User login
Hospitalist's Study Cited in Federal Recovery Audit Legislation Passed by Senate
Society of Hospital Medicine members have a real impact.
A paper published in the Journal of Hospital Medicine in April by Ann Sheehy, MD, MS, and colleagues was recently cited in Sen. Ben Cardin’s (D-Md.) amendment to the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015.1,2 The act aims to improve the accuracy and transparency of recovery audits (RA), which were the subject of testimony given by Dr. Sheehy—a hospitalist at the University of Wisconsin-Madison—by invitation before Congress twice in 2014.
Formally called recovery audit contractors, or RACS, RAs evaluate whether hospitals were overpaid for hospitalizations improperly deemed inpatient rather than outpatient via observation status. In the study cited before the Senate Finance Committee, Dr. Sheehy’s group found a three-fold increase in RA overpayment determinations from 2010 to 2013; concurrently, the number of decisions overturned in favor of cited hospitals, either in discussion or appeal, doubled, going from 36% in 2010 to nearly 70% in 2013.
RAs share a percentage of the money they recover for the Centers for Medicare and Medicaid Services, even when decisions are appealed and won by hospitals. As Dr. Sheehy testified last year: “Unfortunately, these contingency incentives favor aggressive auditing, without transparency, accountability, or repercussions for cases that should never have been audited.”
The bill passed the Senate on June 5, 2015.
References
- Sheehy AM, Locke C, Engel JZ, et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212-219. doi: 10.1002/jhm.2332.
- United States Senate Committee on Finance. Master Amendments of the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015. Accessed July 7, 2015.
Society of Hospital Medicine members have a real impact.
A paper published in the Journal of Hospital Medicine in April by Ann Sheehy, MD, MS, and colleagues was recently cited in Sen. Ben Cardin’s (D-Md.) amendment to the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015.1,2 The act aims to improve the accuracy and transparency of recovery audits (RA), which were the subject of testimony given by Dr. Sheehy—a hospitalist at the University of Wisconsin-Madison—by invitation before Congress twice in 2014.
Formally called recovery audit contractors, or RACS, RAs evaluate whether hospitals were overpaid for hospitalizations improperly deemed inpatient rather than outpatient via observation status. In the study cited before the Senate Finance Committee, Dr. Sheehy’s group found a three-fold increase in RA overpayment determinations from 2010 to 2013; concurrently, the number of decisions overturned in favor of cited hospitals, either in discussion or appeal, doubled, going from 36% in 2010 to nearly 70% in 2013.
RAs share a percentage of the money they recover for the Centers for Medicare and Medicaid Services, even when decisions are appealed and won by hospitals. As Dr. Sheehy testified last year: “Unfortunately, these contingency incentives favor aggressive auditing, without transparency, accountability, or repercussions for cases that should never have been audited.”
The bill passed the Senate on June 5, 2015.
References
- Sheehy AM, Locke C, Engel JZ, et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212-219. doi: 10.1002/jhm.2332.
- United States Senate Committee on Finance. Master Amendments of the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015. Accessed July 7, 2015.
Society of Hospital Medicine members have a real impact.
A paper published in the Journal of Hospital Medicine in April by Ann Sheehy, MD, MS, and colleagues was recently cited in Sen. Ben Cardin’s (D-Md.) amendment to the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015.1,2 The act aims to improve the accuracy and transparency of recovery audits (RA), which were the subject of testimony given by Dr. Sheehy—a hospitalist at the University of Wisconsin-Madison—by invitation before Congress twice in 2014.
Formally called recovery audit contractors, or RACS, RAs evaluate whether hospitals were overpaid for hospitalizations improperly deemed inpatient rather than outpatient via observation status. In the study cited before the Senate Finance Committee, Dr. Sheehy’s group found a three-fold increase in RA overpayment determinations from 2010 to 2013; concurrently, the number of decisions overturned in favor of cited hospitals, either in discussion or appeal, doubled, going from 36% in 2010 to nearly 70% in 2013.
RAs share a percentage of the money they recover for the Centers for Medicare and Medicaid Services, even when decisions are appealed and won by hospitals. As Dr. Sheehy testified last year: “Unfortunately, these contingency incentives favor aggressive auditing, without transparency, accountability, or repercussions for cases that should never have been audited.”
The bill passed the Senate on June 5, 2015.
References
- Sheehy AM, Locke C, Engel JZ, et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212-219. doi: 10.1002/jhm.2332.
- United States Senate Committee on Finance. Master Amendments of the Audit and Appeal Fairness, Integrity, and Reforms in Medicare Act of 2015. Accessed July 7, 2015.
Podcast Series "Before the White Coat" Explores Early Lives of Hospitalists
Editor’s note: This article is adapted from a June 2015 post on SHM’s official blog, “The Hospital Leader”.
When you see him on stage, it’s like he’s always been here. Bob Wachter, MD, one of the pioneers of the hospital medicine movement, has taken the podium at SHM’s annual meetings for more than a decade. Whether he’s uncovering important issues in electronic medical records or covering Elton John songs, he seems like a fixture in our world—and in healthcare.
The Unique Paths of Hospitalist Careers
But, rather than being a fixed, static thing, the life of any hospitalist—including the leaders of the movement—is a progression.
That progression starts in a different place for every hospitalist and is influenced by the people and events in their lives. Some hospitalists knew they wanted to be in medicine from a young age. Others found their calling much later in life.
Every one of those progressions is interspersed with moments of humor. For instance, this piece of hospitalist trivia: Dr. Wachter was the Penn Quaker mascot for the University of Pennsylvania the last time its men’s basketball team made it to the Final Four.
They also include the kinds of profound experiences that get to the very root of what it means to be a hospitalist. For Bob, it was being a resident in the ICU at the University of California San Francisco in the 1980s, just as AIDS was beginning to be diagnosed and understood.
