User login
American Society of Clinical Oncology (ASCO): Annual Meeting
VIDEO: Ibrutinib should be therapy ‘backbone’ in relapsed CLL
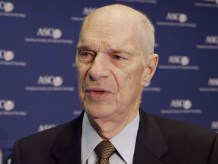
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2015 ASCO ANNUAL MEETING
ASCO: HR-deficient breast cancers more likely to respond to carboplatin
CHICAGO – Homologous recombination (HR) deficiency is a biomarker for benefit from neoadjuvant chemotherapy in women with triple-negative breast cancer (TNBC), suggest data from the GeparSixto trial presented at the annual meeting of the American Society of Clinical Oncology.
Roughly two-thirds of women were found to have HR-deficient tumors, impairing their ability to repair DNA and thereby rendering them susceptible to DNA-damaging agents. These women had more than double the odds of a pathologic complete response (pCR).
“HR deficiency in triple-negative breast cancer appears to be an independent predictor of high pCR rates to the chemotherapies that were given in this study,” summarized Dr. Gunter von Minckwitz on behalf of the German Breast Group and Arbeitsgemeinschaft Gynakologische Onkologie-B (AGO-B) study group.
However, the findings were somewhat inconsistent. Additionally, although the highest pCR rate, at about 65%, was seen in women who had HR-deficient tumors and received carboplatin, women whose tumors were nondeficient also had some benefit from addition of this agent.
“This is why these data have to be confirmed by other studies, for example, the same measurements are currently ongoing in the CALGB 40603 study,” commented Dr. von Minckwitz, a senior physician at the University Women’s Hospital in Frankfurt. “And finally, they have to be set into the context with survival data that we expect at the end of 2015 or beginning of 2016.”
Invited discussant Dr. Pamela N. Munster, a professor at the University of California, San Francisco, noted, “Homologous recombination deficiency mediated through the host or tumor predicts for high responses to chemotherapy and platinum salts in early-stage triple-negative breast cancer.” However, “the role of carboplatin and its optimal setting remains complex.”
She asked about the prevailing clinical practice regarding this agent’s use. “Based on your presentation and your work, what’s the landscape in Europe on the incorporation of carboplatin in the neoadjuvant therapy in triple-negative breast cancer or a subselect group?”
“We made a survey in our group half a year ago, and all members said that they are using carboplatin in triple-negative disease when they get neoadjuvant treatment,” Dr. von Minckwitz replied. “I’m not sure if this was 100% of patients, but I believe it was a more general quote, and this is in concordance with our AGO guideline, which allows the use of carboplatin in general in triple-negative [breast cancer]. It still says in patients with germline mutations, there is a somewhat stronger recommendation to use it, but it’s of course not a must.”
Session attendee Dr. Rebecca Dent of the National Cancer Centre Singapore and the University of Toronto asked whether oncologists should begin clinically applying HR deficiency for patient selection.
“I don’t think that currently these data or the sample size is sufficient to support clinical use tomorrow. … We have to wait for a confirmative study,” Dr. von Minckwitz replied.
Dr. Munster, the discussant, agreed, saying, “I think the HRD percentage is actually quite high in [this] set, so the test may not be as robust as we like to see. So I think part of it is refinement of biomarkers has to be the focus of what we do in the next 10 years.”
Previous results of the randomized phase 2/3 GeparSixto trial have shown that adding carboplatin to a neoadjuvant chemotherapy backbone (paclitaxel, liposomal doxorubicin, and bevacizumab) improves the pCR rate in patients with triple-negative breast cancer, but at the cost of added toxicity (Lancet Oncol. 2014;15:747-56). “Therefore it is of importance to better define the group of patients that might have a higher benefit from the addition of carboplatin,” Dr. von Minckwitz explained.
“We know from previous studies that tumors with a decreased DNA repair capacity, for example, due to a mutation of the BRCA1 or BRCA2 gene are expected to have a higher sensitivity to DNA-damaging agents like platinum compounds. A more extensive way to measure DNA repair capacity is now possible using the HRD assay,” he noted.
The investigators assessed tumor HR deficiency among the 315 trial participants with triple-negative breast cancer. Overall, 70.5% had tumors that were HR deficient (meaning they had a high HRD score or a tumor BRCA mutation).
In the entire cohort, women with HR-deficient tumors were more likely to have a pCR, defined as absence of invasive residual disease in the breast or nodes (ypT0/is ypN0), than peers with HR-nondeficient tumors (55.9% vs. 29.8%). In multivariate analysis, HR deficiency independently predicted pCR (odds ratio, 2.51; P = .009).
Adding carboplatin improved the pCR rate significantly in women who had HR-deficient tumors (from 45.2% to 64.9%, P = .025) but also somewhat in women who had HR-nondeficient tumors (from 20.0% and 40.7%, P = .146). And there was no significant interaction between HR deficiency and carboplatin benefit.
In further analyses, carboplatin had a significant benefit in patients with a high HRD score but intact tumor BRCA, but not in patients with mutated tumor BRCA.
Findings differed slightly when the investigators repeated analyses but instead used a stricter definition of pCR that calls for absence of both invasive and noninvasive (ductal carcinoma in situ) residual disease in the breast and nodes (ypT0 ypN0), according to Dr. von Minckwitz.
Given that the majority of HR-deficient tumors did not have a BRCA mutation, the investigators plan to assess other drivers of HR deficiency, he said.
Dr. von Minckwitz disclosed employment, leadership, and stock ownership relationships with GBG Forschungs GmbH and research funding to his institution by Amgen, AstraZeneca, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi, and Teva. The trial was funded by Teva, Roche Pharma AG, and GlaxoSmithKline.
CHICAGO – Homologous recombination (HR) deficiency is a biomarker for benefit from neoadjuvant chemotherapy in women with triple-negative breast cancer (TNBC), suggest data from the GeparSixto trial presented at the annual meeting of the American Society of Clinical Oncology.
Roughly two-thirds of women were found to have HR-deficient tumors, impairing their ability to repair DNA and thereby rendering them susceptible to DNA-damaging agents. These women had more than double the odds of a pathologic complete response (pCR).
“HR deficiency in triple-negative breast cancer appears to be an independent predictor of high pCR rates to the chemotherapies that were given in this study,” summarized Dr. Gunter von Minckwitz on behalf of the German Breast Group and Arbeitsgemeinschaft Gynakologische Onkologie-B (AGO-B) study group.
However, the findings were somewhat inconsistent. Additionally, although the highest pCR rate, at about 65%, was seen in women who had HR-deficient tumors and received carboplatin, women whose tumors were nondeficient also had some benefit from addition of this agent.
“This is why these data have to be confirmed by other studies, for example, the same measurements are currently ongoing in the CALGB 40603 study,” commented Dr. von Minckwitz, a senior physician at the University Women’s Hospital in Frankfurt. “And finally, they have to be set into the context with survival data that we expect at the end of 2015 or beginning of 2016.”
Invited discussant Dr. Pamela N. Munster, a professor at the University of California, San Francisco, noted, “Homologous recombination deficiency mediated through the host or tumor predicts for high responses to chemotherapy and platinum salts in early-stage triple-negative breast cancer.” However, “the role of carboplatin and its optimal setting remains complex.”
She asked about the prevailing clinical practice regarding this agent’s use. “Based on your presentation and your work, what’s the landscape in Europe on the incorporation of carboplatin in the neoadjuvant therapy in triple-negative breast cancer or a subselect group?”
“We made a survey in our group half a year ago, and all members said that they are using carboplatin in triple-negative disease when they get neoadjuvant treatment,” Dr. von Minckwitz replied. “I’m not sure if this was 100% of patients, but I believe it was a more general quote, and this is in concordance with our AGO guideline, which allows the use of carboplatin in general in triple-negative [breast cancer]. It still says in patients with germline mutations, there is a somewhat stronger recommendation to use it, but it’s of course not a must.”
Session attendee Dr. Rebecca Dent of the National Cancer Centre Singapore and the University of Toronto asked whether oncologists should begin clinically applying HR deficiency for patient selection.
“I don’t think that currently these data or the sample size is sufficient to support clinical use tomorrow. … We have to wait for a confirmative study,” Dr. von Minckwitz replied.
Dr. Munster, the discussant, agreed, saying, “I think the HRD percentage is actually quite high in [this] set, so the test may not be as robust as we like to see. So I think part of it is refinement of biomarkers has to be the focus of what we do in the next 10 years.”
Previous results of the randomized phase 2/3 GeparSixto trial have shown that adding carboplatin to a neoadjuvant chemotherapy backbone (paclitaxel, liposomal doxorubicin, and bevacizumab) improves the pCR rate in patients with triple-negative breast cancer, but at the cost of added toxicity (Lancet Oncol. 2014;15:747-56). “Therefore it is of importance to better define the group of patients that might have a higher benefit from the addition of carboplatin,” Dr. von Minckwitz explained.
“We know from previous studies that tumors with a decreased DNA repair capacity, for example, due to a mutation of the BRCA1 or BRCA2 gene are expected to have a higher sensitivity to DNA-damaging agents like platinum compounds. A more extensive way to measure DNA repair capacity is now possible using the HRD assay,” he noted.
The investigators assessed tumor HR deficiency among the 315 trial participants with triple-negative breast cancer. Overall, 70.5% had tumors that were HR deficient (meaning they had a high HRD score or a tumor BRCA mutation).
In the entire cohort, women with HR-deficient tumors were more likely to have a pCR, defined as absence of invasive residual disease in the breast or nodes (ypT0/is ypN0), than peers with HR-nondeficient tumors (55.9% vs. 29.8%). In multivariate analysis, HR deficiency independently predicted pCR (odds ratio, 2.51; P = .009).
Adding carboplatin improved the pCR rate significantly in women who had HR-deficient tumors (from 45.2% to 64.9%, P = .025) but also somewhat in women who had HR-nondeficient tumors (from 20.0% and 40.7%, P = .146). And there was no significant interaction between HR deficiency and carboplatin benefit.
In further analyses, carboplatin had a significant benefit in patients with a high HRD score but intact tumor BRCA, but not in patients with mutated tumor BRCA.
Findings differed slightly when the investigators repeated analyses but instead used a stricter definition of pCR that calls for absence of both invasive and noninvasive (ductal carcinoma in situ) residual disease in the breast and nodes (ypT0 ypN0), according to Dr. von Minckwitz.
Given that the majority of HR-deficient tumors did not have a BRCA mutation, the investigators plan to assess other drivers of HR deficiency, he said.
Dr. von Minckwitz disclosed employment, leadership, and stock ownership relationships with GBG Forschungs GmbH and research funding to his institution by Amgen, AstraZeneca, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi, and Teva. The trial was funded by Teva, Roche Pharma AG, and GlaxoSmithKline.
CHICAGO – Homologous recombination (HR) deficiency is a biomarker for benefit from neoadjuvant chemotherapy in women with triple-negative breast cancer (TNBC), suggest data from the GeparSixto trial presented at the annual meeting of the American Society of Clinical Oncology.
Roughly two-thirds of women were found to have HR-deficient tumors, impairing their ability to repair DNA and thereby rendering them susceptible to DNA-damaging agents. These women had more than double the odds of a pathologic complete response (pCR).
“HR deficiency in triple-negative breast cancer appears to be an independent predictor of high pCR rates to the chemotherapies that were given in this study,” summarized Dr. Gunter von Minckwitz on behalf of the German Breast Group and Arbeitsgemeinschaft Gynakologische Onkologie-B (AGO-B) study group.
However, the findings were somewhat inconsistent. Additionally, although the highest pCR rate, at about 65%, was seen in women who had HR-deficient tumors and received carboplatin, women whose tumors were nondeficient also had some benefit from addition of this agent.
“This is why these data have to be confirmed by other studies, for example, the same measurements are currently ongoing in the CALGB 40603 study,” commented Dr. von Minckwitz, a senior physician at the University Women’s Hospital in Frankfurt. “And finally, they have to be set into the context with survival data that we expect at the end of 2015 or beginning of 2016.”
Invited discussant Dr. Pamela N. Munster, a professor at the University of California, San Francisco, noted, “Homologous recombination deficiency mediated through the host or tumor predicts for high responses to chemotherapy and platinum salts in early-stage triple-negative breast cancer.” However, “the role of carboplatin and its optimal setting remains complex.”
She asked about the prevailing clinical practice regarding this agent’s use. “Based on your presentation and your work, what’s the landscape in Europe on the incorporation of carboplatin in the neoadjuvant therapy in triple-negative breast cancer or a subselect group?”
“We made a survey in our group half a year ago, and all members said that they are using carboplatin in triple-negative disease when they get neoadjuvant treatment,” Dr. von Minckwitz replied. “I’m not sure if this was 100% of patients, but I believe it was a more general quote, and this is in concordance with our AGO guideline, which allows the use of carboplatin in general in triple-negative [breast cancer]. It still says in patients with germline mutations, there is a somewhat stronger recommendation to use it, but it’s of course not a must.”
Session attendee Dr. Rebecca Dent of the National Cancer Centre Singapore and the University of Toronto asked whether oncologists should begin clinically applying HR deficiency for patient selection.
“I don’t think that currently these data or the sample size is sufficient to support clinical use tomorrow. … We have to wait for a confirmative study,” Dr. von Minckwitz replied.
Dr. Munster, the discussant, agreed, saying, “I think the HRD percentage is actually quite high in [this] set, so the test may not be as robust as we like to see. So I think part of it is refinement of biomarkers has to be the focus of what we do in the next 10 years.”
Previous results of the randomized phase 2/3 GeparSixto trial have shown that adding carboplatin to a neoadjuvant chemotherapy backbone (paclitaxel, liposomal doxorubicin, and bevacizumab) improves the pCR rate in patients with triple-negative breast cancer, but at the cost of added toxicity (Lancet Oncol. 2014;15:747-56). “Therefore it is of importance to better define the group of patients that might have a higher benefit from the addition of carboplatin,” Dr. von Minckwitz explained.
