User login
Things We Do for No Reason™: Routine Coverage of Anaerobes in Aspiration Pneumonia
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
An 88-year-old woman with a history of dementia presents to the emergency room with new-onset dyspnea following 2 days of a self-limited gastrointestinal illness associated with nausea, vomiting, and diarrhea. After noting a new supplemental oxygen requirement of 4 L and a temperature of 38.6 °C, the hospitalist’s exam finds an edentulous patient with bibasilar lung crackles and a nontender abdomen. Taking into account her elevated white blood cell count and chest radiograph with right greater than left bibasilar opacities, the admitting hospitalist diagnoses aspiration pneumonia (AP) and specifically selects an antibiotic regimen with anaerobic coverage.
BACKGROUND
Aspiration, the inhalation of oropharyngeal or gastric materials into the lung, takes one of the following three forms: (1) “microaspiration,” wherein a small number of virulent organisms from oropharynx gains entry into the alveoli, (2) “macroaspiration,” wherein a large volume of typically less virulent organisms gains entry into the airways, or (3) a combination of the two. Hospitalists may struggle to distinguish unwitnessed macroaspiration causing AP from other typical causes of pneumonia, such as community-acquired pneumonia (CAP) or hospital-acquired pneumonia (HAP).1 A hospitalist should suspect macroaspiration—the most common cause of AP—in patients with risk factors such as dysphagia, diminished cough reflex or impaired swallowing, and infiltrates in the dependent bronchopulmonary segments, or of course, in cases of witnessed aspiration.2
Moreover, hospitalists must differentiate AP, an infectious entity, from aspiration pneumonitis, a noninfectious entity caused by macroaspiration of mostly sterile gastric content. Aspiration pneumonitis presents with acute lung injury within hours of an aspiration event, whereas AP entails a gradual onset of symptoms and signs of pneumonia.2 Although aspiration pneumonitis can present dramatically with hypoxemia and pulmonary edema and may evolve into AP, patients do not initially benefit from empiric antibiotics.1
WHY YOU MIGHT THINK SPECIFIC ANAEROBIC COVERAGE IS ESSENTIAL
In the 1970s, several studies of patients who were presumed to have AP because of risk factors for macroaspiration, such as alcohol use disorder, illicit drug use, and seizure disorder, identified anaerobes as major etiologic pathogens. These studies reported the presence of putrid sputum and obtained samples through invasive methods (eg, transtracheal aspirates, thoracentesis, and blood cultures).3,4 Many of the patients studied had radiographic findings of pleuropulmonary disease. For example, in the study by Bartlett et al, 70% of patients had radiographic evidence of abscess or pulmonary necrosis. These findings led to the assumption that anaerobes play a significant role in all cases of aspiration-related pulmonary syndromes. Because anaerobic bacteria live in the gingival sulcus, with an especially high burden in dental plaques, their role as a potential pathogen in AP may seem logical.5 Given the backdrop of those concerns, Kioka et al found that providers treated 90% of presumed AP patients in the intensive care unit with antibiotics that have anaerobic activity despite only 30% meeting the criteria for anaerobic coverage.6
WHY ANAEROBIC COVERAGE IS NOT ROUTINELY NECESSARY
In contrast to the population of patients with AP described from the 1970s, we now diagnose AP more frequently in nursing home residents, the elderly with cognitive impairment, and those with tube feed dependence, dysphagia, or gastrointestinal motility disorders.1 Concurrent with this change in the epidemiology of AP, we have witnessed a shift in recovered bacteria from anaerobes to aerobes in recent studies.7,8 In an intensive care unit study from 1999, respiratory tract organisms of patients with suspected aspiration mirrored those of patients with CAP or HAP.9 In a systematic review of eight observational studies that included studies from 1993 to 2014 and involved elderly patients with uncomplicated AP, only two out of eight studies demonstrated the presence of anaerobes in respiratory cultures. Even in those two studies, anaerobic bacteria frequently coexisted with aerobes. The majority of organisms in all eight studies consisted of aerobic gram-positives, gram-negatives, or both.10
A study by El-Solh et al most frequently isolated pathogenic aerobic gram-negative bacteria (49% of cases), followed by anaerobic bacteria (16%), among institutionalized elderly patients with severe AP diagnosed by clinical features. In that same study, most anaerobes coexisted with aerobic gram-negative bacteria, and the clinical illness promptly resolved in the absence of specific anaerobic coverage.11 AP can be successfully treated without anaerobic coverage due to a variety of factors: the insignificant role of anaerobes in the pathogenesis of uncomplicated AP, lower severity of illness in the absence of abscesses or pulmonary necrosis (uncomplicated), and altered local redox-potential from the elimination of aerobic pathogens, which effectively also treats anaerobes.1 Moreover, anaerobes possess generally less virulence in comparison with aerobes. AP from these organisms typically requires risk for excessive oral growth (eg, periodontal disease) and macroaspiration of a large number of organisms.5
There are also potential harms associated with the unnecessary treatment of anaerobic bacteria. Since anaerobes account for the majority of the bacteria present in the bowel, targeting anaerobes can result in gut dysbiosis.1 Moreover, a prospective study showed an increase in the incidence of vancomycin-resistant enterococci and antibiotic-resistant gram-negative bacteria associated with the empiric use of antibiotics with anaerobic activity.12 Finally, a systematic review detailed the high incidence of Clostridioides difficile infections among patients receiving clindamycin and carbapenems.13
WHEN ANAEROBIC COVERAGE IS INDICATED
Despite the predominance of aerobic organisms in the respiratory tract specimens of patients diagnosed with AP in the current era, situations still exist that require treatment of anaerobes. These include necrotizing pneumonia, empyema, or lung abscess.2 Additionally, patients with severe periodontal disease may harbor anaerobic bacteria such as Bacteroides species, Peptostreptococcus species, and Actinomyces israelii.5 When we suspect macroaspiration leading to AP, patients with severe periodontal disease may benefit from anaerobic coverage. Putrid sputum generation may indicate the presence of anaerobic organisms that produce the characteristic foul odor of short-chain volatile fatty acids observed in patients with lung abscess or empyema.2 It often takes about 8 to 14 days after an aspiration event for lung cavitation or empyema to develop.14 Therefore, a longer duration of illness or putrid sputum production may signal a significant concurrent burden of anaerobes. The 2019 official guidelines of the American Thoracic Society and Infectious Disease Society of America recommend adding anaerobic coverage to CAP only when empyema or lung abscess is suspected (conditional recommendation, very low quality of evidence).15
WHAT YOU SHOULD DO INSTEAD
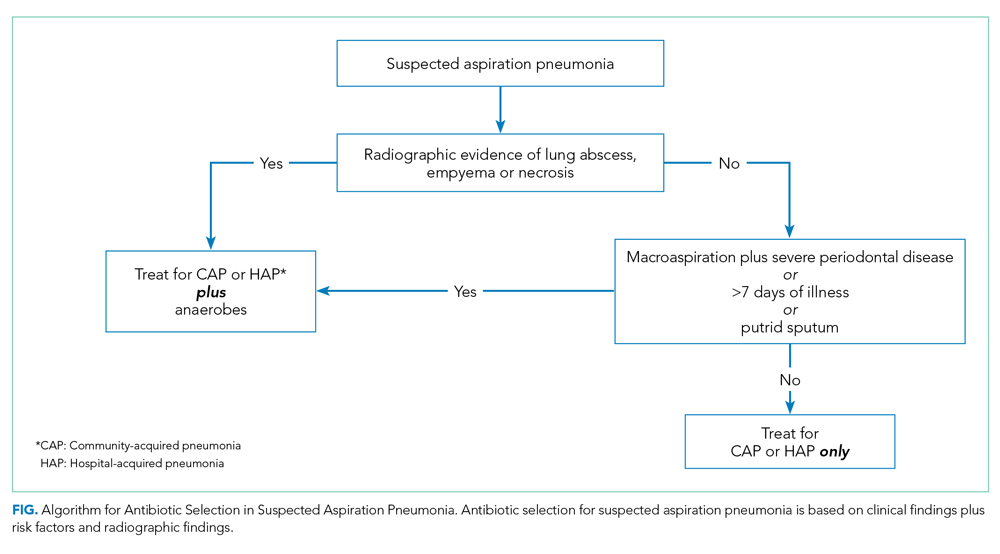
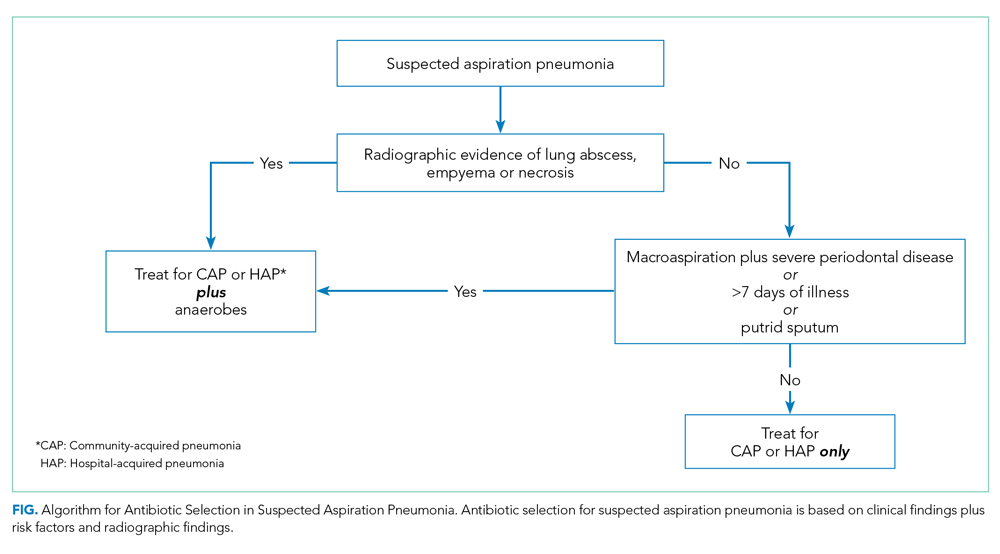
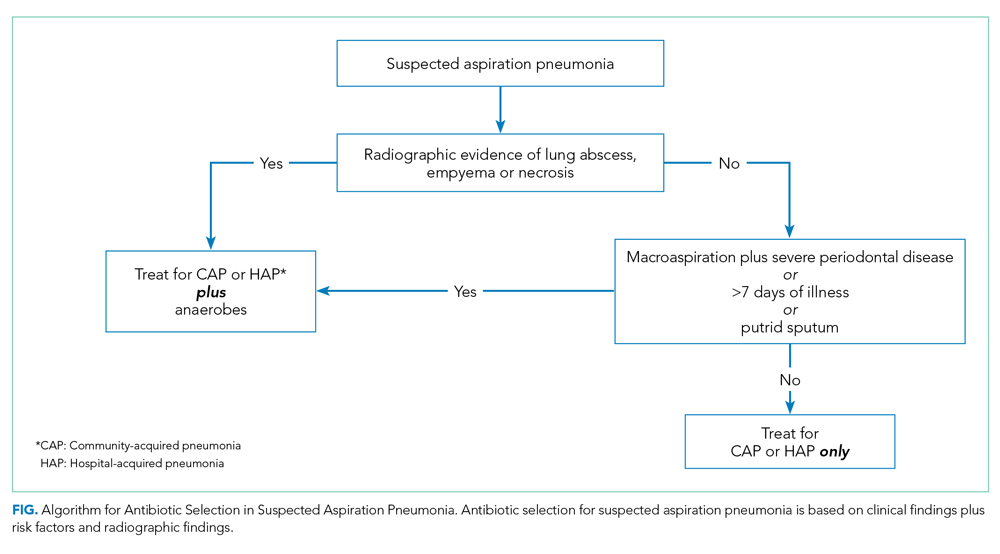
When you suspect AP in a patient, categorize it as either community or hospital acquired based on risk factors similar to CAP or HAP. For patients with witnessed macroaspiration or in patients with substantial macroaspiration risk factors, perform a radiologic evaluation and a thorough oral examination to evaluate for poor dentition, gingival disease (marked redness, tendency to bleed, ulceration), and tongue coating. For patients presenting from the community with suspected AP without complications, treat with the standard therapy (without additional anaerobic coverage) for CAP. Provide empiric anaerobic coverage for complicated AP (eg, lung abscess, necrosis, or empyema) or for macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness. Similarly, treat hospital-acquired AP as HAP (Figure).
When prescribing anaerobic coverage of AP, use combination drugs that include a ß-lactamase inhibitor (eg, ampicillin-sulbactam), clindamycin (either alone or in combination with ß-lactams), or moxifloxacin.1 Most anaerobes have ß-lactamase or cephalosporinase activity, which renders penicillin and cephalosporins ineffective. Despite its potential side effects, such as C difficile infection, treating with clindamycin has the benefit of a relatively low cost and its association with lower rates of methicillin-resistant Staphylococcus aureus emergence after treatment.16 Piperacillin-tazobactam and carbapenems also have excellent anaerobic coverage, but we should reserve them for more severe and complicated cases of AP given their extensive antibacterial activity and concern for the emergence of resistance.8 Although well known and used for decades for its activity against clinically important anaerobes, avoid metronidazole due to its reduced cure rate in lung abscess caused by microaerophilic streptococci of the oral cavity.17 Due to a lack of evidence, we do not recommend the use of metronidazole in lung infections.
RECOMMENDATIONS
- Empirically treat most suspected cases of AP with regimens similar to the standard antibiotics for CAP and HAP. In the absence of specific risk factors for anaerobic infections, do not routinely provide anaerobic coverage.
- Provide anaerobic coverage empirically for AP associated with macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness.
- Provide anaerobic coverage in AP with evidence of necrotizing pneumonia, empyema, or lung abscess.
CONCLUSION
Current evidence does not support routine anaerobic coverage of AP in the absence of identifiable risk factors for an anaerobic lung infection.
In consideration of the clinical case, importantly, she has no periodontal disease and no evidence for necrotizing pneumonia, empyema, or lung abscess radiographically. For these reasons, select an empiric antibiotic regime that targets CAP organisms predominantly and forgo additional anaerobic coverage.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason ™ ”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason ™ ” topics by emailing [email protected].
Disclosures
The authors have no conflicts of interest relevant to this article.
1. Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019;380(7):651-663. https://doi.org/10.1056/nejmra1714562
2. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665-671. https://doi.org/10.1056/nejm200103013440908
3. Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med. 1974;56(2):202-207. https://doi.org/10.1016/0002-9343(74)90598-1
4. Bartlett JG, Gorbach SL. The triple threat of aspiration pneumonia. Chest. 1975;68(4):560-566. https://doi.org/10.1378/chest.68.4.560
5. Sutter VL. Anaerobes as normal oral flora. Rev Infect Dis. 1984;6(suppl 1):S62-S66. https://doi.org/10.1093/clinids/6.supplement_1.s62
6. Kioka MJ, DiGiovine B, Rezik M, Jennings JH. Anaerobic antibiotic usage for pneumonia in the medical intensive care unit. Respirology. 2017;22(8):1656-1661. https://doi.org/10.1111/resp.13111
7. Ott SR, Allewelt M, Lorenz J, Reimnitz P, Lode H; German Lung Abscess Study Group. Moxifloxacin vs ampicillin/sulbactam in aspiration pneumonia and primary lung abscess. Infection. 2008;36(1):23-30. https://doi.org/10.1007/s15010-007-7043-6
8. Tokuyasu H, Harada T, Watanabe E, et al. Effectiveness of meropenem for the treatment of aspiration pneumonia in elderly patients. Intern Med. 2009;48(3):129-135. https://doi.org/10.2169/internalmedicine.48.1308
9. Marik PE, Careau P. The role of anaerobes in patients with ventilator-associated pneumonia and aspiration pneumonia: a prospective study. Chest. 1999;115(1):178-183. https://doi.org/10.1378/chest.115.1.178
10. Bowerman TJ, Zhang J, Waite LM. Antibacterial treatment of aspiration pneumonia in older people: a systematic review. Clin Interv Aging. 2018;13:2201-2213. https://doi.org/10.2147/cia.s183344
11. El-Solh AA, Pietrantoni C, Bhat A, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003;167(12):1650-1654. https://doi.org/10.1164/rccm.200212-1543oc
12. Bhalla A, Pultz NJ, Ray AJ, Hoyen CK, Eckstein EC, Donskey CJ. Antianaerobic antibiotic therapy promotes overgrowth of antibiotic-resistant, gram-negative bacilli and vancomycin-resistant enterococci in the stool of colonized patients. Infect Control Hosp Epidemiol. 2003;24(9):644-649. https://doi.org/10.1086/502267
13. Vardakas KZ, Trigkidis KK, Boukouvala E, Falagas ME. Clostridium difficile infection following systemic antibiotic administration in randomised controlled trials: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;48(1):1-10. https://doi.org/10.1016/j.ijantimicag.2016.03.008
14. Leatherman JW, Iber C, F Davies SF. Cavitation in bacteremic pneumococcal pneumonia. Causal role of mixed infection with anaerobic bacteria. Am Rev Respir Dis. 1984;129(2):317-321.
15. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581st
16. Kadowaki M, Demura Y, Mizuno S, et al. Reappraisal of clindamycin IV monotherapy for treatment of mild-to-moderate aspiration pneumonia in elderly patients. Chest. 2005;127(4):1276-1282. https://doi.org/10.1378/chest.127.4.1276
17. Perlino CA. Metronidazole vs clindamycin treatment of anaerobic pulmonary infection. Failure of metronidazole therapy. Arch Intern Med. 1981;141(11):1424-1427.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
An 88-year-old woman with a history of dementia presents to the emergency room with new-onset dyspnea following 2 days of a self-limited gastrointestinal illness associated with nausea, vomiting, and diarrhea. After noting a new supplemental oxygen requirement of 4 L and a temperature of 38.6 °C, the hospitalist’s exam finds an edentulous patient with bibasilar lung crackles and a nontender abdomen. Taking into account her elevated white blood cell count and chest radiograph with right greater than left bibasilar opacities, the admitting hospitalist diagnoses aspiration pneumonia (AP) and specifically selects an antibiotic regimen with anaerobic coverage.
