User login
IVC Filter Perforations Are Often Asymptomatic
ORLANDO – Roughly half of all inferior vena cava filter perforations voluntarily reported between 2000 and 2011 were asymptomatic and were noted as incidental findings on imaging studies, Dr. Emily A. Wood reported at the annual meeting of the American Venous Forum.
"An important thing to note about IVC perforation is that a large proportion of the patients are actually asymptomatic. Our study noted an average of 47% – almost half – of perforations were incidental findings on imaging," said Dr. Wood, a general surgery resident at Stony Brook (N.Y.) University.
IVC filter placement has more than doubled in the last decade – from 30,756 to 65,041 (J. Am. Coll. Radiol. 2011;8:483-9). While uncomplicated filter placement is a relatively straightforward ambulatory procedure, IVC filter registration and reporting of outcomes are not mandatory. Little is known about the number of adverse events related to these procedures. However, IVC perforation is an easily quantifiable event, said Dr. Wood.
The researchers used the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. They performed a retrospective review of 3,311 reported adverse events using filter/intravascular/cardiovascular product class search criteria from January 2000 to December 2011.
They excluded adverse event descriptions that did not specifically involve IVC perforation, including: device malfunction, failure to deploy device properly, migration/tilting, and cardiopulmonary system involvement. Outcomes of interest included clinical presentation, type of device utilized, and management (including retrievability rates).
The researchers found 391 (11%) instances of IVC perforation were reported over the 11-year period of interest. In particular, a fivefold increase in adverse events related to IVC perforation occurred from 2003 to 2004. The annual distribution of cases was 35 (12%); the annual accrual rate has not significantly increased. "Remember that this is not a universal registry and that it is voluntary. Thus, it is not entirely representative of the type of complications that actually occurred during those years," she said.
The most commonly involved structure was the aorta (43), followed by small bowel (36), vertebral body (14), and others. By far, the most commonly used filter type was the Bard G2 (168), followed by the Bard Recovery (59), the Cook Celect (46), and others.
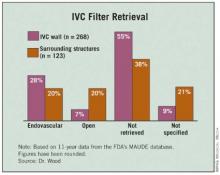
"The majority of these filters are left in place, despite the adverse event. In other words, a perforation alone is not necessarily an indication for device removal," said Dr. Wood (see table).
IVC filter placement is not free from complications and therefore indications for filter placement should be carefully reviewed prior to any procedure. Retrievable filters are commonly involved in IVC perforation. "This gives more weight to the fact that these patients should be followed more closely and that a scheduled date for retrieval should be set, if indicated."
The authors reported that they have no relevant disclosures.
ORLANDO – Roughly half of all inferior vena cava filter perforations voluntarily reported between 2000 and 2011 were asymptomatic and were noted as incidental findings on imaging studies, Dr. Emily A. Wood reported at the annual meeting of the American Venous Forum.
"An important thing to note about IVC perforation is that a large proportion of the patients are actually asymptomatic. Our study noted an average of 47% – almost half – of perforations were incidental findings on imaging," said Dr. Wood, a general surgery resident at Stony Brook (N.Y.) University.
IVC filter placement has more than doubled in the last decade – from 30,756 to 65,041 (J. Am. Coll. Radiol. 2011;8:483-9). While uncomplicated filter placement is a relatively straightforward ambulatory procedure, IVC filter registration and reporting of outcomes are not mandatory. Little is known about the number of adverse events related to these procedures. However, IVC perforation is an easily quantifiable event, said Dr. Wood.
The researchers used the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. They performed a retrospective review of 3,311 reported adverse events using filter/intravascular/cardiovascular product class search criteria from January 2000 to December 2011.
They excluded adverse event descriptions that did not specifically involve IVC perforation, including: device malfunction, failure to deploy device properly, migration/tilting, and cardiopulmonary system involvement. Outcomes of interest included clinical presentation, type of device utilized, and management (including retrievability rates).
