User login
VA's Project Reach Contest to Help Homeless Find Services; DoD Changes Sexual Assault Response; Faster Claims Processing Now Available; NAMI Statement on Afghanistan Tragedy; Mentors Prove Helpful to African American Vets With Diabetes; Veterans With PTSD
Grand Rounds: Man, 62, With New-Onset Atrial Fibrillation
A 62-year-old black nursing home resident was transported to the hospital emergency department with fever of 102°F, new-onset atrial fibrillation (A-fib), and dementia. His medical history was significant for hypertension and multiple strokes.
His inpatient work-up for A-fib and dementia revealed a thyroid-stimulating hormone (TSH) level below 0.005 µIU/mL (normal range, 0.3 to 3.0 µIU/mL). Results of thyroid function testing (TFT) revealed a triiodothyronine (T3) level within normal range but a free thyroxine (T4) level of 2.9 ng/dL (normal range, 0.7 to 1.5 ng/dL) and a total T4 of 17.8 µg/dL (normal, 4.5 to 12.0 µg/dL). The abnormal TSH and T4 levels were considered suggestive of a thyrotoxic state, warranting an endocrinology consult. Cardiology was consulted regarding new-onset A-fib.
During history taking, the patient denied any shortness of breath, cough, palpitations, heat intolerance, anxiety, tremors, insomnia, dysphagia, diarrhea, dysuria, weight loss, or recent ingestion of iodine-containing medications or supplements.
On examination, the patient was febrile, with a blood pressure of 106/71 mm Hg; pulse, 74 beats/min; respiratory rate, 20 breaths/min; and O2 saturation, 98% to 99% on room air. ECG showed a normal sinus rhythm and a ventricular rate of 64 beats/min.
The patient's weight was 58.9 kg, and his height, 63" (BMI, 22.8). The patient had no skin changes, and his mucous membranes were slightly moist. The patient's head was atraumatic and normocephalic. His extraocular movements were intact, and his pupils were equal, round, and reactive to light, with nonicteric sclera. There was no proptosis or ophthalmoplegia. The patient's neck was supple, with no jugular venous distension, tracheal deviation, or thyromegaly.
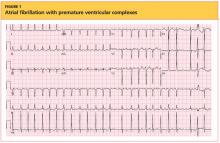
The cardiovascular exam revealed an irregular heartbeat, and repeat ECG showed A-fib with a ventricular rate of 151 beats/min (see Figure 1). The patient's chest was clear, with no wheezing or rhonchi. The abdomen was soft and slightly obese, and bowel sounds were present. The neurologic examination revealed no hyperreflexia. The patient's mental status was altered at times and he was alert, awake, and oriented to others. His speech was slightly slow, and some left-sided weakness was noted.
As recommended during the endocrinology consult, the patient underwent an I-123 sodium iodide thyroid scan, which showed faint uptake at the base of the neck, slightly to the left of midline; and a 24-hour radioactive iodide uptake (RAIU), which measured 2.8% (normal range, 8% to 35%).
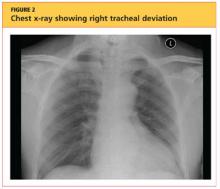
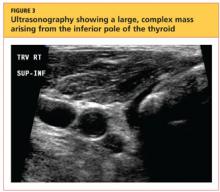
The patient's chest X-ray showed a right tracheal deviation not previously noted on physical examination (see Figure 2); the possible cause of a thyroid mass was considered. Subsequent ultrasonography of the thyroid revealed generally normal dimensions and parenchymal echogenicity. However, a large complex mass was detected, arising from the inferior pole of the thyroid and displacing the trachea toward the right (see Figure 3). According to the radiologist's notes, the mass contained both solid and cystic elements, scattered calcifications, and foci of flow on color Doppler. It measured about 6 cm in the largest (transverse) dimension. A 2.0-mm nodule was noted in the isthmus, slightly to the right of midline, consistent with multinodular goiter.
Following the cardiology consult, a diltiazem drip was initiated, but the patient was later optimized on flecainide for rhythm control and metoprolol for rate control. He was also initially anticoagulated using a heparin drip and bridged to warfarin, with target international normalized ratio (INR) between 2.0 and 3.0. Echocardiography revealed normal systolic function with ejection fraction of 55%, left ventricular hypertrophy, pulmonary artery systolic pressure of 35 mm Hg, and no pericardial effusions or valvular disease.
Regarding the patient's unexplained fever, results of chest imaging were negative for signs of pneumonia or atelectasis, which might have suggested a pulmonary cause. Urinalysis results were normal. Complete blood count showed no leukocytosis. The patient's fever subsided within 48 hours.
The differential diagnosis included Graves' disease, toxic multinodular goiter, Jod-Basedow syndrome, and subacute thyroiditis.
Graves' disease, an autoimmune disease with an unknown trigger, is the most common cause of hyperthyroidism. In affected patients, the thyroid gland overproduces thyroid hormones, leading to thyrotoxicosis. Thyrotoxicosis can result in multiple clinical signs and symptoms, including Graves' ophthalmopathy, pretibial myxedema, and goiter; TFT results typically include elevated T3 and T4 and low TSH.1-5 In the case patient (who had no history of thyroid disease, nor clinical signs or symptoms of Graves' disease), low uptake of iodine on thyroid scan precluded this diagnosis.
Toxic multinodular goiter, the second most common cause of hyperthyroidism, can be responsible for A-fib, tachycardia, and congestive heart failure.6,7 Iodine deficiency causes enlargement of the thyroid gland, where numerous nodules can develop, as seen in the case patient. These nodules can function independently, sometimes producing excess thyroid hormone; this leads to hyperplasia of the thyroid gland, resulting in a nontoxic multinodular goiter. From this goiter, a toxic multinodular goiter can emerge insidiously. However, in this condition, RAIU typically exceeds 30%; in the case patient, low 24-hour RAIU (2.8%) and the absence of functioning nodules on scanning made it possible to rule out this diagnosis.
Jod-Basedow syndrome refers to hyperthyroidism that develops as a result of administration of iodide, either as a dietary supplement or as IV contrast medium, or as an adverse effect of the antiarrhythmic drug amiodarone. This phenomenon is usually seen in a patient with endemic goiter.8-11 The relatively limited nature of the case patient's goiter and absence of a precipitating exposure to iodine made this diagnosis highly unlikely.
Subacute thyroiditis is a condition to which the patient's abnormal TFT results could reasonably be attributed. The patient had a substernal multinodular goiter that could not be palpated on physical examination, but it was visualized in the extended lower neck during thyroid scintigraphy.3 RAIU was minimal—a typical finding in this disorder,6 as TSH is suppressed by leakage of the excessive amounts of thyroid hormone. A tentative diagnosis of subacute thyroiditis was made.
As subacute thyroiditis is a self-limiting disorder, the patient was not started on any medications for hyperthyroidism but was advised to follow up with his primary care provider or an endocrinologist for repeat TFT and for fine-needle aspiration biopsy of the large thyroid nodule (a complex mass, containing cystic elements and calcifications, with a potential for malignancy) to rule out thyroid cancer.
Repeat ECG before discharge showed normal sinus rhythm with a ventricular rate of 74 beats/min. The patient was alert, awake, and oriented at discharge. He was continued on flecainide, metoprolol, and warfarin and advised to follow up with his primary care provider regarding his target INR.
DISCUSSION
The incidence of subacute thyroiditis, according to findings reported in 2003 from the Rochester Epidemiology Project in Olmsted County, Minnesota,12 is 12.1 cases per 100,000/year, with a higher incidence in women than men. It is most common in young adults and decreases with advancing age. Coxsackie virus, adenovirus, mumps, echovirus, influenza, and Epstein-Barr virus have been implicated in the disorder.12,13
Subacute thyroiditis is associated with a triphasic clinical course of hyperthyroidism, then hypothyroidism, then a return to normal thyroid function—as was seen in the case patient. Onset of subacute thyroiditis has been associated with recent viral infection, which may serve as a precipitant. The cause of this patient's high fever was never identified; thus, the etiology may have been viral.
The initial high thyroid hormone levels result from inflammation of thyroid tissue and release of preformed thyroid hormone into the circulation.6 At this point, TSH is suppressed and patients have very low RAIU, as was true in the case patient.