“We know from previous studies that tumors with a decreased DNA repair capacity, for example, due to a mutation of the BRCA1 or BRCA2 gene are expected to have a higher sensitivity to DNA-damaging agents like platinum compounds. A more extensive way to measure DNA repair capacity is now possible using the HRD assay,” he noted.
The investigators assessed tumor HR deficiency among the 315 trial participants with triple-negative breast cancer. Overall, 70.5% had tumors that were HR deficient (meaning they had a high HRD score or a tumor BRCA mutation).
In the entire cohort, women with HR-deficient tumors were more likely to have a pCR, defined as absence of invasive residual disease in the breast or nodes (ypT0/is ypN0), than peers with HR-nondeficient tumors (55.9% vs. 29.8%). In multivariate analysis, HR deficiency independently predicted pCR (odds ratio, 2.51; P = .009).
Adding carboplatin improved the pCR rate significantly in women who had HR-deficient tumors (from 45.2% to 64.9%, P = .025) but also somewhat in women who had HR-nondeficient tumors (from 20.0% and 40.7%, P = .146). And there was no significant interaction between HR deficiency and carboplatin benefit.
In further analyses, carboplatin had a significant benefit in patients with a high HRD score but intact tumor BRCA, but not in patients with mutated tumor BRCA.
Findings differed slightly when the investigators repeated analyses but instead used a stricter definition of pCR that calls for absence of both invasive and noninvasive (ductal carcinoma in situ) residual disease in the breast and nodes (ypT0 ypN0), according to Dr. von Minckwitz.
Given that the majority of HR-deficient tumors did not have a BRCA mutation, the investigators plan to assess other drivers of HR deficiency, he said.
Dr. von Minckwitz disclosed employment, leadership, and stock ownership relationships with GBG Forschungs GmbH and research funding to his institution by Amgen, AstraZeneca, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi, and Teva. The trial was funded by Teva, Roche Pharma AG, and GlaxoSmithKline.
AT THE 2015 ASCO ANNUAL MEETING
Key clinical point: HR deficiency is a biomarker for benefit from neoadjuvant chemotherapy in women with TNBC.
Major finding: Women with HR-deficient tumors had 2.51-fold higher multivariate odds of pathologic complete response.
Data source: An analysis of 315 women with TNBC treated with neoadjuvant chemotherapy in a randomized trial.
Disclosures: Dr. von Minckwitz disclosed employment, leadership, and stock ownership relationships with GBG Forschungs GmbH and research funding to his institution by Amgen, AstraZeneca, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi, and Teva. The trial was funded by Teva, Roche Pharma AG, and GlaxoSmithKline.
Panobinostat combos can treat rel/ref MM
©ASCO/Rodney White
CHICAGO—Combination regimens including the histone deacetylase inhibitor panobinostat can produce durable responses and prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to research presented at the 2015 ASCO Annual Meeting.
In a phase 2 trial, panobinostat plus lenalidomide and dexamethasone produced durable responses, even in high-risk, lenalidomide-refractory MM patients.
In a phase 3 trial, panobinostat in combination with bortezomib and dexamethasone led to a 7.8-month improvement in median PFS over placebo-bortezomib-dexamethasone in patients with relapsed or relapsed and refractory MM who had received 2 or more prior regimens.
Both studies were sponsored by Novartis, the company developing panobinostat.
PANORAMA-1 substudy
PANORAMA-1 was a phase 3, randomized, double-blind, placebo-controlled trial of 768 MM patients. Overall, panobinostat in combination with bortezomib and dexamethasone led to a clinically relevant and statistically significant increase in PFS of about 4 months compared to placebo-bortezomib-dexamethasone.
At ASCO, Jesús San Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain, presented the results of an exploratory analysis of 147 patients in this trial (abstract 8526*).
The patients had relapsed or relapsed and refractory MM and had received 2 or more prior regimens, including bortezomib and an immunomodulatory agent (IMiD).
Disease and treatment characteristics were as follows:
| Panobinostat
(n=73) |
Placebo (n=74) | |
| Disease
characteristics, n (%) |
||
| Relapsed | 39 (53) | 30 (41) |
| Relapsed/refractory | 34 (47) | 43 (58) |
| Prior
therapies, n (%) |
||
| Bortezomib | 73 (100) | 74 (100) |
| Lenalidomide | 28 (38) | 37 (50) |
| Thalidomide | 63 (86) | 50 (68) |
| Bortezomib
+ lenalidomide |
28 (38) | 37 (50) |
| Bortezomib
+ dexamethasone |
69 (95) | 74 (100) |
| Prior
autologous transplant, n (%) |
54 (74) | 47 (64) |
| Median
prior lines of therapy (range) |
3 (2-4) | 3 (2-3) |
The median PFS was 12.5 months in the panobinostat arm, compared to 4.7 months in the placebo arm. Treatment with panobinostat also led to an increase in complete/near complete response rates (21.9% vs 8.1%) and overall response rate (58.9% vs 39.2%).
Common grade 3/4 non-hematologic adverse events in the panobinostat arm and placebo arm, respectively, included diarrhea (33.3% vs 15.1%), asthenia/fatigue (26.4% vs 13.7%), and peripheral neuropathy (16.7% vs 6.8%).
The most common grade 3/4 hematologic abnormalities in the panobinostat arm and placebo arm, respectively, were thrombocytopenia (68.1% vs 44.4%), lymphopenia (48.6% vs 49.3%), and neutropenia (40.3% vs 16.4%).
The percentage of on-treatment deaths was similar between the treatment arms (6.9% vs 6.8%).
“These data provide physicians with a better understanding of the clinical use of panobinostat, an HDAC inhibitor, a promising new drug class for this difficult-to-treat patient population with a high unmet need,” Dr San Miguel said.
Phase 2 trial
Ajai Chari, MD, of Mount Sinai Medical Center in New York, presented the results of a phase 2 study of panobinostat with lenalidomide and weekly dexamethasone in patients with relapsed/refractory MM (abstract 8528*).
There were 20 evaluable patients with a median age of 64 (range, 51-75). They had received a median of 3 prior therapies (range, 1-10). Prior regimens were as follows:
| Prior
therapy |
Exposed/Refractory, n (%) |
| Dexamethasone | 20 (100)/9
(45) |
| Thalidomide | 6 (30)/2
(10) |
| Lenalidomide |
20 (100)/15 (75) |
| Pomalidomide | 7 (35)/7
(35) |
| Bortezomib | 20 (100)/9
(45) |
| Carfilzomib | 6 (30)/6
(30) |
| Autologous
transplant |
15 (75) |
For this study, patients received panobinostat (20 mg on days 1, 3, 5, 15, 17, and 19), lenalidomide (25 mg on days 1-21), and dexamethasone (40 mg on days 1, 8, and 15).
The overall response rate was 45%. This included 1 complete response, 3 very good partial responses, 5 partial responses, and 8 minimal responses. Two patients had stable disease, and 1 progressed.
Among lenalidomide-refractory patients (n=16), the overall response rate was 38%. This included 3 very good partial responses, 3 partial responses, and 7 minimal responses. Two patients had stable disease, and 1 progressed.
The median PFS was 6.5 months overall and among lenalidomide-refractory patients.
Grade 3/4 toxicities were primarily hematologic, including neutropenia (55%), thrombocytopenia (40%), and anemia (5%). Grade 3/4 non-hematologic adverse events included infections (n=4), diarrhea (n=3), pulmonary emboli (n=2), neck pain (n=1), QTc prolongation (n=1), fatigue (n=1), and weight loss (n=1).
“In relapsed/refractory MM patients, panobinostat in combination with lenalidomide and dexamethasone demonstrated durable responses comparable to other recently approved agents, even in lenalidomide-refractory patients with high-risk molecular findings,” Dr Chari said.
“In notable contrast to PANORAMA-1 results, this completely oral regimen is well-tolerated, with no grade 3/4 [gastrointestinal] toxicities and primarily expected hematologic toxicities.” ![]()
*Information in the abstract differs from that presented at the meeting.
©ASCO/Rodney White
CHICAGO—Combination regimens including the histone deacetylase inhibitor panobinostat can produce durable responses and prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to research presented at the 2015 ASCO Annual Meeting.
In a phase 2 trial, panobinostat plus lenalidomide and dexamethasone produced durable responses, even in high-risk, lenalidomide-refractory MM patients.
In a phase 3 trial, panobinostat in combination with bortezomib and dexamethasone led to a 7.8-month improvement in median PFS over placebo-bortezomib-dexamethasone in patients with relapsed or relapsed and refractory MM who had received 2 or more prior regimens.
Both studies were sponsored by Novartis, the company developing panobinostat.
PANORAMA-1 substudy
PANORAMA-1 was a phase 3, randomized, double-blind, placebo-controlled trial of 768 MM patients. Overall, panobinostat in combination with bortezomib and dexamethasone led to a clinically relevant and statistically significant increase in PFS of about 4 months compared to placebo-bortezomib-dexamethasone.
At ASCO, Jesús San Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain, presented the results of an exploratory analysis of 147 patients in this trial (abstract 8526*).
The patients had relapsed or relapsed and refractory MM and had received 2 or more prior regimens, including bortezomib and an immunomodulatory agent (IMiD).
Disease and treatment characteristics were as follows:
| Panobinostat
(n=73) |
Placebo (n=74) | |
| Disease
characteristics, n (%) |
||
| Relapsed | 39 (53) | 30 (41) |
| Relapsed/refractory | 34 (47) | 43 (58) |
| Prior
therapies, n (%) |
||
| Bortezomib | 73 (100) | 74 (100) |
| Lenalidomide | 28 (38) | 37 (50) |
| Thalidomide | 63 (86) | 50 (68) |
| Bortezomib
+ lenalidomide |
28 (38) | 37 (50) |
| Bortezomib
+ dexamethasone |
69 (95) | 74 (100) |
| Prior
autologous transplant, n (%) |
54 (74) | 47 (64) |
| Median
prior lines of therapy (range) |
3 (2-4) | 3 (2-3) |
The median PFS was 12.5 months in the panobinostat arm, compared to 4.7 months in the placebo arm. Treatment with panobinostat also led to an increase in complete/near complete response rates (21.9% vs 8.1%) and overall response rate (58.9% vs 39.2%).
Common grade 3/4 non-hematologic adverse events in the panobinostat arm and placebo arm, respectively, included diarrhea (33.3% vs 15.1%), asthenia/fatigue (26.4% vs 13.7%), and peripheral neuropathy (16.7% vs 6.8%).
The most common grade 3/4 hematologic abnormalities in the panobinostat arm and placebo arm, respectively, were thrombocytopenia (68.1% vs 44.4%), lymphopenia (48.6% vs 49.3%), and neutropenia (40.3% vs 16.4%).
The percentage of on-treatment deaths was similar between the treatment arms (6.9% vs 6.8%).
“These data provide physicians with a better understanding of the clinical use of panobinostat, an HDAC inhibitor, a promising new drug class for this difficult-to-treat patient population with a high unmet need,” Dr San Miguel said.
Phase 2 trial
Ajai Chari, MD, of Mount Sinai Medical Center in New York, presented the results of a phase 2 study of panobinostat with lenalidomide and weekly dexamethasone in patients with relapsed/refractory MM (abstract 8528*).
There were 20 evaluable patients with a median age of 64 (range, 51-75). They had received a median of 3 prior therapies (range, 1-10). Prior regimens were as follows:
| Prior
therapy |
Exposed/Refractory, n (%) |
| Dexamethasone | 20 (100)/9
(45) |
| Thalidomide | 6 (30)/2
(10) |
| Lenalidomide |
20 (100)/15 (75) |
| Pomalidomide | 7 (35)/7
(35) |
| Bortezomib | 20 (100)/9
(45) |
| Carfilzomib | 6 (30)/6
(30) |
| Autologous
transplant |
15 (75) |
For this study, patients received panobinostat (20 mg on days 1, 3, 5, 15, 17, and 19), lenalidomide (25 mg on days 1-21), and dexamethasone (40 mg on days 1, 8, and 15).
The overall response rate was 45%. This included 1 complete response, 3 very good partial responses, 5 partial responses, and 8 minimal responses. Two patients had stable disease, and 1 progressed.
Among lenalidomide-refractory patients (n=16), the overall response rate was 38%. This included 3 very good partial responses, 3 partial responses, and 7 minimal responses. Two patients had stable disease, and 1 progressed.
The median PFS was 6.5 months overall and among lenalidomide-refractory patients.
Grade 3/4 toxicities were primarily hematologic, including neutropenia (55%), thrombocytopenia (40%), and anemia (5%). Grade 3/4 non-hematologic adverse events included infections (n=4), diarrhea (n=3), pulmonary emboli (n=2), neck pain (n=1), QTc prolongation (n=1), fatigue (n=1), and weight loss (n=1).
“In relapsed/refractory MM patients, panobinostat in combination with lenalidomide and dexamethasone demonstrated durable responses comparable to other recently approved agents, even in lenalidomide-refractory patients with high-risk molecular findings,” Dr Chari said.
“In notable contrast to PANORAMA-1 results, this completely oral regimen is well-tolerated, with no grade 3/4 [gastrointestinal] toxicities and primarily expected hematologic toxicities.” ![]()
*Information in the abstract differs from that presented at the meeting.
©ASCO/Rodney White
CHICAGO—Combination regimens including the histone deacetylase inhibitor panobinostat can produce durable responses and prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to research presented at the 2015 ASCO Annual Meeting.
In a phase 2 trial, panobinostat plus lenalidomide and dexamethasone produced durable responses, even in high-risk, lenalidomide-refractory MM patients.
In a phase 3 trial, panobinostat in combination with bortezomib and dexamethasone led to a 7.8-month improvement in median PFS over placebo-bortezomib-dexamethasone in patients with relapsed or relapsed and refractory MM who had received 2 or more prior regimens.
Both studies were sponsored by Novartis, the company developing panobinostat.
