User login
Danielle Scheurer, MD, MSCR, SFHM, is a hospitalist and the chief quality officer at the Medical University of South Carolina (MUSC) in Charleston. She is former SHM physician advisor, an SHM blogger, and member of SHM's Education Committee. She also serves as faculty of SHM's annual meeting "ABIM Maintenance of Certification (MOC) Learning Session" pre-course. Dr. Scheurer earned her undergraduate degree at Emory University in Atlanta, graduated medical school from the University of Tennessee in Knoxville, and trained at Duke University in Durham, N.C. She has served as physician editor of The Hospitalist since 2012.
Have you Googled yourself lately?
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.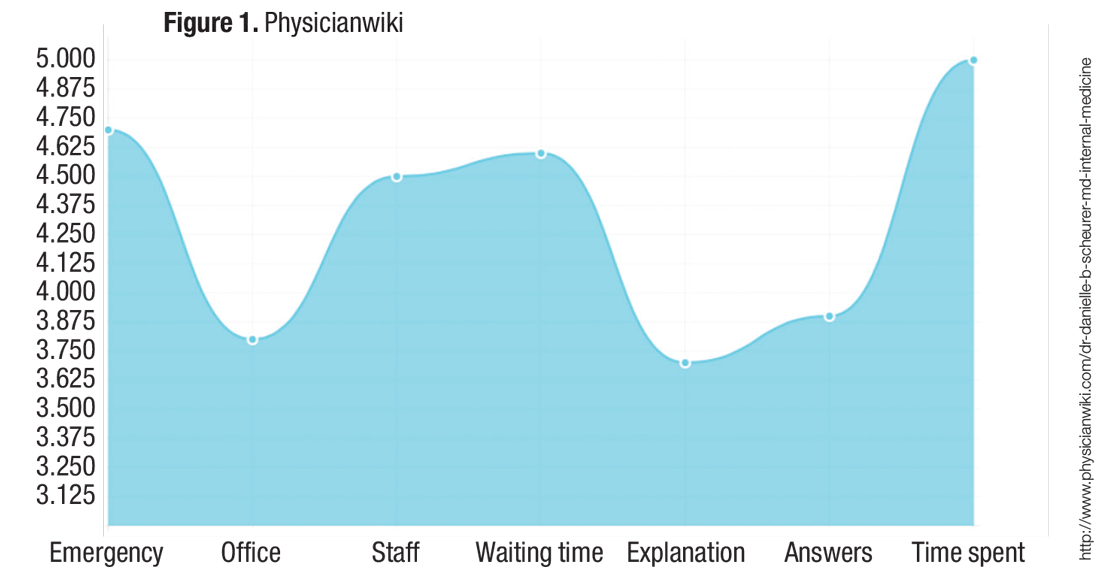
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.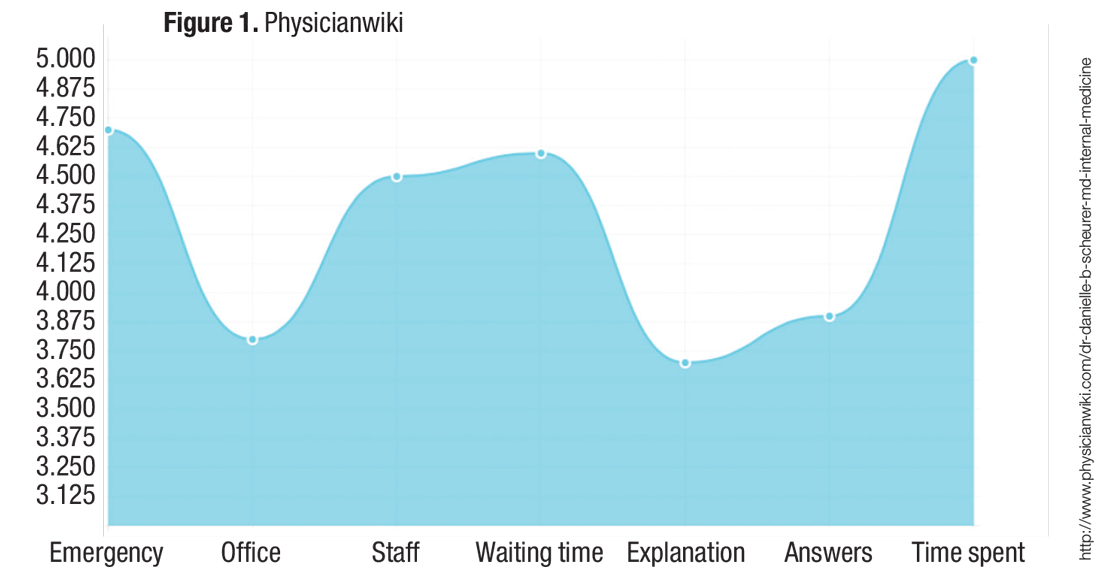
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.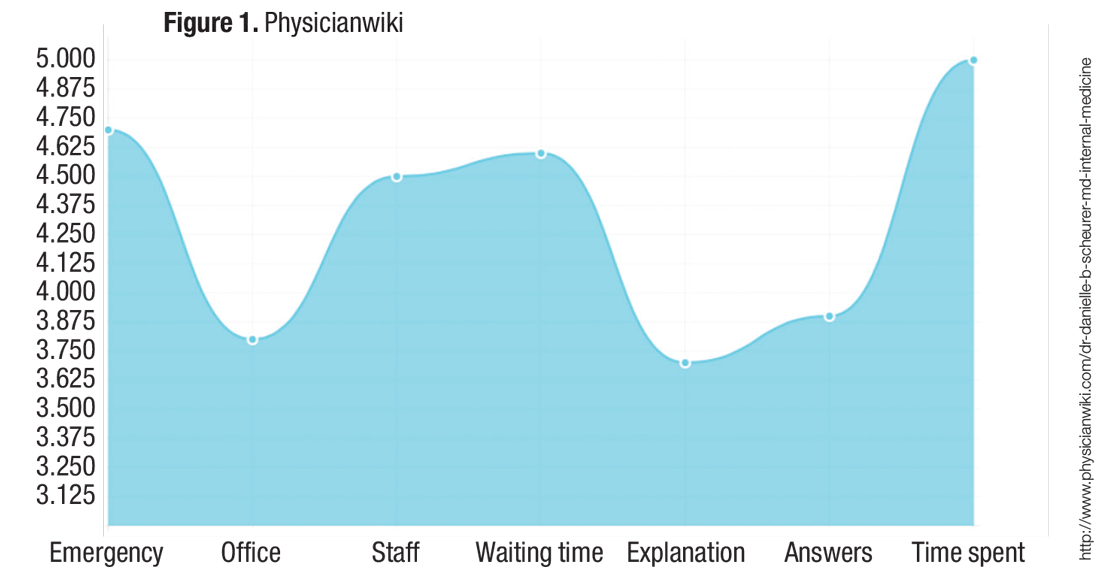
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
What to Know about CMS’s New Emergency Preparedness Requirements
Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

What Hospitalists Can Learn from Basketball Coach Pat Summitt
I’m not exactly a devout follower of women’s college basketball. But having grown up in Knoxville, it was hard not to follow the University of Tennessee Lady Volunteers (“Lady Vols”) and the career of their longtime head coach, Pat Summitt. Summitt recently died from a swift and severe form of early-onset Alzheimer’s disease. In the wake of her death, many have analyzed the impact of her career and the legacy she has left from her lifetime of relentless coaching and developing of athletes. She was an incredible leader who should make us all reflect on the impact we are making in the lives of our patients and their families, our peers, and the next generation of hospitalists.
Early Career
Pat Summitt was born Patricia Sue Head in 1952 in Clarksville, Tenn., the daughter of Richard and Hazel Albright Head and the fourth of five children. When she was in high school, her family moved to another town so she could play basketball (as her local town did not have a girl’s team). Summitt attended the University of Tennessee at the Martin campus and played for its first women’s basketball coach. Although each of Summitt’s three brothers had received an athletic scholarship, at the time there were no athletic scholarships for women, so her parents supported her way through college.1
After college, Summitt started as a graduate assistant at the University of Tennessee. At the start of the 1974 basketball season, the head coach suddenly quit, and she was named the new head coach at the age of 22. (This was before women’s college basketball was even an NCAA-sanctioned sport.) Legend has it she was paid $250 a month and the team had almost no budget. She reportedly washed all the uniforms herself (which were purchased the year before from the proceeds of a doughnut sale) and drove the team van.1
Barely older than most of the players on the team, she coached her first game in December against Mercer University and lost 84–83. From then on, she racked up an incredible number of wins. In her second season, Summitt coached the team to a 16–11 record while working on her master’s degree in physical education.1
By 1978, Summitt recorded her 100th win and coached the Lady Vols in their first Association for Intercollegiate Athletics for Women Final Four. She ended the decade by winning their first-ever Southeastern Conference tournament. A few years later, in 1984, she coached the U.S. women’s team to an Olympic gold medal, becoming the first U.S. Olympian to win a basketball medal and coach a medal-winning team. There were countless other career milestones: She coached the Lady Vols in 16 SEC regular-season championships and 16 SEC tournament titles. She also coached the Lady Vols in 18 NCAA Final Fours.
Legacy
Summitt’s career-win total still stands as the most among NCAA Division I basketball coaches (men or women). Overall, Summitt finished her career with a record of 1,098-208 and a .841 winning percentage.
At the end of her career, there were 78 people mentored directly by her who were coaching basketball or working in administrative positions associated with the sport. Tennessee Athletic Director Dave Hart summarized her legacy:
“Pat Summitt is … truly is a global icon who transcended sports and spent her entire life making a difference in other peoples’ lives. … She was a genuine, humble leader who focused on helping people achieve more than they thought they were capable of accomplishing. … Her legacy will live on through the countless people she touched throughout her career.”2
Every player coached by Summitt finished her undergraduate degree, often with considerable prodding directly from her.
“Across the board with her kids, she also prepared them for life after basketball,” basketball coach Bob Knight said. “Not many people have prepared their players that well for life.”2
You don’t have to be a women’s basketball fan to understand and respect the impact that Summitt had on the lives she touched. She didn’t just win a lot of games—she changed the game. Think about how you will be remembered in your career as a hospitalist. Will you be remembered as someone clocking in and clocking out, just getting by for a paycheck? Or will you be remembered and revered as a “Summitt,” someone who always gave it their all and coached others to their best?
Hospital medicine is still in its relative infancy as a specialty. We all have the potential to pave a positive future for thousands more to come behind us; we all have the potential to be a Summitt. TH
References
1. Gregory S. Q&A: Tennessee Coach Pat Summitt. Time website. Accessed August 7, 2016.
2. Pat Summitt, winningest coach in Division I history, dies at 64. ESPN website. Accessed August 7, 2016.

