User login
RIV spotlights HM-focused research in real-time
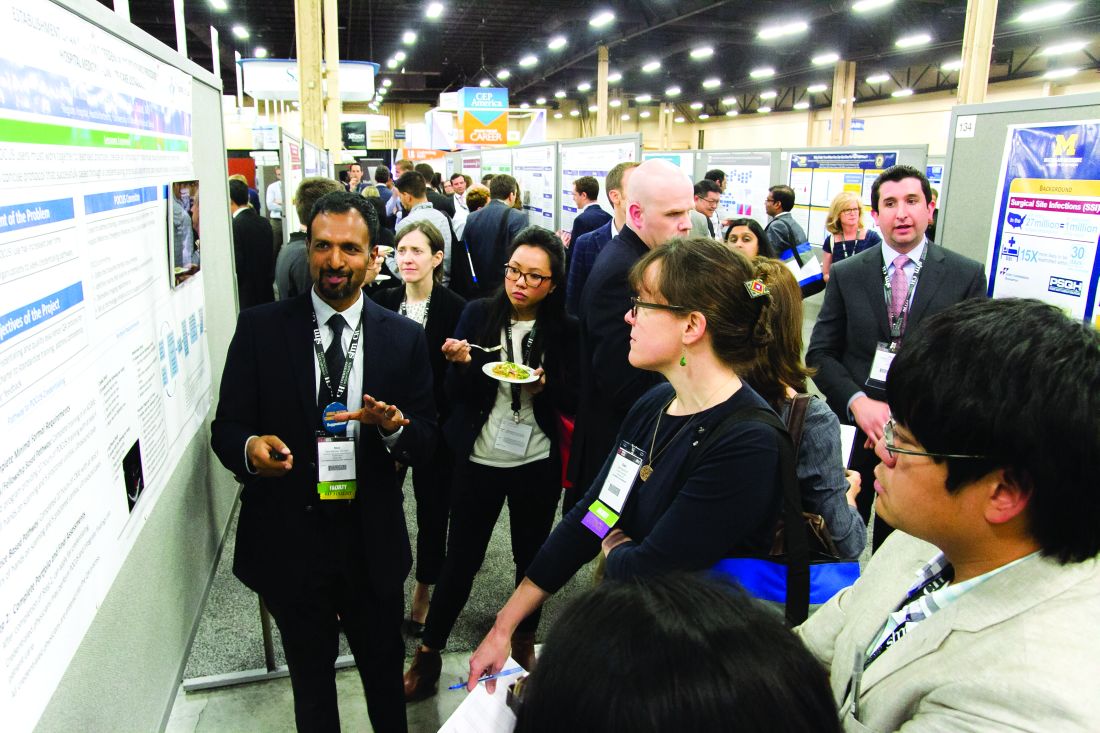
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
Hospitalists share strategies to secure, excel at jobs
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
Hospitalists’ EMR frustrations continue: SHM report
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
12 things pharmacists want hospitalists to know
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
Using shock index in the ED to predict hospital admission and inpatient mortality
CLINICAL QUESTION: Can shock index (SI) in the ED predict the likelihood for hospital admission and inpatient mortality?
STUDY DESIGN: Retrospective chart review.
SETTING: Academic tertiary care center.
SYNOPSIS: All ED patients over 18 years of age over a 12-month period were included in the study for a total of 58,633 charts. Charts were excluded if the patient presented in cardiac arrest, left prior to full evaluation in the ED, or had an incomplete or absent first set of vital signs. Likelihood ratio (LR) values of greater than 5 and 10 were considered moderate and large increases in the outcomes, respectively. Authors found SI greater than 1.2 had a positive LR of 11.69 for admission to the hospital and a positive LR of 5.82 for inpatient mortality.
This study identified potential thresholds for SI but did not validate them. Whether SI would be a useful tool for triage remains unanswered.
BOTTOM LINE: Initial SI greater than 1.2 at presentation to the ED was associated with increased likelihood of hospital admission and inpatient mortality.
CITATIONS: Balhara KS, Hsieh YH, Hamade B, et al. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J. 2017 Feb;34(2):89-94.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Can shock index (SI) in the ED predict the likelihood for hospital admission and inpatient mortality?
STUDY DESIGN: Retrospective chart review.
SETTING: Academic tertiary care center.
