag. They lose an hour of sleep due to diminished sleep opportunity, as work and social obligations are typically not altered to allow for a later awakening. With recurrent delays, this lends to a pattern of chronic sleep deprivation which has significant health consequences.
Losing an hour of sleep opportunity as the clock advances in spring has dire consequences. The transition to DST is associated with increased cardiovascular events, including myocardial infarction, stroke, and admissions for acute atrial fibrillation.3 4 5 A large body of work has shown that acute reduction of sleep is associated with higher sympathetic tone, compromised immunity, and increased inflammation. Further, cognitive consequences can ensue in the form of altered situational awareness, increased risky behavior, and worse reaction time—which manifest as increased motor vehicle accidents, injuries, and fatalities.6 Emergency room visits and bounce-back admissions, medical errors and injuries, and missed appointments increase following the switch to DST.7 Psychiatric outcomes, including deaths due to suicide and overdose, are worse with the spring transition.8
Is the problem with DST merely limited to springtime, when we lose an hour of sleep? Not quite. During the “fall back” period, despite theoretically gaining an hour of sleep opportunity, people exhibit evidence of sleep disruption, psychiatric issues, traffic accidents, and inflammatory bowel disease exacerbations. These consequences likely stem from a discordance between circadian and social time, which leads to an earlier awakening based on circadian physiology as opposed to the clock time.
The acute impact of changing our sleep patterns during transitions in clock time may be appreciated more readily, but the damage is much more insidious. Chronic exposure to light in the late evening creates a state of enhanced arousal when the body should be winding down. The chronic incongruency between clock and solar time leads to dyssynchrony in our usual functions, such as food intake, social and physical activity, and basal temperature. Consequently, there is an impetus to fall asleep later. This leads to an accumulation of sleep debt and its associated negative consequences in the general, already chronically sleep-deprived population. This is especially impactful to adolescents and young adults who tend to have a delay in their sleep and wake patterns and, yet, are socially bound to early morning awakenings for school or work.
The scientific evidence behind the health risk and benefit profile of DST and ST is incontrovertible and in favor of ST. The hallmark of appropriate sleep habits involves consistency and appropriate duration. Changing timing forward or backward increases the likelihood of an alteration of the baseline established sleep and circadian consistency.
Unfortunately, despite multiple polls demonstrating the populace’s dislike of DST, repeat attempts to codify DST and negate ST persist. The latest initiative, the Sunshine Protection Act, which promised permanent DST, was passed by the US Senate but was thankfully foiled by Congress in 2022. The act of setting a time is not one that should be taken lightly or in isolation because there are significant, long-lasting health, safety, and socioeconomic consequences of this decision. Practically, this entails a concerted effort from all major economies since consistency is essential for trade and geopolitical relations. China, Japan, and India don’t practice DST. The European Parliament voted successfully to abolish DST in the European Union in 2019 with a plan to implement ST in 2021. Implementation has yet to be successful due to interruptions from the COVID-19 pandemic as well as the current economic and political climate in Europe. Political or theoretical political victories should not supersede the health and safety of an elected official’s constituents. As a medical community, we should continue to use our collective voice to encourage our representatives to vote in ways that positively affect our patients’ health outcomes.
References:
1. Rishi MA, et al. JCSM. 2024;20(1):121.
2. Gibson M, et al. Rev Econ Stat. 2018;100(5):783.
3. Jansky I, et al. N Engl J Med. 2008;359(18):1966.
4. Sipilia J, et al. Sleep Med. 2016;27-28:20.
5. Chudow JJ, et al. Sleep Med. 2020;69:155.
6. Fritz J, et al. Curr Biol. 2020;30(4):729.
7. Ferrazzi E, et al. J Biol Rhythms. 2018;33(5):555-564.
8. Berk M, et al. Sleep Biol Rhythms. 2008;6(1):22.
The American Academy of Sleep Medicine recently published its position statement reaffirming its support of utilizing permanent Standard Time (ST) as opposed to Daylight Saving Time (DST).1 DST usually occurs on the second Sunday in March when we “spring forward” by advancing the clock by 1 hour. The analogous “fall back” on the first Sunday in November refers to reversion back to the original ST, which is more synchronous with the sun’s natural pattern of rise and fall.
The earliest argument for DST practice dates back to the 1700s when Benjamin Franklin wrote a satirical piece in the Journal of Paris suggesting that advancing the clock to rise earlier in the summer would lead to economization in candle usage and save significant resources for Parisians. The modern version of this assertion infers that increased daylight in the evening will lead to increased consumer activity and work productivity with consequent economic benefits. Interestingly, the adoption of DST has demonstrated the opposite—a reduction in work productivity and economic losses.2 Another often-cited claim is that increased daylight in the evening could lead to fewer motor vehicle accidents. However, the reality is that DST is associated with more frequent car accidents in the morning.
The greatest drawback of DST is that, initially, it leads to sleep deprivation and chronically drives asynchronization between the circadian clock and the social clock. Humans synchronize their internal clock based on several factors, including light, temperature, feeding, and social habits. However, light is the strongest exogenous factor that regulates the internal clock. Light inhibits secretion of melatonin, an endogenous hormone that promotes sleep onset. While there is some individual variation in circadian patterns, exposure to bright light in the morning leads to increased physical, mental, and goal-directed activity.
Conversely, darkness or reduced light exposure in the evening hours promotes decreased activity and sleep onset via melatonin release. DST disrupts this natural process by promoting increased light exposure in the evening. This desynchronizes solar light from our internal clocks, causing a relative phase delay. Acutely, patients experience a form of imposed social jet lag. They lose an hour of sleep due to diminished sleep opportunity, as work and social obligations are typically not altered to allow for a later awakening. With recurrent delays, this lends to a pattern of chronic sleep deprivation which has significant health consequences.
Losing an hour of sleep opportunity as the clock advances in spring has dire consequences. The transition to DST is associated with increased cardiovascular events, including myocardial infarction, stroke, and admissions for acute atrial fibrillation.3 4 5 A large body of work has shown that acute reduction of sleep is associated with higher sympathetic tone, compromised immunity, and increased inflammation. Further, cognitive consequences can ensue in the form of altered situational awareness, increased risky behavior, and worse reaction time—which manifest as increased motor vehicle accidents, injuries, and fatalities.6 Emergency room visits and bounce-back admissions, medical errors and injuries, and missed appointments increase following the switch to DST.7 Psychiatric outcomes, including deaths due to suicide and overdose, are worse with the spring transition.8
Is the problem with DST merely limited to springtime, when we lose an hour of sleep? Not quite. During the “fall back” period, despite theoretically gaining an hour of sleep opportunity, people exhibit evidence of sleep disruption, psychiatric issues, traffic accidents, and inflammatory bowel disease exacerbations. These consequences likely stem from a discordance between circadian and social time, which leads to an earlier awakening based on circadian physiology as opposed to the clock time.
The acute impact of changing our sleep patterns during transitions in clock time may be appreciated more readily, but the damage is much more insidious. Chronic exposure to light in the late evening creates a state of enhanced arousal when the body should be winding down. The chronic incongruency between clock and solar time leads to dyssynchrony in our usual functions, such as food intake, social and physical activity, and basal temperature. Consequently, there is an impetus to fall asleep later. This leads to an accumulation of sleep debt and its associated negative consequences in the general, already chronically sleep-deprived population. This is especially impactful to adolescents and young adults who tend to have a delay in their sleep and wake patterns and, yet, are socially bound to early morning awakenings for school or work.
The scientific evidence behind the health risk and benefit profile of DST and ST is incontrovertible and in favor of ST. The hallmark of appropriate sleep habits involves consistency and appropriate duration. Changing timing forward or backward increases the likelihood of an alteration of the baseline established sleep and circadian consistency.
Unfortunately, despite multiple polls demonstrating the populace’s dislike of DST, repeat attempts to codify DST and negate ST persist. The latest initiative, the Sunshine Protection Act, which promised permanent DST, was passed by the US Senate but was thankfully foiled by Congress in 2022. The act of setting a time is not one that should be taken lightly or in isolation because there are significant, long-lasting health, safety, and socioeconomic consequences of this decision. Practically, this entails a concerted effort from all major economies since consistency is essential for trade and geopolitical relations. China, Japan, and India don’t practice DST. The European Parliament voted successfully to abolish DST in the European Union in 2019 with a plan to implement ST in 2021. Implementation has yet to be successful due to interruptions from the COVID-19 pandemic as well as the current economic and political climate in Europe. Political or theoretical political victories should not supersede the health and safety of an elected official’s constituents. As a medical community, we should continue to use our collective voice to encourage our representatives to vote in ways that positively affect our patients’ health outcomes.
References:
1. Rishi MA, et al. JCSM. 2024;20(1):121.
2. Gibson M, et al. Rev Econ Stat. 2018;100(5):783.
3. Jansky I, et al. N Engl J Med. 2008;359(18):1966.
4. Sipilia J, et al. Sleep Med. 2016;27-28:20.
5. Chudow JJ, et al. Sleep Med. 2020;69:155.
6. Fritz J, et al. Curr Biol. 2020;30(4):729.
7. Ferrazzi E, et al. J Biol Rhythms. 2018;33(5):555-564.
8. Berk M, et al. Sleep Biol Rhythms. 2008;6(1):22.
Patients haunted by fears of living with and dying from severe lung disease
Many patients with chronic progressive pulmonary disease feel anxious and depressed as their conditions advance, as breathing becomes increasingly labored and difficult, and as performing even small daily tasks leaves them exhausted.
Persons with severe COPD frequently report fears of suffocation and death, as well as anxieties about abandoning family and friends, and these negative, intrusive thoughts can have an adverse effect on COPD outcomes.
Disease-related mental distress can lead to increased disability, more frequent use of costly health care resources, higher morbidity, and elevated risk of death, investigators say.
"Individuals with severe COPD are twice as likely to develop depression than patients with mild COPD. Prevalence rates for clinical anxiety in COPD range from 13% to 46% in outpatients and 10% to 55% among inpatients," wrote Abebaw Mengitsu Yohannes, PhD, then from Azusa Pacific University in Azusa, California and colleagues in an article published jointly by The Journal of Family Practice and The Cleveland Clinic Journal of Medicine.
Patients with COPD may experience major depressive disorders, chronic mild depression (dysthymias), and minor depression, as well as generalized anxiety disorder, phobias, and panic disorders, the investigators say.
"Growing evidence suggests that the relationship between mood disorders, particularly depression, and COPD is bidirectional, meaning that mood disorders adversely impact prognosis in COPD, whereas COPD increases the risk of developing depression," Yohannes et al wrote.
Jamie Garfield, MD, professor of thoracic medicine and surgery at Temple University's Lewis Katz School of Medicine in Philadelphia, told Chest Physician that the association between severe chronic diseases and mood disorders is well known.
"I don't think that it's specific to chronic lung diseases; in people with chronic heart disease or malignancies we see that co-existence of depression and anxiety will worsen the course of disease," she said.
Dr. Johannes, who is currently a professor of physical therapy at the University of Alabama School of Health Professionals in Birmingham, said that depression and anxiety are often underdiagnosed and undertreated in patients with obstructive pulmonary diseases because the conditions can share symptoms such as dyspnea (for example, in anxiety) or fatigue (in depression).
"Therefore, unless one begins to explore further, it's hard for physicians to be able to identify these conditions," he said in an interview with Chest Physician.
Fears of dying (and living)
The causes of depression and anxiety among patients with obstructive pulmonary disorders are multi-factorial, and may require a variety of treatment and coping strategies, according to Susann Strang, RN, PhD, and colleagues from the University of Gothenburg, Sweden.
They conducted qualitative in-depth interviews with 31 men and women with stage III or IV COPD, and found that the majority of patients had anxiety associated with their disease.
"Analyses revealed three major themes: death anxiety, life anxiety, and counterweights to anxiety," the investigators wrote in a study published in the journal Palliative and Supportive Care in 2014.
Factors contributing to anxiety surrounding death included fear of suffocation, awareness of impending death, fear of the process of death, and anxiety about being separated from loved ones.
In contrast, some patients expressed dread of living with the limitations and loneliness imposed on them by their disease, so called "life anxiety."
The patients also reported "counterweights" to anxiety as a way of coping. For some this involved trust in their health care professionals and adherence to medication, inhalers, and supplemental oxygen.
"The patients also placed hope in new treatments, better medication, surgery, stem cell treatment, or lung transplants," Dr. Strang and colleagues reported.
Others reported avoiding talking about death, sleeping more, or using humor to "laugh off this difficult subject."
