User login
Overworked Hospitalists Linked to Higher Costs, Longer Lengths of Stay
As hospitalist workloads increase, so do hospital costs and patients' lengths of stay (LOS), according to findings in a recent study.
Those results, says SHM President Burke T. Kealey, MD, SFHM, provide a good starting point to determine an ideal patient census for hospitalists.
"Pushing hospitalist workloads ever higher to meet the demands of patient-care needs or flawed payment models has costs associated with it," says Dr. Kealey, associate medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. "The costs may be borne by the system or by patients, but there are costs."
For the study published in JAMA Internal Medicine, researchers analyzed data from 20,241 hospitalizations involving 13,916 patients seen by hospitalists at the Christiana Care Health System in Newark, Del., between February 2008 and January 2011.
For hospital occupancies less than 75%, they found that LOS increased from 5.5 to 7.5 days as workload increased. For occupancies of 75% to 85%, LOS increased to about 8 days with higher workloads. For occupancies greater than 85%, the LOS decreased slightly and then increased significantly with higher workloads, with this change occurring at about 15 patients or more per hospitalist.
Costs were also significantly associated with an increase in workload. As the study notes, benchmark recommendations for an individual hospitalist’s workload range from 10 to 15 patient encounters per day.
Dr. Kealey says the findings seem to support the conventional wisdom that hospitalists should ideally see no more than 15 patients a day. He notes, however, that deciding the optimal number of cases for a given practice depends on several factors, including duration of shift, the availability of physician extenders, and the addition of surgical or cardiology cases.
"We won't be able as a specialty to fully realize our potential until we understand and apply the learnings about workload into our practices to ensure hospitalist career sustainability, system health, and best patient care," Dr. Kealey says. "This paper really gets the discussion going."
For more from Dr. Kealey on hospitalist workloads, read his recent blog post on "The Hospital Leader." TH
Visit our website for more information about hospitalist workloads.
As hospitalist workloads increase, so do hospital costs and patients' lengths of stay (LOS), according to findings in a recent study.
Those results, says SHM President Burke T. Kealey, MD, SFHM, provide a good starting point to determine an ideal patient census for hospitalists.
"Pushing hospitalist workloads ever higher to meet the demands of patient-care needs or flawed payment models has costs associated with it," says Dr. Kealey, associate medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. "The costs may be borne by the system or by patients, but there are costs."
For the study published in JAMA Internal Medicine, researchers analyzed data from 20,241 hospitalizations involving 13,916 patients seen by hospitalists at the Christiana Care Health System in Newark, Del., between February 2008 and January 2011.
For hospital occupancies less than 75%, they found that LOS increased from 5.5 to 7.5 days as workload increased. For occupancies of 75% to 85%, LOS increased to about 8 days with higher workloads. For occupancies greater than 85%, the LOS decreased slightly and then increased significantly with higher workloads, with this change occurring at about 15 patients or more per hospitalist.
Costs were also significantly associated with an increase in workload. As the study notes, benchmark recommendations for an individual hospitalist’s workload range from 10 to 15 patient encounters per day.
Dr. Kealey says the findings seem to support the conventional wisdom that hospitalists should ideally see no more than 15 patients a day. He notes, however, that deciding the optimal number of cases for a given practice depends on several factors, including duration of shift, the availability of physician extenders, and the addition of surgical or cardiology cases.
"We won't be able as a specialty to fully realize our potential until we understand and apply the learnings about workload into our practices to ensure hospitalist career sustainability, system health, and best patient care," Dr. Kealey says. "This paper really gets the discussion going."
For more from Dr. Kealey on hospitalist workloads, read his recent blog post on "The Hospital Leader." TH
Visit our website for more information about hospitalist workloads.
As hospitalist workloads increase, so do hospital costs and patients' lengths of stay (LOS), according to findings in a recent study.
Those results, says SHM President Burke T. Kealey, MD, SFHM, provide a good starting point to determine an ideal patient census for hospitalists.
"Pushing hospitalist workloads ever higher to meet the demands of patient-care needs or flawed payment models has costs associated with it," says Dr. Kealey, associate medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. "The costs may be borne by the system or by patients, but there are costs."
For the study published in JAMA Internal Medicine, researchers analyzed data from 20,241 hospitalizations involving 13,916 patients seen by hospitalists at the Christiana Care Health System in Newark, Del., between February 2008 and January 2011.
For hospital occupancies less than 75%, they found that LOS increased from 5.5 to 7.5 days as workload increased. For occupancies of 75% to 85%, LOS increased to about 8 days with higher workloads. For occupancies greater than 85%, the LOS decreased slightly and then increased significantly with higher workloads, with this change occurring at about 15 patients or more per hospitalist.