PANORAMA-1 substudy
PANORAMA-1 was a phase 3, randomized, double-blind, placebo-controlled trial of 768 MM patients. Overall, panobinostat in combination with bortezomib and dexamethasone led to a clinically relevant and statistically significant increase in PFS of about 4 months compared to placebo-bortezomib-dexamethasone.
At ASCO, Jesús San Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain, presented the results of an exploratory analysis of 147 patients in this trial (abstract 8526*).
The patients had relapsed or relapsed and refractory MM and had received 2 or more prior regimens, including bortezomib and an immunomodulatory agent (IMiD).
Disease and treatment characteristics were as follows:
| Panobinostat
(n=73) |
Placebo (n=74) | |
| Disease
characteristics, n (%) |
||
| Relapsed | 39 (53) | 30 (41) |
| Relapsed/refractory | 34 (47) | 43 (58) |
| Prior
therapies, n (%) |
||
| Bortezomib | 73 (100) | 74 (100) |
| Lenalidomide | 28 (38) | 37 (50) |
| Thalidomide | 63 (86) | 50 (68) |
| Bortezomib
+ lenalidomide |
28 (38) | 37 (50) |
| Bortezomib
+ dexamethasone |
69 (95) | 74 (100) |
| Prior
autologous transplant, n (%) |
54 (74) | 47 (64) |
| Median
prior lines of therapy (range) |
3 (2-4) | 3 (2-3) |
The median PFS was 12.5 months in the panobinostat arm, compared to 4.7 months in the placebo arm. Treatment with panobinostat also led to an increase in complete/near complete response rates (21.9% vs 8.1%) and overall response rate (58.9% vs 39.2%).
Common grade 3/4 non-hematologic adverse events in the panobinostat arm and placebo arm, respectively, included diarrhea (33.3% vs 15.1%), asthenia/fatigue (26.4% vs 13.7%), and peripheral neuropathy (16.7% vs 6.8%).
The most common grade 3/4 hematologic abnormalities in the panobinostat arm and placebo arm, respectively, were thrombocytopenia (68.1% vs 44.4%), lymphopenia (48.6% vs 49.3%), and neutropenia (40.3% vs 16.4%).
The percentage of on-treatment deaths was similar between the treatment arms (6.9% vs 6.8%).
“These data provide physicians with a better understanding of the clinical use of panobinostat, an HDAC inhibitor, a promising new drug class for this difficult-to-treat patient population with a high unmet need,” Dr San Miguel said.
Phase 2 trial
Ajai Chari, MD, of Mount Sinai Medical Center in New York, presented the results of a phase 2 study of panobinostat with lenalidomide and weekly dexamethasone in patients with relapsed/refractory MM (abstract 8528*).
There were 20 evaluable patients with a median age of 64 (range, 51-75). They had received a median of 3 prior therapies (range, 1-10). Prior regimens were as follows:
| Prior
therapy |
Exposed/Refractory, n (%) |
| Dexamethasone | 20 (100)/9
(45) |
| Thalidomide | 6 (30)/2
(10) |
| Lenalidomide |
20 (100)/15 (75) |
| Pomalidomide | 7 (35)/7
(35) |
| Bortezomib | 20 (100)/9
(45) |
| Carfilzomib | 6 (30)/6
(30) |
| Autologous
transplant |
15 (75) |
For this study, patients received panobinostat (20 mg on days 1, 3, 5, 15, 17, and 19), lenalidomide (25 mg on days 1-21), and dexamethasone (40 mg on days 1, 8, and 15).
The overall response rate was 45%. This included 1 complete response, 3 very good partial responses, 5 partial responses, and 8 minimal responses. Two patients had stable disease, and 1 progressed.
Among lenalidomide-refractory patients (n=16), the overall response rate was 38%. This included 3 very good partial responses, 3 partial responses, and 7 minimal responses. Two patients had stable disease, and 1 progressed.
The median PFS was 6.5 months overall and among lenalidomide-refractory patients.
Grade 3/4 toxicities were primarily hematologic, including neutropenia (55%), thrombocytopenia (40%), and anemia (5%). Grade 3/4 non-hematologic adverse events included infections (n=4), diarrhea (n=3), pulmonary emboli (n=2), neck pain (n=1), QTc prolongation (n=1), fatigue (n=1), and weight loss (n=1).
“In relapsed/refractory MM patients, panobinostat in combination with lenalidomide and dexamethasone demonstrated durable responses comparable to other recently approved agents, even in lenalidomide-refractory patients with high-risk molecular findings,” Dr Chari said.
“In notable contrast to PANORAMA-1 results, this completely oral regimen is well-tolerated, with no grade 3/4 [gastrointestinal] toxicities and primarily expected hematologic toxicities.” ![]()
*Information in the abstract differs from that presented at the meeting.
VIDEO: Consider cost in anastrozole vs. tamoxifen for DCIS
CHICAGO – Anastrozole may top tamoxifen in reducing the risk of disease recurrence in postmenopausal ductal carcinoma in situ (DCIS), particularly in younger women, but which drug holds a cost advantage?
“How much do you want to pay in dollars or in side effects to achieve the extra benefit is an individual decision that a woman has to make with her physician,” said Dr. Richard Margolese, professor of surgical oncology at Jewish General Hospital, McGill University, Montreal.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Margolese discussed the cost and side effect considerations that could determine a decision between anastrozole and tamoxifen.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Anastrozole may top tamoxifen in reducing the risk of disease recurrence in postmenopausal ductal carcinoma in situ (DCIS), particularly in younger women, but which drug holds a cost advantage?
“How much do you want to pay in dollars or in side effects to achieve the extra benefit is an individual decision that a woman has to make with her physician,” said Dr. Richard Margolese, professor of surgical oncology at Jewish General Hospital, McGill University, Montreal.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Margolese discussed the cost and side effect considerations that could determine a decision between anastrozole and tamoxifen.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Anastrozole may top tamoxifen in reducing the risk of disease recurrence in postmenopausal ductal carcinoma in situ (DCIS), particularly in younger women, but which drug holds a cost advantage?
“How much do you want to pay in dollars or in side effects to achieve the extra benefit is an individual decision that a woman has to make with her physician,” said Dr. Richard Margolese, professor of surgical oncology at Jewish General Hospital, McGill University, Montreal.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Margolese discussed the cost and side effect considerations that could determine a decision between anastrozole and tamoxifen.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2015 ASCO ANNUAL MEETING
VIDEO: Pacritinib safe with thrombocytopenia in myelofibrosis
CHICAGO – The investigational oral Janus kinase 2 (JAK2) inhibitor pacritinib may offer a new myelofibrosis treatment option for patients with baseline thrombocytopenia.
Analyses from an ongoing phase III trial of pacritinib, reported at the annual meeting of the American Society of Clinical Oncology, indicate that the JAK2 inhibitor is superior to best available therapy for alleviating splenomegaly and other symptoms of myelofibrosis.
“In the very short term, it very clearly identifies a therapy that’s very impactful for those individuals with significant thrombocytopenia and potentially those with anemia,” noted lead study author Dr. Ruben A. Mesa, deputy director of the Mayo Clinic Cancer Center in Scottsdale, Ariz.
In a video interview, Dr. Mesa discussed the study findings so far and the potential implications for patients with myelofibrosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The investigational oral Janus kinase 2 (JAK2) inhibitor pacritinib may offer a new myelofibrosis treatment option for patients with baseline thrombocytopenia.
Analyses from an ongoing phase III trial of pacritinib, reported at the annual meeting of the American Society of Clinical Oncology, indicate that the JAK2 inhibitor is superior to best available therapy for alleviating splenomegaly and other symptoms of myelofibrosis.
“In the very short term, it very clearly identifies a therapy that’s very impactful for those individuals with significant thrombocytopenia and potentially those with anemia,” noted lead study author Dr. Ruben A. Mesa, deputy director of the Mayo Clinic Cancer Center in Scottsdale, Ariz.
In a video interview, Dr. Mesa discussed the study findings so far and the potential implications for patients with myelofibrosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The investigational oral Janus kinase 2 (JAK2) inhibitor pacritinib may offer a new myelofibrosis treatment option for patients with baseline thrombocytopenia.
Analyses from an ongoing phase III trial of pacritinib, reported at the annual meeting of the American Society of Clinical Oncology, indicate that the JAK2 inhibitor is superior to best available therapy for alleviating splenomegaly and other symptoms of myelofibrosis.
“In the very short term, it very clearly identifies a therapy that’s very impactful for those individuals with significant thrombocytopenia and potentially those with anemia,” noted lead study author Dr. Ruben A. Mesa, deputy director of the Mayo Clinic Cancer Center in Scottsdale, Ariz.
In a video interview, Dr. Mesa discussed the study findings so far and the potential implications for patients with myelofibrosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2015 ASCO ANNUAL MEETING
CAR T-cell therapy seems feasible for NHL, MM

©ASCO/Rodney White
CHICAGO—The CD19-directed chimeric antigen receptor (CAR) T-cell therapy CTL019 has shown promise for treating non-Hodgkin lymphoma (NHL) and may be a feasible treatment option for multiple myeloma (MM) as well, according to researchers.
In an ongoing phase 2 trial, CTL019 has produced durable responses in patients with relapsed or refractory NHL.
And early results of a phase 1 trial suggest CTL019 can provide clinical benefit in heavily pretreated patients with MM.
Both studies were presented at the 2015 ASCO Annual Meeting. The University of Pennsylvania and Novartis have an exclusive global collaboration to research, develop, and commercialize CTL019.
CTL019 in NHL
Stephen Schuster, MD, of the Abramson Cancer Center of the University of Pennsylvania in Philadelphia, presented results of the phase 2 NHL trial (abstract 8516*).
The trial included 20 evaluable patients, 13 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma (FL). At the time of presentation, the median follow-up was 274 days for the patients with DLBCL and 290 days for those with FL.
The overall response rate was 100% in patients with FL and 50% in those with DLBCL. Thirteen patients responded to the therapy, including 11 who achieved a complete response and 2 who experienced a partial response.
Six patients with a partial response to treatment at 3 months achieved a complete response by 6 months. Two patients with a partial response experienced disease progression at 6 and 12 months after treatment.
The researchers said toxicity appeared to be acceptable, with primarily grade 2 cytokine release syndrome (CRS). Two patients developed CRS of grade 3 or higher at peak T-cell expansion. There were no deaths from CRS.
“The results from this ongoing study of CTL019 are encouraging, as we now have data through 6 months showing that patients may have achieved durable overall response rates,” Dr Schuster said. “These data support our ongoing efforts to determine the potential role of CTL019 in improving outcomes for patients with certain types of B-cell lymphomas.”
CTL019 in MM
Alfred Garfall, MD, of the Abramson Cancer Center, presented preliminary results of an ongoing phase 1 study investigating CTL019 in patients with MM (abstract 8517*).
Dr Garfall and his colleagues hypothesized that CTL019 would exhibit efficacy in MM due to low-level CD19 expression on MM plasma cells or CD19 expression in drug-resistant, disease-propagating subsets of the MM clone.
The study included 5 patients who experienced disease progression within a year of a prior autologous stem cell transplant and were medically fit to undergo a second autologous transplant. The patients had received a median of 7.5 prior lines of therapy.
“We found potential evidence of clinical benefit in 3 of 4 patients with more than 100 days of follow-up,” Dr Garfall said.
Two patients experienced longer, deeper responses, and 1 patient experienced CRS.
The data suggest “it is safe and feasible to manufacture and administered CTL019 to refractory multiple myeloma patients,” Dr Garfall said.
*Information in the abstract differs from that presented at the meeting.

©ASCO/Rodney White
CHICAGO—The CD19-directed chimeric antigen receptor (CAR) T-cell therapy CTL019 has shown promise for treating non-Hodgkin lymphoma (NHL) and may be a feasible treatment option for multiple myeloma (MM) as well, according to researchers.
In an ongoing phase 2 trial, CTL019 has produced durable responses in patients with relapsed or refractory NHL.
And early results of a phase 1 trial suggest CTL019 can provide clinical benefit in heavily pretreated patients with MM.
Both studies were presented at the 2015 ASCO Annual Meeting. The University of Pennsylvania and Novartis have an exclusive global collaboration to research, develop, and commercialize CTL019.
CTL019 in NHL
Stephen Schuster, MD, of the Abramson Cancer Center of the University of Pennsylvania in Philadelphia, presented results of the phase 2 NHL trial (abstract 8516*).
The trial included 20 evaluable patients, 13 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma (FL). At the time of presentation, the median follow-up was 274 days for the patients with DLBCL and 290 days for those with FL.
The overall response rate was 100% in patients with FL and 50% in those with DLBCL. Thirteen patients responded to the therapy, including 11 who achieved a complete response and 2 who experienced a partial response.
Six patients with a partial response to treatment at 3 months achieved a complete response by 6 months. Two patients with a partial response experienced disease progression at 6 and 12 months after treatment.
The researchers said toxicity appeared to be acceptable, with primarily grade 2 cytokine release syndrome (CRS). Two patients developed CRS of grade 3 or higher at peak T-cell expansion. There were no deaths from CRS.
“The results from this ongoing study of CTL019 are encouraging, as we now have data through 6 months showing that patients may have achieved durable overall response rates,” Dr Schuster said. “These data support our ongoing efforts to determine the potential role of CTL019 in improving outcomes for patients with certain types of B-cell lymphomas.”
CTL019 in MM
Alfred Garfall, MD, of the Abramson Cancer Center, presented preliminary results of an ongoing phase 1 study investigating CTL019 in patients with MM (abstract 8517*).
Dr Garfall and his colleagues hypothesized that CTL019 would exhibit efficacy in MM due to low-level CD19 expression on MM plasma cells or CD19 expression in drug-resistant, disease-propagating subsets of the MM clone.
The study included 5 patients who experienced disease progression within a year of a prior autologous stem cell transplant and were medically fit to undergo a second autologous transplant. The patients had received a median of 7.5 prior lines of therapy.