Screening and diagnosis
Primary care practitioners are often the first health professionals that patients with COPD see, but these clinicians often don't have the time to add screening to their already crammed schedules. In addition, "the lack of a standardized approach in diagnosis, and inadequate knowledge or confidence in assessing psychological status (particularly given the number of strategies available for screening patients for mood disorders)," can make it difficult for PCPs to detect and manage anxiety and depression in their patients with significant health care burdens from COPD and other obstructive lung diseases, Dr. Yohannes and colleagues noted.
In addition to commonly used screening tools for anxiety and depression such as the Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire (PHQ-9), there are at least two designed to evaluate patients with lung disease: the Anxiety Inventory for Respiratory (AIR) Disease scale, developed by Dr. Johannes and colleagues, and the COPD Anxiety Questionnaire.
The COPD Assessment Testand Clinical COPD Questionnaire, while not specifically designed to screen for mental disorders, include questions that can point to symptoms of distress in patients with COPD, Dr. Yohannes said.
"In truth I think that there are few providers who will routinely do this on all their patients in terms of quantifying the severity or the presence or absence of depression, but in my own practice I very much ask questions that align with the questions in these tools to determine whether my patient appears to have high levels of anxiety and depression," Dr. Garfield said.
Listen to patients and families
Among the most powerful tools that clinicians have at their disposal for treating anxiety and depression in patients with chronic lung disease are their ears and their minds, said Anthony Saleh, MD, a pulmonologist at New York-Presbyterian Brooklyn Methodist Hospital in Brooklyn, New York.
"I think just listening to the patient, that's a little bit forgotten yet so important," he said in an interview with Chest Physician.
"When I have someone with advanced lung disease, like idiopathic pulmonary fibrosis, like advanced emphysema, one of the most important things I think is to listen to the patient, and not just to listen to the answers of your perfunctory 'how's your breathing? Any chest pain?' and those sort of rote medical questions, but listen to their thoughts, and it will given them a safe space to say 'Hey, I'm nervous, hey I'm worried about my family, hey I'm worried if I die what's going to happen to my wife and kids,' and that's something I think is invaluable."
It's also vital to listen to the concerns of the patients family members, who may be the primary caregivers and may share the patient's stresses and anxieties, he said.
Pulmonary Rehabilitation
All of the experts interviewed for this article agreed that a combination of medical, social and mental health support services is important for treatment for patients with chronic obstructive lung diseases.
One of the most effective means of helping patients with both acute breathing problems and with disease-related anxiety and depression is pulmonary rehabilitation. Depending on disease severity, this multidisciplinary approach may involve exercise, patient education, psychological and nutrition counseling, and training patients how to conserve energy and adopt breathing strategies to help them better manage their symptoms.
"I think that pulmonary rehabilitation is one of the first interventions that we should be recommending for our patients," Dr. Garfield said. "It's physical therapy for patients with chronic lung diseases, backed by respiratory therapists, and it offers not only physical rehabilitation - improving strength and coordination, but also it helps our patients get as much as possible out of what they've got."
For example, patients can be taught how to decrease their respiratory rate when they're feeling a sense of urgency or panic. Patients can also learn how to change body positions to help them breathe more effectively when they feel that their breath is limited or restricted, she said.
"Once your into medical interventions, pulmonary rehab is phenomenal," Dr. Saleh said.
Pulmonary rehabilitation helps patients to feel better about themselves and about their abilities, but "unfortunately it's not as available as we like," he said.
Many patients don't live near a pulmonary rehabilitation center, and the typical two to three weekly sessions for 4 to 12 weeks or longer can be a significant burden for patients and caregivers, he acknowledged.
"You have to sit [with the patient] and be honest and tell them it's a lot of diligence involved and you have to be really motivated," he said.
Other treatment options include pharmacological therapy with antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and anxiolytic agents.
"SSRIs are the current first-line drug treatment for depression, and have been shown to significantly improve depression and anxiety in patients with COPD in some, but not all, trials published to date. However, it is important to note that a diagnosis of bipolar disorder must be ruled out before initiating standard antidepressant therapy," Dr. Johannes and colleagues wrote.
Defiant joy
Importantly, even with the burden of life with COPD, many patients found ways to experience what Strang et al called "a defiant joy."
"It was remarkable that when the patients were asked about what gave their lives meaning today, many talked about what had given their life meaning in the past, prior to becoming ill. In the light of the things they had lost because of the disease, many felt that their previous sources of joy no longer existed. Despite this, many still hoped to be able to get out into the fresh air, to be able to do errands or that tomorrow might be better," the investigators wrote.
Dr. Yohannes, Dr. Garfield, and Dr. Saleh all reported having no relevant conflicts of interest to report.
Many patients with chronic progressive pulmonary disease feel anxious and depressed as their conditions advance, as breathing becomes increasingly labored and difficult, and as performing even small daily tasks leaves them exhausted.
Persons with severe COPD frequently report fears of suffocation and death, as well as anxieties about abandoning family and friends, and these negative, intrusive thoughts can have an adverse effect on COPD outcomes.
Disease-related mental distress can lead to increased disability, more frequent use of costly health care resources, higher morbidity, and elevated risk of death, investigators say.
"Individuals with severe COPD are twice as likely to develop depression than patients with mild COPD. Prevalence rates for clinical anxiety in COPD range from 13% to 46% in outpatients and 10% to 55% among inpatients," wrote Abebaw Mengitsu Yohannes, PhD, then from Azusa Pacific University in Azusa, California and colleagues in an article published jointly by The Journal of Family Practice and The Cleveland Clinic Journal of Medicine.
Patients with COPD may experience major depressive disorders, chronic mild depression (dysthymias), and minor depression, as well as generalized anxiety disorder, phobias, and panic disorders, the investigators say.
"Growing evidence suggests that the relationship between mood disorders, particularly depression, and COPD is bidirectional, meaning that mood disorders adversely impact prognosis in COPD, whereas COPD increases the risk of developing depression," Yohannes et al wrote.
Jamie Garfield, MD, professor of thoracic medicine and surgery at Temple University's Lewis Katz School of Medicine in Philadelphia, told Chest Physician that the association between severe chronic diseases and mood disorders is well known.
"I don't think that it's specific to chronic lung diseases; in people with chronic heart disease or malignancies we see that co-existence of depression and anxiety will worsen the course of disease," she said.
Dr. Johannes, who is currently a professor of physical therapy at the University of Alabama School of Health Professionals in Birmingham, said that depression and anxiety are often underdiagnosed and undertreated in patients with obstructive pulmonary diseases because the conditions can share symptoms such as dyspnea (for example, in anxiety) or fatigue (in depression).
"Therefore, unless one begins to explore further, it's hard for physicians to be able to identify these conditions," he said in an interview with Chest Physician.
Fears of dying (and living)
The causes of depression and anxiety among patients with obstructive pulmonary disorders are multi-factorial, and may require a variety of treatment and coping strategies, according to Susann Strang, RN, PhD, and colleagues from the University of Gothenburg, Sweden.
They conducted qualitative in-depth interviews with 31 men and women with stage III or IV COPD, and found that the majority of patients had anxiety associated with their disease.
"Analyses revealed three major themes: death anxiety, life anxiety, and counterweights to anxiety," the investigators wrote in a study published in the journal Palliative and Supportive Care in 2014.
Factors contributing to anxiety surrounding death included fear of suffocation, awareness of impending death, fear of the process of death, and anxiety about being separated from loved ones.
In contrast, some patients expressed dread of living with the limitations and loneliness imposed on them by their disease, so called "life anxiety."
The patients also reported "counterweights" to anxiety as a way of coping. For some this involved trust in their health care professionals and adherence to medication, inhalers, and supplemental oxygen.
"The patients also placed hope in new treatments, better medication, surgery, stem cell treatment, or lung transplants," Dr. Strang and colleagues reported.
Others reported avoiding talking about death, sleeping more, or using humor to "laugh off this difficult subject."
Screening and diagnosis
Primary care practitioners are often the first health professionals that patients with COPD see, but these clinicians often don't have the time to add screening to their already crammed schedules. In addition, "the lack of a standardized approach in diagnosis, and inadequate knowledge or confidence in assessing psychological status (particularly given the number of strategies available for screening patients for mood disorders)," can make it difficult for PCPs to detect and manage anxiety and depression in their patients with significant health care burdens from COPD and other obstructive lung diseases, Dr. Yohannes and colleagues noted.
In addition to commonly used screening tools for anxiety and depression such as the Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire (PHQ-9), there are at least two designed to evaluate patients with lung disease: the Anxiety Inventory for Respiratory (AIR) Disease scale, developed by Dr. Johannes and colleagues, and the COPD Anxiety Questionnaire.
The COPD Assessment Testand Clinical COPD Questionnaire, while not specifically designed to screen for mental disorders, include questions that can point to symptoms of distress in patients with COPD, Dr. Yohannes said.
"In truth I think that there are few providers who will routinely do this on all their patients in terms of quantifying the severity or the presence or absence of depression, but in my own practice I very much ask questions that align with the questions in these tools to determine whether my patient appears to have high levels of anxiety and depression," Dr. Garfield said.
Listen to patients and families
Among the most powerful tools that clinicians have at their disposal for treating anxiety and depression in patients with chronic lung disease are their ears and their minds, said Anthony Saleh, MD, a pulmonologist at New York-Presbyterian Brooklyn Methodist Hospital in Brooklyn, New York.
"I think just listening to the patient, that's a little bit forgotten yet so important," he said in an interview with Chest Physician.
"When I have someone with advanced lung disease, like idiopathic pulmonary fibrosis, like advanced emphysema, one of the most important things I think is to listen to the patient, and not just to listen to the answers of your perfunctory 'how's your breathing? Any chest pain?' and those sort of rote medical questions, but listen to their thoughts, and it will given them a safe space to say 'Hey, I'm nervous, hey I'm worried about my family, hey I'm worried if I die what's going to happen to my wife and kids,' and that's something I think is invaluable."
It's also vital to listen to the concerns of the patients family members, who may be the primary caregivers and may share the patient's stresses and anxieties, he said.
Pulmonary Rehabilitation
All of the experts interviewed for this article agreed that a combination of medical, social and mental health support services is important for treatment for patients with chronic obstructive lung diseases.
One of the most effective means of helping patients with both acute breathing problems and with disease-related anxiety and depression is pulmonary rehabilitation. Depending on disease severity, this multidisciplinary approach may involve exercise, patient education, psychological and nutrition counseling, and training patients how to conserve energy and adopt breathing strategies to help them better manage their symptoms.
"I think that pulmonary rehabilitation is one of the first interventions that we should be recommending for our patients," Dr. Garfield said. "It's physical therapy for patients with chronic lung diseases, backed by respiratory therapists, and it offers not only physical rehabilitation - improving strength and coordination, but also it helps our patients get as much as possible out of what they've got."
For example, patients can be taught how to decrease their respiratory rate when they're feeling a sense of urgency or panic. Patients can also learn how to change body positions to help them breathe more effectively when they feel that their breath is limited or restricted, she said.
"Once your into medical interventions, pulmonary rehab is phenomenal," Dr. Saleh said.
Pulmonary rehabilitation helps patients to feel better about themselves and about their abilities, but "unfortunately it's not as available as we like," he said.
Many patients don't live near a pulmonary rehabilitation center, and the typical two to three weekly sessions for 4 to 12 weeks or longer can be a significant burden for patients and caregivers, he acknowledged.
"You have to sit [with the patient] and be honest and tell them it's a lot of diligence involved and you have to be really motivated," he said.
Other treatment options include pharmacological therapy with antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and anxiolytic agents.
"SSRIs are the current first-line drug treatment for depression, and have been shown to significantly improve depression and anxiety in patients with COPD in some, but not all, trials published to date. However, it is important to note that a diagnosis of bipolar disorder must be ruled out before initiating standard antidepressant therapy," Dr. Johannes and colleagues wrote.
Defiant joy
Importantly, even with the burden of life with COPD, many patients found ways to experience what Strang et al called "a defiant joy."
"It was remarkable that when the patients were asked about what gave their lives meaning today, many talked about what had given their life meaning in the past, prior to becoming ill. In the light of the things they had lost because of the disease, many felt that their previous sources of joy no longer existed. Despite this, many still hoped to be able to get out into the fresh air, to be able to do errands or that tomorrow might be better," the investigators wrote.
Dr. Yohannes, Dr. Garfield, and Dr. Saleh all reported having no relevant conflicts of interest to report.