Costs were also significantly associated with an increase in workload. As the study notes, benchmark recommendations for an individual hospitalist’s workload range from 10 to 15 patient encounters per day.
Dr. Kealey says the findings seem to support the conventional wisdom that hospitalists should ideally see no more than 15 patients a day. He notes, however, that deciding the optimal number of cases for a given practice depends on several factors, including duration of shift, the availability of physician extenders, and the addition of surgical or cardiology cases.
"We won't be able as a specialty to fully realize our potential until we understand and apply the learnings about workload into our practices to ensure hospitalist career sustainability, system health, and best patient care," Dr. Kealey says. "This paper really gets the discussion going."
For more from Dr. Kealey on hospitalist workloads, read his recent blog post on "The Hospital Leader." TH
Visit our website for more information about hospitalist workloads.
Society of Hospital Medicine Sponsors Glycemic Control Mentored Implementation Program
Hyperglycemia is associated with poor outcomes in a broad range of hospitalized patients, and several studies demonstrate improved outcomes with improved glycemic control. Hospitalization presents a frequently missed opportunity to diagnose diabetes, identify those at risk for diabetes, and optimize the care of patients with diabetes via education and medical therapy.
Despite authoritative guidelines and effective methods to achieve good glycemic control safely, poor glycemic control, suboptimal medication regimens, incomplete patient education, and uneven communication with outpatient care providers are prevalent problems in medical centers.
SHM is accepting applications to the Fall 2014 Glycemic Control Mentored Implementation (GCMI) Program (www.hospitalmedicine.org/gcmi). Participants will work directly with SHM mentors, benchmark against other participants, and join the Glycemic Control Community to network with peers.
Hyperglycemia is associated with poor outcomes in a broad range of hospitalized patients, and several studies demonstrate improved outcomes with improved glycemic control. Hospitalization presents a frequently missed opportunity to diagnose diabetes, identify those at risk for diabetes, and optimize the care of patients with diabetes via education and medical therapy.
Despite authoritative guidelines and effective methods to achieve good glycemic control safely, poor glycemic control, suboptimal medication regimens, incomplete patient education, and uneven communication with outpatient care providers are prevalent problems in medical centers.
SHM is accepting applications to the Fall 2014 Glycemic Control Mentored Implementation (GCMI) Program (www.hospitalmedicine.org/gcmi). Participants will work directly with SHM mentors, benchmark against other participants, and join the Glycemic Control Community to network with peers.
Hyperglycemia is associated with poor outcomes in a broad range of hospitalized patients, and several studies demonstrate improved outcomes with improved glycemic control. Hospitalization presents a frequently missed opportunity to diagnose diabetes, identify those at risk for diabetes, and optimize the care of patients with diabetes via education and medical therapy.
Despite authoritative guidelines and effective methods to achieve good glycemic control safely, poor glycemic control, suboptimal medication regimens, incomplete patient education, and uneven communication with outpatient care providers are prevalent problems in medical centers.
SHM is accepting applications to the Fall 2014 Glycemic Control Mentored Implementation (GCMI) Program (www.hospitalmedicine.org/gcmi). Participants will work directly with SHM mentors, benchmark against other participants, and join the Glycemic Control Community to network with peers.
Society of Hospital Medicine Accepting Applications Through August for 2014 Project BOOST Cohort
Reducing unnecessary readmissions continues to be a priority for hospitals across the country, which is why so many hospitals have already enrolled in SHM’s Project BOOST. Project BOOST is an award-winning program that pairs hospitals with the national experts in reducing readmissions and resources to implement programs that work in the real world.
Early research indicates that Project BOOST can be effective: According to research published in the Journal of Hospital Medicine last year, participation in Project BOOST among a small sample set of hospitals appeared to be associated with a decrease in readmission rates.
And hospitals reducing readmissions through Project BOOST are receiving attention from their local communities, too. Recently, Lakes Region General Hospital was featured in an article in the local newspaper, The Laconia Daily Sun, entitled “LRGH finds preventable readmissions program is paying off.”
SHM is accepting applications to the 2014 Project BOOST cohort through August. For more information, visit www.hospitalmedicine.org/boost.
Reducing unnecessary readmissions continues to be a priority for hospitals across the country, which is why so many hospitals have already enrolled in SHM’s Project BOOST. Project BOOST is an award-winning program that pairs hospitals with the national experts in reducing readmissions and resources to implement programs that work in the real world.
Early research indicates that Project BOOST can be effective: According to research published in the Journal of Hospital Medicine last year, participation in Project BOOST among a small sample set of hospitals appeared to be associated with a decrease in readmission rates.