The condition is self-limiting and does not require treatment in the majority of patients, as TFT results return to normal levels within about two months.6 Patients can appear extremely ill due to thyrotoxicosis from subacute thyroiditis, but this usually lasts no longer than six to eight weeks.3 Subacute thyroiditis can be associated with atrial arrhythmia or heart failure.14,15
PATIENT OUTCOME
New-onset A-fib was attributed to the patient's thyrotoxicosis, which in turn was caused by subacute thyroiditis. He had a multinodular goiter, although he had not received any iodine supplements or IV contrast. As in most cases of subacute thyroiditis, no precipitating event was identified. However, given this patient's residence in a nursing facility and presentation with a high fever with no identifiable cause, a viral etiology for his subacute thyroiditis is possible.6
The patient's dementia may have been secondary to acute thyrotoxicosis, as his mental state improved during the hospital stay. His vitamin B12, folate, and A1C levels were within normal range. CT of the head showed multiple chronic infarcts and cerebral atrophy, and MRI of the brain indicated microvascular ischemic disease.
The patient was readmitted one month later for an episode of near-syncope (which, it was concluded, was a vasovagal episode). At that time, his TSH was found normal at 1.350 µIU/mL. Flecainide and metoprolol were discontinued; he was started on diltiazem for continued rate and rhythm control (as recommended by cardiology) and continued on warfarin.
CONCLUSION
In this case, subacute thyroiditis was most likely caused by a viral infection that led to destruction of the normal thyroid follicles and release of their preformed thyroid hormone into the circulation; this in turn led to sudden-onset A-fib. The diagnosis of subacute thyroiditis was suggested based on the abnormalities seen in this patient's TFT results, coupled with the suppressed RAIU—a typical finding in this disease.
Because subacute thyroiditis is a self-limiting condition, there is no role for antithyroid medication. Instead, treatment should be focused on relieving the patient's symptoms, such as ß-blockade or calcium channel blockers for tachycardia and corticosteroids or NSAIDs for neck pain.
REFERENCES
1. Weetman AP. Graves' disease. N Engl J Med. 2000;343(17):1236-1248.
2. Delgado Hurtado JJ, Pineda M. Images in medicine: Graves' disease. N Engl J Med. 2011; 364(20):1955.
3. Al-Sharif AA, Abujbara MA, Chiacchio S, et al. Contribution of radioiodine uptake measurement and thyroid scintigraphy to the differential diagnosis of thyrotoxicosis. Hell J Nucl Med. 2010;13(2):132-137.
4. Buccelletti F, Carroccia A, Marsiliani D, et al. Utility of routine thyroid-stimulating hormone determination in new-onset atrial fibrillation in the ED. Am J Emerg Med. 2011;29(9):1158-1162.
5. Ross DS. Radioiodine therapy for hyperthyroidism. N Engl J Med. 2011;364(6):542-550.
6. Bahn RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract. 2011;17(3):456-520.
7. Erickson D, Gharib H, Li H, van Heerden JA. Treatment of patients with toxic multinodular goiter. Thyroid. 1998;8(4):277-282.
8. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med. 2005;118(7):706-714.
9. Bogazzi F, Bartalena L, Martino E. Approach to the patient with amiodarone-induced thyrotoxicosis. J Clin Endocrinol Metab. 2010;95(6):2529-2535.
10. El-Shirbiny AM, Stavrou SS, Dnistrian A, et al. Jod-Basedow syndrome following oral iodine and radioiodinated-antibody administration. J Nucl Med. 1997;38(11):1816-1817.
11. Stanbury JB, Ermans AE, Bourdoux P, et al. Iodine-induced hyperthyroidism: occurrence and epidemiology. Thyroid. 1998;8(1):83-100.
12. Fatourechi V, Aniszewski JP, Fatourechi GZ, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100-2105.
13. Golden SH, Robinson KA, Saldanha I, et al. Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review. J Clin Endocrinol Metab. 2009;94(6):1853-1878.
14. Volpé R. The management of subacute (DeQuervain's) thyroiditis. Thyroid. 1993;3(3):253-255.
15. Lee SL. Subacute thyroiditis (2009). http://emedicine.medscape.com/article/125648-overview. Accessed April 17, 2012.
A 62-year-old black nursing home resident was transported to the hospital emergency department with fever of 102°F, new-onset atrial fibrillation (A-fib), and dementia. His medical history was significant for hypertension and multiple strokes.
His inpatient work-up for A-fib and dementia revealed a thyroid-stimulating hormone (TSH) level below 0.005 µIU/mL (normal range, 0.3 to 3.0 µIU/mL). Results of thyroid function testing (TFT) revealed a triiodothyronine (T3) level within normal range but a free thyroxine (T4) level of 2.9 ng/dL (normal range, 0.7 to 1.5 ng/dL) and a total T4 of 17.8 µg/dL (normal, 4.5 to 12.0 µg/dL). The abnormal TSH and T4 levels were considered suggestive of a thyrotoxic state, warranting an endocrinology consult. Cardiology was consulted regarding new-onset A-fib.
During history taking, the patient denied any shortness of breath, cough, palpitations, heat intolerance, anxiety, tremors, insomnia, dysphagia, diarrhea, dysuria, weight loss, or recent ingestion of iodine-containing medications or supplements.
On examination, the patient was febrile, with a blood pressure of 106/71 mm Hg; pulse, 74 beats/min; respiratory rate, 20 breaths/min; and O2 saturation, 98% to 99% on room air. ECG showed a normal sinus rhythm and a ventricular rate of 64 beats/min.
The patient's weight was 58.9 kg, and his height, 63" (BMI, 22.8). The patient had no skin changes, and his mucous membranes were slightly moist. The patient's head was atraumatic and normocephalic. His extraocular movements were intact, and his pupils were equal, round, and reactive to light, with nonicteric sclera. There was no proptosis or ophthalmoplegia. The patient's neck was supple, with no jugular venous distension, tracheal deviation, or thyromegaly.
The cardiovascular exam revealed an irregular heartbeat, and repeat ECG showed A-fib with a ventricular rate of 151 beats/min (see Figure 1). The patient's chest was clear, with no wheezing or rhonchi. The abdomen was soft and slightly obese, and bowel sounds were present. The neurologic examination revealed no hyperreflexia. The patient's mental status was altered at times and he was alert, awake, and oriented to others. His speech was slightly slow, and some left-sided weakness was noted.
As recommended during the endocrinology consult, the patient underwent an I-123 sodium iodide thyroid scan, which showed faint uptake at the base of the neck, slightly to the left of midline; and a 24-hour radioactive iodide uptake (RAIU), which measured 2.8% (normal range, 8% to 35%).
The patient's chest X-ray showed a right tracheal deviation not previously noted on physical examination (see Figure 2); the possible cause of a thyroid mass was considered. Subsequent ultrasonography of the thyroid revealed generally normal dimensions and parenchymal echogenicity. However, a large complex mass was detected, arising from the inferior pole of the thyroid and displacing the trachea toward the right (see Figure 3). According to the radiologist's notes, the mass contained both solid and cystic elements, scattered calcifications, and foci of flow on color Doppler. It measured about 6 cm in the largest (transverse) dimension. A 2.0-mm nodule was noted in the isthmus, slightly to the right of midline, consistent with multinodular goiter.
Following the cardiology consult, a diltiazem drip was initiated, but the patient was later optimized on flecainide for rhythm control and metoprolol for rate control. He was also initially anticoagulated using a heparin drip and bridged to warfarin, with target international normalized ratio (INR) between 2.0 and 3.0. Echocardiography revealed normal systolic function with ejection fraction of 55%, left ventricular hypertrophy, pulmonary artery systolic pressure of 35 mm Hg, and no pericardial effusions or valvular disease.
Regarding the patient's unexplained fever, results of chest imaging were negative for signs of pneumonia or atelectasis, which might have suggested a pulmonary cause. Urinalysis results were normal. Complete blood count showed no leukocytosis. The patient's fever subsided within 48 hours.
The differential diagnosis included Graves' disease, toxic multinodular goiter, Jod-Basedow syndrome, and subacute thyroiditis.
Graves' disease, an autoimmune disease with an unknown trigger, is the most common cause of hyperthyroidism. In affected patients, the thyroid gland overproduces thyroid hormones, leading to thyrotoxicosis. Thyrotoxicosis can result in multiple clinical signs and symptoms, including Graves' ophthalmopathy, pretibial myxedema, and goiter; TFT results typically include elevated T3 and T4 and low TSH.1-5 In the case patient (who had no history of thyroid disease, nor clinical signs or symptoms of Graves' disease), low uptake of iodine on thyroid scan precluded this diagnosis.