That’s why I’m proud to introduce “Before the White Coat,” a new podcast from SHM, available on iTunes and other podcast apps. “Before the White Coat” is a 20-minute podcast, presented every two weeks.
Today, you can listen to full interviews between me and Bob Wachter, Ron Greeno of IPC Health, Jeff Wiese at Tulane University, SHM President Bob Harrington, CMS's Chief Medical Officer Patrick Conway and UCLA's Nasim Afsar. And later in September, Before the White Coat will present exclusive insights into the lives of Brian Harte of the Cleveland Clinic and Mark Williams at the University of Kentucky.

—Larry Wellikson, MD, MHM
Next, you’ll hear from Ron Greeno, MD, MHM, FCCP, now chief strategy officer at IPC Healthcare. After that, I’ll talk with many of the other leaders every two weeks, including Pat Conway, MD, MSc, at the Centers for Medicare and Medicaid Services, Mary Jo Gorman, MD, MBA, who founded Advanced ICU Care, and Nasim Afsar, MD, FSHM, at UCLA.
I’m looking forward to exploring the progression of their lives and careers with you. These personal conversations complement the wealth of clinical and practice management information that SHM already offers.
Podcast: A Format That Works for Hospitalists
Hospitalists are busy people. Whether at the hospital or at home, they are almost constantly on their feet. We wanted to present “Before the White Coat” as a podcast—something you can listen to while on the way to the hospital—or on the way home. Or maybe during an off hour in either place.
And we know that hospitalists are interested in podcasts; podcasts produced and distributed by The Hospitalist have been downloaded more than 40,000 times.
In fact, this podcast is modeled on some of the most successful podcasts out there: National Public Radio’s industry-leading podcasts, the new podcasts from Gimlet Media, and Adam Corolla’s “Take a Knee.”
Those podcasts have proven that the format works—and that people are catching on quickly. According to new research from the Pew Research Center, one in three Americans have listened to a podcast, and the number of people who have listened to a podcast in the last month has doubled since 2008.
How to Listen and Share
I hope you’ll join their ranks today. Here’s how:
- Visit the “Before the White Coat” website, www.beforethewhitecoat.org.
- iTunes users can subscribe by searching “Before the White Coat” in the podcast section of iTunes.
- And listeners using other podcast apps can either search for “Before the White Coat” or find details on the podcast website.
This is a new project for SHM, and I hope you’ll tell us what you think. You can tweet your reaction at @SHMLive—use the #B4theWC hashtag.
Finally, if you like it, I hope you’ll share it with friends, colleagues, and others in medicine.
As always, thank you for being an active part of the hospital medicine movement. I hope you’ll enjoy this newest piece of it.
Larry Wellikson is CEO of the Society of Hospital Medicine.
Editor’s note: This article is adapted from a June 2015 post on SHM’s official blog, “The Hospital Leader”.
When you see him on stage, it’s like he’s always been here. Bob Wachter, MD, one of the pioneers of the hospital medicine movement, has taken the podium at SHM’s annual meetings for more than a decade. Whether he’s uncovering important issues in electronic medical records or covering Elton John songs, he seems like a fixture in our world—and in healthcare.
The Unique Paths of Hospitalist Careers
But, rather than being a fixed, static thing, the life of any hospitalist—including the leaders of the movement—is a progression.
That progression starts in a different place for every hospitalist and is influenced by the people and events in their lives. Some hospitalists knew they wanted to be in medicine from a young age. Others found their calling much later in life.
Every one of those progressions is interspersed with moments of humor. For instance, this piece of hospitalist trivia: Dr. Wachter was the Penn Quaker mascot for the University of Pennsylvania the last time its men’s basketball team made it to the Final Four.
They also include the kinds of profound experiences that get to the very root of what it means to be a hospitalist. For Bob, it was being a resident in the ICU at the University of California San Francisco in the 1980s, just as AIDS was beginning to be diagnosed and understood.
That’s why I’m proud to introduce “Before the White Coat,” a new podcast from SHM, available on iTunes and other podcast apps. “Before the White Coat” is a 20-minute podcast, presented every two weeks.
Today, you can listen to full interviews between me and Bob Wachter, Ron Greeno of IPC Health, Jeff Wiese at Tulane University, SHM President Bob Harrington, CMS's Chief Medical Officer Patrick Conway and UCLA's Nasim Afsar. And later in September, Before the White Coat will present exclusive insights into the lives of Brian Harte of the Cleveland Clinic and Mark Williams at the University of Kentucky.

—Larry Wellikson, MD, MHM
Next, you’ll hear from Ron Greeno, MD, MHM, FCCP, now chief strategy officer at IPC Healthcare. After that, I’ll talk with many of the other leaders every two weeks, including Pat Conway, MD, MSc, at the Centers for Medicare and Medicaid Services, Mary Jo Gorman, MD, MBA, who founded Advanced ICU Care, and Nasim Afsar, MD, FSHM, at UCLA.
I’m looking forward to exploring the progression of their lives and careers with you. These personal conversations complement the wealth of clinical and practice management information that SHM already offers.
Podcast: A Format That Works for Hospitalists
Hospitalists are busy people. Whether at the hospital or at home, they are almost constantly on their feet. We wanted to present “Before the White Coat” as a podcast—something you can listen to while on the way to the hospital—or on the way home. Or maybe during an off hour in either place.
And we know that hospitalists are interested in podcasts; podcasts produced and distributed by The Hospitalist have been downloaded more than 40,000 times.
In fact, this podcast is modeled on some of the most successful podcasts out there: National Public Radio’s industry-leading podcasts, the new podcasts from Gimlet Media, and Adam Corolla’s “Take a Knee.”
Those podcasts have proven that the format works—and that people are catching on quickly. According to new research from the Pew Research Center, one in three Americans have listened to a podcast, and the number of people who have listened to a podcast in the last month has doubled since 2008.
