User login
What hospitalists must know about co-management
With patient co-management arrangements between hospitalists and other surgical and medical subspecialists becoming more common, HM17 attendees won’t want to miss Tuesday afternoon’s session at 3:15–4:20 p.m., “Redefining Co-management in Hospital Medicine.”
“We’ll provide hospitalists effective co-management programs at their respective hospitals,” said copresenter William Atchley Jr., MD, FACP, SFHM, a hospitalist with Sentara Heart Hospital in Norfolk, Va.
More hospital medicine groups are getting involved in co-management, the presenters said. There are two primary models: one in which the hospitalist is the attending of record and the subspecialist is the co-manager and another in which the subspecialist is the attending of record and the hospitalist serves as the co-manager. “Either model can work with the right agreements put in place,” Dr. Atchley said.
“We’ll go through some of what we feel are the undiscovered benefits of having a co-management service,” said copresenter Mark Goldin, MD, FACP, a hospitalist at Long Island Jewish Medical Center. “I think a lot of people will be interested to hear that because research on co-management has been mixed, up to this point.” For example, he said, SHM engagement surveys have indicated that hospitalists who do co-management may be at reduced risk of burnout.
Also important is creating a metrics dashboard and monitoring and updating it regularly, Dr. Karlin-Zysman added. “Not only does it keep both sides honest, but it’s how you garner support from the C-suite.”
The Society of Hospital Medicine has resources available to help, Dr. Atchley said. The SHM website includes a white paper on co-management. There also is a listserv called HMS Exchange, in which hospitalists can discuss comanagement topics.
“Co-management is not going away. It’s something that hospitalists are going to be involved with,” Dr. Atchley said. “It’s important to come up with the right agreement and, at the same time, work with everybody in collaboration to improve patient care.”
Redefining Co-management in Hospital Medicine
Tuesday, 3:15–4:20 p.m.
With patient co-management arrangements between hospitalists and other surgical and medical subspecialists becoming more common, HM17 attendees won’t want to miss Tuesday afternoon’s session at 3:15–4:20 p.m., “Redefining Co-management in Hospital Medicine.”
“We’ll provide hospitalists effective co-management programs at their respective hospitals,” said copresenter William Atchley Jr., MD, FACP, SFHM, a hospitalist with Sentara Heart Hospital in Norfolk, Va.
More hospital medicine groups are getting involved in co-management, the presenters said. There are two primary models: one in which the hospitalist is the attending of record and the subspecialist is the co-manager and another in which the subspecialist is the attending of record and the hospitalist serves as the co-manager. “Either model can work with the right agreements put in place,” Dr. Atchley said.
“We’ll go through some of what we feel are the undiscovered benefits of having a co-management service,” said copresenter Mark Goldin, MD, FACP, a hospitalist at Long Island Jewish Medical Center. “I think a lot of people will be interested to hear that because research on co-management has been mixed, up to this point.” For example, he said, SHM engagement surveys have indicated that hospitalists who do co-management may be at reduced risk of burnout.
Also important is creating a metrics dashboard and monitoring and updating it regularly, Dr. Karlin-Zysman added. “Not only does it keep both sides honest, but it’s how you garner support from the C-suite.”
The Society of Hospital Medicine has resources available to help, Dr. Atchley said. The SHM website includes a white paper on co-management. There also is a listserv called HMS Exchange, in which hospitalists can discuss comanagement topics.
“Co-management is not going away. It’s something that hospitalists are going to be involved with,” Dr. Atchley said. “It’s important to come up with the right agreement and, at the same time, work with everybody in collaboration to improve patient care.”
Redefining Co-management in Hospital Medicine
Tuesday, 3:15–4:20 p.m.
With patient co-management arrangements between hospitalists and other surgical and medical subspecialists becoming more common, HM17 attendees won’t want to miss Tuesday afternoon’s session at 3:15–4:20 p.m., “Redefining Co-management in Hospital Medicine.”
“We’ll provide hospitalists effective co-management programs at their respective hospitals,” said copresenter William Atchley Jr., MD, FACP, SFHM, a hospitalist with Sentara Heart Hospital in Norfolk, Va.
More hospital medicine groups are getting involved in co-management, the presenters said. There are two primary models: one in which the hospitalist is the attending of record and the subspecialist is the co-manager and another in which the subspecialist is the attending of record and the hospitalist serves as the co-manager. “Either model can work with the right agreements put in place,” Dr. Atchley said.
“We’ll go through some of what we feel are the undiscovered benefits of having a co-management service,” said copresenter Mark Goldin, MD, FACP, a hospitalist at Long Island Jewish Medical Center. “I think a lot of people will be interested to hear that because research on co-management has been mixed, up to this point.” For example, he said, SHM engagement surveys have indicated that hospitalists who do co-management may be at reduced risk of burnout.
Also important is creating a metrics dashboard and monitoring and updating it regularly, Dr. Karlin-Zysman added. “Not only does it keep both sides honest, but it’s how you garner support from the C-suite.”
The Society of Hospital Medicine has resources available to help, Dr. Atchley said. The SHM website includes a white paper on co-management. There also is a listserv called HMS Exchange, in which hospitalists can discuss comanagement topics.
“Co-management is not going away. It’s something that hospitalists are going to be involved with,” Dr. Atchley said. “It’s important to come up with the right agreement and, at the same time, work with everybody in collaboration to improve patient care.”
Redefining Co-management in Hospital Medicine
Tuesday, 3:15–4:20 p.m.
Hospitalist movers and shakers
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Here’s what’s trending at SHM
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
Decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation
Clinical question: This work group synthesized available data to address whether and when anticoagulant therapy should be interrupted, whether and how anticoagulant bridging with a parenteral agent should be performed, and when and how anticoagulant therapy should be restarted for those who require temporary interruption.
Background: Atrial fibrillation is the most common sustained arrhythmia worldwide. Antithrombotic therapy, with a strong preference to oral anticoagulant (vitamin K antagonists [VKA] or Direct oral anticoagulant [DOAC]) over antiplatelet, is recommended for patients with high thrombotic risk. Temporary interruption is frequently necessary to mitigate bleed risk with surgical or invasive procedures. Although several factors go into the decision to interrupt anticoagulation, practice varies widely.
Study design: Data review and commentary.
Setting: Veterans’ Affairs Hospitals.
For the assessment of patient-related bleed risk, consider the HAS-BLED (Hypertension, Abnormal Renal and Liver Function, Stroke–Bleeding, Labile INRs, Elderly, Drugs or Alcohol) score: bleeding in the preceding 3 months, bleeding with a similar procedure or prior bridging, abnormalities of platelet function, concomitant use of antiplatelet therapy, and/or supratherapeutic international normalized ratio.
Vitamin K Antagonists:
- Do not interrupt for no clinically important or low bleed risk AND absence of patient-related bleed risk factor(s).
- Interrupt for procedures with intermediate or high bleed risk OR procedures with uncertain bleed risk and the presence of patient-related bleed risk factor(s).