Toxic multinodular goiter, the second most common cause of hyperthyroidism, can be responsible for A-fib, tachycardia, and congestive heart failure.6,7 Iodine deficiency causes enlargement of the thyroid gland, where numerous nodules can develop, as seen in the case patient. These nodules can function independently, sometimes producing excess thyroid hormone; this leads to hyperplasia of the thyroid gland, resulting in a nontoxic multinodular goiter. From this goiter, a toxic multinodular goiter can emerge insidiously. However, in this condition, RAIU typically exceeds 30%; in the case patient, low 24-hour RAIU (2.8%) and the absence of functioning nodules on scanning made it possible to rule out this diagnosis.
Jod-Basedow syndrome refers to hyperthyroidism that develops as a result of administration of iodide, either as a dietary supplement or as IV contrast medium, or as an adverse effect of the antiarrhythmic drug amiodarone. This phenomenon is usually seen in a patient with endemic goiter.8-11 The relatively limited nature of the case patient's goiter and absence of a precipitating exposure to iodine made this diagnosis highly unlikely.
Subacute thyroiditis is a condition to which the patient's abnormal TFT results could reasonably be attributed. The patient had a substernal multinodular goiter that could not be palpated on physical examination, but it was visualized in the extended lower neck during thyroid scintigraphy.3 RAIU was minimal—a typical finding in this disorder,6 as TSH is suppressed by leakage of the excessive amounts of thyroid hormone. A tentative diagnosis of subacute thyroiditis was made.
As subacute thyroiditis is a self-limiting disorder, the patient was not started on any medications for hyperthyroidism but was advised to follow up with his primary care provider or an endocrinologist for repeat TFT and for fine-needle aspiration biopsy of the large thyroid nodule (a complex mass, containing cystic elements and calcifications, with a potential for malignancy) to rule out thyroid cancer.
Repeat ECG before discharge showed normal sinus rhythm with a ventricular rate of 74 beats/min. The patient was alert, awake, and oriented at discharge. He was continued on flecainide, metoprolol, and warfarin and advised to follow up with his primary care provider regarding his target INR.
DISCUSSION
The incidence of subacute thyroiditis, according to findings reported in 2003 from the Rochester Epidemiology Project in Olmsted County, Minnesota,12 is 12.1 cases per 100,000/year, with a higher incidence in women than men. It is most common in young adults and decreases with advancing age. Coxsackie virus, adenovirus, mumps, echovirus, influenza, and Epstein-Barr virus have been implicated in the disorder.12,13
Subacute thyroiditis is associated with a triphasic clinical course of hyperthyroidism, then hypothyroidism, then a return to normal thyroid function—as was seen in the case patient. Onset of subacute thyroiditis has been associated with recent viral infection, which may serve as a precipitant. The cause of this patient's high fever was never identified; thus, the etiology may have been viral.
The initial high thyroid hormone levels result from inflammation of thyroid tissue and release of preformed thyroid hormone into the circulation.6 At this point, TSH is suppressed and patients have very low RAIU, as was true in the case patient.
The condition is self-limiting and does not require treatment in the majority of patients, as TFT results return to normal levels within about two months.6 Patients can appear extremely ill due to thyrotoxicosis from subacute thyroiditis, but this usually lasts no longer than six to eight weeks.3 Subacute thyroiditis can be associated with atrial arrhythmia or heart failure.14,15
PATIENT OUTCOME
New-onset A-fib was attributed to the patient's thyrotoxicosis, which in turn was caused by subacute thyroiditis. He had a multinodular goiter, although he had not received any iodine supplements or IV contrast. As in most cases of subacute thyroiditis, no precipitating event was identified. However, given this patient's residence in a nursing facility and presentation with a high fever with no identifiable cause, a viral etiology for his subacute thyroiditis is possible.6
The patient's dementia may have been secondary to acute thyrotoxicosis, as his mental state improved during the hospital stay. His vitamin B12, folate, and A1C levels were within normal range. CT of the head showed multiple chronic infarcts and cerebral atrophy, and MRI of the brain indicated microvascular ischemic disease.
The patient was readmitted one month later for an episode of near-syncope (which, it was concluded, was a vasovagal episode). At that time, his TSH was found normal at 1.350 µIU/mL. Flecainide and metoprolol were discontinued; he was started on diltiazem for continued rate and rhythm control (as recommended by cardiology) and continued on warfarin.
CONCLUSION
In this case, subacute thyroiditis was most likely caused by a viral infection that led to destruction of the normal thyroid follicles and release of their preformed thyroid hormone into the circulation; this in turn led to sudden-onset A-fib. The diagnosis of subacute thyroiditis was suggested based on the abnormalities seen in this patient's TFT results, coupled with the suppressed RAIU—a typical finding in this disease.
Because subacute thyroiditis is a self-limiting condition, there is no role for antithyroid medication. Instead, treatment should be focused on relieving the patient's symptoms, such as ß-blockade or calcium channel blockers for tachycardia and corticosteroids or NSAIDs for neck pain.
REFERENCES
1. Weetman AP. Graves' disease. N Engl J Med. 2000;343(17):1236-1248.
2. Delgado Hurtado JJ, Pineda M. Images in medicine: Graves' disease. N Engl J Med. 2011; 364(20):1955.
3. Al-Sharif AA, Abujbara MA, Chiacchio S, et al. Contribution of radioiodine uptake measurement and thyroid scintigraphy to the differential diagnosis of thyrotoxicosis. Hell J Nucl Med. 2010;13(2):132-137.
4. Buccelletti F, Carroccia A, Marsiliani D, et al. Utility of routine thyroid-stimulating hormone determination in new-onset atrial fibrillation in the ED. Am J Emerg Med. 2011;29(9):1158-1162.
5. Ross DS. Radioiodine therapy for hyperthyroidism. N Engl J Med. 2011;364(6):542-550.
6. Bahn RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract. 2011;17(3):456-520.
7. Erickson D, Gharib H, Li H, van Heerden JA. Treatment of patients with toxic multinodular goiter. Thyroid. 1998;8(4):277-282.
8. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med. 2005;118(7):706-714.
9. Bogazzi F, Bartalena L, Martino E. Approach to the patient with amiodarone-induced thyrotoxicosis. J Clin Endocrinol Metab. 2010;95(6):2529-2535.
10. El-Shirbiny AM, Stavrou SS, Dnistrian A, et al. Jod-Basedow syndrome following oral iodine and radioiodinated-antibody administration. J Nucl Med. 1997;38(11):1816-1817.
11. Stanbury JB, Ermans AE, Bourdoux P, et al. Iodine-induced hyperthyroidism: occurrence and epidemiology. Thyroid. 1998;8(1):83-100.
12. Fatourechi V, Aniszewski JP, Fatourechi GZ, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100-2105.
13. Golden SH, Robinson KA, Saldanha I, et al. Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review. J Clin Endocrinol Metab. 2009;94(6):1853-1878.
14. Volpé R. The management of subacute (DeQuervain's) thyroiditis. Thyroid. 1993;3(3):253-255.
15. Lee SL. Subacute thyroiditis (2009). http://emedicine.medscape.com/article/125648-overview. Accessed April 17, 2012.
A 62-year-old black nursing home resident was transported to the hospital emergency department with fever of 102°F, new-onset atrial fibrillation (A-fib), and dementia. His medical history was significant for hypertension and multiple strokes.
His inpatient work-up for A-fib and dementia revealed a thyroid-stimulating hormone (TSH) level below 0.005 µIU/mL (normal range, 0.3 to 3.0 µIU/mL). Results of thyroid function testing (TFT) revealed a triiodothyronine (T3) level within normal range but a free thyroxine (T4) level of 2.9 ng/dL (normal range, 0.7 to 1.5 ng/dL) and a total T4 of 17.8 µg/dL (normal, 4.5 to 12.0 µg/dL). The abnormal TSH and T4 levels were considered suggestive of a thyrotoxic state, warranting an endocrinology consult. Cardiology was consulted regarding new-onset A-fib.
During history taking, the patient denied any shortness of breath, cough, palpitations, heat intolerance, anxiety, tremors, insomnia, dysphagia, diarrhea, dysuria, weight loss, or recent ingestion of iodine-containing medications or supplements.
On examination, the patient was febrile, with a blood pressure of 106/71 mm Hg; pulse, 74 beats/min; respiratory rate, 20 breaths/min; and O2 saturation, 98% to 99% on room air. ECG showed a normal sinus rhythm and a ventricular rate of 64 beats/min.