“We found potential evidence of clinical benefit in 3 of 4 patients with more than 100 days of follow-up,” Dr Garfall said.
Two patients experienced longer, deeper responses, and 1 patient experienced CRS.
The data suggest “it is safe and feasible to manufacture and administered CTL019 to refractory multiple myeloma patients,” Dr Garfall said.
*Information in the abstract differs from that presented at the meeting.

©ASCO/Rodney White
CHICAGO—The CD19-directed chimeric antigen receptor (CAR) T-cell therapy CTL019 has shown promise for treating non-Hodgkin lymphoma (NHL) and may be a feasible treatment option for multiple myeloma (MM) as well, according to researchers.
In an ongoing phase 2 trial, CTL019 has produced durable responses in patients with relapsed or refractory NHL.
And early results of a phase 1 trial suggest CTL019 can provide clinical benefit in heavily pretreated patients with MM.
Both studies were presented at the 2015 ASCO Annual Meeting. The University of Pennsylvania and Novartis have an exclusive global collaboration to research, develop, and commercialize CTL019.
CTL019 in NHL
Stephen Schuster, MD, of the Abramson Cancer Center of the University of Pennsylvania in Philadelphia, presented results of the phase 2 NHL trial (abstract 8516*).
The trial included 20 evaluable patients, 13 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma (FL). At the time of presentation, the median follow-up was 274 days for the patients with DLBCL and 290 days for those with FL.
The overall response rate was 100% in patients with FL and 50% in those with DLBCL. Thirteen patients responded to the therapy, including 11 who achieved a complete response and 2 who experienced a partial response.
Six patients with a partial response to treatment at 3 months achieved a complete response by 6 months. Two patients with a partial response experienced disease progression at 6 and 12 months after treatment.
The researchers said toxicity appeared to be acceptable, with primarily grade 2 cytokine release syndrome (CRS). Two patients developed CRS of grade 3 or higher at peak T-cell expansion. There were no deaths from CRS.
“The results from this ongoing study of CTL019 are encouraging, as we now have data through 6 months showing that patients may have achieved durable overall response rates,” Dr Schuster said. “These data support our ongoing efforts to determine the potential role of CTL019 in improving outcomes for patients with certain types of B-cell lymphomas.”
CTL019 in MM
Alfred Garfall, MD, of the Abramson Cancer Center, presented preliminary results of an ongoing phase 1 study investigating CTL019 in patients with MM (abstract 8517*).
Dr Garfall and his colleagues hypothesized that CTL019 would exhibit efficacy in MM due to low-level CD19 expression on MM plasma cells or CD19 expression in drug-resistant, disease-propagating subsets of the MM clone.
The study included 5 patients who experienced disease progression within a year of a prior autologous stem cell transplant and were medically fit to undergo a second autologous transplant. The patients had received a median of 7.5 prior lines of therapy.
“We found potential evidence of clinical benefit in 3 of 4 patients with more than 100 days of follow-up,” Dr Garfall said.
Two patients experienced longer, deeper responses, and 1 patient experienced CRS.
The data suggest “it is safe and feasible to manufacture and administered CTL019 to refractory multiple myeloma patients,” Dr Garfall said.
*Information in the abstract differs from that presented at the meeting.
ASCO: Adjuvant denosumab halves fracture risk for breast cancer patients on AIs
CHICAGO – Adjuvant denosumab is efficacious and safe for reducing fracture risk among women taking aromatase inhibitors (AIs) as part of their treatment for early breast cancer, finds the Austrian Breast & Colorectal Cancer Study Group’s study 18 (ABCSG-18).
Compared with peers randomized to placebo in the phase III trial, women randomized to the antiresorptive monoclonal antibody at the dose typically used to treat osteoporosis were half as likely to experience a first clinical fracture, first author Dr. Michael Gnant reported at the annual meeting of the American Society of Clinical Oncology. The benefit was similar whether women had normal bone mineral density at baseline or already had osteopenia.
Patients in the denosumab group did not have a significantly higher rate of adverse events, including the much-feared complication of osteonecrosis of the jaw.
“The actual fracture risk of postmenopausal breast cancer patients on AIs is substantial and may have been underestimated until today,” commented Dr. Gnant, professor of surgery at the Medical University of Vienna. “In these patients with only a modest risk of disease recurrence, adjuvant denosumab significantly reduced the bone side effects of AI treatment. We therefore believe that denosumab 60 mg every 6 months should be considered for clinical practice.”
“Today, several clinical practice guidelines advocate the use of bisphosphonates for breast cancer patients receiving AIs, however, only if they are at high risk for fractures,” he further noted. However, “patients with normal baseline bone mineral density showed a similar fracture risk but also similar benefit from denosumab as compared to patients with baseline T scores below –1, indicating that DEXA scans may be an insufficient way to assess the individual patient’s fracture risk. In view of the benefits in this particular patient subgroup, we may have to rediscuss our current clinical practice guidelines.”
Invited discussant Dr. Robert E. Coleman of the University of Sheffield and Weston Park Hospital in England, said, “It’s very important to dissect out fractures related to subsequent recurrence from fractures due to poor bone health.” Most of the reduction in fracture risk in ABCSG-18 appeared to be because of prevention of fractures before any recurrence, whereas most of that in the AZURE trial (Adjuvant Zoledronic Acid to Reduce Recurrence) of an adjuvant bisphosphonate, another type of antiresorptive agent, appeared to be because of prevention of fractures from bone metastases. “So I think we are seeing something very different with denosumab to what we’ve seen to date with a bisphosphonate,” he said.
“As oncologists, we are somewhat wedded to measuring bone mineral density as the reason for giving bone-targeted therapy to protect [against] bone loss, but there are much better ways of predicting fracture with online algorithms such as FRAX [Fracture Risk Assessment Tool] and others,” Dr. Coleman further commented. “And bone mineral density is a pretty poor predictor of fracture, so it’s perhaps not surprising that the risk reductions were fairly similar” across bone mineral density subgroups.
During a question and answer period, session attendee Dr. Toru Watanabe, Hamamatsu (Japan) Oncology Center, said, “It is really clear that the osteoporosis-related fracture is prevented by denosumab at the dose usually used for the treatment of osteoporosis. That part is very clear. My question is, the same dose is being tested for modifying overall survival or progression-free survival. Don’t you think it’s necessary to conduct some kind of dose-finding trial?”
Two studies are addressing the impact of denosumab on breast cancer outcomes, according to Dr. Gnant: the investigators’ ABCSG-18 study and the Study of Denosumab as Adjuvant Treatment for Women With High-Risk Early Breast Cancer Receiving Neoadjuvant or Adjuvant Therapy (D-CARE), which is using a higher initial dose and tapering after 1 year. “So we will have that indirect comparison at least. My personal expectation would be that there is a trade-off potentially between efficacy and tolerability,” he commented.
The 3,425 postmenopausal breast cancer patients in ABCSG-18 were randomized evenly to receive 60 mg of denosumab or placebo every 6 months. Denosumab is approved by the Food and Drug Administration for the prevention and treatment of fractures due to bone metastases (brand name Xgeva) and osteoporosis after menopause (brand name Prolia), as well as other indications. The study used the dose for postmenopausal osteoporosis, which is much lower than that typically used for bone metastases (120 mg every 4 weeks), Dr. Gnant noted.
Main results showed that denosumab was highly efficacious in reducing the risk of first clinical fractures, meaning those that were clinically evident and causing symptoms (hazard ratio, 0.50; P less than .0001), according to data presented at the meeting and simultaneously published (Lancet 2015 May 31).
The estimated 6-year fracture rate was about 10% in the denosumab group and 20% in the placebo group. “Please note that the frequency of clinical fractures reported in this trial that is focusing on bone health is markedly higher than fracture rates reported in previous large AI trials. Obviously, we had a tendency to underreport them in those trials,” Dr. Gnant commented. “The true magnitude of the problem in clinical practice is likely reflected in the placebo group … with approximately one out of five patients experiencing a new clinical fracture within 5-6 years of adjuvant AI treatment.”
Benefit was similar across numerous patient subgroups studied, including the subgroups of women who had a baseline bone mineral density T-score of less than –1 and women who had a baseline bone mineral density T-score of –1 or greater.
Additionally, the denosumab group had improvements from baseline in bone mineral density of the lumbar spine, total hip, and femoral neck, whereas the placebo group had worsening at all sites (P less than .0001 between groups for each site). And at 36 months, the denosumab group had significantly lower risks of both new vertebral fractures and new or worsening vertebral fractures.
“Adjuvant denosumab at this dose and schedule is safe,” Dr. Gnant maintained. The two groups had similar rates of various adverse events, with musculoskeletal disorders and vascular disorders (including hot flashes) predominating. “This means that we are in essence reporting the side effects of the underlying adjuvant AI treatment,” he noted.
There were 31 cases of dental issues, but none met diagnostic criteria for osteonecrosis of the jaw. “We can safely say that at this dose of denosumab, 60 mg twice yearly, ONJ is not an issue,” Dr. Gnant commented. Additionally, none of the women experienced atypical fractures.
Dr. Gnant disclosed employment of an immediate family member with Sandoz; receipt of honoraria from Amgen, AstraZeneca, GlaxoSmithKline, NanoString Technologies, Novartis, and Roche Pharma AG; a consulting or advisory role with Accelsiors, AstraZeneca, and Novartis; and receipt of research funding from GlaxoSmithKline, Novartis, Pfizer, Roche Pharma AG, Sanofi, and Smiths Medical. The trial was sponsored by Amgen.
CHICAGO – Adjuvant denosumab is efficacious and safe for reducing fracture risk among women taking aromatase inhibitors (AIs) as part of their treatment for early breast cancer, finds the Austrian Breast & Colorectal Cancer Study Group’s study 18 (ABCSG-18).
Compared with peers randomized to placebo in the phase III trial, women randomized to the antiresorptive monoclonal antibody at the dose typically used to treat osteoporosis were half as likely to experience a first clinical fracture, first author Dr. Michael Gnant reported at the annual meeting of the American Society of Clinical Oncology. The benefit was similar whether women had normal bone mineral density at baseline or already had osteopenia.
Patients in the denosumab group did not have a significantly higher rate of adverse events, including the much-feared complication of osteonecrosis of the jaw.
“The actual fracture risk of postmenopausal breast cancer patients on AIs is substantial and may have been underestimated until today,” commented Dr. Gnant, professor of surgery at the Medical University of Vienna. “In these patients with only a modest risk of disease recurrence, adjuvant denosumab significantly reduced the bone side effects of AI treatment. We therefore believe that denosumab 60 mg every 6 months should be considered for clinical practice.”
“Today, several clinical practice guidelines advocate the use of bisphosphonates for breast cancer patients receiving AIs, however, only if they are at high risk for fractures,” he further noted. However, “patients with normal baseline bone mineral density showed a similar fracture risk but also similar benefit from denosumab as compared to patients with baseline T scores below –1, indicating that DEXA scans may be an insufficient way to assess the individual patient’s fracture risk. In view of the benefits in this particular patient subgroup, we may have to rediscuss our current clinical practice guidelines.”
Invited discussant Dr. Robert E. Coleman of the University of Sheffield and Weston Park Hospital in England, said, “It’s very important to dissect out fractures related to subsequent recurrence from fractures due to poor bone health.” Most of the reduction in fracture risk in ABCSG-18 appeared to be because of prevention of fractures before any recurrence, whereas most of that in the AZURE trial (Adjuvant Zoledronic Acid to Reduce Recurrence) of an adjuvant bisphosphonate, another type of antiresorptive agent, appeared to be because of prevention of fractures from bone metastases. “So I think we are seeing something very different with denosumab to what we’ve seen to date with a bisphosphonate,” he said.
“As oncologists, we are somewhat wedded to measuring bone mineral density as the reason for giving bone-targeted therapy to protect [against] bone loss, but there are much better ways of predicting fracture with online algorithms such as FRAX [Fracture Risk Assessment Tool] and others,” Dr. Coleman further commented. “And bone mineral density is a pretty poor predictor of fracture, so it’s perhaps not surprising that the risk reductions were fairly similar” across bone mineral density subgroups.
During a question and answer period, session attendee Dr. Toru Watanabe, Hamamatsu (Japan) Oncology Center, said, “It is really clear that the osteoporosis-related fracture is prevented by denosumab at the dose usually used for the treatment of osteoporosis. That part is very clear. My question is, the same dose is being tested for modifying overall survival or progression-free survival. Don’t you think it’s necessary to conduct some kind of dose-finding trial?”
Two studies are addressing the impact of denosumab on breast cancer outcomes, according to Dr. Gnant: the investigators’ ABCSG-18 study and the Study of Denosumab as Adjuvant Treatment for Women With High-Risk Early Breast Cancer Receiving Neoadjuvant or Adjuvant Therapy (D-CARE), which is using a higher initial dose and tapering after 1 year. “So we will have that indirect comparison at least. My personal expectation would be that there is a trade-off potentially between efficacy and tolerability,” he commented.
The 3,425 postmenopausal breast cancer patients in ABCSG-18 were randomized evenly to receive 60 mg of denosumab or placebo every 6 months. Denosumab is approved by the Food and Drug Administration for the prevention and treatment of fractures due to bone metastases (brand name Xgeva) and osteoporosis after menopause (brand name Prolia), as well as other indications. The study used the dose for postmenopausal osteoporosis, which is much lower than that typically used for bone metastases (120 mg every 4 weeks), Dr. Gnant noted.
Main results showed that denosumab was highly efficacious in reducing the risk of first clinical fractures, meaning those that were clinically evident and causing symptoms (hazard ratio, 0.50; P less than .0001), according to data presented at the meeting and simultaneously published (Lancet 2015 May 31).
The estimated 6-year fracture rate was about 10% in the denosumab group and 20% in the placebo group. “Please note that the frequency of clinical fractures reported in this trial that is focusing on bone health is markedly higher than fracture rates reported in previous large AI trials. Obviously, we had a tendency to underreport them in those trials,” Dr. Gnant commented. “The true magnitude of the problem in clinical practice is likely reflected in the placebo group … with approximately one out of five patients experiencing a new clinical fracture within 5-6 years of adjuvant AI treatment.”