- Consider interruption for procedure with no clinically important or low bleed risk AND the presence of patient-related bleed risk factor(s) OR procedures with uncertain bleed risk AND the absence of patient-related bleed risk factor(s).
Direct Oral Anticoagulants:
Can interrupt therapy for all bleed risks; duration based on creatinine clearance.
A procedure performed at the trough level may allow reinitiation the evening of or the day after the procedure with 1 or fewer dose(s) missed.
Bottom line: VKAs should be held based on surgical and patient bleed risk factors. Guidelines provide tools to calculate and consider. DOACs can always be held, preferably at trough times to minimize interruptions and for durations based on creatinine clearance.
Citation: Doherty JU, Gluckman TJ, Hucker WJ, et al. “2017 ACC Expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation.” J Am Coll Cardiol. 2017 Feb 21;69(7):871-98.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
Clinical question: This work group synthesized available data to address whether and when anticoagulant therapy should be interrupted, whether and how anticoagulant bridging with a parenteral agent should be performed, and when and how anticoagulant therapy should be restarted for those who require temporary interruption.
Background: Atrial fibrillation is the most common sustained arrhythmia worldwide. Antithrombotic therapy, with a strong preference to oral anticoagulant (vitamin K antagonists [VKA] or Direct oral anticoagulant [DOAC]) over antiplatelet, is recommended for patients with high thrombotic risk. Temporary interruption is frequently necessary to mitigate bleed risk with surgical or invasive procedures. Although several factors go into the decision to interrupt anticoagulation, practice varies widely.
Study design: Data review and commentary.
Setting: Veterans’ Affairs Hospitals.
For the assessment of patient-related bleed risk, consider the HAS-BLED (Hypertension, Abnormal Renal and Liver Function, Stroke–Bleeding, Labile INRs, Elderly, Drugs or Alcohol) score: bleeding in the preceding 3 months, bleeding with a similar procedure or prior bridging, abnormalities of platelet function, concomitant use of antiplatelet therapy, and/or supratherapeutic international normalized ratio.
Vitamin K Antagonists:
- Do not interrupt for no clinically important or low bleed risk AND absence of patient-related bleed risk factor(s).
- Interrupt for procedures with intermediate or high bleed risk OR procedures with uncertain bleed risk and the presence of patient-related bleed risk factor(s).
- Consider interruption for procedure with no clinically important or low bleed risk AND the presence of patient-related bleed risk factor(s) OR procedures with uncertain bleed risk AND the absence of patient-related bleed risk factor(s).
Direct Oral Anticoagulants:
Can interrupt therapy for all bleed risks; duration based on creatinine clearance.
A procedure performed at the trough level may allow reinitiation the evening of or the day after the procedure with 1 or fewer dose(s) missed.
Bottom line: VKAs should be held based on surgical and patient bleed risk factors. Guidelines provide tools to calculate and consider. DOACs can always be held, preferably at trough times to minimize interruptions and for durations based on creatinine clearance.
Citation: Doherty JU, Gluckman TJ, Hucker WJ, et al. “2017 ACC Expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation.” J Am Coll Cardiol. 2017 Feb 21;69(7):871-98.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
Clinical question: This work group synthesized available data to address whether and when anticoagulant therapy should be interrupted, whether and how anticoagulant bridging with a parenteral agent should be performed, and when and how anticoagulant therapy should be restarted for those who require temporary interruption.
Background: Atrial fibrillation is the most common sustained arrhythmia worldwide. Antithrombotic therapy, with a strong preference to oral anticoagulant (vitamin K antagonists [VKA] or Direct oral anticoagulant [DOAC]) over antiplatelet, is recommended for patients with high thrombotic risk. Temporary interruption is frequently necessary to mitigate bleed risk with surgical or invasive procedures. Although several factors go into the decision to interrupt anticoagulation, practice varies widely.
Study design: Data review and commentary.
Setting: Veterans’ Affairs Hospitals.
For the assessment of patient-related bleed risk, consider the HAS-BLED (Hypertension, Abnormal Renal and Liver Function, Stroke–Bleeding, Labile INRs, Elderly, Drugs or Alcohol) score: bleeding in the preceding 3 months, bleeding with a similar procedure or prior bridging, abnormalities of platelet function, concomitant use of antiplatelet therapy, and/or supratherapeutic international normalized ratio.
Vitamin K Antagonists:
- Do not interrupt for no clinically important or low bleed risk AND absence of patient-related bleed risk factor(s).
- Interrupt for procedures with intermediate or high bleed risk OR procedures with uncertain bleed risk and the presence of patient-related bleed risk factor(s).
- Consider interruption for procedure with no clinically important or low bleed risk AND the presence of patient-related bleed risk factor(s) OR procedures with uncertain bleed risk AND the absence of patient-related bleed risk factor(s).
Direct Oral Anticoagulants:
Can interrupt therapy for all bleed risks; duration based on creatinine clearance.
A procedure performed at the trough level may allow reinitiation the evening of or the day after the procedure with 1 or fewer dose(s) missed.
Bottom line: VKAs should be held based on surgical and patient bleed risk factors. Guidelines provide tools to calculate and consider. DOACs can always be held, preferably at trough times to minimize interruptions and for durations based on creatinine clearance.
Citation: Doherty JU, Gluckman TJ, Hucker WJ, et al. “2017 ACC Expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation.” J Am Coll Cardiol. 2017 Feb 21;69(7):871-98.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
HM17 satellite symposia schedule, information
Patient Care Transitions in COPD: Improving Collaboration Between Inpatient and Outpatient Providers to Reduce Readmissions
Monday, May 1
5–7 p.m., Mandalay Bay J
Dinner at 5 p.m.
Overview: The faculty panel will be composed of leading experts representing hospital medicine and pulmonary specialties. For detailed faculty information please visit www.practitionersedge.com/shmcopd.
Integrity Continuing Education Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Integrity Continuing Education designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Register: www.practitionersedge.com/shmcopd.
Alcoholic Hepatitis: Advances in Therapeutic Management
Monday, May 1
5:30–7:30 p.m., Jasmine CDGH
Dinner at 5:30 p.m.
Overview: Because alcohol potentiates the fibrosis- and cancer-inducing actions of the hepatitis virus, people with heavy alcohol intake are particularly vulnerable to hepatitis infection and are most in need of treatment. In this activity, we will discuss advances in acute and long-term management of alcoholic hepatitis and liver function. Specifically, we will aim to review guideline-based screening and diagnostic considerations for alcoholic hepatitis; assess standards of care for management of acute alcoholic hepatitis, including lifestyle-, pharmacologic-, and device-related methods; and evaluate investigational methods of treatment with respect to efficacy, safety, and long-term management.
Presenters: Ram Mohan Subramanian, MD, associate professor of medicine and surgery, medical director of liver transplant, Emory University, Atlanta; Julie Thompson, MD, MPH, assistant professor of medicine, division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis.