How to Listen and Share
I hope you’ll join their ranks today. Here’s how:
- Visit the “Before the White Coat” website, www.beforethewhitecoat.org.
- iTunes users can subscribe by searching “Before the White Coat” in the podcast section of iTunes.
- And listeners using other podcast apps can either search for “Before the White Coat” or find details on the podcast website.
This is a new project for SHM, and I hope you’ll tell us what you think. You can tweet your reaction at @SHMLive—use the #B4theWC hashtag.
Finally, if you like it, I hope you’ll share it with friends, colleagues, and others in medicine.
As always, thank you for being an active part of the hospital medicine movement. I hope you’ll enjoy this newest piece of it.
Larry Wellikson is CEO of the Society of Hospital Medicine.
Editor’s note: This article is adapted from a June 2015 post on SHM’s official blog, “The Hospital Leader”.
When you see him on stage, it’s like he’s always been here. Bob Wachter, MD, one of the pioneers of the hospital medicine movement, has taken the podium at SHM’s annual meetings for more than a decade. Whether he’s uncovering important issues in electronic medical records or covering Elton John songs, he seems like a fixture in our world—and in healthcare.
The Unique Paths of Hospitalist Careers
But, rather than being a fixed, static thing, the life of any hospitalist—including the leaders of the movement—is a progression.
That progression starts in a different place for every hospitalist and is influenced by the people and events in their lives. Some hospitalists knew they wanted to be in medicine from a young age. Others found their calling much later in life.
Every one of those progressions is interspersed with moments of humor. For instance, this piece of hospitalist trivia: Dr. Wachter was the Penn Quaker mascot for the University of Pennsylvania the last time its men’s basketball team made it to the Final Four.
They also include the kinds of profound experiences that get to the very root of what it means to be a hospitalist. For Bob, it was being a resident in the ICU at the University of California San Francisco in the 1980s, just as AIDS was beginning to be diagnosed and understood.
That’s why I’m proud to introduce “Before the White Coat,” a new podcast from SHM, available on iTunes and other podcast apps. “Before the White Coat” is a 20-minute podcast, presented every two weeks.
Today, you can listen to full interviews between me and Bob Wachter, Ron Greeno of IPC Health, Jeff Wiese at Tulane University, SHM President Bob Harrington, CMS's Chief Medical Officer Patrick Conway and UCLA's Nasim Afsar. And later in September, Before the White Coat will present exclusive insights into the lives of Brian Harte of the Cleveland Clinic and Mark Williams at the University of Kentucky.

—Larry Wellikson, MD, MHM
Next, you’ll hear from Ron Greeno, MD, MHM, FCCP, now chief strategy officer at IPC Healthcare. After that, I’ll talk with many of the other leaders every two weeks, including Pat Conway, MD, MSc, at the Centers for Medicare and Medicaid Services, Mary Jo Gorman, MD, MBA, who founded Advanced ICU Care, and Nasim Afsar, MD, FSHM, at UCLA.
I’m looking forward to exploring the progression of their lives and careers with you. These personal conversations complement the wealth of clinical and practice management information that SHM already offers.
Podcast: A Format That Works for Hospitalists
Hospitalists are busy people. Whether at the hospital or at home, they are almost constantly on their feet. We wanted to present “Before the White Coat” as a podcast—something you can listen to while on the way to the hospital—or on the way home. Or maybe during an off hour in either place.
And we know that hospitalists are interested in podcasts; podcasts produced and distributed by The Hospitalist have been downloaded more than 40,000 times.
In fact, this podcast is modeled on some of the most successful podcasts out there: National Public Radio’s industry-leading podcasts, the new podcasts from Gimlet Media, and Adam Corolla’s “Take a Knee.”
Those podcasts have proven that the format works—and that people are catching on quickly. According to new research from the Pew Research Center, one in three Americans have listened to a podcast, and the number of people who have listened to a podcast in the last month has doubled since 2008.
How to Listen and Share
I hope you’ll join their ranks today. Here’s how:
- Visit the “Before the White Coat” website, www.beforethewhitecoat.org.
- iTunes users can subscribe by searching “Before the White Coat” in the podcast section of iTunes.
- And listeners using other podcast apps can either search for “Before the White Coat” or find details on the podcast website.
This is a new project for SHM, and I hope you’ll tell us what you think. You can tweet your reaction at @SHMLive—use the #B4theWC hashtag.
Finally, if you like it, I hope you’ll share it with friends, colleagues, and others in medicine.
As always, thank you for being an active part of the hospital medicine movement. I hope you’ll enjoy this newest piece of it.
Larry Wellikson is CEO of the Society of Hospital Medicine.
Specialty Hospitalists May Be Coming to Your Hospital Soon
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
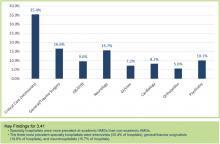
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Nearly 20 years ago, Bob Wachter, MD, coined the term “hospitalist,” defining a new specialty caring for the hospitalized medical patient. Since that time, we’ve seen rapid growth in the numbers of physicians who identify themselves as hospitalists, dominated by training in internal medicine and, to a lesser extent, family practice and pediatrics.
But, what about other specialty hospitalists, trained in the medicine or surgical specialties? How much of a presence do they have in our institutions today and in which specialties? To help us better understand this, a new question in 2014 State of Hospital Medicine survey asked whether specialty hospitalists practice in your hospital or health system.

—Carolyn Sites, DO, FHM
Results show the top three specialty hospitalists to be critical care, at (35.4%), followed by general surgery/trauma (16.6%) and neurology (15.7%), based on the responses of survey participants representing hospital medicine groups (HMGs) that care for adults only. Other specialties included obstetrics (OB), psychiatry, GI, cardiology, and orthopedics (see Figure 1).