Benefit was similar across numerous patient subgroups studied, including the subgroups of women who had a baseline bone mineral density T-score of less than –1 and women who had a baseline bone mineral density T-score of –1 or greater.
Additionally, the denosumab group had improvements from baseline in bone mineral density of the lumbar spine, total hip, and femoral neck, whereas the placebo group had worsening at all sites (P less than .0001 between groups for each site). And at 36 months, the denosumab group had significantly lower risks of both new vertebral fractures and new or worsening vertebral fractures.
“Adjuvant denosumab at this dose and schedule is safe,” Dr. Gnant maintained. The two groups had similar rates of various adverse events, with musculoskeletal disorders and vascular disorders (including hot flashes) predominating. “This means that we are in essence reporting the side effects of the underlying adjuvant AI treatment,” he noted.
There were 31 cases of dental issues, but none met diagnostic criteria for osteonecrosis of the jaw. “We can safely say that at this dose of denosumab, 60 mg twice yearly, ONJ is not an issue,” Dr. Gnant commented. Additionally, none of the women experienced atypical fractures.
Dr. Gnant disclosed employment of an immediate family member with Sandoz; receipt of honoraria from Amgen, AstraZeneca, GlaxoSmithKline, NanoString Technologies, Novartis, and Roche Pharma AG; a consulting or advisory role with Accelsiors, AstraZeneca, and Novartis; and receipt of research funding from GlaxoSmithKline, Novartis, Pfizer, Roche Pharma AG, Sanofi, and Smiths Medical. The trial was sponsored by Amgen.
CHICAGO – Adjuvant denosumab is efficacious and safe for reducing fracture risk among women taking aromatase inhibitors (AIs) as part of their treatment for early breast cancer, finds the Austrian Breast & Colorectal Cancer Study Group’s study 18 (ABCSG-18).
Compared with peers randomized to placebo in the phase III trial, women randomized to the antiresorptive monoclonal antibody at the dose typically used to treat osteoporosis were half as likely to experience a first clinical fracture, first author Dr. Michael Gnant reported at the annual meeting of the American Society of Clinical Oncology. The benefit was similar whether women had normal bone mineral density at baseline or already had osteopenia.
Patients in the denosumab group did not have a significantly higher rate of adverse events, including the much-feared complication of osteonecrosis of the jaw.
“The actual fracture risk of postmenopausal breast cancer patients on AIs is substantial and may have been underestimated until today,” commented Dr. Gnant, professor of surgery at the Medical University of Vienna. “In these patients with only a modest risk of disease recurrence, adjuvant denosumab significantly reduced the bone side effects of AI treatment. We therefore believe that denosumab 60 mg every 6 months should be considered for clinical practice.”
“Today, several clinical practice guidelines advocate the use of bisphosphonates for breast cancer patients receiving AIs, however, only if they are at high risk for fractures,” he further noted. However, “patients with normal baseline bone mineral density showed a similar fracture risk but also similar benefit from denosumab as compared to patients with baseline T scores below –1, indicating that DEXA scans may be an insufficient way to assess the individual patient’s fracture risk. In view of the benefits in this particular patient subgroup, we may have to rediscuss our current clinical practice guidelines.”
Invited discussant Dr. Robert E. Coleman of the University of Sheffield and Weston Park Hospital in England, said, “It’s very important to dissect out fractures related to subsequent recurrence from fractures due to poor bone health.” Most of the reduction in fracture risk in ABCSG-18 appeared to be because of prevention of fractures before any recurrence, whereas most of that in the AZURE trial (Adjuvant Zoledronic Acid to Reduce Recurrence) of an adjuvant bisphosphonate, another type of antiresorptive agent, appeared to be because of prevention of fractures from bone metastases. “So I think we are seeing something very different with denosumab to what we’ve seen to date with a bisphosphonate,” he said.
“As oncologists, we are somewhat wedded to measuring bone mineral density as the reason for giving bone-targeted therapy to protect [against] bone loss, but there are much better ways of predicting fracture with online algorithms such as FRAX [Fracture Risk Assessment Tool] and others,” Dr. Coleman further commented. “And bone mineral density is a pretty poor predictor of fracture, so it’s perhaps not surprising that the risk reductions were fairly similar” across bone mineral density subgroups.
During a question and answer period, session attendee Dr. Toru Watanabe, Hamamatsu (Japan) Oncology Center, said, “It is really clear that the osteoporosis-related fracture is prevented by denosumab at the dose usually used for the treatment of osteoporosis. That part is very clear. My question is, the same dose is being tested for modifying overall survival or progression-free survival. Don’t you think it’s necessary to conduct some kind of dose-finding trial?”
Two studies are addressing the impact of denosumab on breast cancer outcomes, according to Dr. Gnant: the investigators’ ABCSG-18 study and the Study of Denosumab as Adjuvant Treatment for Women With High-Risk Early Breast Cancer Receiving Neoadjuvant or Adjuvant Therapy (D-CARE), which is using a higher initial dose and tapering after 1 year. “So we will have that indirect comparison at least. My personal expectation would be that there is a trade-off potentially between efficacy and tolerability,” he commented.
The 3,425 postmenopausal breast cancer patients in ABCSG-18 were randomized evenly to receive 60 mg of denosumab or placebo every 6 months. Denosumab is approved by the Food and Drug Administration for the prevention and treatment of fractures due to bone metastases (brand name Xgeva) and osteoporosis after menopause (brand name Prolia), as well as other indications. The study used the dose for postmenopausal osteoporosis, which is much lower than that typically used for bone metastases (120 mg every 4 weeks), Dr. Gnant noted.
Main results showed that denosumab was highly efficacious in reducing the risk of first clinical fractures, meaning those that were clinically evident and causing symptoms (hazard ratio, 0.50; P less than .0001), according to data presented at the meeting and simultaneously published (Lancet 2015 May 31).
The estimated 6-year fracture rate was about 10% in the denosumab group and 20% in the placebo group. “Please note that the frequency of clinical fractures reported in this trial that is focusing on bone health is markedly higher than fracture rates reported in previous large AI trials. Obviously, we had a tendency to underreport them in those trials,” Dr. Gnant commented. “The true magnitude of the problem in clinical practice is likely reflected in the placebo group … with approximately one out of five patients experiencing a new clinical fracture within 5-6 years of adjuvant AI treatment.”
Benefit was similar across numerous patient subgroups studied, including the subgroups of women who had a baseline bone mineral density T-score of less than –1 and women who had a baseline bone mineral density T-score of –1 or greater.
Additionally, the denosumab group had improvements from baseline in bone mineral density of the lumbar spine, total hip, and femoral neck, whereas the placebo group had worsening at all sites (P less than .0001 between groups for each site). And at 36 months, the denosumab group had significantly lower risks of both new vertebral fractures and new or worsening vertebral fractures.
“Adjuvant denosumab at this dose and schedule is safe,” Dr. Gnant maintained. The two groups had similar rates of various adverse events, with musculoskeletal disorders and vascular disorders (including hot flashes) predominating. “This means that we are in essence reporting the side effects of the underlying adjuvant AI treatment,” he noted.
There were 31 cases of dental issues, but none met diagnostic criteria for osteonecrosis of the jaw. “We can safely say that at this dose of denosumab, 60 mg twice yearly, ONJ is not an issue,” Dr. Gnant commented. Additionally, none of the women experienced atypical fractures.
Dr. Gnant disclosed employment of an immediate family member with Sandoz; receipt of honoraria from Amgen, AstraZeneca, GlaxoSmithKline, NanoString Technologies, Novartis, and Roche Pharma AG; a consulting or advisory role with Accelsiors, AstraZeneca, and Novartis; and receipt of research funding from GlaxoSmithKline, Novartis, Pfizer, Roche Pharma AG, Sanofi, and Smiths Medical. The trial was sponsored by Amgen.
AT THE 2015 ASCO ANNUAL MEETING
Key clinical point: Denosumab reduces the risk of clinical fractures in postmenopausal women taking AIs for early breast cancer.
Major finding: The denosumab group was half as likely to have a first clinical fracture as the placebo group (HR, 0.50).
Data source: A randomized phase III trial among 3,425 postmenopausal women with early breast cancer taking AIs.
Disclosures: Dr. Gnant disclosed employment of an immediate family member with Sandoz; receipt of honoraria from Amgen, AstraZeneca, GlaxoSmithKline, NanoString Technologies, Novartis, and Roche Pharma AG; a consulting or advisory role with Accelsiors, AstraZeneca, and Novartis; and receipt of research funding from GlaxoSmithKline, Novartis, Pfizer, Roche Pharma AG, Sanofi, and Smiths Medical. The trial was sponsored by Amgen.
A better FLT3 inhibitor for AML?

© ASCO/Scott Morgan
CHICAGO—A dual inhibitor of FLT3 and Axl may produce more durable responses than other FLT3 inhibitors and improve survival in patients with FLT3-positive, relapsed or refractory acute myeloid leukemia (AML), according to a speaker at the 2015 ASCO Annual Meeting.
The FLT3/Axl inhibitor, ASP2215, has not been compared against other FLT3 inhibitors directly, and the data presented were from a phase 1/2 study.
However, the speaker said ASP2215 provided “potent and sustained” inhibition of FLT3 and produced an overall response rate (ORR) of 52% among FLT3-positive patients.
The median duration of response for these patients was 18 weeks, and their median overall survival was about 27 weeks.
Mark J. Levis, MD, PhD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore, Maryland, presented these results at ASCO as abstract 7003.*
“We’ve been studying FLT3 inhibitors for a number of years now,” Dr Levis began, “and we think they show significant clinical promise, [but] they also have problems.”
He noted that some of these drugs haven’t been particularly safe or well-tolerated. They can cause gastrointestinal toxicity, hand-foot syndrome, QT prolongation, and myelosuppression.
However, the most intriguing problem with FLT3 inhibitors, according to Dr Levis, is the emergence of resistance-conferring point mutations observed in studies of some of the newer drugs, such as sorafenib and quizartinib.
“So in that context, here we have ASP2215,” Dr Levis said. “This is a type 1 FLT3 tyrosine kinase inhibitor, and, as such, it has activity against not only wild-type and ITD-mutated FLT3 but also against those resistance-conferring point mutations typically found in the activation loop at the so-called gatekeeper residue (F691L).”
With this in mind, he and his colleagues conducted a phase 1/2 trial of ASP2215. The study was sponsored by Astellas Pharma Global Development, Inc., the company developing ASP2215.
The trial was open to patients with relapsed or refractory AML, irrespective of their FLT3 mutation status. The researchers’ goal was to identify a safe, tolerable dose of ASP2215 that fully inhibited FLT3.
The team used a standard 3+3 design, with dose levels ranging from 20 mg to 450 mg once daily. They expanded every cohort until they reached a dose-limiting toxicity.
In all, the trial enrolled 198 patients, 24 in the dose-escalation cohorts and 174 in the dose-expansion cohorts. The patients’ median age was 62 (range, 21-90), and 53.1% were male.
Nearly 66% of patients had FLT3 mutations, 29.4% were FLT3-negative, and 5.2% had unknown FLT3 status. About 35% of patients had received 1 prior line of therapy, 26.3% had 2, 33.5% had 3 or more, and 5.7% had an unknown number of prior therapies.
Safety results
In the 194 patients who were evaluable for safety, treatment-emergent adverse events included diarrhea (13.4%), fatigue (12.4%), AST increase (11.3%), ALT increase (9.3%), thrombocytopenia (7.7%), anemia (7.2%), peripheral edema (7.2%), constipation (6.7%), nausea (6.7%), dizziness (6.2%), vomiting (5.7%), and dysgeusia (5.2%).
Serious adverse events included febrile neutropenia (27.3%), sepsis (11.9%), disease progression (10.3%), pneumonia (8.8%), hypotension (5.7%), and respiratory failure (5.7%).
“The kinds of side effects we saw were typical for a relapsed/refractory AML population,” Dr Levis said. “Nothing really stood out. Any trial of relapsed/refractory AML is going to have febrile neutropenia and sepsis, and those were our dominant, serious adverse events. There was no real safety signal here that was unique to the drug, we felt.”
The researchers said the maximum-tolerated dose of ASP2215 was 300 mg, as 2 patients who received the 450 mg dose experienced dose-limiting toxicities. One was grade 3 diarrhea, and the other was grade 3 AST elevation.
Response and survival
Among the 127 patients who were FLT3-positive, the ORR was 52% (n=66). The complete response (CR) rate was 6.3% (n=8). The composite CR rate, which includes CRs with incomplete hematologic recovery (CRi) and incomplete platelet recovery (CRp), was 40.9% (n=52). And the partial response (PR) rate was 11% (n=14).
“As we scale up the dose, the PRs shift on over to CRis, and the dominant response is, in fact, a complete response with incomplete count recovery,” Dr Levis said. “The categories where we had the largest number of responses were the 120 mg and 200 mg categories. We didn’t really have enough patients in the 300 mg category to comment on it. ”
For the FLT3-positive patients, the median duration of response was 126 days.
“The duration of response really stood out here,” Dr Levis said. “It’s over 4 months. That is something we really didn’t see with the other drugs, and I suspect that is a reflection of the suppression of the outgrowth of these resistance mutations.”
Unfortunately, FLT3-wild-type patients did not fare as well. The ORR among these patients was 8.8%. None of the patients achieved a CR, 3 had a composite CR (5.3%), and 2 had a PR (3.5%).
Among the FLT3-positive patients, the median overall survival was about 27 weeks. It was 128 days in the 20 mg dose cohort (n=13), 105.5 days in the 40 mg cohort (n=8), 201 days in the 80 mg cohort (n=12), 199 days in the 120 mg cohort (n=40), and 161 days in the 200 mg cohort (n=45). Dr Levis did not present survival data for the 300 mg or 450 mg cohorts, which included 7 and 2 patients, respectively.