And hospitals reducing readmissions through Project BOOST are receiving attention from their local communities, too. Recently, Lakes Region General Hospital was featured in an article in the local newspaper, The Laconia Daily Sun, entitled “LRGH finds preventable readmissions program is paying off.”
SHM is accepting applications to the 2014 Project BOOST cohort through August. For more information, visit www.hospitalmedicine.org/boost.
Reducing unnecessary readmissions continues to be a priority for hospitals across the country, which is why so many hospitals have already enrolled in SHM’s Project BOOST. Project BOOST is an award-winning program that pairs hospitals with the national experts in reducing readmissions and resources to implement programs that work in the real world.
Early research indicates that Project BOOST can be effective: According to research published in the Journal of Hospital Medicine last year, participation in Project BOOST among a small sample set of hospitals appeared to be associated with a decrease in readmission rates.
And hospitals reducing readmissions through Project BOOST are receiving attention from their local communities, too. Recently, Lakes Region General Hospital was featured in an article in the local newspaper, The Laconia Daily Sun, entitled “LRGH finds preventable readmissions program is paying off.”
SHM is accepting applications to the 2014 Project BOOST cohort through August. For more information, visit www.hospitalmedicine.org/boost.
PODCAST: Highlights of the June 2014 issue of The Hospitalist
This month in our issue, 10 medical specialty groups offer Choosing Wisely guidelines for hospitalists. Among them, Dr. Linda Cox notes why comprehensive pulmonary assessment, including spirometry, is important to diagnosing or ruling out asthma; and otolaryngologist Dr. Rahul Shah tells why hospitalists should stop routine radiographic imaging for patients who meet the diagnostic criteria for uncomplicated acute rhinosinusitis. Meanwhile, ABIM Foundation executive vice president and CEO Daniel Wolfson talks about why the Choosing Wisely campaign is not just another attempt at cost-containment.
Also in this issue, legal advice for hospitalists on the intersection of social media and HIPAA rules, clinical practice guidelines on red blood cell transfusions, and our Key Clinical Question explores which patients should be screened for hepatitis C infection.
This month in our issue, 10 medical specialty groups offer Choosing Wisely guidelines for hospitalists. Among them, Dr. Linda Cox notes why comprehensive pulmonary assessment, including spirometry, is important to diagnosing or ruling out asthma; and otolaryngologist Dr. Rahul Shah tells why hospitalists should stop routine radiographic imaging for patients who meet the diagnostic criteria for uncomplicated acute rhinosinusitis. Meanwhile, ABIM Foundation executive vice president and CEO Daniel Wolfson talks about why the Choosing Wisely campaign is not just another attempt at cost-containment.
Also in this issue, legal advice for hospitalists on the intersection of social media and HIPAA rules, clinical practice guidelines on red blood cell transfusions, and our Key Clinical Question explores which patients should be screened for hepatitis C infection.
This month in our issue, 10 medical specialty groups offer Choosing Wisely guidelines for hospitalists. Among them, Dr. Linda Cox notes why comprehensive pulmonary assessment, including spirometry, is important to diagnosing or ruling out asthma; and otolaryngologist Dr. Rahul Shah tells why hospitalists should stop routine radiographic imaging for patients who meet the diagnostic criteria for uncomplicated acute rhinosinusitis. Meanwhile, ABIM Foundation executive vice president and CEO Daniel Wolfson talks about why the Choosing Wisely campaign is not just another attempt at cost-containment.
Also in this issue, legal advice for hospitalists on the intersection of social media and HIPAA rules, clinical practice guidelines on red blood cell transfusions, and our Key Clinical Question explores which patients should be screened for hepatitis C infection.
MERS Cases Put Hospitalists on Alert for Infectious Disease
Patients diagnosed with Middle East Respiratory Syndrome (MERS) in Indiana and Florida have healthcare workers and hospitalists on the lookout for additional cases of the potentially fatal respiratory infection.
Hospitalists should pay attention to patients exhibiting fever and respiratory symptoms who traveled to the Arabian Peninsula in the 14 days prior to disease onset, and contact the hospital epidemiologist if MERS is suspected, says James Pile, MD, vice chair of the department of hospital medicine at the Cleveland Clinic.
The CDC has reported three cases of MERS this month. The first, reported on May 2, involved a healthcare worker from Saudi Arabia who traveled to Indiana to visit family. The second was reported on May 11, when another visiting healthcare worker from Saudi Arabia checked into the emergency department in Orlando, Fla., after he fell ill with fever, chills, and a slight cough. Both patients are considered to be fully recovered.