Perhaps not too surprising, the greatest number of specialty hospitalists are found in university and academic settings. These are our primary training centers, offering fellowship programs and further subspecialization programs. Much like in our own field of hospital medicine, some academic centers have created one-year fellowships for those interested in specific hospital specialty fields, such as OB hospitalist.
For reasons that are less clear, the survey also shows percentages are highest in the western U.S. and lowest in the East.
Critical care hospitalists, also known as intensivists, dominate the spectrum, being present in academic and nonacademic centers, regardless of the employment model of the medical hospitalists at those facilities. This is not unexpected, given the Leapfrog Group’s endorsement of ICU physician staffing with intensivists.
What’s driving the other specialty hospitalist fields? I suspect the reasons are similar to those of our own specialty. OB and neuro hospitalists at my health system cite the challenges of managing outpatient and inpatient practices, the higher inpatient acuity and focused skill set that are required, immediate availability demands, and work-life balance as key factors. Further drivers include external quality/safety governing agencies or groups, such as the Leapfrog example above, or The Joint Commission’s requirements for certification as a Comprehensive Stroke Center with neurointensive care units.
Much like our own field’s exponential growth, we are likely to see further expansion of specialty hospitalists over the next several years. It will be interesting to watch how much and how fast this occurs, and what impact and influence these groups will bring to the care of the hospitalized patient. I’m already looking forward to next year’s SOHM report to see those results.
Dr. Sites is regional medical director of hospital medicine at Providence Health Systems in Oregon and a member of the SHM Practice Analysis Committee.
Regional CMO Robert Zipper, MD, MMM, SFHM, is Proud to Be Known as a Leader
Any hospitalist working for the largest HM group (HMG) in the country has one heck of a top-down perspective. And if you’re Robert Zipper, MD, MMM, SFHM, a regional chief medical officer (CMO) overseeing 25 hospitalist programs in the Pacific Northwest and Northern California for Sound Physicians, you love it.
“In my role, I really like working with younger leaders and those that are the future of the specialty,” he says, “but mostly I like knowing that I am supporting people that are doing incredible work, day in and day out.
“And I am never, ever bored.”
And, while never unengaged in his day-to-day job, Dr. Zipper has also been an active member of SHM. A former member of the Hospital Quality and Patient Safety (HQPS) Committee, Dr. Zipper currently chairs the Leadership Committee. The latest line on his resume is his role as one of seven new members of Team Hospitalist, the volunteer editorial advisory board of SHM’s official newsmagazine.

–Dr. Zipper
Question: Why did you choose a career in medicine?
Answer: Both of my parents were psychotherapists, and I knew that I wanted to do something in healthcare…but not that!
Q: How/when did you decide to become a hospitalist?
A: I always liked inpatient medicine. I did 50/50 inpatient and outpatient for my first three years out of training, and the hospitalist part of that crumbled. That led to the opportunity to do pure hospital medicine in the same community in 2002, and I took it!
Q: Tell me a little more about medical school, residency, etc. Was there a single moment you knew “I can do this?”
A: I chose a single large institution because I wanted to know the people I worked with, as healthcare is all about relationships. In medical school, I didn’t spend more than two months at any given hospital doing rotations, and that didn’t seem like the best way to learn. It wasn’t like the real world. I never had self doubt that I would finish what I had started, partly because I had to work so hard to get into medical school in the first place.
Q: What do you like most about working as a hospitalist?
A: I enjoy the high acuity, but miss the longer-term relationships of outpatient care.
Q: What do you dislike most?
A: My role as regional CMO for a large management company never ends. I’m never “done with my shift,” so to speak. I love my job but would love more family time, too.
Q: What’s the best advice you ever received?
A: I was applying for medical school in the late 1990s, and I worked as a tech in an emergency department in Michigan. Many physicians at that time were jaded, feeling that the golden era of being a doctor had come and gone. The best advice I ever received was to ignore their negativity and to make my own future. This came from an emergency medicine resident named Paul Blackburn, who later went on to be the ED residency director at University of Arizona.
Q: Did you have a mentor during training or early career?
A: Not really, though I thought about oncology, and one of my oncology attendings played a special role for me. I ultimately chose not to do that specialty because I couldn’t deal with the high mortality—I took the grim reality that so many patients face home with me.
Q: What’s the biggest change you’ve seen in HM in your career?
A: Where to start? HM used to be a “thing,” requiring a lot of explanation. Now we have a peer-reviewed journal, and some of the best internists and family physicians in the U.S. choose hospital medicine as a career. Patients are more accepting.
Q: What’s the biggest change you would like to see in HM?
A: This may sound odd, but I would like compensation to stabilize. It will happen, but the continuous upward climb, while benefitting physicians on one hand, also serves to destabilize programs and create difficult financial situations for hospitals, particularly smaller hospitals that are at risk of closing nowadays.
Q: As a leader, why is it important for you to continue seeing patients?
A: I think that being able to see things from a variety of perspectives is very important.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Time management on a hospitalist’s first day is a challenge, as it always takes more time to really understand a patient and their course. Patients generally don’t like being asked the same questions repetitively.
Q: What aspect of patient care is most rewarding?
A: The human connection and feeling that you’ve played an important part in a patient’s and their family’s lives.
Q: What is your biggest professional challenge?
A: The very rapid pace of change when working with several hospitals and systems that each have their own set of strengths and challenges.
Q: What is your biggest professional reward?
A: Feeling like a part of something really meaningful. I am proud of being a leader in my organization, and I have never felt that way in any other job.
Q: What did it mean to you to be elected a Senior Fellow in Hospital Medicine?
A: I was elected SFHM in the first cohort, and I was not sure what to make of it. It has become something that is more meaningful over time as it is more widely recognized.
Q: What’s next professionally?
A: Transitional care. We are working hard to improve care in the post-acute period. The variability there is incredible, and where there is variability, there is waste. Making it work as a business, though, is another matter.