“[Relapsed/refractory AML] is a population that has a median survival of about 3 months with conventional therapy, at least by historical publications,” Dr Levis noted. “If you look at survival in this trial, patients treated at the FLT3-inhibitory doses [had a] greater than 6-month median survival.”
He added that studies of ASP2215 in combination with other agents are ongoing in patients with newly diagnosed AML. And phase 3 trials of ASP2215 at the 120 mg dose, with the option of scaling up to 200 mg, are planned. ![]()
*Information in the abstract differs from that presented at the meeting.

© ASCO/Scott Morgan
CHICAGO—A dual inhibitor of FLT3 and Axl may produce more durable responses than other FLT3 inhibitors and improve survival in patients with FLT3-positive, relapsed or refractory acute myeloid leukemia (AML), according to a speaker at the 2015 ASCO Annual Meeting.
The FLT3/Axl inhibitor, ASP2215, has not been compared against other FLT3 inhibitors directly, and the data presented were from a phase 1/2 study.
However, the speaker said ASP2215 provided “potent and sustained” inhibition of FLT3 and produced an overall response rate (ORR) of 52% among FLT3-positive patients.
The median duration of response for these patients was 18 weeks, and their median overall survival was about 27 weeks.
Mark J. Levis, MD, PhD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore, Maryland, presented these results at ASCO as abstract 7003.*
“We’ve been studying FLT3 inhibitors for a number of years now,” Dr Levis began, “and we think they show significant clinical promise, [but] they also have problems.”
He noted that some of these drugs haven’t been particularly safe or well-tolerated. They can cause gastrointestinal toxicity, hand-foot syndrome, QT prolongation, and myelosuppression.
However, the most intriguing problem with FLT3 inhibitors, according to Dr Levis, is the emergence of resistance-conferring point mutations observed in studies of some of the newer drugs, such as sorafenib and quizartinib.
“So in that context, here we have ASP2215,” Dr Levis said. “This is a type 1 FLT3 tyrosine kinase inhibitor, and, as such, it has activity against not only wild-type and ITD-mutated FLT3 but also against those resistance-conferring point mutations typically found in the activation loop at the so-called gatekeeper residue (F691L).”
With this in mind, he and his colleagues conducted a phase 1/2 trial of ASP2215. The study was sponsored by Astellas Pharma Global Development, Inc., the company developing ASP2215.
The trial was open to patients with relapsed or refractory AML, irrespective of their FLT3 mutation status. The researchers’ goal was to identify a safe, tolerable dose of ASP2215 that fully inhibited FLT3.
The team used a standard 3+3 design, with dose levels ranging from 20 mg to 450 mg once daily. They expanded every cohort until they reached a dose-limiting toxicity.
In all, the trial enrolled 198 patients, 24 in the dose-escalation cohorts and 174 in the dose-expansion cohorts. The patients’ median age was 62 (range, 21-90), and 53.1% were male.
Nearly 66% of patients had FLT3 mutations, 29.4% were FLT3-negative, and 5.2% had unknown FLT3 status. About 35% of patients had received 1 prior line of therapy, 26.3% had 2, 33.5% had 3 or more, and 5.7% had an unknown number of prior therapies.
Safety results
In the 194 patients who were evaluable for safety, treatment-emergent adverse events included diarrhea (13.4%), fatigue (12.4%), AST increase (11.3%), ALT increase (9.3%), thrombocytopenia (7.7%), anemia (7.2%), peripheral edema (7.2%), constipation (6.7%), nausea (6.7%), dizziness (6.2%), vomiting (5.7%), and dysgeusia (5.2%).
Serious adverse events included febrile neutropenia (27.3%), sepsis (11.9%), disease progression (10.3%), pneumonia (8.8%), hypotension (5.7%), and respiratory failure (5.7%).
“The kinds of side effects we saw were typical for a relapsed/refractory AML population,” Dr Levis said. “Nothing really stood out. Any trial of relapsed/refractory AML is going to have febrile neutropenia and sepsis, and those were our dominant, serious adverse events. There was no real safety signal here that was unique to the drug, we felt.”
The researchers said the maximum-tolerated dose of ASP2215 was 300 mg, as 2 patients who received the 450 mg dose experienced dose-limiting toxicities. One was grade 3 diarrhea, and the other was grade 3 AST elevation.
Response and survival
Among the 127 patients who were FLT3-positive, the ORR was 52% (n=66). The complete response (CR) rate was 6.3% (n=8). The composite CR rate, which includes CRs with incomplete hematologic recovery (CRi) and incomplete platelet recovery (CRp), was 40.9% (n=52). And the partial response (PR) rate was 11% (n=14).
“As we scale up the dose, the PRs shift on over to CRis, and the dominant response is, in fact, a complete response with incomplete count recovery,” Dr Levis said. “The categories where we had the largest number of responses were the 120 mg and 200 mg categories. We didn’t really have enough patients in the 300 mg category to comment on it. ”
For the FLT3-positive patients, the median duration of response was 126 days.
“The duration of response really stood out here,” Dr Levis said. “It’s over 4 months. That is something we really didn’t see with the other drugs, and I suspect that is a reflection of the suppression of the outgrowth of these resistance mutations.”
Unfortunately, FLT3-wild-type patients did not fare as well. The ORR among these patients was 8.8%. None of the patients achieved a CR, 3 had a composite CR (5.3%), and 2 had a PR (3.5%).
Among the FLT3-positive patients, the median overall survival was about 27 weeks. It was 128 days in the 20 mg dose cohort (n=13), 105.5 days in the 40 mg cohort (n=8), 201 days in the 80 mg cohort (n=12), 199 days in the 120 mg cohort (n=40), and 161 days in the 200 mg cohort (n=45). Dr Levis did not present survival data for the 300 mg or 450 mg cohorts, which included 7 and 2 patients, respectively.
“[Relapsed/refractory AML] is a population that has a median survival of about 3 months with conventional therapy, at least by historical publications,” Dr Levis noted. “If you look at survival in this trial, patients treated at the FLT3-inhibitory doses [had a] greater than 6-month median survival.”
He added that studies of ASP2215 in combination with other agents are ongoing in patients with newly diagnosed AML. And phase 3 trials of ASP2215 at the 120 mg dose, with the option of scaling up to 200 mg, are planned. ![]()
*Information in the abstract differs from that presented at the meeting.

© ASCO/Scott Morgan
CHICAGO—A dual inhibitor of FLT3 and Axl may produce more durable responses than other FLT3 inhibitors and improve survival in patients with FLT3-positive, relapsed or refractory acute myeloid leukemia (AML), according to a speaker at the 2015 ASCO Annual Meeting.
The FLT3/Axl inhibitor, ASP2215, has not been compared against other FLT3 inhibitors directly, and the data presented were from a phase 1/2 study.
However, the speaker said ASP2215 provided “potent and sustained” inhibition of FLT3 and produced an overall response rate (ORR) of 52% among FLT3-positive patients.
The median duration of response for these patients was 18 weeks, and their median overall survival was about 27 weeks.
Mark J. Levis, MD, PhD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore, Maryland, presented these results at ASCO as abstract 7003.*
“We’ve been studying FLT3 inhibitors for a number of years now,” Dr Levis began, “and we think they show significant clinical promise, [but] they also have problems.”
He noted that some of these drugs haven’t been particularly safe or well-tolerated. They can cause gastrointestinal toxicity, hand-foot syndrome, QT prolongation, and myelosuppression.
However, the most intriguing problem with FLT3 inhibitors, according to Dr Levis, is the emergence of resistance-conferring point mutations observed in studies of some of the newer drugs, such as sorafenib and quizartinib.
“So in that context, here we have ASP2215,” Dr Levis said. “This is a type 1 FLT3 tyrosine kinase inhibitor, and, as such, it has activity against not only wild-type and ITD-mutated FLT3 but also against those resistance-conferring point mutations typically found in the activation loop at the so-called gatekeeper residue (F691L).”
With this in mind, he and his colleagues conducted a phase 1/2 trial of ASP2215. The study was sponsored by Astellas Pharma Global Development, Inc., the company developing ASP2215.
The trial was open to patients with relapsed or refractory AML, irrespective of their FLT3 mutation status. The researchers’ goal was to identify a safe, tolerable dose of ASP2215 that fully inhibited FLT3.
The team used a standard 3+3 design, with dose levels ranging from 20 mg to 450 mg once daily. They expanded every cohort until they reached a dose-limiting toxicity.
In all, the trial enrolled 198 patients, 24 in the dose-escalation cohorts and 174 in the dose-expansion cohorts. The patients’ median age was 62 (range, 21-90), and 53.1% were male.
Nearly 66% of patients had FLT3 mutations, 29.4% were FLT3-negative, and 5.2% had unknown FLT3 status. About 35% of patients had received 1 prior line of therapy, 26.3% had 2, 33.5% had 3 or more, and 5.7% had an unknown number of prior therapies.
Safety results
In the 194 patients who were evaluable for safety, treatment-emergent adverse events included diarrhea (13.4%), fatigue (12.4%), AST increase (11.3%), ALT increase (9.3%), thrombocytopenia (7.7%), anemia (7.2%), peripheral edema (7.2%), constipation (6.7%), nausea (6.7%), dizziness (6.2%), vomiting (5.7%), and dysgeusia (5.2%).
Serious adverse events included febrile neutropenia (27.3%), sepsis (11.9%), disease progression (10.3%), pneumonia (8.8%), hypotension (5.7%), and respiratory failure (5.7%).
“The kinds of side effects we saw were typical for a relapsed/refractory AML population,” Dr Levis said. “Nothing really stood out. Any trial of relapsed/refractory AML is going to have febrile neutropenia and sepsis, and those were our dominant, serious adverse events. There was no real safety signal here that was unique to the drug, we felt.”
The researchers said the maximum-tolerated dose of ASP2215 was 300 mg, as 2 patients who received the 450 mg dose experienced dose-limiting toxicities. One was grade 3 diarrhea, and the other was grade 3 AST elevation.
Response and survival
Among the 127 patients who were FLT3-positive, the ORR was 52% (n=66). The complete response (CR) rate was 6.3% (n=8). The composite CR rate, which includes CRs with incomplete hematologic recovery (CRi) and incomplete platelet recovery (CRp), was 40.9% (n=52). And the partial response (PR) rate was 11% (n=14).
“As we scale up the dose, the PRs shift on over to CRis, and the dominant response is, in fact, a complete response with incomplete count recovery,” Dr Levis said. “The categories where we had the largest number of responses were the 120 mg and 200 mg categories. We didn’t really have enough patients in the 300 mg category to comment on it. ”
For the FLT3-positive patients, the median duration of response was 126 days.
“The duration of response really stood out here,” Dr Levis said. “It’s over 4 months. That is something we really didn’t see with the other drugs, and I suspect that is a reflection of the suppression of the outgrowth of these resistance mutations.”
Unfortunately, FLT3-wild-type patients did not fare as well. The ORR among these patients was 8.8%. None of the patients achieved a CR, 3 had a composite CR (5.3%), and 2 had a PR (3.5%).
Among the FLT3-positive patients, the median overall survival was about 27 weeks. It was 128 days in the 20 mg dose cohort (n=13), 105.5 days in the 40 mg cohort (n=8), 201 days in the 80 mg cohort (n=12), 199 days in the 120 mg cohort (n=40), and 161 days in the 200 mg cohort (n=45). Dr Levis did not present survival data for the 300 mg or 450 mg cohorts, which included 7 and 2 patients, respectively.
“[Relapsed/refractory AML] is a population that has a median survival of about 3 months with conventional therapy, at least by historical publications,” Dr Levis noted. “If you look at survival in this trial, patients treated at the FLT3-inhibitory doses [had a] greater than 6-month median survival.”
He added that studies of ASP2215 in combination with other agents are ongoing in patients with newly diagnosed AML. And phase 3 trials of ASP2215 at the 120 mg dose, with the option of scaling up to 200 mg, are planned. ![]()
*Information in the abstract differs from that presented at the meeting.
Carfilzomib/dex doubles PFS of relapsed myeloma
CHICAGO – It was nice knowing you, bortezomib, but it’s time to move aside and let carfilzomib take over: Progression-free survival of relapsed multiple myeloma was doubled with a combination of double-dose carfilzomib and dexamethasone compared with bortezomib and dexamethasone.
At a median follow-up of 11.2 months, the primary endpoint of median progression-free survival (PFS) among 464 patients assigned to receive carfilzomib (Kyprolis) and dexamethasone (Kd) was 18.7 months, compared with 9.4 months for 465 patients assigned to bortezomib (Velcade) and dexamethasone (Vd), reported Dr. Meletios Dimopoulos of the University of Athens.
“Kd was superior to Vd regardless of age or prior bortezomib exposure, and represents a new standard of care,” Dr. Dimopoulos said at the annual meeting of the American Society of Clinical Oncology.
He reported results from the phase III ENDEAVOR (A Randomized, Open-Label, Phase III Study of Carfilzomib Plus Dexamethasone vs. Bortezomib Plus Dexamethasone in Patients With Relapsed Multiple Myeloma), the first clinical study to pit two proteasome inhibitors head to head in treatment of multiple myeloma.
“It is becoming clearer that carfilzomib is superior to bortezomib, especially at twice the dose,” said Dr. Jeffrey L. Wolf of the University of California, San Francisco. Dr. Wolf was the invited discussant.
Carfilzomib is approved in the United States as single-agent therapy at a dose of 27 mg/m2 infused over 2-10 minutes with dexamethasone for treatment of patients with relapsed or refractory myeloma.
However, in a phase Ib/II study, carfilzomib administered in a 30-minute infusion at a dose of 56 mg/m2 with dexamethasone produced higher response rates with acceptable toxicities, prompting the investigators to explore the higher-dose regimen against the standard of Vd.
