User login
6 Tips for Community Hospitalists Initiating QI Projects
The Society of Hospital Medicine asserts that one of the key principles of an effective hospital medicine group is demonstrating a commitment to continuous quality improvement (QI) and actively participating in initiatives directed at quality and patient safety.1 Large hospitalist groups expect their physicians to contribute to the QI initiatives of the hospitals they staff. But as any hospitalist practicing in a community setting can tell you, QI is much easier said than done.
Acknowledge, Overcome the Obstacles
One of the first hurdles hospitalists must overcome when initiating a QI program is finding the time in their schedule as well as obtaining the time commitment from group leadership and fellow clinicians.
“If a hospitalist has no dedicated time and is working clinically, it is difficult to find time to organize a study,” says Kenneth Epstein, MD, chief medical officer of Hospitalist Consultants, the hospitalist management division of ECI Healthcare Partners, in Traverse City, Mich.
However, many national hospitalist management groups, including ECI and IPC Healthcare of North Hollywood, Calif., expect their clinicians to be continuously engaged in QI projects relative to their facility.
Beyond time, an even tougher obstacle to surmount is a lack of training, according to Kerry Weiner, MD, IPC chief medical officer. He says that each of IPC’s clinical practice leaders must participate in a one-year training program that includes a QI project conducted within their facility and mentored by University of California, San Francisco faculty.
David Nash, MD, founding dean of Jefferson College of Population Health in Philadelphia, says The Joint Commission, as part of its accreditation process, requires hospitals to robustly review errors and “have a performance improvement system in place.” He believes the only way community hospitals can successfully undertake this effort is to make sure hospitalists have adequate training in quality and safety.
Training is available from SHM via its Quality and Safety Educators Academy as well as the American Association for Physician Leadership and the Institute for Healthcare Improvement. However, Dr. Nash recommends graduate-level programs in quality and safety available at several schools including Jefferson, Northwestern University in Chicago, and George Washington University in Washington, D.C.
Yet another hurdle is access to data. Many community hospitals have limited financial and human resources to collect accurate data to use for choosing an area to focus on and measuring improvement.
“Despite all the money invested in electronic medical records, finding timely and accurate data is still challenging,” says Jasen Gundersen, MD, president of Knoxville, Tenn.–based TeamHealth Acute Care Services. “The data may exist, but a community hospital may be limited when it comes to finding people to mine, configure, and analyze the data. Community hospitals tend to be focused on publically reported, whole-hospital data.
“If your project is not related to these metrics, you may have trouble getting quality department support.”
Dr. Weiner echoes that sentiment, noting most community hospitals “react to bad metrics, such as low HCAHPS scores. To get the most support possible,” he says, “design a QI program that people see as a genuine problem that needs to be fixed using their resources.”
Get Involved
Experience is another barrier to community-based QI projects. Dr. Gundersen believes that hospitalists who want to get involved in quality should first join a QI committee.
“One of the best ways to effect change in a hospital is to get to know the players—who’s who, who does what, and who is willing to help,” he says.
Arnu Mohan, MD, chief medical officer of hospital medicine at ApolloMD in Atlanta, agrees with gaining experience before setting out on your own.
“Joining a QI committee is almost never a bad idea,” Dr. Mohan says. “You’ll meet people who can support your work, get insight into the needs of the institution, be exposed to other work being done, and better understand the resources available.”
Choose Your Project Carefully
Dr. Gundersen recommends that before settling on a QI project, hospitalists should first consider what their career goals are.
“Ask yourself why you want to do it,” he says. “Do you have the ambition to become a medical director or chief quality officer? In that case, you need a few QI projects under your belt, and you want to choose a system-wide project. Or is there just something in your everyday life that frustrates you so much you must fix it?”
If the project that compels the clinician is not aligned with the needs of the hospital, “it is worthy of a discussion to make sure you are working on the right project,” he adds. “Is the hospitalist off base, or does the administration need to pay more attention to what is happening on the floor?”
Obtain Buy-in
A QI project has a greater chance at being successful if the participants have a high level of interest in the initiative and there is visible support from the administration: high-level people making public statements, making appearances at QI team meetings, and diverting resources such as information technology and process mapping support to sustain the project. This will only happen if community-based hospitalists are successful at selling their project to the C-suite.
“When you approach senior management, you have only 15 minutes to get their attention about your project,” Dr. Weiner says. “You need to show them that you are bringing part of the solution and your idea will affect their bottom line.”
Jeff Brady, MD, director of the Center for Quality Improvement and Patient Safety, says organization commitment is key to any patient safety initiative.
“In addition to the active engagement of leaders who focus on safety and quality, an organization’s culture is another factor that can either enable or thwart progress toward improving the care they deliver,” he says. “AHRQ [the Agency for Healthcare Research and Quality] developed a collection of instruments—AHRQ Surveys on Patient Safety Culture—to help organizations assess and better understand facilitators and barriers their organizations may encounter as they work to improve safety and quality.”2
Politics also can be a factor. Dr. Gundersen points out that smaller hospitals typically are used to “doing things one way.”
“They may not be receptive to changes a QI program would initiate,” he says. “You have to figure out a way to enlist people to move the project forward. Your ability to drive and influence change may be your most important quality as a physician leader.”
Dr. Mohan believes that the best approach is to find a mentor who has worked on QI initiatives before and can champion your efforts.
“You will need the support of the hospital to access required data, change processes, and implement new tools,” he says. “Many hospitals will have a chief medical officer, chief quality officer, or director of QI who can serve as an important ally to mobilize resources on your behalf.”
Go Beyond Hospital Medicine
Even with administrative support, it is better to assemble a team than attempt to go it alone. Successful QI projects, Dr. Mohan says, tend to be team efforts.
“Finding a community of people who will support your work is critical,” he adds. “A multidisciplinary team, including areas such as nursing, therapy, and administration, that engages people who will complement one another increases the likelihood of success.
“That said, multidisciplinary teams have their challenges. They can be unwieldy to lead and without clear roles and responsibilities. I would recommend a group of two to five people who are passionate about the issue you are trying to solve. And be clear from the beginning what each person’s role is within the group.”
Support can also be found in areas outside of the medical staff.
“Key people in other hospital departments can assist with supplying data, financial solutions, and institutional support,” Dr. Mohan says. “These people may be in various departments, such as quality improvement and case management.
“In the current era of value-based purchasing, where Medicare reimbursement is tied to quality metrics, it’s advantageous to show potential financial impact of the QI initiative on hospital revenue, so assistance by the CFO or others in finance may be helpful.”
Dr. Gundersen suggests hospitalists seek out a “lateral mentor,” someone in a department outside the medical staff who is looking for change and can offer resources.
“For example, physicians are looking for quality improvement, and those in the finance department are looking for good economic return. Physicians can explain medical reasons things need to be done, and the finance people can explain the impact of these choices,” he says. “Working together, they can improve both quality and the bottom line.”
Lateral mentoring also is an effective way to meet the challenge of obtaining accurate data, as it opens up the potential to mine data from various departments.
“At different institutions, data may reside in different departments,” Dr. Epstein says. “For example, patient satisfaction may reside with the CMO, core measures or readmissions may reside with the quality management department, and length of stay may be the purview of the finance department.”
Connections in other departments could be the source of your best data, according to Dr. Epstein.
Consider Incentives, Penalties
In addition to buy-in from administration and professionals in other departments, hospitalists also need the commitment of fellow clinicians. Dr. Weiner believes the only way to do this is through financial incentives.
“In a community setting, start with a meaningful reward for improvement. It must be enough that the hospitalist makes the QI project a priority,” he says.
Dr. Weiner also recommends a small penalty for non-participation.
“Most providers realize QI is just good practice, but for some individuals, you need a consequence. It must be part of the system so it isn’t personal,” Dr. Weiner says. “One way is to mandate that if you do not participate, not only do you not get any of the incentive pay, you might lose some of a productivity bonus. You need to be creative when thinking about how to promote QI.”
In the community hospital setting, Dr. Weiner says, practicality ultimately rules.
“The community hospital has real problems to deal with, so don’t make your project pie-in-the-sky,” he says. “Tie it to the bottom line of the hospital if you can. That’s where you start.” TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Cawley P, Deitelzweig S, Flores L. The key principles and characteristics of an effective hospital medicine group: as assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9:123-128.
- Surveys on patient safety culture. AHRQ website. Accessed October 12, 2015.
- AHRQ Quality Indicators Toolkit for Hospitals: fact sheet. AHRQ website. Accessed October 10, 2015.
- Practice facilitation handbook. AHRQ website. Accessed on September 25, 2015.
- 5. SHM signature programs. SHM website. Accessed October 10, 2015.
The Society of Hospital Medicine asserts that one of the key principles of an effective hospital medicine group is demonstrating a commitment to continuous quality improvement (QI) and actively participating in initiatives directed at quality and patient safety.1 Large hospitalist groups expect their physicians to contribute to the QI initiatives of the hospitals they staff. But as any hospitalist practicing in a community setting can tell you, QI is much easier said than done.
Acknowledge, Overcome the Obstacles
One of the first hurdles hospitalists must overcome when initiating a QI program is finding the time in their schedule as well as obtaining the time commitment from group leadership and fellow clinicians.
“If a hospitalist has no dedicated time and is working clinically, it is difficult to find time to organize a study,” says Kenneth Epstein, MD, chief medical officer of Hospitalist Consultants, the hospitalist management division of ECI Healthcare Partners, in Traverse City, Mich.
However, many national hospitalist management groups, including ECI and IPC Healthcare of North Hollywood, Calif., expect their clinicians to be continuously engaged in QI projects relative to their facility.
Beyond time, an even tougher obstacle to surmount is a lack of training, according to Kerry Weiner, MD, IPC chief medical officer. He says that each of IPC’s clinical practice leaders must participate in a one-year training program that includes a QI project conducted within their facility and mentored by University of California, San Francisco faculty.
David Nash, MD, founding dean of Jefferson College of Population Health in Philadelphia, says The Joint Commission, as part of its accreditation process, requires hospitals to robustly review errors and “have a performance improvement system in place.” He believes the only way community hospitals can successfully undertake this effort is to make sure hospitalists have adequate training in quality and safety.
Training is available from SHM via its Quality and Safety Educators Academy as well as the American Association for Physician Leadership and the Institute for Healthcare Improvement. However, Dr. Nash recommends graduate-level programs in quality and safety available at several schools including Jefferson, Northwestern University in Chicago, and George Washington University in Washington, D.C.
Yet another hurdle is access to data. Many community hospitals have limited financial and human resources to collect accurate data to use for choosing an area to focus on and measuring improvement.
“Despite all the money invested in electronic medical records, finding timely and accurate data is still challenging,” says Jasen Gundersen, MD, president of Knoxville, Tenn.–based TeamHealth Acute Care Services. “The data may exist, but a community hospital may be limited when it comes to finding people to mine, configure, and analyze the data. Community hospitals tend to be focused on publically reported, whole-hospital data.
“If your project is not related to these metrics, you may have trouble getting quality department support.”
Dr. Weiner echoes that sentiment, noting most community hospitals “react to bad metrics, such as low HCAHPS scores. To get the most support possible,” he says, “design a QI program that people see as a genuine problem that needs to be fixed using their resources.”
Get Involved
Experience is another barrier to community-based QI projects. Dr. Gundersen believes that hospitalists who want to get involved in quality should first join a QI committee.
“One of the best ways to effect change in a hospital is to get to know the players—who’s who, who does what, and who is willing to help,” he says.
Arnu Mohan, MD, chief medical officer of hospital medicine at ApolloMD in Atlanta, agrees with gaining experience before setting out on your own.
“Joining a QI committee is almost never a bad idea,” Dr. Mohan says. “You’ll meet people who can support your work, get insight into the needs of the institution, be exposed to other work being done, and better understand the resources available.”
Choose Your Project Carefully
Dr. Gundersen recommends that before settling on a QI project, hospitalists should first consider what their career goals are.
“Ask yourself why you want to do it,” he says. “Do you have the ambition to become a medical director or chief quality officer? In that case, you need a few QI projects under your belt, and you want to choose a system-wide project. Or is there just something in your everyday life that frustrates you so much you must fix it?”
If the project that compels the clinician is not aligned with the needs of the hospital, “it is worthy of a discussion to make sure you are working on the right project,” he adds. “Is the hospitalist off base, or does the administration need to pay more attention to what is happening on the floor?”
Obtain Buy-in
A QI project has a greater chance at being successful if the participants have a high level of interest in the initiative and there is visible support from the administration: high-level people making public statements, making appearances at QI team meetings, and diverting resources such as information technology and process mapping support to sustain the project. This will only happen if community-based hospitalists are successful at selling their project to the C-suite.
“When you approach senior management, you have only 15 minutes to get their attention about your project,” Dr. Weiner says. “You need to show them that you are bringing part of the solution and your idea will affect their bottom line.”
Jeff Brady, MD, director of the Center for Quality Improvement and Patient Safety, says organization commitment is key to any patient safety initiative.
“In addition to the active engagement of leaders who focus on safety and quality, an organization’s culture is another factor that can either enable or thwart progress toward improving the care they deliver,” he says. “AHRQ [the Agency for Healthcare Research and Quality] developed a collection of instruments—AHRQ Surveys on Patient Safety Culture—to help organizations assess and better understand facilitators and barriers their organizations may encounter as they work to improve safety and quality.”2
Politics also can be a factor. Dr. Gundersen points out that smaller hospitals typically are used to “doing things one way.”
“They may not be receptive to changes a QI program would initiate,” he says. “You have to figure out a way to enlist people to move the project forward. Your ability to drive and influence change may be your most important quality as a physician leader.”
Dr. Mohan believes that the best approach is to find a mentor who has worked on QI initiatives before and can champion your efforts.
“You will need the support of the hospital to access required data, change processes, and implement new tools,” he says. “Many hospitals will have a chief medical officer, chief quality officer, or director of QI who can serve as an important ally to mobilize resources on your behalf.”
Go Beyond Hospital Medicine
Even with administrative support, it is better to assemble a team than attempt to go it alone. Successful QI projects, Dr. Mohan says, tend to be team efforts.
“Finding a community of people who will support your work is critical,” he adds. “A multidisciplinary team, including areas such as nursing, therapy, and administration, that engages people who will complement one another increases the likelihood of success.
“That said, multidisciplinary teams have their challenges. They can be unwieldy to lead and without clear roles and responsibilities. I would recommend a group of two to five people who are passionate about the issue you are trying to solve. And be clear from the beginning what each person’s role is within the group.”
Support can also be found in areas outside of the medical staff.
“Key people in other hospital departments can assist with supplying data, financial solutions, and institutional support,” Dr. Mohan says. “These people may be in various departments, such as quality improvement and case management.
“In the current era of value-based purchasing, where Medicare reimbursement is tied to quality metrics, it’s advantageous to show potential financial impact of the QI initiative on hospital revenue, so assistance by the CFO or others in finance may be helpful.”
Dr. Gundersen suggests hospitalists seek out a “lateral mentor,” someone in a department outside the medical staff who is looking for change and can offer resources.
“For example, physicians are looking for quality improvement, and those in the finance department are looking for good economic return. Physicians can explain medical reasons things need to be done, and the finance people can explain the impact of these choices,” he says. “Working together, they can improve both quality and the bottom line.”
Lateral mentoring also is an effective way to meet the challenge of obtaining accurate data, as it opens up the potential to mine data from various departments.
“At different institutions, data may reside in different departments,” Dr. Epstein says. “For example, patient satisfaction may reside with the CMO, core measures or readmissions may reside with the quality management department, and length of stay may be the purview of the finance department.”
Connections in other departments could be the source of your best data, according to Dr. Epstein.
Consider Incentives, Penalties
In addition to buy-in from administration and professionals in other departments, hospitalists also need the commitment of fellow clinicians. Dr. Weiner believes the only way to do this is through financial incentives.
“In a community setting, start with a meaningful reward for improvement. It must be enough that the hospitalist makes the QI project a priority,” he says.
Dr. Weiner also recommends a small penalty for non-participation.
“Most providers realize QI is just good practice, but for some individuals, you need a consequence. It must be part of the system so it isn’t personal,” Dr. Weiner says. “One way is to mandate that if you do not participate, not only do you not get any of the incentive pay, you might lose some of a productivity bonus. You need to be creative when thinking about how to promote QI.”
In the community hospital setting, Dr. Weiner says, practicality ultimately rules.