The patient's weight was 58.9 kg, and his height, 63" (BMI, 22.8). The patient had no skin changes, and his mucous membranes were slightly moist. The patient's head was atraumatic and normocephalic. His extraocular movements were intact, and his pupils were equal, round, and reactive to light, with nonicteric sclera. There was no proptosis or ophthalmoplegia. The patient's neck was supple, with no jugular venous distension, tracheal deviation, or thyromegaly.
The cardiovascular exam revealed an irregular heartbeat, and repeat ECG showed A-fib with a ventricular rate of 151 beats/min (see Figure 1). The patient's chest was clear, with no wheezing or rhonchi. The abdomen was soft and slightly obese, and bowel sounds were present. The neurologic examination revealed no hyperreflexia. The patient's mental status was altered at times and he was alert, awake, and oriented to others. His speech was slightly slow, and some left-sided weakness was noted.
As recommended during the endocrinology consult, the patient underwent an I-123 sodium iodide thyroid scan, which showed faint uptake at the base of the neck, slightly to the left of midline; and a 24-hour radioactive iodide uptake (RAIU), which measured 2.8% (normal range, 8% to 35%).
The patient's chest X-ray showed a right tracheal deviation not previously noted on physical examination (see Figure 2); the possible cause of a thyroid mass was considered. Subsequent ultrasonography of the thyroid revealed generally normal dimensions and parenchymal echogenicity. However, a large complex mass was detected, arising from the inferior pole of the thyroid and displacing the trachea toward the right (see Figure 3). According to the radiologist's notes, the mass contained both solid and cystic elements, scattered calcifications, and foci of flow on color Doppler. It measured about 6 cm in the largest (transverse) dimension. A 2.0-mm nodule was noted in the isthmus, slightly to the right of midline, consistent with multinodular goiter.
Following the cardiology consult, a diltiazem drip was initiated, but the patient was later optimized on flecainide for rhythm control and metoprolol for rate control. He was also initially anticoagulated using a heparin drip and bridged to warfarin, with target international normalized ratio (INR) between 2.0 and 3.0. Echocardiography revealed normal systolic function with ejection fraction of 55%, left ventricular hypertrophy, pulmonary artery systolic pressure of 35 mm Hg, and no pericardial effusions or valvular disease.
Regarding the patient's unexplained fever, results of chest imaging were negative for signs of pneumonia or atelectasis, which might have suggested a pulmonary cause. Urinalysis results were normal. Complete blood count showed no leukocytosis. The patient's fever subsided within 48 hours.
The differential diagnosis included Graves' disease, toxic multinodular goiter, Jod-Basedow syndrome, and subacute thyroiditis.
Graves' disease, an autoimmune disease with an unknown trigger, is the most common cause of hyperthyroidism. In affected patients, the thyroid gland overproduces thyroid hormones, leading to thyrotoxicosis. Thyrotoxicosis can result in multiple clinical signs and symptoms, including Graves' ophthalmopathy, pretibial myxedema, and goiter; TFT results typically include elevated T3 and T4 and low TSH.1-5 In the case patient (who had no history of thyroid disease, nor clinical signs or symptoms of Graves' disease), low uptake of iodine on thyroid scan precluded this diagnosis.
Toxic multinodular goiter, the second most common cause of hyperthyroidism, can be responsible for A-fib, tachycardia, and congestive heart failure.6,7 Iodine deficiency causes enlargement of the thyroid gland, where numerous nodules can develop, as seen in the case patient. These nodules can function independently, sometimes producing excess thyroid hormone; this leads to hyperplasia of the thyroid gland, resulting in a nontoxic multinodular goiter. From this goiter, a toxic multinodular goiter can emerge insidiously. However, in this condition, RAIU typically exceeds 30%; in the case patient, low 24-hour RAIU (2.8%) and the absence of functioning nodules on scanning made it possible to rule out this diagnosis.
Jod-Basedow syndrome refers to hyperthyroidism that develops as a result of administration of iodide, either as a dietary supplement or as IV contrast medium, or as an adverse effect of the antiarrhythmic drug amiodarone. This phenomenon is usually seen in a patient with endemic goiter.8-11 The relatively limited nature of the case patient's goiter and absence of a precipitating exposure to iodine made this diagnosis highly unlikely.
Subacute thyroiditis is a condition to which the patient's abnormal TFT results could reasonably be attributed. The patient had a substernal multinodular goiter that could not be palpated on physical examination, but it was visualized in the extended lower neck during thyroid scintigraphy.3 RAIU was minimal—a typical finding in this disorder,6 as TSH is suppressed by leakage of the excessive amounts of thyroid hormone. A tentative diagnosis of subacute thyroiditis was made.
As subacute thyroiditis is a self-limiting disorder, the patient was not started on any medications for hyperthyroidism but was advised to follow up with his primary care provider or an endocrinologist for repeat TFT and for fine-needle aspiration biopsy of the large thyroid nodule (a complex mass, containing cystic elements and calcifications, with a potential for malignancy) to rule out thyroid cancer.
Repeat ECG before discharge showed normal sinus rhythm with a ventricular rate of 74 beats/min. The patient was alert, awake, and oriented at discharge. He was continued on flecainide, metoprolol, and warfarin and advised to follow up with his primary care provider regarding his target INR.
DISCUSSION
The incidence of subacute thyroiditis, according to findings reported in 2003 from the Rochester Epidemiology Project in Olmsted County, Minnesota,12 is 12.1 cases per 100,000/year, with a higher incidence in women than men. It is most common in young adults and decreases with advancing age. Coxsackie virus, adenovirus, mumps, echovirus, influenza, and Epstein-Barr virus have been implicated in the disorder.12,13
Subacute thyroiditis is associated with a triphasic clinical course of hyperthyroidism, then hypothyroidism, then a return to normal thyroid function—as was seen in the case patient. Onset of subacute thyroiditis has been associated with recent viral infection, which may serve as a precipitant. The cause of this patient's high fever was never identified; thus, the etiology may have been viral.
The initial high thyroid hormone levels result from inflammation of thyroid tissue and release of preformed thyroid hormone into the circulation.6 At this point, TSH is suppressed and patients have very low RAIU, as was true in the case patient.
The condition is self-limiting and does not require treatment in the majority of patients, as TFT results return to normal levels within about two months.6 Patients can appear extremely ill due to thyrotoxicosis from subacute thyroiditis, but this usually lasts no longer than six to eight weeks.3 Subacute thyroiditis can be associated with atrial arrhythmia or heart failure.14,15
PATIENT OUTCOME
New-onset A-fib was attributed to the patient's thyrotoxicosis, which in turn was caused by subacute thyroiditis. He had a multinodular goiter, although he had not received any iodine supplements or IV contrast. As in most cases of subacute thyroiditis, no precipitating event was identified. However, given this patient's residence in a nursing facility and presentation with a high fever with no identifiable cause, a viral etiology for his subacute thyroiditis is possible.6
The patient's dementia may have been secondary to acute thyrotoxicosis, as his mental state improved during the hospital stay. His vitamin B12, folate, and A1C levels were within normal range. CT of the head showed multiple chronic infarcts and cerebral atrophy, and MRI of the brain indicated microvascular ischemic disease.
The patient was readmitted one month later for an episode of near-syncope (which, it was concluded, was a vasovagal episode). At that time, his TSH was found normal at 1.350 µIU/mL. Flecainide and metoprolol were discontinued; he was started on diltiazem for continued rate and rhythm control (as recommended by cardiology) and continued on warfarin.
CONCLUSION
In this case, subacute thyroiditis was most likely caused by a viral infection that led to destruction of the normal thyroid follicles and release of their preformed thyroid hormone into the circulation; this in turn led to sudden-onset A-fib. The diagnosis of subacute thyroiditis was suggested based on the abnormalities seen in this patient's TFT results, coupled with the suppressed RAIU—a typical finding in this disease.
Because subacute thyroiditis is a self-limiting condition, there is no role for antithyroid medication. Instead, treatment should be focused on relieving the patient's symptoms, such as ß-blockade or calcium channel blockers for tachycardia and corticosteroids or NSAIDs for neck pain.
REFERENCES
1. Weetman AP. Graves' disease. N Engl J Med. 2000;343(17):1236-1248.
2. Delgado Hurtado JJ, Pineda M. Images in medicine: Graves' disease. N Engl J Med. 2011; 364(20):1955.
3. Al-Sharif AA, Abujbara MA, Chiacchio S, et al. Contribution of radioiodine uptake measurement and thyroid scintigraphy to the differential diagnosis of thyrotoxicosis. Hell J Nucl Med. 2010;13(2):132-137.