ENDEAVOR
A total of 929 patients, stratified by prior proteasome inhibitor therapy, prior lines of treatment, International Staging System (ISS) score, and route of bortezomib administration (IV vs. subcutaneous) were randomized to either Kd or Vd (with bortezomib delivered either by IV bolus or subcutaneous injection), with both regimens to be continued until disease progression or unacceptable toxicity.
The patients had been treated with at least one but not more than three prior lines of therapy, and could have previously received a proteasome inhibitor if they had a partial response or better to prior treatment, had not been treated with a proteasome inhibitor within the last 6 months, and had not discontinued prior therapy because of toxicity.
The patients also had to have adequate cardiac function (left ventricular ejection fraction of 40% or greater) and creatinine clearance (at least 15 mL/min).
As noted before, median PFS at a median follow-up of 11.2 months was 18.7 months with Kd, vs. 9.4 months with Vd (hazard ratio [HR] 0.53, P < .0001).
PFS was superior with Kd across all subgroups of age, performance status, prior peripheral neuropathy, ISS stage, or risk category. The only exception was among patients with compromised renal function (creatinine clearance less than 30 mL/min), who had comparable PFS in each arm.
PFS was also better with Kd among patients with prior bortezomib exposure (median PFS 15.6 vs. 8.1 months) or no bortezomib exposure (median PFS not reached vs. 11.2 months).
The data are not sufficiently mature for an overall survival analysis, and the study will continue until a final OS analysis can be performed, Dr. Dimopoulos said.
For the secondary endpoint of response rates, Kd also showed superiority, with 77% of patients having some degrees of response, compared with 63% of patients assigned to Vd (P <. 0001). Patients treated with Kd had significantly more complete responses (13% vs. 6%, P < .0001) and very good partial responses (54% vs. 29%, P < .0001).
The median duration of response was 21.3 months for Kd, vs. 10.4 months for Vd (P not shown).
There were more grade 3 or greater adverse events among patients on Kd vs. Vd (73% of patients vs 67%, respectively), and more serious adverse events (48% vs. 36%), but more patients in the Vd arm required dose reduction because of side effects (23% vs. 48%), and more patients on Vd discontinued treatment because of disease progression (25% vs. 36%) or adverse events (14% vs. 16%). In all, four patients on Kd and 3 on Vd died from a cause related to an adverse event.
Rates of dyspnea, hypertension, and cardiac failure were slightly more than twice as high with Kd vs. Vd. Peripheral neuropathy was more common among patients on bortezomib, despite three-fourths of patients in this arm receiving it in the subcutaneous injection form, which has been associated with lower rates of neuropathy than with the IV form of bortezomib.
Dr. Wolf noted that the excess in peripheral neuropathy was not surprising, given that bortezomib was delivered twice weekly and that about 25% of patients received it intravenously.
He also noted that among treatment options for patients with relapsed myeloma, Kd was associated with a cost per progression-free month of about $1,222, compared with $1,059 for Vd, $859 for a combination of carfilzomib, lenalidomide (Revlimid) and dexamethasone, and $1,158 for the combination of elotuzumab, lenalidomide, and dexamethasone, used in the ELOQUENT-2 trial, also presented at ASCO 2015.
The study was sponsored by Onyx, a subsidiary of Amgen. Dr. Dimopoulos disclosed receiving honoraria from and consulting for the company. Dr. Wolf disclosed consulting with Onyx and Amgen, serving on the speakers bureau for Milennium, and receiving travel expense from Onyx Consulting and Milennium.
CHICAGO – It was nice knowing you, bortezomib, but it’s time to move aside and let carfilzomib take over: Progression-free survival of relapsed multiple myeloma was doubled with a combination of double-dose carfilzomib and dexamethasone compared with bortezomib and dexamethasone.
At a median follow-up of 11.2 months, the primary endpoint of median progression-free survival (PFS) among 464 patients assigned to receive carfilzomib (Kyprolis) and dexamethasone (Kd) was 18.7 months, compared with 9.4 months for 465 patients assigned to bortezomib (Velcade) and dexamethasone (Vd), reported Dr. Meletios Dimopoulos of the University of Athens.
“Kd was superior to Vd regardless of age or prior bortezomib exposure, and represents a new standard of care,” Dr. Dimopoulos said at the annual meeting of the American Society of Clinical Oncology.
He reported results from the phase III ENDEAVOR (A Randomized, Open-Label, Phase III Study of Carfilzomib Plus Dexamethasone vs. Bortezomib Plus Dexamethasone in Patients With Relapsed Multiple Myeloma), the first clinical study to pit two proteasome inhibitors head to head in treatment of multiple myeloma.
“It is becoming clearer that carfilzomib is superior to bortezomib, especially at twice the dose,” said Dr. Jeffrey L. Wolf of the University of California, San Francisco. Dr. Wolf was the invited discussant.
Carfilzomib is approved in the United States as single-agent therapy at a dose of 27 mg/m2 infused over 2-10 minutes with dexamethasone for treatment of patients with relapsed or refractory myeloma.
However, in a phase Ib/II study, carfilzomib administered in a 30-minute infusion at a dose of 56 mg/m2 with dexamethasone produced higher response rates with acceptable toxicities, prompting the investigators to explore the higher-dose regimen against the standard of Vd.
ENDEAVOR
A total of 929 patients, stratified by prior proteasome inhibitor therapy, prior lines of treatment, International Staging System (ISS) score, and route of bortezomib administration (IV vs. subcutaneous) were randomized to either Kd or Vd (with bortezomib delivered either by IV bolus or subcutaneous injection), with both regimens to be continued until disease progression or unacceptable toxicity.
The patients had been treated with at least one but not more than three prior lines of therapy, and could have previously received a proteasome inhibitor if they had a partial response or better to prior treatment, had not been treated with a proteasome inhibitor within the last 6 months, and had not discontinued prior therapy because of toxicity.
The patients also had to have adequate cardiac function (left ventricular ejection fraction of 40% or greater) and creatinine clearance (at least 15 mL/min).
As noted before, median PFS at a median follow-up of 11.2 months was 18.7 months with Kd, vs. 9.4 months with Vd (hazard ratio [HR] 0.53, P < .0001).
PFS was superior with Kd across all subgroups of age, performance status, prior peripheral neuropathy, ISS stage, or risk category. The only exception was among patients with compromised renal function (creatinine clearance less than 30 mL/min), who had comparable PFS in each arm.
PFS was also better with Kd among patients with prior bortezomib exposure (median PFS 15.6 vs. 8.1 months) or no bortezomib exposure (median PFS not reached vs. 11.2 months).
The data are not sufficiently mature for an overall survival analysis, and the study will continue until a final OS analysis can be performed, Dr. Dimopoulos said.
For the secondary endpoint of response rates, Kd also showed superiority, with 77% of patients having some degrees of response, compared with 63% of patients assigned to Vd (P <. 0001). Patients treated with Kd had significantly more complete responses (13% vs. 6%, P < .0001) and very good partial responses (54% vs. 29%, P < .0001).
The median duration of response was 21.3 months for Kd, vs. 10.4 months for Vd (P not shown).
There were more grade 3 or greater adverse events among patients on Kd vs. Vd (73% of patients vs 67%, respectively), and more serious adverse events (48% vs. 36%), but more patients in the Vd arm required dose reduction because of side effects (23% vs. 48%), and more patients on Vd discontinued treatment because of disease progression (25% vs. 36%) or adverse events (14% vs. 16%). In all, four patients on Kd and 3 on Vd died from a cause related to an adverse event.
Rates of dyspnea, hypertension, and cardiac failure were slightly more than twice as high with Kd vs. Vd. Peripheral neuropathy was more common among patients on bortezomib, despite three-fourths of patients in this arm receiving it in the subcutaneous injection form, which has been associated with lower rates of neuropathy than with the IV form of bortezomib.
Dr. Wolf noted that the excess in peripheral neuropathy was not surprising, given that bortezomib was delivered twice weekly and that about 25% of patients received it intravenously.
He also noted that among treatment options for patients with relapsed myeloma, Kd was associated with a cost per progression-free month of about $1,222, compared with $1,059 for Vd, $859 for a combination of carfilzomib, lenalidomide (Revlimid) and dexamethasone, and $1,158 for the combination of elotuzumab, lenalidomide, and dexamethasone, used in the ELOQUENT-2 trial, also presented at ASCO 2015.
The study was sponsored by Onyx, a subsidiary of Amgen. Dr. Dimopoulos disclosed receiving honoraria from and consulting for the company. Dr. Wolf disclosed consulting with Onyx and Amgen, serving on the speakers bureau for Milennium, and receiving travel expense from Onyx Consulting and Milennium.
CHICAGO – It was nice knowing you, bortezomib, but it’s time to move aside and let carfilzomib take over: Progression-free survival of relapsed multiple myeloma was doubled with a combination of double-dose carfilzomib and dexamethasone compared with bortezomib and dexamethasone.
At a median follow-up of 11.2 months, the primary endpoint of median progression-free survival (PFS) among 464 patients assigned to receive carfilzomib (Kyprolis) and dexamethasone (Kd) was 18.7 months, compared with 9.4 months for 465 patients assigned to bortezomib (Velcade) and dexamethasone (Vd), reported Dr. Meletios Dimopoulos of the University of Athens.
“Kd was superior to Vd regardless of age or prior bortezomib exposure, and represents a new standard of care,” Dr. Dimopoulos said at the annual meeting of the American Society of Clinical Oncology.
He reported results from the phase III ENDEAVOR (A Randomized, Open-Label, Phase III Study of Carfilzomib Plus Dexamethasone vs. Bortezomib Plus Dexamethasone in Patients With Relapsed Multiple Myeloma), the first clinical study to pit two proteasome inhibitors head to head in treatment of multiple myeloma.
“It is becoming clearer that carfilzomib is superior to bortezomib, especially at twice the dose,” said Dr. Jeffrey L. Wolf of the University of California, San Francisco. Dr. Wolf was the invited discussant.
Carfilzomib is approved in the United States as single-agent therapy at a dose of 27 mg/m2 infused over 2-10 minutes with dexamethasone for treatment of patients with relapsed or refractory myeloma.
However, in a phase Ib/II study, carfilzomib administered in a 30-minute infusion at a dose of 56 mg/m2 with dexamethasone produced higher response rates with acceptable toxicities, prompting the investigators to explore the higher-dose regimen against the standard of Vd.
ENDEAVOR
A total of 929 patients, stratified by prior proteasome inhibitor therapy, prior lines of treatment, International Staging System (ISS) score, and route of bortezomib administration (IV vs. subcutaneous) were randomized to either Kd or Vd (with bortezomib delivered either by IV bolus or subcutaneous injection), with both regimens to be continued until disease progression or unacceptable toxicity.
The patients had been treated with at least one but not more than three prior lines of therapy, and could have previously received a proteasome inhibitor if they had a partial response or better to prior treatment, had not been treated with a proteasome inhibitor within the last 6 months, and had not discontinued prior therapy because of toxicity.
The patients also had to have adequate cardiac function (left ventricular ejection fraction of 40% or greater) and creatinine clearance (at least 15 mL/min).
As noted before, median PFS at a median follow-up of 11.2 months was 18.7 months with Kd, vs. 9.4 months with Vd (hazard ratio [HR] 0.53, P < .0001).
PFS was superior with Kd across all subgroups of age, performance status, prior peripheral neuropathy, ISS stage, or risk category. The only exception was among patients with compromised renal function (creatinine clearance less than 30 mL/min), who had comparable PFS in each arm.
PFS was also better with Kd among patients with prior bortezomib exposure (median PFS 15.6 vs. 8.1 months) or no bortezomib exposure (median PFS not reached vs. 11.2 months).
The data are not sufficiently mature for an overall survival analysis, and the study will continue until a final OS analysis can be performed, Dr. Dimopoulos said.
For the secondary endpoint of response rates, Kd also showed superiority, with 77% of patients having some degrees of response, compared with 63% of patients assigned to Vd (P <. 0001). Patients treated with Kd had significantly more complete responses (13% vs. 6%, P < .0001) and very good partial responses (54% vs. 29%, P < .0001).
The median duration of response was 21.3 months for Kd, vs. 10.4 months for Vd (P not shown).
There were more grade 3 or greater adverse events among patients on Kd vs. Vd (73% of patients vs 67%, respectively), and more serious adverse events (48% vs. 36%), but more patients in the Vd arm required dose reduction because of side effects (23% vs. 48%), and more patients on Vd discontinued treatment because of disease progression (25% vs. 36%) or adverse events (14% vs. 16%). In all, four patients on Kd and 3 on Vd died from a cause related to an adverse event.
Rates of dyspnea, hypertension, and cardiac failure were slightly more than twice as high with Kd vs. Vd. Peripheral neuropathy was more common among patients on bortezomib, despite three-fourths of patients in this arm receiving it in the subcutaneous injection form, which has been associated with lower rates of neuropathy than with the IV form of bortezomib.
Dr. Wolf noted that the excess in peripheral neuropathy was not surprising, given that bortezomib was delivered twice weekly and that about 25% of patients received it intravenously.
He also noted that among treatment options for patients with relapsed myeloma, Kd was associated with a cost per progression-free month of about $1,222, compared with $1,059 for Vd, $859 for a combination of carfilzomib, lenalidomide (Revlimid) and dexamethasone, and $1,158 for the combination of elotuzumab, lenalidomide, and dexamethasone, used in the ELOQUENT-2 trial, also presented at ASCO 2015.
The study was sponsored by Onyx, a subsidiary of Amgen. Dr. Dimopoulos disclosed receiving honoraria from and consulting for the company. Dr. Wolf disclosed consulting with Onyx and Amgen, serving on the speakers bureau for Milennium, and receiving travel expense from Onyx Consulting and Milennium.
FROM THE 2015 ASCO ANNUAL MEETING
Key clinical point: In a head-to-head trial, carfilzomib/dexamethasone doubled progression-free survival (PFS) compared with bortezomib/dexamethasone.