“The community hospital has real problems to deal with, so don’t make your project pie-in-the-sky,” he says. “Tie it to the bottom line of the hospital if you can. That’s where you start.” TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Cawley P, Deitelzweig S, Flores L. The key principles and characteristics of an effective hospital medicine group: as assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9:123-128.
- Surveys on patient safety culture. AHRQ website. Accessed October 12, 2015.
- AHRQ Quality Indicators Toolkit for Hospitals: fact sheet. AHRQ website. Accessed October 10, 2015.
- Practice facilitation handbook. AHRQ website. Accessed on September 25, 2015.
- 5. SHM signature programs. SHM website. Accessed October 10, 2015.
The Society of Hospital Medicine asserts that one of the key principles of an effective hospital medicine group is demonstrating a commitment to continuous quality improvement (QI) and actively participating in initiatives directed at quality and patient safety.1 Large hospitalist groups expect their physicians to contribute to the QI initiatives of the hospitals they staff. But as any hospitalist practicing in a community setting can tell you, QI is much easier said than done.
Acknowledge, Overcome the Obstacles
One of the first hurdles hospitalists must overcome when initiating a QI program is finding the time in their schedule as well as obtaining the time commitment from group leadership and fellow clinicians.
“If a hospitalist has no dedicated time and is working clinically, it is difficult to find time to organize a study,” says Kenneth Epstein, MD, chief medical officer of Hospitalist Consultants, the hospitalist management division of ECI Healthcare Partners, in Traverse City, Mich.
However, many national hospitalist management groups, including ECI and IPC Healthcare of North Hollywood, Calif., expect their clinicians to be continuously engaged in QI projects relative to their facility.
Beyond time, an even tougher obstacle to surmount is a lack of training, according to Kerry Weiner, MD, IPC chief medical officer. He says that each of IPC’s clinical practice leaders must participate in a one-year training program that includes a QI project conducted within their facility and mentored by University of California, San Francisco faculty.
David Nash, MD, founding dean of Jefferson College of Population Health in Philadelphia, says The Joint Commission, as part of its accreditation process, requires hospitals to robustly review errors and “have a performance improvement system in place.” He believes the only way community hospitals can successfully undertake this effort is to make sure hospitalists have adequate training in quality and safety.
Training is available from SHM via its Quality and Safety Educators Academy as well as the American Association for Physician Leadership and the Institute for Healthcare Improvement. However, Dr. Nash recommends graduate-level programs in quality and safety available at several schools including Jefferson, Northwestern University in Chicago, and George Washington University in Washington, D.C.
Yet another hurdle is access to data. Many community hospitals have limited financial and human resources to collect accurate data to use for choosing an area to focus on and measuring improvement.
“Despite all the money invested in electronic medical records, finding timely and accurate data is still challenging,” says Jasen Gundersen, MD, president of Knoxville, Tenn.–based TeamHealth Acute Care Services. “The data may exist, but a community hospital may be limited when it comes to finding people to mine, configure, and analyze the data. Community hospitals tend to be focused on publically reported, whole-hospital data.
“If your project is not related to these metrics, you may have trouble getting quality department support.”
Dr. Weiner echoes that sentiment, noting most community hospitals “react to bad metrics, such as low HCAHPS scores. To get the most support possible,” he says, “design a QI program that people see as a genuine problem that needs to be fixed using their resources.”
Get Involved
Experience is another barrier to community-based QI projects. Dr. Gundersen believes that hospitalists who want to get involved in quality should first join a QI committee.
“One of the best ways to effect change in a hospital is to get to know the players—who’s who, who does what, and who is willing to help,” he says.
Arnu Mohan, MD, chief medical officer of hospital medicine at ApolloMD in Atlanta, agrees with gaining experience before setting out on your own.
“Joining a QI committee is almost never a bad idea,” Dr. Mohan says. “You’ll meet people who can support your work, get insight into the needs of the institution, be exposed to other work being done, and better understand the resources available.”
Choose Your Project Carefully
Dr. Gundersen recommends that before settling on a QI project, hospitalists should first consider what their career goals are.
“Ask yourself why you want to do it,” he says. “Do you have the ambition to become a medical director or chief quality officer? In that case, you need a few QI projects under your belt, and you want to choose a system-wide project. Or is there just something in your everyday life that frustrates you so much you must fix it?”
If the project that compels the clinician is not aligned with the needs of the hospital, “it is worthy of a discussion to make sure you are working on the right project,” he adds. “Is the hospitalist off base, or does the administration need to pay more attention to what is happening on the floor?”
Obtain Buy-in
A QI project has a greater chance at being successful if the participants have a high level of interest in the initiative and there is visible support from the administration: high-level people making public statements, making appearances at QI team meetings, and diverting resources such as information technology and process mapping support to sustain the project. This will only happen if community-based hospitalists are successful at selling their project to the C-suite.
“When you approach senior management, you have only 15 minutes to get their attention about your project,” Dr. Weiner says. “You need to show them that you are bringing part of the solution and your idea will affect their bottom line.”
Jeff Brady, MD, director of the Center for Quality Improvement and Patient Safety, says organization commitment is key to any patient safety initiative.
“In addition to the active engagement of leaders who focus on safety and quality, an organization’s culture is another factor that can either enable or thwart progress toward improving the care they deliver,” he says. “AHRQ [the Agency for Healthcare Research and Quality] developed a collection of instruments—AHRQ Surveys on Patient Safety Culture—to help organizations assess and better understand facilitators and barriers their organizations may encounter as they work to improve safety and quality.”2
Politics also can be a factor. Dr. Gundersen points out that smaller hospitals typically are used to “doing things one way.”
“They may not be receptive to changes a QI program would initiate,” he says. “You have to figure out a way to enlist people to move the project forward. Your ability to drive and influence change may be your most important quality as a physician leader.”
Dr. Mohan believes that the best approach is to find a mentor who has worked on QI initiatives before and can champion your efforts.
“You will need the support of the hospital to access required data, change processes, and implement new tools,” he says. “Many hospitals will have a chief medical officer, chief quality officer, or director of QI who can serve as an important ally to mobilize resources on your behalf.”
Go Beyond Hospital Medicine
Even with administrative support, it is better to assemble a team than attempt to go it alone. Successful QI projects, Dr. Mohan says, tend to be team efforts.
“Finding a community of people who will support your work is critical,” he adds. “A multidisciplinary team, including areas such as nursing, therapy, and administration, that engages people who will complement one another increases the likelihood of success.
“That said, multidisciplinary teams have their challenges. They can be unwieldy to lead and without clear roles and responsibilities. I would recommend a group of two to five people who are passionate about the issue you are trying to solve. And be clear from the beginning what each person’s role is within the group.”
Support can also be found in areas outside of the medical staff.
“Key people in other hospital departments can assist with supplying data, financial solutions, and institutional support,” Dr. Mohan says. “These people may be in various departments, such as quality improvement and case management.
“In the current era of value-based purchasing, where Medicare reimbursement is tied to quality metrics, it’s advantageous to show potential financial impact of the QI initiative on hospital revenue, so assistance by the CFO or others in finance may be helpful.”
Dr. Gundersen suggests hospitalists seek out a “lateral mentor,” someone in a department outside the medical staff who is looking for change and can offer resources.
“For example, physicians are looking for quality improvement, and those in the finance department are looking for good economic return. Physicians can explain medical reasons things need to be done, and the finance people can explain the impact of these choices,” he says. “Working together, they can improve both quality and the bottom line.”
Lateral mentoring also is an effective way to meet the challenge of obtaining accurate data, as it opens up the potential to mine data from various departments.
“At different institutions, data may reside in different departments,” Dr. Epstein says. “For example, patient satisfaction may reside with the CMO, core measures or readmissions may reside with the quality management department, and length of stay may be the purview of the finance department.”
Connections in other departments could be the source of your best data, according to Dr. Epstein.
Consider Incentives, Penalties
In addition to buy-in from administration and professionals in other departments, hospitalists also need the commitment of fellow clinicians. Dr. Weiner believes the only way to do this is through financial incentives.
“In a community setting, start with a meaningful reward for improvement. It must be enough that the hospitalist makes the QI project a priority,” he says.
Dr. Weiner also recommends a small penalty for non-participation.
“Most providers realize QI is just good practice, but for some individuals, you need a consequence. It must be part of the system so it isn’t personal,” Dr. Weiner says. “One way is to mandate that if you do not participate, not only do you not get any of the incentive pay, you might lose some of a productivity bonus. You need to be creative when thinking about how to promote QI.”
In the community hospital setting, Dr. Weiner says, practicality ultimately rules.
“The community hospital has real problems to deal with, so don’t make your project pie-in-the-sky,” he says. “Tie it to the bottom line of the hospital if you can. That’s where you start.” TH
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Cawley P, Deitelzweig S, Flores L. The key principles and characteristics of an effective hospital medicine group: as assessment guide for hospitals and hospitalists. J Hosp Med. 2014;9:123-128.
- Surveys on patient safety culture. AHRQ website. Accessed October 12, 2015.
- AHRQ Quality Indicators Toolkit for Hospitals: fact sheet. AHRQ website. Accessed October 10, 2015.
- Practice facilitation handbook. AHRQ website. Accessed on September 25, 2015.
- 5. SHM signature programs. SHM website. Accessed October 10, 2015.
Using Brochures, Business Cards to Make Personal Connection with Patients
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
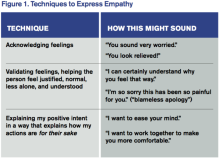
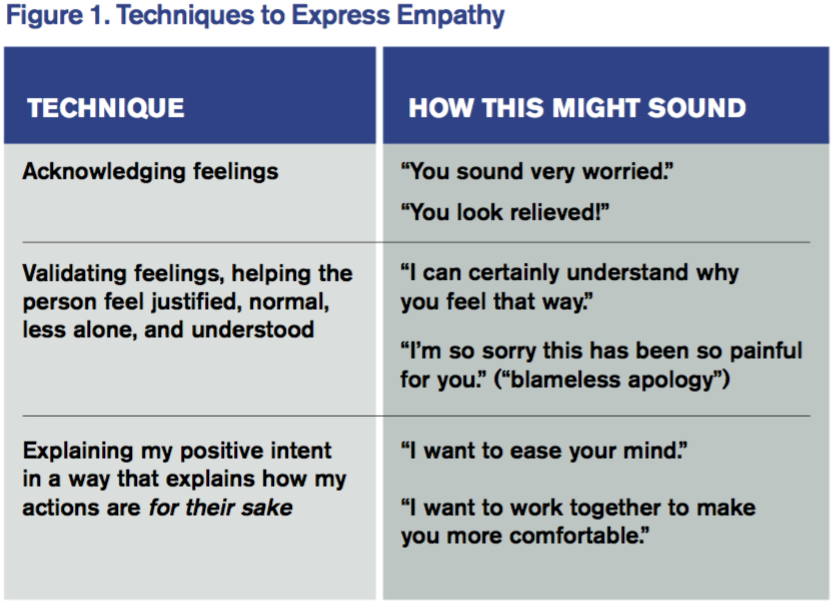
View a chart outlining key communication tactics
What I Say and Do
I sit down at patients’ eye level during patient visits and use a team brochure/personal business card for all new patients.
Why I Do It
One of the major concerns expressed by patients is the time spent with them by their provider. Sitting down at patients’ eye level lets them know that you are not in a hurry and you are there to give them whatever time they need. Sitting also causes your patients to perceive that you spent more time with them than if you spent the same amount of time while standing. This practice is not only advocated by patient-care consultants but is something I had reinforced during my firsthand experience as a patient several years ago when I had a surgical procedure. Every time the surgeon came into my hospital room, he sat in the chair, leisurely crossed his legs, and spoke to me from that position while writing in the chart. I knew exactly what he was doing, and it still made a difference to me! It put me more at ease and made me feel that he was there for me, ready to give me whatever time I needed and answer any questions that I had (and I had them). Sitting also puts you on an even level with your patients so they feel that you are talking with them, not down to them. This eases tension, adds comfort and trust to the situation, and is much more engaging.
How I Do It
After I greet patients, I look for a place to sit. If there is a chair, I pull it over to the bedside, sit in a relaxed manner, and continue the visit. If there is no chair in the room, I will sit on the windowsill, the bedside table (I have even been known to lower the bedside tray table and sit on the end with the support post if there is room on it), or whatever I can utilize to physically put myself on patients’ level. As a last resort, as long as there is not an isolatable infection, I will ask permission to sit on the edge of the bed. I make a point of telling them during this process that I am looking for a place to sit and talk so that they know this is my goal.
After the initial conversation and exam, if the patients are new to the service, I walk them through our team brochure and reiterate how we act as their PCP in the hospital and how we communicate with their PCP. I also make a point to show the team photo roster, which personalizes our team to patients, and say, “I also want you to have one of my baseball cards. We call our business cards ‘baseball cards’ because they have our pictures and a lot of ‘stats’ on them: our training, personal interests. That way, you know more about the person who is helping to take care of you.” I almost always see these cards out on patients’ trays or bedside tables on subsequent visits. Patients seem appreciative of the cards and the information. If I see another provider’s baseball card, I will ask patients a question about that provider as a way to continue to foster relations between our patients and our team. The more our patients can relate to us, the more they will trust us and the better their experience will be. TH
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
View a chart outlining key communication tactics
What I Say and Do
I sit down at patients’ eye level during patient visits and use a team brochure/personal business card for all new patients.
Why I Do It
One of the major concerns expressed by patients is the time spent with them by their provider. Sitting down at patients’ eye level lets them know that you are not in a hurry and you are there to give them whatever time they need. Sitting also causes your patients to perceive that you spent more time with them than if you spent the same amount of time while standing. This practice is not only advocated by patient-care consultants but is something I had reinforced during my firsthand experience as a patient several years ago when I had a surgical procedure. Every time the surgeon came into my hospital room, he sat in the chair, leisurely crossed his legs, and spoke to me from that position while writing in the chart. I knew exactly what he was doing, and it still made a difference to me! It put me more at ease and made me feel that he was there for me, ready to give me whatever time I needed and answer any questions that I had (and I had them). Sitting also puts you on an even level with your patients so they feel that you are talking with them, not down to them. This eases tension, adds comfort and trust to the situation, and is much more engaging.
How I Do It
After I greet patients, I look for a place to sit. If there is a chair, I pull it over to the bedside, sit in a relaxed manner, and continue the visit. If there is no chair in the room, I will sit on the windowsill, the bedside table (I have even been known to lower the bedside tray table and sit on the end with the support post if there is room on it), or whatever I can utilize to physically put myself on patients’ level. As a last resort, as long as there is not an isolatable infection, I will ask permission to sit on the edge of the bed. I make a point of telling them during this process that I am looking for a place to sit and talk so that they know this is my goal.
After the initial conversation and exam, if the patients are new to the service, I walk them through our team brochure and reiterate how we act as their PCP in the hospital and how we communicate with their PCP. I also make a point to show the team photo roster, which personalizes our team to patients, and say, “I also want you to have one of my baseball cards. We call our business cards ‘baseball cards’ because they have our pictures and a lot of ‘stats’ on them: our training, personal interests. That way, you know more about the person who is helping to take care of you.” I almost always see these cards out on patients’ trays or bedside tables on subsequent visits. Patients seem appreciative of the cards and the information. If I see another provider’s baseball card, I will ask patients a question about that provider as a way to continue to foster relations between our patients and our team. The more our patients can relate to us, the more they will trust us and the better their experience will be. TH
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
View a chart outlining key communication tactics
What I Say and Do
I sit down at patients’ eye level during patient visits and use a team brochure/personal business card for all new patients.
Why I Do It
One of the major concerns expressed by patients is the time spent with them by their provider. Sitting down at patients’ eye level lets them know that you are not in a hurry and you are there to give them whatever time they need. Sitting also causes your patients to perceive that you spent more time with them than if you spent the same amount of time while standing. This practice is not only advocated by patient-care consultants but is something I had reinforced during my firsthand experience as a patient several years ago when I had a surgical procedure. Every time the surgeon came into my hospital room, he sat in the chair, leisurely crossed his legs, and spoke to me from that position while writing in the chart. I knew exactly what he was doing, and it still made a difference to me! It put me more at ease and made me feel that he was there for me, ready to give me whatever time I needed and answer any questions that I had (and I had them). Sitting also puts you on an even level with your patients so they feel that you are talking with them, not down to them. This eases tension, adds comfort and trust to the situation, and is much more engaging.