Q: If you weren’t a doctor, what would you be doing right now?
A: Probably either in information technology in some fashion—I built my first PC back when the 386 processor was king—or in music. I’ve played drums for a long time and still do whenever I get the chance.
Q: When you aren’t working, what is important to you?
A: Given that I travel quite a bit, I like to spend time with my family. We live in Bend, Ore., which offers great outdoor activities like mountain biking and skiing. We like to stay active as a family.
Q: What’s the best book you’ve read recently?
A: Being Mortal by Atul Gawande.
Any hospitalist working for the largest HM group (HMG) in the country has one heck of a top-down perspective. And if you’re Robert Zipper, MD, MMM, SFHM, a regional chief medical officer (CMO) overseeing 25 hospitalist programs in the Pacific Northwest and Northern California for Sound Physicians, you love it.
“In my role, I really like working with younger leaders and those that are the future of the specialty,” he says, “but mostly I like knowing that I am supporting people that are doing incredible work, day in and day out.
“And I am never, ever bored.”
And, while never unengaged in his day-to-day job, Dr. Zipper has also been an active member of SHM. A former member of the Hospital Quality and Patient Safety (HQPS) Committee, Dr. Zipper currently chairs the Leadership Committee. The latest line on his resume is his role as one of seven new members of Team Hospitalist, the volunteer editorial advisory board of SHM’s official newsmagazine.

–Dr. Zipper
Question: Why did you choose a career in medicine?
Answer: Both of my parents were psychotherapists, and I knew that I wanted to do something in healthcare…but not that!
Q: How/when did you decide to become a hospitalist?
A: I always liked inpatient medicine. I did 50/50 inpatient and outpatient for my first three years out of training, and the hospitalist part of that crumbled. That led to the opportunity to do pure hospital medicine in the same community in 2002, and I took it!
Q: Tell me a little more about medical school, residency, etc. Was there a single moment you knew “I can do this?”
A: I chose a single large institution because I wanted to know the people I worked with, as healthcare is all about relationships. In medical school, I didn’t spend more than two months at any given hospital doing rotations, and that didn’t seem like the best way to learn. It wasn’t like the real world. I never had self doubt that I would finish what I had started, partly because I had to work so hard to get into medical school in the first place.
Q: What do you like most about working as a hospitalist?
A: I enjoy the high acuity, but miss the longer-term relationships of outpatient care.
Q: What do you dislike most?
A: My role as regional CMO for a large management company never ends. I’m never “done with my shift,” so to speak. I love my job but would love more family time, too.
Q: What’s the best advice you ever received?
A: I was applying for medical school in the late 1990s, and I worked as a tech in an emergency department in Michigan. Many physicians at that time were jaded, feeling that the golden era of being a doctor had come and gone. The best advice I ever received was to ignore their negativity and to make my own future. This came from an emergency medicine resident named Paul Blackburn, who later went on to be the ED residency director at University of Arizona.
Q: Did you have a mentor during training or early career?
A: Not really, though I thought about oncology, and one of my oncology attendings played a special role for me. I ultimately chose not to do that specialty because I couldn’t deal with the high mortality—I took the grim reality that so many patients face home with me.
Q: What’s the biggest change you’ve seen in HM in your career?
A: Where to start? HM used to be a “thing,” requiring a lot of explanation. Now we have a peer-reviewed journal, and some of the best internists and family physicians in the U.S. choose hospital medicine as a career. Patients are more accepting.
Q: What’s the biggest change you would like to see in HM?
A: This may sound odd, but I would like compensation to stabilize. It will happen, but the continuous upward climb, while benefitting physicians on one hand, also serves to destabilize programs and create difficult financial situations for hospitals, particularly smaller hospitals that are at risk of closing nowadays.
Q: As a leader, why is it important for you to continue seeing patients?
A: I think that being able to see things from a variety of perspectives is very important.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Time management on a hospitalist’s first day is a challenge, as it always takes more time to really understand a patient and their course. Patients generally don’t like being asked the same questions repetitively.
Q: What aspect of patient care is most rewarding?
A: The human connection and feeling that you’ve played an important part in a patient’s and their family’s lives.
Q: What is your biggest professional challenge?
A: The very rapid pace of change when working with several hospitals and systems that each have their own set of strengths and challenges.
Q: What is your biggest professional reward?
A: Feeling like a part of something really meaningful. I am proud of being a leader in my organization, and I have never felt that way in any other job.
Q: What did it mean to you to be elected a Senior Fellow in Hospital Medicine?
A: I was elected SFHM in the first cohort, and I was not sure what to make of it. It has become something that is more meaningful over time as it is more widely recognized.
Q: What’s next professionally?
A: Transitional care. We are working hard to improve care in the post-acute period. The variability there is incredible, and where there is variability, there is waste. Making it work as a business, though, is another matter.
Q: If you weren’t a doctor, what would you be doing right now?
A: Probably either in information technology in some fashion—I built my first PC back when the 386 processor was king—or in music. I’ve played drums for a long time and still do whenever I get the chance.
Q: When you aren’t working, what is important to you?
A: Given that I travel quite a bit, I like to spend time with my family. We live in Bend, Ore., which offers great outdoor activities like mountain biking and skiing. We like to stay active as a family.
Q: What’s the best book you’ve read recently?
A: Being Mortal by Atul Gawande.
Any hospitalist working for the largest HM group (HMG) in the country has one heck of a top-down perspective. And if you’re Robert Zipper, MD, MMM, SFHM, a regional chief medical officer (CMO) overseeing 25 hospitalist programs in the Pacific Northwest and Northern California for Sound Physicians, you love it.
“In my role, I really like working with younger leaders and those that are the future of the specialty,” he says, “but mostly I like knowing that I am supporting people that are doing incredible work, day in and day out.