Many patients with chronic progressive pulmonary disease feel anxious and depressed as their conditions advance, as breathing becomes increasingly labored and difficult, and as performing even small daily tasks leaves them exhausted.
Persons with severe COPD frequently report fears of suffocation and death, as well as anxieties about abandoning family and friends, and these negative, intrusive thoughts can have an adverse effect on COPD outcomes.
Disease-related mental distress can lead to increased disability, more frequent use of costly health care resources, higher morbidity, and elevated risk of death, investigators say.
"Individuals with severe COPD are twice as likely to develop depression than patients with mild COPD. Prevalence rates for clinical anxiety in COPD range from 13% to 46% in outpatients and 10% to 55% among inpatients," wrote Abebaw Mengitsu Yohannes, PhD, then from Azusa Pacific University in Azusa, California and colleagues in an article published jointly by The Journal of Family Practice and The Cleveland Clinic Journal of Medicine.
Patients with COPD may experience major depressive disorders, chronic mild depression (dysthymias), and minor depression, as well as generalized anxiety disorder, phobias, and panic disorders, the investigators say.
"Growing evidence suggests that the relationship between mood disorders, particularly depression, and COPD is bidirectional, meaning that mood disorders adversely impact prognosis in COPD, whereas COPD increases the risk of developing depression," Yohannes et al wrote.
Jamie Garfield, MD, professor of thoracic medicine and surgery at Temple University's Lewis Katz School of Medicine in Philadelphia, told Chest Physician that the association between severe chronic diseases and mood disorders is well known.
"I don't think that it's specific to chronic lung diseases; in people with chronic heart disease or malignancies we see that co-existence of depression and anxiety will worsen the course of disease," she said.
Dr. Johannes, who is currently a professor of physical therapy at the University of Alabama School of Health Professionals in Birmingham, said that depression and anxiety are often underdiagnosed and undertreated in patients with obstructive pulmonary diseases because the conditions can share symptoms such as dyspnea (for example, in anxiety) or fatigue (in depression).
"Therefore, unless one begins to explore further, it's hard for physicians to be able to identify these conditions," he said in an interview with Chest Physician.
Fears of dying (and living)
The causes of depression and anxiety among patients with obstructive pulmonary disorders are multi-factorial, and may require a variety of treatment and coping strategies, according to Susann Strang, RN, PhD, and colleagues from the University of Gothenburg, Sweden.
They conducted qualitative in-depth interviews with 31 men and women with stage III or IV COPD, and found that the majority of patients had anxiety associated with their disease.
"Analyses revealed three major themes: death anxiety, life anxiety, and counterweights to anxiety," the investigators wrote in a study published in the journal Palliative and Supportive Care in 2014.
Factors contributing to anxiety surrounding death included fear of suffocation, awareness of impending death, fear of the process of death, and anxiety about being separated from loved ones.
In contrast, some patients expressed dread of living with the limitations and loneliness imposed on them by their disease, so called "life anxiety."
The patients also reported "counterweights" to anxiety as a way of coping. For some this involved trust in their health care professionals and adherence to medication, inhalers, and supplemental oxygen.
"The patients also placed hope in new treatments, better medication, surgery, stem cell treatment, or lung transplants," Dr. Strang and colleagues reported.
Others reported avoiding talking about death, sleeping more, or using humor to "laugh off this difficult subject."
Screening and diagnosis
Primary care practitioners are often the first health professionals that patients with COPD see, but these clinicians often don't have the time to add screening to their already crammed schedules. In addition, "the lack of a standardized approach in diagnosis, and inadequate knowledge or confidence in assessing psychological status (particularly given the number of strategies available for screening patients for mood disorders)," can make it difficult for PCPs to detect and manage anxiety and depression in their patients with significant health care burdens from COPD and other obstructive lung diseases, Dr. Yohannes and colleagues noted.
In addition to commonly used screening tools for anxiety and depression such as the Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire (PHQ-9), there are at least two designed to evaluate patients with lung disease: the Anxiety Inventory for Respiratory (AIR) Disease scale, developed by Dr. Johannes and colleagues, and the COPD Anxiety Questionnaire.
The COPD Assessment Testand Clinical COPD Questionnaire, while not specifically designed to screen for mental disorders, include questions that can point to symptoms of distress in patients with COPD, Dr. Yohannes said.
"In truth I think that there are few providers who will routinely do this on all their patients in terms of quantifying the severity or the presence or absence of depression, but in my own practice I very much ask questions that align with the questions in these tools to determine whether my patient appears to have high levels of anxiety and depression," Dr. Garfield said.
Listen to patients and families
Among the most powerful tools that clinicians have at their disposal for treating anxiety and depression in patients with chronic lung disease are their ears and their minds, said Anthony Saleh, MD, a pulmonologist at New York-Presbyterian Brooklyn Methodist Hospital in Brooklyn, New York.
"I think just listening to the patient, that's a little bit forgotten yet so important," he said in an interview with Chest Physician.
"When I have someone with advanced lung disease, like idiopathic pulmonary fibrosis, like advanced emphysema, one of the most important things I think is to listen to the patient, and not just to listen to the answers of your perfunctory 'how's your breathing? Any chest pain?' and those sort of rote medical questions, but listen to their thoughts, and it will given them a safe space to say 'Hey, I'm nervous, hey I'm worried about my family, hey I'm worried if I die what's going to happen to my wife and kids,' and that's something I think is invaluable."
It's also vital to listen to the concerns of the patients family members, who may be the primary caregivers and may share the patient's stresses and anxieties, he said.
Pulmonary Rehabilitation
All of the experts interviewed for this article agreed that a combination of medical, social and mental health support services is important for treatment for patients with chronic obstructive lung diseases.
One of the most effective means of helping patients with both acute breathing problems and with disease-related anxiety and depression is pulmonary rehabilitation. Depending on disease severity, this multidisciplinary approach may involve exercise, patient education, psychological and nutrition counseling, and training patients how to conserve energy and adopt breathing strategies to help them better manage their symptoms.
"I think that pulmonary rehabilitation is one of the first interventions that we should be recommending for our patients," Dr. Garfield said. "It's physical therapy for patients with chronic lung diseases, backed by respiratory therapists, and it offers not only physical rehabilitation - improving strength and coordination, but also it helps our patients get as much as possible out of what they've got."
For example, patients can be taught how to decrease their respiratory rate when they're feeling a sense of urgency or panic. Patients can also learn how to change body positions to help them breathe more effectively when they feel that their breath is limited or restricted, she said.
"Once your into medical interventions, pulmonary rehab is phenomenal," Dr. Saleh said.
Pulmonary rehabilitation helps patients to feel better about themselves and about their abilities, but "unfortunately it's not as available as we like," he said.
Many patients don't live near a pulmonary rehabilitation center, and the typical two to three weekly sessions for 4 to 12 weeks or longer can be a significant burden for patients and caregivers, he acknowledged.
"You have to sit [with the patient] and be honest and tell them it's a lot of diligence involved and you have to be really motivated," he said.
Other treatment options include pharmacological therapy with antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and anxiolytic agents.
"SSRIs are the current first-line drug treatment for depression, and have been shown to significantly improve depression and anxiety in patients with COPD in some, but not all, trials published to date. However, it is important to note that a diagnosis of bipolar disorder must be ruled out before initiating standard antidepressant therapy," Dr. Johannes and colleagues wrote.
Defiant joy
Importantly, even with the burden of life with COPD, many patients found ways to experience what Strang et al called "a defiant joy."
"It was remarkable that when the patients were asked about what gave their lives meaning today, many talked about what had given their life meaning in the past, prior to becoming ill. In the light of the things they had lost because of the disease, many felt that their previous sources of joy no longer existed. Despite this, many still hoped to be able to get out into the fresh air, to be able to do errands or that tomorrow might be better," the investigators wrote.
Dr. Yohannes, Dr. Garfield, and Dr. Saleh all reported having no relevant conflicts of interest to report.
Older Age Confers a Higher Risk for Second Primary Melanoma: Study
TOPLINE:
.
METHODOLOGY:
- Knowledge about one’s risk for a second primary invasive melanoma over time remains incomplete.
- Using data from the Cancer Registry of Norway, researchers performed a cohort study of 19,196 individuals diagnosed with invasive melanomas during 2008-2020; 51% were women. The mean age at the first primary melanoma diagnosis was 62 years.
- The main outcome of interest was the incidence rate of second primary invasive melanoma after the first diagnosis.
- The researchers used accelerated failure time models to examine potential associations with patient and tumor characteristics. They also calculated the median time between first and second melanomas and the likelihood of second primary melanomas on the same or different site as the first primary melanoma.
TAKEAWAY:
- The incidence rate of a second primary melanoma in the year following a first primary melanoma was 16.8 (95% CI, 14.9-18.7) per 1000 person-years. This decreased to 7.3 (95% CI, 6.0-8.6) per 1000 person-years during the second year and remained stable after that.
- Patient age influenced the median time between first and second primaries. The median interval was 37 months (95% CI, 8-49) in patients aged < 40 years, 18 months (95% CI, 13-24) in patients aged 50-59 years, and 11 months (95% CI, 7-18) in patients aged ≥ 80 years.
- The body site of the second primary melanoma was the same as the first primary in 47% of patients but was located on a different body site in the remaining 53% of patients.
- Among patients who developed a second primary melanoma on the same site as the first, the median interval was shorter for men compared with women: A median of 12 (95% CI, 7-19) months vs 22 (95% CI, 11-35) months, respectively.
IN PRACTICE:
“Our findings suggest that increased surveillance may be considered for older patients, especially men, for at least the first 3 years after their initial diagnosis, regardless of the characteristics of their first melanoma,” the authors wrote.
SOURCE:
Corresponding author Reza Ghiasvand, PhD, of the Oslo Centre for Biostatistics and Epidemiology, Oslo University Hospital, Oslo, Norway, and colleagues conducted the research, published online on February 28, 2024, in JAMA Dermatology.
LIMITATIONS:
Information was lacking on phenotypic characteristics, personal ultraviolet radiation (UVR) exposure, genetic factors, and the number of follow-up skin examinations.
DISCLOSURES:
The study was supported by the South-Eastern Norway Regional Health Authority. The authors reported having no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Knowledge about one’s risk for a second primary invasive melanoma over time remains incomplete.
- Using data from the Cancer Registry of Norway, researchers performed a cohort study of 19,196 individuals diagnosed with invasive melanomas during 2008-2020; 51% were women. The mean age at the first primary melanoma diagnosis was 62 years.
- The main outcome of interest was the incidence rate of second primary invasive melanoma after the first diagnosis.
- The researchers used accelerated failure time models to examine potential associations with patient and tumor characteristics. They also calculated the median time between first and second melanomas and the likelihood of second primary melanomas on the same or different site as the first primary melanoma.
TAKEAWAY:
- The incidence rate of a second primary melanoma in the year following a first primary melanoma was 16.8 (95% CI, 14.9-18.7) per 1000 person-years. This decreased to 7.3 (95% CI, 6.0-8.6) per 1000 person-years during the second year and remained stable after that.
- Patient age influenced the median time between first and second primaries. The median interval was 37 months (95% CI, 8-49) in patients aged < 40 years, 18 months (95% CI, 13-24) in patients aged 50-59 years, and 11 months (95% CI, 7-18) in patients aged ≥ 80 years.
- The body site of the second primary melanoma was the same as the first primary in 47% of patients but was located on a different body site in the remaining 53% of patients.
- Among patients who developed a second primary melanoma on the same site as the first, the median interval was shorter for men compared with women: A median of 12 (95% CI, 7-19) months vs 22 (95% CI, 11-35) months, respectively.
IN PRACTICE:
“Our findings suggest that increased surveillance may be considered for older patients, especially men, for at least the first 3 years after their initial diagnosis, regardless of the characteristics of their first melanoma,” the authors wrote.
SOURCE:
Corresponding author Reza Ghiasvand, PhD, of the Oslo Centre for Biostatistics and Epidemiology, Oslo University Hospital, Oslo, Norway, and colleagues conducted the research, published online on February 28, 2024, in JAMA Dermatology.
LIMITATIONS:
Information was lacking on phenotypic characteristics, personal ultraviolet radiation (UVR) exposure, genetic factors, and the number of follow-up skin examinations.
DISCLOSURES:
The study was supported by the South-Eastern Norway Regional Health Authority. The authors reported having no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Knowledge about one’s risk for a second primary invasive melanoma over time remains incomplete.
- Using data from the Cancer Registry of Norway, researchers performed a cohort study of 19,196 individuals diagnosed with invasive melanomas during 2008-2020; 51% were women. The mean age at the first primary melanoma diagnosis was 62 years.