How I Do It
After I greet patients, I look for a place to sit. If there is a chair, I pull it over to the bedside, sit in a relaxed manner, and continue the visit. If there is no chair in the room, I will sit on the windowsill, the bedside table (I have even been known to lower the bedside tray table and sit on the end with the support post if there is room on it), or whatever I can utilize to physically put myself on patients’ level. As a last resort, as long as there is not an isolatable infection, I will ask permission to sit on the edge of the bed. I make a point of telling them during this process that I am looking for a place to sit and talk so that they know this is my goal.
After the initial conversation and exam, if the patients are new to the service, I walk them through our team brochure and reiterate how we act as their PCP in the hospital and how we communicate with their PCP. I also make a point to show the team photo roster, which personalizes our team to patients, and say, “I also want you to have one of my baseball cards. We call our business cards ‘baseball cards’ because they have our pictures and a lot of ‘stats’ on them: our training, personal interests. That way, you know more about the person who is helping to take care of you.” I almost always see these cards out on patients’ trays or bedside tables on subsequent visits. Patients seem appreciative of the cards and the information. If I see another provider’s baseball card, I will ask patients a question about that provider as a way to continue to foster relations between our patients and our team. The more our patients can relate to us, the more they will trust us and the better their experience will be. TH
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla.
VIDEO: Is Hospital Medicine a Career Choice or a Pit Stop?
Dr. Scott Krugman, Chair of Pediatrics and Director of Medical Education at MedStar Franklin Square Medical Center in Baltimore, and Dr. Miguel Villagra, Medical Director of the Hospitalist Department at White River Medical Center in Batesville, AR talk about how residents and early career MDs process that decision.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Scott Krugman, Chair of Pediatrics and Director of Medical Education at MedStar Franklin Square Medical Center in Baltimore, and Dr. Miguel Villagra, Medical Director of the Hospitalist Department at White River Medical Center in Batesville, AR talk about how residents and early career MDs process that decision.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Scott Krugman, Chair of Pediatrics and Director of Medical Education at MedStar Franklin Square Medical Center in Baltimore, and Dr. Miguel Villagra, Medical Director of the Hospitalist Department at White River Medical Center in Batesville, AR talk about how residents and early career MDs process that decision.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HM Turns 20: A Look at the Evolution of Hospital Medicine
Editor's Note: Listen to Dr. Goldman, Dr. Wachter, Dr. Gandhi, Dr. Bessler, Dr. Gorman, and Dr. Merlino share more of their views on hospital medicine.
When Lee Goldman, MD, became chair of medicine at the University of California at San Francisco (UCSF) in January 1995, the construct of the medical service wasn’t all that different from when he had left as a resident 20 years earlier.
“It was still largely one month a year attending,” he recalls. “A couple of people did two months, I think. Some physicians still took care of their own patients even though there were teaching attending.”
Sure, it was an antiquated way to manage inpatient care, but since it had worked well enough for decades, who was going to change it?
“I got the idea that we could do better than that,” Dr. Goldman says.
He was right.
Dr. Goldman lured a young physician over from San Francisco General Hospital. The guy was a rising star of sorts. Robert Wachter, MD, MHM, had helped run the International AIDS Conference, held in the City by the Bay in 1990. He joined the faculty at San Francisco General that year and two years later became UCSF’s residency program director.
Then, Dr. Goldman asked Dr. Wachter to take on a new role as chief of the medical center at UCSF Medical Center. The charge was simple: “Come up with a new and innovative model by which fewer, selected faculty each spent multiple months as inpatient attendings and teachers.”
The model Dr. Wachter settled on—internal medicine physicians who practice solely in the hospital—wasn’t entirely novel. He recalled an American College of Physicians (ACP) presentation at 7 a.m. on a Sunday in 1995, the sort of session most conventioneers choose sleep over. Also, some doctors nationwide, in Minnesota and Arizona, for instance, were hospital-based as healthcare maintenance organizations (HMOs) struggled to make care more efficient and less costly to provide.
But those efforts were few and far between. And they were nearly all in the community setting. No one had tried to staff inpatient services with committed generalists in an academic setting.
Until Dr. Wachter and Dr. Goldman.
On Aug. 15, 1996, their article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” was published in the New England Journal of Medicine (NEJM).
A burgeoning specialty was given a name.
Its practitioners were called “hospitalists.”
And the rest, as they say, is history.
The Early Days
The idea of hospital-based physicians seems obvious in the rubric of medical history. There are now an estimated 44,000 hospitalists nationwide. The Society of Hospital Medicine (SHM) bills itself as the fastest-growing specialty in healthcare.
But it wasn’t always this way.
The novelty of hospital-based practitioners taking over care for some or all inpatient admissions wasn’t immediately embraced as a positive paradigm shift. Just ask Rob Bessler, MD, chief executive officer of Sound Physicians of Tacoma, Wash., among the largest hospitalist management groups (HMGs) in the country, with more than 2,200 hospitalists, ED physicians, intensivists, and post-acute-care physicians.
When the NEJM piece bestowing a name on hospitalists was published, Dr. Bessler was just finishing medical school at Case Western Reserve University School of Medicine in Cleveland. He started out in private practice and immediately saw issues in how hospitalized patients were treated.
“As an ED physician, nobody wanted to admit my patients as they were too busy in their office. I felt that those docs that were practicing in the hospital were using evidence that was 15 years old from when they finished their training,” he says. “I raised my hand to the hospital CEO to do things differently.”
Pushback against a new model came from multiple stakeholders. For every Dr. Bessler who was interested in a new way of doing things, there were physicians worried about turf battles.
“Doctors in practice around the county were afraid that these hospitalists would become mandatory,” says Dr. Goldman, who now is Dean of the Faculties of Health Sciences and Medicine, and chief executive at Columbia University Medical Center in New York City. “Some states actually had medical societies that passed resolutions saying they couldn’t become mandatory.”
In the early days, there were more critics than advocates. Critical-care doctors were one group that was, at best, ambivalent about the new model.
“The biggest brush fire in the early days was with critical care, which kind of surprised me,” Dr. Wachter says. “But ICU doctors had spent a huge amount of energy in the prior 20 years establishing their role. When hospitalists came out and often began to manage ICU cases—usually collaboratively with intensivists and partly filling a massive national shortage in intensivists—the leaders of the critical-care field felt like we were encroaching on their turf.”
Perhaps the biggest concerns to hospital medicine in the beginning came from the residents at UCSF. Initially, residents worried—some aloud—that hospitalists would become too controlling and “take away their delegated and graduated autonomy,” Dr. Goldman recalls.
At a meeting with the medical residents, “some actually said this could be awful and maybe they shouldn’t have come here,” he says, “maybe they should tell the internship applicants this would be a bad place to come because they wouldn’t have much autonomy, and I still remember asking a specific question to them. ‘Imagine your mother is admitted to the medical service at the teaching hospital back home where you live. What’s the first question you would ask?’
“And someone raised their hand and said, ‘Who’s the doctor?’
“And I said, ‘You mean who’s the intern?’
“They said, ‘No.’
“I said, ‘Or who’s the ward resident?’
“They said, ‘No.’
“And then, ‘Who is the attending?’
“And they said, ‘Yes.’
“So I said, ‘We have to have a good answer to that question when Mom gets admitted. Now that we’ve figured out how to get Mom the best care, let’s figure out how to make this the best possible teaching service.’”
Dr. Wachter and Dr. Goldman also prepared for some fears that didn’t pan out. One was the clout of specialists who might oppose the new model.
Some “specialists worried that if hospitalists were more knowledgeable than once-a-month-a-year attendings, and knew more about what was going on, they would be less likely to consult a specialist,” Dr. Goldman explains, adding he and Dr. Wachter thought that would be an unintended consequence of HM. “If there was a reduction in requested consults, that expertise would somehow be lost.”
Dr. Wachter and other early leaders also worried that patients, used to continuity of care with their primary-care doctors, would not take well to hospitalists. Would patients revolt against the idea of a new doctor seeing them every day?
“Yes, there were patients who felt that they wanted to see their regular doctor in the hospital. But for every one of them, there was another one or two that said this actually worked better,” Dr. Wachter says.
Community Views
Of course, the early success and adoption of the model in academic settings didn’t necessarily translate to community settings. Former SHM President Mary Jo Gorman, MD, MBA, MHM, who had just completed her MBA at Washington University in St. Louis when the NEJM article was published, wrote a business plan for her degree on implementing a hospitalist-style program at her institution, SSM DePaul Health Center, also in St. Louis.
She didn’t use the terms “hospital medicine” or “hospitalist.” They didn’t exist yet.
She was writing about what she was witnessing in her hospital: primary-care physicians (PCPs) who no longer wanted to visit hospitals because there simply wasn’t enough to do and make the trip worthwhile. In addition, she saw many of those same doctors no longer wanting to pick up ED calls.
So she pitched a model (same as Dr. Wachter was doing on the West Coast) of having someone in the hospital dedicated to inpatients as their sole responsibility. A “vocal minority” rebelled.
“It was a battlefield,” she recounts. “No other way to describe it. There were multiple hospital committees that reviewed it. There were letters of protest to the hospitals.”
Two major complaints emerged early on, Dr. Gorman says. Number one was the notion that hospitalists were enablers, allowing PCPs to shirk their long-established duty of shepherding their patients’ care through the walls of their local hospital. Number two, ironically, was the opposite: PCPs who didn’t want to cede control of their patients also moonlit taking ED calls that could generate patients for their own practice.
“It didn’t shock me at the time because I had already made major changes in our intensive-care unit at the hospital, which were unpopular,” Dr. Gorman says, adding all of the changes were good for patients and produced “fabulous” results. “But it was new. And it was different. And people don’t like to change the status quo.”
Perfect Timing
The seeds of hospitalist practice were planted before the NEJM article published. But the NEJM audience was nationwide, even beyond American borders. And the playing field was set up particularly well, says James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division. In 1996, the AIDS crisis was full-blown and a particular burden in inpatient wards.
“It was before we really had any of these amazing drugs that have turned HIV/AIDS into a quiet disease as opposed to a killer,” Dr. Merlino says. “At least 50% of the patients on the floors that we were rotating through [then] had patients, unfortunately, who were succumbing to AIDS.”
Dr. Merlino says he’s proud of the specialists who rotated through the hospital rooms of AIDS patients. But so many disparate doctors with no “quarterback” to manage the process holistically meant consistency in treatment was generally lacking.
“The role of the hospitalist often is to take recommendations from a lot of different specialties and come up with the best plan for the patient,” says Tejal Gandhi, MD, MPH, CPPS, president and CEO of the National Patient Safety Foundation. “They’re the true patient advocate who is getting the cardiologist’s opinion, the rheumatologist’s opinion, and the surgeon’s opinion, and they come up with the best plan for the patient.”
Dr. Merlino has an even blunter viewpoint: “I reflect back on that and think today about what the hospitalist model brings to us; it is an amazing transformation on how the hospitalist model really delivers.”
That type of optimism permeated nascent hospitalist groups. But it was time to start proving the anecdotal stories. Nearly two years to the day after the Wachter/Goldman paper published, a team led by Herbert Diamond, MD, published “The Effect of Full-Time Faculty Hospitalists on the Efficiency of Care at a Community Teaching Hospital” in the Annals of Internal Medicine.1 It was among the first reports to show evidence that hospitalists improved care.
Results published in that article showed median length of stay (LOS) decreased to 5.01 days from 6.01 days (P<0.001). It showed median cost of care decreased to $3,552 from $4,139 (P<0.001), and the 14-day readmission rate decreased to 4.64 readmissions per 100 admissions from 9.9 per 100 (P<0.001). In the comparison groups, LOS decreased, but both cost of care and readmission rates increased.
The research was so early on that the paper’s background section noted that “hospitalists are increasingly being used for inpatient care.”
“What we found, of course, was that they were providing an excellent service. They were well-trained, and you could get hospital people instead of having family-practice people managing the patients,” says nurse practitioner Robert Donaldson, NPC, clinical director of emergency medicine at Ellenville Regional Hospital in upstate New York and a veteran of working alongside hospitalists since the specialty arrived in the late 1990s. “We were getting better throughput times, better receipt of patients from our emergency rooms, and, I think, better outcomes as well.”
Growth Spurt
The refrain was familiar across the country as HM spread from health system to health system. Early results were looking good. The model was taking hold in more hospitals, both academic and community. Initial research studies supported the premise that the model improved efficiency without compromising quality or patient experience.
“My feeling at the time was this was a good idea,” Dr. Wachter says. “The trend toward our system being pushed to deliver better, more efficient care was going to be enduring, and the old model of the primary-care doc being your hospital doc … couldn’t possibly achieve the goal of producing the highest value.”
Dr. Wachter and other early leaders pushed the field to become involved in systems-improvement work. This turned out to be prophetic in December 1999, when patient safety zoomed to the national forefront with the publication of the Institute of Medicine (IOM) report “To Err Is Human.” Its conclusions, by now, are well-known. It showed between 44,000 and 98,000 people a year die from preventable medical errors, the equivalent of a jumbo jet a day crashing.
The impact was profound, and safety initiatives became a focal point of hospitals. The federal Agency for Health Care Policy and Research was renamed the Agency for Healthcare Research and Quality (ARHQ) to indicate the change in focus.
“When the IOM report came out, it gave us a focus and a language that we didn’t have before,” says Dr. Wachter, who served as president of SHM’s Board of Directors and to this day lectures at SHM annual meetings. “But I think the general sensibility that hospitalists are about improving quality and safety and patients’ experience and efficiency—I think that was baked in from the start.”
Two years later, IOM followed up its safety push with “Crossing the Quality Chasm: A New Health System for the 21st Century.” The sequel study laid out focus areas and guidelines to start reducing the spate of medical mistakes that “To Err Is Human” lay bare.
Hospitalists were seen as people to lead the charge for safety because they were already taking care of patients, already focused on reducing LOS and improving care delivery—and never to be underestimated, they were omnipresent, Dr. Gandhi says of her experience with hospitalists around 2000 at Brigham and Women’s Hospital in Boston.
“At least where I was, hospitalists truly were leaders in the quality and safety space, and it was just a really good fit for the kind of mindset and personality of a hospitalist because they’re very much … integrators of care across hospitals,” she says. “They interface with so many different areas of the hospital and then try to make all of that work better.”
Revenue Rules the Day
Dr. Gorman saw a different playing field in community hospitals where she worked. She was named chief medical officer for IPC Healthcare, Inc., in North Hollywood, Calif., in 2003 amid the push for quality and safety. And while the specialty’s early adoption of those initiatives clearly was a major reason for the exponential growth of hospitalists, Dr. Gorman doesn’t want people to forget that the cost of care was what motivated community facilities.
“This has all been an economic move,” she says. “People sort of forget that, I think. It was discovered by some of the HMOs on the West Coast, and it was really not the HMOs, it was the medical groups that were taking risks—economic risks for their group of patients—that figured out if they sent … primary-care people to the hospital and they assigned them on a rotation of a week at a time, that they can bring down the LOS in the hospital.
“That meant more money in their own pockets because the medical group was taking the risk.”
Once hospitalists set up practice in a hospital, C-suite administrators quickly saw them gaining patient share and began realizing that they could be partners.
“They woke up one day, and just like that, they pay attention to how many cases the orthopedist does,” she says. “[They said], ‘Oh, Dr. Smith did 10 cases last week, he did 10 cases this week, then he did no cases or he did two cases. … They started to come to the hospitalists and say, ‘Look, you’re controlling X% of my patients a day. We’re having a length of stay problem; we’re having an early-discharge problem.’ Whatever it was, they were looking for partners to try to solve these issues.”
And when hospitalists grew in number again as the model continued to take hold and blossom as an effective care-delivery method, hospitalists again were turned to as partners.
“Once you get to that point, that you’re seeing enough patients and you’re enough of a movement,” Dr. Gorman says, “you get asked to be on the pharmacy committee and this committee, and chairman of the medical staff, and all those sort of things, and those evolve over time.”
Tech Effect
In the last 20 years, HM and technology have drastically changed the hospital landscape. But was HM pushed along by generational advances in computing power, smart devices in the shape of phones and tablets, and the software that powered those machines? Or was technology spurred on by having people it could serve directly in the hospital, as opposed to the traditionally fragmented system that preceded HM?
“Bob [Wachter] and others used to joke that the only people that actually understand the computer system are the hospitalists,” Dr. Goldman notes.
“Chicken or the egg, right?” adds Dr. Merlino of Press Ganey. “Technology is an enabler that helps providers deliver better care. I think healthcare quality in general has been helped by both.
“It doesn’t just help make hospitalists work better. It makes nursing better. It makes surgeons better. It makes pharmacy better.”