This activity has been approved for AMA PRA Category 1 Credit(s)™. Full accreditation information available: www.akhcme.com/SHM. This activity is supported by an educational grant from Vital Therapies, Inc. Register: https://akhinc.formstack.com/forms/shm.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Tuesday, May 2
Noon–1 p.m., Oceanside G
Overview: This course educates on the dangers of lawsuits in the healthcare community. Focused primarily toward physicians and how they should be structured to protect themselves.
Presenter: Art McOmber business owner, retired FBI Agent.
Sponsored by Legally Mine.
A Master Class in Understanding & Applying Updated Treatment Guidelines and Scientific Advances to Reduce Mortality and Hospitalizations in Chronic Heart Failure Patients
Tuesday, May 2
7:30–9:30 p.m., Breakers ABGH
Dinner at 7 p.m.
Presenters: Alpesh Amin, MD, MBA, MACP, SFHM, University of California Irvine, California; Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas.
This CME activity is jointly provided by Medical Learning Institute and PVI, PeerView Institute for Medical Education. This activity is accredited by the ACCME to provide continuing medical education for physicians.
The Medical Learning Institute designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credits™. This activity is supported by educational grants from Novartis Pharmaceuticals Corporation and ZS Pharma, a member of the AstraZeneca Group. Register: www.peerviewpress.com/CHF2017.
Assessing VTE Risk in Medically Ill Patients: The Critical Role of the Hospitalist
Tuesday, May 2
7:30–9:30 p.m., Jasmine CDGH
Dinner at 7 p.m.
Presenters: Ebrahim Barkoudah, MD, MPH, instructor in medicine, associate director, global clinical scholars research training program, office of global education, Harvard Medical School, associate director, hospital medicine unit, department of medicine, Brigham and Women’s Hospital (BWH), Boston; Elaine M. Hylek, MD, MPH, professor of medicine, Boston University School of Medicine, director, thrombosis and anticoagulation service, Boston Medical Center; Aaron P. Kithcart, MD, PhD, vascular medicine fellow, BWH; John Fanikos, RPh, MBA, assistant professor of clinical pharmacy practice at Northeastern University, Massachusetts College of Pharmacy, director of pharmacy business and financial services, BWH; Arman Qamar, MD, vascular medicine and cardiology fellow, BWH.
This activity is held in conjunction with the North American Thrombosis Forum and with HM17.
Medscape LLC is accredited by the American Nurses Credentialing Center (ANCC), the Accreditation Council for Pharmacy Education (ACPE), and the Accreditation Council for Continuing Medical Education (ACCME), to provide continuing education for the health care team. Medscape LLC designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This activity is supported by an independent educational grant from Portola Pharmaceuticals. Register: www.medscape.org/townhall/vte-risk.
Understanding and Managing Hyponatremia: Key Information for Today’s Hospitalist
Wednesday, May 3
7:30 - 9:30 p.m., Jasmine CDGH
Dinner at 7:30 p.m.
Presenters: Jeffrey S. Shapiro, MD, regional medical director and hospitalist, Southern California Hospitalist Network, Anaheim; Alpesh N. Amin, MD, MBA, MACP, SFHM, FACC, Thomas and Mary Cesario chair, Department of Medicine, professor of medicine, business, public health, nursing science, and biomedical engineering, executive director, hospitalist program, University of California, Irvine; Mohammed S. Ahmed, DO, CSH, FASN, associate professor, Department of Internal Medicine, Midwestern University, Chicago College of Osteopathic Medicine
Sponsored by Otsuka Pharmaceuticals.
Patient Care Transitions in COPD: Improving Collaboration Between Inpatient and Outpatient Providers to Reduce Readmissions
Monday, May 1
5–7 p.m., Mandalay Bay J
Dinner at 5 p.m.
Overview: The faculty panel will be composed of leading experts representing hospital medicine and pulmonary specialties. For detailed faculty information please visit www.practitionersedge.com/shmcopd.
Integrity Continuing Education Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Integrity Continuing Education designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Register: www.practitionersedge.com/shmcopd.
Alcoholic Hepatitis: Advances in Therapeutic Management
Monday, May 1
5:30–7:30 p.m., Jasmine CDGH
Dinner at 5:30 p.m.
Overview: Because alcohol potentiates the fibrosis- and cancer-inducing actions of the hepatitis virus, people with heavy alcohol intake are particularly vulnerable to hepatitis infection and are most in need of treatment. In this activity, we will discuss advances in acute and long-term management of alcoholic hepatitis and liver function. Specifically, we will aim to review guideline-based screening and diagnostic considerations for alcoholic hepatitis; assess standards of care for management of acute alcoholic hepatitis, including lifestyle-, pharmacologic-, and device-related methods; and evaluate investigational methods of treatment with respect to efficacy, safety, and long-term management.
Presenters: Ram Mohan Subramanian, MD, associate professor of medicine and surgery, medical director of liver transplant, Emory University, Atlanta; Julie Thompson, MD, MPH, assistant professor of medicine, division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis.
This activity has been approved for AMA PRA Category 1 Credit(s)™. Full accreditation information available: www.akhcme.com/SHM. This activity is supported by an educational grant from Vital Therapies, Inc. Register: https://akhinc.formstack.com/forms/shm.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Tuesday, May 2
Noon–1 p.m., Oceanside G
Overview: This course educates on the dangers of lawsuits in the healthcare community. Focused primarily toward physicians and how they should be structured to protect themselves.
Presenter: Art McOmber business owner, retired FBI Agent.
Sponsored by Legally Mine.
A Master Class in Understanding & Applying Updated Treatment Guidelines and Scientific Advances to Reduce Mortality and Hospitalizations in Chronic Heart Failure Patients
Tuesday, May 2
7:30–9:30 p.m., Breakers ABGH
Dinner at 7 p.m.
Presenters: Alpesh Amin, MD, MBA, MACP, SFHM, University of California Irvine, California; Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas.
This CME activity is jointly provided by Medical Learning Institute and PVI, PeerView Institute for Medical Education. This activity is accredited by the ACCME to provide continuing medical education for physicians.
The Medical Learning Institute designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credits™. This activity is supported by educational grants from Novartis Pharmaceuticals Corporation and ZS Pharma, a member of the AstraZeneca Group. Register: www.peerviewpress.com/CHF2017.
Assessing VTE Risk in Medically Ill Patients: The Critical Role of the Hospitalist
Tuesday, May 2
7:30–9:30 p.m., Jasmine CDGH
Dinner at 7 p.m.
Presenters: Ebrahim Barkoudah, MD, MPH, instructor in medicine, associate director, global clinical scholars research training program, office of global education, Harvard Medical School, associate director, hospital medicine unit, department of medicine, Brigham and Women’s Hospital (BWH), Boston; Elaine M. Hylek, MD, MPH, professor of medicine, Boston University School of Medicine, director, thrombosis and anticoagulation service, Boston Medical Center; Aaron P. Kithcart, MD, PhD, vascular medicine fellow, BWH; John Fanikos, RPh, MBA, assistant professor of clinical pharmacy practice at Northeastern University, Massachusetts College of Pharmacy, director of pharmacy business and financial services, BWH; Arman Qamar, MD, vascular medicine and cardiology fellow, BWH.