I’m not exactly a devout follower of women’s college basketball. But having grown up in Knoxville, it was hard not to follow the University of Tennessee Lady Volunteers (“Lady Vols”) and the career of their longtime head coach, Pat Summitt. Summitt recently died from a swift and severe form of early-onset Alzheimer’s disease. In the wake of her death, many have analyzed the impact of her career and the legacy she has left from her lifetime of relentless coaching and developing of athletes. She was an incredible leader who should make us all reflect on the impact we are making in the lives of our patients and their families, our peers, and the next generation of hospitalists.
Early Career
Pat Summitt was born Patricia Sue Head in 1952 in Clarksville, Tenn., the daughter of Richard and Hazel Albright Head and the fourth of five children. When she was in high school, her family moved to another town so she could play basketball (as her local town did not have a girl’s team). Summitt attended the University of Tennessee at the Martin campus and played for its first women’s basketball coach. Although each of Summitt’s three brothers had received an athletic scholarship, at the time there were no athletic scholarships for women, so her parents supported her way through college.1
After college, Summitt started as a graduate assistant at the University of Tennessee. At the start of the 1974 basketball season, the head coach suddenly quit, and she was named the new head coach at the age of 22. (This was before women’s college basketball was even an NCAA-sanctioned sport.) Legend has it she was paid $250 a month and the team had almost no budget. She reportedly washed all the uniforms herself (which were purchased the year before from the proceeds of a doughnut sale) and drove the team van.1
Barely older than most of the players on the team, she coached her first game in December against Mercer University and lost 84–83. From then on, she racked up an incredible number of wins. In her second season, Summitt coached the team to a 16–11 record while working on her master’s degree in physical education.1
By 1978, Summitt recorded her 100th win and coached the Lady Vols in their first Association for Intercollegiate Athletics for Women Final Four. She ended the decade by winning their first-ever Southeastern Conference tournament. A few years later, in 1984, she coached the U.S. women’s team to an Olympic gold medal, becoming the first U.S. Olympian to win a basketball medal and coach a medal-winning team. There were countless other career milestones: She coached the Lady Vols in 16 SEC regular-season championships and 16 SEC tournament titles. She also coached the Lady Vols in 18 NCAA Final Fours.
Legacy
Summitt’s career-win total still stands as the most among NCAA Division I basketball coaches (men or women). Overall, Summitt finished her career with a record of 1,098-208 and a .841 winning percentage.
At the end of her career, there were 78 people mentored directly by her who were coaching basketball or working in administrative positions associated with the sport. Tennessee Athletic Director Dave Hart summarized her legacy:
“Pat Summitt is … truly is a global icon who transcended sports and spent her entire life making a difference in other peoples’ lives. … She was a genuine, humble leader who focused on helping people achieve more than they thought they were capable of accomplishing. … Her legacy will live on through the countless people she touched throughout her career.”2
Every player coached by Summitt finished her undergraduate degree, often with considerable prodding directly from her.
“Across the board with her kids, she also prepared them for life after basketball,” basketball coach Bob Knight said. “Not many people have prepared their players that well for life.”2
You don’t have to be a women’s basketball fan to understand and respect the impact that Summitt had on the lives she touched. She didn’t just win a lot of games—she changed the game. Think about how you will be remembered in your career as a hospitalist. Will you be remembered as someone clocking in and clocking out, just getting by for a paycheck? Or will you be remembered and revered as a “Summitt,” someone who always gave it their all and coached others to their best?
Hospital medicine is still in its relative infancy as a specialty. We all have the potential to pave a positive future for thousands more to come behind us; we all have the potential to be a Summitt. TH
References
1. Gregory S. Q&A: Tennessee Coach Pat Summitt. Time website. Accessed August 7, 2016.
2. Pat Summitt, winningest coach in Division I history, dies at 64. ESPN website. Accessed August 7, 2016.

I’m not exactly a devout follower of women’s college basketball. But having grown up in Knoxville, it was hard not to follow the University of Tennessee Lady Volunteers (“Lady Vols”) and the career of their longtime head coach, Pat Summitt. Summitt recently died from a swift and severe form of early-onset Alzheimer’s disease. In the wake of her death, many have analyzed the impact of her career and the legacy she has left from her lifetime of relentless coaching and developing of athletes. She was an incredible leader who should make us all reflect on the impact we are making in the lives of our patients and their families, our peers, and the next generation of hospitalists.
Early Career
Pat Summitt was born Patricia Sue Head in 1952 in Clarksville, Tenn., the daughter of Richard and Hazel Albright Head and the fourth of five children. When she was in high school, her family moved to another town so she could play basketball (as her local town did not have a girl’s team). Summitt attended the University of Tennessee at the Martin campus and played for its first women’s basketball coach. Although each of Summitt’s three brothers had received an athletic scholarship, at the time there were no athletic scholarships for women, so her parents supported her way through college.1
After college, Summitt started as a graduate assistant at the University of Tennessee. At the start of the 1974 basketball season, the head coach suddenly quit, and she was named the new head coach at the age of 22. (This was before women’s college basketball was even an NCAA-sanctioned sport.) Legend has it she was paid $250 a month and the team had almost no budget. She reportedly washed all the uniforms herself (which were purchased the year before from the proceeds of a doughnut sale) and drove the team van.1
Barely older than most of the players on the team, she coached her first game in December against Mercer University and lost 84–83. From then on, she racked up an incredible number of wins. In her second season, Summitt coached the team to a 16–11 record while working on her master’s degree in physical education.1
By 1978, Summitt recorded her 100th win and coached the Lady Vols in their first Association for Intercollegiate Athletics for Women Final Four. She ended the decade by winning their first-ever Southeastern Conference tournament. A few years later, in 1984, she coached the U.S. women’s team to an Olympic gold medal, becoming the first U.S. Olympian to win a basketball medal and coach a medal-winning team. There were countless other career milestones: She coached the Lady Vols in 16 SEC regular-season championships and 16 SEC tournament titles. She also coached the Lady Vols in 18 NCAA Final Fours.
Legacy
Summitt’s career-win total still stands as the most among NCAA Division I basketball coaches (men or women). Overall, Summitt finished her career with a record of 1,098-208 and a .841 winning percentage.
At the end of her career, there were 78 people mentored directly by her who were coaching basketball or working in administrative positions associated with the sport. Tennessee Athletic Director Dave Hart summarized her legacy:
“Pat Summitt is … truly is a global icon who transcended sports and spent her entire life making a difference in other peoples’ lives. … She was a genuine, humble leader who focused on helping people achieve more than they thought they were capable of accomplishing. … Her legacy will live on through the countless people she touched throughout her career.”2
Every player coached by Summitt finished her undergraduate degree, often with considerable prodding directly from her.
“Across the board with her kids, she also prepared them for life after basketball,” basketball coach Bob Knight said. “Not many people have prepared their players that well for life.”2
You don’t have to be a women’s basketball fan to understand and respect the impact that Summitt had on the lives she touched. She didn’t just win a lot of games—she changed the game. Think about how you will be remembered in your career as a hospitalist. Will you be remembered as someone clocking in and clocking out, just getting by for a paycheck? Or will you be remembered and revered as a “Summitt,” someone who always gave it their all and coached others to their best?
Hospital medicine is still in its relative infancy as a specialty. We all have the potential to pave a positive future for thousands more to come behind us; we all have the potential to be a Summitt. TH
References
1. Gregory S. Q&A: Tennessee Coach Pat Summitt. Time website. Accessed August 7, 2016.
2. Pat Summitt, winningest coach in Division I history, dies at 64. ESPN website. Accessed August 7, 2016.

Should Physicians Care about Costs?
The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