Dr. Bessler of Sound Physicians notes that advances in technology have come with their hurdles as well. Take the oft-maligned world of electronic medical records (EMRs).
“EMRs are great for data, but they’re not workflow solutions,” Dr. Bessler says. “They don’t tell you what do next.”
So Sound Physicians created its own technology platform, dubbed Sound Connect, that interacts with in-place EMRs at hospitals across the country. The in-house system takes the functional documentation of EMRs and overlays productivity protocols, Dr. Bessler says.
“It allows us to run a standard workflow and drive reproducible results and put meaningful data in the hands of the docs on a daily basis in the way that an EMR is just not set up to do,” he adds. Technology will continue “to be instrumental, of course, but I think the key thing is interoperability, which plenty has been written on, so we’re not unique in that. The more the public demands and the clinicians demand … the better patient care will be. I think the concept of EMR companies not being easy to work with has to end.”
Kendall Rogers, MD, CPE, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, believes that hospitalists have to take ownership of health information technology (HIT) in their own buildings.
He and other SHM officials have pushed hospitalists for the past few years to formalize their HIT duties by seeing if they would qualify to take the exam for board certification in medical informatics, which was created in 2013 by the American Board of Medical Specialties (ABMS). Between certification of that skill set and working more with technology vendors and others to improve HIT, Dr. Rogers sees HM being able to help reform much of the current technology woes in just a few years.
“To me, this is the new frontier,” Dr. Wachter says. “If our defining mantra as a field is, ‘How do we make care better for patients, and how do we create a better system?’ … well, I don’t see how you say that without really owning the issue of informatics.”
Teamwork: An HM Tradition
Hospitalists are often referred to as the quarterbacks of the hospital. But even the best QB needs a good team to succeed. For HMGs, that roster increasingly includes nurse practitioners (NPs) and physician assistants (PAs).
Recent State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs, and SHM earlier this year added Tracy Cardin, ACNP-BC, SFHM, as its first non-physician voting board member.
Dr. Donaldson believes that integrating hospitalists and non-physician providers (NPPs) allows both sets of practitioners to “work at the top of their license.”
“Any time when nurse practitioners and other providers get together, there is always this challenge of professions,” he says. “You’re doing this or you’re doing that, and once you get people who understand what the capabilities are past the title name and what you can do, it’s just amazing.”
Dr. Donaldson sees SHM’s acceptance of NPs and PAs as a good sign for HM.
“The day is upon us where we need to strongly consider nurse practitioners and physician assistants as equal in the field,” he says. “We’re going to find a much better continuity of care for all our patients at various institutions with hospital medicine and … a nurse practitioner who is at the top of their license.”
The Post-Acute Space
Aside from NPs and PAs, another extension of HM has been the gravitation in recent years of hospitalists into post-acute-care settings, including skilled-nursing facilities (SNFs), long-term care facilities, post-discharge clinics, and patient-centered homes.
Dr. Bessler says that as HMGs continued to focus on improving quality and lowering costs, they had little choice but to get involved in activities outside the hospital.
“We got into post-acute medicines because there was an abyss in quality,” he says. “We were accountable to send patients out, and there was nobody to send them to. Or the quality of the facilities was terrible, or the docs or clinicians weren’t going to see those patients regularly. That’s how we got into solving post-acute.”
Dr. Gorman, formerly the chief executive of St. Louis–based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine, agrees that for hospitalists to exert even more control over quality of care, they have to team with people outside the hospital.
“If we can’t build what I think of as a pyramid of care with one doctor and many, many other people supporting a broad group of patients, I don’t think we’re going to be able to find the scale to take care of the aging population that’s coming at us,” she says.
Caring for patients once they are discharged means including home nurses, pharmacists, physical therapists, dietitians, hired caregivers, and others in the process, Dr. Gorman says. But that doesn’t mean overburdening the wrong people with the wrong tasks. The same way no one would think to allow a social worker to prescribe medication is the same way that a hospitalist shouldn’t be the one checking up on a patient to make sure there is food in that person’s fridge.
And while the hospitalist can work in concert with others and run many things from the hospital, maybe hospital-based physicians aren’t always the best physicians for the task.
“There are certain things that only the doctor can do, of course, but there are a lot more things that somebody else can do,” Dr. Gorman says, adding, “some of the times, you’re going to need the physician, it’s going to be escalated to a medication change, but sometimes maybe you need to escalate to a dietary visit or you need to escalate to three physical therapy visits.
“The nitty-gritty of taking care of people outside of the hospital is so complex and problematic, and most of the solutions are not really medical, but you need the medical part of the dynamic. So rather [than a hospitalist running cases], it’s a super-talented social worker, nurse, or physical therapist. I don’t know, but somebody who can make sure that all of that works and it’s a process that can be leveraged.”
Whoever it is, the gravitation beyond the walls of the hospital has been tied to a growing sea change in how healthcare will compensate providers. Medicare has been migrating from fee-for-service to payments based on the totality of care for decades. The names change, of course. In the early 1980s, it was an “inpatient prospective payment system.”
Five years ago, it was accountable care organizations and value-based purchasing that SHM glommed on to as programs to be embraced as heralding the future.
Now it’s the Bundled Payments for Care Improvement initiative (BCPI), introduced by the Center for Medicare & Medicaid Innovation (CMMI) at the Centers for Medicare & Medicaid Services (CMS) back in 2011 and now compiling its first data sets for the next frontier of payments for episodic care.
BCPI was mandated by the Patient Protection and Affordable Care Act (ACA) of 2009, which included a provision that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association. BCPI now has more than 650 participating organizations, not including thousands of physicians who then partner with those groups, over four models. The initiative covers 48 defined episodes of care, both medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“The bundled model [BCPI] gives us the flexibility, scale, and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
A Score of Success
Twenty years of unbridled growth is great in any business. Put in perspective, the first iPhone, which redefined personal communication, is just nine years old, and already, stock analysts question whether Apple can grow any bigger or if it’s plateaued.
To be sure, the field of HM and its leaders have accomplished more than even Dr. Wachter and Dr. Goldman envisioned 20 summers ago. Much of it may seem so easily established by now, but when pioneering hospitalists John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM, founded the National Association of Inpatient Physicians (NAIP) a year after the NEJM paper, they promoted and held a special session at UCSF’s first “Management of the Hospitalized Patient” conference in April 1997.
By 2003, the term “hospitalist” had become ubiquitous enough that NAIP was renamed the Society of Hospital Medicine.
Again, progress followed quickly.
By 2007, SHM had launched Project BOOST (Better Outcomes by Optimizing Safe Transitions), an award-winning mentored-implementation program to reduce LOS, adverse events, and unnecessary 30-day readmissions. Other mentored-implementation programs followed. The Glycemic Control Mentored Implementation (GCMI) program focuses on preventing hypoglycemia, while the Venous Thromboembolism Prevention Collaborative (VTE PC) seeks to give practical assistance on how to reduce blood clots via a VTE prevention program.
In 2012, SHM earned the 2011 John M. Eisenberg Patient Safety and Quality Award for Innovation in Patient Safety and Quality at the National Level, thanks to its mentored-implementation programs. SHM was the first professional society to earn the award, bestowed by the National Quality Forum (NQF) and The Joint Commission.
And earlier this year, CMS announced that by this time next year hospitalists would be assigned their own specialty designation code. SHM’s Public Policy Committee lobbied for the move for more than two years.
Dr. Merlino says it’s not just accomplishments that have set the field apart in its first 20 years. It’s the people.
Take Modern Healthcare’s list of the 50 Most Influential Physician Executives and Leaders of 2016. Third on the list is pediatric hospitalist Patrick Conway, MD, MSc, MHM, deputy administrator for innovation and quality and CMS’s chief medical officer. One spot behind him is Dr. Wachter, who in addition to being an architect of the HM movement was the first hospitalist to serve as chair of the Board of Directors of the American Board of Internal Medicine, which provides certification for the majority of working hospitalists.
Rounding out HM’s presence on the list is Vivek Murthy, MD, MBA, a Boston hospitalist and the current U.S. Surgeon General.
“It does demonstrate the emergence of their leadership,” Dr. Merlino says. “I don’t think yet they’re viewed as being the leaders, but I would add to that I don’t think they have yet the respect they deserve for the work they’re doing. When people who have worked with them can understand the value that they bring to clinical care, they clearly view hospitalists as being critical leaders.”
The Future
So what now? For all the talk of SHM’s success, HM’s positive impacts, and the specialty’s rocket growth trajectory, the work isn’t done, industry leaders say.
Hospitalists are not just working toward a more valuable delivery of care, they’re also increasingly viewed as leaders of projects all around the hospital because, well, they are always there, according to Dr. Gandhi.
“Hospitalists really are a leader in the hospital around quality and safety issues because they are there on the wards all the time,” she says. “They really have an interest in being the physician champions around various initiatives, so [in my hospital tenures] I partnered with many of my hospitalist colleagues on ways to improve care, such as test-result management, medication reconciliation, and similar efforts. We often would establish multidisciplinary committees to work on things, and almost always there was a hospitalist who was chairing or co-chairing or participating very actively in that group.”
Dr. Gandhi, who was finishing her second year of residency at Duke Medical Center in Raleigh, N.C., when the NEJM paper was published, sees the acuity of patients getting worse in the coming years as America rapidly ages. Baby boomers will start turning 80 in the next decade, and longer life spans translate to increasing medical problems that will often require hospitalization.
And while hospitalists have already moved into post-acute-care settings, Dr. Bessler says that will become an even bigger focus in the next 20 years of the specialty.
“It’s not generally been the psyche of the hospitalist in the past to feel accountable beyond the walls of the hospital,” he says. “But between episodic care [and] bundled payments … you can’t just wash your hands of it. You have to understand your next site-of-care decision. You need to make sure care happens at the right location.”
At a time of once-in-a-generation reform to healthcare in this country, the leaders of HM can’t afford to rest on their laurels, says Dr. Goldman. Three years ago, he wrote a paper for the Journal of Hospital Medicine titled “An Intellectual Agenda for Hospitalists.” In short, Dr. Goldman would like to see hospitalists move more into advancing science themselves rather than implementing the scientific discoveries of others. He cautions anyone against taking that as criticism of the field.
“If hospitalists are going to be the people who implement what other people have found, they run the risk of being the ones who make sure everybody gets perioperative beta-blockers even if they don’t really work,” he says. “If you want to take it to the illogical extreme, you could have people who were experts in how most efficiently to do bloodletting.
“The future for hospitalists, if they’re going to get to the next level—I think they can and will—is that they have to be in the discovery zone as well as the implementation zone.”
Dr. Wachter says it’s about staying ahead of the curve. For 20 years, the field has been on the cutting edge of how hospitals treat patients. To grow even more, it will be crucial to keep that focus.
Hospitalists need to continue to take C-suite positions at hospitals and policy roles at think tanks and governmental agencies. They need to continue to master technology, clinical care, and the ever-growing importance of where those two intersect.
Most of all, the field can’t get lazy. Otherwise, the “better mousetrap” of HM might one day be replaced by the next group of physicians willing to work harder to implement their great idea.
“If we continue to be the vanguard of innovation, the vanguard of making the system work better than it ever has before,” Dr. Wachter says, “the field that creates new models of care, that integrates technology in new ways, and that has this can-do attitude and optimism, then the sky is the limit.” TH
Richard Quinn is a freelance writer in New Jersey.
References
- Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med. 1998;129(3):197-203.
Editor's Note: Listen to Dr. Goldman, Dr. Wachter, Dr. Gandhi, Dr. Bessler, Dr. Gorman, and Dr. Merlino share more of their views on hospital medicine.
When Lee Goldman, MD, became chair of medicine at the University of California at San Francisco (UCSF) in January 1995, the construct of the medical service wasn’t all that different from when he had left as a resident 20 years earlier.
“It was still largely one month a year attending,” he recalls. “A couple of people did two months, I think. Some physicians still took care of their own patients even though there were teaching attending.”
Sure, it was an antiquated way to manage inpatient care, but since it had worked well enough for decades, who was going to change it?
“I got the idea that we could do better than that,” Dr. Goldman says.
He was right.
Dr. Goldman lured a young physician over from San Francisco General Hospital. The guy was a rising star of sorts. Robert Wachter, MD, MHM, had helped run the International AIDS Conference, held in the City by the Bay in 1990. He joined the faculty at San Francisco General that year and two years later became UCSF’s residency program director.
Then, Dr. Goldman asked Dr. Wachter to take on a new role as chief of the medical center at UCSF Medical Center. The charge was simple: “Come up with a new and innovative model by which fewer, selected faculty each spent multiple months as inpatient attendings and teachers.”
The model Dr. Wachter settled on—internal medicine physicians who practice solely in the hospital—wasn’t entirely novel. He recalled an American College of Physicians (ACP) presentation at 7 a.m. on a Sunday in 1995, the sort of session most conventioneers choose sleep over. Also, some doctors nationwide, in Minnesota and Arizona, for instance, were hospital-based as healthcare maintenance organizations (HMOs) struggled to make care more efficient and less costly to provide.
But those efforts were few and far between. And they were nearly all in the community setting. No one had tried to staff inpatient services with committed generalists in an academic setting.
Until Dr. Wachter and Dr. Goldman.
On Aug. 15, 1996, their article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” was published in the New England Journal of Medicine (NEJM).
A burgeoning specialty was given a name.
Its practitioners were called “hospitalists.”
And the rest, as they say, is history.
The Early Days
The idea of hospital-based physicians seems obvious in the rubric of medical history. There are now an estimated 44,000 hospitalists nationwide. The Society of Hospital Medicine (SHM) bills itself as the fastest-growing specialty in healthcare.
But it wasn’t always this way.
The novelty of hospital-based practitioners taking over care for some or all inpatient admissions wasn’t immediately embraced as a positive paradigm shift. Just ask Rob Bessler, MD, chief executive officer of Sound Physicians of Tacoma, Wash., among the largest hospitalist management groups (HMGs) in the country, with more than 2,200 hospitalists, ED physicians, intensivists, and post-acute-care physicians.
When the NEJM piece bestowing a name on hospitalists was published, Dr. Bessler was just finishing medical school at Case Western Reserve University School of Medicine in Cleveland. He started out in private practice and immediately saw issues in how hospitalized patients were treated.
“As an ED physician, nobody wanted to admit my patients as they were too busy in their office. I felt that those docs that were practicing in the hospital were using evidence that was 15 years old from when they finished their training,” he says. “I raised my hand to the hospital CEO to do things differently.”
Pushback against a new model came from multiple stakeholders. For every Dr. Bessler who was interested in a new way of doing things, there were physicians worried about turf battles.
“Doctors in practice around the county were afraid that these hospitalists would become mandatory,” says Dr. Goldman, who now is Dean of the Faculties of Health Sciences and Medicine, and chief executive at Columbia University Medical Center in New York City. “Some states actually had medical societies that passed resolutions saying they couldn’t become mandatory.”
In the early days, there were more critics than advocates. Critical-care doctors were one group that was, at best, ambivalent about the new model.
“The biggest brush fire in the early days was with critical care, which kind of surprised me,” Dr. Wachter says. “But ICU doctors had spent a huge amount of energy in the prior 20 years establishing their role. When hospitalists came out and often began to manage ICU cases—usually collaboratively with intensivists and partly filling a massive national shortage in intensivists—the leaders of the critical-care field felt like we were encroaching on their turf.”
Perhaps the biggest concerns to hospital medicine in the beginning came from the residents at UCSF. Initially, residents worried—some aloud—that hospitalists would become too controlling and “take away their delegated and graduated autonomy,” Dr. Goldman recalls.
At a meeting with the medical residents, “some actually said this could be awful and maybe they shouldn’t have come here,” he says, “maybe they should tell the internship applicants this would be a bad place to come because they wouldn’t have much autonomy, and I still remember asking a specific question to them. ‘Imagine your mother is admitted to the medical service at the teaching hospital back home where you live. What’s the first question you would ask?’
“And someone raised their hand and said, ‘Who’s the doctor?’
“And I said, ‘You mean who’s the intern?’
“They said, ‘No.’
“I said, ‘Or who’s the ward resident?’
“They said, ‘No.’
“And then, ‘Who is the attending?’
“And they said, ‘Yes.’
“So I said, ‘We have to have a good answer to that question when Mom gets admitted. Now that we’ve figured out how to get Mom the best care, let’s figure out how to make this the best possible teaching service.’”