This activity is held in conjunction with the North American Thrombosis Forum and with HM17.
Medscape LLC is accredited by the American Nurses Credentialing Center (ANCC), the Accreditation Council for Pharmacy Education (ACPE), and the Accreditation Council for Continuing Medical Education (ACCME), to provide continuing education for the health care team. Medscape LLC designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This activity is supported by an independent educational grant from Portola Pharmaceuticals. Register: www.medscape.org/townhall/vte-risk.
Understanding and Managing Hyponatremia: Key Information for Today’s Hospitalist
Wednesday, May 3
7:30 - 9:30 p.m., Jasmine CDGH
Dinner at 7:30 p.m.
Presenters: Jeffrey S. Shapiro, MD, regional medical director and hospitalist, Southern California Hospitalist Network, Anaheim; Alpesh N. Amin, MD, MBA, MACP, SFHM, FACC, Thomas and Mary Cesario chair, Department of Medicine, professor of medicine, business, public health, nursing science, and biomedical engineering, executive director, hospitalist program, University of California, Irvine; Mohammed S. Ahmed, DO, CSH, FASN, associate professor, Department of Internal Medicine, Midwestern University, Chicago College of Osteopathic Medicine
Sponsored by Otsuka Pharmaceuticals.
Patient Care Transitions in COPD: Improving Collaboration Between Inpatient and Outpatient Providers to Reduce Readmissions
Monday, May 1
5–7 p.m., Mandalay Bay J
Dinner at 5 p.m.
Overview: The faculty panel will be composed of leading experts representing hospital medicine and pulmonary specialties. For detailed faculty information please visit www.practitionersedge.com/shmcopd.
Integrity Continuing Education Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Integrity Continuing Education designates this live activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Register: www.practitionersedge.com/shmcopd.
Alcoholic Hepatitis: Advances in Therapeutic Management
Monday, May 1
5:30–7:30 p.m., Jasmine CDGH
Dinner at 5:30 p.m.
Overview: Because alcohol potentiates the fibrosis- and cancer-inducing actions of the hepatitis virus, people with heavy alcohol intake are particularly vulnerable to hepatitis infection and are most in need of treatment. In this activity, we will discuss advances in acute and long-term management of alcoholic hepatitis and liver function. Specifically, we will aim to review guideline-based screening and diagnostic considerations for alcoholic hepatitis; assess standards of care for management of acute alcoholic hepatitis, including lifestyle-, pharmacologic-, and device-related methods; and evaluate investigational methods of treatment with respect to efficacy, safety, and long-term management.
Presenters: Ram Mohan Subramanian, MD, associate professor of medicine and surgery, medical director of liver transplant, Emory University, Atlanta; Julie Thompson, MD, MPH, assistant professor of medicine, division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis.
This activity has been approved for AMA PRA Category 1 Credit(s)™. Full accreditation information available: www.akhcme.com/SHM. This activity is supported by an educational grant from Vital Therapies, Inc. Register: https://akhinc.formstack.com/forms/shm.
A Physician’s Keys to Locking Out Lawsuits and Reducing Taxes
Tuesday, May 2
Noon–1 p.m., Oceanside G
Overview: This course educates on the dangers of lawsuits in the healthcare community. Focused primarily toward physicians and how they should be structured to protect themselves.
Presenter: Art McOmber business owner, retired FBI Agent.
Sponsored by Legally Mine.
A Master Class in Understanding & Applying Updated Treatment Guidelines and Scientific Advances to Reduce Mortality and Hospitalizations in Chronic Heart Failure Patients
Tuesday, May 2
7:30–9:30 p.m., Breakers ABGH
Dinner at 7 p.m.
Presenters: Alpesh Amin, MD, MBA, MACP, SFHM, University of California Irvine, California; Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas.
This CME activity is jointly provided by Medical Learning Institute and PVI, PeerView Institute for Medical Education. This activity is accredited by the ACCME to provide continuing medical education for physicians.
The Medical Learning Institute designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credits™. This activity is supported by educational grants from Novartis Pharmaceuticals Corporation and ZS Pharma, a member of the AstraZeneca Group. Register: www.peerviewpress.com/CHF2017.
Assessing VTE Risk in Medically Ill Patients: The Critical Role of the Hospitalist
Tuesday, May 2
7:30–9:30 p.m., Jasmine CDGH
Dinner at 7 p.m.
Presenters: Ebrahim Barkoudah, MD, MPH, instructor in medicine, associate director, global clinical scholars research training program, office of global education, Harvard Medical School, associate director, hospital medicine unit, department of medicine, Brigham and Women’s Hospital (BWH), Boston; Elaine M. Hylek, MD, MPH, professor of medicine, Boston University School of Medicine, director, thrombosis and anticoagulation service, Boston Medical Center; Aaron P. Kithcart, MD, PhD, vascular medicine fellow, BWH; John Fanikos, RPh, MBA, assistant professor of clinical pharmacy practice at Northeastern University, Massachusetts College of Pharmacy, director of pharmacy business and financial services, BWH; Arman Qamar, MD, vascular medicine and cardiology fellow, BWH.
This activity is held in conjunction with the North American Thrombosis Forum and with HM17.
Medscape LLC is accredited by the American Nurses Credentialing Center (ANCC), the Accreditation Council for Pharmacy Education (ACPE), and the Accreditation Council for Continuing Medical Education (ACCME), to provide continuing education for the health care team. Medscape LLC designates this live activity for a maximum of 2.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This activity is supported by an independent educational grant from Portola Pharmaceuticals. Register: www.medscape.org/townhall/vte-risk.
Understanding and Managing Hyponatremia: Key Information for Today’s Hospitalist
Wednesday, May 3
7:30 - 9:30 p.m., Jasmine CDGH
Dinner at 7:30 p.m.
Presenters: Jeffrey S. Shapiro, MD, regional medical director and hospitalist, Southern California Hospitalist Network, Anaheim; Alpesh N. Amin, MD, MBA, MACP, SFHM, FACC, Thomas and Mary Cesario chair, Department of Medicine, professor of medicine, business, public health, nursing science, and biomedical engineering, executive director, hospitalist program, University of California, Irvine; Mohammed S. Ahmed, DO, CSH, FASN, associate professor, Department of Internal Medicine, Midwestern University, Chicago College of Osteopathic Medicine
Sponsored by Otsuka Pharmaceuticals.
Bezlotoxumab for prevention of recurrent Clostridium difficile infection
Clinical question: Does administration of monoclonal antibodies to C. difficile toxins A and B, in addition to standard-of-care antibiotics, prevent recurrent infection?
Background: Currently, no therapy has been approved to prevent recurrent C. difficile infection. A new approach to the prevention of recurrent C. difficile infection is the administration of monoclonal antibodies against C. difficile toxins (in addition to antibiotic therapy) as a form of passive immunity. Actoxumab and bezlotoxumab are fully human monoclonal antibodies that bind and neutralize C. difficile toxins A and B, respectively. In humans, the level of circulating antibodies against toxin A or toxin B has been correlated with protection against primary and recurrent C. difficile infection.