4. Buccelletti F, Carroccia A, Marsiliani D, et al. Utility of routine thyroid-stimulating hormone determination in new-onset atrial fibrillation in the ED. Am J Emerg Med. 2011;29(9):1158-1162.
5. Ross DS. Radioiodine therapy for hyperthyroidism. N Engl J Med. 2011;364(6):542-550.
6. Bahn RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Endocr Pract. 2011;17(3):456-520.
7. Erickson D, Gharib H, Li H, van Heerden JA. Treatment of patients with toxic multinodular goiter. Thyroid. 1998;8(4):277-282.
8. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med. 2005;118(7):706-714.
9. Bogazzi F, Bartalena L, Martino E. Approach to the patient with amiodarone-induced thyrotoxicosis. J Clin Endocrinol Metab. 2010;95(6):2529-2535.
10. El-Shirbiny AM, Stavrou SS, Dnistrian A, et al. Jod-Basedow syndrome following oral iodine and radioiodinated-antibody administration. J Nucl Med. 1997;38(11):1816-1817.
11. Stanbury JB, Ermans AE, Bourdoux P, et al. Iodine-induced hyperthyroidism: occurrence and epidemiology. Thyroid. 1998;8(1):83-100.
12. Fatourechi V, Aniszewski JP, Fatourechi GZ, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100-2105.
13. Golden SH, Robinson KA, Saldanha I, et al. Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review. J Clin Endocrinol Metab. 2009;94(6):1853-1878.
14. Volpé R. The management of subacute (DeQuervain's) thyroiditis. Thyroid. 1993;3(3):253-255.
15. Lee SL. Subacute thyroiditis (2009). http://emedicine.medscape.com/article/125648-overview. Accessed April 17, 2012.
The "Holy Grail," Where Do We Go From Here?
As physicians, we are always trying to keep up with the latest techniques and technology to provide the best possible care for our patients. However, history shows us that many of the “newest and greatest” devices have poorly understood, or maybe even, unknown consequences. You may remember the excitement over the Gortex ligament augmentation device (LAD) for ACL reconstruction in the 1970’s or the thermal capsular shrinkage “heat probe” of the 1990’s. The orthopedic annals are littered with groundbreaking technologies that proved to be, at best, merely failures,or, at worst, dangerous to the patients we are trying to heal.
We are now in a time of rapidly changing technology and information overload, clogged with access to reams of information through our PDAs and the internet. Patients learn about new techniques and technology not from their physician, but from advertisements in the media or online. This dissemination of information without any real “filter” to verify accuracy and safety has heightened the burden on us, as surgeons, to be up to speed and critical of every “better mousetrap.” Patients may request or even demand a certain technique based on limited study of online discussions, chat rooms, or non–peer reviewed data. It is our obligation to “first, do no harm” even if the patient demands it.
How can we possibly provide the best for our patients and keep up with technology that may prove to be “the holy grail”? We must rely on well planned, peer-reviewed research studies that clearly analyze not only the positive results, but also the potential complications of new technology. In this month’s issue, E. Carlos Rodríguez-Merchán MD, PhD, (‘‘The Treatment of Cartilage Defects in the Knee Joint: Microfracture, Mosaicplasty, and Autologous Chondrocyte Implantation,’’click here) reviews the treatment of cartilage defects in the knee joint: comparing microfracture, mosaicplasty, and autologous chondrocyte implantation (ACI). However, he concludes that good level I evidence is lacking to show significant difference between any of the 3 commonly performed techniques. Does this mean that all of the procedures result in equal outcomes? No. Does this mean that we should abandon the more costly procedures, such as ACI? No. What Dr. Rodríguez-Merchán does is highlight the need for carefully designed level I studies to define the real outcomes, indications, and complications of our new technologies.
What is the holy grail in orthopedics? I would argue that the ability to take an easily obtained and prepared stem cell line and use the appropriate growth factors and chemical signals to cause the cells to differentiate into different tissue types (eg, bone, cartilage, ligament, etc.) represents this holy grail. Think about all of the potential uses for this technology and it is easy to see the whole field of orthopedic surgery being transformed during my lifetime. Imagine being able to grow new cartilage or ligament tissue and direct the body’s response to these new tissues. However, with these possibilities also come enormous risk.
One significant unpredicted outcome or inappropriate application could lead to huge consequences, terrible complications, bad publicity, and loss of patient-physician trust. Just imagine the late night television commercials and billboards advertising for the local law firm that “you may be entitled to compensation.” Or just imagine the uncertainty injected into the physician-patient relationship, “you aren’t going to put one of those recalled parts in me are you?” You may have followed the recent controversy over “pink slime,” the “lean, finely textured beef” added to processed hamburger patties. Although used for decades, the recent media coverage of beef filler has severely affected the public’s trust in the food industry. Can you imagine how a similar public relations nightmare over failed technology could affect the orthopedic industry?
I have often been guilty of complaining about the arduous task of getting new technology approved though the regulatory bodies in the United States, compared with the perceived progressive nature of the process in Europe. I do believe that we should have a streamlined process for some new technology that may save lives, especially chemotherapy medications. However, a more diligent, and thorough process must be applied to new technology used for elective procedures, as in most orthopedic applications. Unfortunately, until sufficient safety data and good outcomes research is completed and analyzed, we must temper the enthusiasm of doctors and patients alike.
Author's Disclosure Statement. The author reports no actual or potential conflict of interest in relation to this article.
As physicians, we are always trying to keep up with the latest techniques and technology to provide the best possible care for our patients. However, history shows us that many of the “newest and greatest” devices have poorly understood, or maybe even, unknown consequences. You may remember the excitement over the Gortex ligament augmentation device (LAD) for ACL reconstruction in the 1970’s or the thermal capsular shrinkage “heat probe” of the 1990’s. The orthopedic annals are littered with groundbreaking technologies that proved to be, at best, merely failures,or, at worst, dangerous to the patients we are trying to heal.
We are now in a time of rapidly changing technology and information overload, clogged with access to reams of information through our PDAs and the internet. Patients learn about new techniques and technology not from their physician, but from advertisements in the media or online. This dissemination of information without any real “filter” to verify accuracy and safety has heightened the burden on us, as surgeons, to be up to speed and critical of every “better mousetrap.” Patients may request or even demand a certain technique based on limited study of online discussions, chat rooms, or non–peer reviewed data. It is our obligation to “first, do no harm” even if the patient demands it.
How can we possibly provide the best for our patients and keep up with technology that may prove to be “the holy grail”? We must rely on well planned, peer-reviewed research studies that clearly analyze not only the positive results, but also the potential complications of new technology. In this month’s issue, E. Carlos Rodríguez-Merchán MD, PhD, (‘‘The Treatment of Cartilage Defects in the Knee Joint: Microfracture, Mosaicplasty, and Autologous Chondrocyte Implantation,’’click here) reviews the treatment of cartilage defects in the knee joint: comparing microfracture, mosaicplasty, and autologous chondrocyte implantation (ACI). However, he concludes that good level I evidence is lacking to show significant difference between any of the 3 commonly performed techniques. Does this mean that all of the procedures result in equal outcomes? No. Does this mean that we should abandon the more costly procedures, such as ACI? No. What Dr. Rodríguez-Merchán does is highlight the need for carefully designed level I studies to define the real outcomes, indications, and complications of our new technologies.
What is the holy grail in orthopedics? I would argue that the ability to take an easily obtained and prepared stem cell line and use the appropriate growth factors and chemical signals to cause the cells to differentiate into different tissue types (eg, bone, cartilage, ligament, etc.) represents this holy grail. Think about all of the potential uses for this technology and it is easy to see the whole field of orthopedic surgery being transformed during my lifetime. Imagine being able to grow new cartilage or ligament tissue and direct the body’s response to these new tissues. However, with these possibilities also come enormous risk.
One significant unpredicted outcome or inappropriate application could lead to huge consequences, terrible complications, bad publicity, and loss of patient-physician trust. Just imagine the late night television commercials and billboards advertising for the local law firm that “you may be entitled to compensation.” Or just imagine the uncertainty injected into the physician-patient relationship, “you aren’t going to put one of those recalled parts in me are you?” You may have followed the recent controversy over “pink slime,” the “lean, finely textured beef” added to processed hamburger patties. Although used for decades, the recent media coverage of beef filler has severely affected the public’s trust in the food industry. Can you imagine how a similar public relations nightmare over failed technology could affect the orthopedic industry?