The researchers found 391 (11%) instances of IVC perforation were reported over the 11-year period of interest. In particular, a fivefold increase in adverse events related to IVC perforation occurred from 2003 to 2004. The annual distribution of cases was 35 (12%); the annual accrual rate has not significantly increased. "Remember that this is not a universal registry and that it is voluntary. Thus, it is not entirely representative of the type of complications that actually occurred during those years," she said.
The most commonly involved structure was the aorta (43), followed by small bowel (36), vertebral body (14), and others. By far, the most commonly used filter type was the Bard G2 (168), followed by the Bard Recovery (59), the Cook Celect (46), and others.
"The majority of these filters are left in place, despite the adverse event. In other words, a perforation alone is not necessarily an indication for device removal," said Dr. Wood (see table).
IVC filter placement is not free from complications and therefore indications for filter placement should be carefully reviewed prior to any procedure. Retrievable filters are commonly involved in IVC perforation. "This gives more weight to the fact that these patients should be followed more closely and that a scheduled date for retrieval should be set, if indicated."
The authors reported that they have no relevant disclosures.
ORLANDO – Roughly half of all inferior vena cava filter perforations voluntarily reported between 2000 and 2011 were asymptomatic and were noted as incidental findings on imaging studies, Dr. Emily A. Wood reported at the annual meeting of the American Venous Forum.
"An important thing to note about IVC perforation is that a large proportion of the patients are actually asymptomatic. Our study noted an average of 47% – almost half – of perforations were incidental findings on imaging," said Dr. Wood, a general surgery resident at Stony Brook (N.Y.) University.
IVC filter placement has more than doubled in the last decade – from 30,756 to 65,041 (J. Am. Coll. Radiol. 2011;8:483-9). While uncomplicated filter placement is a relatively straightforward ambulatory procedure, IVC filter registration and reporting of outcomes are not mandatory. Little is known about the number of adverse events related to these procedures. However, IVC perforation is an easily quantifiable event, said Dr. Wood.
The researchers used the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. They performed a retrospective review of 3,311 reported adverse events using filter/intravascular/cardiovascular product class search criteria from January 2000 to December 2011.
They excluded adverse event descriptions that did not specifically involve IVC perforation, including: device malfunction, failure to deploy device properly, migration/tilting, and cardiopulmonary system involvement. Outcomes of interest included clinical presentation, type of device utilized, and management (including retrievability rates).
The researchers found 391 (11%) instances of IVC perforation were reported over the 11-year period of interest. In particular, a fivefold increase in adverse events related to IVC perforation occurred from 2003 to 2004. The annual distribution of cases was 35 (12%); the annual accrual rate has not significantly increased. "Remember that this is not a universal registry and that it is voluntary. Thus, it is not entirely representative of the type of complications that actually occurred during those years," she said.
The most commonly involved structure was the aorta (43), followed by small bowel (36), vertebral body (14), and others. By far, the most commonly used filter type was the Bard G2 (168), followed by the Bard Recovery (59), the Cook Celect (46), and others.
"The majority of these filters are left in place, despite the adverse event. In other words, a perforation alone is not necessarily an indication for device removal," said Dr. Wood (see table).
IVC filter placement is not free from complications and therefore indications for filter placement should be carefully reviewed prior to any procedure. Retrievable filters are commonly involved in IVC perforation. "This gives more weight to the fact that these patients should be followed more closely and that a scheduled date for retrieval should be set, if indicated."
The authors reported that they have no relevant disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN VENOUS FORUM
Major Finding: Forty-seven percent of IVC filter perforations were incidental findings on imaging.
Data Source: The data are from a retrospective review of 3,311 cases reported in the Food and Drug Administration’s Manufacture and User Facility Device Experience (MAUDE) database between 2000 and 2011.
Disclosures: The authors reported that they have no relevant disclosures.
Infections, Pulmonary Complications Up Risk of Thrombotic Events
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN VENOUS FORUM