Dr. Wachter and Dr. Goldman also prepared for some fears that didn’t pan out. One was the clout of specialists who might oppose the new model.
Some “specialists worried that if hospitalists were more knowledgeable than once-a-month-a-year attendings, and knew more about what was going on, they would be less likely to consult a specialist,” Dr. Goldman explains, adding he and Dr. Wachter thought that would be an unintended consequence of HM. “If there was a reduction in requested consults, that expertise would somehow be lost.”
Dr. Wachter and other early leaders also worried that patients, used to continuity of care with their primary-care doctors, would not take well to hospitalists. Would patients revolt against the idea of a new doctor seeing them every day?
“Yes, there were patients who felt that they wanted to see their regular doctor in the hospital. But for every one of them, there was another one or two that said this actually worked better,” Dr. Wachter says.
Community Views
Of course, the early success and adoption of the model in academic settings didn’t necessarily translate to community settings. Former SHM President Mary Jo Gorman, MD, MBA, MHM, who had just completed her MBA at Washington University in St. Louis when the NEJM article was published, wrote a business plan for her degree on implementing a hospitalist-style program at her institution, SSM DePaul Health Center, also in St. Louis.
She didn’t use the terms “hospital medicine” or “hospitalist.” They didn’t exist yet.
She was writing about what she was witnessing in her hospital: primary-care physicians (PCPs) who no longer wanted to visit hospitals because there simply wasn’t enough to do and make the trip worthwhile. In addition, she saw many of those same doctors no longer wanting to pick up ED calls.
So she pitched a model (same as Dr. Wachter was doing on the West Coast) of having someone in the hospital dedicated to inpatients as their sole responsibility. A “vocal minority” rebelled.
“It was a battlefield,” she recounts. “No other way to describe it. There were multiple hospital committees that reviewed it. There were letters of protest to the hospitals.”
Two major complaints emerged early on, Dr. Gorman says. Number one was the notion that hospitalists were enablers, allowing PCPs to shirk their long-established duty of shepherding their patients’ care through the walls of their local hospital. Number two, ironically, was the opposite: PCPs who didn’t want to cede control of their patients also moonlit taking ED calls that could generate patients for their own practice.
“It didn’t shock me at the time because I had already made major changes in our intensive-care unit at the hospital, which were unpopular,” Dr. Gorman says, adding all of the changes were good for patients and produced “fabulous” results. “But it was new. And it was different. And people don’t like to change the status quo.”
Perfect Timing
The seeds of hospitalist practice were planted before the NEJM article published. But the NEJM audience was nationwide, even beyond American borders. And the playing field was set up particularly well, says James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division. In 1996, the AIDS crisis was full-blown and a particular burden in inpatient wards.
“It was before we really had any of these amazing drugs that have turned HIV/AIDS into a quiet disease as opposed to a killer,” Dr. Merlino says. “At least 50% of the patients on the floors that we were rotating through [then] had patients, unfortunately, who were succumbing to AIDS.”
Dr. Merlino says he’s proud of the specialists who rotated through the hospital rooms of AIDS patients. But so many disparate doctors with no “quarterback” to manage the process holistically meant consistency in treatment was generally lacking.
“The role of the hospitalist often is to take recommendations from a lot of different specialties and come up with the best plan for the patient,” says Tejal Gandhi, MD, MPH, CPPS, president and CEO of the National Patient Safety Foundation. “They’re the true patient advocate who is getting the cardiologist’s opinion, the rheumatologist’s opinion, and the surgeon’s opinion, and they come up with the best plan for the patient.”
Dr. Merlino has an even blunter viewpoint: “I reflect back on that and think today about what the hospitalist model brings to us; it is an amazing transformation on how the hospitalist model really delivers.”
That type of optimism permeated nascent hospitalist groups. But it was time to start proving the anecdotal stories. Nearly two years to the day after the Wachter/Goldman paper published, a team led by Herbert Diamond, MD, published “The Effect of Full-Time Faculty Hospitalists on the Efficiency of Care at a Community Teaching Hospital” in the Annals of Internal Medicine.1 It was among the first reports to show evidence that hospitalists improved care.
Results published in that article showed median length of stay (LOS) decreased to 5.01 days from 6.01 days (P<0.001). It showed median cost of care decreased to $3,552 from $4,139 (P<0.001), and the 14-day readmission rate decreased to 4.64 readmissions per 100 admissions from 9.9 per 100 (P<0.001). In the comparison groups, LOS decreased, but both cost of care and readmission rates increased.
The research was so early on that the paper’s background section noted that “hospitalists are increasingly being used for inpatient care.”
“What we found, of course, was that they were providing an excellent service. They were well-trained, and you could get hospital people instead of having family-practice people managing the patients,” says nurse practitioner Robert Donaldson, NPC, clinical director of emergency medicine at Ellenville Regional Hospital in upstate New York and a veteran of working alongside hospitalists since the specialty arrived in the late 1990s. “We were getting better throughput times, better receipt of patients from our emergency rooms, and, I think, better outcomes as well.”
Growth Spurt
The refrain was familiar across the country as HM spread from health system to health system. Early results were looking good. The model was taking hold in more hospitals, both academic and community. Initial research studies supported the premise that the model improved efficiency without compromising quality or patient experience.
“My feeling at the time was this was a good idea,” Dr. Wachter says. “The trend toward our system being pushed to deliver better, more efficient care was going to be enduring, and the old model of the primary-care doc being your hospital doc … couldn’t possibly achieve the goal of producing the highest value.”
Dr. Wachter and other early leaders pushed the field to become involved in systems-improvement work. This turned out to be prophetic in December 1999, when patient safety zoomed to the national forefront with the publication of the Institute of Medicine (IOM) report “To Err Is Human.” Its conclusions, by now, are well-known. It showed between 44,000 and 98,000 people a year die from preventable medical errors, the equivalent of a jumbo jet a day crashing.
The impact was profound, and safety initiatives became a focal point of hospitals. The federal Agency for Health Care Policy and Research was renamed the Agency for Healthcare Research and Quality (ARHQ) to indicate the change in focus.
“When the IOM report came out, it gave us a focus and a language that we didn’t have before,” says Dr. Wachter, who served as president of SHM’s Board of Directors and to this day lectures at SHM annual meetings. “But I think the general sensibility that hospitalists are about improving quality and safety and patients’ experience and efficiency—I think that was baked in from the start.”
Two years later, IOM followed up its safety push with “Crossing the Quality Chasm: A New Health System for the 21st Century.” The sequel study laid out focus areas and guidelines to start reducing the spate of medical mistakes that “To Err Is Human” lay bare.
Hospitalists were seen as people to lead the charge for safety because they were already taking care of patients, already focused on reducing LOS and improving care delivery—and never to be underestimated, they were omnipresent, Dr. Gandhi says of her experience with hospitalists around 2000 at Brigham and Women’s Hospital in Boston.
“At least where I was, hospitalists truly were leaders in the quality and safety space, and it was just a really good fit for the kind of mindset and personality of a hospitalist because they’re very much … integrators of care across hospitals,” she says. “They interface with so many different areas of the hospital and then try to make all of that work better.”
Revenue Rules the Day
Dr. Gorman saw a different playing field in community hospitals where she worked. She was named chief medical officer for IPC Healthcare, Inc., in North Hollywood, Calif., in 2003 amid the push for quality and safety. And while the specialty’s early adoption of those initiatives clearly was a major reason for the exponential growth of hospitalists, Dr. Gorman doesn’t want people to forget that the cost of care was what motivated community facilities.
“This has all been an economic move,” she says. “People sort of forget that, I think. It was discovered by some of the HMOs on the West Coast, and it was really not the HMOs, it was the medical groups that were taking risks—economic risks for their group of patients—that figured out if they sent … primary-care people to the hospital and they assigned them on a rotation of a week at a time, that they can bring down the LOS in the hospital.
“That meant more money in their own pockets because the medical group was taking the risk.”
Once hospitalists set up practice in a hospital, C-suite administrators quickly saw them gaining patient share and began realizing that they could be partners.
“They woke up one day, and just like that, they pay attention to how many cases the orthopedist does,” she says. “[They said], ‘Oh, Dr. Smith did 10 cases last week, he did 10 cases this week, then he did no cases or he did two cases. … They started to come to the hospitalists and say, ‘Look, you’re controlling X% of my patients a day. We’re having a length of stay problem; we’re having an early-discharge problem.’ Whatever it was, they were looking for partners to try to solve these issues.”
And when hospitalists grew in number again as the model continued to take hold and blossom as an effective care-delivery method, hospitalists again were turned to as partners.
“Once you get to that point, that you’re seeing enough patients and you’re enough of a movement,” Dr. Gorman says, “you get asked to be on the pharmacy committee and this committee, and chairman of the medical staff, and all those sort of things, and those evolve over time.”
Tech Effect
In the last 20 years, HM and technology have drastically changed the hospital landscape. But was HM pushed along by generational advances in computing power, smart devices in the shape of phones and tablets, and the software that powered those machines? Or was technology spurred on by having people it could serve directly in the hospital, as opposed to the traditionally fragmented system that preceded HM?
“Bob [Wachter] and others used to joke that the only people that actually understand the computer system are the hospitalists,” Dr. Goldman notes.
“Chicken or the egg, right?” adds Dr. Merlino of Press Ganey. “Technology is an enabler that helps providers deliver better care. I think healthcare quality in general has been helped by both.
“It doesn’t just help make hospitalists work better. It makes nursing better. It makes surgeons better. It makes pharmacy better.”
Dr. Bessler of Sound Physicians notes that advances in technology have come with their hurdles as well. Take the oft-maligned world of electronic medical records (EMRs).
“EMRs are great for data, but they’re not workflow solutions,” Dr. Bessler says. “They don’t tell you what do next.”
So Sound Physicians created its own technology platform, dubbed Sound Connect, that interacts with in-place EMRs at hospitals across the country. The in-house system takes the functional documentation of EMRs and overlays productivity protocols, Dr. Bessler says.
“It allows us to run a standard workflow and drive reproducible results and put meaningful data in the hands of the docs on a daily basis in the way that an EMR is just not set up to do,” he adds. Technology will continue “to be instrumental, of course, but I think the key thing is interoperability, which plenty has been written on, so we’re not unique in that. The more the public demands and the clinicians demand … the better patient care will be. I think the concept of EMR companies not being easy to work with has to end.”
Kendall Rogers, MD, CPE, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, believes that hospitalists have to take ownership of health information technology (HIT) in their own buildings.
He and other SHM officials have pushed hospitalists for the past few years to formalize their HIT duties by seeing if they would qualify to take the exam for board certification in medical informatics, which was created in 2013 by the American Board of Medical Specialties (ABMS). Between certification of that skill set and working more with technology vendors and others to improve HIT, Dr. Rogers sees HM being able to help reform much of the current technology woes in just a few years.
“To me, this is the new frontier,” Dr. Wachter says. “If our defining mantra as a field is, ‘How do we make care better for patients, and how do we create a better system?’ … well, I don’t see how you say that without really owning the issue of informatics.”
Teamwork: An HM Tradition
Hospitalists are often referred to as the quarterbacks of the hospital. But even the best QB needs a good team to succeed. For HMGs, that roster increasingly includes nurse practitioners (NPs) and physician assistants (PAs).
Recent State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs, and SHM earlier this year added Tracy Cardin, ACNP-BC, SFHM, as its first non-physician voting board member.
Dr. Donaldson believes that integrating hospitalists and non-physician providers (NPPs) allows both sets of practitioners to “work at the top of their license.”
“Any time when nurse practitioners and other providers get together, there is always this challenge of professions,” he says. “You’re doing this or you’re doing that, and once you get people who understand what the capabilities are past the title name and what you can do, it’s just amazing.”
Dr. Donaldson sees SHM’s acceptance of NPs and PAs as a good sign for HM.
“The day is upon us where we need to strongly consider nurse practitioners and physician assistants as equal in the field,” he says. “We’re going to find a much better continuity of care for all our patients at various institutions with hospital medicine and … a nurse practitioner who is at the top of their license.”
The Post-Acute Space
Aside from NPs and PAs, another extension of HM has been the gravitation in recent years of hospitalists into post-acute-care settings, including skilled-nursing facilities (SNFs), long-term care facilities, post-discharge clinics, and patient-centered homes.
Dr. Bessler says that as HMGs continued to focus on improving quality and lowering costs, they had little choice but to get involved in activities outside the hospital.
“We got into post-acute medicines because there was an abyss in quality,” he says. “We were accountable to send patients out, and there was nobody to send them to. Or the quality of the facilities was terrible, or the docs or clinicians weren’t going to see those patients regularly. That’s how we got into solving post-acute.”
Dr. Gorman, formerly the chief executive of St. Louis–based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine, agrees that for hospitalists to exert even more control over quality of care, they have to team with people outside the hospital.
“If we can’t build what I think of as a pyramid of care with one doctor and many, many other people supporting a broad group of patients, I don’t think we’re going to be able to find the scale to take care of the aging population that’s coming at us,” she says.
Caring for patients once they are discharged means including home nurses, pharmacists, physical therapists, dietitians, hired caregivers, and others in the process, Dr. Gorman says. But that doesn’t mean overburdening the wrong people with the wrong tasks. The same way no one would think to allow a social worker to prescribe medication is the same way that a hospitalist shouldn’t be the one checking up on a patient to make sure there is food in that person’s fridge.
And while the hospitalist can work in concert with others and run many things from the hospital, maybe hospital-based physicians aren’t always the best physicians for the task.
“There are certain things that only the doctor can do, of course, but there are a lot more things that somebody else can do,” Dr. Gorman says, adding, “some of the times, you’re going to need the physician, it’s going to be escalated to a medication change, but sometimes maybe you need to escalate to a dietary visit or you need to escalate to three physical therapy visits.
“The nitty-gritty of taking care of people outside of the hospital is so complex and problematic, and most of the solutions are not really medical, but you need the medical part of the dynamic. So rather [than a hospitalist running cases], it’s a super-talented social worker, nurse, or physical therapist. I don’t know, but somebody who can make sure that all of that works and it’s a process that can be leveraged.”
Whoever it is, the gravitation beyond the walls of the hospital has been tied to a growing sea change in how healthcare will compensate providers. Medicare has been migrating from fee-for-service to payments based on the totality of care for decades. The names change, of course. In the early 1980s, it was an “inpatient prospective payment system.”
Five years ago, it was accountable care organizations and value-based purchasing that SHM glommed on to as programs to be embraced as heralding the future.
Now it’s the Bundled Payments for Care Improvement initiative (BCPI), introduced by the Center for Medicare & Medicaid Innovation (CMMI) at the Centers for Medicare & Medicaid Services (CMS) back in 2011 and now compiling its first data sets for the next frontier of payments for episodic care.
BCPI was mandated by the Patient Protection and Affordable Care Act (ACA) of 2009, which included a provision that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association. BCPI now has more than 650 participating organizations, not including thousands of physicians who then partner with those groups, over four models. The initiative covers 48 defined episodes of care, both medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“The bundled model [BCPI] gives us the flexibility, scale, and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
A Score of Success
Twenty years of unbridled growth is great in any business. Put in perspective, the first iPhone, which redefined personal communication, is just nine years old, and already, stock analysts question whether Apple can grow any bigger or if it’s plateaued.
To be sure, the field of HM and its leaders have accomplished more than even Dr. Wachter and Dr. Goldman envisioned 20 summers ago. Much of it may seem so easily established by now, but when pioneering hospitalists John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM, founded the National Association of Inpatient Physicians (NAIP) a year after the NEJM paper, they promoted and held a special session at UCSF’s first “Management of the Hospitalized Patient” conference in April 1997.
By 2003, the term “hospitalist” had become ubiquitous enough that NAIP was renamed the Society of Hospital Medicine.
Again, progress followed quickly.
By 2007, SHM had launched Project BOOST (Better Outcomes by Optimizing Safe Transitions), an award-winning mentored-implementation program to reduce LOS, adverse events, and unnecessary 30-day readmissions. Other mentored-implementation programs followed. The Glycemic Control Mentored Implementation (GCMI) program focuses on preventing hypoglycemia, while the Venous Thromboembolism Prevention Collaborative (VTE PC) seeks to give practical assistance on how to reduce blood clots via a VTE prevention program.
In 2012, SHM earned the 2011 John M. Eisenberg Patient Safety and Quality Award for Innovation in Patient Safety and Quality at the National Level, thanks to its mentored-implementation programs. SHM was the first professional society to earn the award, bestowed by the National Quality Forum (NQF) and The Joint Commission.