“And I am never, ever bored.”
And, while never unengaged in his day-to-day job, Dr. Zipper has also been an active member of SHM. A former member of the Hospital Quality and Patient Safety (HQPS) Committee, Dr. Zipper currently chairs the Leadership Committee. The latest line on his resume is his role as one of seven new members of Team Hospitalist, the volunteer editorial advisory board of SHM’s official newsmagazine.

–Dr. Zipper
Question: Why did you choose a career in medicine?
Answer: Both of my parents were psychotherapists, and I knew that I wanted to do something in healthcare…but not that!
Q: How/when did you decide to become a hospitalist?
A: I always liked inpatient medicine. I did 50/50 inpatient and outpatient for my first three years out of training, and the hospitalist part of that crumbled. That led to the opportunity to do pure hospital medicine in the same community in 2002, and I took it!
Q: Tell me a little more about medical school, residency, etc. Was there a single moment you knew “I can do this?”
A: I chose a single large institution because I wanted to know the people I worked with, as healthcare is all about relationships. In medical school, I didn’t spend more than two months at any given hospital doing rotations, and that didn’t seem like the best way to learn. It wasn’t like the real world. I never had self doubt that I would finish what I had started, partly because I had to work so hard to get into medical school in the first place.
Q: What do you like most about working as a hospitalist?
A: I enjoy the high acuity, but miss the longer-term relationships of outpatient care.
Q: What do you dislike most?
A: My role as regional CMO for a large management company never ends. I’m never “done with my shift,” so to speak. I love my job but would love more family time, too.
Q: What’s the best advice you ever received?
A: I was applying for medical school in the late 1990s, and I worked as a tech in an emergency department in Michigan. Many physicians at that time were jaded, feeling that the golden era of being a doctor had come and gone. The best advice I ever received was to ignore their negativity and to make my own future. This came from an emergency medicine resident named Paul Blackburn, who later went on to be the ED residency director at University of Arizona.
Q: Did you have a mentor during training or early career?
A: Not really, though I thought about oncology, and one of my oncology attendings played a special role for me. I ultimately chose not to do that specialty because I couldn’t deal with the high mortality—I took the grim reality that so many patients face home with me.
Q: What’s the biggest change you’ve seen in HM in your career?
A: Where to start? HM used to be a “thing,” requiring a lot of explanation. Now we have a peer-reviewed journal, and some of the best internists and family physicians in the U.S. choose hospital medicine as a career. Patients are more accepting.
Q: What’s the biggest change you would like to see in HM?
A: This may sound odd, but I would like compensation to stabilize. It will happen, but the continuous upward climb, while benefitting physicians on one hand, also serves to destabilize programs and create difficult financial situations for hospitals, particularly smaller hospitals that are at risk of closing nowadays.
Q: As a leader, why is it important for you to continue seeing patients?
A: I think that being able to see things from a variety of perspectives is very important.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Time management on a hospitalist’s first day is a challenge, as it always takes more time to really understand a patient and their course. Patients generally don’t like being asked the same questions repetitively.
Q: What aspect of patient care is most rewarding?
A: The human connection and feeling that you’ve played an important part in a patient’s and their family’s lives.
Q: What is your biggest professional challenge?
A: The very rapid pace of change when working with several hospitals and systems that each have their own set of strengths and challenges.
Q: What is your biggest professional reward?
A: Feeling like a part of something really meaningful. I am proud of being a leader in my organization, and I have never felt that way in any other job.
Q: What did it mean to you to be elected a Senior Fellow in Hospital Medicine?
A: I was elected SFHM in the first cohort, and I was not sure what to make of it. It has become something that is more meaningful over time as it is more widely recognized.
Q: What’s next professionally?
A: Transitional care. We are working hard to improve care in the post-acute period. The variability there is incredible, and where there is variability, there is waste. Making it work as a business, though, is another matter.
Q: If you weren’t a doctor, what would you be doing right now?
A: Probably either in information technology in some fashion—I built my first PC back when the 386 processor was king—or in music. I’ve played drums for a long time and still do whenever I get the chance.
Q: When you aren’t working, what is important to you?
A: Given that I travel quite a bit, I like to spend time with my family. We live in Bend, Ore., which offers great outdoor activities like mountain biking and skiing. We like to stay active as a family.
Q: What’s the best book you’ve read recently?
A: Being Mortal by Atul Gawande.
PPI Usage with SBP Prophylaxis Predicts Recurrent Infections in Cirrhosis
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Nontoxigenic C. diff Spores May Decrease Rates of Recurrent CDI
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Retrievable IVC Plus Anticoagulation Does Not Reduce Risk of Recurrent Pulmonary Embolism
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
Joint Commission Leaders Call on Physicians to Embrace Quality Improvement
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
Hospitalists Choose Quality Metrics Most Important to Them
Fantasy sports, hospital medicine, and quality metrics. Those were the unique elements of an RIV poster presented by Noppon Setji, MD, medical director of the Duke University Medical Center’s hospital medicine program in Durham, N.C., at HM15.
Dr. Setji, who participates in a fantasy football league for physicians, says he aimed to apply the approaches of fantasy sports leagues to hospitalist quality metrics.1 Dr. Setji wanted to find a way to recognize high-performing hospitalists in his group on a regular basis, beyond the group metrics that had been reported to faculty members—and to create greater accountability and evaluate physicians’ performance over time.
A team developed a survey instrument compiling common clinical process and outcome measures for hospitalists, and faculty members were asked to rate how important the various metrics were to them individually as indicators of physician performance. Their responses were combined into a weighted, composite hospital medicine provider performance score, which reflects the relative value practicing hospitalists assign to available performance measures. Results are easily tabulated on an Excel spreadsheet, Dr. Setji says.
Every three months—or football quarter—the top overall performer is awarded two bottles of wine and possession of the traveling trophy.