Study design: Two (MODIFY [MK-6072 and MK-3415A in Participants Receiving Antibiotic Therapy for Clostridium Difficile Infection] I and MODIFY II) double-blind, randomized, placebo-controlled, phase III trials.
Setting: 322 sites (~68% inpatient) in 30 countries from Nov. 1, 2011, through May 22, 2015.
Synopsis: Trials pooled data from 2,174 adults who were receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infections. Participants received an infusion of either bezlotoxumab, actoxumab plus bezlotoxumab, or placebo for MODIFY II; actoxumab alone was also given in MODIFY I. The primary endpoint was recurrent infection within 12 weeks.
The rate of recurrent C. difficile infection was significantly lower with bezlotoxumab alone than with placebo (MODIFY I: 17% vs. 28%; 95% CI, −15.9 to −4.3; P less than .001; MODIFY II: 16% vs. 26%; 95% CI, −15.5 to −4.3; P less than .001) and was significantly lower with actoxumab plus bezlotoxumab than with placebo (MODIFY I: 16% vs. 28%; 95% CI, −17.4 to −5.9; P less than .001; MODIFY II: 15% vs. 26%; 95% CI, −16.4 to −5.1; P less than .001).
The serious adverse events were similar with most groups, the exception being actoxumab alone. Given the higher rate of recurrent infection and deaths in the actoxumab group from interim analysis, the enrollment was discontinued in MODIFY I.
Investigators did admit that safety assessments were limited because of the relatively small number of patients who received bezlotoxumab, making it difficult to detect potentially serious but low-frequency toxic effects.
Bottom line: In patients receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infection, a single intravenous infusion of bezlotoxumab was associated with a significantly lower rate of recurrent infection than placebo and had a safety profile similar to that of placebo.
Citation: Wilcox MH, Gerding DN, Poxton IR, et al. “Bezlotoxumab for prevention of recurrent Clostridium difficile infection.” N Engl J Med. 2017 Jan 26;376(4):305-17.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
Clinical question: Does administration of monoclonal antibodies to C. difficile toxins A and B, in addition to standard-of-care antibiotics, prevent recurrent infection?
Background: Currently, no therapy has been approved to prevent recurrent C. difficile infection. A new approach to the prevention of recurrent C. difficile infection is the administration of monoclonal antibodies against C. difficile toxins (in addition to antibiotic therapy) as a form of passive immunity. Actoxumab and bezlotoxumab are fully human monoclonal antibodies that bind and neutralize C. difficile toxins A and B, respectively. In humans, the level of circulating antibodies against toxin A or toxin B has been correlated with protection against primary and recurrent C. difficile infection.
Study design: Two (MODIFY [MK-6072 and MK-3415A in Participants Receiving Antibiotic Therapy for Clostridium Difficile Infection] I and MODIFY II) double-blind, randomized, placebo-controlled, phase III trials.
Setting: 322 sites (~68% inpatient) in 30 countries from Nov. 1, 2011, through May 22, 2015.
Synopsis: Trials pooled data from 2,174 adults who were receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infections. Participants received an infusion of either bezlotoxumab, actoxumab plus bezlotoxumab, or placebo for MODIFY II; actoxumab alone was also given in MODIFY I. The primary endpoint was recurrent infection within 12 weeks.
The rate of recurrent C. difficile infection was significantly lower with bezlotoxumab alone than with placebo (MODIFY I: 17% vs. 28%; 95% CI, −15.9 to −4.3; P less than .001; MODIFY II: 16% vs. 26%; 95% CI, −15.5 to −4.3; P less than .001) and was significantly lower with actoxumab plus bezlotoxumab than with placebo (MODIFY I: 16% vs. 28%; 95% CI, −17.4 to −5.9; P less than .001; MODIFY II: 15% vs. 26%; 95% CI, −16.4 to −5.1; P less than .001).
The serious adverse events were similar with most groups, the exception being actoxumab alone. Given the higher rate of recurrent infection and deaths in the actoxumab group from interim analysis, the enrollment was discontinued in MODIFY I.
Investigators did admit that safety assessments were limited because of the relatively small number of patients who received bezlotoxumab, making it difficult to detect potentially serious but low-frequency toxic effects.
Bottom line: In patients receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infection, a single intravenous infusion of bezlotoxumab was associated with a significantly lower rate of recurrent infection than placebo and had a safety profile similar to that of placebo.
Citation: Wilcox MH, Gerding DN, Poxton IR, et al. “Bezlotoxumab for prevention of recurrent Clostridium difficile infection.” N Engl J Med. 2017 Jan 26;376(4):305-17.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
Clinical question: Does administration of monoclonal antibodies to C. difficile toxins A and B, in addition to standard-of-care antibiotics, prevent recurrent infection?
Background: Currently, no therapy has been approved to prevent recurrent C. difficile infection. A new approach to the prevention of recurrent C. difficile infection is the administration of monoclonal antibodies against C. difficile toxins (in addition to antibiotic therapy) as a form of passive immunity. Actoxumab and bezlotoxumab are fully human monoclonal antibodies that bind and neutralize C. difficile toxins A and B, respectively. In humans, the level of circulating antibodies against toxin A or toxin B has been correlated with protection against primary and recurrent C. difficile infection.
Study design: Two (MODIFY [MK-6072 and MK-3415A in Participants Receiving Antibiotic Therapy for Clostridium Difficile Infection] I and MODIFY II) double-blind, randomized, placebo-controlled, phase III trials.
Setting: 322 sites (~68% inpatient) in 30 countries from Nov. 1, 2011, through May 22, 2015.
Synopsis: Trials pooled data from 2,174 adults who were receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infections. Participants received an infusion of either bezlotoxumab, actoxumab plus bezlotoxumab, or placebo for MODIFY II; actoxumab alone was also given in MODIFY I. The primary endpoint was recurrent infection within 12 weeks.
The rate of recurrent C. difficile infection was significantly lower with bezlotoxumab alone than with placebo (MODIFY I: 17% vs. 28%; 95% CI, −15.9 to −4.3; P less than .001; MODIFY II: 16% vs. 26%; 95% CI, −15.5 to −4.3; P less than .001) and was significantly lower with actoxumab plus bezlotoxumab than with placebo (MODIFY I: 16% vs. 28%; 95% CI, −17.4 to −5.9; P less than .001; MODIFY II: 15% vs. 26%; 95% CI, −16.4 to −5.1; P less than .001).
The serious adverse events were similar with most groups, the exception being actoxumab alone. Given the higher rate of recurrent infection and deaths in the actoxumab group from interim analysis, the enrollment was discontinued in MODIFY I.
Investigators did admit that safety assessments were limited because of the relatively small number of patients who received bezlotoxumab, making it difficult to detect potentially serious but low-frequency toxic effects.