And earlier this year, CMS announced that by this time next year hospitalists would be assigned their own specialty designation code. SHM’s Public Policy Committee lobbied for the move for more than two years.
Dr. Merlino says it’s not just accomplishments that have set the field apart in its first 20 years. It’s the people.
Take Modern Healthcare’s list of the 50 Most Influential Physician Executives and Leaders of 2016. Third on the list is pediatric hospitalist Patrick Conway, MD, MSc, MHM, deputy administrator for innovation and quality and CMS’s chief medical officer. One spot behind him is Dr. Wachter, who in addition to being an architect of the HM movement was the first hospitalist to serve as chair of the Board of Directors of the American Board of Internal Medicine, which provides certification for the majority of working hospitalists.
Rounding out HM’s presence on the list is Vivek Murthy, MD, MBA, a Boston hospitalist and the current U.S. Surgeon General.
“It does demonstrate the emergence of their leadership,” Dr. Merlino says. “I don’t think yet they’re viewed as being the leaders, but I would add to that I don’t think they have yet the respect they deserve for the work they’re doing. When people who have worked with them can understand the value that they bring to clinical care, they clearly view hospitalists as being critical leaders.”
The Future
So what now? For all the talk of SHM’s success, HM’s positive impacts, and the specialty’s rocket growth trajectory, the work isn’t done, industry leaders say.
Hospitalists are not just working toward a more valuable delivery of care, they’re also increasingly viewed as leaders of projects all around the hospital because, well, they are always there, according to Dr. Gandhi.
“Hospitalists really are a leader in the hospital around quality and safety issues because they are there on the wards all the time,” she says. “They really have an interest in being the physician champions around various initiatives, so [in my hospital tenures] I partnered with many of my hospitalist colleagues on ways to improve care, such as test-result management, medication reconciliation, and similar efforts. We often would establish multidisciplinary committees to work on things, and almost always there was a hospitalist who was chairing or co-chairing or participating very actively in that group.”
Dr. Gandhi, who was finishing her second year of residency at Duke Medical Center in Raleigh, N.C., when the NEJM paper was published, sees the acuity of patients getting worse in the coming years as America rapidly ages. Baby boomers will start turning 80 in the next decade, and longer life spans translate to increasing medical problems that will often require hospitalization.
And while hospitalists have already moved into post-acute-care settings, Dr. Bessler says that will become an even bigger focus in the next 20 years of the specialty.
“It’s not generally been the psyche of the hospitalist in the past to feel accountable beyond the walls of the hospital,” he says. “But between episodic care [and] bundled payments … you can’t just wash your hands of it. You have to understand your next site-of-care decision. You need to make sure care happens at the right location.”
At a time of once-in-a-generation reform to healthcare in this country, the leaders of HM can’t afford to rest on their laurels, says Dr. Goldman. Three years ago, he wrote a paper for the Journal of Hospital Medicine titled “An Intellectual Agenda for Hospitalists.” In short, Dr. Goldman would like to see hospitalists move more into advancing science themselves rather than implementing the scientific discoveries of others. He cautions anyone against taking that as criticism of the field.
“If hospitalists are going to be the people who implement what other people have found, they run the risk of being the ones who make sure everybody gets perioperative beta-blockers even if they don’t really work,” he says. “If you want to take it to the illogical extreme, you could have people who were experts in how most efficiently to do bloodletting.
“The future for hospitalists, if they’re going to get to the next level—I think they can and will—is that they have to be in the discovery zone as well as the implementation zone.”
Dr. Wachter says it’s about staying ahead of the curve. For 20 years, the field has been on the cutting edge of how hospitals treat patients. To grow even more, it will be crucial to keep that focus.
Hospitalists need to continue to take C-suite positions at hospitals and policy roles at think tanks and governmental agencies. They need to continue to master technology, clinical care, and the ever-growing importance of where those two intersect.
Most of all, the field can’t get lazy. Otherwise, the “better mousetrap” of HM might one day be replaced by the next group of physicians willing to work harder to implement their great idea.
“If we continue to be the vanguard of innovation, the vanguard of making the system work better than it ever has before,” Dr. Wachter says, “the field that creates new models of care, that integrates technology in new ways, and that has this can-do attitude and optimism, then the sky is the limit.” TH
Richard Quinn is a freelance writer in New Jersey.
References
- Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med. 1998;129(3):197-203.
Editor's Note: Listen to Dr. Goldman, Dr. Wachter, Dr. Gandhi, Dr. Bessler, Dr. Gorman, and Dr. Merlino share more of their views on hospital medicine.
When Lee Goldman, MD, became chair of medicine at the University of California at San Francisco (UCSF) in January 1995, the construct of the medical service wasn’t all that different from when he had left as a resident 20 years earlier.
“It was still largely one month a year attending,” he recalls. “A couple of people did two months, I think. Some physicians still took care of their own patients even though there were teaching attending.”
Sure, it was an antiquated way to manage inpatient care, but since it had worked well enough for decades, who was going to change it?
“I got the idea that we could do better than that,” Dr. Goldman says.
He was right.
Dr. Goldman lured a young physician over from San Francisco General Hospital. The guy was a rising star of sorts. Robert Wachter, MD, MHM, had helped run the International AIDS Conference, held in the City by the Bay in 1990. He joined the faculty at San Francisco General that year and two years later became UCSF’s residency program director.
Then, Dr. Goldman asked Dr. Wachter to take on a new role as chief of the medical center at UCSF Medical Center. The charge was simple: “Come up with a new and innovative model by which fewer, selected faculty each spent multiple months as inpatient attendings and teachers.”
The model Dr. Wachter settled on—internal medicine physicians who practice solely in the hospital—wasn’t entirely novel. He recalled an American College of Physicians (ACP) presentation at 7 a.m. on a Sunday in 1995, the sort of session most conventioneers choose sleep over. Also, some doctors nationwide, in Minnesota and Arizona, for instance, were hospital-based as healthcare maintenance organizations (HMOs) struggled to make care more efficient and less costly to provide.
But those efforts were few and far between. And they were nearly all in the community setting. No one had tried to staff inpatient services with committed generalists in an academic setting.
Until Dr. Wachter and Dr. Goldman.
On Aug. 15, 1996, their article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” was published in the New England Journal of Medicine (NEJM).
A burgeoning specialty was given a name.
Its practitioners were called “hospitalists.”
And the rest, as they say, is history.
The Early Days
The idea of hospital-based physicians seems obvious in the rubric of medical history. There are now an estimated 44,000 hospitalists nationwide. The Society of Hospital Medicine (SHM) bills itself as the fastest-growing specialty in healthcare.
But it wasn’t always this way.
The novelty of hospital-based practitioners taking over care for some or all inpatient admissions wasn’t immediately embraced as a positive paradigm shift. Just ask Rob Bessler, MD, chief executive officer of Sound Physicians of Tacoma, Wash., among the largest hospitalist management groups (HMGs) in the country, with more than 2,200 hospitalists, ED physicians, intensivists, and post-acute-care physicians.
When the NEJM piece bestowing a name on hospitalists was published, Dr. Bessler was just finishing medical school at Case Western Reserve University School of Medicine in Cleveland. He started out in private practice and immediately saw issues in how hospitalized patients were treated.
“As an ED physician, nobody wanted to admit my patients as they were too busy in their office. I felt that those docs that were practicing in the hospital were using evidence that was 15 years old from when they finished their training,” he says. “I raised my hand to the hospital CEO to do things differently.”
Pushback against a new model came from multiple stakeholders. For every Dr. Bessler who was interested in a new way of doing things, there were physicians worried about turf battles.
“Doctors in practice around the county were afraid that these hospitalists would become mandatory,” says Dr. Goldman, who now is Dean of the Faculties of Health Sciences and Medicine, and chief executive at Columbia University Medical Center in New York City. “Some states actually had medical societies that passed resolutions saying they couldn’t become mandatory.”
In the early days, there were more critics than advocates. Critical-care doctors were one group that was, at best, ambivalent about the new model.
“The biggest brush fire in the early days was with critical care, which kind of surprised me,” Dr. Wachter says. “But ICU doctors had spent a huge amount of energy in the prior 20 years establishing their role. When hospitalists came out and often began to manage ICU cases—usually collaboratively with intensivists and partly filling a massive national shortage in intensivists—the leaders of the critical-care field felt like we were encroaching on their turf.”
Perhaps the biggest concerns to hospital medicine in the beginning came from the residents at UCSF. Initially, residents worried—some aloud—that hospitalists would become too controlling and “take away their delegated and graduated autonomy,” Dr. Goldman recalls.
At a meeting with the medical residents, “some actually said this could be awful and maybe they shouldn’t have come here,” he says, “maybe they should tell the internship applicants this would be a bad place to come because they wouldn’t have much autonomy, and I still remember asking a specific question to them. ‘Imagine your mother is admitted to the medical service at the teaching hospital back home where you live. What’s the first question you would ask?’
“And someone raised their hand and said, ‘Who’s the doctor?’
“And I said, ‘You mean who’s the intern?’
“They said, ‘No.’
“I said, ‘Or who’s the ward resident?’
“They said, ‘No.’
“And then, ‘Who is the attending?’
“And they said, ‘Yes.’
“So I said, ‘We have to have a good answer to that question when Mom gets admitted. Now that we’ve figured out how to get Mom the best care, let’s figure out how to make this the best possible teaching service.’”
Dr. Wachter and Dr. Goldman also prepared for some fears that didn’t pan out. One was the clout of specialists who might oppose the new model.
Some “specialists worried that if hospitalists were more knowledgeable than once-a-month-a-year attendings, and knew more about what was going on, they would be less likely to consult a specialist,” Dr. Goldman explains, adding he and Dr. Wachter thought that would be an unintended consequence of HM. “If there was a reduction in requested consults, that expertise would somehow be lost.”
Dr. Wachter and other early leaders also worried that patients, used to continuity of care with their primary-care doctors, would not take well to hospitalists. Would patients revolt against the idea of a new doctor seeing them every day?
“Yes, there were patients who felt that they wanted to see their regular doctor in the hospital. But for every one of them, there was another one or two that said this actually worked better,” Dr. Wachter says.
Community Views
Of course, the early success and adoption of the model in academic settings didn’t necessarily translate to community settings. Former SHM President Mary Jo Gorman, MD, MBA, MHM, who had just completed her MBA at Washington University in St. Louis when the NEJM article was published, wrote a business plan for her degree on implementing a hospitalist-style program at her institution, SSM DePaul Health Center, also in St. Louis.
She didn’t use the terms “hospital medicine” or “hospitalist.” They didn’t exist yet.
She was writing about what she was witnessing in her hospital: primary-care physicians (PCPs) who no longer wanted to visit hospitals because there simply wasn’t enough to do and make the trip worthwhile. In addition, she saw many of those same doctors no longer wanting to pick up ED calls.
So she pitched a model (same as Dr. Wachter was doing on the West Coast) of having someone in the hospital dedicated to inpatients as their sole responsibility. A “vocal minority” rebelled.
“It was a battlefield,” she recounts. “No other way to describe it. There were multiple hospital committees that reviewed it. There were letters of protest to the hospitals.”
Two major complaints emerged early on, Dr. Gorman says. Number one was the notion that hospitalists were enablers, allowing PCPs to shirk their long-established duty of shepherding their patients’ care through the walls of their local hospital. Number two, ironically, was the opposite: PCPs who didn’t want to cede control of their patients also moonlit taking ED calls that could generate patients for their own practice.
“It didn’t shock me at the time because I had already made major changes in our intensive-care unit at the hospital, which were unpopular,” Dr. Gorman says, adding all of the changes were good for patients and produced “fabulous” results. “But it was new. And it was different. And people don’t like to change the status quo.”
Perfect Timing
The seeds of hospitalist practice were planted before the NEJM article published. But the NEJM audience was nationwide, even beyond American borders. And the playing field was set up particularly well, says James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division. In 1996, the AIDS crisis was full-blown and a particular burden in inpatient wards.
“It was before we really had any of these amazing drugs that have turned HIV/AIDS into a quiet disease as opposed to a killer,” Dr. Merlino says. “At least 50% of the patients on the floors that we were rotating through [then] had patients, unfortunately, who were succumbing to AIDS.”
Dr. Merlino says he’s proud of the specialists who rotated through the hospital rooms of AIDS patients. But so many disparate doctors with no “quarterback” to manage the process holistically meant consistency in treatment was generally lacking.
“The role of the hospitalist often is to take recommendations from a lot of different specialties and come up with the best plan for the patient,” says Tejal Gandhi, MD, MPH, CPPS, president and CEO of the National Patient Safety Foundation. “They’re the true patient advocate who is getting the cardiologist’s opinion, the rheumatologist’s opinion, and the surgeon’s opinion, and they come up with the best plan for the patient.”
Dr. Merlino has an even blunter viewpoint: “I reflect back on that and think today about what the hospitalist model brings to us; it is an amazing transformation on how the hospitalist model really delivers.”
That type of optimism permeated nascent hospitalist groups. But it was time to start proving the anecdotal stories. Nearly two years to the day after the Wachter/Goldman paper published, a team led by Herbert Diamond, MD, published “The Effect of Full-Time Faculty Hospitalists on the Efficiency of Care at a Community Teaching Hospital” in the Annals of Internal Medicine.1 It was among the first reports to show evidence that hospitalists improved care.
Results published in that article showed median length of stay (LOS) decreased to 5.01 days from 6.01 days (P<0.001). It showed median cost of care decreased to $3,552 from $4,139 (P<0.001), and the 14-day readmission rate decreased to 4.64 readmissions per 100 admissions from 9.9 per 100 (P<0.001). In the comparison groups, LOS decreased, but both cost of care and readmission rates increased.
The research was so early on that the paper’s background section noted that “hospitalists are increasingly being used for inpatient care.”
“What we found, of course, was that they were providing an excellent service. They were well-trained, and you could get hospital people instead of having family-practice people managing the patients,” says nurse practitioner Robert Donaldson, NPC, clinical director of emergency medicine at Ellenville Regional Hospital in upstate New York and a veteran of working alongside hospitalists since the specialty arrived in the late 1990s. “We were getting better throughput times, better receipt of patients from our emergency rooms, and, I think, better outcomes as well.”
Growth Spurt
The refrain was familiar across the country as HM spread from health system to health system. Early results were looking good. The model was taking hold in more hospitals, both academic and community. Initial research studies supported the premise that the model improved efficiency without compromising quality or patient experience.
“My feeling at the time was this was a good idea,” Dr. Wachter says. “The trend toward our system being pushed to deliver better, more efficient care was going to be enduring, and the old model of the primary-care doc being your hospital doc … couldn’t possibly achieve the goal of producing the highest value.”
Dr. Wachter and other early leaders pushed the field to become involved in systems-improvement work. This turned out to be prophetic in December 1999, when patient safety zoomed to the national forefront with the publication of the Institute of Medicine (IOM) report “To Err Is Human.” Its conclusions, by now, are well-known. It showed between 44,000 and 98,000 people a year die from preventable medical errors, the equivalent of a jumbo jet a day crashing.
The impact was profound, and safety initiatives became a focal point of hospitals. The federal Agency for Health Care Policy and Research was renamed the Agency for Healthcare Research and Quality (ARHQ) to indicate the change in focus.
“When the IOM report came out, it gave us a focus and a language that we didn’t have before,” says Dr. Wachter, who served as president of SHM’s Board of Directors and to this day lectures at SHM annual meetings. “But I think the general sensibility that hospitalists are about improving quality and safety and patients’ experience and efficiency—I think that was baked in from the start.”
Two years later, IOM followed up its safety push with “Crossing the Quality Chasm: A New Health System for the 21st Century.” The sequel study laid out focus areas and guidelines to start reducing the spate of medical mistakes that “To Err Is Human” lay bare.
Hospitalists were seen as people to lead the charge for safety because they were already taking care of patients, already focused on reducing LOS and improving care delivery—and never to be underestimated, they were omnipresent, Dr. Gandhi says of her experience with hospitalists around 2000 at Brigham and Women’s Hospital in Boston.
“At least where I was, hospitalists truly were leaders in the quality and safety space, and it was just a really good fit for the kind of mindset and personality of a hospitalist because they’re very much … integrators of care across hospitals,” she says. “They interface with so many different areas of the hospital and then try to make all of that work better.”
Revenue Rules the Day
Dr. Gorman saw a different playing field in community hospitals where she worked. She was named chief medical officer for IPC Healthcare, Inc., in North Hollywood, Calif., in 2003 amid the push for quality and safety. And while the specialty’s early adoption of those initiatives clearly was a major reason for the exponential growth of hospitalists, Dr. Gorman doesn’t want people to forget that the cost of care was what motivated community facilities.