SYNOPSIS: All ED patients over 18 years of age over a 12-month period were included in the study for a total of 58,633 charts. Charts were excluded if the patient presented in cardiac arrest, left prior to full evaluation in the ED, or had an incomplete or absent first set of vital signs. Likelihood ratio (LR) values of greater than 5 and 10 were considered moderate and large increases in the outcomes, respectively. Authors found SI greater than 1.2 had a positive LR of 11.69 for admission to the hospital and a positive LR of 5.82 for inpatient mortality.
This study identified potential thresholds for SI but did not validate them. Whether SI would be a useful tool for triage remains unanswered.
BOTTOM LINE: Initial SI greater than 1.2 at presentation to the ED was associated with increased likelihood of hospital admission and inpatient mortality.
CITATIONS: Balhara KS, Hsieh YH, Hamade B, et al. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J. 2017 Feb;34(2):89-94.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Can shock index (SI) in the ED predict the likelihood for hospital admission and inpatient mortality?
STUDY DESIGN: Retrospective chart review.
SETTING: Academic tertiary care center.
SYNOPSIS: All ED patients over 18 years of age over a 12-month period were included in the study for a total of 58,633 charts. Charts were excluded if the patient presented in cardiac arrest, left prior to full evaluation in the ED, or had an incomplete or absent first set of vital signs. Likelihood ratio (LR) values of greater than 5 and 10 were considered moderate and large increases in the outcomes, respectively. Authors found SI greater than 1.2 had a positive LR of 11.69 for admission to the hospital and a positive LR of 5.82 for inpatient mortality.
This study identified potential thresholds for SI but did not validate them. Whether SI would be a useful tool for triage remains unanswered.
BOTTOM LINE: Initial SI greater than 1.2 at presentation to the ED was associated with increased likelihood of hospital admission and inpatient mortality.
CITATIONS: Balhara KS, Hsieh YH, Hamade B, et al. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J. 2017 Feb;34(2):89-94.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Perioperative statin associated with reduction in all-cause perioperative mortality in noncardiac surgery
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does perioperative statin use reduce 30-day mortality in noncardiac surgery?
BACKGROUND: Current perioperative guidelines focus on continuation of existing therapy in long-term statin users with weak recommendations of potential efficacy in reducing perioperative complications.
STUDY DESIGN: Retrospective, observational cohort analysis.
SYNOPSIS: Using the Veterans Affairs Surgical Quality Improvement Program database, 96,486 patients were studied who were undergoing elective or emergent noncardiac surgery (vascular, general, orthopedic, neurosurgery, otolaryngology, and urology). 96.3% were men. Patients who died the day of the surgery or the day after were excluded, as were patients with multiple surgeries during the assessment period. Statin exposure on the day of or the day after surgery was compared with no statin use. The primary outcome was 30-day mortality and the secondary outcomes were significant reduction in any other complication.
Statin exposure was associated with reduced 30-day all-cause mortality with a marginally favorable effect with longer-term statin use (6 months to 1 year before admission). For the secondary outcomes, there was significant risk reduction in cardiac, infectious, respiratory, and renal complications but no significant change in central nervous system or nonatherosclerotic thrombotic complications.
Statin exposure may be associated with adherence to medical treatment and follow-up thus causing a selection bias.
BOTTOM LINE: Perioperative statin use was associated with a reduction in 30-day mortality and other complications.
CITATIONS: London MJ, Schwartz GG, Hur K, Henderson WG. Association of perioperative statin use with mortality and morbidity after major noncardiac surgery. JAMA Intern Med. 2017 Feb 1;177(2):231-42.
Dr. Dietsche is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Nontraditional med student hopes to bridge common understanding gaps in health care
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
Male vs. female hospitalists, a comparison in mortality and readmission rate for Medicare patients
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Does physician sex affect hospitalized patient outcomes?
BACKGROUND: Previous studies had suggested different practice patterns between male and female physicians in process measure of quality. No prior evaluation of patient outcomes examining those differences was studied in the past.
STUDY DESIGN: Observational, cross-sectional study.