Bottom line: In patients receiving oral standard-of-care antibiotics for primary or recurrent C. difficile infection, a single intravenous infusion of bezlotoxumab was associated with a significantly lower rate of recurrent infection than placebo and had a safety profile similar to that of placebo.
Citation: Wilcox MH, Gerding DN, Poxton IR, et al. “Bezlotoxumab for prevention of recurrent Clostridium difficile infection.” N Engl J Med. 2017 Jan 26;376(4):305-17.
Dr. White is an instructor in the Division of Hospital Medicine, Loyola University Chicago.
Hospitalists: Leading health care innovation
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
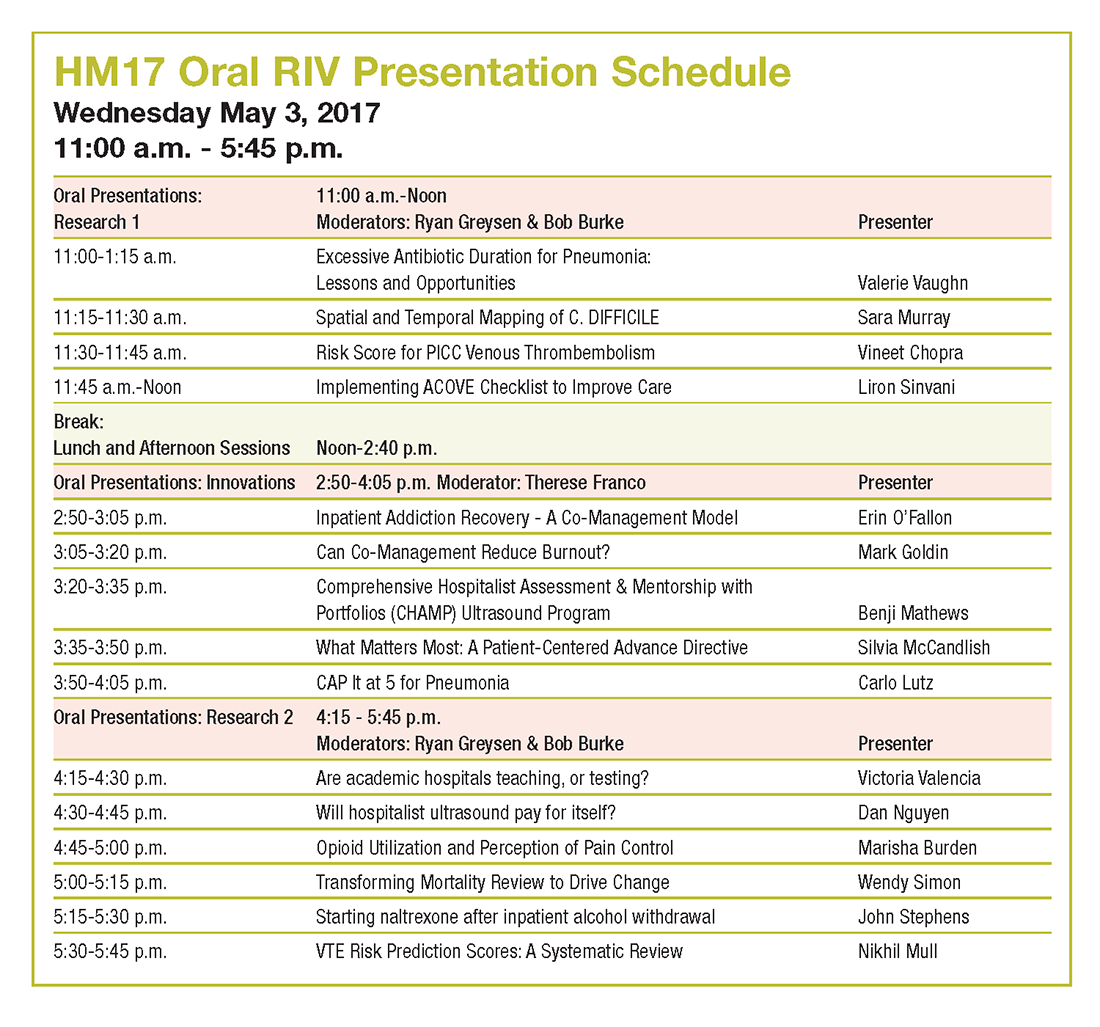
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
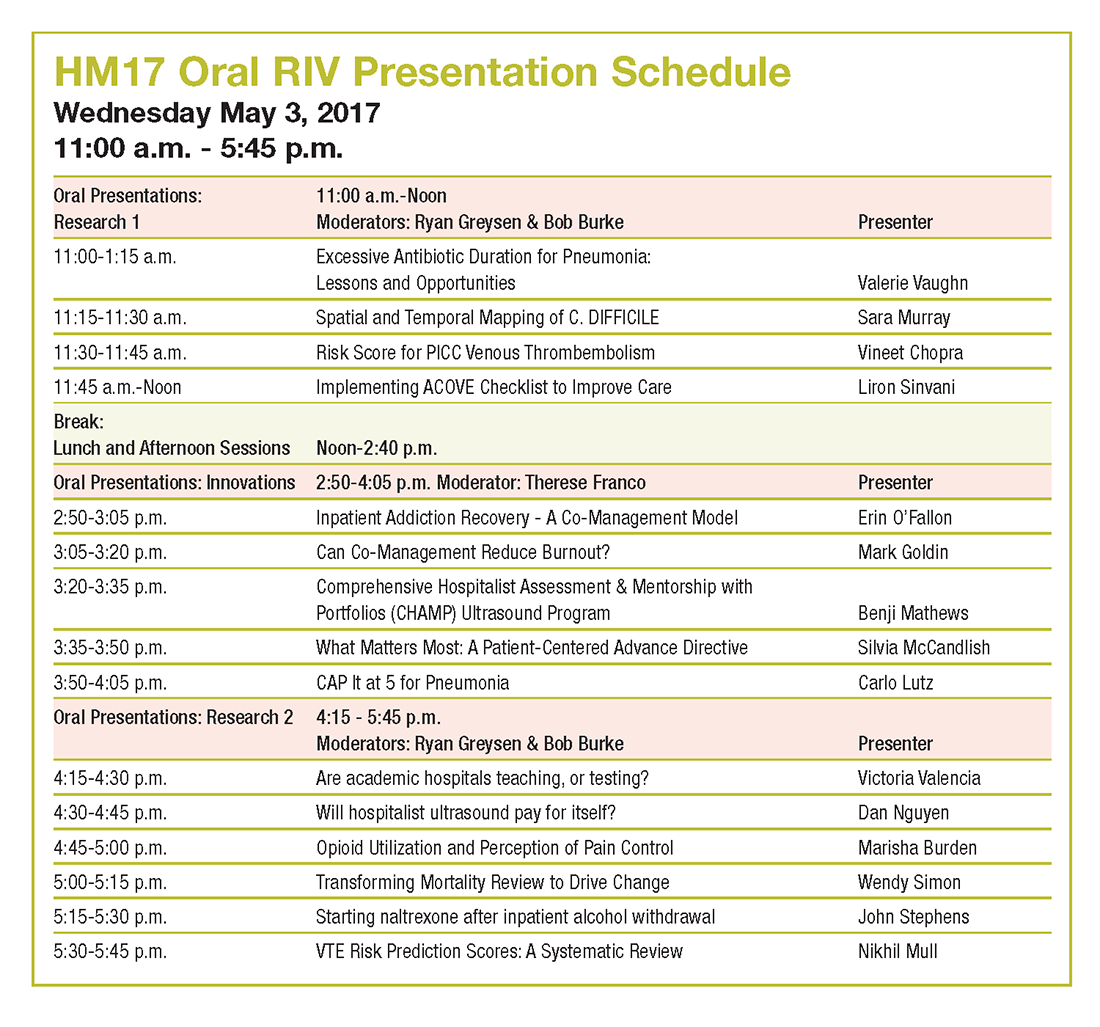
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
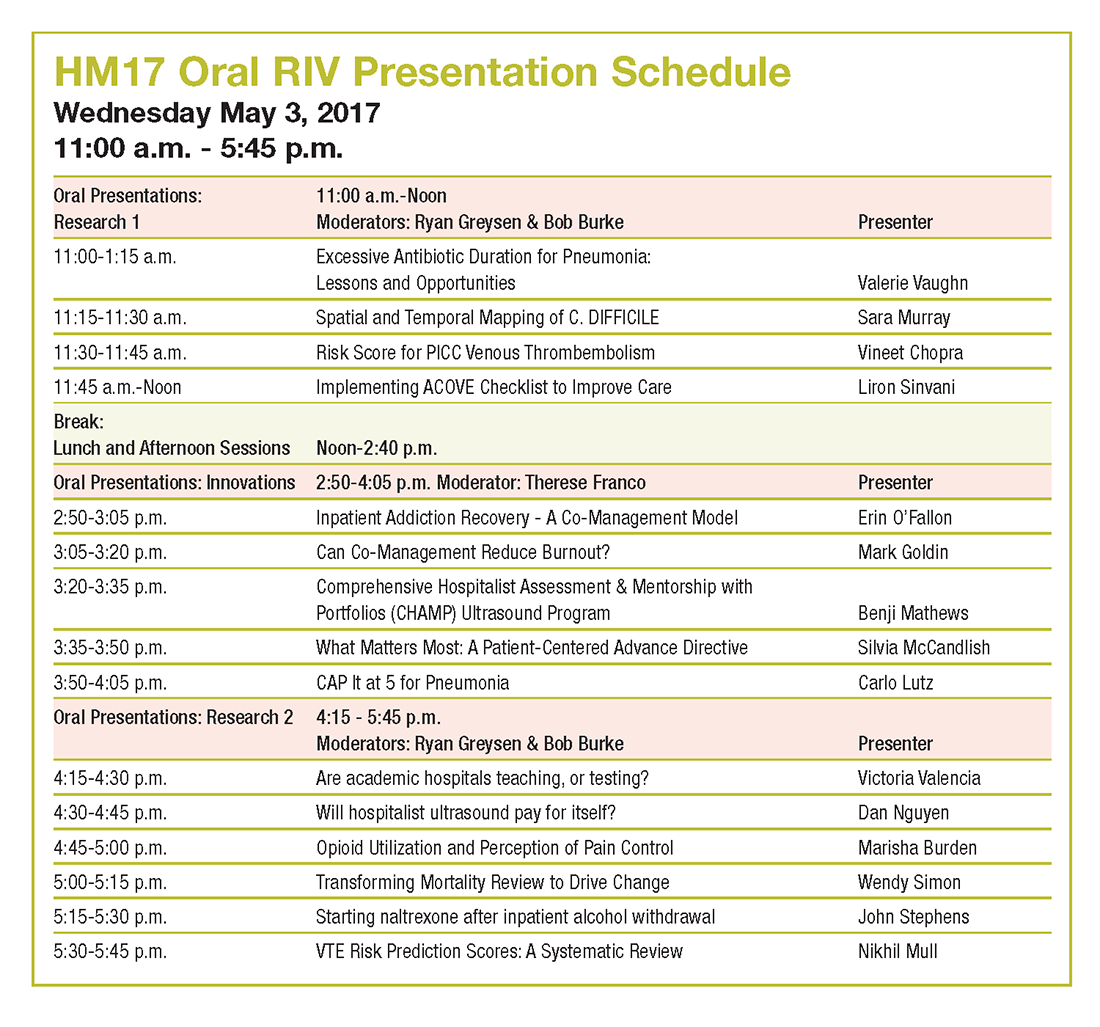
What drives readmissions within 90 days after MI hospitalization
WASHINGTON – In a large population of Medicare patients hospitalized for acute MI, four factors stood out as predictors of increased likelihood of readmission within 90 days, Aaron D. Kugelmass, MD, reported at the annual meeting of the American College of Cardiology.
These four predictors of 90-day readmission were end-stage renal disease at the time of the initial admission for MI, which in a logistic regression model was independently associated with an 88% relative increase in readmission risk; no percutaneous coronary intervention (PCI) during the index hospitalization, which carried a 64% increase in risk; type 1 diabetes, with a 57% increased readmission rate; and heart failure at the initial hospitalization, with an associated 34% greater risk, according to Dr. Kugelmass, chief of cardiology and medical director of the heart and vascular center at Baystate Medical Center in Springfield, Mass.