- The main outcome of interest was the incidence rate of second primary invasive melanoma after the first diagnosis.
- The researchers used accelerated failure time models to examine potential associations with patient and tumor characteristics. They also calculated the median time between first and second melanomas and the likelihood of second primary melanomas on the same or different site as the first primary melanoma.
TAKEAWAY:
- The incidence rate of a second primary melanoma in the year following a first primary melanoma was 16.8 (95% CI, 14.9-18.7) per 1000 person-years. This decreased to 7.3 (95% CI, 6.0-8.6) per 1000 person-years during the second year and remained stable after that.
- Patient age influenced the median time between first and second primaries. The median interval was 37 months (95% CI, 8-49) in patients aged < 40 years, 18 months (95% CI, 13-24) in patients aged 50-59 years, and 11 months (95% CI, 7-18) in patients aged ≥ 80 years.
- The body site of the second primary melanoma was the same as the first primary in 47% of patients but was located on a different body site in the remaining 53% of patients.
- Among patients who developed a second primary melanoma on the same site as the first, the median interval was shorter for men compared with women: A median of 12 (95% CI, 7-19) months vs 22 (95% CI, 11-35) months, respectively.
IN PRACTICE:
“Our findings suggest that increased surveillance may be considered for older patients, especially men, for at least the first 3 years after their initial diagnosis, regardless of the characteristics of their first melanoma,” the authors wrote.
SOURCE:
Corresponding author Reza Ghiasvand, PhD, of the Oslo Centre for Biostatistics and Epidemiology, Oslo University Hospital, Oslo, Norway, and colleagues conducted the research, published online on February 28, 2024, in JAMA Dermatology.
LIMITATIONS:
Information was lacking on phenotypic characteristics, personal ultraviolet radiation (UVR) exposure, genetic factors, and the number of follow-up skin examinations.
DISCLOSURES:
The study was supported by the South-Eastern Norway Regional Health Authority. The authors reported having no disclosures.
A version of this article appeared on Medscape.com.
Study Evaluates Factors Driving Fatigue in Patients With Psoriasis, PsA
TOPLINE:
Many factors may influence fatigue in patients with psoriasis and psoriatic arthritis (PsA), researchers report.
METHODOLOGY:
- The individual components of fatigue in psoriasis and PsA have not been examined thoroughly.
- Researchers drew from the nationwide prospective Danish Skin Cohort to identify 2741 adults with dermatologist-diagnosed psoriasis (of which 593 also had PsA) and 3788 controls in the general population.
- All adults in the analysis completed the multidimensional fatigue inventory (MIF-20), a validated 20-item tool that measures five dimensions of fatigue: General fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue. A higher score indicates more severe fatigue.
- All adults were also asked about their current intensity of joint pain over the previous 7 days, severity of pruritus and skin pain over the previous 24 hours, and sleep problems over the previous 72 hours on a numerical rating scale (NRS). The researchers applied linear regression models to continuous outcomes and adjusted for age, sex, socioeconomic status, psoriasis severity, and joint pain intensity, and beta coefficients (β) for the slopes were estimated with 95% CIs.
TAKEAWAY:
- Compared with the general population, higher total MFI-20 scores were observed for psoriasis and PsA, respectively. However, on the adjusted analysis, the impact on total fatigue was greatest for those with PsA (β = 5.23; 95% CI, 3.55-6.90), followed by psoriasis (β = 2.10; 95% CI, 0.96-3.25) compared with the general population (P trend < .0001).
- Increasing age was associated with a lower impact on total fatigue in psoriasis (β = −0.13; 95% CI, −0.18 to −0.08) and in PsA (β = −0.10; 95% CI, −0.19 to −0.01).
- Among patients with psoriasis with or without PsA, increasing joint pain intensity was associated with overall fatigue (β = 2.23; 95% CI, 2.03-2.44) for each one-point increase in joint pain on the NRS.
- In other findings, greater intensity of itch was associated with higher fatigue scores for both psoriasis and PsA, while skin pain was significantly associated with fatigue in PsA (β = 0.65; 95% CI, 0.08-1.22) but not in psoriasis without PsA (P = .2043).
IN PRACTICE:
“The when treating psoriasis, rather than focusing on objective severity measures alone,” the authors wrote.
SOURCE:
Corresponding author Alexander Egeberg, MD, of the Department of Dermatology at Bispebjerg Hospital, University of Copenhagen, Copenhagen, Denmark, and colleagues conducted the research, which was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The researchers were unable to assess whether the pain was inflammatory or noninflammatory or the number of affected joints. They also lacked information about the use of methotrexate, which commonly causes fatigue.
DISCLOSURES:
Dr. Egeberg is now an employee at LEO Pharma. He has received research funding from Pfizer, Eli Lilly, the Danish National Psoriasis Foundation, and the Royal Hofbundtmager Aage Bang Foundation, and honoraria as a consultant and/or speaker from AbbVie, Almirall, Bristol-Myers Squibb, Leo Pharma, Samsung Bioepis Co., Ltd., Pfizer, Eli Lilly, Novartis, UCB, Union Therapeutics, Horizon Therapeutics, Galderma, and Janssen Pharmaceuticals. Three of the coauthors reported being a consultant to, an adviser for, and/or having received research support from many pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Many factors may influence fatigue in patients with psoriasis and psoriatic arthritis (PsA), researchers report.
METHODOLOGY:
- The individual components of fatigue in psoriasis and PsA have not been examined thoroughly.
- Researchers drew from the nationwide prospective Danish Skin Cohort to identify 2741 adults with dermatologist-diagnosed psoriasis (of which 593 also had PsA) and 3788 controls in the general population.
- All adults in the analysis completed the multidimensional fatigue inventory (MIF-20), a validated 20-item tool that measures five dimensions of fatigue: General fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue. A higher score indicates more severe fatigue.
- All adults were also asked about their current intensity of joint pain over the previous 7 days, severity of pruritus and skin pain over the previous 24 hours, and sleep problems over the previous 72 hours on a numerical rating scale (NRS). The researchers applied linear regression models to continuous outcomes and adjusted for age, sex, socioeconomic status, psoriasis severity, and joint pain intensity, and beta coefficients (β) for the slopes were estimated with 95% CIs.
TAKEAWAY:
- Compared with the general population, higher total MFI-20 scores were observed for psoriasis and PsA, respectively. However, on the adjusted analysis, the impact on total fatigue was greatest for those with PsA (β = 5.23; 95% CI, 3.55-6.90), followed by psoriasis (β = 2.10; 95% CI, 0.96-3.25) compared with the general population (P trend < .0001).
- Increasing age was associated with a lower impact on total fatigue in psoriasis (β = −0.13; 95% CI, −0.18 to −0.08) and in PsA (β = −0.10; 95% CI, −0.19 to −0.01).
- Among patients with psoriasis with or without PsA, increasing joint pain intensity was associated with overall fatigue (β = 2.23; 95% CI, 2.03-2.44) for each one-point increase in joint pain on the NRS.
- In other findings, greater intensity of itch was associated with higher fatigue scores for both psoriasis and PsA, while skin pain was significantly associated with fatigue in PsA (β = 0.65; 95% CI, 0.08-1.22) but not in psoriasis without PsA (P = .2043).
IN PRACTICE:
“The when treating psoriasis, rather than focusing on objective severity measures alone,” the authors wrote.
SOURCE:
Corresponding author Alexander Egeberg, MD, of the Department of Dermatology at Bispebjerg Hospital, University of Copenhagen, Copenhagen, Denmark, and colleagues conducted the research, which was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The researchers were unable to assess whether the pain was inflammatory or noninflammatory or the number of affected joints. They also lacked information about the use of methotrexate, which commonly causes fatigue.
DISCLOSURES:
Dr. Egeberg is now an employee at LEO Pharma. He has received research funding from Pfizer, Eli Lilly, the Danish National Psoriasis Foundation, and the Royal Hofbundtmager Aage Bang Foundation, and honoraria as a consultant and/or speaker from AbbVie, Almirall, Bristol-Myers Squibb, Leo Pharma, Samsung Bioepis Co., Ltd., Pfizer, Eli Lilly, Novartis, UCB, Union Therapeutics, Horizon Therapeutics, Galderma, and Janssen Pharmaceuticals. Three of the coauthors reported being a consultant to, an adviser for, and/or having received research support from many pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Many factors may influence fatigue in patients with psoriasis and psoriatic arthritis (PsA), researchers report.
METHODOLOGY:
- The individual components of fatigue in psoriasis and PsA have not been examined thoroughly.
- Researchers drew from the nationwide prospective Danish Skin Cohort to identify 2741 adults with dermatologist-diagnosed psoriasis (of which 593 also had PsA) and 3788 controls in the general population.
- All adults in the analysis completed the multidimensional fatigue inventory (MIF-20), a validated 20-item tool that measures five dimensions of fatigue: General fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue. A higher score indicates more severe fatigue.
- All adults were also asked about their current intensity of joint pain over the previous 7 days, severity of pruritus and skin pain over the previous 24 hours, and sleep problems over the previous 72 hours on a numerical rating scale (NRS). The researchers applied linear regression models to continuous outcomes and adjusted for age, sex, socioeconomic status, psoriasis severity, and joint pain intensity, and beta coefficients (β) for the slopes were estimated with 95% CIs.
TAKEAWAY:
- Compared with the general population, higher total MFI-20 scores were observed for psoriasis and PsA, respectively. However, on the adjusted analysis, the impact on total fatigue was greatest for those with PsA (β = 5.23; 95% CI, 3.55-6.90), followed by psoriasis (β = 2.10; 95% CI, 0.96-3.25) compared with the general population (P trend < .0001).
- Increasing age was associated with a lower impact on total fatigue in psoriasis (β = −0.13; 95% CI, −0.18 to −0.08) and in PsA (β = −0.10; 95% CI, −0.19 to −0.01).
- Among patients with psoriasis with or without PsA, increasing joint pain intensity was associated with overall fatigue (β = 2.23; 95% CI, 2.03-2.44) for each one-point increase in joint pain on the NRS.
- In other findings, greater intensity of itch was associated with higher fatigue scores for both psoriasis and PsA, while skin pain was significantly associated with fatigue in PsA (β = 0.65; 95% CI, 0.08-1.22) but not in psoriasis without PsA (P = .2043).
IN PRACTICE:
“The when treating psoriasis, rather than focusing on objective severity measures alone,” the authors wrote.
SOURCE:
Corresponding author Alexander Egeberg, MD, of the Department of Dermatology at Bispebjerg Hospital, University of Copenhagen, Copenhagen, Denmark, and colleagues conducted the research, which was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The researchers were unable to assess whether the pain was inflammatory or noninflammatory or the number of affected joints. They also lacked information about the use of methotrexate, which commonly causes fatigue.
DISCLOSURES:
Dr. Egeberg is now an employee at LEO Pharma. He has received research funding from Pfizer, Eli Lilly, the Danish National Psoriasis Foundation, and the Royal Hofbundtmager Aage Bang Foundation, and honoraria as a consultant and/or speaker from AbbVie, Almirall, Bristol-Myers Squibb, Leo Pharma, Samsung Bioepis Co., Ltd., Pfizer, Eli Lilly, Novartis, UCB, Union Therapeutics, Horizon Therapeutics, Galderma, and Janssen Pharmaceuticals. Three of the coauthors reported being a consultant to, an adviser for, and/or having received research support from many pharmaceutical companies.
A version of this article appeared on Medscape.com.
Be Wary of TikTok Content on Infantile Hemangiomas: Study
TOPLINE:
.
METHODOLOGY:
- New parents may turn to TikTok for information about IHs, but little is known about the quality of videos on the social media platform related to the topic.
- Using the search term “hemangioma,” researchers reviewed the top 50 English-language TikTok videos that resulted from the query in November 2022.
- The researchers analyzed the videos for their content source, accuracy, and purpose and used Infantile Hemangioma Referral Score criteria to determine if the lesions pictured on the videos met criteria for referral to a specialist or not.
TAKEAWAY:
- Combined, the 50 videos were viewed 25.1 million times, had 2.6 million likes, and received 17,600 comments.
- Only 36 were considered likely to be IH. Of those 36 videos, the researchers deemed 33 (92%) to be potentially problematic, meriting referral to a specialist. The remaining three lesions could not be classified because of insufficient information.
- Of the 50 videos, 45 were created by individuals personally affected by IH (parents of a child with IH or young adults living with residual impacts), and only three were created by physicians (two by plastic surgeons and one by a neonatologist).