The third MERS case is in an Illinois man who had a business meeting with the patient from Indiana and represents the first case of the virus being contracted in the U.S. A blood test confirmed that the Illinois man had been infected with the virus, but he’s reported that he no longer feels sick.
Caused by a coronavirus called MERS-CoV, MERS was first reported in Saudi Arabia in 2012. So far, there have been more than 600 confirmed cases around the world and 181 people have died, according to the World Health Organization.
"The CDC suggests that the index U.S. case represents a very low threat to the general population in this country, and my sense is that that this will not turn out to be a major issue for the U.S. healthcare system, but there’s still a lot we don’t know about MERS," Dr. Pile says. “The scope of the issue should become much clearer over the next couple of months.”
For more information on MERS, check out this CDC fact sheet.
Read physician editor Danielle Scheurer's recent blog post on the MERS situation.
Visit our website for more information about hospitalists and infectious disease care.
Patients diagnosed with Middle East Respiratory Syndrome (MERS) in Indiana and Florida have healthcare workers and hospitalists on the lookout for additional cases of the potentially fatal respiratory infection.
Hospitalists should pay attention to patients exhibiting fever and respiratory symptoms who traveled to the Arabian Peninsula in the 14 days prior to disease onset, and contact the hospital epidemiologist if MERS is suspected, says James Pile, MD, vice chair of the department of hospital medicine at the Cleveland Clinic.
The CDC has reported three cases of MERS this month. The first, reported on May 2, involved a healthcare worker from Saudi Arabia who traveled to Indiana to visit family. The second was reported on May 11, when another visiting healthcare worker from Saudi Arabia checked into the emergency department in Orlando, Fla., after he fell ill with fever, chills, and a slight cough. Both patients are considered to be fully recovered.
The third MERS case is in an Illinois man who had a business meeting with the patient from Indiana and represents the first case of the virus being contracted in the U.S. A blood test confirmed that the Illinois man had been infected with the virus, but he’s reported that he no longer feels sick.
Caused by a coronavirus called MERS-CoV, MERS was first reported in Saudi Arabia in 2012. So far, there have been more than 600 confirmed cases around the world and 181 people have died, according to the World Health Organization.
"The CDC suggests that the index U.S. case represents a very low threat to the general population in this country, and my sense is that that this will not turn out to be a major issue for the U.S. healthcare system, but there’s still a lot we don’t know about MERS," Dr. Pile says. “The scope of the issue should become much clearer over the next couple of months.”
For more information on MERS, check out this CDC fact sheet.
Read physician editor Danielle Scheurer's recent blog post on the MERS situation.
Visit our website for more information about hospitalists and infectious disease care.
Patients diagnosed with Middle East Respiratory Syndrome (MERS) in Indiana and Florida have healthcare workers and hospitalists on the lookout for additional cases of the potentially fatal respiratory infection.
Hospitalists should pay attention to patients exhibiting fever and respiratory symptoms who traveled to the Arabian Peninsula in the 14 days prior to disease onset, and contact the hospital epidemiologist if MERS is suspected, says James Pile, MD, vice chair of the department of hospital medicine at the Cleveland Clinic.
The CDC has reported three cases of MERS this month. The first, reported on May 2, involved a healthcare worker from Saudi Arabia who traveled to Indiana to visit family. The second was reported on May 11, when another visiting healthcare worker from Saudi Arabia checked into the emergency department in Orlando, Fla., after he fell ill with fever, chills, and a slight cough. Both patients are considered to be fully recovered.
The third MERS case is in an Illinois man who had a business meeting with the patient from Indiana and represents the first case of the virus being contracted in the U.S. A blood test confirmed that the Illinois man had been infected with the virus, but he’s reported that he no longer feels sick.
Caused by a coronavirus called MERS-CoV, MERS was first reported in Saudi Arabia in 2012. So far, there have been more than 600 confirmed cases around the world and 181 people have died, according to the World Health Organization.
"The CDC suggests that the index U.S. case represents a very low threat to the general population in this country, and my sense is that that this will not turn out to be a major issue for the U.S. healthcare system, but there’s still a lot we don’t know about MERS," Dr. Pile says. “The scope of the issue should become much clearer over the next couple of months.”
For more information on MERS, check out this CDC fact sheet.
Read physician editor Danielle Scheurer's recent blog post on the MERS situation.
Visit our website for more information about hospitalists and infectious disease care.
New SHM Board Member Ron Greeno, MD, FCCP, MHM, Sets High Bar for Health System Improvements
Ron Greeno, MD, FCCP, MHM, says he plans to bring his passion for improving the U.S. healthcare system to his new role representing the interests of hospitalists as a member of the Society of Hospital Medicine's Board of Directors.