“This is going to be a learning curve for everyone,” he said.
“The best way to deal with this change is to understand the factors driving costs and morbidity and mortality,” Dr. Kugelmass said, in explaining why he conducted a retrospective study of readmissions within 90 days in a population of 143,286 Medicare beneficiaries hospitalized for acute MI in 2014. The study focus was on readmissions because they add so much to total cost of care for a 90-day episode.
Twenty-eight percent of patients were readmitted at least once within 90 days of discharge following their acute MI. The Medicare bundled payment plan divides MI patients into two separate groups: those who undergo PCI during their initial hospitalization and those who receive medical management only. Thirty-one percent of the readmitted patients in Dr. Kugelmass’s study had undergone PCI during their index hospitalization, while the other 69% were managed medically.
Heart failure was the No. 1 reason for readmission within 90 days in patients who had PCI during the index hospitalization. It was the primary reason for 17.6% of readmissions. Next came recurrent angina or chest pain, which accounted for 6.6% of readmissions; chronic obstructive pulmonary disease or pneumonia, 6.3%; and GI bleeding with hemorrhage, which was the primary reason for 6.0% of readmissions. Together these four causes accounted for more than 36% of all readmissions in the PCI group.
“The GI bleeding data were really interesting,” the cardiologist said. “There’s a lot of talk now about reducing the duration of dual-antiplatelet therapy [DAPT] after PCI. This is an administrative data set that’s quite large, and it shows that GI bleeding in a post-PCI group early in the duration of DAPT is in fact a significant cause of readmission and poses significant hazard.”