BACKGROUND
Aspiration, the inhalation of oropharyngeal or gastric materials into the lung, takes one of the following three forms: (1) “microaspiration,” wherein a small number of virulent organisms from oropharynx gains entry into the alveoli, (2) “macroaspiration,” wherein a large volume of typically less virulent organisms gains entry into the airways, or (3) a combination of the two. Hospitalists may struggle to distinguish unwitnessed macroaspiration causing AP from other typical causes of pneumonia, such as community-acquired pneumonia (CAP) or hospital-acquired pneumonia (HAP).1 A hospitalist should suspect macroaspiration—the most common cause of AP—in patients with risk factors such as dysphagia, diminished cough reflex or impaired swallowing, and infiltrates in the dependent bronchopulmonary segments, or of course, in cases of witnessed aspiration.2
Moreover, hospitalists must differentiate AP, an infectious entity, from aspiration pneumonitis, a noninfectious entity caused by macroaspiration of mostly sterile gastric content. Aspiration pneumonitis presents with acute lung injury within hours of an aspiration event, whereas AP entails a gradual onset of symptoms and signs of pneumonia.2 Although aspiration pneumonitis can present dramatically with hypoxemia and pulmonary edema and may evolve into AP, patients do not initially benefit from empiric antibiotics.1
WHY YOU MIGHT THINK SPECIFIC ANAEROBIC COVERAGE IS ESSENTIAL
In the 1970s, several studies of patients who were presumed to have AP because of risk factors for macroaspiration, such as alcohol use disorder, illicit drug use, and seizure disorder, identified anaerobes as major etiologic pathogens. These studies reported the presence of putrid sputum and obtained samples through invasive methods (eg, transtracheal aspirates, thoracentesis, and blood cultures).3,4 Many of the patients studied had radiographic findings of pleuropulmonary disease. For example, in the study by Bartlett et al, 70% of patients had radiographic evidence of abscess or pulmonary necrosis. These findings led to the assumption that anaerobes play a significant role in all cases of aspiration-related pulmonary syndromes. Because anaerobic bacteria live in the gingival sulcus, with an especially high burden in dental plaques, their role as a potential pathogen in AP may seem logical.5 Given the backdrop of those concerns, Kioka et al found that providers treated 90% of presumed AP patients in the intensive care unit with antibiotics that have anaerobic activity despite only 30% meeting the criteria for anaerobic coverage.6
WHY ANAEROBIC COVERAGE IS NOT ROUTINELY NECESSARY
In contrast to the population of patients with AP described from the 1970s, we now diagnose AP more frequently in nursing home residents, the elderly with cognitive impairment, and those with tube feed dependence, dysphagia, or gastrointestinal motility disorders.1 Concurrent with this change in the epidemiology of AP, we have witnessed a shift in recovered bacteria from anaerobes to aerobes in recent studies.7,8 In an intensive care unit study from 1999, respiratory tract organisms of patients with suspected aspiration mirrored those of patients with CAP or HAP.9 In a systematic review of eight observational studies that included studies from 1993 to 2014 and involved elderly patients with uncomplicated AP, only two out of eight studies demonstrated the presence of anaerobes in respiratory cultures. Even in those two studies, anaerobic bacteria frequently coexisted with aerobes. The majority of organisms in all eight studies consisted of aerobic gram-positives, gram-negatives, or both.10
A study by El-Solh et al most frequently isolated pathogenic aerobic gram-negative bacteria (49% of cases), followed by anaerobic bacteria (16%), among institutionalized elderly patients with severe AP diagnosed by clinical features. In that same study, most anaerobes coexisted with aerobic gram-negative bacteria, and the clinical illness promptly resolved in the absence of specific anaerobic coverage.11 AP can be successfully treated without anaerobic coverage due to a variety of factors: the insignificant role of anaerobes in the pathogenesis of uncomplicated AP, lower severity of illness in the absence of abscesses or pulmonary necrosis (uncomplicated), and altered local redox-potential from the elimination of aerobic pathogens, which effectively also treats anaerobes.1 Moreover, anaerobes possess generally less virulence in comparison with aerobes. AP from these organisms typically requires risk for excessive oral growth (eg, periodontal disease) and macroaspiration of a large number of organisms.5
There are also potential harms associated with the unnecessary treatment of anaerobic bacteria. Since anaerobes account for the majority of the bacteria present in the bowel, targeting anaerobes can result in gut dysbiosis.1 Moreover, a prospective study showed an increase in the incidence of vancomycin-resistant enterococci and antibiotic-resistant gram-negative bacteria associated with the empiric use of antibiotics with anaerobic activity.12 Finally, a systematic review detailed the high incidence of Clostridioides difficile infections among patients receiving clindamycin and carbapenems.13
WHEN ANAEROBIC COVERAGE IS INDICATED
Despite the predominance of aerobic organisms in the respiratory tract specimens of patients diagnosed with AP in the current era, situations still exist that require treatment of anaerobes. These include necrotizing pneumonia, empyema, or lung abscess.2 Additionally, patients with severe periodontal disease may harbor anaerobic bacteria such as Bacteroides species, Peptostreptococcus species, and Actinomyces israelii.5 When we suspect macroaspiration leading to AP, patients with severe periodontal disease may benefit from anaerobic coverage. Putrid sputum generation may indicate the presence of anaerobic organisms that produce the characteristic foul odor of short-chain volatile fatty acids observed in patients with lung abscess or empyema.2 It often takes about 8 to 14 days after an aspiration event for lung cavitation or empyema to develop.14 Therefore, a longer duration of illness or putrid sputum production may signal a significant concurrent burden of anaerobes. The 2019 official guidelines of the American Thoracic Society and Infectious Disease Society of America recommend adding anaerobic coverage to CAP only when empyema or lung abscess is suspected (conditional recommendation, very low quality of evidence).15
WHAT YOU SHOULD DO INSTEAD
When you suspect AP in a patient, categorize it as either community or hospital acquired based on risk factors similar to CAP or HAP. For patients with witnessed macroaspiration or in patients with substantial macroaspiration risk factors, perform a radiologic evaluation and a thorough oral examination to evaluate for poor dentition, gingival disease (marked redness, tendency to bleed, ulceration), and tongue coating. For patients presenting from the community with suspected AP without complications, treat with the standard therapy (without additional anaerobic coverage) for CAP. Provide empiric anaerobic coverage for complicated AP (eg, lung abscess, necrosis, or empyema) or for macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness. Similarly, treat hospital-acquired AP as HAP (Figure).
When prescribing anaerobic coverage of AP, use combination drugs that include a ß-lactamase inhibitor (eg, ampicillin-sulbactam), clindamycin (either alone or in combination with ß-lactams), or moxifloxacin.1 Most anaerobes have ß-lactamase or cephalosporinase activity, which renders penicillin and cephalosporins ineffective. Despite its potential side effects, such as C difficile infection, treating with clindamycin has the benefit of a relatively low cost and its association with lower rates of methicillin-resistant Staphylococcus aureus emergence after treatment.16 Piperacillin-tazobactam and carbapenems also have excellent anaerobic coverage, but we should reserve them for more severe and complicated cases of AP given their extensive antibacterial activity and concern for the emergence of resistance.8 Although well known and used for decades for its activity against clinically important anaerobes, avoid metronidazole due to its reduced cure rate in lung abscess caused by microaerophilic streptococci of the oral cavity.17 Due to a lack of evidence, we do not recommend the use of metronidazole in lung infections.
RECOMMENDATIONS
- Empirically treat most suspected cases of AP with regimens similar to the standard antibiotics for CAP and HAP. In the absence of specific risk factors for anaerobic infections, do not routinely provide anaerobic coverage.
- Provide anaerobic coverage empirically for AP associated with macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness.
- Provide anaerobic coverage in AP with evidence of necrotizing pneumonia, empyema, or lung abscess.
CONCLUSION
Current evidence does not support routine anaerobic coverage of AP in the absence of identifiable risk factors for an anaerobic lung infection.
In consideration of the clinical case, importantly, she has no periodontal disease and no evidence for necrotizing pneumonia, empyema, or lung abscess radiographically. For these reasons, select an empiric antibiotic regime that targets CAP organisms predominantly and forgo additional anaerobic coverage.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason ™ ”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason ™ ” topics by emailing [email protected].
Disclosures
The authors have no conflicts of interest relevant to this article.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
An 88-year-old woman with a history of dementia presents to the emergency room with new-onset dyspnea following 2 days of a self-limited gastrointestinal illness associated with nausea, vomiting, and diarrhea. After noting a new supplemental oxygen requirement of 4 L and a temperature of 38.6 °C, the hospitalist’s exam finds an edentulous patient with bibasilar lung crackles and a nontender abdomen. Taking into account her elevated white blood cell count and chest radiograph with right greater than left bibasilar opacities, the admitting hospitalist diagnoses aspiration pneumonia (AP) and specifically selects an antibiotic regimen with anaerobic coverage.
BACKGROUND
Aspiration, the inhalation of oropharyngeal or gastric materials into the lung, takes one of the following three forms: (1) “microaspiration,” wherein a small number of virulent organisms from oropharynx gains entry into the alveoli, (2) “macroaspiration,” wherein a large volume of typically less virulent organisms gains entry into the airways, or (3) a combination of the two. Hospitalists may struggle to distinguish unwitnessed macroaspiration causing AP from other typical causes of pneumonia, such as community-acquired pneumonia (CAP) or hospital-acquired pneumonia (HAP).1 A hospitalist should suspect macroaspiration—the most common cause of AP—in patients with risk factors such as dysphagia, diminished cough reflex or impaired swallowing, and infiltrates in the dependent bronchopulmonary segments, or of course, in cases of witnessed aspiration.2
Moreover, hospitalists must differentiate AP, an infectious entity, from aspiration pneumonitis, a noninfectious entity caused by macroaspiration of mostly sterile gastric content. Aspiration pneumonitis presents with acute lung injury within hours of an aspiration event, whereas AP entails a gradual onset of symptoms and signs of pneumonia.2 Although aspiration pneumonitis can present dramatically with hypoxemia and pulmonary edema and may evolve into AP, patients do not initially benefit from empiric antibiotics.1
WHY YOU MIGHT THINK SPECIFIC ANAEROBIC COVERAGE IS ESSENTIAL
In the 1970s, several studies of patients who were presumed to have AP because of risk factors for macroaspiration, such as alcohol use disorder, illicit drug use, and seizure disorder, identified anaerobes as major etiologic pathogens. These studies reported the presence of putrid sputum and obtained samples through invasive methods (eg, transtracheal aspirates, thoracentesis, and blood cultures).3,4 Many of the patients studied had radiographic findings of pleuropulmonary disease. For example, in the study by Bartlett et al, 70% of patients had radiographic evidence of abscess or pulmonary necrosis. These findings led to the assumption that anaerobes play a significant role in all cases of aspiration-related pulmonary syndromes. Because anaerobic bacteria live in the gingival sulcus, with an especially high burden in dental plaques, their role as a potential pathogen in AP may seem logical.5 Given the backdrop of those concerns, Kioka et al found that providers treated 90% of presumed AP patients in the intensive care unit with antibiotics that have anaerobic activity despite only 30% meeting the criteria for anaerobic coverage.6
WHY ANAEROBIC COVERAGE IS NOT ROUTINELY NECESSARY
In contrast to the population of patients with AP described from the 1970s, we now diagnose AP more frequently in nursing home residents, the elderly with cognitive impairment, and those with tube feed dependence, dysphagia, or gastrointestinal motility disorders.1 Concurrent with this change in the epidemiology of AP, we have witnessed a shift in recovered bacteria from anaerobes to aerobes in recent studies.7,8 In an intensive care unit study from 1999, respiratory tract organisms of patients with suspected aspiration mirrored those of patients with CAP or HAP.9 In a systematic review of eight observational studies that included studies from 1993 to 2014 and involved elderly patients with uncomplicated AP, only two out of eight studies demonstrated the presence of anaerobes in respiratory cultures. Even in those two studies, anaerobic bacteria frequently coexisted with aerobes. The majority of organisms in all eight studies consisted of aerobic gram-positives, gram-negatives, or both.10
A study by El-Solh et al most frequently isolated pathogenic aerobic gram-negative bacteria (49% of cases), followed by anaerobic bacteria (16%), among institutionalized elderly patients with severe AP diagnosed by clinical features. In that same study, most anaerobes coexisted with aerobic gram-negative bacteria, and the clinical illness promptly resolved in the absence of specific anaerobic coverage.11 AP can be successfully treated without anaerobic coverage due to a variety of factors: the insignificant role of anaerobes in the pathogenesis of uncomplicated AP, lower severity of illness in the absence of abscesses or pulmonary necrosis (uncomplicated), and altered local redox-potential from the elimination of aerobic pathogens, which effectively also treats anaerobes.1 Moreover, anaerobes possess generally less virulence in comparison with aerobes. AP from these organisms typically requires risk for excessive oral growth (eg, periodontal disease) and macroaspiration of a large number of organisms.5
There are also potential harms associated with the unnecessary treatment of anaerobic bacteria. Since anaerobes account for the majority of the bacteria present in the bowel, targeting anaerobes can result in gut dysbiosis.1 Moreover, a prospective study showed an increase in the incidence of vancomycin-resistant enterococci and antibiotic-resistant gram-negative bacteria associated with the empiric use of antibiotics with anaerobic activity.12 Finally, a systematic review detailed the high incidence of Clostridioides difficile infections among patients receiving clindamycin and carbapenems.13
WHEN ANAEROBIC COVERAGE IS INDICATED
Despite the predominance of aerobic organisms in the respiratory tract specimens of patients diagnosed with AP in the current era, situations still exist that require treatment of anaerobes. These include necrotizing pneumonia, empyema, or lung abscess.2 Additionally, patients with severe periodontal disease may harbor anaerobic bacteria such as Bacteroides species, Peptostreptococcus species, and Actinomyces israelii.5 When we suspect macroaspiration leading to AP, patients with severe periodontal disease may benefit from anaerobic coverage. Putrid sputum generation may indicate the presence of anaerobic organisms that produce the characteristic foul odor of short-chain volatile fatty acids observed in patients with lung abscess or empyema.2 It often takes about 8 to 14 days after an aspiration event for lung cavitation or empyema to develop.14 Therefore, a longer duration of illness or putrid sputum production may signal a significant concurrent burden of anaerobes. The 2019 official guidelines of the American Thoracic Society and Infectious Disease Society of America recommend adding anaerobic coverage to CAP only when empyema or lung abscess is suspected (conditional recommendation, very low quality of evidence).15
WHAT YOU SHOULD DO INSTEAD
When you suspect AP in a patient, categorize it as either community or hospital acquired based on risk factors similar to CAP or HAP. For patients with witnessed macroaspiration or in patients with substantial macroaspiration risk factors, perform a radiologic evaluation and a thorough oral examination to evaluate for poor dentition, gingival disease (marked redness, tendency to bleed, ulceration), and tongue coating. For patients presenting from the community with suspected AP without complications, treat with the standard therapy (without additional anaerobic coverage) for CAP. Provide empiric anaerobic coverage for complicated AP (eg, lung abscess, necrosis, or empyema) or for macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness. Similarly, treat hospital-acquired AP as HAP (Figure).
When prescribing anaerobic coverage of AP, use combination drugs that include a ß-lactamase inhibitor (eg, ampicillin-sulbactam), clindamycin (either alone or in combination with ß-lactams), or moxifloxacin.1 Most anaerobes have ß-lactamase or cephalosporinase activity, which renders penicillin and cephalosporins ineffective. Despite its potential side effects, such as C difficile infection, treating with clindamycin has the benefit of a relatively low cost and its association with lower rates of methicillin-resistant Staphylococcus aureus emergence after treatment.16 Piperacillin-tazobactam and carbapenems also have excellent anaerobic coverage, but we should reserve them for more severe and complicated cases of AP given their extensive antibacterial activity and concern for the emergence of resistance.8 Although well known and used for decades for its activity against clinically important anaerobes, avoid metronidazole due to its reduced cure rate in lung abscess caused by microaerophilic streptococci of the oral cavity.17 Due to a lack of evidence, we do not recommend the use of metronidazole in lung infections.
RECOMMENDATIONS
- Empirically treat most suspected cases of AP with regimens similar to the standard antibiotics for CAP and HAP. In the absence of specific risk factors for anaerobic infections, do not routinely provide anaerobic coverage.
- Provide anaerobic coverage empirically for AP associated with macroaspiration in the setting of severe periodontal disease, putrid sputum, or longer duration of illness.
- Provide anaerobic coverage in AP with evidence of necrotizing pneumonia, empyema, or lung abscess.
CONCLUSION
Current evidence does not support routine anaerobic coverage of AP in the absence of identifiable risk factors for an anaerobic lung infection.
In consideration of the clinical case, importantly, she has no periodontal disease and no evidence for necrotizing pneumonia, empyema, or lung abscess radiographically. For these reasons, select an empiric antibiotic regime that targets CAP organisms predominantly and forgo additional anaerobic coverage.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason ™ ”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason ™ ” topics by emailing [email protected].
Disclosures
The authors have no conflicts of interest relevant to this article.
1. Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019;380(7):651-663. https://doi.org/10.1056/nejmra1714562
2. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665-671. https://doi.org/10.1056/nejm200103013440908
3. Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med. 1974;56(2):202-207. https://doi.org/10.1016/0002-9343(74)90598-1
4. Bartlett JG, Gorbach SL. The triple threat of aspiration pneumonia. Chest. 1975;68(4):560-566. https://doi.org/10.1378/chest.68.4.560
5. Sutter VL. Anaerobes as normal oral flora. Rev Infect Dis. 1984;6(suppl 1):S62-S66. https://doi.org/10.1093/clinids/6.supplement_1.s62
6. Kioka MJ, DiGiovine B, Rezik M, Jennings JH. Anaerobic antibiotic usage for pneumonia in the medical intensive care unit. Respirology. 2017;22(8):1656-1661. https://doi.org/10.1111/resp.13111
7. Ott SR, Allewelt M, Lorenz J, Reimnitz P, Lode H; German Lung Abscess Study Group. Moxifloxacin vs ampicillin/sulbactam in aspiration pneumonia and primary lung abscess. Infection. 2008;36(1):23-30. https://doi.org/10.1007/s15010-007-7043-6
8. Tokuyasu H, Harada T, Watanabe E, et al. Effectiveness of meropenem for the treatment of aspiration pneumonia in elderly patients. Intern Med. 2009;48(3):129-135. https://doi.org/10.2169/internalmedicine.48.1308
9. Marik PE, Careau P. The role of anaerobes in patients with ventilator-associated pneumonia and aspiration pneumonia: a prospective study. Chest. 1999;115(1):178-183. https://doi.org/10.1378/chest.115.1.178
10. Bowerman TJ, Zhang J, Waite LM. Antibacterial treatment of aspiration pneumonia in older people: a systematic review. Clin Interv Aging. 2018;13:2201-2213. https://doi.org/10.2147/cia.s183344
11. El-Solh AA, Pietrantoni C, Bhat A, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003;167(12):1650-1654. https://doi.org/10.1164/rccm.200212-1543oc
12. Bhalla A, Pultz NJ, Ray AJ, Hoyen CK, Eckstein EC, Donskey CJ. Antianaerobic antibiotic therapy promotes overgrowth of antibiotic-resistant, gram-negative bacilli and vancomycin-resistant enterococci in the stool of colonized patients. Infect Control Hosp Epidemiol. 2003;24(9):644-649. https://doi.org/10.1086/502267
13. Vardakas KZ, Trigkidis KK, Boukouvala E, Falagas ME. Clostridium difficile infection following systemic antibiotic administration in randomised controlled trials: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;48(1):1-10. https://doi.org/10.1016/j.ijantimicag.2016.03.008
14. Leatherman JW, Iber C, F Davies SF. Cavitation in bacteremic pneumococcal pneumonia. Causal role of mixed infection with anaerobic bacteria. Am Rev Respir Dis. 1984;129(2):317-321.
15. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581st
16. Kadowaki M, Demura Y, Mizuno S, et al. Reappraisal of clindamycin IV monotherapy for treatment of mild-to-moderate aspiration pneumonia in elderly patients. Chest. 2005;127(4):1276-1282. https://doi.org/10.1378/chest.127.4.1276
17. Perlino CA. Metronidazole vs clindamycin treatment of anaerobic pulmonary infection. Failure of metronidazole therapy. Arch Intern Med. 1981;141(11):1424-1427.
1. Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019;380(7):651-663. https://doi.org/10.1056/nejmra1714562
2. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665-671. https://doi.org/10.1056/nejm200103013440908
3. Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med. 1974;56(2):202-207. https://doi.org/10.1016/0002-9343(74)90598-1
4. Bartlett JG, Gorbach SL. The triple threat of aspiration pneumonia. Chest. 1975;68(4):560-566. https://doi.org/10.1378/chest.68.4.560
5. Sutter VL. Anaerobes as normal oral flora. Rev Infect Dis. 1984;6(suppl 1):S62-S66. https://doi.org/10.1093/clinids/6.supplement_1.s62
6. Kioka MJ, DiGiovine B, Rezik M, Jennings JH. Anaerobic antibiotic usage for pneumonia in the medical intensive care unit. Respirology. 2017;22(8):1656-1661. https://doi.org/10.1111/resp.13111
7. Ott SR, Allewelt M, Lorenz J, Reimnitz P, Lode H; German Lung Abscess Study Group. Moxifloxacin vs ampicillin/sulbactam in aspiration pneumonia and primary lung abscess. Infection. 2008;36(1):23-30. https://doi.org/10.1007/s15010-007-7043-6
8. Tokuyasu H, Harada T, Watanabe E, et al. Effectiveness of meropenem for the treatment of aspiration pneumonia in elderly patients. Intern Med. 2009;48(3):129-135. https://doi.org/10.2169/internalmedicine.48.1308
9. Marik PE, Careau P. The role of anaerobes in patients with ventilator-associated pneumonia and aspiration pneumonia: a prospective study. Chest. 1999;115(1):178-183. https://doi.org/10.1378/chest.115.1.178
10. Bowerman TJ, Zhang J, Waite LM. Antibacterial treatment of aspiration pneumonia in older people: a systematic review. Clin Interv Aging. 2018;13:2201-2213. https://doi.org/10.2147/cia.s183344
11. El-Solh AA, Pietrantoni C, Bhat A, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003;167(12):1650-1654. https://doi.org/10.1164/rccm.200212-1543oc
12. Bhalla A, Pultz NJ, Ray AJ, Hoyen CK, Eckstein EC, Donskey CJ. Antianaerobic antibiotic therapy promotes overgrowth of antibiotic-resistant, gram-negative bacilli and vancomycin-resistant enterococci in the stool of colonized patients. Infect Control Hosp Epidemiol. 2003;24(9):644-649. https://doi.org/10.1086/502267
13. Vardakas KZ, Trigkidis KK, Boukouvala E, Falagas ME. Clostridium difficile infection following systemic antibiotic administration in randomised controlled trials: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;48(1):1-10. https://doi.org/10.1016/j.ijantimicag.2016.03.008
14. Leatherman JW, Iber C, F Davies SF. Cavitation in bacteremic pneumococcal pneumonia. Causal role of mixed infection with anaerobic bacteria. Am Rev Respir Dis. 1984;129(2):317-321.
15. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. https://doi.org/10.1164/rccm.201908-1581st
16. Kadowaki M, Demura Y, Mizuno S, et al. Reappraisal of clindamycin IV monotherapy for treatment of mild-to-moderate aspiration pneumonia in elderly patients. Chest. 2005;127(4):1276-1282. https://doi.org/10.1378/chest.127.4.1276
17. Perlino CA. Metronidazole vs clindamycin treatment of anaerobic pulmonary infection. Failure of metronidazole therapy. Arch Intern Med. 1981;141(11):1424-1427.
© 2020 Society of Hospital Medicine
Things We Do For No Reason™: Treatment of Infection-Related Fever in Hospitalized Patients
CLINICAL SCENARIO
The hospitalist admitted a 56-year-old man with hypertension and hyperlipidemia to the general medical unit for community-acquired pneumonia and started him on appropriate antimicrobial therapy. On the evening of admission, the nurse woke the patient to take his vital signs and noted a fever of 39.1°C (102.4°F). The patient had a pulse of 90 beats per minute, normal blood pressure, and a stable supplemental oxygen requirement via nasal cannula. The nurse noted an oral acetaminophen “as needed” order for fever. She woke the patient again to administer acetaminophen and notified the hospitalist.
BACKGROUND
Hospitalists frequently encounter febrile patients. According to one large hospital survey, fever occurs in 25% of pediatric and 31% of adult medical patients.1 Fever in hospitalized patients most commonly results from infection, but autoimmune disease, malignancy, and an array of other inflammatory conditions cause fevers as well.1
Defined as an elevated body temperature resulting from a raised hypothalamic set point2, hospitalists often treat fever with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). These routinely administered medications act centrally to temporarily lower the hypothalamic set point and relieve fever.2,3 Standard hospital admission order sets commonly include an as-needed antipyretic every 4 to 6 hours for treatment of fever, regardless of the presence of fever-related symptoms.
Fever is differentiated from hyperthermia, where temperature increases because of dysregulated peripheral processes despite a normal hypothalamic set point.2 Examples of hyperthermia include heat stroke, malignant hyperthermia, and neuroleptic malignant syndrome. Notably, antipyretic medications have no effect on hyperthermia, but physical means, such as cooling blankets, can lead to temperature reduction.2
WHY YOU MIGHT THINK TREATMENT OF INFECTION-RELATED FEVER IS HELPFUL IN HOSPITALIZED PATIENTS
Hospitalists prescribe antipyretic medication to alleviate fever-related symptoms, including headache, chills and sweats, and joint and muscle aches.3 While researchers have sparingly studied this practice, available evidence and experience suggest that fever-related symptoms decline in parallel with defervescence after administration of acetaminophen or NSAIDs in both adult and pediatric populations.4,5 One randomized, controlled, double-blind study of nearly 400 adult outpatients in Germany with febrile upper respiratory tract infections showed that both aspirin and acetaminophen bested the placebo in reducing fever and associated headache, achiness, and discomfort over a span of 6 hours.4 In another study, this time with pediatric patients hospitalized with fever and uncomplicated respiratory tract infections, patients who received acetaminophen had statistically significant improvements in activity, alertness, mood, comfort, appetite, and fluid intake 6 hours after receiving that therapy.5
Physicians, nurses, and caregivers also commonly believe that fever is inherently noxious and that treatment of infection-related fever contributes to fighting the infection itself.2,3,6 The pediatric literature describes parents, caretakers, and clinicians who suffer from “fever phobia,” the worry that fevers contribute to long-term neurologic complications, recurrent febrile seizures, and death.6,7
Finally, healthcare providers administer antipyretic medication to mitigate the demand fever places on the cardiovascular and pulmonary systems.3 An elevated temperature increases the body’s metabolic rate, oxygen consumption, and cardiac output that critically ill patients who have acute and/or chronic compromise to those systems may not tolerate. For example, patients requiring pressor support for hemodynamic shock or mechanical ventilation for respiratory failure may not tolerate an elevated temperature.8
WHY THERE IS NO REASON TO TREAT INFECTION-RELATED FEVER IN ASYMPTOMATIC HOSPITALIZED PATIENTS
Fever serves as an adaptive host response to infection, boosting innate and adaptive immunity in a multitude of ways.8 In animal models, fever slows the replication of pathogenic bacteria and enhances the activity of antibiotic agents.8 In vitro studies demonstrate that fever increases mobility of leukocytes, phagocytic activity, and proliferation of T cells.8 Retrospective case-control studies of patients hospitalized with severe bacterial illnesses, including gram-negative bacteremia, spontaneous bacterial peritonitis, and community-acquired pneumonia, found that patients with a documented febrile response had increased survival compared with those who remained afebrile during the infection.9 In addition, a large retrospective cohort study of septic ICU patients found a progressive decline in mortality in association with increasing peak temperature on the day of ICU admission.10
In addition to the above studies supporting the important role of fever in fighting infection, recent evidence definitively demonstrates no mortality or morbidity benefit of using antipyretic medications in infected patients. A 2017 meta-analysis that included eight observational and eight randomized studies, totaling 18,939 adult septic ICU patients, demonstrated no difference in hospital and 28-day mortality in patients treated with antipyretics vs those who were not.11 The authors again found no mortality benefit with antipyretic use when separately analyzing data from only the randomized controlled trials (1,507 patients) or when stratifying patients based on the type of antipyretic received (acetaminophen, NSAIDs, or physical cooling).11 They reported no differences in predefined secondary outcomes of shock reversal or nosocomial infections. The authors commented that these robust results likely would not change even with more data from additional trials. In children, a recent meta-analysis of three randomized controlled trials (540 patients) did not find the use of acetaminophen, ibuprofen, or diclofenac effective in preventing febrile seizures.12Pediatric practice guidelines consistently recommend using antipyretic medication to alleviate discomfort caused by fever and not solely to reduce temperature.13,14
Antipyretic agents interfere with the effectiveness of the body’s immune response, as demonstrated in a number of infectious diseases.2,15-18 Two randomized controlled studies conducted in healthy adult volunteers challenged with rhinovirus reported increased viral shedding and decreased antibody response in those subjects who received aspirin or acetaminophen, compared with those given placebo.15,16 In another randomized controlled trial conducted in African children with malaria, paracetamol use delayed parasite clearance by 16 hours.17 A large case-control study correlated the use of NSAIDs with an increased risk of severe skin and soft-tissue complications in children with varicella and in adults with varicella zoster. 18 The international scientific community has raised concerns about worse outcomes with NSAID use in patients with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); NSAIDs should be avoided in stable patients with COVID-19 until more data are available. 19
Additional risks and potential harms accompany antipyretic fever therapy. First, NSAIDs or acetaminophen may adversely affect patients with renal or hepatic insufficiency.2,3 Second, masking fevers may impair the clinician’s ability to diagnose or evaluate response to treatment. Third, unnecessarily waking a sleeping patient to check temperature or administer unneeded antipyretics can contribute to hospital-associated problems, including delirium, insomnia, and falls. Treating these iatrogenic problems in turn may require additional medications or interventions. These unintended consequences may potentially prolong hospital stays, increase medication errors and polypharmacy, and detract from a patient’s overall healing and recovery.
While the use of antipyretic medications improves fever-related symptoms, it comes at the cost of blunting a protective host response and exposes patients to medication risks without providing a clinical benefit. In sleeping, asymptomatic, or minimally symptomatic hospitalized patients, the risks of administering antipyretic medications clearly outweigh the benefits.
WHEN TREATING FEVER IS INDICATED
Treatment with antipyretic medication can alleviate fever-related symptoms in those patients who have significant headache, body aches, chills, or sweats and in pediatric patients with notable malaise, irritability, or poor oral intake. Debate continues on the use of antipyretics in the ICU setting when managing critically ill patients with severe cardiopulmonary compromise who may not tolerate the additional hemodynamic strain a fever produces (eg, patients with shock requiring vasopressor support or respiratory failure requiring mechanical ventilation). Remember, decrease body temperature in hyperthermia syndromes by physical means.
WHAT WE SHOULD DO INSTEAD
Withhold antipyretic medication (ie, allow permissive fever) in well-appearing general medical patients with asymptomatic infection-related fevers. In patients who tolerate fever with minimal or no symptoms, potential benefits of permissive fever include decreased time to infection resolution and/or decreased risk of hospital-acquired infections. This may result in shorter hospital stays and significant cost savings. If we do not treat patients with asymptomatic fevers, then it follows that we should not check overnight temperatures in hospitalized patients sleeping comfortably.
RECOMMENDATIONS
- Do not order as-needed antipyretic medication for stable patients on general medical units with infection solely to reduce temperature or achieve normothermia.
- Only treat infected febrile patients with antipyretic medications for fever-related symptoms (headache, chills, or body aches or, in pediatric patients, irritability, malaise, or poor oral intake).
- Treat pathologically elevated temperatures (ie, hyperthermia syndromes) with physical measures because antipyretic medications will be ineffective.
CONCLUSIONS
In the clinical scenario, the hospitalist admitted the patient in stable condition for treatment of a community-acquired pneumonia. He mounted a febrile response to infection, which suggests that his active immune system may aid in recovery. The nurse noted the fever while the patient slept comfortably without fever-related symptoms.
After discussing these facts with the patient’s concerned nurse, the clinician should discontinue the order for as-needed acetaminophen for fever and instead recommend permissive fever without administration of antipyretic medication. This may facilitate recovery, avoid unnecessary polypharmacy, and allow the medical care team to follow his fever curve to ensure that the infection is adequately treated. If the patient develops bothersome fever-related symptoms, the hospitalist can reasonably treat with a single-dose of acetaminophen or NSAID.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
1. McGowan JE Jr, Rose RC, Jacobs NF, Schaberg DR, Haley RW. Fever in hospitalized patients, with special reference to the medical service. Am J Med. 1987;82(3):580-586. https://doi.org/10.1016/0002-9343(87)90103-3.
2. Plaisance K, Mackowiak P. Antipyretic therapy. Arch Intern Med. 2000;160:449-456. https://doi.org/10.1001/archinte.160.4.449.
3. Greisman LA, Mackowiak PA. Fever: beneficial and detrimental effects of antipyretics. Curr Opin Infect Dis. 2002;15:241-245. https://doi.org/10.1097/00001432-200206000-00005.
4. Bachert C, Chuchalin AG, Eisebitt R, Netayzhenko VZ, Voelker M. Aspirin compared with acetaminophen in the treatment of fever and other symptoms of upper respiratory tract infection in adults: a multicenter, randomized, double-blind, double-dummy, placebo-controlled, parallel-group, single-dose, 6-hour dose-ranging study. Clin Ther. 2005;27(7):993-1003. https://doi.org/10.1016/j.clinthera.2005.06.002.
5. Gupta H, Shah D, Gupta P, Sharma KK. Role of paracetamol in treatment of childhood fever: a double-blind randomized placebo controlled trial. Indian Pediatr. 2007;44:903-911.
6. Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. 1980;134(2):176-181.
7. Karwowska A, Nijssen-Jordan C, Johnson D, Davies HD. Parental and health care provider understanding of childhood fever: a Canadian perspective. CJEM. 2002;4(6):394-400. https://doi.org/10.1017/s1481803500007892.
8. Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI. Fever effects and treatment in critical care: literature review. Aust Crit Care. 2013;26:130-135. https://doi.org/10.1016/j.aucc.2012.10.004.
9. Hasday JD, Fairchild KD, Shanholtz C. The role of fever in the infected host. Microbes Infect. 2000;2(15):1891-1894. https://doi.org/10.1016/s1286-4579(00)01337-x.
10. Young PJ, Saxena M, Beasley R, et al. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med. 2012;38:437-444. https://doi.org/10.1007/s00134-012-2478-3.
11. Drewry A, Ablordeppey E, Murray E, et al. Antipyretic therapy in critically ill septic patients: a systematic review and meta-analysis. Crit Care Med. 2017;45(5):806-813. https://doi.org/10.1097/CCM.0000000000002285.
12. Rosenbloom E, Finkelstein Y, Adams-Webber T, Kozer E. Do antipyretics prevent the recurrence of febrile seizures in children? a systematic review of randomized controlled trials and meta-analysis. Eur J Paediatr Neuro. 2013;17:585-588. https://doi.org/10.1016/j.ejpn.2013.04.008.
13. Chiappini J, Venturini E, Remaschi G. 2016 Update of the Italian Pediatric Society Guidelines for management of fever in children. J Pediatr. 2017;180:177-183. https://doi.org/10.1016/j.jpeds.2016.09.043.
14. Fields E, Chard J, Murphy MS, Richardson M, Guideline Development Group and Technical Team. Assessment and initial management of feverish illness in children younger than five years: summary of updated NICE guidance. BMJ. 2013;346:f2866. https://doi.org/10.1136/bmj.f2866.
15. Stanley ED, Jackson GG, Panusarn C, Rubenis M, Dirda V. Increased viral shedding with aspirin treatment of rhinovirus infection. JAMA. 1975;231:1248-1251. https://doi.org/10.1001/jama.1975.03240240018017.
16. Graham NM, Burrell CJ, Douglas RM, Debelle P, Davies L. Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. J Infect Dis. 1990;162:1277-1282. https://doi.org/10.1093/infdis/162.6.1277.
17. Brandts CH, Ndjave M, Graninger W, Kremsner PG. Effect of paracetamol on parasite clearance time in Plasmodium falciparum malaria. Lancet. 1997;350:704-709. https://doi.org/10.1016/S0140-6736(97)02255-1.