"SHM is a nontraditional professional society in that we do believe in advocacy for members, but we also believe we're advocating for patients and the integrity of the American healthcare system," he says.
On his to-do list as an SHM board member, Dr. Greeno plans to focus on overhauling the observation status admissions system, developing solutions to fix the flawed Medicare Sustainable Growth Rate formula, and improving how the quality of patient care provided by hospitalists is measured.
As executive vice president for strategy and innovation at Brentwood, Tenn.–based Cogent Healthcare, Dr. Greeno says his enthusiasm for system improvement has only increased over the years. In his concurrent role as Chairman of SHM's Public Policy Committee, Dr. Greeno and committee members will continue to provide input on hospital management practices to such federal agencies as the Centers for Medicare & Medicaid Services and offer feedback on improving the Affordable Care Act.
SHM Board Member Brian Harte, MD, SFHM, who is treasurer of SHM's Public Policy Committee, says Dr. Greeno's passion for policy is infectious.
"Ron brings an enthusiasm to the issues that really energize the committee," Dr. Harte says. "He does a really good job facilitating an equitable discussion and reaching consensus on a position to recommend to the SHM board."
Ron Greeno, MD, FCCP, MHM, says he plans to bring his passion for improving the U.S. healthcare system to his new role representing the interests of hospitalists as a member of the Society of Hospital Medicine's Board of Directors.
"SHM is a nontraditional professional society in that we do believe in advocacy for members, but we also believe we're advocating for patients and the integrity of the American healthcare system," he says.
On his to-do list as an SHM board member, Dr. Greeno plans to focus on overhauling the observation status admissions system, developing solutions to fix the flawed Medicare Sustainable Growth Rate formula, and improving how the quality of patient care provided by hospitalists is measured.
As executive vice president for strategy and innovation at Brentwood, Tenn.–based Cogent Healthcare, Dr. Greeno says his enthusiasm for system improvement has only increased over the years. In his concurrent role as Chairman of SHM's Public Policy Committee, Dr. Greeno and committee members will continue to provide input on hospital management practices to such federal agencies as the Centers for Medicare & Medicaid Services and offer feedback on improving the Affordable Care Act.
SHM Board Member Brian Harte, MD, SFHM, who is treasurer of SHM's Public Policy Committee, says Dr. Greeno's passion for policy is infectious.
"Ron brings an enthusiasm to the issues that really energize the committee," Dr. Harte says. "He does a really good job facilitating an equitable discussion and reaching consensus on a position to recommend to the SHM board."
Ron Greeno, MD, FCCP, MHM, says he plans to bring his passion for improving the U.S. healthcare system to his new role representing the interests of hospitalists as a member of the Society of Hospital Medicine's Board of Directors.
"SHM is a nontraditional professional society in that we do believe in advocacy for members, but we also believe we're advocating for patients and the integrity of the American healthcare system," he says.
On his to-do list as an SHM board member, Dr. Greeno plans to focus on overhauling the observation status admissions system, developing solutions to fix the flawed Medicare Sustainable Growth Rate formula, and improving how the quality of patient care provided by hospitalists is measured.
As executive vice president for strategy and innovation at Brentwood, Tenn.–based Cogent Healthcare, Dr. Greeno says his enthusiasm for system improvement has only increased over the years. In his concurrent role as Chairman of SHM's Public Policy Committee, Dr. Greeno and committee members will continue to provide input on hospital management practices to such federal agencies as the Centers for Medicare & Medicaid Services and offer feedback on improving the Affordable Care Act.
SHM Board Member Brian Harte, MD, SFHM, who is treasurer of SHM's Public Policy Committee, says Dr. Greeno's passion for policy is infectious.
"Ron brings an enthusiasm to the issues that really energize the committee," Dr. Harte says. "He does a really good job facilitating an equitable discussion and reaching consensus on a position to recommend to the SHM board."
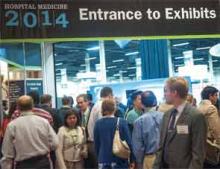
Hospital Medicine Movement Grows in Scope, Impact
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
Frustrated with Existing Systems, Hospitalists Collaborate to Improve Health Information Technology
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
LAS VEGAS—Hospitalist Amy Knight, MD, isn’t a chief medical informatics officer (CMIO). She calls herself a “CMIO lite,” a nod to her title as medical advisor to the department of information services at her home hospital, Johns Hopkins Bayview Medical Center in Baltimore.
But, CMIO or not, she was among the first cohort of 450 medical professionals to be board-certified in medical informatics last fall after an exam for the specialty was created by the American Board of Medical Specialties.
Now Dr. Knight, who serves as a technology advocate for SHM, thinks more hospitalists should follow her lead.
