User login
Uterine Artery Embolization Improves Urinary Symptoms
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE SOCIETY OF INTERVENTIONAL RADIOLOGY
Major Finding: Women who underwent UAE for fibroids had an average improvement of 23 points on the UDI-6, which was significant.
Data Source: Prospective study of 46 women treated with UAE for fibroids.
Disclosures: Dr. Spies and his associates reported they had no relevant financial disclosures.
Uterine Artery Embolization Improves Urinary Symptoms
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
CHICAGO – Uterine artery embolization for the treatment of fibroids also appears to improve lower urinary tract symptoms, a small study has shown.
Women who underwent uterine artery embolization (UAE) for fibroids had an average improvement of 23 points on the Urinary Distress Inventory (UDI-6).
"We had a significant improvement in all of the measures, except for the number of accidents," said Dr. James B. Spies, professor and chairman of radiology at Georgetown University, Washington.
The researchers recruited 46 women (average age, 44 years), who were undergoing UAE at the George Washington University Medical Center between 2008 and 2010. Each patient completed a set of validated questionnaires assessing urinary symptoms and quality of life impact, and fibroid symptoms and quality of life impact, as well as a 48-hour urinary diary before and after UAE. The women also completed these questionnaires and a urinary diary at 3 months post procedure.
Lower urinary tract symptoms included an increased frequency of urination, a sudden urgent need to urinate, difficulty urinating (retention), and incontinence.
The researchers used several validated tools to assess improvement in urinary symptoms, including the UDI-6, the Incontinence Impact Questionnaire (IIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QoL), and a standardized 48-hour bladder diary.
The Patient Global Impression of Improvement (PGI-I) also was used to assess patient satisfaction with the procedure. The primary outcome was the measure of subjective improvement in lower urinary tract symptoms at 3 months, as measured by the UDI-6.
In addition to improvement on the UDI-6, there was a mean reduction of 15 points on the IIQ-7. There were also significant decreases in the mean scores for the PISQ-12 and UFS-QoL, Dr. Spies said at the annual meeting of the Society of Interventional Radiology.
Using regression modeling, the researchers found that uterine volume, dominant fibroid volume, location of the fibroid, and bladder compression did not affect the scores, but obesity did. For each unit increase in body mass index, the improvement in the UDI-6 scores was decreased by 1.8.
Dr. Spies and his associates reported they had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE SOCIETY OF INTERVENTIONAL RADIOLOGY
Major Finding: Women who underwent UAE for fibroids had an average improvement of 23 points on the UDI-6, which was significant.
Data Source: Prospective study of 46 women treated with UAE for fibroids.
Disclosures: Dr. Spies and his associates reported they had no relevant financial disclosures.
Pelvic Artery Embolization Stops Postpartum Hemorrhage
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
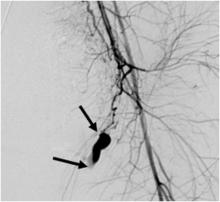
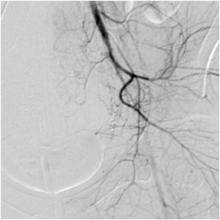
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE SOCIETY FOR INTERVENTIONAL RADIOLOGY
Major Finding: A single pelvic artery embolization procedure stopped postpartum hemorrhage in 86% of women. A second procedure stopped bleeding in 89%.
Data Source: A retrospective study of 225 women who underwent PAE to stop postpartum hemorrhage.
Disclosures: Dr. Shin reported that he had no relevant financial disclosures.
Pelvic Artery Embolization Stops Postpartum Hemorrhage
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE SOCIETY FOR INTERVENTIONAL RADIOLOGY
Major Finding: A single pelvic artery embolization procedure stopped postpartum hemorrhage in 86% of women. A second procedure stopped bleeding in 89%.
Data Source: A retrospective study of 225 women who underwent PAE to stop postpartum hemorrhage.
Disclosures: Dr. Shin reported that he had no relevant financial disclosures.