SYNOPSIS: This observational study assessed the difference in patients’ outcomes that were treated by a male or female physician. 30-days mortality rate was analyzed from 1,583,028 hospitalizations. The mortality rate of patients cared for by female physicians was lower and statistically significant: 11.07% vs. 11.49% (adjusted risk difference, –0.43%; 95% CI, –0.57% to –0.28%; P less than .001). The difference did not change after considering patient and physician characteristics as well as when looking at hospital fixed effects (that is, hospital indicators). In order to prevent one death, a female physician needs to treat 233 patients.
Also, 30-day readmission rate, after adjustment readmissions (from 1,540,797 hospitalizations) was 15.02% vs. 15.57% (adjusted risk difference, –0.55%; 95% confidence interval, –0.71% to 0.39%; P less than .001) showing that the care provided by a female physician can reduce one readmission when treating 182 patients.
BOTTOM LINE: Patients older than 65 years have lower 30-day mortality and readmission rates when receiving inpatient care from a female internist, compared with care by a male internist.
CITATIONS: Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med. 2017 Feb;177(2):206-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora.
End-of-rotation resident transition in care and mortality among hospitalized patients
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
CLINICAL QUESTION: Are hospitalized patients experiencing an increased mortality risk at the end-rotation resident transition in care and is this association related to the Accreditation Council for Graduate Medical Education (ACGME) 2011 duty-hour regulations?
BACKGROUND: Prior studies of physicians’ transitions in care were associated with potential adverse patient events and outcomes. A higher mortality risk was suggested among patients with a complex hospital course or prolonged length of stay in association to house-staff transitions of care.
SETTING: 10 University-affiliated U.S. Veterans Health Administration hospitals.
SYNOPSIS: 230,701 patient discharges (mean age, 65.6 years; 95.8% male sex; median length of stay, 3 days) were included. The transition group included patients admitted at any time prior to an end-of-rotation who were either discharged or deceased within 7 days of transition. All other discharges were considered controls.
The primary outcome was in-hospital mortality rate; secondary outcomes included 30-day and 90-day mortality and readmission rates. An absolute increase of 1.5% to 1.9% in a unadjusted in-hospitality risk was found. The 30-day and 90-day mortality odds ratios were 1.10 and 1.21, respectively. A possible stronger association was found among interns’ transitions in care and the in-hospital and after-discharge mortality post-ACGME 2011 duty hour regulations. The latter raises questions about the interns’ inexperience and their amount of shift-to-shift handoffs. An adjusted analysis of the readmission rates at 30-day and 90-day was not significantly different between transition vs. control patients.
BOTTOM LINE: Elevated in-hospital mortality was seen among patients admitted to the inpatient medicine service at the end-of-rotation resident transitions in care. The association was stronger after the duty-hour ACGME (2011) regulations.
CITATIONS: Denson JL, Jensen A, Saag HS, et al. Association between end-of-rotation resident transition in care and mortality among hospitalized patients. JAMA. 2016 Dec 6;316(21):2204-13.
Dr. Orjuela is assistant professor of neurology at the University of Colorado School of Medicine, Aurora
Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: What are the benefits and harms of perioperative pharmacological thromboprophylaxis in cancer patients undergoing surgery?
STUDY DESIGN: Systematic review and meta-analysis.
SYNOPSIS: Thirty-nine trials were deemed eligible for inclusion in the meta-analysis. Twenty-five of these were prospective and 14 were retrospective. The overall incidence of deep venous thrombosis (DVT) and pulmonary embolism was 0.9% (across 20 studies) and 0.3% (across 19 studies), respectively. Pharmacologic prophylaxis overall reduced DVT incidence (0.5% vs. 1.2%; relative risk, 0.51; P = .03). Subgroup analysis demonstrated this was significant for abdominal/pelvic surgeries and with low molecular weight heparin. Six studies compared duration of standard prophylaxis (10 days) with extended prophylaxis (4 weeks), with a lower VTE rate in the extended group. Bleeding events were noted in 13 studies and pharmacologic prophylaxis significantly increased bleeding risk (2.7% vs. 8%; RR, 2.51; P less than .0001).
BOTTOM LINE: Perioperative pharmacologic prophylaxis reduces DVT risk in patients with cancer, with greatest risk reduction seen in patients undergoing abdominal/pelvic surgeries. This comes at the cost of increased bleeding complications.
CITATIONS: Guo Q, Huang B, Zhao J, et al. Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg. 2016 Nov. doi: 10.1097/SLA.0000000000002074.
Dr. Patil is a clinical instructor, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.