“I had a little chip on my shoulder because I didn’t do a fellowship in informatics,” said Dr. Knight, who nonetheless worked on Bayview’s implementation of computerized provider order entry and electronic provider documentation systems. “I wanted some sort of recognition for everything I’d been doing. We’re already doing it, so let’s get some recognition for it, some credentials—and also, some standards for what the minimum needed to do a good job are.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque and chair of SHM’s Information Technology Committee, agrees. He wants as many hospitalists as possible to “establish ourselves for the informatics role we have taken.”
Whether it was lamenting clunky electronic health records (EHR) systems, discussing Dr. Rogers’ push for so-called “techno-docs” to consider the new board certification, or lobbying for people to interact more with SHM’s Hospital Medicine Exchange (HMX), hospitalists at HM14 took the opportunity to focus on the growing pains of health information technology (IT).
For Mohammed Morad, MD, a hospitalist at Indiana University Health Ball Memorial Hospital in Muncie, the paramount frustration is the trouble providers have with EHR systems that are built for physicians but don’t seem to consider the end user.
“These EHRs are designed to make your billing easier,” Dr. Morad said. “[They’re] not designed for patient safety or quality measures. Now they’re trying to implement some of these tools, but the usability...is very challenging, especially for physicians who are not tech-savvy enough. Even [for] newly graduated doctors with iPhones, it’s still a challenge. It’s not user-friendly.”
Dr. Morad’s biggest frustration with the technology is how time-consuming it is. Although electronic input is clearly more advanced, more communal, and more privacy-focused than hand-written notes, current systems that require physicians to spend hours upon hours building order sets or typing out notes waste too much valuable time, he said.
“You spend more time with these EHRs than you spend with your patients, because you have to put the orders in, you have to write the note, you have to look at previous reports,” Dr. Morad added. “In a way, it helps in gathering the information that you need in one place so before I even see the patient I know what the echo[cardiogram] showed, what the chest X-ray showed, what the previous consultant had seen....but how easy is it to get all this? It takes more time than it should.”
Despite expressing frustration with current systems, most hospitalists are cautiously optimistic about advances in technology. Dr. Morad is hopeful that future iterations of the systems will be “more intuitive” and consider physicians’ needs instead of creating templates that individual institutions have to spend time and money customizing.
“Compared to any other software, they’re behind,” he said. “They’re not going to get better unless some people step up and try to make them better, especially from a physician perspective.”
Gaurav Chaturvedi, MD, head of the hospitalist team at Northwestern Lake Forest (Ill.) Hospital and chair of SHM’s IT Quality Subcommittee, said part of the problem is that vendors have a captive audience. Hospitals are motivated to take advantage of health IT incentive payments, which were funded under the Health Information Technology for Economic and Clinical Health Act provisions of the American Recovery and Reinvestment Act of 2009. Because healthcare reform is pushing the industry to digitize medical records, IT firms have built-in customers. That, Dr. Chaturvedi said, has stifled competition and hampered innovations tailored to doctors’ needs.
Hospitalists must work together to discuss end-user issues and prompt improvement, he added. To that end, SHM technology committees are working on white papers that will recommend best practices related to health information technology. While the papers are still in the planning and polishing phase, the idea is to view the overall landscape to give HM group leaders a framework of what they should be focused on.
“We want to keep vendor-neutral,” Dr. Chaturvedi said. “We all have the same types of issues to work with. We should work it out together.”
Dr. Rogers noted that SHM has met proactively with vendors to provide input on potential improvements, but that the process is ongoing and will likely take years.
“The best is still pretty bad out there,” he added.
Meanwhile, he urged hospitalists to share concerns, complaints, and success stories via HMX, an online portal hospitalists can use to communicate their views on a variety of topics, post responses, and share files. The online community—launched three years ago but rebranded under its current name in 2012—can be a repository for advice, ideas, or commiseration but is useful only if it is adopted. If more hospitalists log into the system and begin to use it, participation will breed greater value and vice versa, he added.
“We’re still in the build-up phase,” Dr. Rogers said. “We want to get people in all discussion forums to a tipping point.”
Hospitalists Share Patient Care Tips, Strategies at HM14 Annual RIV Competition
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
LAS VEGAS—To an untrained eye, the poster looked a lot like the hundreds of others that lined the exhibit hall here at Mandalay Bay Resort and Casino. But this one belonged to hospitalist Cathy Jones, MD, an associate chief medical officer (CMO) for medical services at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
The poster, “The Daily Safety Check-In: A Strategy For Reducing Serious Harm to Patients,” highlighted the hospital’s use of a daily safety check-in (DSCI) that gathers hospitalists, nurses, infection-control staff, and at least one representative from its CMO office to discuss the patient census. The meeting—held without fail each morning at 9:05, 365 days a year, including holidays—takes at least 30 minutes, time that might seem like too much to some observers who couldn’t imagine squeezing another half-hour meeting into their schedule.