The healthcare industry is under major stress from steady declines in all sources of revenue. The drivers are multifactorial but include declining reimbursement from payors, a shift from fee-for-service to pay-for-performance, and state-by-state variability in patients covered by Medicaid, by high-deductible plans, or by being uninsured. In academic medical centers, rising overhead costs coupled with a reticence to raise student tuition and declining research funding streams have further compounded the situation.
Regardless of the actual numbers, all healthcare institutions are feeling the financial pinch. Most are intensely focused on cost-reduction efforts. The question is, what do physicians think about their role in these efforts, and what efforts will be most effective?
A recent survey of a large physician group practice found that many physicians do not know what their cost drivers are or do not think it is their role to participate in cost-reduction efforts.1 Of note, the group practice in the survey is a Pioneer Medicare accountable care organization (ACO) and participates in a combination of fee-for-service and capitated contracts.
Within the survey, the researchers embedded a cost-consciousness scale, which is a validated survey tool designed to assess daily cost consciousness. They also embedded other survey items to determine the physicians’ concerns for malpractice, comfort with diagnostic uncertainty, and perception of patient-family pressure for utilization of services. The average overall cost-consciousness score was 29 out of 44, with higher scores indicating more cost consciousness.
Almost all physicians agreed that they need to reduce unnecessary testing (97%), need to adhere to guidelines (98%), and have a responsibility to control costs (92%). However, 33% felt it was unfair for them to have to be both cost-conscious and concerned with the welfare of their patients.
Approximately a third of respondents also felt that there was too much emphasis on cost and that physicians are too busy to worry about costs.
More than a third (37%) said they did not have good knowledge about test-procedure cost within their system.
More than half of physicians felt pressure from patients to perform tests and procedures (from 68% of primary-care physicians, 58% of medical specialists, and 56% of surgical specialists) and felt pressure to refer to consultants (from 65% of primary-care physicians, 35% of medical specialists, and 34% of surgical specialists).
Based on this survey and other literature about physicians’ perceptions of their role and their ability to control costs, it is clear that the first step in understanding how to engage physicians in cost-reducing efforts is to understand what the drivers are for utilization and what the concerns are for reducing cost. Many hypothesize that the drivers to support the status quo include a fear of litigation, fear of missing a diagnosis, and patient demands for services. Another major driver of current utilization is that there is ongoing support for the status quo, as the majority of reimbursement for providers is still based on fee-for-service.
Change Efforts
One cost-reducing effort that has gained widespread enthusiasm from medical societies is the Choosing Wisely campaign. This campaign is an effort originally driven by the American Board of Internal Medicine (ABIM) Foundation to help physicians become aware of and reduce unnecessary utilization of resources. Each Choosing Wisely list is generated and endorsed by the relevant medical society and widely advertised to physicians via a variety of mechanisms. More than 70 medical societies have participated in the effort to date.
The recommendations are often widely accepted by those in the specialty since they are evidence-based and derived and advertised by their own specialty societies. In the survey mentioned above, almost all physicians agreed that their Choosing Wisely was a good source of guidance (ranging from 92% of surgical specialties to 97% of primary-care physicians). In order to drive the movement from the patient perspective, Consumer Reports has developed educational materials aimed at the consumer side of healthcare (ie, patients and families).
As Consumer Reports suggests, the first step to implementing cost-conscious care is to measure awareness of cost and causes of overutilization. By first understanding behaviors, a group can then work to impact such behaviors. It is highly likely that the drivers are different based on the specialty of the physician, the patient population being served, and the local healthcare market drivers. As such, there will not be a single, across-the-board solution to reducing unnecessary utilization of services (and therefore cost), but interventions will need to be tailored to different groups depending on the drivers of cost locally.
Depending on the issues within a group, successful interventions could include:
- Decision support tools (for appropriate use of consultants and diagnostic tests)
- Display of testing costs (not just at the time of ordering)
- Efforts aimed at patient education (both as general consumers as well as at the point of care)
- Malpractice reform to support physicians trying to balance cost consciousness with patient welfare
In Sum
We have a long way to go in engaging physicians in efforts to reduce unnecessary utilization and cost. I recommend that hospitalist practices utilize the survey tool used in this study to understand the perceived barriers and drivers of cost within their practice and work with their local administrative teams to better understand patterns of overutilization among their group. Then interventions can be designed to be evidence-based, tailored to local workflow, and both reliable and sustainable.
If done well, hospitalists can have a huge impact on utilization and cost and position their groups and their hospitals well to succeed in this cost-constrained era of healthcare. TH
References
- Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perception of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337-343.

Recognizing Contributions Physician Personalities Make to the Greater Good
My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

U.S. Surgeon General Encourages Hospitalists to Remain Hopeful, Motivated
Hopefully, many of you were able to attend the Society of Hospital Medicine’s annual meeting this year in San Diego. (I know at least 4,000 of you made it!) Each year, the annual meeting is a time of catching up with hospitalists from around the country (many of whom I only see once a year) and catching up on what is going on in the medical industry.
This year was not particularly unique in that many sessions focused on the myriad challenges we should expect to see in the medical industry in the coming years. There was much discussion about future payment models; although there is ongoing ambiguity about exactly how these models are going to be operationalized, there is certainly no ambiguity that the Centers for Medicare & Medicaid Services (CMS) is hard driving the amount of payments that will be tied to some form of alternative payment model (50% by 2018).
We also heard about ongoing challenges in quality and safety, where a stunning number of patients continue to suffer preventable harm on a daily basis within our hospital walls. And we heard much about the ongoing and mounting opiate abuse epidemic. All of these are monumentally difficult challenges that remain unsolved and without a clear path forward to resolution.
Contrast that with the message from the U.S. Surgeon General during the opening plenary of the annual meeting. Vivek Murthy, MD, was named Surgeon General at a time in the U.S. when all of the above challenges are being added to the abounding issues of chronic disease, mental illness, and extraordinary healthcare costs. He is the highest leader in the nation ordained with trying to improve the health of all Americans at a time when we have never been unhealthier. But despite these monumental challenges, his message was not about the average American body mass index (BMI), smoking status, or heroin addiction. Much different, his message was chock full of amazing stories of community engagement and resilience, focused on innovation and fresh thinking, and about creative problem-solving despite lean and unforgiving budgets.
What Dr. Murthy offered were endless stories of hope and goodness, which he was able to find in each and every city he has visited in his short time as the nation’s “top doc.”
During his tenure, he has visited innumerable communities and engaged with locals in listening sessions. His takeaway from these sessions is “you wouldn’t believe how much good is out there.” One of his many stories was of a hospital and a YMCA that joined forces to improve the health and well-being of the hospital patients, employees, and entire community. This was at a time when both were struggling with lean budgets and stagnant progress in healthy living.
This pragmatic optimism reminds me a bit of one of my life mentors, my Aunt Karen. She is extremely realistic and grounded and knows in great detail the trials and tribulations of being alive for 66 years (including being a 10-year survivor of recurrent ovarian rhabdomyosarcoma). What Aunt Karen does that is so uniquely different than anyone else I know is that she creates goodness. I did not fully understand this until a few years ago, but I noticed that she goes out of her way to create extreme goodness out of extreme ordinariness. I have often joked that she purposely befriends pregnant women just to have an excuse to host a baby shower. She goes overboard to make any and every excuse to celebrate relatively ordinary life milestones (anniversaries, Valentine’s Day, St. Patrick’s Day). In her words, “you have to have a buffer for the funerals.”
Flip Your Switch
And so while Dr. Murthy and Aunt Karen have little else in common, they do share the priceless ability to help others see the goodness in everything around them even when surrounded by remarkable challenges and uncertainty. What a unique gift they have.
But are there simple ways we can all incorporate such goodness into our lives and start to routinely build in these buffers?
In your own personal life and work life, what are your buffers? How could you routinely and repeatedly “find the good” in all things around you?
A few months ago, I started searching for what I call “inbox buffers” as I noticed my email inbox was routinely chock full of requests for time, advice, or resources (all of which can be limited). I found a daily email called “The Daily Good.” It comes into my inbox early each morning and typically covers a human-interest story that is short, interesting, and inspiring. I have found these help me reset my mindset and attitude toward one that is more resilient and forgiving; in other words, it helps me find the good even within the crevices of a cranky email inbox. I have many other buffers, but I cite this one as it is simple, easy, free, predictable, dependable, and routinely inspiring!
So in this time when hospitalists are facing monumental change, unpredictable conflict, and unending challenges, we all need to purposely and repeatedly build in buffers to keep us hopeful and motivated and to seamlessly and routinely find the good in all we do. TH

Hopefully, many of you were able to attend the Society of Hospital Medicine’s annual meeting this year in San Diego. (I know at least 4,000 of you made it!) Each year, the annual meeting is a time of catching up with hospitalists from around the country (many of whom I only see once a year) and catching up on what is going on in the medical industry.
This year was not particularly unique in that many sessions focused on the myriad challenges we should expect to see in the medical industry in the coming years. There was much discussion about future payment models; although there is ongoing ambiguity about exactly how these models are going to be operationalized, there is certainly no ambiguity that the Centers for Medicare & Medicaid Services (CMS) is hard driving the amount of payments that will be tied to some form of alternative payment model (50% by 2018).
We also heard about ongoing challenges in quality and safety, where a stunning number of patients continue to suffer preventable harm on a daily basis within our hospital walls. And we heard much about the ongoing and mounting opiate abuse epidemic. All of these are monumentally difficult challenges that remain unsolved and without a clear path forward to resolution.
Contrast that with the message from the U.S. Surgeon General during the opening plenary of the annual meeting. Vivek Murthy, MD, was named Surgeon General at a time in the U.S. when all of the above challenges are being added to the abounding issues of chronic disease, mental illness, and extraordinary healthcare costs. He is the highest leader in the nation ordained with trying to improve the health of all Americans at a time when we have never been unhealthier. But despite these monumental challenges, his message was not about the average American body mass index (BMI), smoking status, or heroin addiction. Much different, his message was chock full of amazing stories of community engagement and resilience, focused on innovation and fresh thinking, and about creative problem-solving despite lean and unforgiving budgets.
What Dr. Murthy offered were endless stories of hope and goodness, which he was able to find in each and every city he has visited in his short time as the nation’s “top doc.”
During his tenure, he has visited innumerable communities and engaged with locals in listening sessions. His takeaway from these sessions is “you wouldn’t believe how much good is out there.” One of his many stories was of a hospital and a YMCA that joined forces to improve the health and well-being of the hospital patients, employees, and entire community. This was at a time when both were struggling with lean budgets and stagnant progress in healthy living.
This pragmatic optimism reminds me a bit of one of my life mentors, my Aunt Karen. She is extremely realistic and grounded and knows in great detail the trials and tribulations of being alive for 66 years (including being a 10-year survivor of recurrent ovarian rhabdomyosarcoma). What Aunt Karen does that is so uniquely different than anyone else I know is that she creates goodness. I did not fully understand this until a few years ago, but I noticed that she goes out of her way to create extreme goodness out of extreme ordinariness. I have often joked that she purposely befriends pregnant women just to have an excuse to host a baby shower. She goes overboard to make any and every excuse to celebrate relatively ordinary life milestones (anniversaries, Valentine’s Day, St. Patrick’s Day). In her words, “you have to have a buffer for the funerals.”
Flip Your Switch
And so while Dr. Murthy and Aunt Karen have little else in common, they do share the priceless ability to help others see the goodness in everything around them even when surrounded by remarkable challenges and uncertainty. What a unique gift they have.
But are there simple ways we can all incorporate such goodness into our lives and start to routinely build in these buffers?
In your own personal life and work life, what are your buffers? How could you routinely and repeatedly “find the good” in all things around you?
A few months ago, I started searching for what I call “inbox buffers” as I noticed my email inbox was routinely chock full of requests for time, advice, or resources (all of which can be limited). I found a daily email called “The Daily Good.” It comes into my inbox early each morning and typically covers a human-interest story that is short, interesting, and inspiring. I have found these help me reset my mindset and attitude toward one that is more resilient and forgiving; in other words, it helps me find the good even within the crevices of a cranky email inbox. I have many other buffers, but I cite this one as it is simple, easy, free, predictable, dependable, and routinely inspiring!
So in this time when hospitalists are facing monumental change, unpredictable conflict, and unending challenges, we all need to purposely and repeatedly build in buffers to keep us hopeful and motivated and to seamlessly and routinely find the good in all we do. TH