Among patients who were medically managed during their index hospitalization, the top four reasons for readmission were heart failure, accounting for 20.6% of readmissions; cardiac surgery, 13.5%; sepsis, 7.8%; and chronic obstructive pulmonary disease/pneumonia, 6.3%. GI bleeding wasn’t a significant cause of readmission in this group.
“I think what we need to do next is dive deeper into the medically managed group. There is a cohort in there that’s incredibly sick and are likely to drive costs and be prone to readmission. And there’s another component of the medically managed group that had to be fairly healthy because they were able to undergo coronary artery bypass surgery within 90 days,” Dr. Kugelmass said.
He reported having no financial conflicts regarding his study.
WASHINGTON – In a large population of Medicare patients hospitalized for acute MI, four factors stood out as predictors of increased likelihood of readmission within 90 days, Aaron D. Kugelmass, MD, reported at the annual meeting of the American College of Cardiology.
These four predictors of 90-day readmission were end-stage renal disease at the time of the initial admission for MI, which in a logistic regression model was independently associated with an 88% relative increase in readmission risk; no percutaneous coronary intervention (PCI) during the index hospitalization, which carried a 64% increase in risk; type 1 diabetes, with a 57% increased readmission rate; and heart failure at the initial hospitalization, with an associated 34% greater risk, according to Dr. Kugelmass, chief of cardiology and medical director of the heart and vascular center at Baystate Medical Center in Springfield, Mass.
“This is going to be a learning curve for everyone,” he said.
“The best way to deal with this change is to understand the factors driving costs and morbidity and mortality,” Dr. Kugelmass said, in explaining why he conducted a retrospective study of readmissions within 90 days in a population of 143,286 Medicare beneficiaries hospitalized for acute MI in 2014. The study focus was on readmissions because they add so much to total cost of care for a 90-day episode.
Twenty-eight percent of patients were readmitted at least once within 90 days of discharge following their acute MI. The Medicare bundled payment plan divides MI patients into two separate groups: those who undergo PCI during their initial hospitalization and those who receive medical management only. Thirty-one percent of the readmitted patients in Dr. Kugelmass’s study had undergone PCI during their index hospitalization, while the other 69% were managed medically.
Heart failure was the No. 1 reason for readmission within 90 days in patients who had PCI during the index hospitalization. It was the primary reason for 17.6% of readmissions. Next came recurrent angina or chest pain, which accounted for 6.6% of readmissions; chronic obstructive pulmonary disease or pneumonia, 6.3%; and GI bleeding with hemorrhage, which was the primary reason for 6.0% of readmissions. Together these four causes accounted for more than 36% of all readmissions in the PCI group.
“The GI bleeding data were really interesting,” the cardiologist said. “There’s a lot of talk now about reducing the duration of dual-antiplatelet therapy [DAPT] after PCI. This is an administrative data set that’s quite large, and it shows that GI bleeding in a post-PCI group early in the duration of DAPT is in fact a significant cause of readmission and poses significant hazard.”
Among patients who were medically managed during their index hospitalization, the top four reasons for readmission were heart failure, accounting for 20.6% of readmissions; cardiac surgery, 13.5%; sepsis, 7.8%; and chronic obstructive pulmonary disease/pneumonia, 6.3%. GI bleeding wasn’t a significant cause of readmission in this group.
“I think what we need to do next is dive deeper into the medically managed group. There is a cohort in there that’s incredibly sick and are likely to drive costs and be prone to readmission. And there’s another component of the medically managed group that had to be fairly healthy because they were able to undergo coronary artery bypass surgery within 90 days,” Dr. Kugelmass said.
He reported having no financial conflicts regarding his study.
WASHINGTON – In a large population of Medicare patients hospitalized for acute MI, four factors stood out as predictors of increased likelihood of readmission within 90 days, Aaron D. Kugelmass, MD, reported at the annual meeting of the American College of Cardiology.
These four predictors of 90-day readmission were end-stage renal disease at the time of the initial admission for MI, which in a logistic regression model was independently associated with an 88% relative increase in readmission risk; no percutaneous coronary intervention (PCI) during the index hospitalization, which carried a 64% increase in risk; type 1 diabetes, with a 57% increased readmission rate; and heart failure at the initial hospitalization, with an associated 34% greater risk, according to Dr. Kugelmass, chief of cardiology and medical director of the heart and vascular center at Baystate Medical Center in Springfield, Mass.
“This is going to be a learning curve for everyone,” he said.
“The best way to deal with this change is to understand the factors driving costs and morbidity and mortality,” Dr. Kugelmass said, in explaining why he conducted a retrospective study of readmissions within 90 days in a population of 143,286 Medicare beneficiaries hospitalized for acute MI in 2014. The study focus was on readmissions because they add so much to total cost of care for a 90-day episode.
Twenty-eight percent of patients were readmitted at least once within 90 days of discharge following their acute MI. The Medicare bundled payment plan divides MI patients into two separate groups: those who undergo PCI during their initial hospitalization and those who receive medical management only. Thirty-one percent of the readmitted patients in Dr. Kugelmass’s study had undergone PCI during their index hospitalization, while the other 69% were managed medically.
Heart failure was the No. 1 reason for readmission within 90 days in patients who had PCI during the index hospitalization. It was the primary reason for 17.6% of readmissions. Next came recurrent angina or chest pain, which accounted for 6.6% of readmissions; chronic obstructive pulmonary disease or pneumonia, 6.3%; and GI bleeding with hemorrhage, which was the primary reason for 6.0% of readmissions. Together these four causes accounted for more than 36% of all readmissions in the PCI group.
“The GI bleeding data were really interesting,” the cardiologist said. “There’s a lot of talk now about reducing the duration of dual-antiplatelet therapy [DAPT] after PCI. This is an administrative data set that’s quite large, and it shows that GI bleeding in a post-PCI group early in the duration of DAPT is in fact a significant cause of readmission and poses significant hazard.”
Among patients who were medically managed during their index hospitalization, the top four reasons for readmission were heart failure, accounting for 20.6% of readmissions; cardiac surgery, 13.5%; sepsis, 7.8%; and chronic obstructive pulmonary disease/pneumonia, 6.3%. GI bleeding wasn’t a significant cause of readmission in this group.
“I think what we need to do next is dive deeper into the medically managed group. There is a cohort in there that’s incredibly sick and are likely to drive costs and be prone to readmission. And there’s another component of the medically managed group that had to be fairly healthy because they were able to undergo coronary artery bypass surgery within 90 days,” Dr. Kugelmass said.
He reported having no financial conflicts regarding his study.
Key clinical point:
Major finding: Twenty-eight percent of Medicare patients hospitalized for acute MI were readmitted within 90 days.
Data source: A retrospective study of readmissions within 90 days among more than 143,000 Medicare beneficiaries hospitalized for acute MI in 2014.
Disclosures: The study presenter reported having no financial conflicts.
Crossing the personal quality chasm: QI enthusiast to QI leader
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.