I have often been guilty of complaining about the arduous task of getting new technology approved though the regulatory bodies in the United States, compared with the perceived progressive nature of the process in Europe. I do believe that we should have a streamlined process for some new technology that may save lives, especially chemotherapy medications. However, a more diligent, and thorough process must be applied to new technology used for elective procedures, as in most orthopedic applications. Unfortunately, until sufficient safety data and good outcomes research is completed and analyzed, we must temper the enthusiasm of doctors and patients alike.
Author's Disclosure Statement. The author reports no actual or potential conflict of interest in relation to this article.
As physicians, we are always trying to keep up with the latest techniques and technology to provide the best possible care for our patients. However, history shows us that many of the “newest and greatest” devices have poorly understood, or maybe even, unknown consequences. You may remember the excitement over the Gortex ligament augmentation device (LAD) for ACL reconstruction in the 1970’s or the thermal capsular shrinkage “heat probe” of the 1990’s. The orthopedic annals are littered with groundbreaking technologies that proved to be, at best, merely failures,or, at worst, dangerous to the patients we are trying to heal.
We are now in a time of rapidly changing technology and information overload, clogged with access to reams of information through our PDAs and the internet. Patients learn about new techniques and technology not from their physician, but from advertisements in the media or online. This dissemination of information without any real “filter” to verify accuracy and safety has heightened the burden on us, as surgeons, to be up to speed and critical of every “better mousetrap.” Patients may request or even demand a certain technique based on limited study of online discussions, chat rooms, or non–peer reviewed data. It is our obligation to “first, do no harm” even if the patient demands it.
How can we possibly provide the best for our patients and keep up with technology that may prove to be “the holy grail”? We must rely on well planned, peer-reviewed research studies that clearly analyze not only the positive results, but also the potential complications of new technology. In this month’s issue, E. Carlos Rodríguez-Merchán MD, PhD, (‘‘The Treatment of Cartilage Defects in the Knee Joint: Microfracture, Mosaicplasty, and Autologous Chondrocyte Implantation,’’click here) reviews the treatment of cartilage defects in the knee joint: comparing microfracture, mosaicplasty, and autologous chondrocyte implantation (ACI). However, he concludes that good level I evidence is lacking to show significant difference between any of the 3 commonly performed techniques. Does this mean that all of the procedures result in equal outcomes? No. Does this mean that we should abandon the more costly procedures, such as ACI? No. What Dr. Rodríguez-Merchán does is highlight the need for carefully designed level I studies to define the real outcomes, indications, and complications of our new technologies.
What is the holy grail in orthopedics? I would argue that the ability to take an easily obtained and prepared stem cell line and use the appropriate growth factors and chemical signals to cause the cells to differentiate into different tissue types (eg, bone, cartilage, ligament, etc.) represents this holy grail. Think about all of the potential uses for this technology and it is easy to see the whole field of orthopedic surgery being transformed during my lifetime. Imagine being able to grow new cartilage or ligament tissue and direct the body’s response to these new tissues. However, with these possibilities also come enormous risk.
One significant unpredicted outcome or inappropriate application could lead to huge consequences, terrible complications, bad publicity, and loss of patient-physician trust. Just imagine the late night television commercials and billboards advertising for the local law firm that “you may be entitled to compensation.” Or just imagine the uncertainty injected into the physician-patient relationship, “you aren’t going to put one of those recalled parts in me are you?” You may have followed the recent controversy over “pink slime,” the “lean, finely textured beef” added to processed hamburger patties. Although used for decades, the recent media coverage of beef filler has severely affected the public’s trust in the food industry. Can you imagine how a similar public relations nightmare over failed technology could affect the orthopedic industry?
I have often been guilty of complaining about the arduous task of getting new technology approved though the regulatory bodies in the United States, compared with the perceived progressive nature of the process in Europe. I do believe that we should have a streamlined process for some new technology that may save lives, especially chemotherapy medications. However, a more diligent, and thorough process must be applied to new technology used for elective procedures, as in most orthopedic applications. Unfortunately, until sufficient safety data and good outcomes research is completed and analyzed, we must temper the enthusiasm of doctors and patients alike.
Author's Disclosure Statement. The author reports no actual or potential conflict of interest in relation to this article.
The Treatment of Cartilage Defects in the Knee Joint: Microfracture, Mosaicplasty, and Autologous Chondrocyte Implantation
Bone Graft Extenders and Substitutes in the Thoracolumbar Spine
An Innovative Approach to Concave-Convex Allograft Junctions: A Biomechanical Study
Epithelioid Sarcoma: An Unusual Presentation in the Distal Phalanx of the Toe
Alopecia in an Ophiasis Pattern: Traction Alopecia Versus Alopecia Areata
"Hemorrhoids" turn out to be cancer … and more
“Hemorrhoids” turn out to be cancer
A 49-YEAR-OLD WOMAN, whose husband was on active duty with the US Army, went to an army community hospital in March complaining of hemorrhoids, back pain, and itching, burning, and pain with bowel movements. A guaiac-based fecal occult blood test was positive; no further testing was done to rule out rectal cancer.
The woman was discharged with pain medication but returned the following day, reporting intense anal pain despite taking the medication and bright red blood in her stools. The symptoms were attributed to hemorrhoids, and the patient was given a toilet “donut” and topical medication. Although her records noted a referral to a general surgeon, the referral wasn’t arranged or scheduled.
The patient returned to the hospital in April, May, and June with continuing complaints that included unrelieved constipation. A laxative was prescribed, but no further testing was done, nor was the patient referred to a surgeon.
In August, she went to the emergency department because of rectal bleeding for the previous 2 weeks, abdominal pain, blood in her urine, and difficulty breathing. Once again the symptoms were blamed on hemorrhoids even though the patient questioned the diagnosis.
The patient continued to see various providers at the army community hospital for the rest of the year, during which time she turned 50. None of them recommended a colonoscopy despite standard recommendations to begin colorectal cancer screening at 50 years of age and the woman’s symptoms, which suggested colorectal cancer.
In March of the following year, the patient consulted a bariatric surgeon in private practice, who recommended evaluating the patient’s bloody stools and offered to perform a diagnostic colonoscopy if authorized. The army hospital didn’t immediately authorize the procedure, and it wasn’t performed.
In late September, the patient consulted a surgeon at the hospital, by which time bright red blood was squirting from her anal region and appeared in the toilet water after every bowel movement. She had never undergone a full colon evaluation.
Less than a week after the surgery consult, the patient’s husband was transferred to another military base. Her doctors said that a surgeon at the new base would be told about her medical condition, but that didn’t happen.
Five months later, a surgery consultation at the new military base found a rectal lesion extending 8 cm into the rectum from the anal verge. Pathology confirmed stage IIIC mucinous adenocarcinoma that had spread to the lymph nodes. Two years later, after several surgeries, chemotherapy, and radiation, the patient died at 53 years of age.
PLAINTIFF’S CLAIM If testing to rule out rectal cancer, such as a colonoscopy, had been performed earlier, the cancer would have been diagnosed at a curable stage.
THE DEFENSE No information about the defense is available.
VERDICT $2.15 million Tennessee settlement.
COMMENT Recurrent, unrelenting symptoms should prompt the alert clinician to explore alternative diagnoses.
For want of diagnosis and treatment, kidney function is lost
A FEBRILE ILLNESS prompted a patient to visit his primary care physician. After 3 months of treatment by the primary care doctor, the patient sought a second opinion and treatment from a federally funded community health clinic, where he was treated for 2 more months. During that time, the patient developed signs and symptoms of impaired kidney function, which laboratory results confirmed.
The clinic staff didn’t address the possible loss of kidney function. Three days after his last examination at the clinic, the patient went to a hospital emergency department, where he was promptly diagnosed with subacute bacterial endocarditis. His kidney function could not be restored.
PLAINTIFF’S CLAIM The primary care physician and the staff at the clinic were negligent in failing to diagnose and treat the kidney issues. Also, they didn’t recognize and treat the signs and symptoms of subacute bacterial endocarditis.
THE DEFENSE The primary care physician claimed that the patient’s injuries resulted solely from negligence on the part of the clinic staff. He maintained that the patient’s kidney function was normal when the man left his care. The federal government, on behalf of the clinic staff, claimed that the primary care physician was at least 50% responsible for the patient’s injuries.
VERDICT $1.45 million Texas settlement.
COMMENT Subacute bacterial endocarditis can be a challenging diagnosis because of the subtlety and variety of presentations. Remember the zebras when confronted with unexplained symptoms and signs.