Hopefully, many of you were able to attend the Society of Hospital Medicine’s annual meeting this year in San Diego. (I know at least 4,000 of you made it!) Each year, the annual meeting is a time of catching up with hospitalists from around the country (many of whom I only see once a year) and catching up on what is going on in the medical industry.
This year was not particularly unique in that many sessions focused on the myriad challenges we should expect to see in the medical industry in the coming years. There was much discussion about future payment models; although there is ongoing ambiguity about exactly how these models are going to be operationalized, there is certainly no ambiguity that the Centers for Medicare & Medicaid Services (CMS) is hard driving the amount of payments that will be tied to some form of alternative payment model (50% by 2018).
We also heard about ongoing challenges in quality and safety, where a stunning number of patients continue to suffer preventable harm on a daily basis within our hospital walls. And we heard much about the ongoing and mounting opiate abuse epidemic. All of these are monumentally difficult challenges that remain unsolved and without a clear path forward to resolution.
Contrast that with the message from the U.S. Surgeon General during the opening plenary of the annual meeting. Vivek Murthy, MD, was named Surgeon General at a time in the U.S. when all of the above challenges are being added to the abounding issues of chronic disease, mental illness, and extraordinary healthcare costs. He is the highest leader in the nation ordained with trying to improve the health of all Americans at a time when we have never been unhealthier. But despite these monumental challenges, his message was not about the average American body mass index (BMI), smoking status, or heroin addiction. Much different, his message was chock full of amazing stories of community engagement and resilience, focused on innovation and fresh thinking, and about creative problem-solving despite lean and unforgiving budgets.
What Dr. Murthy offered were endless stories of hope and goodness, which he was able to find in each and every city he has visited in his short time as the nation’s “top doc.”
During his tenure, he has visited innumerable communities and engaged with locals in listening sessions. His takeaway from these sessions is “you wouldn’t believe how much good is out there.” One of his many stories was of a hospital and a YMCA that joined forces to improve the health and well-being of the hospital patients, employees, and entire community. This was at a time when both were struggling with lean budgets and stagnant progress in healthy living.
This pragmatic optimism reminds me a bit of one of my life mentors, my Aunt Karen. She is extremely realistic and grounded and knows in great detail the trials and tribulations of being alive for 66 years (including being a 10-year survivor of recurrent ovarian rhabdomyosarcoma). What Aunt Karen does that is so uniquely different than anyone else I know is that she creates goodness. I did not fully understand this until a few years ago, but I noticed that she goes out of her way to create extreme goodness out of extreme ordinariness. I have often joked that she purposely befriends pregnant women just to have an excuse to host a baby shower. She goes overboard to make any and every excuse to celebrate relatively ordinary life milestones (anniversaries, Valentine’s Day, St. Patrick’s Day). In her words, “you have to have a buffer for the funerals.”
Flip Your Switch
And so while Dr. Murthy and Aunt Karen have little else in common, they do share the priceless ability to help others see the goodness in everything around them even when surrounded by remarkable challenges and uncertainty. What a unique gift they have.
But are there simple ways we can all incorporate such goodness into our lives and start to routinely build in these buffers?
In your own personal life and work life, what are your buffers? How could you routinely and repeatedly “find the good” in all things around you?
A few months ago, I started searching for what I call “inbox buffers” as I noticed my email inbox was routinely chock full of requests for time, advice, or resources (all of which can be limited). I found a daily email called “The Daily Good.” It comes into my inbox early each morning and typically covers a human-interest story that is short, interesting, and inspiring. I have found these help me reset my mindset and attitude toward one that is more resilient and forgiving; in other words, it helps me find the good even within the crevices of a cranky email inbox. I have many other buffers, but I cite this one as it is simple, easy, free, predictable, dependable, and routinely inspiring!
So in this time when hospitalists are facing monumental change, unpredictable conflict, and unending challenges, we all need to purposely and repeatedly build in buffers to keep us hopeful and motivated and to seamlessly and routinely find the good in all we do. TH

QUIZ: Which Strategy Should Hospitalists Employ to Reduce the Risk of Opioid Misuse?
[WpProQuiz 6]
[WpProQuiz_toplist 6]
[WpProQuiz 6]
[WpProQuiz_toplist 6]
[WpProQuiz 6]
[WpProQuiz_toplist 6]
Care Teams Work Best When Members Have a Voice
I stumbled upon an absolutely brilliant TED talk about how we need to forget about the “pecking order” within workplaces and how we need to focus on team social connectedness as a strategy to enhance teamwork and productivity.1 I found the analogy in the presenter’s talk so incredibly poignant for the work we do every day in hospital medicine. As we work to solve incredibly challenging problems daily, we do so among continuously changing and highly charged teams. How can we create our teams to be the most effective and productive to serve the greater good?
The speaker, Margaret Heffernan, is an entrepreneur and former CEO of five companies. She tells a story about a study performed by an evolutionary biologist by the name of William Muir of Purdue University in West Lafayette, Ind.2 Muir undertook a series of studies evaluating the social order and productivity of chickens (as measured by egg production) and the team characteristics that make chickens more or less productive. After watching flocks of chickens for several generations, he picked out the most productive chickens and put them all together in a “super flock.” He then watched their productivity over the next several generations and compared their productivity to those in the regular flock.
What he found was that the regular flock became more productive and most of the members of the super flock were dead!
The most productive members of the super flock had essentially pecked the other members to death. He surmised that the only reason the super chickens were initially productive was by suppressing the productivity of the original flock members. The chickens in the regular flock that were initially less aggressive (and less productive) over time sustained fewer injuries and were able to be more productive in the absence of super chickens. The energy that the animals had previously invested in negative behaviors (pecking, injuries, and healing) was redirected into positive behaviors (making eggs).
Muir and his team have gone on to research a tool to predict social aggressiveness and social agreeableness in individual animals. Those high on the socially agreeable scales (and low on the socially aggressive scales) are more valuable for producing highly effective teams of agricultural animals by enhancing group dynamics, social interactions, and actual productivity.
Backward Thinking
Heffernan argues that we have run most businesses (hospitals included) and many societies (at least capitalistic ones) in the super chicken model. In this model, we view leadership as a trait to be individually owned and perfected, and we think that leaders are supposed to have all the answers. In order to determine our leaders, we charge highly competent people to compete against one another as if in a talent contest. It has long been thought that to be successful as teams, we should recruit the best and brightest, pit them against on another, and see who wins, then promote the winner, put them in charge of everything, and give them all the resources they could want or need to be a super chicken.
But this model inevitably suppresses the remainder of the flock and leads to aggression and waste.
In many scenarios in our hospitals, physicians view themselves as and act like super chickens; we try to be the hardest working, the brightest, and the most powerful. How many times have we heard of or witnessed circumstances where a physician suppresses the candor or opinion from other disciplines on the care team? I think we all know physicians (ourselves included) who demand the role of decision maker and ignore the opinions or needs of the remainder of the team, including patients or their family.
Alternatives
So if we should not be subscribing to the super chicken theory, then what type of leadership structures should we be subscribing to within medical teams to produce the best outcomes for ourselves and for our patients and their families?
A study performed by MIT scientists gives us some insight. Researchers found that when random groups of people are given very difficult problems to solve (e.g., think about diagnostic dilemmas or very difficult patients), certain group attributes made it more likely that the group would be successful in solving these difficult problems. The groups that were most effective were not those with a few people with extremely high IQs or with the highest collective IQ. The teams that were most effective and able to solve difficult problems were those that showed high degrees of social sensitivity among members (i.e., empathy). The highest-performing teams gave roughly equal time to each member (e.g., think about physicians, pharmacists, social workers, case managers, consultants on a typical medical team). They also found the highest-performing teams had more women in them. (I feel so redeemed!)
In summary, what they learned from these experiments was that the most successful teams were more socially connected and more highly attuned and sensitive to one another. This is not to say that highly successful teams were leaderless. There is absolutely a vital role that leaders play in such teams. In Jim Collins’ famous book Good to Great, in studying leadership and teams, he did not find the best leaders were super chickens who autocratically made unilateral decisions. Instead, he found the best leaders function more like facilitators, having the humility and skill to draw out shared solutions from large participatory teams.3 Doesn’t this sound like how a hospitalist should run multidisciplinary rounds?
The other major attribute that the MIT researchers noticed about highly functional teams is that each and every member of the team was extremely willing and able to give and receive help. They found that teams with high mutual understanding and trust were more likely to seamlessly—and almost effortlessly—give and receive help from one another. They ended up acting as one another’s social support network. If any team member was confronted by a difficult problem or situation, each felt confident that it could be easily solved with the collective skill and wisdom of the team.
As a result of such research, some companies have developed and implemented strategies to enhance such social capital, such as synchronizing coffee breaks and disallowing coffee mugs at individual desks. These companies consider it a vital strategic mission to ensure that team members get to know and understand one another and that they serve as a social support network at work. They believe that it is reliance and interdependency that ensures trust and enhances productivity.
So what really matters is the mortar, not just the bricks.
HM Takeaway
For hospital medicine teams, what we need to do is accept that teams work best when every member has a voice and is valued. When others look to us (usually seen as team leaders) to make all the decisions (as if we are super chickens), we need to empower our team members to make decisions with us.
We need to actively work toward this model of being a team leader, break any cycles of dependency that we have set up, and produce better outcomes.
We need to avoid acting like super chickens and appreciate and empower a true team effort.
We need to stop accepting that management and promotions occur by talent contests that pit employees against one another and insist that rivalry at every level has to be replaced by social capital and social connectedness.
Only then will our leadership result in creating effective and productive bricks and mortar. TH
References
- Heffernan M. Margaret Heffernan: why it’s time to forget the pecking order at work. TED Talks. June 16, 2015. Available at: https://www.youtube.com/watch?v=Vyn_xLrtZaY&feature=youtu.be.
- Steeves SA. Scientists find method to pick non-competitive animals, improve production. Available at: https://news.uns.purdue.edu/x/2007a/070212MuirSelection.html.
- Collins J. Good to Great. New York, N.Y.: HarperBusiness; 2011.