18. Mikaeloff Y, Kezouh A, Suissa S. Nonsteroidal anti-inflammatory drug use and the risk of severe skin and soft tissue complications in patients with varicella or zoster disease. Br J Clin Pharmacol. 2007;65:2:203-209. https://doi.org/10.1016/S0140-6736(97)02255-1.
19. Day M. COVID-19: ibuprofen should not be used for managing symptoms, say doctors and scientists. BMJ. 2020;368:m1086. https://doi.org/10.1136/bmj.m1086.
CLINICAL SCENARIO
The hospitalist admitted a 56-year-old man with hypertension and hyperlipidemia to the general medical unit for community-acquired pneumonia and started him on appropriate antimicrobial therapy. On the evening of admission, the nurse woke the patient to take his vital signs and noted a fever of 39.1°C (102.4°F). The patient had a pulse of 90 beats per minute, normal blood pressure, and a stable supplemental oxygen requirement via nasal cannula. The nurse noted an oral acetaminophen “as needed” order for fever. She woke the patient again to administer acetaminophen and notified the hospitalist.
BACKGROUND
Hospitalists frequently encounter febrile patients. According to one large hospital survey, fever occurs in 25% of pediatric and 31% of adult medical patients.1 Fever in hospitalized patients most commonly results from infection, but autoimmune disease, malignancy, and an array of other inflammatory conditions cause fevers as well.1
Defined as an elevated body temperature resulting from a raised hypothalamic set point2, hospitalists often treat fever with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). These routinely administered medications act centrally to temporarily lower the hypothalamic set point and relieve fever.2,3 Standard hospital admission order sets commonly include an as-needed antipyretic every 4 to 6 hours for treatment of fever, regardless of the presence of fever-related symptoms.
Fever is differentiated from hyperthermia, where temperature increases because of dysregulated peripheral processes despite a normal hypothalamic set point.2 Examples of hyperthermia include heat stroke, malignant hyperthermia, and neuroleptic malignant syndrome. Notably, antipyretic medications have no effect on hyperthermia, but physical means, such as cooling blankets, can lead to temperature reduction.2
WHY YOU MIGHT THINK TREATMENT OF INFECTION-RELATED FEVER IS HELPFUL IN HOSPITALIZED PATIENTS
Hospitalists prescribe antipyretic medication to alleviate fever-related symptoms, including headache, chills and sweats, and joint and muscle aches.3 While researchers have sparingly studied this practice, available evidence and experience suggest that fever-related symptoms decline in parallel with defervescence after administration of acetaminophen or NSAIDs in both adult and pediatric populations.4,5 One randomized, controlled, double-blind study of nearly 400 adult outpatients in Germany with febrile upper respiratory tract infections showed that both aspirin and acetaminophen bested the placebo in reducing fever and associated headache, achiness, and discomfort over a span of 6 hours.4 In another study, this time with pediatric patients hospitalized with fever and uncomplicated respiratory tract infections, patients who received acetaminophen had statistically significant improvements in activity, alertness, mood, comfort, appetite, and fluid intake 6 hours after receiving that therapy.5
Physicians, nurses, and caregivers also commonly believe that fever is inherently noxious and that treatment of infection-related fever contributes to fighting the infection itself.2,3,6 The pediatric literature describes parents, caretakers, and clinicians who suffer from “fever phobia,” the worry that fevers contribute to long-term neurologic complications, recurrent febrile seizures, and death.6,7
Finally, healthcare providers administer antipyretic medication to mitigate the demand fever places on the cardiovascular and pulmonary systems.3 An elevated temperature increases the body’s metabolic rate, oxygen consumption, and cardiac output that critically ill patients who have acute and/or chronic compromise to those systems may not tolerate. For example, patients requiring pressor support for hemodynamic shock or mechanical ventilation for respiratory failure may not tolerate an elevated temperature.8
WHY THERE IS NO REASON TO TREAT INFECTION-RELATED FEVER IN ASYMPTOMATIC HOSPITALIZED PATIENTS
Fever serves as an adaptive host response to infection, boosting innate and adaptive immunity in a multitude of ways.8 In animal models, fever slows the replication of pathogenic bacteria and enhances the activity of antibiotic agents.8 In vitro studies demonstrate that fever increases mobility of leukocytes, phagocytic activity, and proliferation of T cells.8 Retrospective case-control studies of patients hospitalized with severe bacterial illnesses, including gram-negative bacteremia, spontaneous bacterial peritonitis, and community-acquired pneumonia, found that patients with a documented febrile response had increased survival compared with those who remained afebrile during the infection.9 In addition, a large retrospective cohort study of septic ICU patients found a progressive decline in mortality in association with increasing peak temperature on the day of ICU admission.10
In addition to the above studies supporting the important role of fever in fighting infection, recent evidence definitively demonstrates no mortality or morbidity benefit of using antipyretic medications in infected patients. A 2017 meta-analysis that included eight observational and eight randomized studies, totaling 18,939 adult septic ICU patients, demonstrated no difference in hospital and 28-day mortality in patients treated with antipyretics vs those who were not.11 The authors again found no mortality benefit with antipyretic use when separately analyzing data from only the randomized controlled trials (1,507 patients) or when stratifying patients based on the type of antipyretic received (acetaminophen, NSAIDs, or physical cooling).11 They reported no differences in predefined secondary outcomes of shock reversal or nosocomial infections. The authors commented that these robust results likely would not change even with more data from additional trials. In children, a recent meta-analysis of three randomized controlled trials (540 patients) did not find the use of acetaminophen, ibuprofen, or diclofenac effective in preventing febrile seizures.12Pediatric practice guidelines consistently recommend using antipyretic medication to alleviate discomfort caused by fever and not solely to reduce temperature.13,14
Antipyretic agents interfere with the effectiveness of the body’s immune response, as demonstrated in a number of infectious diseases.2,15-18 Two randomized controlled studies conducted in healthy adult volunteers challenged with rhinovirus reported increased viral shedding and decreased antibody response in those subjects who received aspirin or acetaminophen, compared with those given placebo.15,16 In another randomized controlled trial conducted in African children with malaria, paracetamol use delayed parasite clearance by 16 hours.17 A large case-control study correlated the use of NSAIDs with an increased risk of severe skin and soft-tissue complications in children with varicella and in adults with varicella zoster. 18 The international scientific community has raised concerns about worse outcomes with NSAID use in patients with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); NSAIDs should be avoided in stable patients with COVID-19 until more data are available. 19
Additional risks and potential harms accompany antipyretic fever therapy. First, NSAIDs or acetaminophen may adversely affect patients with renal or hepatic insufficiency.2,3 Second, masking fevers may impair the clinician’s ability to diagnose or evaluate response to treatment. Third, unnecessarily waking a sleeping patient to check temperature or administer unneeded antipyretics can contribute to hospital-associated problems, including delirium, insomnia, and falls. Treating these iatrogenic problems in turn may require additional medications or interventions. These unintended consequences may potentially prolong hospital stays, increase medication errors and polypharmacy, and detract from a patient’s overall healing and recovery.
While the use of antipyretic medications improves fever-related symptoms, it comes at the cost of blunting a protective host response and exposes patients to medication risks without providing a clinical benefit. In sleeping, asymptomatic, or minimally symptomatic hospitalized patients, the risks of administering antipyretic medications clearly outweigh the benefits.
WHEN TREATING FEVER IS INDICATED
Treatment with antipyretic medication can alleviate fever-related symptoms in those patients who have significant headache, body aches, chills, or sweats and in pediatric patients with notable malaise, irritability, or poor oral intake. Debate continues on the use of antipyretics in the ICU setting when managing critically ill patients with severe cardiopulmonary compromise who may not tolerate the additional hemodynamic strain a fever produces (eg, patients with shock requiring vasopressor support or respiratory failure requiring mechanical ventilation). Remember, decrease body temperature in hyperthermia syndromes by physical means.
WHAT WE SHOULD DO INSTEAD
Withhold antipyretic medication (ie, allow permissive fever) in well-appearing general medical patients with asymptomatic infection-related fevers. In patients who tolerate fever with minimal or no symptoms, potential benefits of permissive fever include decreased time to infection resolution and/or decreased risk of hospital-acquired infections. This may result in shorter hospital stays and significant cost savings. If we do not treat patients with asymptomatic fevers, then it follows that we should not check overnight temperatures in hospitalized patients sleeping comfortably.
RECOMMENDATIONS
- Do not order as-needed antipyretic medication for stable patients on general medical units with infection solely to reduce temperature or achieve normothermia.
- Only treat infected febrile patients with antipyretic medications for fever-related symptoms (headache, chills, or body aches or, in pediatric patients, irritability, malaise, or poor oral intake).
- Treat pathologically elevated temperatures (ie, hyperthermia syndromes) with physical measures because antipyretic medications will be ineffective.
CONCLUSIONS
In the clinical scenario, the hospitalist admitted the patient in stable condition for treatment of a community-acquired pneumonia. He mounted a febrile response to infection, which suggests that his active immune system may aid in recovery. The nurse noted the fever while the patient slept comfortably without fever-related symptoms.
After discussing these facts with the patient’s concerned nurse, the clinician should discontinue the order for as-needed acetaminophen for fever and instead recommend permissive fever without administration of antipyretic medication. This may facilitate recovery, avoid unnecessary polypharmacy, and allow the medical care team to follow his fever curve to ensure that the infection is adequately treated. If the patient develops bothersome fever-related symptoms, the hospitalist can reasonably treat with a single-dose of acetaminophen or NSAID.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
CLINICAL SCENARIO
The hospitalist admitted a 56-year-old man with hypertension and hyperlipidemia to the general medical unit for community-acquired pneumonia and started him on appropriate antimicrobial therapy. On the evening of admission, the nurse woke the patient to take his vital signs and noted a fever of 39.1°C (102.4°F). The patient had a pulse of 90 beats per minute, normal blood pressure, and a stable supplemental oxygen requirement via nasal cannula. The nurse noted an oral acetaminophen “as needed” order for fever. She woke the patient again to administer acetaminophen and notified the hospitalist.
BACKGROUND
Hospitalists frequently encounter febrile patients. According to one large hospital survey, fever occurs in 25% of pediatric and 31% of adult medical patients.1 Fever in hospitalized patients most commonly results from infection, but autoimmune disease, malignancy, and an array of other inflammatory conditions cause fevers as well.1
Defined as an elevated body temperature resulting from a raised hypothalamic set point2, hospitalists often treat fever with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). These routinely administered medications act centrally to temporarily lower the hypothalamic set point and relieve fever.2,3 Standard hospital admission order sets commonly include an as-needed antipyretic every 4 to 6 hours for treatment of fever, regardless of the presence of fever-related symptoms.
Fever is differentiated from hyperthermia, where temperature increases because of dysregulated peripheral processes despite a normal hypothalamic set point.2 Examples of hyperthermia include heat stroke, malignant hyperthermia, and neuroleptic malignant syndrome. Notably, antipyretic medications have no effect on hyperthermia, but physical means, such as cooling blankets, can lead to temperature reduction.2
WHY YOU MIGHT THINK TREATMENT OF INFECTION-RELATED FEVER IS HELPFUL IN HOSPITALIZED PATIENTS
Hospitalists prescribe antipyretic medication to alleviate fever-related symptoms, including headache, chills and sweats, and joint and muscle aches.3 While researchers have sparingly studied this practice, available evidence and experience suggest that fever-related symptoms decline in parallel with defervescence after administration of acetaminophen or NSAIDs in both adult and pediatric populations.4,5 One randomized, controlled, double-blind study of nearly 400 adult outpatients in Germany with febrile upper respiratory tract infections showed that both aspirin and acetaminophen bested the placebo in reducing fever and associated headache, achiness, and discomfort over a span of 6 hours.4 In another study, this time with pediatric patients hospitalized with fever and uncomplicated respiratory tract infections, patients who received acetaminophen had statistically significant improvements in activity, alertness, mood, comfort, appetite, and fluid intake 6 hours after receiving that therapy.5
Physicians, nurses, and caregivers also commonly believe that fever is inherently noxious and that treatment of infection-related fever contributes to fighting the infection itself.2,3,6 The pediatric literature describes parents, caretakers, and clinicians who suffer from “fever phobia,” the worry that fevers contribute to long-term neurologic complications, recurrent febrile seizures, and death.6,7
Finally, healthcare providers administer antipyretic medication to mitigate the demand fever places on the cardiovascular and pulmonary systems.3 An elevated temperature increases the body’s metabolic rate, oxygen consumption, and cardiac output that critically ill patients who have acute and/or chronic compromise to those systems may not tolerate. For example, patients requiring pressor support for hemodynamic shock or mechanical ventilation for respiratory failure may not tolerate an elevated temperature.8
WHY THERE IS NO REASON TO TREAT INFECTION-RELATED FEVER IN ASYMPTOMATIC HOSPITALIZED PATIENTS
Fever serves as an adaptive host response to infection, boosting innate and adaptive immunity in a multitude of ways.8 In animal models, fever slows the replication of pathogenic bacteria and enhances the activity of antibiotic agents.8 In vitro studies demonstrate that fever increases mobility of leukocytes, phagocytic activity, and proliferation of T cells.8 Retrospective case-control studies of patients hospitalized with severe bacterial illnesses, including gram-negative bacteremia, spontaneous bacterial peritonitis, and community-acquired pneumonia, found that patients with a documented febrile response had increased survival compared with those who remained afebrile during the infection.9 In addition, a large retrospective cohort study of septic ICU patients found a progressive decline in mortality in association with increasing peak temperature on the day of ICU admission.10
In addition to the above studies supporting the important role of fever in fighting infection, recent evidence definitively demonstrates no mortality or morbidity benefit of using antipyretic medications in infected patients. A 2017 meta-analysis that included eight observational and eight randomized studies, totaling 18,939 adult septic ICU patients, demonstrated no difference in hospital and 28-day mortality in patients treated with antipyretics vs those who were not.11 The authors again found no mortality benefit with antipyretic use when separately analyzing data from only the randomized controlled trials (1,507 patients) or when stratifying patients based on the type of antipyretic received (acetaminophen, NSAIDs, or physical cooling).11 They reported no differences in predefined secondary outcomes of shock reversal or nosocomial infections. The authors commented that these robust results likely would not change even with more data from additional trials. In children, a recent meta-analysis of three randomized controlled trials (540 patients) did not find the use of acetaminophen, ibuprofen, or diclofenac effective in preventing febrile seizures.12Pediatric practice guidelines consistently recommend using antipyretic medication to alleviate discomfort caused by fever and not solely to reduce temperature.13,14
Antipyretic agents interfere with the effectiveness of the body’s immune response, as demonstrated in a number of infectious diseases.2,15-18 Two randomized controlled studies conducted in healthy adult volunteers challenged with rhinovirus reported increased viral shedding and decreased antibody response in those subjects who received aspirin or acetaminophen, compared with those given placebo.15,16 In another randomized controlled trial conducted in African children with malaria, paracetamol use delayed parasite clearance by 16 hours.17 A large case-control study correlated the use of NSAIDs with an increased risk of severe skin and soft-tissue complications in children with varicella and in adults with varicella zoster. 18 The international scientific community has raised concerns about worse outcomes with NSAID use in patients with COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); NSAIDs should be avoided in stable patients with COVID-19 until more data are available. 19
Additional risks and potential harms accompany antipyretic fever therapy. First, NSAIDs or acetaminophen may adversely affect patients with renal or hepatic insufficiency.2,3 Second, masking fevers may impair the clinician’s ability to diagnose or evaluate response to treatment. Third, unnecessarily waking a sleeping patient to check temperature or administer unneeded antipyretics can contribute to hospital-associated problems, including delirium, insomnia, and falls. Treating these iatrogenic problems in turn may require additional medications or interventions. These unintended consequences may potentially prolong hospital stays, increase medication errors and polypharmacy, and detract from a patient’s overall healing and recovery.
While the use of antipyretic medications improves fever-related symptoms, it comes at the cost of blunting a protective host response and exposes patients to medication risks without providing a clinical benefit. In sleeping, asymptomatic, or minimally symptomatic hospitalized patients, the risks of administering antipyretic medications clearly outweigh the benefits.
WHEN TREATING FEVER IS INDICATED
Treatment with antipyretic medication can alleviate fever-related symptoms in those patients who have significant headache, body aches, chills, or sweats and in pediatric patients with notable malaise, irritability, or poor oral intake. Debate continues on the use of antipyretics in the ICU setting when managing critically ill patients with severe cardiopulmonary compromise who may not tolerate the additional hemodynamic strain a fever produces (eg, patients with shock requiring vasopressor support or respiratory failure requiring mechanical ventilation). Remember, decrease body temperature in hyperthermia syndromes by physical means.
WHAT WE SHOULD DO INSTEAD
Withhold antipyretic medication (ie, allow permissive fever) in well-appearing general medical patients with asymptomatic infection-related fevers. In patients who tolerate fever with minimal or no symptoms, potential benefits of permissive fever include decreased time to infection resolution and/or decreased risk of hospital-acquired infections. This may result in shorter hospital stays and significant cost savings. If we do not treat patients with asymptomatic fevers, then it follows that we should not check overnight temperatures in hospitalized patients sleeping comfortably.
RECOMMENDATIONS
- Do not order as-needed antipyretic medication for stable patients on general medical units with infection solely to reduce temperature or achieve normothermia.
- Only treat infected febrile patients with antipyretic medications for fever-related symptoms (headache, chills, or body aches or, in pediatric patients, irritability, malaise, or poor oral intake).
- Treat pathologically elevated temperatures (ie, hyperthermia syndromes) with physical measures because antipyretic medications will be ineffective.
CONCLUSIONS
In the clinical scenario, the hospitalist admitted the patient in stable condition for treatment of a community-acquired pneumonia. He mounted a febrile response to infection, which suggests that his active immune system may aid in recovery. The nurse noted the fever while the patient slept comfortably without fever-related symptoms.
After discussing these facts with the patient’s concerned nurse, the clinician should discontinue the order for as-needed acetaminophen for fever and instead recommend permissive fever without administration of antipyretic medication. This may facilitate recovery, avoid unnecessary polypharmacy, and allow the medical care team to follow his fever curve to ensure that the infection is adequately treated. If the patient develops bothersome fever-related symptoms, the hospitalist can reasonably treat with a single-dose of acetaminophen or NSAID.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
1. McGowan JE Jr, Rose RC, Jacobs NF, Schaberg DR, Haley RW. Fever in hospitalized patients, with special reference to the medical service. Am J Med. 1987;82(3):580-586. https://doi.org/10.1016/0002-9343(87)90103-3.