- In terms of content, 2 of the 45 videos created by someone personally affected by IH contained inaccurate information, while all three of videos created by physicians contained inaccurate information, such as oversimplification of the prognosis or incorrect nomenclature.
IN PRACTICE:
“Providers should be aware that TikTok may be useful for promoting birthmark awareness, but that it should not be relied on for accurate information about IHs,” the authors wrote.
SOURCE:
First author Sonora Yun, a medical student at Columbia University College of Physicians and Surgeons, New York City, conducted the research with Maria C. Garzon, MD, and Kimberly D. Morel, MD, who are board-certified pediatric dermatologists at Columbia. The study was published in Pediatric Dermatology.
LIMITATIONS:
The authors noted no specific limitations to the study.
DISCLOSURES:
The researchers reported having no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- New parents may turn to TikTok for information about IHs, but little is known about the quality of videos on the social media platform related to the topic.
- Using the search term “hemangioma,” researchers reviewed the top 50 English-language TikTok videos that resulted from the query in November 2022.
- The researchers analyzed the videos for their content source, accuracy, and purpose and used Infantile Hemangioma Referral Score criteria to determine if the lesions pictured on the videos met criteria for referral to a specialist or not.
TAKEAWAY:
- Combined, the 50 videos were viewed 25.1 million times, had 2.6 million likes, and received 17,600 comments.
- Only 36 were considered likely to be IH. Of those 36 videos, the researchers deemed 33 (92%) to be potentially problematic, meriting referral to a specialist. The remaining three lesions could not be classified because of insufficient information.
- Of the 50 videos, 45 were created by individuals personally affected by IH (parents of a child with IH or young adults living with residual impacts), and only three were created by physicians (two by plastic surgeons and one by a neonatologist).
- In terms of content, 2 of the 45 videos created by someone personally affected by IH contained inaccurate information, while all three of videos created by physicians contained inaccurate information, such as oversimplification of the prognosis or incorrect nomenclature.
IN PRACTICE:
“Providers should be aware that TikTok may be useful for promoting birthmark awareness, but that it should not be relied on for accurate information about IHs,” the authors wrote.
SOURCE:
First author Sonora Yun, a medical student at Columbia University College of Physicians and Surgeons, New York City, conducted the research with Maria C. Garzon, MD, and Kimberly D. Morel, MD, who are board-certified pediatric dermatologists at Columbia. The study was published in Pediatric Dermatology.
LIMITATIONS:
The authors noted no specific limitations to the study.
DISCLOSURES:
The researchers reported having no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- New parents may turn to TikTok for information about IHs, but little is known about the quality of videos on the social media platform related to the topic.
- Using the search term “hemangioma,” researchers reviewed the top 50 English-language TikTok videos that resulted from the query in November 2022.
- The researchers analyzed the videos for their content source, accuracy, and purpose and used Infantile Hemangioma Referral Score criteria to determine if the lesions pictured on the videos met criteria for referral to a specialist or not.
TAKEAWAY:
- Combined, the 50 videos were viewed 25.1 million times, had 2.6 million likes, and received 17,600 comments.
- Only 36 were considered likely to be IH. Of those 36 videos, the researchers deemed 33 (92%) to be potentially problematic, meriting referral to a specialist. The remaining three lesions could not be classified because of insufficient information.
- Of the 50 videos, 45 were created by individuals personally affected by IH (parents of a child with IH or young adults living with residual impacts), and only three were created by physicians (two by plastic surgeons and one by a neonatologist).
- In terms of content, 2 of the 45 videos created by someone personally affected by IH contained inaccurate information, while all three of videos created by physicians contained inaccurate information, such as oversimplification of the prognosis or incorrect nomenclature.
IN PRACTICE:
“Providers should be aware that TikTok may be useful for promoting birthmark awareness, but that it should not be relied on for accurate information about IHs,” the authors wrote.
SOURCE:
First author Sonora Yun, a medical student at Columbia University College of Physicians and Surgeons, New York City, conducted the research with Maria C. Garzon, MD, and Kimberly D. Morel, MD, who are board-certified pediatric dermatologists at Columbia. The study was published in Pediatric Dermatology.
LIMITATIONS:
The authors noted no specific limitations to the study.
DISCLOSURES:
The researchers reported having no disclosures.
A version of this article appeared on Medscape.com.
‘Remarkable’ Study Tracks Timeline of Biomarker Changes 20 Years Before Alzheimer’s disease
, something that hasn’t previously been extensively investigated in longitudinal studies.
By analyzing cerebral spinal fluid (CSF), as well as cognitive and brain imaging assessments conducted every few years for two decades, researchers were able to plot the course of changing levels of amyloid-beta 42 (Abeta42), phosphorylated tau 181 (p-tau181), and neurofilament light chain (NfL) in adults with Alzheimer’s disease and mark when those levels began to deviate from those of adults without Alzheimer’s disease.
Levels of Abeta42 in CSF and the ratio of Abeta42 to Abeta40 in people who developed Alzheimer’s disease diverged from those of peers who remained cognitively normal at 18 years and 14 years, respectively, before clinical signs of disease appeared.
The level of p-tau181 in CSF increased 11 years before disease onset, and NfL levels, a measure of neurodegeneration, increased 9 years before diagnosis.
These changes were followed by hippocampal atrophy and cognitive decline a few years later.
The results also show “an apparent accelerated change in concentrations of CSF biomarkers followed by a slowing of this change up to the time of diagnosis,” report the authors, led by Jianping Jia, MD, PhD, with the Innovation Center for Neurological Disorders, Xuanwu Hospital, Capital Medical University, Beijing, China.
The study was published online in The New England Journal of Medicine.
Time Course of Biomarker Changes
Dr. Jia and colleagues conducted a nested case-control study within the China Cognition and Aging Study (COAST). They matched 648 adults who developed Alzheimer’s disease to 648 who remained cognitively normal. CSF, cognitive, and brain imaging assessments were performed every 2-3 years for a median of about 20 years.
Within both groups, men slightly outnumbered women. At baseline, CSF biomarker levels, cognitive scores, and hippocampal volumes were similar in the two groups. Adults who developed Alzheimer’s disease were more likely than their matched controls to be carriers of the APOE epsilon-4 allele (37% vs 20%).
In terms of CSF Abeta42, the level of this biomarker in those who developed Alzheimer’s disease diverged from the level in controls an estimated 18 years before clinical diagnosis. At that time, the level was lower by a mean 59.13 pg/mL in the Alzheimer’s disease group.
A difference in the ratio of CSF Abeta42 to Abeta40 between the two groups appeared an estimated 14 years before the diagnosis of Alzheimer’s disease (difference in mean values, −0.01 pg/mL).
Differences between the two groups in CSF p-tau181 and total tau concentrations were apparent roughly 11 and 10 years before diagnosis, respectively. At those times, the mean differences in p-tau181 and total tau concentrations were 7.10 pg/mL and 87.10 pg/mL, respectively.
In terms of NfL, a difference between the groups was observed 9 years before diagnosis, with its trajectory progressively deviating from the concentrations observed in cognitively normal groups at that time, to a final mean difference in NfL of 228.29 pg/mL.
Bilateral hippocampal volume decreased with age in both groups. However, the decrease began to differ between the two groups 8 years before Alzheimer’s disease diagnosis, at which time volume was lower by 358.94 mm3 in the Alzheimer’s disease group compared with the control group.
Average Clinical Dementia Rating–Sum of Boxes (CDR-SB) scores in the Alzheimer’s disease group began to worsen compared with the control group at about 6 years before diagnosis.
As Alzheimer’s disease progressed, changes in CSF biomarkers increased before reaching a plateau.
Important Contribution
In a linked editorial, Richard Mayeux, MD, Department of Neurology, Columbia University, New York, said the importance of this work “cannot be overstated. Knowledge of the timing of these physiological events is critical to provide clinicians with useful starting points for prevention and therapeutic strategies.”
Dr. Mayeux said this “remarkable” longitudinal study spanning 2 decades “not only confirms the hypotheses of previous investigators but extends and validates the sequence of changes” in sporadic Alzheimer’s disease.
Dr. Mayeux acknowledged that one might consider the finding in this study to be limited owing to the inclusion of only individuals of Han Chinese ancestry.
However, longitudinal studies of plasma biomarkers in individuals of Asian, European, African, and Hispanic ancestry have shown similar trends in biomarker changes preceding the onset of Alzheimer’s disease, he noted.
“Ethnic variation in these biomarkers is known, but that fact does not lessen the effect of the results reported. It merely highlights that similar studies must continue and must be inclusive of other groups,” Dr. Mayeux concluded.
The study had no commercial funding. Disclosures for authors and editorialist are available at NEJM.org.
A version of this article appeared on Medscape.com.
, something that hasn’t previously been extensively investigated in longitudinal studies.
By analyzing cerebral spinal fluid (CSF), as well as cognitive and brain imaging assessments conducted every few years for two decades, researchers were able to plot the course of changing levels of amyloid-beta 42 (Abeta42), phosphorylated tau 181 (p-tau181), and neurofilament light chain (NfL) in adults with Alzheimer’s disease and mark when those levels began to deviate from those of adults without Alzheimer’s disease.
Levels of Abeta42 in CSF and the ratio of Abeta42 to Abeta40 in people who developed Alzheimer’s disease diverged from those of peers who remained cognitively normal at 18 years and 14 years, respectively, before clinical signs of disease appeared.
The level of p-tau181 in CSF increased 11 years before disease onset, and NfL levels, a measure of neurodegeneration, increased 9 years before diagnosis.
These changes were followed by hippocampal atrophy and cognitive decline a few years later.
The results also show “an apparent accelerated change in concentrations of CSF biomarkers followed by a slowing of this change up to the time of diagnosis,” report the authors, led by Jianping Jia, MD, PhD, with the Innovation Center for Neurological Disorders, Xuanwu Hospital, Capital Medical University, Beijing, China.
The study was published online in The New England Journal of Medicine.
Time Course of Biomarker Changes
Dr. Jia and colleagues conducted a nested case-control study within the China Cognition and Aging Study (COAST). They matched 648 adults who developed Alzheimer’s disease to 648 who remained cognitively normal. CSF, cognitive, and brain imaging assessments were performed every 2-3 years for a median of about 20 years.
Within both groups, men slightly outnumbered women. At baseline, CSF biomarker levels, cognitive scores, and hippocampal volumes were similar in the two groups. Adults who developed Alzheimer’s disease were more likely than their matched controls to be carriers of the APOE epsilon-4 allele (37% vs 20%).
In terms of CSF Abeta42, the level of this biomarker in those who developed Alzheimer’s disease diverged from the level in controls an estimated 18 years before clinical diagnosis. At that time, the level was lower by a mean 59.13 pg/mL in the Alzheimer’s disease group.
A difference in the ratio of CSF Abeta42 to Abeta40 between the two groups appeared an estimated 14 years before the diagnosis of Alzheimer’s disease (difference in mean values, −0.01 pg/mL).
Differences between the two groups in CSF p-tau181 and total tau concentrations were apparent roughly 11 and 10 years before diagnosis, respectively. At those times, the mean differences in p-tau181 and total tau concentrations were 7.10 pg/mL and 87.10 pg/mL, respectively.
In terms of NfL, a difference between the groups was observed 9 years before diagnosis, with its trajectory progressively deviating from the concentrations observed in cognitively normal groups at that time, to a final mean difference in NfL of 228.29 pg/mL.
Bilateral hippocampal volume decreased with age in both groups. However, the decrease began to differ between the two groups 8 years before Alzheimer’s disease diagnosis, at which time volume was lower by 358.94 mm3 in the Alzheimer’s disease group compared with the control group.
Average Clinical Dementia Rating–Sum of Boxes (CDR-SB) scores in the Alzheimer’s disease group began to worsen compared with the control group at about 6 years before diagnosis.
As Alzheimer’s disease progressed, changes in CSF biomarkers increased before reaching a plateau.
Important Contribution
In a linked editorial, Richard Mayeux, MD, Department of Neurology, Columbia University, New York, said the importance of this work “cannot be overstated. Knowledge of the timing of these physiological events is critical to provide clinicians with useful starting points for prevention and therapeutic strategies.”
Dr. Mayeux said this “remarkable” longitudinal study spanning 2 decades “not only confirms the hypotheses of previous investigators but extends and validates the sequence of changes” in sporadic Alzheimer’s disease.
Dr. Mayeux acknowledged that one might consider the finding in this study to be limited owing to the inclusion of only individuals of Han Chinese ancestry.