But to Dr. Jones, the DSCI is worth every second, and she wanted—practically needed—to share it. “We think this is saving lives in our organization,” she says. “Maybe somebody else will see this and say, ‘We could do that,’ and maybe it would make a difference there, too.”
Therein lies the point of the annual Research, Innovations, and Clinical Vignettes (RIV) poster competition: hospitalists sharing profound thoughts, creative pilot programs, and unique cases with their brethren from around the country.
“Sometimes you’re so close to a problem, you just can’t figure it out,” says Dr. Jones, whose poster came in second place in the Innovations category. “You keep trying the same old things and they don’t work. Then you come here and you say, ‘Oh, they’ve done some training (on) that problem at our hospital.’ And often you have the opportunity to talk to the person and say, “Tell me, what’s your curriculum? Who teaches it?’... This sharing of ideas is what’s so nice about the poster sessions.”
Some ideas, such as Dr. Jones’ DSCI, might seem too big to tackle. Others, like a paper presented by third-year internal medicine resident Lekshmi Santhosh, MD, from the University of California at San Francisco (UCSF), can be as simple as an innovative update on how doctors send and receive electronic pages.
Dr. Santhosh’s poster, “CareWeb Messenger: A Facebook/Twitter/Paging Hybrid for Collaborative Care,” showcases a web-based paging tool that combines features of Facebook and Twitter and allows users to send, receive, view, search, and store messages on a patient’s “wall,” while routing each message to a provider’s pager and wireless phone. The idea is to ease the perceived burden of answering pages while also improving communication skills.
The concept resonates well; a panel of judges awarded it the best poster by a trainee in the Innovations competition. And, while Dr. Santhosh was humbly honored, she says talking to other physicians is the reason she was excited to present.
“Somebody from (the University of Pennsylvania) came up to me—totally opposite coast—and he showed me what they’re using, which is basically an SMS text-based system,” Dr. Santhosh adds. “I was sharing ideas with him. I would never have been able to meet him or even hear about what they’re doing at Penn if not for forums like this.”
The ability to crowd-source ideas at the poster competition appealed to Susan Hunt, MD, a hospitalist at Seattle Children’s Hospital and the University of Washington Medical Center and one of SHM’s judges for the Innovations portion of the poster competition. Dr. Hunt says it’s difficult choosing winners because there are so many good presentations, but, more importantly, hospitalists should use the competition as a chance to see the best of the best and then pick out concepts that might work at their hospital.
“How translatable is it?” Dr. Hunt says, listing off judging criteria. “How applicable is it to the general hospitalist population? Community hospitalists? Academic hospitalists? How will this help them provide better care for their patients, better job satisfaction, better training? Some of the ones that didn’t win are still great ideas.”
Take the project presented by a trio of hospitalists from Rush University Medical Center in Chicago. The poster, “Guidelines, Education, and Email Alerts Can Decrease Transfusions in General Medicine Patients,” explained a project to “increase adherence to a restrictive transfusion guideline for patients admitted to general medicine floors.” The intervention suggested a transfusion threshold of Hgb<7 in upper GI bleed patients, except in cases of hemodynamic instability. In all other indications, the threshold was Hgb<8.
The research found that when samples from three months before the intervention were compared with samples collected three months post-intervention, the number of transfused units dropped to 273 from 481. In the pre-intervention sample, there were 95 units of blood delivered with a pre-transfusion Hgb>8; in the post-intervention group, only 18 units were delivered.
But Rush hospitalist Jisu Kim, MD, FHM, isn’t stopping with a poster. “This is one of the endpoints,” Dr. Kim says. “We want to see how much further we can go. Can this be a publishable paper? What’s the next step for our other projects? We’re getting motivated by it.”
Dr. Kim believes that in addition to sharing information, getting the next generation of physicians involved in the poster competition inspires young physicians to further engage in their specialty. To that end, residents Manya Gupta, MD, and Lesley Schmaltz, MD, say they are grateful to be part of the presentation.
“It’s very rewarding because it makes you want to keep moving forward and keep making those improvements,” says Dr. Schmaltz. “That’s why I think we all do our posters and presentations: to help the greater good of all physicians throughout the country.”
“It’s been a really great learning experience to get your feet wet,” Dr. Gupta says. “You just have to try it out once and find out what it’s like; otherwise it seems so daunting. Then you realize, ‘We can do this.’”