2. Plaisance K, Mackowiak P. Antipyretic therapy. Arch Intern Med. 2000;160:449-456. https://doi.org/10.1001/archinte.160.4.449.
3. Greisman LA, Mackowiak PA. Fever: beneficial and detrimental effects of antipyretics. Curr Opin Infect Dis. 2002;15:241-245. https://doi.org/10.1097/00001432-200206000-00005.
4. Bachert C, Chuchalin AG, Eisebitt R, Netayzhenko VZ, Voelker M. Aspirin compared with acetaminophen in the treatment of fever and other symptoms of upper respiratory tract infection in adults: a multicenter, randomized, double-blind, double-dummy, placebo-controlled, parallel-group, single-dose, 6-hour dose-ranging study. Clin Ther. 2005;27(7):993-1003. https://doi.org/10.1016/j.clinthera.2005.06.002.
5. Gupta H, Shah D, Gupta P, Sharma KK. Role of paracetamol in treatment of childhood fever: a double-blind randomized placebo controlled trial. Indian Pediatr. 2007;44:903-911.
6. Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. 1980;134(2):176-181.
7. Karwowska A, Nijssen-Jordan C, Johnson D, Davies HD. Parental and health care provider understanding of childhood fever: a Canadian perspective. CJEM. 2002;4(6):394-400. https://doi.org/10.1017/s1481803500007892.
8. Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI. Fever effects and treatment in critical care: literature review. Aust Crit Care. 2013;26:130-135. https://doi.org/10.1016/j.aucc.2012.10.004.
9. Hasday JD, Fairchild KD, Shanholtz C. The role of fever in the infected host. Microbes Infect. 2000;2(15):1891-1894. https://doi.org/10.1016/s1286-4579(00)01337-x.
10. Young PJ, Saxena M, Beasley R, et al. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med. 2012;38:437-444. https://doi.org/10.1007/s00134-012-2478-3.
11. Drewry A, Ablordeppey E, Murray E, et al. Antipyretic therapy in critically ill septic patients: a systematic review and meta-analysis. Crit Care Med. 2017;45(5):806-813. https://doi.org/10.1097/CCM.0000000000002285.
12. Rosenbloom E, Finkelstein Y, Adams-Webber T, Kozer E. Do antipyretics prevent the recurrence of febrile seizures in children? a systematic review of randomized controlled trials and meta-analysis. Eur J Paediatr Neuro. 2013;17:585-588. https://doi.org/10.1016/j.ejpn.2013.04.008.
13. Chiappini J, Venturini E, Remaschi G. 2016 Update of the Italian Pediatric Society Guidelines for management of fever in children. J Pediatr. 2017;180:177-183. https://doi.org/10.1016/j.jpeds.2016.09.043.
14. Fields E, Chard J, Murphy MS, Richardson M, Guideline Development Group and Technical Team. Assessment and initial management of feverish illness in children younger than five years: summary of updated NICE guidance. BMJ. 2013;346:f2866. https://doi.org/10.1136/bmj.f2866.
15. Stanley ED, Jackson GG, Panusarn C, Rubenis M, Dirda V. Increased viral shedding with aspirin treatment of rhinovirus infection. JAMA. 1975;231:1248-1251. https://doi.org/10.1001/jama.1975.03240240018017.
16. Graham NM, Burrell CJ, Douglas RM, Debelle P, Davies L. Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. J Infect Dis. 1990;162:1277-1282. https://doi.org/10.1093/infdis/162.6.1277.
17. Brandts CH, Ndjave M, Graninger W, Kremsner PG. Effect of paracetamol on parasite clearance time in Plasmodium falciparum malaria. Lancet. 1997;350:704-709. https://doi.org/10.1016/S0140-6736(97)02255-1.
18. Mikaeloff Y, Kezouh A, Suissa S. Nonsteroidal anti-inflammatory drug use and the risk of severe skin and soft tissue complications in patients with varicella or zoster disease. Br J Clin Pharmacol. 2007;65:2:203-209. https://doi.org/10.1016/S0140-6736(97)02255-1.
19. Day M. COVID-19: ibuprofen should not be used for managing symptoms, say doctors and scientists. BMJ. 2020;368:m1086. https://doi.org/10.1136/bmj.m1086.
1. McGowan JE Jr, Rose RC, Jacobs NF, Schaberg DR, Haley RW. Fever in hospitalized patients, with special reference to the medical service. Am J Med. 1987;82(3):580-586. https://doi.org/10.1016/0002-9343(87)90103-3.
2. Plaisance K, Mackowiak P. Antipyretic therapy. Arch Intern Med. 2000;160:449-456. https://doi.org/10.1001/archinte.160.4.449.
3. Greisman LA, Mackowiak PA. Fever: beneficial and detrimental effects of antipyretics. Curr Opin Infect Dis. 2002;15:241-245. https://doi.org/10.1097/00001432-200206000-00005.
4. Bachert C, Chuchalin AG, Eisebitt R, Netayzhenko VZ, Voelker M. Aspirin compared with acetaminophen in the treatment of fever and other symptoms of upper respiratory tract infection in adults: a multicenter, randomized, double-blind, double-dummy, placebo-controlled, parallel-group, single-dose, 6-hour dose-ranging study. Clin Ther. 2005;27(7):993-1003. https://doi.org/10.1016/j.clinthera.2005.06.002.
5. Gupta H, Shah D, Gupta P, Sharma KK. Role of paracetamol in treatment of childhood fever: a double-blind randomized placebo controlled trial. Indian Pediatr. 2007;44:903-911.
6. Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. 1980;134(2):176-181.
7. Karwowska A, Nijssen-Jordan C, Johnson D, Davies HD. Parental and health care provider understanding of childhood fever: a Canadian perspective. CJEM. 2002;4(6):394-400. https://doi.org/10.1017/s1481803500007892.
8. Kiekkas P, Aretha D, Bakalis N, Karpouhtsi I, Marneras C, Baltopoulos GI. Fever effects and treatment in critical care: literature review. Aust Crit Care. 2013;26:130-135. https://doi.org/10.1016/j.aucc.2012.10.004.
9. Hasday JD, Fairchild KD, Shanholtz C. The role of fever in the infected host. Microbes Infect. 2000;2(15):1891-1894. https://doi.org/10.1016/s1286-4579(00)01337-x.
10. Young PJ, Saxena M, Beasley R, et al. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med. 2012;38:437-444. https://doi.org/10.1007/s00134-012-2478-3.
11. Drewry A, Ablordeppey E, Murray E, et al. Antipyretic therapy in critically ill septic patients: a systematic review and meta-analysis. Crit Care Med. 2017;45(5):806-813. https://doi.org/10.1097/CCM.0000000000002285.
12. Rosenbloom E, Finkelstein Y, Adams-Webber T, Kozer E. Do antipyretics prevent the recurrence of febrile seizures in children? a systematic review of randomized controlled trials and meta-analysis. Eur J Paediatr Neuro. 2013;17:585-588. https://doi.org/10.1016/j.ejpn.2013.04.008.
13. Chiappini J, Venturini E, Remaschi G. 2016 Update of the Italian Pediatric Society Guidelines for management of fever in children. J Pediatr. 2017;180:177-183. https://doi.org/10.1016/j.jpeds.2016.09.043.
14. Fields E, Chard J, Murphy MS, Richardson M, Guideline Development Group and Technical Team. Assessment and initial management of feverish illness in children younger than five years: summary of updated NICE guidance. BMJ. 2013;346:f2866. https://doi.org/10.1136/bmj.f2866.
15. Stanley ED, Jackson GG, Panusarn C, Rubenis M, Dirda V. Increased viral shedding with aspirin treatment of rhinovirus infection. JAMA. 1975;231:1248-1251. https://doi.org/10.1001/jama.1975.03240240018017.
16. Graham NM, Burrell CJ, Douglas RM, Debelle P, Davies L. Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. J Infect Dis. 1990;162:1277-1282. https://doi.org/10.1093/infdis/162.6.1277.
17. Brandts CH, Ndjave M, Graninger W, Kremsner PG. Effect of paracetamol on parasite clearance time in Plasmodium falciparum malaria. Lancet. 1997;350:704-709. https://doi.org/10.1016/S0140-6736(97)02255-1.
18. Mikaeloff Y, Kezouh A, Suissa S. Nonsteroidal anti-inflammatory drug use and the risk of severe skin and soft tissue complications in patients with varicella or zoster disease. Br J Clin Pharmacol. 2007;65:2:203-209. https://doi.org/10.1016/S0140-6736(97)02255-1.
19. Day M. COVID-19: ibuprofen should not be used for managing symptoms, say doctors and scientists. BMJ. 2020;368:m1086. https://doi.org/10.1136/bmj.m1086.
© 2020 Society of Hospital Medicine
Things We Do For No Reason™: Routine Overnight Vital Sign Checks
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™”(TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits a 73-year-old man with non–insulin dependent diabetes and essential hypertension to the general medicine ward for lower extremity cellulitis. The hospitalist uses standard admission orders, encourages him to elevate his leg above his heart, starts intravenous antibiotics, and monitors him throughout the day and night with regular vital signs. On his second day of admission, the patient’s cellulitis clinically improves, and the team prepares for discharge. However, the nurse notes that the patient did not sleep well and has not slept since his 4
WHY YOU MIGHT THINK Q4 VITAL SIGNS OVERNIGHT ARE HELPFUL
General medicine floors commonly default frequency for measuring vital signs to every 4 hours (Q4), a practice that dates back more than a century to the time of Florence Nightingale.This custom remains in place to ensure the ability to identify and intervene for those at risk for clinical deterioration and preventable death. Research supports the notion that frequent and consistent vital sign checks can minimize mortality and morbidity in the hospital. In fact, validated scoring systems incorporate vital signs with other clinical findings as a way of quickly identifying a patient with worsening clinical status.1 Further, trends and trajectories in vital signs may enable us to identify those with impending decompensation.2 A 2008 consensus statement made by experts in patient safety encouraged hospitals to use frequent vital sign monitoring of patients when available and affordable.3 These interventions aim to help identify and treat patients with early clinical deterioration to prevent poor outcomes.
WHY Q4 VITAL SIGNS OVERNIGHT MIGHT NOT BE NECESSARY
The practice of checking vital signs every 4 hours throughout the night dates to long before the modern era of evidence-based medicine. Research thus far has not focused on the necessity of vital sign checks every 4 hours throughout the night, despite affecting almost every hospitalized patient. Further, patient acuity or need for monitoring does not drive the frequency of overnight vital signs; instead habit and defaults do. We often monitor patients at high risk for clinical deterioration just as frequently as patients at low risk.4
While evidence-based medicine influences much of clinical care, “real-world” needs encountered at the bedside often drive early adapters to innovate. Nurses, who spend the most time at the bedside and conduct the most regular patient assessments, have recognized that not all patients need vital signs checked every 4 hours throughout the night. In 2013, Hands et al conducted a chart review of hospital patterns and found that nurses obtained complete vital sign checks on patients less frequently throughout the night than during the day.5 Their work further showed that nurses used their clinical judgment to make decisions about risk: Those patients deemed low risk by the nurses received fewer vital sign checks while the sicker patients received monitoring every 4 hours throughout the night.
Few researchers have quantitatively identified reasons why nurses may choose to not conduct frequent observations for some patients, beyond the providers’ own experience and judgment. In one study, Hope et al conducted a qualitative analysis of nurses to better understand their reasoning behind who should and should not receive overnight monitoring.6 The results of the analysis revealed that nurses recognize the importance of sleep in support of health and healing and use their clinical judgement when deciding which patients and conditions can forgo frequent observations.Stiver et al conducted trailblazing work that examines the outcomes of decreasing overnight vital sign checks for low-risk hospitalized patients through a randomized pilot study.7 In order to ensure patient safety, their group employed regular nurse observations throughout the night without waking the patient. Those patients assigned to less monitoring overnight reported a trend toward better sleep during hospitalization without the occurrence of any adverse events or escalation in care.
Most important, evidence indicates that sleep disruptions in the hospital worsen health and impede healing; further supporting nurses’ instincts and practices. Hospitalized adults without comorbidities who experience inadequate sleep during hospitalization have a higher perception of pain.8 Similarly, research has associated hospital-induced sleep deprivation and a higher odds of elevated blood glucose in those without diabetes, or “hyperglycemia of hospitalization.” 9 Furthermore, national organizations have recognized the importance of sleep. The American Academy of Nursing, as part of its Choosing Wisely™ campaign, states that, in the hospital, nurses should not disturb a patient’s sleep “unless the patient’s condition or care specifically requires it.”10
Finally, in the era of COVID-19, any opportunity to support physical distancing and to limit face-to-face interaction could protect our patients and staff from acquiring SARS-CoV-2.
WHAT WE SHOULD DO INSTEAD
While consistent vital sign checks allow for early identification of those trending toward clinical deterioration, risk stratification of ward patients can identify those who may benefit from overnight Q4 vital sign checks. While clinicians often use their judgment to identify a subset of low-risk patients for de-escalation of overnight care, artificial intelligence such as Modified Early Warning Score (MEWS) and Pediatric Early Warning Signs (PEWS) may have a role to play. These validated systems use physiologic symptoms that present prior to significant vital sign alterations to identify patients at risk for clinical deterioration.11 As an example, one randomized, controlled trial used a risk stratification tool to eliminate overnight monitoring for low-risk patients. Patients slept more soundly and reported fewer noise disruptions and higher satisfaction with the nursing staff. No adverse events were reported for those who were electronically stratified as low risk.12Further, forcing clinicians to decide on the need for overnight vitals by removing the Q4 vital sign default in the electronic health records (EHR) may minimize overnight disruptions. The University of Chicago in Illinois has implemented “sleep-friendly” options for vital sign ordering in the EHR for both children and adults. Enhanced order sets force providers to consider whether patients qualify for fewer overnight interventions. This change, alongside staff education and empowerment, reduced interruptions overnight for both populations and improved patient experience.13 This patient-centered practice mirrors a recent recommendation from the American Academy of Nursing to minimize sleep disruptions for hospitalized patients by letting low-risk patients sleep.10
RECOMMENDATIONS
- Use clinical judgment or an existing risk stratification system, such as MEWS or PEWS, to identify patients who may benefit from more or less monitoring.
- Forgo overnight vital sign checks for low-risk patients.
- Check overnight vitals for low-risk patients at 10
pm and 6am. - Use pulse oximetry or regular nurse checks as a balancing measure, especially in the pediatric population.
CONCLUSION
Minimizing unnecessary sleep disruptors for hospitalized patients is essential for healing and health. The patient in the clinical scenario had iatrogenic comorbidities added during his hospitalization and an increase in length of stay that resulted from sleep-associated delirium. Hospitalists should take the lead in developing sleep protocols that can leverage current technology to “nudge” clinicians to improve patient sleep. We can modify the frequency of checking vital signs for low-acuity patients and alter environmental factors that may impair sleep, such as noise, light, and temperature, for high-risk patients who cannot forgo overnight vital sign checks. In addition to clinical judgment, artificial intelligence can enable hospitalists and nurses to determine which patients may benefit least from overnight vital sign checks. Finally, if we stop disrupting low-risk patients’ sleep, we can better target resources to patients at high risk for clinical deterioration. Let’s start improving inpatient sleep by eliminating the disruptive things we do for no reason.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
1. Moon A, Cosgrove JF, Lea D, Fairs A, Cressey DM. An eight-year audit before and after the introduction of Modified Early Warning Score (MEWS) charts, of patients admitted to a tertiary referral intensive care unit after CPR. Resuscitation. 2011;82(2):150-154. https://doi.org/10.1016/j.resuscitation.2010.09.480.
2. Churpek MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation 2016;102(5):1-5. https://doi.org/10.1016/j.resuscitation.2016.02.005.
3. DeVita MA, Smith GB, Adam SK, et al. ‘‘Identifying the hospitalized patient in crisis’’—a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81(4):375-382. https://doi.org/10.1016/j.resuscitation.2009.12.008.
4. Yoder JC, Yuen TC, Churpek MM, Arora VM, Edelson DP. A prospective study of nighttime vital sign monitoring frequency and risk of clinical deterioration. JAMA Intern Med. 2013;173(16):1554-1555. https://doi.org/10.1001/jamainternmed.2013.7791
5. Hands C, Reid E, Meredith P, et al. Patterns in the recording of vital sign and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf. 2013;22(9):719-726. https://doi.org/10.1136/bmjqs-2013-001954
6. Hope J, Recio-Saucedo A, Fogg C, et al. A fundamental conflict of care: nurses’ accounts of balancing patients’ sleep with taking vital sign observations at night. J Clin Nurs. 2018;27:1860-1871. https://doi.org/10.1111/jocn.14234.
7. Stiver K, Sharma N, Geller K, Smith L, Stephens J. “Quiet at night”: reduced overnight vital sign monitoring linked to both safety and improvements in patients’ perception of hospital sleep quality. Patient Exp J. 2017;4(1):Article 10. https://doi.org/10.35680/2372-0247.1185.
8. Raymond I, Nielsen TA, Lavigne G, Manzini C, Choiniere M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;93(3):381-388. https://doi.org/10.1016/s0304-3959(01)00282-2.
9. DePietro RH, Knutson KL, Spampinato L, et al. Association between inpatient sleep loss and hyperglycemia of hospitalization. Diabetes Care. 2017;40(2):188-193. https://doi.org/10.2337/dc16-1683.
10. American Academy of Nursing. Choosing Wisely. Twenty-Five Things Nurses and Patients Should Question. July 2018. https://www.choosingwisely.org/wp-content/uploads/2015/02/AANursing-Choosing-Wisely-List.pdf.
11. van Galen LS, Dijkstra CC, Ludikhuize J, Kramer MHH, Nanayakkara PWB. A protocolised once a day Modified Early Warning Score (MEWS) measurement is an appropriate screening tool for major adverse events in a general hospital population. PLoS One. 2016;11(8):e0160811. https://doi.org/10.1371/journal.pone.0160811.