I stumbled upon an absolutely brilliant TED talk about how we need to forget about the “pecking order” within workplaces and how we need to focus on team social connectedness as a strategy to enhance teamwork and productivity.1 I found the analogy in the presenter’s talk so incredibly poignant for the work we do every day in hospital medicine. As we work to solve incredibly challenging problems daily, we do so among continuously changing and highly charged teams. How can we create our teams to be the most effective and productive to serve the greater good?
The speaker, Margaret Heffernan, is an entrepreneur and former CEO of five companies. She tells a story about a study performed by an evolutionary biologist by the name of William Muir of Purdue University in West Lafayette, Ind.2 Muir undertook a series of studies evaluating the social order and productivity of chickens (as measured by egg production) and the team characteristics that make chickens more or less productive. After watching flocks of chickens for several generations, he picked out the most productive chickens and put them all together in a “super flock.” He then watched their productivity over the next several generations and compared their productivity to those in the regular flock.
What he found was that the regular flock became more productive and most of the members of the super flock were dead!
The most productive members of the super flock had essentially pecked the other members to death. He surmised that the only reason the super chickens were initially productive was by suppressing the productivity of the original flock members. The chickens in the regular flock that were initially less aggressive (and less productive) over time sustained fewer injuries and were able to be more productive in the absence of super chickens. The energy that the animals had previously invested in negative behaviors (pecking, injuries, and healing) was redirected into positive behaviors (making eggs).
Muir and his team have gone on to research a tool to predict social aggressiveness and social agreeableness in individual animals. Those high on the socially agreeable scales (and low on the socially aggressive scales) are more valuable for producing highly effective teams of agricultural animals by enhancing group dynamics, social interactions, and actual productivity.
Backward Thinking
Heffernan argues that we have run most businesses (hospitals included) and many societies (at least capitalistic ones) in the super chicken model. In this model, we view leadership as a trait to be individually owned and perfected, and we think that leaders are supposed to have all the answers. In order to determine our leaders, we charge highly competent people to compete against one another as if in a talent contest. It has long been thought that to be successful as teams, we should recruit the best and brightest, pit them against on another, and see who wins, then promote the winner, put them in charge of everything, and give them all the resources they could want or need to be a super chicken.
But this model inevitably suppresses the remainder of the flock and leads to aggression and waste.
In many scenarios in our hospitals, physicians view themselves as and act like super chickens; we try to be the hardest working, the brightest, and the most powerful. How many times have we heard of or witnessed circumstances where a physician suppresses the candor or opinion from other disciplines on the care team? I think we all know physicians (ourselves included) who demand the role of decision maker and ignore the opinions or needs of the remainder of the team, including patients or their family.
Alternatives
So if we should not be subscribing to the super chicken theory, then what type of leadership structures should we be subscribing to within medical teams to produce the best outcomes for ourselves and for our patients and their families?
A study performed by MIT scientists gives us some insight. Researchers found that when random groups of people are given very difficult problems to solve (e.g., think about diagnostic dilemmas or very difficult patients), certain group attributes made it more likely that the group would be successful in solving these difficult problems. The groups that were most effective were not those with a few people with extremely high IQs or with the highest collective IQ. The teams that were most effective and able to solve difficult problems were those that showed high degrees of social sensitivity among members (i.e., empathy). The highest-performing teams gave roughly equal time to each member (e.g., think about physicians, pharmacists, social workers, case managers, consultants on a typical medical team). They also found the highest-performing teams had more women in them. (I feel so redeemed!)
In summary, what they learned from these experiments was that the most successful teams were more socially connected and more highly attuned and sensitive to one another. This is not to say that highly successful teams were leaderless. There is absolutely a vital role that leaders play in such teams. In Jim Collins’ famous book Good to Great, in studying leadership and teams, he did not find the best leaders were super chickens who autocratically made unilateral decisions. Instead, he found the best leaders function more like facilitators, having the humility and skill to draw out shared solutions from large participatory teams.3 Doesn’t this sound like how a hospitalist should run multidisciplinary rounds?
The other major attribute that the MIT researchers noticed about highly functional teams is that each and every member of the team was extremely willing and able to give and receive help. They found that teams with high mutual understanding and trust were more likely to seamlessly—and almost effortlessly—give and receive help from one another. They ended up acting as one another’s social support network. If any team member was confronted by a difficult problem or situation, each felt confident that it could be easily solved with the collective skill and wisdom of the team.
As a result of such research, some companies have developed and implemented strategies to enhance such social capital, such as synchronizing coffee breaks and disallowing coffee mugs at individual desks. These companies consider it a vital strategic mission to ensure that team members get to know and understand one another and that they serve as a social support network at work. They believe that it is reliance and interdependency that ensures trust and enhances productivity.
So what really matters is the mortar, not just the bricks.
HM Takeaway
For hospital medicine teams, what we need to do is accept that teams work best when every member has a voice and is valued. When others look to us (usually seen as team leaders) to make all the decisions (as if we are super chickens), we need to empower our team members to make decisions with us.
We need to actively work toward this model of being a team leader, break any cycles of dependency that we have set up, and produce better outcomes.
We need to avoid acting like super chickens and appreciate and empower a true team effort.
We need to stop accepting that management and promotions occur by talent contests that pit employees against one another and insist that rivalry at every level has to be replaced by social capital and social connectedness.
Only then will our leadership result in creating effective and productive bricks and mortar. TH
References
- Heffernan M. Margaret Heffernan: why it’s time to forget the pecking order at work. TED Talks. June 16, 2015. Available at: https://www.youtube.com/watch?v=Vyn_xLrtZaY&feature=youtu.be.
- Steeves SA. Scientists find method to pick non-competitive animals, improve production. Available at: https://news.uns.purdue.edu/x/2007a/070212MuirSelection.html.
- Collins J. Good to Great. New York, N.Y.: HarperBusiness; 2011.

I stumbled upon an absolutely brilliant TED talk about how we need to forget about the “pecking order” within workplaces and how we need to focus on team social connectedness as a strategy to enhance teamwork and productivity.1 I found the analogy in the presenter’s talk so incredibly poignant for the work we do every day in hospital medicine. As we work to solve incredibly challenging problems daily, we do so among continuously changing and highly charged teams. How can we create our teams to be the most effective and productive to serve the greater good?
The speaker, Margaret Heffernan, is an entrepreneur and former CEO of five companies. She tells a story about a study performed by an evolutionary biologist by the name of William Muir of Purdue University in West Lafayette, Ind.2 Muir undertook a series of studies evaluating the social order and productivity of chickens (as measured by egg production) and the team characteristics that make chickens more or less productive. After watching flocks of chickens for several generations, he picked out the most productive chickens and put them all together in a “super flock.” He then watched their productivity over the next several generations and compared their productivity to those in the regular flock.
What he found was that the regular flock became more productive and most of the members of the super flock were dead!
The most productive members of the super flock had essentially pecked the other members to death. He surmised that the only reason the super chickens were initially productive was by suppressing the productivity of the original flock members. The chickens in the regular flock that were initially less aggressive (and less productive) over time sustained fewer injuries and were able to be more productive in the absence of super chickens. The energy that the animals had previously invested in negative behaviors (pecking, injuries, and healing) was redirected into positive behaviors (making eggs).
Muir and his team have gone on to research a tool to predict social aggressiveness and social agreeableness in individual animals. Those high on the socially agreeable scales (and low on the socially aggressive scales) are more valuable for producing highly effective teams of agricultural animals by enhancing group dynamics, social interactions, and actual productivity.
Backward Thinking
Heffernan argues that we have run most businesses (hospitals included) and many societies (at least capitalistic ones) in the super chicken model. In this model, we view leadership as a trait to be individually owned and perfected, and we think that leaders are supposed to have all the answers. In order to determine our leaders, we charge highly competent people to compete against one another as if in a talent contest. It has long been thought that to be successful as teams, we should recruit the best and brightest, pit them against on another, and see who wins, then promote the winner, put them in charge of everything, and give them all the resources they could want or need to be a super chicken.
But this model inevitably suppresses the remainder of the flock and leads to aggression and waste.
In many scenarios in our hospitals, physicians view themselves as and act like super chickens; we try to be the hardest working, the brightest, and the most powerful. How many times have we heard of or witnessed circumstances where a physician suppresses the candor or opinion from other disciplines on the care team? I think we all know physicians (ourselves included) who demand the role of decision maker and ignore the opinions or needs of the remainder of the team, including patients or their family.
Alternatives
So if we should not be subscribing to the super chicken theory, then what type of leadership structures should we be subscribing to within medical teams to produce the best outcomes for ourselves and for our patients and their families?
A study performed by MIT scientists gives us some insight. Researchers found that when random groups of people are given very difficult problems to solve (e.g., think about diagnostic dilemmas or very difficult patients), certain group attributes made it more likely that the group would be successful in solving these difficult problems. The groups that were most effective were not those with a few people with extremely high IQs or with the highest collective IQ. The teams that were most effective and able to solve difficult problems were those that showed high degrees of social sensitivity among members (i.e., empathy). The highest-performing teams gave roughly equal time to each member (e.g., think about physicians, pharmacists, social workers, case managers, consultants on a typical medical team). They also found the highest-performing teams had more women in them. (I feel so redeemed!)
In summary, what they learned from these experiments was that the most successful teams were more socially connected and more highly attuned and sensitive to one another. This is not to say that highly successful teams were leaderless. There is absolutely a vital role that leaders play in such teams. In Jim Collins’ famous book Good to Great, in studying leadership and teams, he did not find the best leaders were super chickens who autocratically made unilateral decisions. Instead, he found the best leaders function more like facilitators, having the humility and skill to draw out shared solutions from large participatory teams.3 Doesn’t this sound like how a hospitalist should run multidisciplinary rounds?
The other major attribute that the MIT researchers noticed about highly functional teams is that each and every member of the team was extremely willing and able to give and receive help. They found that teams with high mutual understanding and trust were more likely to seamlessly—and almost effortlessly—give and receive help from one another. They ended up acting as one another’s social support network. If any team member was confronted by a difficult problem or situation, each felt confident that it could be easily solved with the collective skill and wisdom of the team.
As a result of such research, some companies have developed and implemented strategies to enhance such social capital, such as synchronizing coffee breaks and disallowing coffee mugs at individual desks. These companies consider it a vital strategic mission to ensure that team members get to know and understand one another and that they serve as a social support network at work. They believe that it is reliance and interdependency that ensures trust and enhances productivity.
So what really matters is the mortar, not just the bricks.
HM Takeaway
For hospital medicine teams, what we need to do is accept that teams work best when every member has a voice and is valued. When others look to us (usually seen as team leaders) to make all the decisions (as if we are super chickens), we need to empower our team members to make decisions with us.
We need to actively work toward this model of being a team leader, break any cycles of dependency that we have set up, and produce better outcomes.
We need to avoid acting like super chickens and appreciate and empower a true team effort.
We need to stop accepting that management and promotions occur by talent contests that pit employees against one another and insist that rivalry at every level has to be replaced by social capital and social connectedness.
Only then will our leadership result in creating effective and productive bricks and mortar. TH
References
- Heffernan M. Margaret Heffernan: why it’s time to forget the pecking order at work. TED Talks. June 16, 2015. Available at: https://www.youtube.com/watch?v=Vyn_xLrtZaY&feature=youtu.be.
- Steeves SA. Scientists find method to pick non-competitive animals, improve production. Available at: https://news.uns.purdue.edu/x/2007a/070212MuirSelection.html.
- Collins J. Good to Great. New York, N.Y.: HarperBusiness; 2011.