“This has all been an economic move,” she says. “People sort of forget that, I think. It was discovered by some of the HMOs on the West Coast, and it was really not the HMOs, it was the medical groups that were taking risks—economic risks for their group of patients—that figured out if they sent … primary-care people to the hospital and they assigned them on a rotation of a week at a time, that they can bring down the LOS in the hospital.
“That meant more money in their own pockets because the medical group was taking the risk.”
Once hospitalists set up practice in a hospital, C-suite administrators quickly saw them gaining patient share and began realizing that they could be partners.
“They woke up one day, and just like that, they pay attention to how many cases the orthopedist does,” she says. “[They said], ‘Oh, Dr. Smith did 10 cases last week, he did 10 cases this week, then he did no cases or he did two cases. … They started to come to the hospitalists and say, ‘Look, you’re controlling X% of my patients a day. We’re having a length of stay problem; we’re having an early-discharge problem.’ Whatever it was, they were looking for partners to try to solve these issues.”
And when hospitalists grew in number again as the model continued to take hold and blossom as an effective care-delivery method, hospitalists again were turned to as partners.
“Once you get to that point, that you’re seeing enough patients and you’re enough of a movement,” Dr. Gorman says, “you get asked to be on the pharmacy committee and this committee, and chairman of the medical staff, and all those sort of things, and those evolve over time.”
Tech Effect
In the last 20 years, HM and technology have drastically changed the hospital landscape. But was HM pushed along by generational advances in computing power, smart devices in the shape of phones and tablets, and the software that powered those machines? Or was technology spurred on by having people it could serve directly in the hospital, as opposed to the traditionally fragmented system that preceded HM?
“Bob [Wachter] and others used to joke that the only people that actually understand the computer system are the hospitalists,” Dr. Goldman notes.
“Chicken or the egg, right?” adds Dr. Merlino of Press Ganey. “Technology is an enabler that helps providers deliver better care. I think healthcare quality in general has been helped by both.
“It doesn’t just help make hospitalists work better. It makes nursing better. It makes surgeons better. It makes pharmacy better.”
Dr. Bessler of Sound Physicians notes that advances in technology have come with their hurdles as well. Take the oft-maligned world of electronic medical records (EMRs).
“EMRs are great for data, but they’re not workflow solutions,” Dr. Bessler says. “They don’t tell you what do next.”
So Sound Physicians created its own technology platform, dubbed Sound Connect, that interacts with in-place EMRs at hospitals across the country. The in-house system takes the functional documentation of EMRs and overlays productivity protocols, Dr. Bessler says.
“It allows us to run a standard workflow and drive reproducible results and put meaningful data in the hands of the docs on a daily basis in the way that an EMR is just not set up to do,” he adds. Technology will continue “to be instrumental, of course, but I think the key thing is interoperability, which plenty has been written on, so we’re not unique in that. The more the public demands and the clinicians demand … the better patient care will be. I think the concept of EMR companies not being easy to work with has to end.”
Kendall Rogers, MD, CPE, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, believes that hospitalists have to take ownership of health information technology (HIT) in their own buildings.
He and other SHM officials have pushed hospitalists for the past few years to formalize their HIT duties by seeing if they would qualify to take the exam for board certification in medical informatics, which was created in 2013 by the American Board of Medical Specialties (ABMS). Between certification of that skill set and working more with technology vendors and others to improve HIT, Dr. Rogers sees HM being able to help reform much of the current technology woes in just a few years.
“To me, this is the new frontier,” Dr. Wachter says. “If our defining mantra as a field is, ‘How do we make care better for patients, and how do we create a better system?’ … well, I don’t see how you say that without really owning the issue of informatics.”
Teamwork: An HM Tradition
Hospitalists are often referred to as the quarterbacks of the hospital. But even the best QB needs a good team to succeed. For HMGs, that roster increasingly includes nurse practitioners (NPs) and physician assistants (PAs).
Recent State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs, and SHM earlier this year added Tracy Cardin, ACNP-BC, SFHM, as its first non-physician voting board member.
Dr. Donaldson believes that integrating hospitalists and non-physician providers (NPPs) allows both sets of practitioners to “work at the top of their license.”
“Any time when nurse practitioners and other providers get together, there is always this challenge of professions,” he says. “You’re doing this or you’re doing that, and once you get people who understand what the capabilities are past the title name and what you can do, it’s just amazing.”
Dr. Donaldson sees SHM’s acceptance of NPs and PAs as a good sign for HM.
“The day is upon us where we need to strongly consider nurse practitioners and physician assistants as equal in the field,” he says. “We’re going to find a much better continuity of care for all our patients at various institutions with hospital medicine and … a nurse practitioner who is at the top of their license.”
The Post-Acute Space
Aside from NPs and PAs, another extension of HM has been the gravitation in recent years of hospitalists into post-acute-care settings, including skilled-nursing facilities (SNFs), long-term care facilities, post-discharge clinics, and patient-centered homes.
Dr. Bessler says that as HMGs continued to focus on improving quality and lowering costs, they had little choice but to get involved in activities outside the hospital.
“We got into post-acute medicines because there was an abyss in quality,” he says. “We were accountable to send patients out, and there was nobody to send them to. Or the quality of the facilities was terrible, or the docs or clinicians weren’t going to see those patients regularly. That’s how we got into solving post-acute.”
Dr. Gorman, formerly the chief executive of St. Louis–based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine, agrees that for hospitalists to exert even more control over quality of care, they have to team with people outside the hospital.
“If we can’t build what I think of as a pyramid of care with one doctor and many, many other people supporting a broad group of patients, I don’t think we’re going to be able to find the scale to take care of the aging population that’s coming at us,” she says.
Caring for patients once they are discharged means including home nurses, pharmacists, physical therapists, dietitians, hired caregivers, and others in the process, Dr. Gorman says. But that doesn’t mean overburdening the wrong people with the wrong tasks. The same way no one would think to allow a social worker to prescribe medication is the same way that a hospitalist shouldn’t be the one checking up on a patient to make sure there is food in that person’s fridge.
And while the hospitalist can work in concert with others and run many things from the hospital, maybe hospital-based physicians aren’t always the best physicians for the task.
“There are certain things that only the doctor can do, of course, but there are a lot more things that somebody else can do,” Dr. Gorman says, adding, “some of the times, you’re going to need the physician, it’s going to be escalated to a medication change, but sometimes maybe you need to escalate to a dietary visit or you need to escalate to three physical therapy visits.
“The nitty-gritty of taking care of people outside of the hospital is so complex and problematic, and most of the solutions are not really medical, but you need the medical part of the dynamic. So rather [than a hospitalist running cases], it’s a super-talented social worker, nurse, or physical therapist. I don’t know, but somebody who can make sure that all of that works and it’s a process that can be leveraged.”
Whoever it is, the gravitation beyond the walls of the hospital has been tied to a growing sea change in how healthcare will compensate providers. Medicare has been migrating from fee-for-service to payments based on the totality of care for decades. The names change, of course. In the early 1980s, it was an “inpatient prospective payment system.”
Five years ago, it was accountable care organizations and value-based purchasing that SHM glommed on to as programs to be embraced as heralding the future.
Now it’s the Bundled Payments for Care Improvement initiative (BCPI), introduced by the Center for Medicare & Medicaid Innovation (CMMI) at the Centers for Medicare & Medicaid Services (CMS) back in 2011 and now compiling its first data sets for the next frontier of payments for episodic care.
BCPI was mandated by the Patient Protection and Affordable Care Act (ACA) of 2009, which included a provision that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association. BCPI now has more than 650 participating organizations, not including thousands of physicians who then partner with those groups, over four models. The initiative covers 48 defined episodes of care, both medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“The bundled model [BCPI] gives us the flexibility, scale, and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
A Score of Success
Twenty years of unbridled growth is great in any business. Put in perspective, the first iPhone, which redefined personal communication, is just nine years old, and already, stock analysts question whether Apple can grow any bigger or if it’s plateaued.
To be sure, the field of HM and its leaders have accomplished more than even Dr. Wachter and Dr. Goldman envisioned 20 summers ago. Much of it may seem so easily established by now, but when pioneering hospitalists John Nelson, MD, MHM, and Winthrop Whitcomb, MD, MHM, founded the National Association of Inpatient Physicians (NAIP) a year after the NEJM paper, they promoted and held a special session at UCSF’s first “Management of the Hospitalized Patient” conference in April 1997.
By 2003, the term “hospitalist” had become ubiquitous enough that NAIP was renamed the Society of Hospital Medicine.
Again, progress followed quickly.
By 2007, SHM had launched Project BOOST (Better Outcomes by Optimizing Safe Transitions), an award-winning mentored-implementation program to reduce LOS, adverse events, and unnecessary 30-day readmissions. Other mentored-implementation programs followed. The Glycemic Control Mentored Implementation (GCMI) program focuses on preventing hypoglycemia, while the Venous Thromboembolism Prevention Collaborative (VTE PC) seeks to give practical assistance on how to reduce blood clots via a VTE prevention program.
In 2012, SHM earned the 2011 John M. Eisenberg Patient Safety and Quality Award for Innovation in Patient Safety and Quality at the National Level, thanks to its mentored-implementation programs. SHM was the first professional society to earn the award, bestowed by the National Quality Forum (NQF) and The Joint Commission.
And earlier this year, CMS announced that by this time next year hospitalists would be assigned their own specialty designation code. SHM’s Public Policy Committee lobbied for the move for more than two years.
Dr. Merlino says it’s not just accomplishments that have set the field apart in its first 20 years. It’s the people.
Take Modern Healthcare’s list of the 50 Most Influential Physician Executives and Leaders of 2016. Third on the list is pediatric hospitalist Patrick Conway, MD, MSc, MHM, deputy administrator for innovation and quality and CMS’s chief medical officer. One spot behind him is Dr. Wachter, who in addition to being an architect of the HM movement was the first hospitalist to serve as chair of the Board of Directors of the American Board of Internal Medicine, which provides certification for the majority of working hospitalists.
Rounding out HM’s presence on the list is Vivek Murthy, MD, MBA, a Boston hospitalist and the current U.S. Surgeon General.
“It does demonstrate the emergence of their leadership,” Dr. Merlino says. “I don’t think yet they’re viewed as being the leaders, but I would add to that I don’t think they have yet the respect they deserve for the work they’re doing. When people who have worked with them can understand the value that they bring to clinical care, they clearly view hospitalists as being critical leaders.”
The Future
So what now? For all the talk of SHM’s success, HM’s positive impacts, and the specialty’s rocket growth trajectory, the work isn’t done, industry leaders say.
Hospitalists are not just working toward a more valuable delivery of care, they’re also increasingly viewed as leaders of projects all around the hospital because, well, they are always there, according to Dr. Gandhi.
“Hospitalists really are a leader in the hospital around quality and safety issues because they are there on the wards all the time,” she says. “They really have an interest in being the physician champions around various initiatives, so [in my hospital tenures] I partnered with many of my hospitalist colleagues on ways to improve care, such as test-result management, medication reconciliation, and similar efforts. We often would establish multidisciplinary committees to work on things, and almost always there was a hospitalist who was chairing or co-chairing or participating very actively in that group.”
Dr. Gandhi, who was finishing her second year of residency at Duke Medical Center in Raleigh, N.C., when the NEJM paper was published, sees the acuity of patients getting worse in the coming years as America rapidly ages. Baby boomers will start turning 80 in the next decade, and longer life spans translate to increasing medical problems that will often require hospitalization.
And while hospitalists have already moved into post-acute-care settings, Dr. Bessler says that will become an even bigger focus in the next 20 years of the specialty.
“It’s not generally been the psyche of the hospitalist in the past to feel accountable beyond the walls of the hospital,” he says. “But between episodic care [and] bundled payments … you can’t just wash your hands of it. You have to understand your next site-of-care decision. You need to make sure care happens at the right location.”
At a time of once-in-a-generation reform to healthcare in this country, the leaders of HM can’t afford to rest on their laurels, says Dr. Goldman. Three years ago, he wrote a paper for the Journal of Hospital Medicine titled “An Intellectual Agenda for Hospitalists.” In short, Dr. Goldman would like to see hospitalists move more into advancing science themselves rather than implementing the scientific discoveries of others. He cautions anyone against taking that as criticism of the field.
“If hospitalists are going to be the people who implement what other people have found, they run the risk of being the ones who make sure everybody gets perioperative beta-blockers even if they don’t really work,” he says. “If you want to take it to the illogical extreme, you could have people who were experts in how most efficiently to do bloodletting.
“The future for hospitalists, if they’re going to get to the next level—I think they can and will—is that they have to be in the discovery zone as well as the implementation zone.”
Dr. Wachter says it’s about staying ahead of the curve. For 20 years, the field has been on the cutting edge of how hospitals treat patients. To grow even more, it will be crucial to keep that focus.
Hospitalists need to continue to take C-suite positions at hospitals and policy roles at think tanks and governmental agencies. They need to continue to master technology, clinical care, and the ever-growing importance of where those two intersect.
Most of all, the field can’t get lazy. Otherwise, the “better mousetrap” of HM might one day be replaced by the next group of physicians willing to work harder to implement their great idea.
“If we continue to be the vanguard of innovation, the vanguard of making the system work better than it ever has before,” Dr. Wachter says, “the field that creates new models of care, that integrates technology in new ways, and that has this can-do attitude and optimism, then the sky is the limit.” TH
Richard Quinn is a freelance writer in New Jersey.
References
- Diamond HS, Goldberg E, Janosky JE. The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med. 1998;129(3):197-203.
AAP Proposes Update to Evaluating, Managing Febrile Infants Guideline
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
Presenter: Kenneth Roberts, MD
One of PHM16’s most highly attended sessions was about anticipated updated from the American Academy of Pediatrics (AAP) to its guidelines for febrile infants ages 7¬–90 days. The proposed update stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The proposed inclusion criteria for infants for this algorithm require an infant to be full-term (37–43 weeks’ gestation), aged 7–90 days, well-appearing, and presenting with a temperature of 38°C. Proposed exclusion criteria include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
The proposed guideline update will aim to stratify management by ages 7–28 days, 29–60 days, and 61–90 days to provide the most appropriate and directed treatment. It will also include a role for inflammatory markers and allow for a “kinder, gentler” approach, including withholding certain treatments and procedures if infants are at low risk of infection. An active need for observation may be appropriate for certain infants as well.
Key Takeaway
It is likely that the AAP will update its algorithm for the management of well-appearing febrile infants ages 7–28 days, 29–60 days and 60–90 days. It will help standardize care in this population but should not be used as a substitute for clinical judgment. The new guidelines are expected to be published in early 2017.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System and instructor of pediatrics at George Washington University School of Medicine & Health Sciences in Washington, D.C.
PHM16: Tips on Meeting Needs of Children with a Medical Complexity
Presenters: Mary L Ehlenbach, MD, FAAP; Megan Z Cardoso, MD, FAAP; and Christina Kleier, ARNP, PNP
This session at PHM16 was focused on logistical tips on how to build a pediatric complex care program. Presenters opened with a discussion of how to define children with medical complexity going through a variety of different methods including some research based aggregation of ICD-10 codes, referral from both families and other providers, and identifying patients by consumption of hospital resources. The presentation continued by highlighting that although medically complex children make up only a small percentage of the overall population of children, they account for about 1/3 of healthcare spending and due to advances in technology and medicine this group of children is growing in numbers. This group makes up about 10% of all pediatric admissions.
The session then went on to break down into four small groups which focused on details about how to create a complex care program and how to evaluate effectiveness of the program. Group 1 discussed methods of identifying patients that the program will serve. This included setting guidelines if a certain group or diagnosis should be excluded from the program. Different models of what services were also discussed which ranged from providing a comprehensive medical home to inpatient consults or care coordination services. The second group focused on what team members it may be beneficial to have involved. Team composition varied widely usually including MDs, NPs, social workers, RNs and at times a documentation expert who could aid with proper billing to boost revenue. The third group focused on how to measure quality services including family surveys of quantitative impact and satisfaction, PCP satisfaction. The final session consisted of the business and financial considerations of beginning a complex care program.
Key Takeaways:
- Children with medical complexity are a growing population on which a large proportion of healthcare resources are utilized. A program dedicated to serving the needs of this population may be helpful in reducing costs and improving the patient and family experience during hospitalizations.