12. Edelson DP, Carey K, Twu NM, et al. Acuity-based nighttime vital sign assessments: a randomized controlled trial. Abstract presented at: Hospital Medicine 2019; March 24-27, 2019; National Harbor, Maryland. https://www.shmabstracts.com/abstract/acuity-based-nighttime-vital-sign-assessments-a-randomized-controlled-trial/. Accessed March 20, 2020
13. Arora VM, Machado N, Anderson SL, et al. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14(1):38-41. https://doi.org/10.12788/jhm.3091.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™”(TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits a 73-year-old man with non–insulin dependent diabetes and essential hypertension to the general medicine ward for lower extremity cellulitis. The hospitalist uses standard admission orders, encourages him to elevate his leg above his heart, starts intravenous antibiotics, and monitors him throughout the day and night with regular vital signs. On his second day of admission, the patient’s cellulitis clinically improves, and the team prepares for discharge. However, the nurse notes that the patient did not sleep well and has not slept since his 4
WHY YOU MIGHT THINK Q4 VITAL SIGNS OVERNIGHT ARE HELPFUL
General medicine floors commonly default frequency for measuring vital signs to every 4 hours (Q4), a practice that dates back more than a century to the time of Florence Nightingale.This custom remains in place to ensure the ability to identify and intervene for those at risk for clinical deterioration and preventable death. Research supports the notion that frequent and consistent vital sign checks can minimize mortality and morbidity in the hospital. In fact, validated scoring systems incorporate vital signs with other clinical findings as a way of quickly identifying a patient with worsening clinical status.1 Further, trends and trajectories in vital signs may enable us to identify those with impending decompensation.2 A 2008 consensus statement made by experts in patient safety encouraged hospitals to use frequent vital sign monitoring of patients when available and affordable.3 These interventions aim to help identify and treat patients with early clinical deterioration to prevent poor outcomes.
WHY Q4 VITAL SIGNS OVERNIGHT MIGHT NOT BE NECESSARY
The practice of checking vital signs every 4 hours throughout the night dates to long before the modern era of evidence-based medicine. Research thus far has not focused on the necessity of vital sign checks every 4 hours throughout the night, despite affecting almost every hospitalized patient. Further, patient acuity or need for monitoring does not drive the frequency of overnight vital signs; instead habit and defaults do. We often monitor patients at high risk for clinical deterioration just as frequently as patients at low risk.4
While evidence-based medicine influences much of clinical care, “real-world” needs encountered at the bedside often drive early adapters to innovate. Nurses, who spend the most time at the bedside and conduct the most regular patient assessments, have recognized that not all patients need vital signs checked every 4 hours throughout the night. In 2013, Hands et al conducted a chart review of hospital patterns and found that nurses obtained complete vital sign checks on patients less frequently throughout the night than during the day.5 Their work further showed that nurses used their clinical judgment to make decisions about risk: Those patients deemed low risk by the nurses received fewer vital sign checks while the sicker patients received monitoring every 4 hours throughout the night.
Few researchers have quantitatively identified reasons why nurses may choose to not conduct frequent observations for some patients, beyond the providers’ own experience and judgment. In one study, Hope et al conducted a qualitative analysis of nurses to better understand their reasoning behind who should and should not receive overnight monitoring.6 The results of the analysis revealed that nurses recognize the importance of sleep in support of health and healing and use their clinical judgement when deciding which patients and conditions can forgo frequent observations.Stiver et al conducted trailblazing work that examines the outcomes of decreasing overnight vital sign checks for low-risk hospitalized patients through a randomized pilot study.7 In order to ensure patient safety, their group employed regular nurse observations throughout the night without waking the patient. Those patients assigned to less monitoring overnight reported a trend toward better sleep during hospitalization without the occurrence of any adverse events or escalation in care.
Most important, evidence indicates that sleep disruptions in the hospital worsen health and impede healing; further supporting nurses’ instincts and practices. Hospitalized adults without comorbidities who experience inadequate sleep during hospitalization have a higher perception of pain.8 Similarly, research has associated hospital-induced sleep deprivation and a higher odds of elevated blood glucose in those without diabetes, or “hyperglycemia of hospitalization.” 9 Furthermore, national organizations have recognized the importance of sleep. The American Academy of Nursing, as part of its Choosing Wisely™ campaign, states that, in the hospital, nurses should not disturb a patient’s sleep “unless the patient’s condition or care specifically requires it.”10
Finally, in the era of COVID-19, any opportunity to support physical distancing and to limit face-to-face interaction could protect our patients and staff from acquiring SARS-CoV-2.
WHAT WE SHOULD DO INSTEAD
While consistent vital sign checks allow for early identification of those trending toward clinical deterioration, risk stratification of ward patients can identify those who may benefit from overnight Q4 vital sign checks. While clinicians often use their judgment to identify a subset of low-risk patients for de-escalation of overnight care, artificial intelligence such as Modified Early Warning Score (MEWS) and Pediatric Early Warning Signs (PEWS) may have a role to play. These validated systems use physiologic symptoms that present prior to significant vital sign alterations to identify patients at risk for clinical deterioration.11 As an example, one randomized, controlled trial used a risk stratification tool to eliminate overnight monitoring for low-risk patients. Patients slept more soundly and reported fewer noise disruptions and higher satisfaction with the nursing staff. No adverse events were reported for those who were electronically stratified as low risk.12Further, forcing clinicians to decide on the need for overnight vitals by removing the Q4 vital sign default in the electronic health records (EHR) may minimize overnight disruptions. The University of Chicago in Illinois has implemented “sleep-friendly” options for vital sign ordering in the EHR for both children and adults. Enhanced order sets force providers to consider whether patients qualify for fewer overnight interventions. This change, alongside staff education and empowerment, reduced interruptions overnight for both populations and improved patient experience.13 This patient-centered practice mirrors a recent recommendation from the American Academy of Nursing to minimize sleep disruptions for hospitalized patients by letting low-risk patients sleep.10
RECOMMENDATIONS
- Use clinical judgment or an existing risk stratification system, such as MEWS or PEWS, to identify patients who may benefit from more or less monitoring.
- Forgo overnight vital sign checks for low-risk patients.
- Check overnight vitals for low-risk patients at 10
pm and 6am. - Use pulse oximetry or regular nurse checks as a balancing measure, especially in the pediatric population.
CONCLUSION
Minimizing unnecessary sleep disruptors for hospitalized patients is essential for healing and health. The patient in the clinical scenario had iatrogenic comorbidities added during his hospitalization and an increase in length of stay that resulted from sleep-associated delirium. Hospitalists should take the lead in developing sleep protocols that can leverage current technology to “nudge” clinicians to improve patient sleep. We can modify the frequency of checking vital signs for low-acuity patients and alter environmental factors that may impair sleep, such as noise, light, and temperature, for high-risk patients who cannot forgo overnight vital sign checks. In addition to clinical judgment, artificial intelligence can enable hospitalists and nurses to determine which patients may benefit least from overnight vital sign checks. Finally, if we stop disrupting low-risk patients’ sleep, we can better target resources to patients at high risk for clinical deterioration. Let’s start improving inpatient sleep by eliminating the disruptive things we do for no reason.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™”(TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits a 73-year-old man with non–insulin dependent diabetes and essential hypertension to the general medicine ward for lower extremity cellulitis. The hospitalist uses standard admission orders, encourages him to elevate his leg above his heart, starts intravenous antibiotics, and monitors him throughout the day and night with regular vital signs. On his second day of admission, the patient’s cellulitis clinically improves, and the team prepares for discharge. However, the nurse notes that the patient did not sleep well and has not slept since his 4
WHY YOU MIGHT THINK Q4 VITAL SIGNS OVERNIGHT ARE HELPFUL
General medicine floors commonly default frequency for measuring vital signs to every 4 hours (Q4), a practice that dates back more than a century to the time of Florence Nightingale.This custom remains in place to ensure the ability to identify and intervene for those at risk for clinical deterioration and preventable death. Research supports the notion that frequent and consistent vital sign checks can minimize mortality and morbidity in the hospital. In fact, validated scoring systems incorporate vital signs with other clinical findings as a way of quickly identifying a patient with worsening clinical status.1 Further, trends and trajectories in vital signs may enable us to identify those with impending decompensation.2 A 2008 consensus statement made by experts in patient safety encouraged hospitals to use frequent vital sign monitoring of patients when available and affordable.3 These interventions aim to help identify and treat patients with early clinical deterioration to prevent poor outcomes.
WHY Q4 VITAL SIGNS OVERNIGHT MIGHT NOT BE NECESSARY
The practice of checking vital signs every 4 hours throughout the night dates to long before the modern era of evidence-based medicine. Research thus far has not focused on the necessity of vital sign checks every 4 hours throughout the night, despite affecting almost every hospitalized patient. Further, patient acuity or need for monitoring does not drive the frequency of overnight vital signs; instead habit and defaults do. We often monitor patients at high risk for clinical deterioration just as frequently as patients at low risk.4
While evidence-based medicine influences much of clinical care, “real-world” needs encountered at the bedside often drive early adapters to innovate. Nurses, who spend the most time at the bedside and conduct the most regular patient assessments, have recognized that not all patients need vital signs checked every 4 hours throughout the night. In 2013, Hands et al conducted a chart review of hospital patterns and found that nurses obtained complete vital sign checks on patients less frequently throughout the night than during the day.5 Their work further showed that nurses used their clinical judgment to make decisions about risk: Those patients deemed low risk by the nurses received fewer vital sign checks while the sicker patients received monitoring every 4 hours throughout the night.
Few researchers have quantitatively identified reasons why nurses may choose to not conduct frequent observations for some patients, beyond the providers’ own experience and judgment. In one study, Hope et al conducted a qualitative analysis of nurses to better understand their reasoning behind who should and should not receive overnight monitoring.6 The results of the analysis revealed that nurses recognize the importance of sleep in support of health and healing and use their clinical judgement when deciding which patients and conditions can forgo frequent observations.Stiver et al conducted trailblazing work that examines the outcomes of decreasing overnight vital sign checks for low-risk hospitalized patients through a randomized pilot study.7 In order to ensure patient safety, their group employed regular nurse observations throughout the night without waking the patient. Those patients assigned to less monitoring overnight reported a trend toward better sleep during hospitalization without the occurrence of any adverse events or escalation in care.
Most important, evidence indicates that sleep disruptions in the hospital worsen health and impede healing; further supporting nurses’ instincts and practices. Hospitalized adults without comorbidities who experience inadequate sleep during hospitalization have a higher perception of pain.8 Similarly, research has associated hospital-induced sleep deprivation and a higher odds of elevated blood glucose in those without diabetes, or “hyperglycemia of hospitalization.” 9 Furthermore, national organizations have recognized the importance of sleep. The American Academy of Nursing, as part of its Choosing Wisely™ campaign, states that, in the hospital, nurses should not disturb a patient’s sleep “unless the patient’s condition or care specifically requires it.”10
Finally, in the era of COVID-19, any opportunity to support physical distancing and to limit face-to-face interaction could protect our patients and staff from acquiring SARS-CoV-2.
WHAT WE SHOULD DO INSTEAD
While consistent vital sign checks allow for early identification of those trending toward clinical deterioration, risk stratification of ward patients can identify those who may benefit from overnight Q4 vital sign checks. While clinicians often use their judgment to identify a subset of low-risk patients for de-escalation of overnight care, artificial intelligence such as Modified Early Warning Score (MEWS) and Pediatric Early Warning Signs (PEWS) may have a role to play. These validated systems use physiologic symptoms that present prior to significant vital sign alterations to identify patients at risk for clinical deterioration.11 As an example, one randomized, controlled trial used a risk stratification tool to eliminate overnight monitoring for low-risk patients. Patients slept more soundly and reported fewer noise disruptions and higher satisfaction with the nursing staff. No adverse events were reported for those who were electronically stratified as low risk.12Further, forcing clinicians to decide on the need for overnight vitals by removing the Q4 vital sign default in the electronic health records (EHR) may minimize overnight disruptions. The University of Chicago in Illinois has implemented “sleep-friendly” options for vital sign ordering in the EHR for both children and adults. Enhanced order sets force providers to consider whether patients qualify for fewer overnight interventions. This change, alongside staff education and empowerment, reduced interruptions overnight for both populations and improved patient experience.13 This patient-centered practice mirrors a recent recommendation from the American Academy of Nursing to minimize sleep disruptions for hospitalized patients by letting low-risk patients sleep.10
RECOMMENDATIONS
- Use clinical judgment or an existing risk stratification system, such as MEWS or PEWS, to identify patients who may benefit from more or less monitoring.
- Forgo overnight vital sign checks for low-risk patients.
- Check overnight vitals for low-risk patients at 10
pm and 6am. - Use pulse oximetry or regular nurse checks as a balancing measure, especially in the pediatric population.
CONCLUSION
Minimizing unnecessary sleep disruptors for hospitalized patients is essential for healing and health. The patient in the clinical scenario had iatrogenic comorbidities added during his hospitalization and an increase in length of stay that resulted from sleep-associated delirium. Hospitalists should take the lead in developing sleep protocols that can leverage current technology to “nudge” clinicians to improve patient sleep. We can modify the frequency of checking vital signs for low-acuity patients and alter environmental factors that may impair sleep, such as noise, light, and temperature, for high-risk patients who cannot forgo overnight vital sign checks. In addition to clinical judgment, artificial intelligence can enable hospitalists and nurses to determine which patients may benefit least from overnight vital sign checks. Finally, if we stop disrupting low-risk patients’ sleep, we can better target resources to patients at high risk for clinical deterioration. Let’s start improving inpatient sleep by eliminating the disruptive things we do for no reason.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing [email protected].
1. Moon A, Cosgrove JF, Lea D, Fairs A, Cressey DM. An eight-year audit before and after the introduction of Modified Early Warning Score (MEWS) charts, of patients admitted to a tertiary referral intensive care unit after CPR. Resuscitation. 2011;82(2):150-154. https://doi.org/10.1016/j.resuscitation.2010.09.480.
2. Churpek MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation 2016;102(5):1-5. https://doi.org/10.1016/j.resuscitation.2016.02.005.
3. DeVita MA, Smith GB, Adam SK, et al. ‘‘Identifying the hospitalized patient in crisis’’—a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81(4):375-382. https://doi.org/10.1016/j.resuscitation.2009.12.008.
4. Yoder JC, Yuen TC, Churpek MM, Arora VM, Edelson DP. A prospective study of nighttime vital sign monitoring frequency and risk of clinical deterioration. JAMA Intern Med. 2013;173(16):1554-1555. https://doi.org/10.1001/jamainternmed.2013.7791
5. Hands C, Reid E, Meredith P, et al. Patterns in the recording of vital sign and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf. 2013;22(9):719-726. https://doi.org/10.1136/bmjqs-2013-001954
6. Hope J, Recio-Saucedo A, Fogg C, et al. A fundamental conflict of care: nurses’ accounts of balancing patients’ sleep with taking vital sign observations at night. J Clin Nurs. 2018;27:1860-1871. https://doi.org/10.1111/jocn.14234.
7. Stiver K, Sharma N, Geller K, Smith L, Stephens J. “Quiet at night”: reduced overnight vital sign monitoring linked to both safety and improvements in patients’ perception of hospital sleep quality. Patient Exp J. 2017;4(1):Article 10. https://doi.org/10.35680/2372-0247.1185.
8. Raymond I, Nielsen TA, Lavigne G, Manzini C, Choiniere M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;93(3):381-388. https://doi.org/10.1016/s0304-3959(01)00282-2.
9. DePietro RH, Knutson KL, Spampinato L, et al. Association between inpatient sleep loss and hyperglycemia of hospitalization. Diabetes Care. 2017;40(2):188-193. https://doi.org/10.2337/dc16-1683.
10. American Academy of Nursing. Choosing Wisely. Twenty-Five Things Nurses and Patients Should Question. July 2018. https://www.choosingwisely.org/wp-content/uploads/2015/02/AANursing-Choosing-Wisely-List.pdf.
11. van Galen LS, Dijkstra CC, Ludikhuize J, Kramer MHH, Nanayakkara PWB. A protocolised once a day Modified Early Warning Score (MEWS) measurement is an appropriate screening tool for major adverse events in a general hospital population. PLoS One. 2016;11(8):e0160811. https://doi.org/10.1371/journal.pone.0160811.
12. Edelson DP, Carey K, Twu NM, et al. Acuity-based nighttime vital sign assessments: a randomized controlled trial. Abstract presented at: Hospital Medicine 2019; March 24-27, 2019; National Harbor, Maryland. https://www.shmabstracts.com/abstract/acuity-based-nighttime-vital-sign-assessments-a-randomized-controlled-trial/. Accessed March 20, 2020
13. Arora VM, Machado N, Anderson SL, et al. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14(1):38-41. https://doi.org/10.12788/jhm.3091.
1. Moon A, Cosgrove JF, Lea D, Fairs A, Cressey DM. An eight-year audit before and after the introduction of Modified Early Warning Score (MEWS) charts, of patients admitted to a tertiary referral intensive care unit after CPR. Resuscitation. 2011;82(2):150-154. https://doi.org/10.1016/j.resuscitation.2010.09.480.
2. Churpek MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation 2016;102(5):1-5. https://doi.org/10.1016/j.resuscitation.2016.02.005.
3. DeVita MA, Smith GB, Adam SK, et al. ‘‘Identifying the hospitalized patient in crisis’’—a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81(4):375-382. https://doi.org/10.1016/j.resuscitation.2009.12.008.
4. Yoder JC, Yuen TC, Churpek MM, Arora VM, Edelson DP. A prospective study of nighttime vital sign monitoring frequency and risk of clinical deterioration. JAMA Intern Med. 2013;173(16):1554-1555. https://doi.org/10.1001/jamainternmed.2013.7791
5. Hands C, Reid E, Meredith P, et al. Patterns in the recording of vital sign and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf. 2013;22(9):719-726. https://doi.org/10.1136/bmjqs-2013-001954
6. Hope J, Recio-Saucedo A, Fogg C, et al. A fundamental conflict of care: nurses’ accounts of balancing patients’ sleep with taking vital sign observations at night. J Clin Nurs. 2018;27:1860-1871. https://doi.org/10.1111/jocn.14234.
7. Stiver K, Sharma N, Geller K, Smith L, Stephens J. “Quiet at night”: reduced overnight vital sign monitoring linked to both safety and improvements in patients’ perception of hospital sleep quality. Patient Exp J. 2017;4(1):Article 10. https://doi.org/10.35680/2372-0247.1185.