However, longitudinal studies of plasma biomarkers in individuals of Asian, European, African, and Hispanic ancestry have shown similar trends in biomarker changes preceding the onset of Alzheimer’s disease, he noted.
“Ethnic variation in these biomarkers is known, but that fact does not lessen the effect of the results reported. It merely highlights that similar studies must continue and must be inclusive of other groups,” Dr. Mayeux concluded.
The study had no commercial funding. Disclosures for authors and editorialist are available at NEJM.org.
A version of this article appeared on Medscape.com.
, something that hasn’t previously been extensively investigated in longitudinal studies.
By analyzing cerebral spinal fluid (CSF), as well as cognitive and brain imaging assessments conducted every few years for two decades, researchers were able to plot the course of changing levels of amyloid-beta 42 (Abeta42), phosphorylated tau 181 (p-tau181), and neurofilament light chain (NfL) in adults with Alzheimer’s disease and mark when those levels began to deviate from those of adults without Alzheimer’s disease.
Levels of Abeta42 in CSF and the ratio of Abeta42 to Abeta40 in people who developed Alzheimer’s disease diverged from those of peers who remained cognitively normal at 18 years and 14 years, respectively, before clinical signs of disease appeared.
The level of p-tau181 in CSF increased 11 years before disease onset, and NfL levels, a measure of neurodegeneration, increased 9 years before diagnosis.
These changes were followed by hippocampal atrophy and cognitive decline a few years later.
The results also show “an apparent accelerated change in concentrations of CSF biomarkers followed by a slowing of this change up to the time of diagnosis,” report the authors, led by Jianping Jia, MD, PhD, with the Innovation Center for Neurological Disorders, Xuanwu Hospital, Capital Medical University, Beijing, China.
The study was published online in The New England Journal of Medicine.
Time Course of Biomarker Changes
Dr. Jia and colleagues conducted a nested case-control study within the China Cognition and Aging Study (COAST). They matched 648 adults who developed Alzheimer’s disease to 648 who remained cognitively normal. CSF, cognitive, and brain imaging assessments were performed every 2-3 years for a median of about 20 years.
Within both groups, men slightly outnumbered women. At baseline, CSF biomarker levels, cognitive scores, and hippocampal volumes were similar in the two groups. Adults who developed Alzheimer’s disease were more likely than their matched controls to be carriers of the APOE epsilon-4 allele (37% vs 20%).
In terms of CSF Abeta42, the level of this biomarker in those who developed Alzheimer’s disease diverged from the level in controls an estimated 18 years before clinical diagnosis. At that time, the level was lower by a mean 59.13 pg/mL in the Alzheimer’s disease group.
A difference in the ratio of CSF Abeta42 to Abeta40 between the two groups appeared an estimated 14 years before the diagnosis of Alzheimer’s disease (difference in mean values, −0.01 pg/mL).
Differences between the two groups in CSF p-tau181 and total tau concentrations were apparent roughly 11 and 10 years before diagnosis, respectively. At those times, the mean differences in p-tau181 and total tau concentrations were 7.10 pg/mL and 87.10 pg/mL, respectively.
In terms of NfL, a difference between the groups was observed 9 years before diagnosis, with its trajectory progressively deviating from the concentrations observed in cognitively normal groups at that time, to a final mean difference in NfL of 228.29 pg/mL.
Bilateral hippocampal volume decreased with age in both groups. However, the decrease began to differ between the two groups 8 years before Alzheimer’s disease diagnosis, at which time volume was lower by 358.94 mm3 in the Alzheimer’s disease group compared with the control group.
Average Clinical Dementia Rating–Sum of Boxes (CDR-SB) scores in the Alzheimer’s disease group began to worsen compared with the control group at about 6 years before diagnosis.
As Alzheimer’s disease progressed, changes in CSF biomarkers increased before reaching a plateau.
Important Contribution
In a linked editorial, Richard Mayeux, MD, Department of Neurology, Columbia University, New York, said the importance of this work “cannot be overstated. Knowledge of the timing of these physiological events is critical to provide clinicians with useful starting points for prevention and therapeutic strategies.”
Dr. Mayeux said this “remarkable” longitudinal study spanning 2 decades “not only confirms the hypotheses of previous investigators but extends and validates the sequence of changes” in sporadic Alzheimer’s disease.
Dr. Mayeux acknowledged that one might consider the finding in this study to be limited owing to the inclusion of only individuals of Han Chinese ancestry.
However, longitudinal studies of plasma biomarkers in individuals of Asian, European, African, and Hispanic ancestry have shown similar trends in biomarker changes preceding the onset of Alzheimer’s disease, he noted.
“Ethnic variation in these biomarkers is known, but that fact does not lessen the effect of the results reported. It merely highlights that similar studies must continue and must be inclusive of other groups,” Dr. Mayeux concluded.
The study had no commercial funding. Disclosures for authors and editorialist are available at NEJM.org.
A version of this article appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Omalizumab for Food Allergies: What PCPs Should Know
Sandra Hong, MD, chair of allergy and immunology and director of the Food Allergy Center of Excellence at Cleveland Clinic, in Ohio, sees firsthand how situations that feel ordinary to most people strike fear in the hearts of her patients with food allergies.
Not only do some experience reactions to milk when they eat a cheese pizza — they can’t be in the same room with someone enjoying a slice nearby. “That would be terrifying,” Dr. Hong said.
Omalizumab (Xolair), recently approved by the US Food and Drug Administration as monotherapy for the treatment of food allergies, may now bring peace of mind to these patients and their families by reducing their risk of dangerous allergic reactions to accidental exposure.
While the drug does not cure food allergies, a phase 3, placebo-controlled trial found that after 16 weeks of treatment, two thirds of participants were able to tolerate at least 600 mg of peanut protein — equal to about 2.5 peanuts — without experiencing moderate to severe reactions.
An open-label extension trial also found the monoclonal antibody reduced the likelihood of serious reactions to eggs by 67%, milk by 66%, and cashews by 42%. The results of the study were published in The New England Journal of Medicine.
The treatment is approved for children as young as the age of 1 year and is the only treatment approved for multiple food allergies. It does not treat anaphylaxis or other emergency situations.
Patient Selection Key
While 8% of children and 10% of adults in the United States have a true food allergy, Brian Vickery, MD, chief of allergy and immunology and director of the Food Allergy Center at Children’s Healthcare of Atlanta, noted that a significantly higher proportion of the population restricts their diet based on perceived food intolerances.
“Most important for family doctors prior to prescribing the medication will be to be sure that the diagnosis is correct,” Kim said. “We know that allergy blood and skin testing is good but not perfect, and false positive results can occur,” said Edwin Kim, MD, chief of the Division of Pediatric Allergy and Immunology and director of the University of North Carolina Food Allergy Initiative at the University of North Carolina School of Medicine, Chapel Hill, who was a coauthor on the study in the New England Journal of Medicine. “ An allergist can conduct food challenges to confirm the diagnosis if results are unclear.”
Even for patients with confirmed IgE-mediated allergies, Dr. Hong said selecting patients who are good candidates for the therapy has “nuances.”
Patients must be willing and able to commit to injections every 2-4 weeks. Dosing depends on body weight and the total IgE levels of each patient. Patients with IgE levels > 1850 UI/mL likely will be disqualified from treatment since the clinical trial did not enroll patients with total IgE above this level and the appropriate dose in those patients is unknown.
“My recommendation for family physicians who are counseling food-allergic patients interested in omalizumab treatment is to partner with an allergist-immunologist, if at all possible,” Dr. Vickery said. He added that patients should have a comprehensive workup before beginning treatment because starting omalizumab would reduce reactivity and alter the outcome a diagnostic oral food challenge.
Two populations Dr. Hong thinks might particularly benefit from the therapy are college students and preschoolers, who may be unable to completely avoid allergens because of poor impulse control and food sharing in group settings.
“The concerns we have about this age group are whether or not there might be other factors involved that may impede their ability to make good decisions.”
Less control of the environment in dorms or other group living situations also could increase the risk of accidental exposure to a food allergen.
For the right patients, the treatment regimen has significant advantages over oral immunotherapy treatment (OIT), including the fact that it’s not a daily medication and it has the potential to treat allergic asthma at the same time.
“The biggest pro for omalizumab is that it can treat all of your food allergies, whether you have one or many, and do it all in one medication,” Dr. Kim said.
Managing Potential Harms
Omalizumab carries risks both primary care providers and patients must consider. First among them is that the drug carries a “black box” warning for an increased risk of anaphylaxis, Dr. Hong said.
Although patients with multiple food allergies typically already have prescriptions for epinephrine, primary care physicians (PCPs) considering offering omalizumab must be comfortable treating severe systemic reactions and their offices capable of post-dose monitoring, Dr. Hong said.
Anaphylaxis “can occur after the first dose or it can be delayed,” she said. “Typically, allergists will give these in our offices and we’ll actually have people wait for delayed amounts of time, for hours.”
The drug has been available since 2003 as a treatment for allergic asthma and urticaria. In addition to the warning for anaphylaxis, common reactions include joint pain and injection-site reactions. It also increases the risk for parasitic infection, and some studies show an increase in the risk for cancer.
Still, Dr. Kim said omalizumab’s safety profile is reassuring and noted it has advantages over OIT. “Since the patient is not exposing themselves to the food they are allergic to like in OIT, the safety is expected to be far better,” he said.
Lifelong Treatment
Dr. Vickery, Dr. Hong, and Dr. Kim all cautioned that patients should understand that, while omalizumab offers protection against accidental exposure and can meaningfully improve quality of life, it won’t allow them to loosen their allergen-avoidant diets.
Further, maintaining protection requires receiving injections every 2-4 weeks for life. For those without insurance, or whose insurance does not cover the treatment, costs could reach thousands of dollars each month, Dr. Hong said.
Omalizumab “has been well covered by insurance for asthma and chronic hives, but we will have to see what it looks like for food allergy. The range of plans and out-of-pocket deductibles available to patients will also play a big role,” Dr. Kim said.
Other novel approaches to food allergies are currently in clinical trials, and both Dr. Hong and Dr. Vickery are optimistic about potential options in the pipeline.
“We’re just on the brink of really exciting therapies coming forward in the future,” Dr. Hong said.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Center for Advancing Translational Sciences, both part of the National Institutes of Health; the Claudia and Steve Stange Family Fund; Genentech; and Novartis. Dr. Hong, Dr. Kim, and Dr. Vickery reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Sandra Hong, MD, chair of allergy and immunology and director of the Food Allergy Center of Excellence at Cleveland Clinic, in Ohio, sees firsthand how situations that feel ordinary to most people strike fear in the hearts of her patients with food allergies.
Not only do some experience reactions to milk when they eat a cheese pizza — they can’t be in the same room with someone enjoying a slice nearby. “That would be terrifying,” Dr. Hong said.
Omalizumab (Xolair), recently approved by the US Food and Drug Administration as monotherapy for the treatment of food allergies, may now bring peace of mind to these patients and their families by reducing their risk of dangerous allergic reactions to accidental exposure.
While the drug does not cure food allergies, a phase 3, placebo-controlled trial found that after 16 weeks of treatment, two thirds of participants were able to tolerate at least 600 mg of peanut protein — equal to about 2.5 peanuts — without experiencing moderate to severe reactions.
An open-label extension trial also found the monoclonal antibody reduced the likelihood of serious reactions to eggs by 67%, milk by 66%, and cashews by 42%. The results of the study were published in The New England Journal of Medicine.
The treatment is approved for children as young as the age of 1 year and is the only treatment approved for multiple food allergies. It does not treat anaphylaxis or other emergency situations.
Patient Selection Key
While 8% of children and 10% of adults in the United States have a true food allergy, Brian Vickery, MD, chief of allergy and immunology and director of the Food Allergy Center at Children’s Healthcare of Atlanta, noted that a significantly higher proportion of the population restricts their diet based on perceived food intolerances.
“Most important for family doctors prior to prescribing the medication will be to be sure that the diagnosis is correct,” Kim said. “We know that allergy blood and skin testing is good but not perfect, and false positive results can occur,” said Edwin Kim, MD, chief of the Division of Pediatric Allergy and Immunology and director of the University of North Carolina Food Allergy Initiative at the University of North Carolina School of Medicine, Chapel Hill, who was a coauthor on the study in the New England Journal of Medicine. “ An allergist can conduct food challenges to confirm the diagnosis if results are unclear.”
Even for patients with confirmed IgE-mediated allergies, Dr. Hong said selecting patients who are good candidates for the therapy has “nuances.”
