User login
Who’s in charge here?
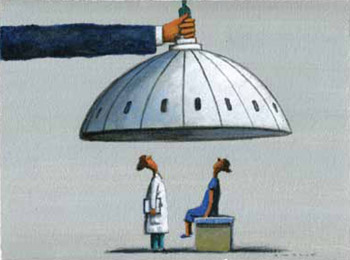
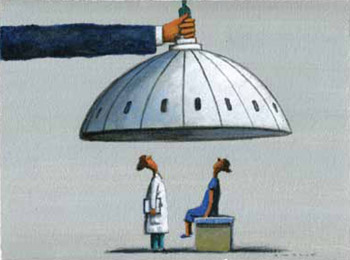
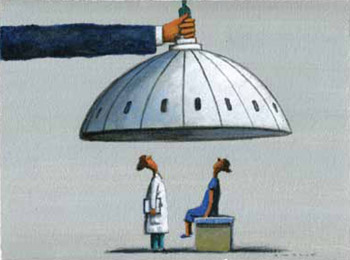
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
Who’s in charge here?
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
Who’s in charge here?
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