Does Life, Liberty, and the Pursuit of Happiness Apply to Hospital Medicine?
Every American knows this well-known phrase from the Declaration of Independence, which describes the three “unalienable rights” ordained on humans by their Creator and which governments are bound to dutifully protect. But I wonder if the last unalienable right has implications for career happiness in the healthcare industry, particularly for hospitalists. With the phrase now being 240 years old, it has understandably permeated every inch of American society and affected every crevice of the American psyche. Despite having this decreed inalienable right of the pursuit of happiness, there is evidence of widespread dissatisfaction and unhappiness within our profession.
Speaking of happiness, I was listening to a 60 Minutes podcast entitled “Heroin in the Heartland.” It described a widespread affliction of heroin among mainstream middle- and upper-class suburban youths.1 During the piece, they interviewed several addicted youngsters and their parents. I was struck by the story of a young woman named Hannah; she described how and why she became addicted to heroin in her upper-middle-class high school in Columbus, Ohio. She described how heroin made her feel. On a scale of 1–10 in happiness, she said it made her feel like a “26.” She and many of her friends became addicted to the feeling of happiness that was infused into them, a feeling that could not be replicated without the use of the drug. She and her friends started their road to addiction in a quest for their unalienable right of the pursuit of happiness.
Contrast that story with the “unhappiness factor” that plagues U.S. physicians. A 2014 survey found that 54% of physicians reported at least one symptom of burnout.2 That figure was up from 46% in a 2011 survey. From 2011 to 2014, satisfaction with work-life balance dropped to 41% from 49%. Within that same time frame, burnout and dissatisfaction showed very little change in other U.S. working adults, widening the gap in dissatisfaction between physicians and non-physicians. Even after adjusting for age, sex, relationship status, and hours worked, physicians still were almost twice as likely to experience burnout than other working U.S. adults, and they only had an odds ratio of satisfaction of 0.68 (95% CI, 0.62–0.75) compared with non-physicians. In another recent (and sobering) meta-analysis, researchers found that about a third of all resident physicians report depression or depressive symptoms during their training (ranging from 21% to 43%, depending on the instrument used).3
Could it be that physicians in the U.S., in their quest for the pursuit of happiness, are looking for happiness in all the wrong ways? I read an article recently on DailyGood entitled “Does Trying to Be Happy Make Us Unhappy?”4 It describes several studies that purport that the more value people place on trying to become happy, the less happy they actually become. It turns out that in order for us to figure out if we are happy, we are forced to evaluate our current level of happiness and set that against some benchmark (usually from our own past) to analyze where we are. The mere act of doing this moves us from an experiential mode to an evaluation mode, which puts us out of touch with those things in life that can bring us joy and contentment.
Social scientists have found that when we are immersed in the present, we don’t report being happy in that moment, but we do report happiness later when reflecting on those moments. Ruminating about whether we are unhappy, depressed, burned out, or unsatisfied makes us inwardly focused and makes us lose the ability to become immersed in the present.
Scientists also have found that we tend to overestimate how external influences, such as getting a promotion or moving into a new job, will inflate our happiness and that we all adapt to new experiences and quickly return to our baseline happiness (as if the change never occurred). They’ve also found that when we pursue happiness as an individual state, we become inwardly focused and less likely to actually achieve happiness. People who are more outwardly focused on how others feel (and not how they themselves feel) are much more likely to achieve a state of sustained happiness.
Finally, researchers have found that happiness is more likely achieved by pursuing frequent positive emotions rather than intense positive emotions. Many of us search for single intense emotional experiences (the winning of a gold medal) in the pursuit of happiness, but researchers found that the frequency of positive emotions are much more important than the intensity of positive emotions.
So maybe, as physicians in pursuit of happiness, we are going about this pursuit all wrong, with resultant depression, dissatisfaction, and burnout. We can’t change the Declaration of Independence or the American psyche, but we can change how we perceive that pursuit.
Happiness is not a goal to be achieved but a state of mind to be savored. Immersing ourselves in our daily life, we should be outwardly focused on our colleagues and our patients. If we take this approach, there is no other profession better suited to actually achieving sustained happiness. TH
References
1. Preview: heroin in the heartland. CBS News website. Available at: www.cbsnews.com/videos/preview-heroin-in-the-heartland. Accessed Feb. 1, 2016.
2. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. doi:10.1016/j.maocop.2015.08.023.
3. Mata DA, Ramos MA, Bansal N. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383. doi:10.1001/jama.2015.15845.
4. Grant A. Does trying to be happy make us unhappy? DailyGood website. Available at: http://www.dailygood.org/story/1187/does-trying-to-be-happy-make-us-unhappy-adam-grant/. Accessed Feb. 1, 2016.

Every American knows this well-known phrase from the Declaration of Independence, which describes the three “unalienable rights” ordained on humans by their Creator and which governments are bound to dutifully protect. But I wonder if the last unalienable right has implications for career happiness in the healthcare industry, particularly for hospitalists. With the phrase now being 240 years old, it has understandably permeated every inch of American society and affected every crevice of the American psyche. Despite having this decreed inalienable right of the pursuit of happiness, there is evidence of widespread dissatisfaction and unhappiness within our profession.
Speaking of happiness, I was listening to a 60 Minutes podcast entitled “Heroin in the Heartland.” It described a widespread affliction of heroin among mainstream middle- and upper-class suburban youths.1 During the piece, they interviewed several addicted youngsters and their parents. I was struck by the story of a young woman named Hannah; she described how and why she became addicted to heroin in her upper-middle-class high school in Columbus, Ohio. She described how heroin made her feel. On a scale of 1–10 in happiness, she said it made her feel like a “26.” She and many of her friends became addicted to the feeling of happiness that was infused into them, a feeling that could not be replicated without the use of the drug. She and her friends started their road to addiction in a quest for their unalienable right of the pursuit of happiness.
Contrast that story with the “unhappiness factor” that plagues U.S. physicians. A 2014 survey found that 54% of physicians reported at least one symptom of burnout.2 That figure was up from 46% in a 2011 survey. From 2011 to 2014, satisfaction with work-life balance dropped to 41% from 49%. Within that same time frame, burnout and dissatisfaction showed very little change in other U.S. working adults, widening the gap in dissatisfaction between physicians and non-physicians. Even after adjusting for age, sex, relationship status, and hours worked, physicians still were almost twice as likely to experience burnout than other working U.S. adults, and they only had an odds ratio of satisfaction of 0.68 (95% CI, 0.62–0.75) compared with non-physicians. In another recent (and sobering) meta-analysis, researchers found that about a third of all resident physicians report depression or depressive symptoms during their training (ranging from 21% to 43%, depending on the instrument used).3
Could it be that physicians in the U.S., in their quest for the pursuit of happiness, are looking for happiness in all the wrong ways? I read an article recently on DailyGood entitled “Does Trying to Be Happy Make Us Unhappy?”4 It describes several studies that purport that the more value people place on trying to become happy, the less happy they actually become. It turns out that in order for us to figure out if we are happy, we are forced to evaluate our current level of happiness and set that against some benchmark (usually from our own past) to analyze where we are. The mere act of doing this moves us from an experiential mode to an evaluation mode, which puts us out of touch with those things in life that can bring us joy and contentment.
Social scientists have found that when we are immersed in the present, we don’t report being happy in that moment, but we do report happiness later when reflecting on those moments. Ruminating about whether we are unhappy, depressed, burned out, or unsatisfied makes us inwardly focused and makes us lose the ability to become immersed in the present.
Scientists also have found that we tend to overestimate how external influences, such as getting a promotion or moving into a new job, will inflate our happiness and that we all adapt to new experiences and quickly return to our baseline happiness (as if the change never occurred). They’ve also found that when we pursue happiness as an individual state, we become inwardly focused and less likely to actually achieve happiness. People who are more outwardly focused on how others feel (and not how they themselves feel) are much more likely to achieve a state of sustained happiness.
Finally, researchers have found that happiness is more likely achieved by pursuing frequent positive emotions rather than intense positive emotions. Many of us search for single intense emotional experiences (the winning of a gold medal) in the pursuit of happiness, but researchers found that the frequency of positive emotions are much more important than the intensity of positive emotions.
So maybe, as physicians in pursuit of happiness, we are going about this pursuit all wrong, with resultant depression, dissatisfaction, and burnout. We can’t change the Declaration of Independence or the American psyche, but we can change how we perceive that pursuit.
Happiness is not a goal to be achieved but a state of mind to be savored. Immersing ourselves in our daily life, we should be outwardly focused on our colleagues and our patients. If we take this approach, there is no other profession better suited to actually achieving sustained happiness. TH
References
1. Preview: heroin in the heartland. CBS News website. Available at: www.cbsnews.com/videos/preview-heroin-in-the-heartland. Accessed Feb. 1, 2016.
2. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. doi:10.1016/j.maocop.2015.08.023.
3. Mata DA, Ramos MA, Bansal N. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383. doi:10.1001/jama.2015.15845.
4. Grant A. Does trying to be happy make us unhappy? DailyGood website. Available at: http://www.dailygood.org/story/1187/does-trying-to-be-happy-make-us-unhappy-adam-grant/. Accessed Feb. 1, 2016.