Patients must be willing and able to commit to injections every 2-4 weeks. Dosing depends on body weight and the total IgE levels of each patient. Patients with IgE levels > 1850 UI/mL likely will be disqualified from treatment since the clinical trial did not enroll patients with total IgE above this level and the appropriate dose in those patients is unknown.
“My recommendation for family physicians who are counseling food-allergic patients interested in omalizumab treatment is to partner with an allergist-immunologist, if at all possible,” Dr. Vickery said. He added that patients should have a comprehensive workup before beginning treatment because starting omalizumab would reduce reactivity and alter the outcome a diagnostic oral food challenge.
Two populations Dr. Hong thinks might particularly benefit from the therapy are college students and preschoolers, who may be unable to completely avoid allergens because of poor impulse control and food sharing in group settings.
“The concerns we have about this age group are whether or not there might be other factors involved that may impede their ability to make good decisions.”
Less control of the environment in dorms or other group living situations also could increase the risk of accidental exposure to a food allergen.
For the right patients, the treatment regimen has significant advantages over oral immunotherapy treatment (OIT), including the fact that it’s not a daily medication and it has the potential to treat allergic asthma at the same time.
“The biggest pro for omalizumab is that it can treat all of your food allergies, whether you have one or many, and do it all in one medication,” Dr. Kim said.
Managing Potential Harms
Omalizumab carries risks both primary care providers and patients must consider. First among them is that the drug carries a “black box” warning for an increased risk of anaphylaxis, Dr. Hong said.
Although patients with multiple food allergies typically already have prescriptions for epinephrine, primary care physicians (PCPs) considering offering omalizumab must be comfortable treating severe systemic reactions and their offices capable of post-dose monitoring, Dr. Hong said.
Anaphylaxis “can occur after the first dose or it can be delayed,” she said. “Typically, allergists will give these in our offices and we’ll actually have people wait for delayed amounts of time, for hours.”
The drug has been available since 2003 as a treatment for allergic asthma and urticaria. In addition to the warning for anaphylaxis, common reactions include joint pain and injection-site reactions. It also increases the risk for parasitic infection, and some studies show an increase in the risk for cancer.
Still, Dr. Kim said omalizumab’s safety profile is reassuring and noted it has advantages over OIT. “Since the patient is not exposing themselves to the food they are allergic to like in OIT, the safety is expected to be far better,” he said.
Lifelong Treatment
Dr. Vickery, Dr. Hong, and Dr. Kim all cautioned that patients should understand that, while omalizumab offers protection against accidental exposure and can meaningfully improve quality of life, it won’t allow them to loosen their allergen-avoidant diets.
Further, maintaining protection requires receiving injections every 2-4 weeks for life. For those without insurance, or whose insurance does not cover the treatment, costs could reach thousands of dollars each month, Dr. Hong said.
Omalizumab “has been well covered by insurance for asthma and chronic hives, but we will have to see what it looks like for food allergy. The range of plans and out-of-pocket deductibles available to patients will also play a big role,” Dr. Kim said.
Other novel approaches to food allergies are currently in clinical trials, and both Dr. Hong and Dr. Vickery are optimistic about potential options in the pipeline.
“We’re just on the brink of really exciting therapies coming forward in the future,” Dr. Hong said.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Center for Advancing Translational Sciences, both part of the National Institutes of Health; the Claudia and Steve Stange Family Fund; Genentech; and Novartis. Dr. Hong, Dr. Kim, and Dr. Vickery reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Sandra Hong, MD, chair of allergy and immunology and director of the Food Allergy Center of Excellence at Cleveland Clinic, in Ohio, sees firsthand how situations that feel ordinary to most people strike fear in the hearts of her patients with food allergies.
Not only do some experience reactions to milk when they eat a cheese pizza — they can’t be in the same room with someone enjoying a slice nearby. “That would be terrifying,” Dr. Hong said.
Omalizumab (Xolair), recently approved by the US Food and Drug Administration as monotherapy for the treatment of food allergies, may now bring peace of mind to these patients and their families by reducing their risk of dangerous allergic reactions to accidental exposure.
While the drug does not cure food allergies, a phase 3, placebo-controlled trial found that after 16 weeks of treatment, two thirds of participants were able to tolerate at least 600 mg of peanut protein — equal to about 2.5 peanuts — without experiencing moderate to severe reactions.
An open-label extension trial also found the monoclonal antibody reduced the likelihood of serious reactions to eggs by 67%, milk by 66%, and cashews by 42%. The results of the study were published in The New England Journal of Medicine.
The treatment is approved for children as young as the age of 1 year and is the only treatment approved for multiple food allergies. It does not treat anaphylaxis or other emergency situations.
Patient Selection Key
While 8% of children and 10% of adults in the United States have a true food allergy, Brian Vickery, MD, chief of allergy and immunology and director of the Food Allergy Center at Children’s Healthcare of Atlanta, noted that a significantly higher proportion of the population restricts their diet based on perceived food intolerances.
“Most important for family doctors prior to prescribing the medication will be to be sure that the diagnosis is correct,” Kim said. “We know that allergy blood and skin testing is good but not perfect, and false positive results can occur,” said Edwin Kim, MD, chief of the Division of Pediatric Allergy and Immunology and director of the University of North Carolina Food Allergy Initiative at the University of North Carolina School of Medicine, Chapel Hill, who was a coauthor on the study in the New England Journal of Medicine. “ An allergist can conduct food challenges to confirm the diagnosis if results are unclear.”
Even for patients with confirmed IgE-mediated allergies, Dr. Hong said selecting patients who are good candidates for the therapy has “nuances.”
Patients must be willing and able to commit to injections every 2-4 weeks. Dosing depends on body weight and the total IgE levels of each patient. Patients with IgE levels > 1850 UI/mL likely will be disqualified from treatment since the clinical trial did not enroll patients with total IgE above this level and the appropriate dose in those patients is unknown.
“My recommendation for family physicians who are counseling food-allergic patients interested in omalizumab treatment is to partner with an allergist-immunologist, if at all possible,” Dr. Vickery said. He added that patients should have a comprehensive workup before beginning treatment because starting omalizumab would reduce reactivity and alter the outcome a diagnostic oral food challenge.
Two populations Dr. Hong thinks might particularly benefit from the therapy are college students and preschoolers, who may be unable to completely avoid allergens because of poor impulse control and food sharing in group settings.
“The concerns we have about this age group are whether or not there might be other factors involved that may impede their ability to make good decisions.”
Less control of the environment in dorms or other group living situations also could increase the risk of accidental exposure to a food allergen.
For the right patients, the treatment regimen has significant advantages over oral immunotherapy treatment (OIT), including the fact that it’s not a daily medication and it has the potential to treat allergic asthma at the same time.
“The biggest pro for omalizumab is that it can treat all of your food allergies, whether you have one or many, and do it all in one medication,” Dr. Kim said.
Managing Potential Harms
Omalizumab carries risks both primary care providers and patients must consider. First among them is that the drug carries a “black box” warning for an increased risk of anaphylaxis, Dr. Hong said.
Although patients with multiple food allergies typically already have prescriptions for epinephrine, primary care physicians (PCPs) considering offering omalizumab must be comfortable treating severe systemic reactions and their offices capable of post-dose monitoring, Dr. Hong said.
Anaphylaxis “can occur after the first dose or it can be delayed,” she said. “Typically, allergists will give these in our offices and we’ll actually have people wait for delayed amounts of time, for hours.”
The drug has been available since 2003 as a treatment for allergic asthma and urticaria. In addition to the warning for anaphylaxis, common reactions include joint pain and injection-site reactions. It also increases the risk for parasitic infection, and some studies show an increase in the risk for cancer.
Still, Dr. Kim said omalizumab’s safety profile is reassuring and noted it has advantages over OIT. “Since the patient is not exposing themselves to the food they are allergic to like in OIT, the safety is expected to be far better,” he said.
Lifelong Treatment
Dr. Vickery, Dr. Hong, and Dr. Kim all cautioned that patients should understand that, while omalizumab offers protection against accidental exposure and can meaningfully improve quality of life, it won’t allow them to loosen their allergen-avoidant diets.
Further, maintaining protection requires receiving injections every 2-4 weeks for life. For those without insurance, or whose insurance does not cover the treatment, costs could reach thousands of dollars each month, Dr. Hong said.
Omalizumab “has been well covered by insurance for asthma and chronic hives, but we will have to see what it looks like for food allergy. The range of plans and out-of-pocket deductibles available to patients will also play a big role,” Dr. Kim said.
Other novel approaches to food allergies are currently in clinical trials, and both Dr. Hong and Dr. Vickery are optimistic about potential options in the pipeline.
“We’re just on the brink of really exciting therapies coming forward in the future,” Dr. Hong said.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Center for Advancing Translational Sciences, both part of the National Institutes of Health; the Claudia and Steve Stange Family Fund; Genentech; and Novartis. Dr. Hong, Dr. Kim, and Dr. Vickery reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
5 Interesting Neurology Studies
This transcript has been edited for clarity.
Dear colleagues, I’m Christoph Diener from the medical faculty of University Duisburg-Essen in Germany. Today I would like to tell you about five interesting studies that were published in January 2024.
Long COVID
I would like to start with long COVID. There is an ongoing discussion about whether this condition — which means symptoms like dizziness, vertigo, fatigue, headache, and cognitive impairment that persist for more than 6 months — is either a consequence of the infection, functional symptoms, psychosomatic disease, or a depression.
There is an important paper that came out in Science. The group investigated 39 controls and 113 patients who had COVID-19. At 6 months, 40 of them had long COVID. The researchers repeatedly measured more than 6500 proteins in serum. The patients with long COVID had a significant increase in complement activation, which persisted even beyond 6 months. These patients also showed increased tissue lesion markers in the blood and activation of the endothelium.
Also, they had increased platelet activation and autoantibodies with increased anti-cytomegalovirus and anti-Epstein-Barr virus immunoglobulins. These are very strong indicators that COVID-19 leads to long-term changes in our immune system, and different activations of complement factors could explain the variety of symptoms that these patients display. Whether this has consequences for treatment is unclear at the moment.
Parkinson’s Classification
Let me come to another issue, which is the future treatment of Parkinson’s disease, covered in a paper in The Lancet Neurology. I think you are all aware that once patients display symptoms like rigidity, bradykinesia, or tremor, it’s most probably too late for neuroprotective therapy because 70% of the dopaminergic neurons are already dead.
The authors propose a new biological diagnosis of the disease in the preclinical state. This early preclinical diagnosis has three components. One is to show the presence of synuclein either in skin biopsy or in serum. The second is proof of neurodegeneration either by MRI or by PET imaging. The third involves genetic markers.
On top of this, we know that we have preclinical manifestations of Parkinson’s disease, like REM sleep disorders, autonomic disturbances, and cognitive impairment. With this new classification, we should be able to identify the preclinical phase of Parkinson’s disease and include these patients in future trials for neuroprotection.
Niemann-Pick Disease
My third study, in The New England Journal of Medicine, deals with Niemann-Pick disease type C (Trial of N-Acetyl-l-Leucine in Niemann–Pick Disease Type C. This is a rare autosomal recessive disorder that involves impaired lysosomal storage. This disease, which manifests usually in childhood, goes along with systemic, psychiatric, and neurologic abnormalities, and in particular, ataxia. Until now, there has been only one therapy, with miglustat. which has many side effects.
The group of authors found a new therapeutic approach with N-acetyl-L-leucine, which primarily increases mitochondrial energy production. This was a small, placebo-controlled, crossover trial with 2 x 12 weeks of treatment. This new compound showed efficacy and was very well tolerated. This shows that we definitely need long-term studies with this new, well-tolerated drug in this rare disease.
Anticoagulation in Subclinical AF
My fourth study comes from the stroke-prevention field, published in The New England Journal of Medicine. I think you are aware of subclinical atrail fibrillation. These are high-frequency episodes in ECG, usually identified by pacemakers or ECG monitoring systems. The international ARTESIA study included more than 4000 patients randomized either to apixaban 5 mg twice daily or aspirin 81 mg.
After 3.5 years, the investigators showed a small but significant decrease in the rate of stroke, with a relative risk reduction of 37%, but also, unfortunately, a significantly increased risk for major bleeding with apixaban. This means that we need a careful discussion with the patient, the family, and the GP to decide whether these patients should be anticoagulated or not.
Migraine and Depression
My final study, published in the European Journal of Neurology, deals with the comorbidity of depression and migraine. This study in the Netherlands included 108 patients treated with erenumab and 90 with fremanezumab; 68 were controls.