Neuropathy blamed on belated diabetes diagnosis
A PATIENT IN A FAMILY PRACTICE was treated by several of the doctors and a physician assistant in the group over about a decade. After the patient developed neuropathy in his arms and legs, he was diagnosed with type 2 diabetes.
PLAINTIFF’S CLAIM Earlier diagnosis of the diabetes would have prevented development of neuropathy. High blood glucose levels identified on tests weren’t addressed.
THE DEFENSE Only 3 tests had shown excessive levels of glucose; the patient had many comorbidities that required attention. A special diet had been prescribed that would have helped control glucose levels. This was an appropriate initial step to address a diagnosis of type 2 diabetes.
VERDICT $285,000 New York settlement.
COMMENT It’s easy to overlook or postpone treatment of apparently less urgent issues such as glucose intolerance. Clear documentation and explicit discussion with patients might help mitigate the risk of adverse judgments.
Too many narcotic prescriptions
A WOMAN TREATED FOR CHRONIC SINUSITIS by an ear, nose, and throat physician received prescriptions for oxycodone, acetaminophen and oxycodone, and methadone for years to relieve headaches and facial pain. She died at 40 years of age from a methadone overdose. The physician admitted in a deposition that he’d kept on prescribing the medications even after the patient’s health insurer informed him that she was obtaining narcotics from multiple providers.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.05 million New Jersey settlement.
COMMENT Strict tracking and oversight of opioid administration is essential. Clear documentation and regular follow-up remain very important.
Delayed Tx turns skin breakdown into a long-term problem
A NEARLY IMMOBILE WOMAN was discharged from a hospital—where she’d been treated for congestive heart failure, hypertension, diabetes, altered mental status, severe arthritis, and gout—and transported by ambulance to her home. Discharge diagnoses included possible obstructive sleep apnea and hypercapnia. Because the patient needed a great deal of help with activities of daily living, her physician ordered home health services.
Twelve days after discharge, a representative from the home health agency performed an initial assessment in the patient’s home, at which time the patient’s daughter reported that her mother had developed some skin breakdown on her buttocks that required care. The home health nurse allegedly told the daughter that the agency would need an order from her mother’s physician before starting home treatment for the skin breakdown.
The daughter phoned the physician every day for the next few days to get treatment authorization, but the doctor didn’t return her calls. The home health agency didn’t seek authorization from the doctor.
When the home health nurse returned to the patient’s home a week later to begin care, the daughter again mentioned the areas of skin breakdown, which by that time had become pressure sores. The nurse didn’t treat the pressure sores. The home health agency tried to contact the patient’s physician, who didn’t return their calls.
The agency finally received an order to treat the pressure sores 6 days after the home health nurse had begun caring for the patient, by which time the sores were infected and considerably larger. Healing required more than a year of treatment.
PLAINTIFF’S CLAIM As a result of the delay in treating the pressure sores, the patient’s condition was worse that it otherwise would have been.
THE DEFENSE The defendants denied any negligence.
VERDICT Alabama defense verdict.
COMMENT Better communication and coordination of care between home health providers and a patient’s medical home are important to provide optimal care—and avoid lawsuits.
“Hemorrhoids” turn out to be cancer
A 49-YEAR-OLD WOMAN, whose husband was on active duty with the US Army, went to an army community hospital in March complaining of hemorrhoids, back pain, and itching, burning, and pain with bowel movements. A guaiac-based fecal occult blood test was positive; no further testing was done to rule out rectal cancer.
The woman was discharged with pain medication but returned the following day, reporting intense anal pain despite taking the medication and bright red blood in her stools. The symptoms were attributed to hemorrhoids, and the patient was given a toilet “donut” and topical medication. Although her records noted a referral to a general surgeon, the referral wasn’t arranged or scheduled.
The patient returned to the hospital in April, May, and June with continuing complaints that included unrelieved constipation. A laxative was prescribed, but no further testing was done, nor was the patient referred to a surgeon.
In August, she went to the emergency department because of rectal bleeding for the previous 2 weeks, abdominal pain, blood in her urine, and difficulty breathing. Once again the symptoms were blamed on hemorrhoids even though the patient questioned the diagnosis.
The patient continued to see various providers at the army community hospital for the rest of the year, during which time she turned 50. None of them recommended a colonoscopy despite standard recommendations to begin colorectal cancer screening at 50 years of age and the woman’s symptoms, which suggested colorectal cancer.
In March of the following year, the patient consulted a bariatric surgeon in private practice, who recommended evaluating the patient’s bloody stools and offered to perform a diagnostic colonoscopy if authorized. The army hospital didn’t immediately authorize the procedure, and it wasn’t performed.
In late September, the patient consulted a surgeon at the hospital, by which time bright red blood was squirting from her anal region and appeared in the toilet water after every bowel movement. She had never undergone a full colon evaluation.
Less than a week after the surgery consult, the patient’s husband was transferred to another military base. Her doctors said that a surgeon at the new base would be told about her medical condition, but that didn’t happen.
Five months later, a surgery consultation at the new military base found a rectal lesion extending 8 cm into the rectum from the anal verge. Pathology confirmed stage IIIC mucinous adenocarcinoma that had spread to the lymph nodes. Two years later, after several surgeries, chemotherapy, and radiation, the patient died at 53 years of age.
PLAINTIFF’S CLAIM If testing to rule out rectal cancer, such as a colonoscopy, had been performed earlier, the cancer would have been diagnosed at a curable stage.
THE DEFENSE No information about the defense is available.
VERDICT $2.15 million Tennessee settlement.
COMMENT Recurrent, unrelenting symptoms should prompt the alert clinician to explore alternative diagnoses.
For want of diagnosis and treatment, kidney function is lost
A FEBRILE ILLNESS prompted a patient to visit his primary care physician. After 3 months of treatment by the primary care doctor, the patient sought a second opinion and treatment from a federally funded community health clinic, where he was treated for 2 more months. During that time, the patient developed signs and symptoms of impaired kidney function, which laboratory results confirmed.
The clinic staff didn’t address the possible loss of kidney function. Three days after his last examination at the clinic, the patient went to a hospital emergency department, where he was promptly diagnosed with subacute bacterial endocarditis. His kidney function could not be restored.
PLAINTIFF’S CLAIM The primary care physician and the staff at the clinic were negligent in failing to diagnose and treat the kidney issues. Also, they didn’t recognize and treat the signs and symptoms of subacute bacterial endocarditis.
THE DEFENSE The primary care physician claimed that the patient’s injuries resulted solely from negligence on the part of the clinic staff. He maintained that the patient’s kidney function was normal when the man left his care. The federal government, on behalf of the clinic staff, claimed that the primary care physician was at least 50% responsible for the patient’s injuries.
VERDICT $1.45 million Texas settlement.
COMMENT Subacute bacterial endocarditis can be a challenging diagnosis because of the subtlety and variety of presentations. Remember the zebras when confronted with unexplained symptoms and signs.
Neuropathy blamed on belated diabetes diagnosis
A PATIENT IN A FAMILY PRACTICE was treated by several of the doctors and a physician assistant in the group over about a decade. After the patient developed neuropathy in his arms and legs, he was diagnosed with type 2 diabetes.
PLAINTIFF’S CLAIM Earlier diagnosis of the diabetes would have prevented development of neuropathy. High blood glucose levels identified on tests weren’t addressed.
THE DEFENSE Only 3 tests had shown excessive levels of glucose; the patient had many comorbidities that required attention. A special diet had been prescribed that would have helped control glucose levels. This was an appropriate initial step to address a diagnosis of type 2 diabetes.
VERDICT $285,000 New York settlement.
COMMENT It’s easy to overlook or postpone treatment of apparently less urgent issues such as glucose intolerance. Clear documentation and explicit discussion with patients might help mitigate the risk of adverse judgments.
Too many narcotic prescriptions
A WOMAN TREATED FOR CHRONIC SINUSITIS by an ear, nose, and throat physician received prescriptions for oxycodone, acetaminophen and oxycodone, and methadone for years to relieve headaches and facial pain. She died at 40 years of age from a methadone overdose. The physician admitted in a deposition that he’d kept on prescribing the medications even after the patient’s health insurer informed him that she was obtaining narcotics from multiple providers.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.05 million New Jersey settlement.
COMMENT Strict tracking and oversight of opioid administration is essential. Clear documentation and regular follow-up remain very important.