- When working to initiate a complex care program:
- Set clear guidelines about which children the program is intended to serve and in what capacity it will function.
- Ensure the team composition is sustainable and meets the needs of the patients.
- Aggregate data about if the program is helping. This may be difficult to quantify since these are mostly qualitative measures.
- Include team members who are non-clinical to aid in improving hospital revenue and highlighting program benefits to the institution.
Margaret Rush, MD, is a hospitalist fellow at Children's National Medical Center in Washington D.C.
Presenters: Mary L Ehlenbach, MD, FAAP; Megan Z Cardoso, MD, FAAP; and Christina Kleier, ARNP, PNP
This session at PHM16 was focused on logistical tips on how to build a pediatric complex care program. Presenters opened with a discussion of how to define children with medical complexity going through a variety of different methods including some research based aggregation of ICD-10 codes, referral from both families and other providers, and identifying patients by consumption of hospital resources. The presentation continued by highlighting that although medically complex children make up only a small percentage of the overall population of children, they account for about 1/3 of healthcare spending and due to advances in technology and medicine this group of children is growing in numbers. This group makes up about 10% of all pediatric admissions.
The session then went on to break down into four small groups which focused on details about how to create a complex care program and how to evaluate effectiveness of the program. Group 1 discussed methods of identifying patients that the program will serve. This included setting guidelines if a certain group or diagnosis should be excluded from the program. Different models of what services were also discussed which ranged from providing a comprehensive medical home to inpatient consults or care coordination services. The second group focused on what team members it may be beneficial to have involved. Team composition varied widely usually including MDs, NPs, social workers, RNs and at times a documentation expert who could aid with proper billing to boost revenue. The third group focused on how to measure quality services including family surveys of quantitative impact and satisfaction, PCP satisfaction. The final session consisted of the business and financial considerations of beginning a complex care program.
Key Takeaways:
- Children with medical complexity are a growing population on which a large proportion of healthcare resources are utilized. A program dedicated to serving the needs of this population may be helpful in reducing costs and improving the patient and family experience during hospitalizations.
- When working to initiate a complex care program:
- Set clear guidelines about which children the program is intended to serve and in what capacity it will function.
- Ensure the team composition is sustainable and meets the needs of the patients.
- Aggregate data about if the program is helping. This may be difficult to quantify since these are mostly qualitative measures.
- Include team members who are non-clinical to aid in improving hospital revenue and highlighting program benefits to the institution.
Margaret Rush, MD, is a hospitalist fellow at Children's National Medical Center in Washington D.C.
Presenters: Mary L Ehlenbach, MD, FAAP; Megan Z Cardoso, MD, FAAP; and Christina Kleier, ARNP, PNP
This session at PHM16 was focused on logistical tips on how to build a pediatric complex care program. Presenters opened with a discussion of how to define children with medical complexity going through a variety of different methods including some research based aggregation of ICD-10 codes, referral from both families and other providers, and identifying patients by consumption of hospital resources. The presentation continued by highlighting that although medically complex children make up only a small percentage of the overall population of children, they account for about 1/3 of healthcare spending and due to advances in technology and medicine this group of children is growing in numbers. This group makes up about 10% of all pediatric admissions.
The session then went on to break down into four small groups which focused on details about how to create a complex care program and how to evaluate effectiveness of the program. Group 1 discussed methods of identifying patients that the program will serve. This included setting guidelines if a certain group or diagnosis should be excluded from the program. Different models of what services were also discussed which ranged from providing a comprehensive medical home to inpatient consults or care coordination services. The second group focused on what team members it may be beneficial to have involved. Team composition varied widely usually including MDs, NPs, social workers, RNs and at times a documentation expert who could aid with proper billing to boost revenue. The third group focused on how to measure quality services including family surveys of quantitative impact and satisfaction, PCP satisfaction. The final session consisted of the business and financial considerations of beginning a complex care program.
Key Takeaways:
- Children with medical complexity are a growing population on which a large proportion of healthcare resources are utilized. A program dedicated to serving the needs of this population may be helpful in reducing costs and improving the patient and family experience during hospitalizations.
- When working to initiate a complex care program:
- Set clear guidelines about which children the program is intended to serve and in what capacity it will function.
- Ensure the team composition is sustainable and meets the needs of the patients.
- Aggregate data about if the program is helping. This may be difficult to quantify since these are mostly qualitative measures.
- Include team members who are non-clinical to aid in improving hospital revenue and highlighting program benefits to the institution.
Margaret Rush, MD, is a hospitalist fellow at Children's National Medical Center in Washington D.C.
PHM16: Visual Clues Can Help Establish a Diagnosis
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16’s Visual Diagnosis: Signs and Why They Matter session led by Dr. Kenneth Roberts and guest presenters was a review of case presentations in which visual clues were vital to establishing a diagnosis. Though much of the content was presented with pictures, the emphasis was placed on the importance of correct diagnosis to avoid both misdiagnoses/over-diagnoses and the potential harm that may result from inappropriate treatment. This may also translate into poor utilization of resources and significant financial burden that can result from the unnecessary hospitalization of a patient.
Many of the presented cases (such as the Gianotti-Crosti toddler over-diagnosed as eczema herpeticum, a child with pseudochromhidrosis misdiagnosed as a cyanotic disease, the case of phytophotodermatitis mistaken as child abuse, and a teen treated for 2 years for JIA before diagnosis of hypertrophic osteoarthropathy was made) highlighted examples in which there was extensive workup, hospitalization, subspecialty evaluation, and even incorrect treatment of patients.
In other instances, such as Henoch-Schonlein purpura, Waardenburg syndrome, or McCune-Albright syndrome, the correct diagnosis is necessary to help guide management and future treatment, including subspecialty evaluation.
Many diseases with visual presentations also have a benign course and require no treatment, and acknowledging this is important in providing reassurance to a family that may be very anxious over the physical appearance of their child.
This session underscores the need for experience and exposure to various signs, not only with rare medical conditions, but also in common illnesses such as Kawasaki and scarlet fever that may present similarly.
Key Takeaway:
Providers should have a high index of suspicion and use visual clues to make the correct diagnosis in order to guide treatment, avoid harm in children, and ensure appropriate utilization of resources.
Chandani DeZure, MD, FAAP, is a pediatric Hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16: The New AAP Clinical Practice Guideline on Evaluating, Managing Febrile Infants
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
One of PHM16’s most highly-attended sessions was an update on the anticipated AAP guidelines for febrile infants between ages 7-90 days given by Dr. Kenneth Roberts. The goal is to give evidence-based guidelines, not rules, from the most recent literature available. It also stresses the need to separate individual components of serious bacterial infections (UTI, bacteremia, and meningitis) as the incidence and clinical course can vary greatly in this population.
The inclusion criteria for infants for this upcoming algorithm require an infant to be full-term (37-43 weeks gestation), aged 7-90 days, well-appearing, and presenting with a temperature of 38 degrees Celsius.
Exclusion criteria include perinatal/prenatal/neonatal: maternal fever, infection, or antimicrobial treatment, the presence of any evident infection, being technology-dependent, and the presence of congenital anomalies.
The updated guideline will aim to stratify management by age 7-28 days, 29-60 days, and 61 to 90 days to provide the most appropriate and directed treatment.
It will also include a role for inflammatory markers, and allow for a “kinder, gentler” approach to the management of febrile infants aged 7-90 days including withholding certain treatments and procedures if infants are at low risk of infection. An active, not passive, need for observation may be appropriate for certain infants as well. These guidelines should be tailored for individual patients to provide the best care possible while minimizing risk in this population.
Key Takeaway:
An updated AAP Practice guideline algorithm for the management of well-appearing febrile infants 7-28 days, 29-60 days, and 60-90 days will be coming in the near future that will help standardize care in this population, but should not be used as a substitute for clinical judgment.
Chandani DeZure, MD, FAAP, is a pediatric hospitalist at Children’s National Health System, Instruction of Pediatrics at George Washington University’s School of Medicine and Health Sciences in Washington, D.C.
PHM16: How to Design, Improve Educational Programs at Community Hospitals
Facilitators: Christopher Russo, MD, FAAP, Laura Hodo, MD, and Lauren Wilson, MD
This session discussed ways to design and improve education within community hospital settings. It was done via a didactic session, breakout groups, and an electronic assessment tool that can be used beyond the session. Facilitators included the workshop leaders and co-leaders along with current PHM fellows and educators from community and academic settings.
During the didactic session a general background of importance of education during times of increasing academic and community site affiliations was discussed. This included the strengths of community hospitals for learners such as “appropriate learner autonomy”, “exposure to different career paths”, and “transfer decision-making”.
Some of the challenges discussed in regards to developing an educational structure in community settings included:
- Logistics
- Making the case for education
- Legal framework (i.e. Affiliation agreements, Liability)
- Finances (i.e. GME funding)
- Paperwork burden (ex. Licensing, Credentialing)
- Learning Environment
- Complementing clinical work with materials
- Autonomy/Supervision balancing
- Developing Clinical teachers
The didactic session also reviewed the 6 steps for curriculum development: General Needs Assessment, Targeted Needs Assessment, Goals and Objectives, Educational Strategies, Implementation, and Evaluation/Feedback. Each of these was described in further detail with relevant examples.
Groups were broken out into small groups based on four learner types: Medical Students, Family Medicine Residents, Pediatric Residents, and PHM Fellows. Within each group a “Program Development Matrix” was distributed to assess the support from leadership and logistics within each setting. Each one of these was separated into subgroups such as credentialing, financial support, housing/travel, and preceptor recruitment.
A separate “Curriculum Development Matrix” was utilized during breakout groups that focused on curriculum development. This matrix was broken into 3 areas: Educational Strategies, Implementation, and Evaluation/Feedback. These were broken down into subgroups such as content, identifying resources, and remediation planning. The group was asked to determine short and long term goals with action steps for both of these matrix subgroups.
Overall the session presented a structured way of assessing the educational environment for learners in community settings. It gave tangible tools to develop a needs assessment and planning to achieve the defined goals that can be readily used by sites who wish to develop or improve their current educational framework.
Dr. Francisco Alvarez, MD, FAAP, is a pediatric hospitalist and director of the Children's National Health System Community Hospital Services in Washington, D.C.
Facilitators: Christopher Russo, MD, FAAP, Laura Hodo, MD, and Lauren Wilson, MD
This session discussed ways to design and improve education within community hospital settings. It was done via a didactic session, breakout groups, and an electronic assessment tool that can be used beyond the session. Facilitators included the workshop leaders and co-leaders along with current PHM fellows and educators from community and academic settings.
During the didactic session a general background of importance of education during times of increasing academic and community site affiliations was discussed. This included the strengths of community hospitals for learners such as “appropriate learner autonomy”, “exposure to different career paths”, and “transfer decision-making”.
Some of the challenges discussed in regards to developing an educational structure in community settings included:
- Logistics
- Making the case for education
- Legal framework (i.e. Affiliation agreements, Liability)
- Finances (i.e. GME funding)
- Paperwork burden (ex. Licensing, Credentialing)
- Learning Environment
- Complementing clinical work with materials
- Autonomy/Supervision balancing
- Developing Clinical teachers
The didactic session also reviewed the 6 steps for curriculum development: General Needs Assessment, Targeted Needs Assessment, Goals and Objectives, Educational Strategies, Implementation, and Evaluation/Feedback. Each of these was described in further detail with relevant examples.
Groups were broken out into small groups based on four learner types: Medical Students, Family Medicine Residents, Pediatric Residents, and PHM Fellows. Within each group a “Program Development Matrix” was distributed to assess the support from leadership and logistics within each setting. Each one of these was separated into subgroups such as credentialing, financial support, housing/travel, and preceptor recruitment.
A separate “Curriculum Development Matrix” was utilized during breakout groups that focused on curriculum development. This matrix was broken into 3 areas: Educational Strategies, Implementation, and Evaluation/Feedback. These were broken down into subgroups such as content, identifying resources, and remediation planning. The group was asked to determine short and long term goals with action steps for both of these matrix subgroups.
Overall the session presented a structured way of assessing the educational environment for learners in community settings. It gave tangible tools to develop a needs assessment and planning to achieve the defined goals that can be readily used by sites who wish to develop or improve their current educational framework.
Dr. Francisco Alvarez, MD, FAAP, is a pediatric hospitalist and director of the Children's National Health System Community Hospital Services in Washington, D.C.
Facilitators: Christopher Russo, MD, FAAP, Laura Hodo, MD, and Lauren Wilson, MD
This session discussed ways to design and improve education within community hospital settings. It was done via a didactic session, breakout groups, and an electronic assessment tool that can be used beyond the session. Facilitators included the workshop leaders and co-leaders along with current PHM fellows and educators from community and academic settings.
During the didactic session a general background of importance of education during times of increasing academic and community site affiliations was discussed. This included the strengths of community hospitals for learners such as “appropriate learner autonomy”, “exposure to different career paths”, and “transfer decision-making”.
Some of the challenges discussed in regards to developing an educational structure in community settings included:
- Logistics
- Making the case for education
- Legal framework (i.e. Affiliation agreements, Liability)
- Finances (i.e. GME funding)
- Paperwork burden (ex. Licensing, Credentialing)
- Learning Environment
- Complementing clinical work with materials
- Autonomy/Supervision balancing
- Developing Clinical teachers
The didactic session also reviewed the 6 steps for curriculum development: General Needs Assessment, Targeted Needs Assessment, Goals and Objectives, Educational Strategies, Implementation, and Evaluation/Feedback. Each of these was described in further detail with relevant examples.
Groups were broken out into small groups based on four learner types: Medical Students, Family Medicine Residents, Pediatric Residents, and PHM Fellows. Within each group a “Program Development Matrix” was distributed to assess the support from leadership and logistics within each setting. Each one of these was separated into subgroups such as credentialing, financial support, housing/travel, and preceptor recruitment.
A separate “Curriculum Development Matrix” was utilized during breakout groups that focused on curriculum development. This matrix was broken into 3 areas: Educational Strategies, Implementation, and Evaluation/Feedback. These were broken down into subgroups such as content, identifying resources, and remediation planning. The group was asked to determine short and long term goals with action steps for both of these matrix subgroups.
Overall the session presented a structured way of assessing the educational environment for learners in community settings. It gave tangible tools to develop a needs assessment and planning to achieve the defined goals that can be readily used by sites who wish to develop or improve their current educational framework.
Dr. Francisco Alvarez, MD, FAAP, is a pediatric hospitalist and director of the Children's National Health System Community Hospital Services in Washington, D.C.
Tips for Communicating with Empathy
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each column will focus on how the contributor applies one of the “Key Communication” areas in practice.
View a chart outlining key communication tactics
What I Say and Do
In interactions with patients and families, I make sure I communicate with empathy. By communicating with empathy, I mean not only listening for and understanding a patient’s experiences, concerns, and perspective but also communicating this understanding with my intention to help.
Why I Do It
Time constraints, endless to-do lists, and racing minds can eclipse empathic, attentive, and personalized care. When empathy is missing from the patient-clinician relationship, patients and clinicians suffer. Patients feel disengaged from their clinician; they remain anxious and lose trust. And physicians miss out on the gratification of feeling connected with patients and on achieving the best possible patient engagement and outcomes.
Physician empathy is associated with not only higher levels of patient satisfaction and survey scores but also with patient engagement, adherence to care plans, and positive health outcomes as well as physician job satisfaction.1–3
How I Do It
I start with mindfulness. I sustain eye contact, sit eye to eye, and give the person my undivided attention, listening to their words and nonverbal behavior—without judgment.
Then I draw on several techniques that express empathy. My favorites are these:
On a Personal Note
Albert Schweitzer said, “At times, our own light goes out and is rekindled by a spark from another person. Each of us has cause to think with deep gratitude of those who have lighted the flame within us.” Communicating with empathy, to me, is the spark that rekindles the lights of patients, families, and colleagues in our relationships with them. TH
Wendy Leebov is founder and partner in Language of Caring, LLC, author of The Language of Caring Guide for Physicians, and developer of the Language of Caring for Physicians web-based learning program. Reach her at [email protected].
References
- Leebov W, Rotering C. The Language of Caring Guide for Physicians: Communication Essentials for Patient-Centered Care. 2nd ed. Language of Caring, LLC; 2015.
- Butterfield S. New research links empathy to outcomes. ACP Internist website. Available at: http://www.acpinternist.org/archives/2013/03/empathy.htm. Accessed July 8, 2016.
- Hojat M, Louis D, Maio V, Gonnella J. Empathy and health care quality. Am J Medical Quality. 2013;28(1):6-7.