8. Raymond I, Nielsen TA, Lavigne G, Manzini C, Choiniere M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;93(3):381-388. https://doi.org/10.1016/s0304-3959(01)00282-2.
9. DePietro RH, Knutson KL, Spampinato L, et al. Association between inpatient sleep loss and hyperglycemia of hospitalization. Diabetes Care. 2017;40(2):188-193. https://doi.org/10.2337/dc16-1683.
10. American Academy of Nursing. Choosing Wisely. Twenty-Five Things Nurses and Patients Should Question. July 2018. https://www.choosingwisely.org/wp-content/uploads/2015/02/AANursing-Choosing-Wisely-List.pdf.
11. van Galen LS, Dijkstra CC, Ludikhuize J, Kramer MHH, Nanayakkara PWB. A protocolised once a day Modified Early Warning Score (MEWS) measurement is an appropriate screening tool for major adverse events in a general hospital population. PLoS One. 2016;11(8):e0160811. https://doi.org/10.1371/journal.pone.0160811.
12. Edelson DP, Carey K, Twu NM, et al. Acuity-based nighttime vital sign assessments: a randomized controlled trial. Abstract presented at: Hospital Medicine 2019; March 24-27, 2019; National Harbor, Maryland. https://www.shmabstracts.com/abstract/acuity-based-nighttime-vital-sign-assessments-a-randomized-controlled-trial/. Accessed March 20, 2020
13. Arora VM, Machado N, Anderson SL, et al. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14(1):38-41. https://doi.org/10.12788/jhm.3091.
© 2020 Society of Hospital Medicine
Things We Do for No Reason™: Obtaining an Abdominal X-ray to Assess for Constipation in Children

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 5-year old boy is admitted to the hospital for a bowel clean-out after presenting with abdominal pain and having an abdominal x-ray that demonstrated a “moderate stool burden.” After ingestion of the bowel prep, he develops worsening abdominal cramping and diarrhea. Upon reviewing the bowel history with his mother afterward, the team learns that he has had a bowel movement every 1-2 days as usual and has been having soft stools without any straining, pain, or blood present.
BACKGROUND
Functional constipation is a common clinical problem in pediatrics and constitutes a large number of admissions into hospitals and visits to clinics and emergency departments. In the United States, up to 36% of children are affected.Associated healthcare costs for children with constipation are estimated at $5.9 billion per year, which is $3.9 billion more than the general pediatric population without constipation.1 In 2011, American children aged 17 years and younger had more than 270,000 visits to the emergency department for constipation.2 As many as 70% of children who are given a diagnosis of constipation in the emergency department have an abdominal x-ray completed.3 The carcinogenic effects of radiation from radiography are well known. Unnecessary imaging places the child at risk for these effects while adding to the overall cost of medical care.4
WHY AN ABDOMINAL X-RAY MAY SEEM HELPFUL
The overall utilization of diagnostic imaging is increasing in pediatric emergency departments.4 When questioning why this is the case, one should consider the method of problem solving used by most physicians. After formulating initial hypotheses based on available information, prior knowledge, and experience, physicians aim to obtain additional data to confirm or reject each hypothesis.5
A 2017 study surveyed 24 pediatric gastroenterologists after 72 patient encounters and found that the most common cause for obtaining an abdominal x-ray was for evaluation of stool burden (70%).5 Other reasons included assessing the need for a bowel clean-out (35%), diagnosing fecal impaction (27%), finding the cause for abdominal pain (24%), and demonstrating stool burden to a family (14%). This same study found that most of the polled providers used an abdominal x-ray to assess for constipation, and nearly half changed their management based on the findings.
WHY ABDOMINAL X-RAYS ARE NOT HELPFUL
Many systematic reviews and retrospective studies have investigated the efficacy of abdominal x-rays for diagnosing constipation. One retrospective review involving 160 children with defecation complaints assessed the accuracy of different radiologic scoring methods in identifying children with constipation.6 Three pediatric gastroenterologists and 1 pediatric radiologist blindly applied 4 scoring methods: colonic transit time, Leech score, Barr score, and fecal loading. The results showed that all x-ray scoring methods had low sensitivity for diagnosing constipation, variable specificity, and low interobserver reproducibility of scores.6 There was also poor ability to differentiate between patients with constipation and nonretentive fecal incontinence. Fecal loading had the worst performance in differentiating between these 2. Greater than 20% of children with clinically diagnosed constipation had normal Barr and Leech scores.6 Another systematic review also found no evidence for a diagnostic association between clinical symptoms of constipation and fecal loading on abdominal x-rays.7 In this study, the sensitivity and specificity of the x-ray were as low as 61% and 55%, respectively, which indicate poor overall diagnostic accuracy. Abdominal x-rays are subjective, not standardized, and represent a single observation in time. The amount of fecal loading seen on imaging is subject to daily variation depending on the timing of last food intake and timing of last defecation. There is a large variance in interpretation of fecal loading, and any stool seen on an x-ray does not rule out another potential diagnosis causing abdominal pain.
In 2014, the North American Society for Pediatric Gastroenterology, Hepatology, & Nutrition (NASPGHAN) and the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) released joint clinical guidelines that the evidence supports not obtaining an abdominal x-ray to diagnose functional constipation.8 Similarly, the National Institute for Health and Care Excellence (NICE) stated that abdominal x-rays should not be recommended as an additional test for constipation in children.9 These groups advocate for diagnosing functional constipation clinically by using a careful history and physical exam.
WHY ABDOMINAL X-RAYS ARE POTENTIALLY HARMFUL
The primary patient harm associated with abdominal x-rays is radiation exposure. While the amount of radiation in a single x-ray is low, children with constipation tend to have frequent revisits, significantly more than children with other common chronic conditions (eg, asthma and migraine headaches).10
One multicenter retrospective cohort study that included approximately 282,000 children diagnosed with constipation found that children who received an abdominal x-ray were twice as likely to return to the emergency department with a clinically significant alternate diagnosis (0.33% vs 0.17%). The 2 most common missed diagnoses were acute appendicitis and intussusception.3 Another retrospective study that included about 3,700 children also found that x-rays were performed more frequently in children who were misdiagnosed than in those who did not have a significant alternate diagnosis (75% vs 46%).11 In this case, both of these groups had a similar amount of stool on the x-rays as determined by the mean Leech scores. While this study identified an association between abdominal x-ray use and misdiagnoses, a causative effect was not necessarily discovered between the 2. The authors felt that even relatively large amounts of stool on an x-ray should not discount serious causes of abdominal pain or tenderness.11 A third retrospective study determined that children who received an abdominal x-ray and were diagnosed with constipation were significantly more likely to be admitted to the hospital, further raising healthcare costs.12 In this study, having an x-ray reduced the odds of being discharged home by about half. They also found that abdominal x-rays could be avoided if digital rectal exams were performed.12
HOW CONSTIPATION SHOULD BE DIAGNOSED
Functional constipation is a clinical diagnosis based on a thorough collection of history and a complete physical exam in children of all ages, including digital examination of the rectum to assess for fecal impaction, if necessary.
The Rome IV criteria for chronic constipation can be helpful and includes at least 2 of the following features for at least 1 month in infants up to 4 years of age: 2 or fewer stools per week, history of excessive stool retention, history of painful or hard bowel movements, history of large-diameter stools, and presence of a large fecal mass in the rectum.13 In children who are toilet trained, 2 additional criteria may be used: at least 1 episode of fecal incontinence per week after being toilet-trained and history of large-diameter stools that may obstruct the toilet.13
The NASPGHAN and ESPGHAN joint guidelines from 2014 state that, while constipation is based on history and physical exam, a major role of the history and physical exam is to exclude other disorders that also present with difficulty in defecation.8 This can help identify red-flag features or complications and guide further investigation. While evidence did not support routine use of a digital rectal exam in diagnosing constipation, the guidelines stated that a rectal exam (visual and digital) helps to evaluate for anorectal malformations, anal stenosis, rectal tone, distension, erythema, skin tags, anal fissures, or a fecal mass.8
In regard to history, approximately 0.4%-20% of healthy children without constipation have at least 1 clinical feature listed above. Therefore, the use of a single clinical finding to diagnose constipation, such as decreased bowel frequency, can result in an inappropriate diagnosis. Children experience large variations in stool output depending on diet, genetics, and environmental factors.10 The usual pattern of bowel habits in humans range from 3 times daily to every 3 days.14 Importantly, there are times to order an abdominal x-ray for patients with abdominal pain. The NASPGHAN and ESPGHAN joint guidelines recommend obtaining abdominal x-rays to evaluate children who have concerning features, such as previous abdominal surgeries, known genetic conditions or malformations, bilious emesis, or severe abdominal distension.8
RECOMMENDATIONS
- Functional constipation should be diagnosed based purely on a thorough history and physical examination, including a rectal exam
- Abdominal x-rays (ordered for any reason) should not be used to diagnose or assess for functional constipation
CONCLUSIONS
Performing abdominal x-rays to assess for pediatric functional constipation is not beneficial and potentially harmful to patients. Multiple retrospective studies revealed no diagnostic association between clinical symptoms or severity of constipation and findings on abdominal radiography. X-rays have very low sensitivity and specificity for diagnosing constipation. In the pediatric emergency department, abdominal x-rays completed for patients diagnosed with constipation have been associated with missed diagnoses, false reassurance of constipation, more frequent admissions into the hospital, longer hospital stays, higher healthcare costs, and unnecessary radiation exposure. The NICE as well as 2014 NASPGHAN and ESPGHAN clinical guidelines recommend against obtaining x-rays to diagnose constipation. The most effective way to diagnose functional constipation in children is with a thorough collection of history and physical exam. In the introductory case, the boy received an osmotic laxative based on abdominal x-ray findings, which resulted in the adverse effect of diarrhea. This case demonstrates how using abdominal x-rays to assess for constipation can be misleading and emphasizes the importance of collecting a thorough history and physical exam.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].
1. Afzal NA, Tighe MP, Thomson MA. (2011, June 13). Constipation in children. Ital J Pediatr. 2011;37:28. https://doi.org/10.1186/1824-7288-37-28.
2. Sommers T, Corban C, Sengupta N, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110(4):572-579. https://doi.org/10.1038/ajg.2015.64.
3. Freedman SB, Rodean J, Hall M, et al. (2017). Delayed diagnoses in children with constipation: multicenter retrospective cohort study. J Pediatr. 186, 87-94.e16. https://doi.org/10.1016/j.jpeds.2017.03.061.
4. Reed MH. Imaging utilization commentary: A radiology perspective. Pediatr Radiol. 2008;38 (Suppl 4):S660-S663. https://doi.org/10.1007/s00247-008-0982-y.
5. Beinvogl B, Sabharwal S, McSweeney M, Nurko S. Are we using abdominal radiographs appropriately in the management of pediatric constipation? J Pediatr. 2017;191:179-183. https://doi.org/10.1016/j.jpeds.2017.08.075.
6. Pensabene L, Buonomo C, Fishman L, Chitkara D, Nurko S. Lack of utility of abdominal x-rays in the evaluation of children with constipation: Comparison of different scoring methods. J Pediatr Gastroenterol Nutr. 2010;51(2):155-159. https://doi.org/10.1097/MPG.0b013e3181cb4309.
7. Berger MY, Tabbers MM, Kurver MJ, Boluyt N, Benninga MA. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: A systematic review. J Pediatr. 2012;161(1):44–50.e502. https://doi.org/10.1016/j.jpeds.2011.12.045.
8. Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: Evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258-274. https://doi.org/10.1097/mpg.0000000000000266.
9. Bardisa-Ezcurra L, Ullman R, Gordon J; Guideline Development Group. Diagnosis and management of idiopathic childhood constipation: summary of NICE guidance. BMJ. 2010;340:c2585. https://doi.org/10.1136/bmj.c2585.
10. Rajindrajith S, Manjuri Devanarayana N, Benninga MA. Defecation Disorders in Children: Constipation and Functional Fecal Incontinence. In: Guandalini S, Dhawan A, Branski D. eds. Textbook of Pediatric Gastroenterology, Hepatology and Nutrition: A Comprehensive Guide to Practice (1st ed.). Basingstoke, England: Springer; 2016:247-260.
11. Freedman SB, Thull-Freedman J, Manson D, et al. Pediatric abdominal radiograph use, constipation, and significant misdiagnoses. J Pediatr. 2014;164(1):83-88.e2. https://doi.org/10.1016/j.jpeds.2013.08.074.
12. Chumpitazi CE, Rees CA, Camp EA, Henkel EB, Valdez KL, Chumpitazi BP. Diagnostic approach to constipation impacts pediatric emergency department disposition. Am J Emerg Med. 2017;35(10):1490-1493. https://doi.org/10.1016/j.ajem.2017.04.060.
13. Benninga MA, Nurko S, Faure C, Hyman PE, St. James Roberts I, Schechter NL. Childhood functional GI disorders: Neonate/toddler. Gastroenterology. 2016;150(6):1443-1455. https://doi.org/10.1053/j.gastro.2016.02.016.
14. Walter SA, Kjellström L, Nyhlin H, Talley NJ, Agréus L. Assessment of normal bowel habits in the general adult population: the Popcol study. Scand J Gastroenterol. 2010;45(5):556-566. https://doi.org/10.3109/00365520903551332.

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 5-year old boy is admitted to the hospital for a bowel clean-out after presenting with abdominal pain and having an abdominal x-ray that demonstrated a “moderate stool burden.” After ingestion of the bowel prep, he develops worsening abdominal cramping and diarrhea. Upon reviewing the bowel history with his mother afterward, the team learns that he has had a bowel movement every 1-2 days as usual and has been having soft stools without any straining, pain, or blood present.
BACKGROUND
Functional constipation is a common clinical problem in pediatrics and constitutes a large number of admissions into hospitals and visits to clinics and emergency departments. In the United States, up to 36% of children are affected.Associated healthcare costs for children with constipation are estimated at $5.9 billion per year, which is $3.9 billion more than the general pediatric population without constipation.1 In 2011, American children aged 17 years and younger had more than 270,000 visits to the emergency department for constipation.2 As many as 70% of children who are given a diagnosis of constipation in the emergency department have an abdominal x-ray completed.3 The carcinogenic effects of radiation from radiography are well known. Unnecessary imaging places the child at risk for these effects while adding to the overall cost of medical care.4
WHY AN ABDOMINAL X-RAY MAY SEEM HELPFUL
The overall utilization of diagnostic imaging is increasing in pediatric emergency departments.4 When questioning why this is the case, one should consider the method of problem solving used by most physicians. After formulating initial hypotheses based on available information, prior knowledge, and experience, physicians aim to obtain additional data to confirm or reject each hypothesis.5
A 2017 study surveyed 24 pediatric gastroenterologists after 72 patient encounters and found that the most common cause for obtaining an abdominal x-ray was for evaluation of stool burden (70%).5 Other reasons included assessing the need for a bowel clean-out (35%), diagnosing fecal impaction (27%), finding the cause for abdominal pain (24%), and demonstrating stool burden to a family (14%). This same study found that most of the polled providers used an abdominal x-ray to assess for constipation, and nearly half changed their management based on the findings.
WHY ABDOMINAL X-RAYS ARE NOT HELPFUL
Many systematic reviews and retrospective studies have investigated the efficacy of abdominal x-rays for diagnosing constipation. One retrospective review involving 160 children with defecation complaints assessed the accuracy of different radiologic scoring methods in identifying children with constipation.6 Three pediatric gastroenterologists and 1 pediatric radiologist blindly applied 4 scoring methods: colonic transit time, Leech score, Barr score, and fecal loading. The results showed that all x-ray scoring methods had low sensitivity for diagnosing constipation, variable specificity, and low interobserver reproducibility of scores.6 There was also poor ability to differentiate between patients with constipation and nonretentive fecal incontinence. Fecal loading had the worst performance in differentiating between these 2. Greater than 20% of children with clinically diagnosed constipation had normal Barr and Leech scores.6 Another systematic review also found no evidence for a diagnostic association between clinical symptoms of constipation and fecal loading on abdominal x-rays.7 In this study, the sensitivity and specificity of the x-ray were as low as 61% and 55%, respectively, which indicate poor overall diagnostic accuracy. Abdominal x-rays are subjective, not standardized, and represent a single observation in time. The amount of fecal loading seen on imaging is subject to daily variation depending on the timing of last food intake and timing of last defecation. There is a large variance in interpretation of fecal loading, and any stool seen on an x-ray does not rule out another potential diagnosis causing abdominal pain.
In 2014, the North American Society for Pediatric Gastroenterology, Hepatology, & Nutrition (NASPGHAN) and the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) released joint clinical guidelines that the evidence supports not obtaining an abdominal x-ray to diagnose functional constipation.8 Similarly, the National Institute for Health and Care Excellence (NICE) stated that abdominal x-rays should not be recommended as an additional test for constipation in children.9 These groups advocate for diagnosing functional constipation clinically by using a careful history and physical exam.
WHY ABDOMINAL X-RAYS ARE POTENTIALLY HARMFUL
The primary patient harm associated with abdominal x-rays is radiation exposure. While the amount of radiation in a single x-ray is low, children with constipation tend to have frequent revisits, significantly more than children with other common chronic conditions (eg, asthma and migraine headaches).10
One multicenter retrospective cohort study that included approximately 282,000 children diagnosed with constipation found that children who received an abdominal x-ray were twice as likely to return to the emergency department with a clinically significant alternate diagnosis (0.33% vs 0.17%). The 2 most common missed diagnoses were acute appendicitis and intussusception.3 Another retrospective study that included about 3,700 children also found that x-rays were performed more frequently in children who were misdiagnosed than in those who did not have a significant alternate diagnosis (75% vs 46%).11 In this case, both of these groups had a similar amount of stool on the x-rays as determined by the mean Leech scores. While this study identified an association between abdominal x-ray use and misdiagnoses, a causative effect was not necessarily discovered between the 2. The authors felt that even relatively large amounts of stool on an x-ray should not discount serious causes of abdominal pain or tenderness.11 A third retrospective study determined that children who received an abdominal x-ray and were diagnosed with constipation were significantly more likely to be admitted to the hospital, further raising healthcare costs.12 In this study, having an x-ray reduced the odds of being discharged home by about half. They also found that abdominal x-rays could be avoided if digital rectal exams were performed.12
HOW CONSTIPATION SHOULD BE DIAGNOSED
Functional constipation is a clinical diagnosis based on a thorough collection of history and a complete physical exam in children of all ages, including digital examination of the rectum to assess for fecal impaction, if necessary.