Every American knows this well-known phrase from the Declaration of Independence, which describes the three “unalienable rights” ordained on humans by their Creator and which governments are bound to dutifully protect. But I wonder if the last unalienable right has implications for career happiness in the healthcare industry, particularly for hospitalists. With the phrase now being 240 years old, it has understandably permeated every inch of American society and affected every crevice of the American psyche. Despite having this decreed inalienable right of the pursuit of happiness, there is evidence of widespread dissatisfaction and unhappiness within our profession.
Speaking of happiness, I was listening to a 60 Minutes podcast entitled “Heroin in the Heartland.” It described a widespread affliction of heroin among mainstream middle- and upper-class suburban youths.1 During the piece, they interviewed several addicted youngsters and their parents. I was struck by the story of a young woman named Hannah; she described how and why she became addicted to heroin in her upper-middle-class high school in Columbus, Ohio. She described how heroin made her feel. On a scale of 1–10 in happiness, she said it made her feel like a “26.” She and many of her friends became addicted to the feeling of happiness that was infused into them, a feeling that could not be replicated without the use of the drug. She and her friends started their road to addiction in a quest for their unalienable right of the pursuit of happiness.
Contrast that story with the “unhappiness factor” that plagues U.S. physicians. A 2014 survey found that 54% of physicians reported at least one symptom of burnout.2 That figure was up from 46% in a 2011 survey. From 2011 to 2014, satisfaction with work-life balance dropped to 41% from 49%. Within that same time frame, burnout and dissatisfaction showed very little change in other U.S. working adults, widening the gap in dissatisfaction between physicians and non-physicians. Even after adjusting for age, sex, relationship status, and hours worked, physicians still were almost twice as likely to experience burnout than other working U.S. adults, and they only had an odds ratio of satisfaction of 0.68 (95% CI, 0.62–0.75) compared with non-physicians. In another recent (and sobering) meta-analysis, researchers found that about a third of all resident physicians report depression or depressive symptoms during their training (ranging from 21% to 43%, depending on the instrument used).3
Could it be that physicians in the U.S., in their quest for the pursuit of happiness, are looking for happiness in all the wrong ways? I read an article recently on DailyGood entitled “Does Trying to Be Happy Make Us Unhappy?”4 It describes several studies that purport that the more value people place on trying to become happy, the less happy they actually become. It turns out that in order for us to figure out if we are happy, we are forced to evaluate our current level of happiness and set that against some benchmark (usually from our own past) to analyze where we are. The mere act of doing this moves us from an experiential mode to an evaluation mode, which puts us out of touch with those things in life that can bring us joy and contentment.
Social scientists have found that when we are immersed in the present, we don’t report being happy in that moment, but we do report happiness later when reflecting on those moments. Ruminating about whether we are unhappy, depressed, burned out, or unsatisfied makes us inwardly focused and makes us lose the ability to become immersed in the present.
Scientists also have found that we tend to overestimate how external influences, such as getting a promotion or moving into a new job, will inflate our happiness and that we all adapt to new experiences and quickly return to our baseline happiness (as if the change never occurred). They’ve also found that when we pursue happiness as an individual state, we become inwardly focused and less likely to actually achieve happiness. People who are more outwardly focused on how others feel (and not how they themselves feel) are much more likely to achieve a state of sustained happiness.
Finally, researchers have found that happiness is more likely achieved by pursuing frequent positive emotions rather than intense positive emotions. Many of us search for single intense emotional experiences (the winning of a gold medal) in the pursuit of happiness, but researchers found that the frequency of positive emotions are much more important than the intensity of positive emotions.
So maybe, as physicians in pursuit of happiness, we are going about this pursuit all wrong, with resultant depression, dissatisfaction, and burnout. We can’t change the Declaration of Independence or the American psyche, but we can change how we perceive that pursuit.
Happiness is not a goal to be achieved but a state of mind to be savored. Immersing ourselves in our daily life, we should be outwardly focused on our colleagues and our patients. If we take this approach, there is no other profession better suited to actually achieving sustained happiness. TH
References
1. Preview: heroin in the heartland. CBS News website. Available at: www.cbsnews.com/videos/preview-heroin-in-the-heartland. Accessed Feb. 1, 2016.
2. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. doi:10.1016/j.maocop.2015.08.023.
3. Mata DA, Ramos MA, Bansal N. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383. doi:10.1001/jama.2015.15845.
4. Grant A. Does trying to be happy make us unhappy? DailyGood website. Available at: http://www.dailygood.org/story/1187/does-trying-to-be-happy-make-us-unhappy-adam-grant/. Accessed Feb. 1, 2016.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Move to Allow Patients to Request 'Refund' Appealing and Risky
We’ve all seen hundreds of commercials from companies advertising products and services with a money-back guarantee. The Men’s Warehouse, for example, has been promising men across the globe for over a decade, “You’re going to like the way you look. I guarantee it!” But to date, no one has made such a “guarantee” in the healthcare industry. Buying a suit is not exactly like getting your gallbladder removed.
We know that medical diagnoses and treatments are filled with uncertainty in expected processes and outcomes, because the factors that are dependent on these processes and outcomes are endless. These include patient factors (overall health, functional status, comorbid conditions), procedural factors (emergency versus elective, time of day or night), and facility factors (having the optimal team with skills that match the patient need, having all the right products and equipment). Although we know that many medical procedures have a relatively predictable risk of complications, unpredictable complications still occur, so how can we ever offer a guarantee for the interventions we perform on patients?
First of Its Kind
David Feinberg, MD, MBA, president and CEO of Geisinger Health System, is doing just that. This healthcare system has developed an application, called the Geisinger ProvenExperience, which can be downloaded onto a smartphone. After a procedure, each patient is given a code for the condition that was treated. With that code, the patient can enter feedback on the services provided and can then request a refund if they are not fully satisfied.
Most remarkably, the request for a refund is based on the judgment of the recipient, not on that of the provider(s). At a recent public meeting, Dr. Feinberg said of the new program: “We’re going to do everything right. That’s our job, that’s our promise to you … and you’re the judge. If you don’t think so, we’re going to apologize, we’re going to try to fix it for the next guy, and, as a small token of appreciation, we’re going to give you some money back.”1
Although many are skeptical about whether or not the program will be successful, much less viable, Dr. Feinberg contends that early feedback on the program has shown that most patients don’t actually want their money back. Instead, if their needs have not been met, most have just wanted a sincere apology and a commitment to make things better for others. Dr. Feinberg also contests that even if this is not the best or only approach to improving healthcare (quickly), we should all feel compelled to do something about our repeated failures in meeting patient expectations in the quality and/or experience of their care; and because no other industry works this way, other than healthcare. Typically, when consumers get fed up with poor service in other industries, disruptive innovations (Uber, for example) are created to satisfy customers’ desires.
A New Paradigm?
In healthcare, patients certainly should be dissatisfied if they experience a preventable harm event. Some types of harm are considered “always preventable,” such as wrong-site surgery. These events are extremely rare and, thus, do not constitute most cases of harm in hospitals these days. Such “never events” are relatively well defined and have been adopted for nonpayment by Medicare and other insurers, which can serve to buffer a patient’s financial liability in the small number of these cases. For other, more common, types of preventable harm, some hospitals have instituted apology and disclosure policies, and some will also relieve the patient of the portion of the bill attributable to the preventable harm. But not all hospitals have adopted such policies, despite the fact that they are widely endorsed by influential agencies, including The Joint Commission, the American Medical Association, Leapfrog Group, the National Quality Forum, and the Agency for Healthcare Research and Quality.
And, even for hospitals that have adopted such “best practice” policies, there is not always clear consensus on what constitutes preventable harm. Generally, the “judgment call” about what constitutes preventable harm is made by healthcare systems and providers—not patients. In addition, many cases of harm that are not necessarily preventable can often result in great dissatisfaction for the patient. There are countless stories of patients who are unfortunately harmed in the course of medical procedures, but who were informed of the possible risks of the procedure and consented to have the procedure performed despite the risks. These situations, which are agonizingly difficult for the system, the providers, and the patients, have no good solutions. Systems cannot “own” all harm, such as those resulting from the disease process itself or from risky and invasive procedures intended to benefit the patient. And there is ongoing inconsistency in healthcare systems when it comes to their willingness and ability to consistently define preventable harm or to disclose, apologize, and forgive payments in such cases.
So, while this move to allow patients to ask for a “refund” seems both extremely appealing and extremely risky, it certainly seems as though it will greatly enhance the trust of patients and their families in the Geisinger Health System.
I, among others, will eagerly follow the results of this program; while getting a cholecystectomy is not the same as buying a men’s suit, I do hope that someday, I will be able to say to every patient entering my healthcare system that before they leave, “You’re going to like the way you feel. I guarantee it!” TH
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. Guydish M. Geisinger CEO: money-back guarantee for health care coming. November 6, 2015. Times Leader website. Available at: http://timesleader.com/news/492790/geisinger-ceo-money-back-guarantee-for-health-car-coming. Accessed December 5, 2015.
2. Luthra S. When something goes wrong at the hospital, who pays? November 11, 2015. Kaiser Health News. Available at: http://khn.org/news/when-something-goes-wrong-at-the-hospital-who-pays/?utm_source=Managed&utm_campaign=9e17712a95-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-9e17712a95-319388717. Accessed December 5, 2015.