Hospital Medicine Leaders Share Practice Management Pearls at HM14
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”
LAS VEGAS—Susan Eschenburg, practice program manager at Independent Hospitalist Practice in Jackson, Mich., sat in the practice management pre-course at HM14 and listened to a panel of experts discuss hospitalists’ growing role in post-acute care centers such as skilled nursing facilities.
You could almost hear the bell go off in her head.
“We work in an underserved area, and we’ve just [been asked] if we would be interested in supplying a hospitalist in some of these nursing homes,” Eschenburg said. “We’re going to listen to a spiel next month about that. That was real-time and interesting to listen to.”
That was the point of the practice management sessions at SHM’s annual meeting here at the Mandalay Bay Resort and Casino: to give the most current updates available to administrators, group leaders, and rank-and-file hospitalists about best practices in the day-to-day operation of a group.
For Eschenburg, the lessons learned here are particularly helpful; her group just launched its hospitalist program in September and is dealing with a variety of implementation questions, including whether to use scribes to enhance patient-physician interaction, improve documentation, save physician time, and reduce technology-related errors. Other issues that resonate with her include scheduling and the amount of time that administrative leaders should spend in the clinical setting.
The meeting helped “[us] to see if there’s anything out there that we haven’t thought about or talked about,” Eschenburg said. “We’re not this big corporate giant that can’t make quick movements.”
Whether a hospitalist is working at a new practice in an underserved area or as a department head at a massive academic institution, a new white paper from SHM can provide information on how to move toward those best practices. “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” (http://onlinelibrary.wiley.com/doi/10.1002/jhm.2119/full), published in February in the Journal of Hospital Medicine, lists 10 guiding principles and 47 individual characteristics as a launching point for best practices.
Although the white paper is a first-of-its-kind initiative, SHM isn’t stopping there. Society staff and committee members are working to roll out a pilot program later this year that will ask group leaders to validate the key characteristics. SHM will provide back-up documentation, such as sample business plans or other toolkits, to implement some of the recommendations. Group leaders will be asked to use the documentation to determine whether or not it helps them achieve the goals.

–Dr. Wellikson
“One valuable thing that could come out of the pilot is not just feedback from you that will help us refine the key characteristics, but also ideas about resources that SHM can provide to help you better accomplish the things the key characteristics set forth,” said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants, a member of SHM’s Practice Analysis Committee, and a co-director for the popular practice management pre-course, “Where the Rubber Meets the Road: Managing in the Era of Healthcare Reform.”
Put more simply by Flores’ consulting colleague, John Nelson, MD, MHM, FACP: “We’ll learn from each other the best ways to do this.”
SHM senior vice president Joe Miller added that the white paper “simply identifies the characteristics and includes a rationale as to why they’re included.” The pilot program, however, will produce “a more enriched tool that you can use in a more directed fashion,” Miller said, “but we felt it was important to get this out right now and get the sense that we’ve identified the right issues.”
SHM CEO Larry Wellikson, MD, SFHM, said the initiative is “bold” and encouraged HM groups that are below standard in any area to step up their games.
“What we’re saying to you and your colleagues is that some of you aren’t performing necessarily at the best level you can,” Dr. Wellikson said. “We want to give you a pathway to get better, because at the end of the day, we’re all in this to deliver the best care we can to our patients. So we recognize where we aren’t perfect, and we try to improve.”
Those seeking practice management advice said they’re always thinking about ways to improve, and being with 3,600 like-minded folks often helps tease out tidbits and strategies to get better.
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., said he enjoys hearing HM leaders give advice, whether they’re practice administrators in individual sessions or keynote speakers in large ballrooms.
“When you’re [an] individual physician, you don’t know what to expect in the future,” Dr. Kartham said. “When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
Preparing for what the future might bring is what drew Angelo Barile, MD, to the meeting. As the head of the hospitalist group at Cleveland Clinic Lorain Family Health and Surgery Center in Lorain, Ohio, he’s always looking for tips on how to improve the practical side of running a 12-FTE group.
“It helps to see how other people do it, and you get a nice framework of how to do it,” said Dr. Barile. “As busy as we are, running the group [and] seeing patients, it’s nice to get away from the pager [and] get away from my administrators and my bosses and say, ‘I want to try to learn something here.’ It is refreshing.”
Education doesn’t end with the meeting’s finale. Dr. Barile traditionally holds a sit-down with his staff as soon as he returns home. The doctors discuss the new ideas Dr. Barile learned and determine as a group what could work in their practice.
Eschenburg, the nascent program manager in Michigan, said she gets the same reaction when she returns from professional meetings.
“It’s certainly something that people are looking for when you get back,” she said. “What did you learn? What can you share with us?”