“We’re always looking for ways to measure our performance,” Dr. Setji says, “and we all want to know how we’re doing relative to our peers.”
Reference
- Setji NP, Bae JG, Griffith BC, Daley C. Fantasy physician leagues? Introducing the physician equivalent of the Qbr (Quarterly Metric-Based Rating) [abstract]. J Hosp Med. 2015;10(suppl 2).
Fantasy sports, hospital medicine, and quality metrics. Those were the unique elements of an RIV poster presented by Noppon Setji, MD, medical director of the Duke University Medical Center’s hospital medicine program in Durham, N.C., at HM15.
Dr. Setji, who participates in a fantasy football league for physicians, says he aimed to apply the approaches of fantasy sports leagues to hospitalist quality metrics.1 Dr. Setji wanted to find a way to recognize high-performing hospitalists in his group on a regular basis, beyond the group metrics that had been reported to faculty members—and to create greater accountability and evaluate physicians’ performance over time.
A team developed a survey instrument compiling common clinical process and outcome measures for hospitalists, and faculty members were asked to rate how important the various metrics were to them individually as indicators of physician performance. Their responses were combined into a weighted, composite hospital medicine provider performance score, which reflects the relative value practicing hospitalists assign to available performance measures. Results are easily tabulated on an Excel spreadsheet, Dr. Setji says.
Every three months—or football quarter—the top overall performer is awarded two bottles of wine and possession of the traveling trophy.
“We’re always looking for ways to measure our performance,” Dr. Setji says, “and we all want to know how we’re doing relative to our peers.”
Reference
- Setji NP, Bae JG, Griffith BC, Daley C. Fantasy physician leagues? Introducing the physician equivalent of the Qbr (Quarterly Metric-Based Rating) [abstract]. J Hosp Med. 2015;10(suppl 2).
Fantasy sports, hospital medicine, and quality metrics. Those were the unique elements of an RIV poster presented by Noppon Setji, MD, medical director of the Duke University Medical Center’s hospital medicine program in Durham, N.C., at HM15.
Dr. Setji, who participates in a fantasy football league for physicians, says he aimed to apply the approaches of fantasy sports leagues to hospitalist quality metrics.1 Dr. Setji wanted to find a way to recognize high-performing hospitalists in his group on a regular basis, beyond the group metrics that had been reported to faculty members—and to create greater accountability and evaluate physicians’ performance over time.
A team developed a survey instrument compiling common clinical process and outcome measures for hospitalists, and faculty members were asked to rate how important the various metrics were to them individually as indicators of physician performance. Their responses were combined into a weighted, composite hospital medicine provider performance score, which reflects the relative value practicing hospitalists assign to available performance measures. Results are easily tabulated on an Excel spreadsheet, Dr. Setji says.
Every three months—or football quarter—the top overall performer is awarded two bottles of wine and possession of the traveling trophy.
“We’re always looking for ways to measure our performance,” Dr. Setji says, “and we all want to know how we’re doing relative to our peers.”
Reference
- Setji NP, Bae JG, Griffith BC, Daley C. Fantasy physician leagues? Introducing the physician equivalent of the Qbr (Quarterly Metric-Based Rating) [abstract]. J Hosp Med. 2015;10(suppl 2).
Rivaroxaban Less Expensive for Low-Risk VTE
NEW YORK (Reuters Health) - For patients with low-risk venous thromboembolism (VTE) who can safely be discharged from the emergency department, rivaroxaban is a less costly treatment than heparin and warfarin, according to results of a case-control study.
"The biggest surprise to me was that using the Hestia criteria in the emergency department produced a low-enough risk population that we had zero incidence of either recurrent clots or bleeding," Dr. Jeffrey A. Kline, from Indiana University School of Medicine in Indianapolis, told Reuters Health by email. "The second surprise was the strength of gratitude by the patients that they did not have to have injections and take warfarin."
Dr. Kline's team developed a protocol for home treatment of low-risk patients with VTE using a target-specific anticoagulant like rivaroxaban. They compared the costs of medical care accrued by 50 patients treated with rivaroxaban and 47 matched controls who received bridging low-molecular-weight heparin (LMWH) for five to seven days and were then transitioned to warfarin.
All 50 rivaroxaban patients were discharged home from the emergency department on the day of diagnosis, whereas only 18 control patients were treated at home, according to the June 25 Academic Emergency Medicine online report.
Over the six months of follow-up, median total charges were $4787 with rivaroxaban, compared with $11,128 with LMWH-warfarin.
When the analysis was confined to patients who were never hospitalized, rivaroxaban was still less costly (median, $5932 vs $9016), although the difference was not statistically significant.
In-patient pharmacy median charges were significantly less with rivaroxaban than with LMWH-warfarin (median, $215 vs $742), but a survey of hospital outpatient pharmacies found the median cash cost of rivaroxaban to be significantly higher than that of LMWH-warfarin ($1856 vs $724 for six months).
"In low-risk patients, target-specific anticoagulants require minimal maintenance, and patients can be managed with no coagulation testing at all, and almost no other laboratory monitoring unless other factors suggest anemia or a reason to suspect change in renal function," Dr. Kline said.
Dr. Nathan T. Connell, from Brigham and Women's Hospital in Boston, told Reuters Health by email, "Recently, there has been a lot of discussion about cost differences between various anticoagulation strategies. This paper helps put the cost in perspective and that treatment with rivaroxaban may be more cost-effective in the long term."
"This difference went away when hospitalized patients were removed from the analysis, suggesting that the cost of hospitalization was the major driver for cost difference between the two strategies," Dr. Connell said. "For well-selected low-risk patients, however, rivaroxaban is an attractive choice because it often allows direct discharge from the Emergency Department. Also, we know from other studies that the risk of certain types of serious bleeding, such as intracerebral hemorrhage, is lower with rivaroxaban as compared to warfarin."