Major finding: At a median follow-up of 11.2 months, median PFS was 18.7 months for carfilzomib/dexamethasone vs. 9.4 months for bortezomib dexamethasone.
Data source: Randomized controlled trial of 929 patients with relapsed multiple myeloma.
Disclosures: The study was sponsored by Onyx, a subsidiary of Amgen. Dr. Dimopoulos disclosed receiving honoraria from and consulting for the company. Dr. Wolf disclosed consulting with Onyx and Amgen, serving on the speakers bureau for Milennium, and receiving travel expense from Onyx Consulting and Milennium.
ASCO: Transplant boosts stringent complete response rate in newly diagnosed myeloma
CHICAGO – Incorporating autologous stem cell transplantation into an extended treatment regimen for patients with newly diagnosed multiple myeloma was associated with a more than twofold increase in the rate of stringent complete responses compared with historical controls, the results of a small study indicate.
Members of the Multiple Myeloma Research Consortium (MMRC) conducted an open-label phase II trial in which autologous stem cell transplantation (ASCT) was performed after four cycles of induction therapy with carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (KRd), followed by KRd consolidation and maintenance, and additional maintenance with lenalidomide.
At the end of eight cycles, the stringent complete response rate (complete response with a normal free light chain ratio in serum and absence of clonal cells in bone marrow on either immunofluorescence or immunohistochemistry) was 71%, compared with 30% for historical controls who underwent KRd induction and consolidation without ASCT.
“The depth of the response improved with the duration of treatment, as we’ve seen in a number of trials,” Dr. Todd M. Zimmerman of the University of Chicago Comprehensive Cancer Center reported at the annual meeting of the American Society of Clinical Oncology.
The stringent complete response rate improved further to 87% after maintenance KRd was completed, and there were high rates of only minimal residual disease at the end of KRd consolidation (85%) and after KRd maintenance (100%), Dr. Zimmerman said.
Although only eight patients had reached the lenalidomide maintenance phase by the time of data cutoff in March of 2015, these early results are encouraging and warrant further exploration of early ASCT in eligible patients in randomized trials, he said.
The combination of four cycles of KRd induction followed by ASCT, four cycles of KRd consolidation, and 10 cycles of KRd maintenance may be the modern equivalent of the chemotherapy- and ASCT-based “Total Therapy” concept introduced by Dr. Bart Barlogie at the University of Arkansas, Little Rock, in 1989, said Dr. Saad Zafar Usmani, director of the division of plasma cell disorders at the Levine Cancer Institute–Carolinas Healthcare System in Charlotte, N.C.
“What we’re seeing with this combination of novel induction, transplant, novel consolidation, and novel maintenance is an unprecedented depth of response, albeit in a small number of patients,” said Dr. Usmani, the invited discussant.
The new data are not sufficient to support changing practice, but support a head-to-head comparison of KRd with lenalidomide, bortezomib (Velcade), and dexamethasone in a modern Total Therapy approach, he added.
In a phase I/II MMRC study, KRd produced an stringent complete response rate of 55% in patients who had newly diagnosed multiple myeloma and were not eligible for immediate transplant or who wished to defer transplant, and was associated with a 3-year progression-free survival rate of 79%. The flip side of that coin, of course, is that 45% of patients did not achieve a stringent complete response, and 21% had disease progression, including relapses, over 3 years, Dr. Zimmerman said.To see whether they could improve on those odds, the researchers conducted the current study, in which 62 transplant-eligible patients with good performance status and adequate bone marrow, cardiac, and renal function initiated therapy.
They received four cycles of KRd induction, followed by stem-cell mobilization with granulocyte-colony stimulating factors with or without plerixafor (Mozobil), transplant, KRd consolidation for an additional four cycles, KRd maintenance for cycles 9-18, and (off protocol) lenalidomide maintenance until progression. Details of the regimen can be found in the study abstract.
At the time of Dr. Zimmerman’s presentation, 47 patients had proceeded to ASCT, 37 had initiated and 24 had completed the consolidation phase, 24 had started the KRd maintenance phase, and 8 had completed KRd maintenance and have gone on to lenalidomide maintenance.
Response rates have improved over the course of treatment, with 85% of 48 patients who completed induction having at least a very good partial response, including 21% with a near complete response, 12% with a complete response, and 8% with a stringent complete response.
Of the 8 patients who had completed KRd therapy, all had at least a near complete response, and 7 had both complete responses and stringent complete responses.At a median follow-up of 11 months, with longest follow-up out to 26 months, all 62 patients were alive, and all but one were free from disease progression.
Adverse events (not including ASCT-related events) included grade 3 or 4 thrombocytopenias in 11.3% of all patients, leukopenias in 9.7%, lymphopenias in 25.8%, and anemias in 6.5%.
The rates and types of adverse events were in the range of historical data with KRd, Dr. Zimmerman said.
The MMRC study was supported in part by Onyx Pharmaceuticals. Dr. Zimmerman disclosed receiving honoraria, consulting, and serving on the speakers bureau for the company.
CHICAGO – Incorporating autologous stem cell transplantation into an extended treatment regimen for patients with newly diagnosed multiple myeloma was associated with a more than twofold increase in the rate of stringent complete responses compared with historical controls, the results of a small study indicate.
Members of the Multiple Myeloma Research Consortium (MMRC) conducted an open-label phase II trial in which autologous stem cell transplantation (ASCT) was performed after four cycles of induction therapy with carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (KRd), followed by KRd consolidation and maintenance, and additional maintenance with lenalidomide.
At the end of eight cycles, the stringent complete response rate (complete response with a normal free light chain ratio in serum and absence of clonal cells in bone marrow on either immunofluorescence or immunohistochemistry) was 71%, compared with 30% for historical controls who underwent KRd induction and consolidation without ASCT.
“The depth of the response improved with the duration of treatment, as we’ve seen in a number of trials,” Dr. Todd M. Zimmerman of the University of Chicago Comprehensive Cancer Center reported at the annual meeting of the American Society of Clinical Oncology.
The stringent complete response rate improved further to 87% after maintenance KRd was completed, and there were high rates of only minimal residual disease at the end of KRd consolidation (85%) and after KRd maintenance (100%), Dr. Zimmerman said.
Although only eight patients had reached the lenalidomide maintenance phase by the time of data cutoff in March of 2015, these early results are encouraging and warrant further exploration of early ASCT in eligible patients in randomized trials, he said.
The combination of four cycles of KRd induction followed by ASCT, four cycles of KRd consolidation, and 10 cycles of KRd maintenance may be the modern equivalent of the chemotherapy- and ASCT-based “Total Therapy” concept introduced by Dr. Bart Barlogie at the University of Arkansas, Little Rock, in 1989, said Dr. Saad Zafar Usmani, director of the division of plasma cell disorders at the Levine Cancer Institute–Carolinas Healthcare System in Charlotte, N.C.
“What we’re seeing with this combination of novel induction, transplant, novel consolidation, and novel maintenance is an unprecedented depth of response, albeit in a small number of patients,” said Dr. Usmani, the invited discussant.
The new data are not sufficient to support changing practice, but support a head-to-head comparison of KRd with lenalidomide, bortezomib (Velcade), and dexamethasone in a modern Total Therapy approach, he added.
In a phase I/II MMRC study, KRd produced an stringent complete response rate of 55% in patients who had newly diagnosed multiple myeloma and were not eligible for immediate transplant or who wished to defer transplant, and was associated with a 3-year progression-free survival rate of 79%. The flip side of that coin, of course, is that 45% of patients did not achieve a stringent complete response, and 21% had disease progression, including relapses, over 3 years, Dr. Zimmerman said.To see whether they could improve on those odds, the researchers conducted the current study, in which 62 transplant-eligible patients with good performance status and adequate bone marrow, cardiac, and renal function initiated therapy.
They received four cycles of KRd induction, followed by stem-cell mobilization with granulocyte-colony stimulating factors with or without plerixafor (Mozobil), transplant, KRd consolidation for an additional four cycles, KRd maintenance for cycles 9-18, and (off protocol) lenalidomide maintenance until progression. Details of the regimen can be found in the study abstract.
At the time of Dr. Zimmerman’s presentation, 47 patients had proceeded to ASCT, 37 had initiated and 24 had completed the consolidation phase, 24 had started the KRd maintenance phase, and 8 had completed KRd maintenance and have gone on to lenalidomide maintenance.
Response rates have improved over the course of treatment, with 85% of 48 patients who completed induction having at least a very good partial response, including 21% with a near complete response, 12% with a complete response, and 8% with a stringent complete response.
Of the 8 patients who had completed KRd therapy, all had at least a near complete response, and 7 had both complete responses and stringent complete responses.At a median follow-up of 11 months, with longest follow-up out to 26 months, all 62 patients were alive, and all but one were free from disease progression.
Adverse events (not including ASCT-related events) included grade 3 or 4 thrombocytopenias in 11.3% of all patients, leukopenias in 9.7%, lymphopenias in 25.8%, and anemias in 6.5%.
The rates and types of adverse events were in the range of historical data with KRd, Dr. Zimmerman said.
The MMRC study was supported in part by Onyx Pharmaceuticals. Dr. Zimmerman disclosed receiving honoraria, consulting, and serving on the speakers bureau for the company.
CHICAGO – Incorporating autologous stem cell transplantation into an extended treatment regimen for patients with newly diagnosed multiple myeloma was associated with a more than twofold increase in the rate of stringent complete responses compared with historical controls, the results of a small study indicate.
Members of the Multiple Myeloma Research Consortium (MMRC) conducted an open-label phase II trial in which autologous stem cell transplantation (ASCT) was performed after four cycles of induction therapy with carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (KRd), followed by KRd consolidation and maintenance, and additional maintenance with lenalidomide.
At the end of eight cycles, the stringent complete response rate (complete response with a normal free light chain ratio in serum and absence of clonal cells in bone marrow on either immunofluorescence or immunohistochemistry) was 71%, compared with 30% for historical controls who underwent KRd induction and consolidation without ASCT.
“The depth of the response improved with the duration of treatment, as we’ve seen in a number of trials,” Dr. Todd M. Zimmerman of the University of Chicago Comprehensive Cancer Center reported at the annual meeting of the American Society of Clinical Oncology.
The stringent complete response rate improved further to 87% after maintenance KRd was completed, and there were high rates of only minimal residual disease at the end of KRd consolidation (85%) and after KRd maintenance (100%), Dr. Zimmerman said.
Although only eight patients had reached the lenalidomide maintenance phase by the time of data cutoff in March of 2015, these early results are encouraging and warrant further exploration of early ASCT in eligible patients in randomized trials, he said.
The combination of four cycles of KRd induction followed by ASCT, four cycles of KRd consolidation, and 10 cycles of KRd maintenance may be the modern equivalent of the chemotherapy- and ASCT-based “Total Therapy” concept introduced by Dr. Bart Barlogie at the University of Arkansas, Little Rock, in 1989, said Dr. Saad Zafar Usmani, director of the division of plasma cell disorders at the Levine Cancer Institute–Carolinas Healthcare System in Charlotte, N.C.
“What we’re seeing with this combination of novel induction, transplant, novel consolidation, and novel maintenance is an unprecedented depth of response, albeit in a small number of patients,” said Dr. Usmani, the invited discussant.
The new data are not sufficient to support changing practice, but support a head-to-head comparison of KRd with lenalidomide, bortezomib (Velcade), and dexamethasone in a modern Total Therapy approach, he added.
In a phase I/II MMRC study, KRd produced an stringent complete response rate of 55% in patients who had newly diagnosed multiple myeloma and were not eligible for immediate transplant or who wished to defer transplant, and was associated with a 3-year progression-free survival rate of 79%. The flip side of that coin, of course, is that 45% of patients did not achieve a stringent complete response, and 21% had disease progression, including relapses, over 3 years, Dr. Zimmerman said.To see whether they could improve on those odds, the researchers conducted the current study, in which 62 transplant-eligible patients with good performance status and adequate bone marrow, cardiac, and renal function initiated therapy.
They received four cycles of KRd induction, followed by stem-cell mobilization with granulocyte-colony stimulating factors with or without plerixafor (Mozobil), transplant, KRd consolidation for an additional four cycles, KRd maintenance for cycles 9-18, and (off protocol) lenalidomide maintenance until progression. Details of the regimen can be found in the study abstract.
At the time of Dr. Zimmerman’s presentation, 47 patients had proceeded to ASCT, 37 had initiated and 24 had completed the consolidation phase, 24 had started the KRd maintenance phase, and 8 had completed KRd maintenance and have gone on to lenalidomide maintenance.
Response rates have improved over the course of treatment, with 85% of 48 patients who completed induction having at least a very good partial response, including 21% with a near complete response, 12% with a complete response, and 8% with a stringent complete response.
Of the 8 patients who had completed KRd therapy, all had at least a near complete response, and 7 had both complete responses and stringent complete responses.At a median follow-up of 11 months, with longest follow-up out to 26 months, all 62 patients were alive, and all but one were free from disease progression.
Adverse events (not including ASCT-related events) included grade 3 or 4 thrombocytopenias in 11.3% of all patients, leukopenias in 9.7%, lymphopenias in 25.8%, and anemias in 6.5%.
The rates and types of adverse events were in the range of historical data with KRd, Dr. Zimmerman said.
The MMRC study was supported in part by Onyx Pharmaceuticals. Dr. Zimmerman disclosed receiving honoraria, consulting, and serving on the speakers bureau for the company.
AT THE 2015 ASCO ANNUAL MEETING
Key clinical point: Adding stem cell transplantation to KRd therapy improves responses in patients with newly diagnosed multiple myeloma.
Major finding: Stringent complete responses rates with carfilzomib, lenalidomide, and dexamethasone plus ASCT were 87%, compared with 30% for KRd without transplant (historical controls).
Data source: Open-label phase II study of 62 patients with newly diagnosed myeloma.
Disclosures: The MMRC study was supported in part by Onyx Pharmaceuticals. Dr. Zimmerman disclosed receiving honoraria, consulting, and serving on the speakers bureau for the company.