Delayed Tx turns skin breakdown into a long-term problem
A NEARLY IMMOBILE WOMAN was discharged from a hospital—where she’d been treated for congestive heart failure, hypertension, diabetes, altered mental status, severe arthritis, and gout—and transported by ambulance to her home. Discharge diagnoses included possible obstructive sleep apnea and hypercapnia. Because the patient needed a great deal of help with activities of daily living, her physician ordered home health services.
Twelve days after discharge, a representative from the home health agency performed an initial assessment in the patient’s home, at which time the patient’s daughter reported that her mother had developed some skin breakdown on her buttocks that required care. The home health nurse allegedly told the daughter that the agency would need an order from her mother’s physician before starting home treatment for the skin breakdown.
The daughter phoned the physician every day for the next few days to get treatment authorization, but the doctor didn’t return her calls. The home health agency didn’t seek authorization from the doctor.
When the home health nurse returned to the patient’s home a week later to begin care, the daughter again mentioned the areas of skin breakdown, which by that time had become pressure sores. The nurse didn’t treat the pressure sores. The home health agency tried to contact the patient’s physician, who didn’t return their calls.
The agency finally received an order to treat the pressure sores 6 days after the home health nurse had begun caring for the patient, by which time the sores were infected and considerably larger. Healing required more than a year of treatment.
PLAINTIFF’S CLAIM As a result of the delay in treating the pressure sores, the patient’s condition was worse that it otherwise would have been.
THE DEFENSE The defendants denied any negligence.
VERDICT Alabama defense verdict.
COMMENT Better communication and coordination of care between home health providers and a patient’s medical home are important to provide optimal care—and avoid lawsuits.
“Hemorrhoids” turn out to be cancer
A 49-YEAR-OLD WOMAN, whose husband was on active duty with the US Army, went to an army community hospital in March complaining of hemorrhoids, back pain, and itching, burning, and pain with bowel movements. A guaiac-based fecal occult blood test was positive; no further testing was done to rule out rectal cancer.
The woman was discharged with pain medication but returned the following day, reporting intense anal pain despite taking the medication and bright red blood in her stools. The symptoms were attributed to hemorrhoids, and the patient was given a toilet “donut” and topical medication. Although her records noted a referral to a general surgeon, the referral wasn’t arranged or scheduled.
The patient returned to the hospital in April, May, and June with continuing complaints that included unrelieved constipation. A laxative was prescribed, but no further testing was done, nor was the patient referred to a surgeon.
In August, she went to the emergency department because of rectal bleeding for the previous 2 weeks, abdominal pain, blood in her urine, and difficulty breathing. Once again the symptoms were blamed on hemorrhoids even though the patient questioned the diagnosis.
The patient continued to see various providers at the army community hospital for the rest of the year, during which time she turned 50. None of them recommended a colonoscopy despite standard recommendations to begin colorectal cancer screening at 50 years of age and the woman’s symptoms, which suggested colorectal cancer.
In March of the following year, the patient consulted a bariatric surgeon in private practice, who recommended evaluating the patient’s bloody stools and offered to perform a diagnostic colonoscopy if authorized. The army hospital didn’t immediately authorize the procedure, and it wasn’t performed.
In late September, the patient consulted a surgeon at the hospital, by which time bright red blood was squirting from her anal region and appeared in the toilet water after every bowel movement. She had never undergone a full colon evaluation.
Less than a week after the surgery consult, the patient’s husband was transferred to another military base. Her doctors said that a surgeon at the new base would be told about her medical condition, but that didn’t happen.
Five months later, a surgery consultation at the new military base found a rectal lesion extending 8 cm into the rectum from the anal verge. Pathology confirmed stage IIIC mucinous adenocarcinoma that had spread to the lymph nodes. Two years later, after several surgeries, chemotherapy, and radiation, the patient died at 53 years of age.
PLAINTIFF’S CLAIM If testing to rule out rectal cancer, such as a colonoscopy, had been performed earlier, the cancer would have been diagnosed at a curable stage.
THE DEFENSE No information about the defense is available.
VERDICT $2.15 million Tennessee settlement.
COMMENT Recurrent, unrelenting symptoms should prompt the alert clinician to explore alternative diagnoses.
For want of diagnosis and treatment, kidney function is lost
A FEBRILE ILLNESS prompted a patient to visit his primary care physician. After 3 months of treatment by the primary care doctor, the patient sought a second opinion and treatment from a federally funded community health clinic, where he was treated for 2 more months. During that time, the patient developed signs and symptoms of impaired kidney function, which laboratory results confirmed.
The clinic staff didn’t address the possible loss of kidney function. Three days after his last examination at the clinic, the patient went to a hospital emergency department, where he was promptly diagnosed with subacute bacterial endocarditis. His kidney function could not be restored.
PLAINTIFF’S CLAIM The primary care physician and the staff at the clinic were negligent in failing to diagnose and treat the kidney issues. Also, they didn’t recognize and treat the signs and symptoms of subacute bacterial endocarditis.
THE DEFENSE The primary care physician claimed that the patient’s injuries resulted solely from negligence on the part of the clinic staff. He maintained that the patient’s kidney function was normal when the man left his care. The federal government, on behalf of the clinic staff, claimed that the primary care physician was at least 50% responsible for the patient’s injuries.
VERDICT $1.45 million Texas settlement.
COMMENT Subacute bacterial endocarditis can be a challenging diagnosis because of the subtlety and variety of presentations. Remember the zebras when confronted with unexplained symptoms and signs.
Neuropathy blamed on belated diabetes diagnosis
A PATIENT IN A FAMILY PRACTICE was treated by several of the doctors and a physician assistant in the group over about a decade. After the patient developed neuropathy in his arms and legs, he was diagnosed with type 2 diabetes.
PLAINTIFF’S CLAIM Earlier diagnosis of the diabetes would have prevented development of neuropathy. High blood glucose levels identified on tests weren’t addressed.
THE DEFENSE Only 3 tests had shown excessive levels of glucose; the patient had many comorbidities that required attention. A special diet had been prescribed that would have helped control glucose levels. This was an appropriate initial step to address a diagnosis of type 2 diabetes.
VERDICT $285,000 New York settlement.
COMMENT It’s easy to overlook or postpone treatment of apparently less urgent issues such as glucose intolerance. Clear documentation and explicit discussion with patients might help mitigate the risk of adverse judgments.
Too many narcotic prescriptions
A WOMAN TREATED FOR CHRONIC SINUSITIS by an ear, nose, and throat physician received prescriptions for oxycodone, acetaminophen and oxycodone, and methadone for years to relieve headaches and facial pain. She died at 40 years of age from a methadone overdose. The physician admitted in a deposition that he’d kept on prescribing the medications even after the patient’s health insurer informed him that she was obtaining narcotics from multiple providers.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.05 million New Jersey settlement.
COMMENT Strict tracking and oversight of opioid administration is essential. Clear documentation and regular follow-up remain very important.
Delayed Tx turns skin breakdown into a long-term problem
A NEARLY IMMOBILE WOMAN was discharged from a hospital—where she’d been treated for congestive heart failure, hypertension, diabetes, altered mental status, severe arthritis, and gout—and transported by ambulance to her home. Discharge diagnoses included possible obstructive sleep apnea and hypercapnia. Because the patient needed a great deal of help with activities of daily living, her physician ordered home health services.
Twelve days after discharge, a representative from the home health agency performed an initial assessment in the patient’s home, at which time the patient’s daughter reported that her mother had developed some skin breakdown on her buttocks that required care. The home health nurse allegedly told the daughter that the agency would need an order from her mother’s physician before starting home treatment for the skin breakdown.
The daughter phoned the physician every day for the next few days to get treatment authorization, but the doctor didn’t return her calls. The home health agency didn’t seek authorization from the doctor.
When the home health nurse returned to the patient’s home a week later to begin care, the daughter again mentioned the areas of skin breakdown, which by that time had become pressure sores. The nurse didn’t treat the pressure sores. The home health agency tried to contact the patient’s physician, who didn’t return their calls.
The agency finally received an order to treat the pressure sores 6 days after the home health nurse had begun caring for the patient, by which time the sores were infected and considerably larger. Healing required more than a year of treatment.
PLAINTIFF’S CLAIM As a result of the delay in treating the pressure sores, the patient’s condition was worse that it otherwise would have been.
THE DEFENSE The defendants denied any negligence.
VERDICT Alabama defense verdict.
COMMENT Better communication and coordination of care between home health providers and a patient’s medical home are important to provide optimal care—and avoid lawsuits.
The latest recommendations from the USPSTF
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.