We’ve all seen hundreds of commercials from companies advertising products and services with a money-back guarantee. The Men’s Warehouse, for example, has been promising men across the globe for over a decade, “You’re going to like the way you look. I guarantee it!” But to date, no one has made such a “guarantee” in the healthcare industry. Buying a suit is not exactly like getting your gallbladder removed.
We know that medical diagnoses and treatments are filled with uncertainty in expected processes and outcomes, because the factors that are dependent on these processes and outcomes are endless. These include patient factors (overall health, functional status, comorbid conditions), procedural factors (emergency versus elective, time of day or night), and facility factors (having the optimal team with skills that match the patient need, having all the right products and equipment). Although we know that many medical procedures have a relatively predictable risk of complications, unpredictable complications still occur, so how can we ever offer a guarantee for the interventions we perform on patients?
First of Its Kind
David Feinberg, MD, MBA, president and CEO of Geisinger Health System, is doing just that. This healthcare system has developed an application, called the Geisinger ProvenExperience, which can be downloaded onto a smartphone. After a procedure, each patient is given a code for the condition that was treated. With that code, the patient can enter feedback on the services provided and can then request a refund if they are not fully satisfied.
Most remarkably, the request for a refund is based on the judgment of the recipient, not on that of the provider(s). At a recent public meeting, Dr. Feinberg said of the new program: “We’re going to do everything right. That’s our job, that’s our promise to you … and you’re the judge. If you don’t think so, we’re going to apologize, we’re going to try to fix it for the next guy, and, as a small token of appreciation, we’re going to give you some money back.”1
Although many are skeptical about whether or not the program will be successful, much less viable, Dr. Feinberg contends that early feedback on the program has shown that most patients don’t actually want their money back. Instead, if their needs have not been met, most have just wanted a sincere apology and a commitment to make things better for others. Dr. Feinberg also contests that even if this is not the best or only approach to improving healthcare (quickly), we should all feel compelled to do something about our repeated failures in meeting patient expectations in the quality and/or experience of their care; and because no other industry works this way, other than healthcare. Typically, when consumers get fed up with poor service in other industries, disruptive innovations (Uber, for example) are created to satisfy customers’ desires.
A New Paradigm?
In healthcare, patients certainly should be dissatisfied if they experience a preventable harm event. Some types of harm are considered “always preventable,” such as wrong-site surgery. These events are extremely rare and, thus, do not constitute most cases of harm in hospitals these days. Such “never events” are relatively well defined and have been adopted for nonpayment by Medicare and other insurers, which can serve to buffer a patient’s financial liability in the small number of these cases. For other, more common, types of preventable harm, some hospitals have instituted apology and disclosure policies, and some will also relieve the patient of the portion of the bill attributable to the preventable harm. But not all hospitals have adopted such policies, despite the fact that they are widely endorsed by influential agencies, including The Joint Commission, the American Medical Association, Leapfrog Group, the National Quality Forum, and the Agency for Healthcare Research and Quality.
And, even for hospitals that have adopted such “best practice” policies, there is not always clear consensus on what constitutes preventable harm. Generally, the “judgment call” about what constitutes preventable harm is made by healthcare systems and providers—not patients. In addition, many cases of harm that are not necessarily preventable can often result in great dissatisfaction for the patient. There are countless stories of patients who are unfortunately harmed in the course of medical procedures, but who were informed of the possible risks of the procedure and consented to have the procedure performed despite the risks. These situations, which are agonizingly difficult for the system, the providers, and the patients, have no good solutions. Systems cannot “own” all harm, such as those resulting from the disease process itself or from risky and invasive procedures intended to benefit the patient. And there is ongoing inconsistency in healthcare systems when it comes to their willingness and ability to consistently define preventable harm or to disclose, apologize, and forgive payments in such cases.
So, while this move to allow patients to ask for a “refund” seems both extremely appealing and extremely risky, it certainly seems as though it will greatly enhance the trust of patients and their families in the Geisinger Health System.
I, among others, will eagerly follow the results of this program; while getting a cholecystectomy is not the same as buying a men’s suit, I do hope that someday, I will be able to say to every patient entering my healthcare system that before they leave, “You’re going to like the way you feel. I guarantee it!” TH
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. Guydish M. Geisinger CEO: money-back guarantee for health care coming. November 6, 2015. Times Leader website. Available at: http://timesleader.com/news/492790/geisinger-ceo-money-back-guarantee-for-health-car-coming. Accessed December 5, 2015.
2. Luthra S. When something goes wrong at the hospital, who pays? November 11, 2015. Kaiser Health News. Available at: http://khn.org/news/when-something-goes-wrong-at-the-hospital-who-pays/?utm_source=Managed&utm_campaign=9e17712a95-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-9e17712a95-319388717. Accessed December 5, 2015.
We’ve all seen hundreds of commercials from companies advertising products and services with a money-back guarantee. The Men’s Warehouse, for example, has been promising men across the globe for over a decade, “You’re going to like the way you look. I guarantee it!” But to date, no one has made such a “guarantee” in the healthcare industry. Buying a suit is not exactly like getting your gallbladder removed.
We know that medical diagnoses and treatments are filled with uncertainty in expected processes and outcomes, because the factors that are dependent on these processes and outcomes are endless. These include patient factors (overall health, functional status, comorbid conditions), procedural factors (emergency versus elective, time of day or night), and facility factors (having the optimal team with skills that match the patient need, having all the right products and equipment). Although we know that many medical procedures have a relatively predictable risk of complications, unpredictable complications still occur, so how can we ever offer a guarantee for the interventions we perform on patients?
First of Its Kind
David Feinberg, MD, MBA, president and CEO of Geisinger Health System, is doing just that. This healthcare system has developed an application, called the Geisinger ProvenExperience, which can be downloaded onto a smartphone. After a procedure, each patient is given a code for the condition that was treated. With that code, the patient can enter feedback on the services provided and can then request a refund if they are not fully satisfied.
Most remarkably, the request for a refund is based on the judgment of the recipient, not on that of the provider(s). At a recent public meeting, Dr. Feinberg said of the new program: “We’re going to do everything right. That’s our job, that’s our promise to you … and you’re the judge. If you don’t think so, we’re going to apologize, we’re going to try to fix it for the next guy, and, as a small token of appreciation, we’re going to give you some money back.”1
Although many are skeptical about whether or not the program will be successful, much less viable, Dr. Feinberg contends that early feedback on the program has shown that most patients don’t actually want their money back. Instead, if their needs have not been met, most have just wanted a sincere apology and a commitment to make things better for others. Dr. Feinberg also contests that even if this is not the best or only approach to improving healthcare (quickly), we should all feel compelled to do something about our repeated failures in meeting patient expectations in the quality and/or experience of their care; and because no other industry works this way, other than healthcare. Typically, when consumers get fed up with poor service in other industries, disruptive innovations (Uber, for example) are created to satisfy customers’ desires.
A New Paradigm?
In healthcare, patients certainly should be dissatisfied if they experience a preventable harm event. Some types of harm are considered “always preventable,” such as wrong-site surgery. These events are extremely rare and, thus, do not constitute most cases of harm in hospitals these days. Such “never events” are relatively well defined and have been adopted for nonpayment by Medicare and other insurers, which can serve to buffer a patient’s financial liability in the small number of these cases. For other, more common, types of preventable harm, some hospitals have instituted apology and disclosure policies, and some will also relieve the patient of the portion of the bill attributable to the preventable harm. But not all hospitals have adopted such policies, despite the fact that they are widely endorsed by influential agencies, including The Joint Commission, the American Medical Association, Leapfrog Group, the National Quality Forum, and the Agency for Healthcare Research and Quality.
And, even for hospitals that have adopted such “best practice” policies, there is not always clear consensus on what constitutes preventable harm. Generally, the “judgment call” about what constitutes preventable harm is made by healthcare systems and providers—not patients. In addition, many cases of harm that are not necessarily preventable can often result in great dissatisfaction for the patient. There are countless stories of patients who are unfortunately harmed in the course of medical procedures, but who were informed of the possible risks of the procedure and consented to have the procedure performed despite the risks. These situations, which are agonizingly difficult for the system, the providers, and the patients, have no good solutions. Systems cannot “own” all harm, such as those resulting from the disease process itself or from risky and invasive procedures intended to benefit the patient. And there is ongoing inconsistency in healthcare systems when it comes to their willingness and ability to consistently define preventable harm or to disclose, apologize, and forgive payments in such cases.
So, while this move to allow patients to ask for a “refund” seems both extremely appealing and extremely risky, it certainly seems as though it will greatly enhance the trust of patients and their families in the Geisinger Health System.
I, among others, will eagerly follow the results of this program; while getting a cholecystectomy is not the same as buying a men’s suit, I do hope that someday, I will be able to say to every patient entering my healthcare system that before they leave, “You’re going to like the way you feel. I guarantee it!” TH
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1. Guydish M. Geisinger CEO: money-back guarantee for health care coming. November 6, 2015. Times Leader website. Available at: http://timesleader.com/news/492790/geisinger-ceo-money-back-guarantee-for-health-car-coming. Accessed December 5, 2015.
2. Luthra S. When something goes wrong at the hospital, who pays? November 11, 2015. Kaiser Health News. Available at: http://khn.org/news/when-something-goes-wrong-at-the-hospital-who-pays/?utm_source=Managed&utm_campaign=9e17712a95-Quality+%26+Patient+Safety+Update&utm_medium=email&utm_term=0_ebe1fa6178-9e17712a95-319388717. Accessed December 5, 2015.