Dr. Connell noted, "This is a retrospective study, which can have issues with selection bias. The authors took several steps to minimize this bias, such as matching on a comorbidity score, in an attempt to make sure the two comparison groups were as balanced as possible."
NEW YORK (Reuters Health) - For patients with low-risk venous thromboembolism (VTE) who can safely be discharged from the emergency department, rivaroxaban is a less costly treatment than heparin and warfarin, according to results of a case-control study.
"The biggest surprise to me was that using the Hestia criteria in the emergency department produced a low-enough risk population that we had zero incidence of either recurrent clots or bleeding," Dr. Jeffrey A. Kline, from Indiana University School of Medicine in Indianapolis, told Reuters Health by email. "The second surprise was the strength of gratitude by the patients that they did not have to have injections and take warfarin."
Dr. Kline's team developed a protocol for home treatment of low-risk patients with VTE using a target-specific anticoagulant like rivaroxaban. They compared the costs of medical care accrued by 50 patients treated with rivaroxaban and 47 matched controls who received bridging low-molecular-weight heparin (LMWH) for five to seven days and were then transitioned to warfarin.
All 50 rivaroxaban patients were discharged home from the emergency department on the day of diagnosis, whereas only 18 control patients were treated at home, according to the June 25 Academic Emergency Medicine online report.
Over the six months of follow-up, median total charges were $4787 with rivaroxaban, compared with $11,128 with LMWH-warfarin.
When the analysis was confined to patients who were never hospitalized, rivaroxaban was still less costly (median, $5932 vs $9016), although the difference was not statistically significant.
In-patient pharmacy median charges were significantly less with rivaroxaban than with LMWH-warfarin (median, $215 vs $742), but a survey of hospital outpatient pharmacies found the median cash cost of rivaroxaban to be significantly higher than that of LMWH-warfarin ($1856 vs $724 for six months).
"In low-risk patients, target-specific anticoagulants require minimal maintenance, and patients can be managed with no coagulation testing at all, and almost no other laboratory monitoring unless other factors suggest anemia or a reason to suspect change in renal function," Dr. Kline said.
Dr. Nathan T. Connell, from Brigham and Women's Hospital in Boston, told Reuters Health by email, "Recently, there has been a lot of discussion about cost differences between various anticoagulation strategies. This paper helps put the cost in perspective and that treatment with rivaroxaban may be more cost-effective in the long term."
"This difference went away when hospitalized patients were removed from the analysis, suggesting that the cost of hospitalization was the major driver for cost difference between the two strategies," Dr. Connell said. "For well-selected low-risk patients, however, rivaroxaban is an attractive choice because it often allows direct discharge from the Emergency Department. Also, we know from other studies that the risk of certain types of serious bleeding, such as intracerebral hemorrhage, is lower with rivaroxaban as compared to warfarin."
Dr. Connell noted, "This is a retrospective study, which can have issues with selection bias. The authors took several steps to minimize this bias, such as matching on a comorbidity score, in an attempt to make sure the two comparison groups were as balanced as possible."
NEW YORK (Reuters Health) - For patients with low-risk venous thromboembolism (VTE) who can safely be discharged from the emergency department, rivaroxaban is a less costly treatment than heparin and warfarin, according to results of a case-control study.
"The biggest surprise to me was that using the Hestia criteria in the emergency department produced a low-enough risk population that we had zero incidence of either recurrent clots or bleeding," Dr. Jeffrey A. Kline, from Indiana University School of Medicine in Indianapolis, told Reuters Health by email. "The second surprise was the strength of gratitude by the patients that they did not have to have injections and take warfarin."
Dr. Kline's team developed a protocol for home treatment of low-risk patients with VTE using a target-specific anticoagulant like rivaroxaban. They compared the costs of medical care accrued by 50 patients treated with rivaroxaban and 47 matched controls who received bridging low-molecular-weight heparin (LMWH) for five to seven days and were then transitioned to warfarin.
All 50 rivaroxaban patients were discharged home from the emergency department on the day of diagnosis, whereas only 18 control patients were treated at home, according to the June 25 Academic Emergency Medicine online report.
Over the six months of follow-up, median total charges were $4787 with rivaroxaban, compared with $11,128 with LMWH-warfarin.
When the analysis was confined to patients who were never hospitalized, rivaroxaban was still less costly (median, $5932 vs $9016), although the difference was not statistically significant.
In-patient pharmacy median charges were significantly less with rivaroxaban than with LMWH-warfarin (median, $215 vs $742), but a survey of hospital outpatient pharmacies found the median cash cost of rivaroxaban to be significantly higher than that of LMWH-warfarin ($1856 vs $724 for six months).
"In low-risk patients, target-specific anticoagulants require minimal maintenance, and patients can be managed with no coagulation testing at all, and almost no other laboratory monitoring unless other factors suggest anemia or a reason to suspect change in renal function," Dr. Kline said.
Dr. Nathan T. Connell, from Brigham and Women's Hospital in Boston, told Reuters Health by email, "Recently, there has been a lot of discussion about cost differences between various anticoagulation strategies. This paper helps put the cost in perspective and that treatment with rivaroxaban may be more cost-effective in the long term."
"This difference went away when hospitalized patients were removed from the analysis, suggesting that the cost of hospitalization was the major driver for cost difference between the two strategies," Dr. Connell said. "For well-selected low-risk patients, however, rivaroxaban is an attractive choice because it often allows direct discharge from the Emergency Department. Also, we know from other studies that the risk of certain types of serious bleeding, such as intracerebral hemorrhage, is lower with rivaroxaban as compared to warfarin."
Dr. Connell noted, "This is a retrospective study, which can have issues with selection bias. The authors took several steps to minimize this bias, such as matching on a comorbidity score, in an attempt to make sure the two comparison groups were as balanced as possible."