The Rome IV criteria for chronic constipation can be helpful and includes at least 2 of the following features for at least 1 month in infants up to 4 years of age: 2 or fewer stools per week, history of excessive stool retention, history of painful or hard bowel movements, history of large-diameter stools, and presence of a large fecal mass in the rectum.13 In children who are toilet trained, 2 additional criteria may be used: at least 1 episode of fecal incontinence per week after being toilet-trained and history of large-diameter stools that may obstruct the toilet.13
The NASPGHAN and ESPGHAN joint guidelines from 2014 state that, while constipation is based on history and physical exam, a major role of the history and physical exam is to exclude other disorders that also present with difficulty in defecation.8 This can help identify red-flag features or complications and guide further investigation. While evidence did not support routine use of a digital rectal exam in diagnosing constipation, the guidelines stated that a rectal exam (visual and digital) helps to evaluate for anorectal malformations, anal stenosis, rectal tone, distension, erythema, skin tags, anal fissures, or a fecal mass.8
In regard to history, approximately 0.4%-20% of healthy children without constipation have at least 1 clinical feature listed above. Therefore, the use of a single clinical finding to diagnose constipation, such as decreased bowel frequency, can result in an inappropriate diagnosis. Children experience large variations in stool output depending on diet, genetics, and environmental factors.10 The usual pattern of bowel habits in humans range from 3 times daily to every 3 days.14 Importantly, there are times to order an abdominal x-ray for patients with abdominal pain. The NASPGHAN and ESPGHAN joint guidelines recommend obtaining abdominal x-rays to evaluate children who have concerning features, such as previous abdominal surgeries, known genetic conditions or malformations, bilious emesis, or severe abdominal distension.8
RECOMMENDATIONS
- Functional constipation should be diagnosed based purely on a thorough history and physical examination, including a rectal exam
- Abdominal x-rays (ordered for any reason) should not be used to diagnose or assess for functional constipation
CONCLUSIONS
Performing abdominal x-rays to assess for pediatric functional constipation is not beneficial and potentially harmful to patients. Multiple retrospective studies revealed no diagnostic association between clinical symptoms or severity of constipation and findings on abdominal radiography. X-rays have very low sensitivity and specificity for diagnosing constipation. In the pediatric emergency department, abdominal x-rays completed for patients diagnosed with constipation have been associated with missed diagnoses, false reassurance of constipation, more frequent admissions into the hospital, longer hospital stays, higher healthcare costs, and unnecessary radiation exposure. The NICE as well as 2014 NASPGHAN and ESPGHAN clinical guidelines recommend against obtaining x-rays to diagnose constipation. The most effective way to diagnose functional constipation in children is with a thorough collection of history and physical exam. In the introductory case, the boy received an osmotic laxative based on abdominal x-ray findings, which resulted in the adverse effect of diarrhea. This case demonstrates how using abdominal x-rays to assess for constipation can be misleading and emphasizes the importance of collecting a thorough history and physical exam.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 5-year old boy is admitted to the hospital for a bowel clean-out after presenting with abdominal pain and having an abdominal x-ray that demonstrated a “moderate stool burden.” After ingestion of the bowel prep, he develops worsening abdominal cramping and diarrhea. Upon reviewing the bowel history with his mother afterward, the team learns that he has had a bowel movement every 1-2 days as usual and has been having soft stools without any straining, pain, or blood present.
BACKGROUND
Functional constipation is a common clinical problem in pediatrics and constitutes a large number of admissions into hospitals and visits to clinics and emergency departments. In the United States, up to 36% of children are affected.Associated healthcare costs for children with constipation are estimated at $5.9 billion per year, which is $3.9 billion more than the general pediatric population without constipation.1 In 2011, American children aged 17 years and younger had more than 270,000 visits to the emergency department for constipation.2 As many as 70% of children who are given a diagnosis of constipation in the emergency department have an abdominal x-ray completed.3 The carcinogenic effects of radiation from radiography are well known. Unnecessary imaging places the child at risk for these effects while adding to the overall cost of medical care.4
WHY AN ABDOMINAL X-RAY MAY SEEM HELPFUL
The overall utilization of diagnostic imaging is increasing in pediatric emergency departments.4 When questioning why this is the case, one should consider the method of problem solving used by most physicians. After formulating initial hypotheses based on available information, prior knowledge, and experience, physicians aim to obtain additional data to confirm or reject each hypothesis.5
A 2017 study surveyed 24 pediatric gastroenterologists after 72 patient encounters and found that the most common cause for obtaining an abdominal x-ray was for evaluation of stool burden (70%).5 Other reasons included assessing the need for a bowel clean-out (35%), diagnosing fecal impaction (27%), finding the cause for abdominal pain (24%), and demonstrating stool burden to a family (14%). This same study found that most of the polled providers used an abdominal x-ray to assess for constipation, and nearly half changed their management based on the findings.
WHY ABDOMINAL X-RAYS ARE NOT HELPFUL
Many systematic reviews and retrospective studies have investigated the efficacy of abdominal x-rays for diagnosing constipation. One retrospective review involving 160 children with defecation complaints assessed the accuracy of different radiologic scoring methods in identifying children with constipation.6 Three pediatric gastroenterologists and 1 pediatric radiologist blindly applied 4 scoring methods: colonic transit time, Leech score, Barr score, and fecal loading. The results showed that all x-ray scoring methods had low sensitivity for diagnosing constipation, variable specificity, and low interobserver reproducibility of scores.6 There was also poor ability to differentiate between patients with constipation and nonretentive fecal incontinence. Fecal loading had the worst performance in differentiating between these 2. Greater than 20% of children with clinically diagnosed constipation had normal Barr and Leech scores.6 Another systematic review also found no evidence for a diagnostic association between clinical symptoms of constipation and fecal loading on abdominal x-rays.7 In this study, the sensitivity and specificity of the x-ray were as low as 61% and 55%, respectively, which indicate poor overall diagnostic accuracy. Abdominal x-rays are subjective, not standardized, and represent a single observation in time. The amount of fecal loading seen on imaging is subject to daily variation depending on the timing of last food intake and timing of last defecation. There is a large variance in interpretation of fecal loading, and any stool seen on an x-ray does not rule out another potential diagnosis causing abdominal pain.
In 2014, the North American Society for Pediatric Gastroenterology, Hepatology, & Nutrition (NASPGHAN) and the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) released joint clinical guidelines that the evidence supports not obtaining an abdominal x-ray to diagnose functional constipation.8 Similarly, the National Institute for Health and Care Excellence (NICE) stated that abdominal x-rays should not be recommended as an additional test for constipation in children.9 These groups advocate for diagnosing functional constipation clinically by using a careful history and physical exam.
WHY ABDOMINAL X-RAYS ARE POTENTIALLY HARMFUL
The primary patient harm associated with abdominal x-rays is radiation exposure. While the amount of radiation in a single x-ray is low, children with constipation tend to have frequent revisits, significantly more than children with other common chronic conditions (eg, asthma and migraine headaches).10
One multicenter retrospective cohort study that included approximately 282,000 children diagnosed with constipation found that children who received an abdominal x-ray were twice as likely to return to the emergency department with a clinically significant alternate diagnosis (0.33% vs 0.17%). The 2 most common missed diagnoses were acute appendicitis and intussusception.3 Another retrospective study that included about 3,700 children also found that x-rays were performed more frequently in children who were misdiagnosed than in those who did not have a significant alternate diagnosis (75% vs 46%).11 In this case, both of these groups had a similar amount of stool on the x-rays as determined by the mean Leech scores. While this study identified an association between abdominal x-ray use and misdiagnoses, a causative effect was not necessarily discovered between the 2. The authors felt that even relatively large amounts of stool on an x-ray should not discount serious causes of abdominal pain or tenderness.11 A third retrospective study determined that children who received an abdominal x-ray and were diagnosed with constipation were significantly more likely to be admitted to the hospital, further raising healthcare costs.12 In this study, having an x-ray reduced the odds of being discharged home by about half. They also found that abdominal x-rays could be avoided if digital rectal exams were performed.12
HOW CONSTIPATION SHOULD BE DIAGNOSED
Functional constipation is a clinical diagnosis based on a thorough collection of history and a complete physical exam in children of all ages, including digital examination of the rectum to assess for fecal impaction, if necessary.
The Rome IV criteria for chronic constipation can be helpful and includes at least 2 of the following features for at least 1 month in infants up to 4 years of age: 2 or fewer stools per week, history of excessive stool retention, history of painful or hard bowel movements, history of large-diameter stools, and presence of a large fecal mass in the rectum.13 In children who are toilet trained, 2 additional criteria may be used: at least 1 episode of fecal incontinence per week after being toilet-trained and history of large-diameter stools that may obstruct the toilet.13
The NASPGHAN and ESPGHAN joint guidelines from 2014 state that, while constipation is based on history and physical exam, a major role of the history and physical exam is to exclude other disorders that also present with difficulty in defecation.8 This can help identify red-flag features or complications and guide further investigation. While evidence did not support routine use of a digital rectal exam in diagnosing constipation, the guidelines stated that a rectal exam (visual and digital) helps to evaluate for anorectal malformations, anal stenosis, rectal tone, distension, erythema, skin tags, anal fissures, or a fecal mass.8
In regard to history, approximately 0.4%-20% of healthy children without constipation have at least 1 clinical feature listed above. Therefore, the use of a single clinical finding to diagnose constipation, such as decreased bowel frequency, can result in an inappropriate diagnosis. Children experience large variations in stool output depending on diet, genetics, and environmental factors.10 The usual pattern of bowel habits in humans range from 3 times daily to every 3 days.14 Importantly, there are times to order an abdominal x-ray for patients with abdominal pain. The NASPGHAN and ESPGHAN joint guidelines recommend obtaining abdominal x-rays to evaluate children who have concerning features, such as previous abdominal surgeries, known genetic conditions or malformations, bilious emesis, or severe abdominal distension.8
RECOMMENDATIONS
- Functional constipation should be diagnosed based purely on a thorough history and physical examination, including a rectal exam
- Abdominal x-rays (ordered for any reason) should not be used to diagnose or assess for functional constipation
CONCLUSIONS
Performing abdominal x-rays to assess for pediatric functional constipation is not beneficial and potentially harmful to patients. Multiple retrospective studies revealed no diagnostic association between clinical symptoms or severity of constipation and findings on abdominal radiography. X-rays have very low sensitivity and specificity for diagnosing constipation. In the pediatric emergency department, abdominal x-rays completed for patients diagnosed with constipation have been associated with missed diagnoses, false reassurance of constipation, more frequent admissions into the hospital, longer hospital stays, higher healthcare costs, and unnecessary radiation exposure. The NICE as well as 2014 NASPGHAN and ESPGHAN clinical guidelines recommend against obtaining x-rays to diagnose constipation. The most effective way to diagnose functional constipation in children is with a thorough collection of history and physical exam. In the introductory case, the boy received an osmotic laxative based on abdominal x-ray findings, which resulted in the adverse effect of diarrhea. This case demonstrates how using abdominal x-rays to assess for constipation can be misleading and emphasizes the importance of collecting a thorough history and physical exam.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].
1. Afzal NA, Tighe MP, Thomson MA. (2011, June 13). Constipation in children. Ital J Pediatr. 2011;37:28. https://doi.org/10.1186/1824-7288-37-28.
2. Sommers T, Corban C, Sengupta N, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110(4):572-579. https://doi.org/10.1038/ajg.2015.64.
3. Freedman SB, Rodean J, Hall M, et al. (2017). Delayed diagnoses in children with constipation: multicenter retrospective cohort study. J Pediatr. 186, 87-94.e16. https://doi.org/10.1016/j.jpeds.2017.03.061.
4. Reed MH. Imaging utilization commentary: A radiology perspective. Pediatr Radiol. 2008;38 (Suppl 4):S660-S663. https://doi.org/10.1007/s00247-008-0982-y.
5. Beinvogl B, Sabharwal S, McSweeney M, Nurko S. Are we using abdominal radiographs appropriately in the management of pediatric constipation? J Pediatr. 2017;191:179-183. https://doi.org/10.1016/j.jpeds.2017.08.075.
6. Pensabene L, Buonomo C, Fishman L, Chitkara D, Nurko S. Lack of utility of abdominal x-rays in the evaluation of children with constipation: Comparison of different scoring methods. J Pediatr Gastroenterol Nutr. 2010;51(2):155-159. https://doi.org/10.1097/MPG.0b013e3181cb4309.
7. Berger MY, Tabbers MM, Kurver MJ, Boluyt N, Benninga MA. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: A systematic review. J Pediatr. 2012;161(1):44–50.e502. https://doi.org/10.1016/j.jpeds.2011.12.045.
8. Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: Evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258-274. https://doi.org/10.1097/mpg.0000000000000266.
9. Bardisa-Ezcurra L, Ullman R, Gordon J; Guideline Development Group. Diagnosis and management of idiopathic childhood constipation: summary of NICE guidance. BMJ. 2010;340:c2585. https://doi.org/10.1136/bmj.c2585.
10. Rajindrajith S, Manjuri Devanarayana N, Benninga MA. Defecation Disorders in Children: Constipation and Functional Fecal Incontinence. In: Guandalini S, Dhawan A, Branski D. eds. Textbook of Pediatric Gastroenterology, Hepatology and Nutrition: A Comprehensive Guide to Practice (1st ed.). Basingstoke, England: Springer; 2016:247-260.
11. Freedman SB, Thull-Freedman J, Manson D, et al. Pediatric abdominal radiograph use, constipation, and significant misdiagnoses. J Pediatr. 2014;164(1):83-88.e2. https://doi.org/10.1016/j.jpeds.2013.08.074.
12. Chumpitazi CE, Rees CA, Camp EA, Henkel EB, Valdez KL, Chumpitazi BP. Diagnostic approach to constipation impacts pediatric emergency department disposition. Am J Emerg Med. 2017;35(10):1490-1493. https://doi.org/10.1016/j.ajem.2017.04.060.
13. Benninga MA, Nurko S, Faure C, Hyman PE, St. James Roberts I, Schechter NL. Childhood functional GI disorders: Neonate/toddler. Gastroenterology. 2016;150(6):1443-1455. https://doi.org/10.1053/j.gastro.2016.02.016.
14. Walter SA, Kjellström L, Nyhlin H, Talley NJ, Agréus L. Assessment of normal bowel habits in the general adult population: the Popcol study. Scand J Gastroenterol. 2010;45(5):556-566. https://doi.org/10.3109/00365520903551332.
1. Afzal NA, Tighe MP, Thomson MA. (2011, June 13). Constipation in children. Ital J Pediatr. 2011;37:28. https://doi.org/10.1186/1824-7288-37-28.
2. Sommers T, Corban C, Sengupta N, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110(4):572-579. https://doi.org/10.1038/ajg.2015.64.
3. Freedman SB, Rodean J, Hall M, et al. (2017). Delayed diagnoses in children with constipation: multicenter retrospective cohort study. J Pediatr. 186, 87-94.e16. https://doi.org/10.1016/j.jpeds.2017.03.061.
4. Reed MH. Imaging utilization commentary: A radiology perspective. Pediatr Radiol. 2008;38 (Suppl 4):S660-S663. https://doi.org/10.1007/s00247-008-0982-y.
5. Beinvogl B, Sabharwal S, McSweeney M, Nurko S. Are we using abdominal radiographs appropriately in the management of pediatric constipation? J Pediatr. 2017;191:179-183. https://doi.org/10.1016/j.jpeds.2017.08.075.
6. Pensabene L, Buonomo C, Fishman L, Chitkara D, Nurko S. Lack of utility of abdominal x-rays in the evaluation of children with constipation: Comparison of different scoring methods. J Pediatr Gastroenterol Nutr. 2010;51(2):155-159. https://doi.org/10.1097/MPG.0b013e3181cb4309.
7. Berger MY, Tabbers MM, Kurver MJ, Boluyt N, Benninga MA. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: A systematic review. J Pediatr. 2012;161(1):44–50.e502. https://doi.org/10.1016/j.jpeds.2011.12.045.
8. Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: Evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258-274. https://doi.org/10.1097/mpg.0000000000000266.
9. Bardisa-Ezcurra L, Ullman R, Gordon J; Guideline Development Group. Diagnosis and management of idiopathic childhood constipation: summary of NICE guidance. BMJ. 2010;340:c2585. https://doi.org/10.1136/bmj.c2585.
10. Rajindrajith S, Manjuri Devanarayana N, Benninga MA. Defecation Disorders in Children: Constipation and Functional Fecal Incontinence. In: Guandalini S, Dhawan A, Branski D. eds. Textbook of Pediatric Gastroenterology, Hepatology and Nutrition: A Comprehensive Guide to Practice (1st ed.). Basingstoke, England: Springer; 2016:247-260.
11. Freedman SB, Thull-Freedman J, Manson D, et al. Pediatric abdominal radiograph use, constipation, and significant misdiagnoses. J Pediatr. 2014;164(1):83-88.e2. https://doi.org/10.1016/j.jpeds.2013.08.074.
12. Chumpitazi CE, Rees CA, Camp EA, Henkel EB, Valdez KL, Chumpitazi BP. Diagnostic approach to constipation impacts pediatric emergency department disposition. Am J Emerg Med. 2017;35(10):1490-1493. https://doi.org/10.1016/j.ajem.2017.04.060.
13. Benninga MA, Nurko S, Faure C, Hyman PE, St. James Roberts I, Schechter NL. Childhood functional GI disorders: Neonate/toddler. Gastroenterology. 2016;150(6):1443-1455. https://doi.org/10.1053/j.gastro.2016.02.016.
14. Walter SA, Kjellström L, Nyhlin H, Talley NJ, Agréus L. Assessment of normal bowel habits in the general adult population: the Popcol study. Scand J Gastroenterol. 2010;45(5):556-566. https://doi.org/10.3109/00365520903551332.
© 2020 Society of Hospital Medicine
Things We Do for No Reason™: Card Flipping Rounds
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing [email protected].
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
© 2020 Society of Hospital Medicine