They used two depression scales. They showed that treatment with the monoclonal antibodies improved at least one of the two depression scales. I think this is an important study because it indicates that you can improve comorbid depression in people with severe migraine, even if this study did not show a correlation between the reduction in monthly migraine days and the improvement of depression.
What we learned for clinical practice is that we have to identify depression in people with migraine and we have to deal with it. Whether it’s with the treatment of monoclonal antibodies or antidepressant therapy doesn’t really matter.
Dear colleagues, we had interesting studies this month. I think the most spectacular one was published in Science on long COVID. Thank you very much for listening and watching. I’m Christoph Diener from University Duisburg-Essen.
Dr. Diener is Professor, Department of Neurology, Stroke Center-Headache Center, University Duisburg-Essen, Essen, Germany. He disclosed ties with Abbott; Addex Pharma; Alder; Allergan; Almirall; Amgen; Autonomic Technology; AstraZeneca; Bayer Vital; Berlin Chemie; Bristol-Myers Squibb; Boehringer Ingelheim; Chordate; CoAxia; Corimmun; Covidien; Coherex; CoLucid; Daiichi-Sankyo; D-Pharml Electrocore; Fresenius; GlaxoSmithKline; Grunenthal; Janssen-Cilag; Labrys Biologics Lilly; La Roche; 3M Medica; MSD; Medtronic; Menarini; MindFrame; Minster; Neuroscore; Neurobiological Technologies; Novartis; Novo-Nordisk; Johnson & Johnson; Knoll; Paion; Parke-Davis; Pierre Fabre; Pfizer Inc; Schaper and Brummer; sanofi-aventis; Schering-Plough; Servier; Solvay; Syngis; St. Jude; Talecris; Thrombogenics; WebMD Global; Weber and Weber; Wyeth; and Yamanouchi.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I’m Christoph Diener from the medical faculty of University Duisburg-Essen in Germany. Today I would like to tell you about five interesting studies that were published in January 2024.
Long COVID
I would like to start with long COVID. There is an ongoing discussion about whether this condition — which means symptoms like dizziness, vertigo, fatigue, headache, and cognitive impairment that persist for more than 6 months — is either a consequence of the infection, functional symptoms, psychosomatic disease, or a depression.
There is an important paper that came out in Science. The group investigated 39 controls and 113 patients who had COVID-19. At 6 months, 40 of them had long COVID. The researchers repeatedly measured more than 6500 proteins in serum. The patients with long COVID had a significant increase in complement activation, which persisted even beyond 6 months. These patients also showed increased tissue lesion markers in the blood and activation of the endothelium.
Also, they had increased platelet activation and autoantibodies with increased anti-cytomegalovirus and anti-Epstein-Barr virus immunoglobulins. These are very strong indicators that COVID-19 leads to long-term changes in our immune system, and different activations of complement factors could explain the variety of symptoms that these patients display. Whether this has consequences for treatment is unclear at the moment.
Parkinson’s Classification
Let me come to another issue, which is the future treatment of Parkinson’s disease, covered in a paper in The Lancet Neurology. I think you are all aware that once patients display symptoms like rigidity, bradykinesia, or tremor, it’s most probably too late for neuroprotective therapy because 70% of the dopaminergic neurons are already dead.
The authors propose a new biological diagnosis of the disease in the preclinical state. This early preclinical diagnosis has three components. One is to show the presence of synuclein either in skin biopsy or in serum. The second is proof of neurodegeneration either by MRI or by PET imaging. The third involves genetic markers.
On top of this, we know that we have preclinical manifestations of Parkinson’s disease, like REM sleep disorders, autonomic disturbances, and cognitive impairment. With this new classification, we should be able to identify the preclinical phase of Parkinson’s disease and include these patients in future trials for neuroprotection.
Niemann-Pick Disease
My third study, in The New England Journal of Medicine, deals with Niemann-Pick disease type C (Trial of N-Acetyl-l-Leucine in Niemann–Pick Disease Type C. This is a rare autosomal recessive disorder that involves impaired lysosomal storage. This disease, which manifests usually in childhood, goes along with systemic, psychiatric, and neurologic abnormalities, and in particular, ataxia. Until now, there has been only one therapy, with miglustat. which has many side effects.
The group of authors found a new therapeutic approach with N-acetyl-L-leucine, which primarily increases mitochondrial energy production. This was a small, placebo-controlled, crossover trial with 2 x 12 weeks of treatment. This new compound showed efficacy and was very well tolerated. This shows that we definitely need long-term studies with this new, well-tolerated drug in this rare disease.
Anticoagulation in Subclinical AF
My fourth study comes from the stroke-prevention field, published in The New England Journal of Medicine. I think you are aware of subclinical atrail fibrillation. These are high-frequency episodes in ECG, usually identified by pacemakers or ECG monitoring systems. The international ARTESIA study included more than 4000 patients randomized either to apixaban 5 mg twice daily or aspirin 81 mg.
After 3.5 years, the investigators showed a small but significant decrease in the rate of stroke, with a relative risk reduction of 37%, but also, unfortunately, a significantly increased risk for major bleeding with apixaban. This means that we need a careful discussion with the patient, the family, and the GP to decide whether these patients should be anticoagulated or not.
Migraine and Depression
My final study, published in the European Journal of Neurology, deals with the comorbidity of depression and migraine. This study in the Netherlands included 108 patients treated with erenumab and 90 with fremanezumab; 68 were controls.
They used two depression scales. They showed that treatment with the monoclonal antibodies improved at least one of the two depression scales. I think this is an important study because it indicates that you can improve comorbid depression in people with severe migraine, even if this study did not show a correlation between the reduction in monthly migraine days and the improvement of depression.
What we learned for clinical practice is that we have to identify depression in people with migraine and we have to deal with it. Whether it’s with the treatment of monoclonal antibodies or antidepressant therapy doesn’t really matter.
Dear colleagues, we had interesting studies this month. I think the most spectacular one was published in Science on long COVID. Thank you very much for listening and watching. I’m Christoph Diener from University Duisburg-Essen.
Dr. Diener is Professor, Department of Neurology, Stroke Center-Headache Center, University Duisburg-Essen, Essen, Germany. He disclosed ties with Abbott; Addex Pharma; Alder; Allergan; Almirall; Amgen; Autonomic Technology; AstraZeneca; Bayer Vital; Berlin Chemie; Bristol-Myers Squibb; Boehringer Ingelheim; Chordate; CoAxia; Corimmun; Covidien; Coherex; CoLucid; Daiichi-Sankyo; D-Pharml Electrocore; Fresenius; GlaxoSmithKline; Grunenthal; Janssen-Cilag; Labrys Biologics Lilly; La Roche; 3M Medica; MSD; Medtronic; Menarini; MindFrame; Minster; Neuroscore; Neurobiological Technologies; Novartis; Novo-Nordisk; Johnson & Johnson; Knoll; Paion; Parke-Davis; Pierre Fabre; Pfizer Inc; Schaper and Brummer; sanofi-aventis; Schering-Plough; Servier; Solvay; Syngis; St. Jude; Talecris; Thrombogenics; WebMD Global; Weber and Weber; Wyeth; and Yamanouchi.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I’m Christoph Diener from the medical faculty of University Duisburg-Essen in Germany. Today I would like to tell you about five interesting studies that were published in January 2024.
Long COVID
I would like to start with long COVID. There is an ongoing discussion about whether this condition — which means symptoms like dizziness, vertigo, fatigue, headache, and cognitive impairment that persist for more than 6 months — is either a consequence of the infection, functional symptoms, psychosomatic disease, or a depression.
There is an important paper that came out in Science. The group investigated 39 controls and 113 patients who had COVID-19. At 6 months, 40 of them had long COVID. The researchers repeatedly measured more than 6500 proteins in serum. The patients with long COVID had a significant increase in complement activation, which persisted even beyond 6 months. These patients also showed increased tissue lesion markers in the blood and activation of the endothelium.
Also, they had increased platelet activation and autoantibodies with increased anti-cytomegalovirus and anti-Epstein-Barr virus immunoglobulins. These are very strong indicators that COVID-19 leads to long-term changes in our immune system, and different activations of complement factors could explain the variety of symptoms that these patients display. Whether this has consequences for treatment is unclear at the moment.
Parkinson’s Classification
Let me come to another issue, which is the future treatment of Parkinson’s disease, covered in a paper in The Lancet Neurology. I think you are all aware that once patients display symptoms like rigidity, bradykinesia, or tremor, it’s most probably too late for neuroprotective therapy because 70% of the dopaminergic neurons are already dead.
The authors propose a new biological diagnosis of the disease in the preclinical state. This early preclinical diagnosis has three components. One is to show the presence of synuclein either in skin biopsy or in serum. The second is proof of neurodegeneration either by MRI or by PET imaging. The third involves genetic markers.
On top of this, we know that we have preclinical manifestations of Parkinson’s disease, like REM sleep disorders, autonomic disturbances, and cognitive impairment. With this new classification, we should be able to identify the preclinical phase of Parkinson’s disease and include these patients in future trials for neuroprotection.
Niemann-Pick Disease
My third study, in The New England Journal of Medicine, deals with Niemann-Pick disease type C (Trial of N-Acetyl-l-Leucine in Niemann–Pick Disease Type C. This is a rare autosomal recessive disorder that involves impaired lysosomal storage. This disease, which manifests usually in childhood, goes along with systemic, psychiatric, and neurologic abnormalities, and in particular, ataxia. Until now, there has been only one therapy, with miglustat. which has many side effects.
The group of authors found a new therapeutic approach with N-acetyl-L-leucine, which primarily increases mitochondrial energy production. This was a small, placebo-controlled, crossover trial with 2 x 12 weeks of treatment. This new compound showed efficacy and was very well tolerated. This shows that we definitely need long-term studies with this new, well-tolerated drug in this rare disease.
Anticoagulation in Subclinical AF
My fourth study comes from the stroke-prevention field, published in The New England Journal of Medicine. I think you are aware of subclinical atrail fibrillation. These are high-frequency episodes in ECG, usually identified by pacemakers or ECG monitoring systems. The international ARTESIA study included more than 4000 patients randomized either to apixaban 5 mg twice daily or aspirin 81 mg.
After 3.5 years, the investigators showed a small but significant decrease in the rate of stroke, with a relative risk reduction of 37%, but also, unfortunately, a significantly increased risk for major bleeding with apixaban. This means that we need a careful discussion with the patient, the family, and the GP to decide whether these patients should be anticoagulated or not.
Migraine and Depression
My final study, published in the European Journal of Neurology, deals with the comorbidity of depression and migraine. This study in the Netherlands included 108 patients treated with erenumab and 90 with fremanezumab; 68 were controls.
They used two depression scales. They showed that treatment with the monoclonal antibodies improved at least one of the two depression scales. I think this is an important study because it indicates that you can improve comorbid depression in people with severe migraine, even if this study did not show a correlation between the reduction in monthly migraine days and the improvement of depression.
What we learned for clinical practice is that we have to identify depression in people with migraine and we have to deal with it. Whether it’s with the treatment of monoclonal antibodies or antidepressant therapy doesn’t really matter.
Dear colleagues, we had interesting studies this month. I think the most spectacular one was published in Science on long COVID. Thank you very much for listening and watching. I’m Christoph Diener from University Duisburg-Essen.
Dr. Diener is Professor, Department of Neurology, Stroke Center-Headache Center, University Duisburg-Essen, Essen, Germany. He disclosed ties with Abbott; Addex Pharma; Alder; Allergan; Almirall; Amgen; Autonomic Technology; AstraZeneca; Bayer Vital; Berlin Chemie; Bristol-Myers Squibb; Boehringer Ingelheim; Chordate; CoAxia; Corimmun; Covidien; Coherex; CoLucid; Daiichi-Sankyo; D-Pharml Electrocore; Fresenius; GlaxoSmithKline; Grunenthal; Janssen-Cilag; Labrys Biologics Lilly; La Roche; 3M Medica; MSD; Medtronic; Menarini; MindFrame; Minster; Neuroscore; Neurobiological Technologies; Novartis; Novo-Nordisk; Johnson & Johnson; Knoll; Paion; Parke-Davis; Pierre Fabre; Pfizer Inc; Schaper and Brummer; sanofi-aventis; Schering-Plough; Servier; Solvay; Syngis; St. Jude; Talecris; Thrombogenics; WebMD Global; Weber and Weber; Wyeth; and Yamanouchi.
A version of this article appeared on Medscape.com.