User login
President’s report
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
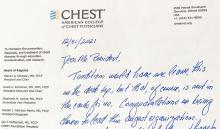
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
Meet our new CHEST President-Designate
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
A mentor in medicine ... a mentor in life
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward C. Rosenow III, MD, Master FCCP/Master Endowment - Master Teacher Endowment Lecture
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
Partnership news from the CHEST Foundation: New grant concentrated on diversity, equity, and inclusion
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.
This month in the journal CHEST®
Editor’s picks
Bronchial thermoplasty in severe asthmatics at 5 years: The PAS2 study. By Dr. G. Chupp, et al.
Significant spirometric transitions and preserved ratio-impaired spirometry (PRISm) among ever-smokers. By Dr. E. Wan, et al.
Addressing advance care planning in patients with COPD. By Dr. E. Rose, et al.
The cost of ARDS: A systematic review. By Dr. P. Boucher, et al.
Acute management of high- and intermediate-risk pulmonary embolism in children: A review. By Dr. C. Ross, et al.
Surgical outcomes for early-stage non-small cell lung cancer at facilities with stereotactic body radiation therapy programs. By Dr. Y. Syed, et al.
Editor’s picks
Editor’s picks
Bronchial thermoplasty in severe asthmatics at 5 years: The PAS2 study. By Dr. G. Chupp, et al.
Significant spirometric transitions and preserved ratio-impaired spirometry (PRISm) among ever-smokers. By Dr. E. Wan, et al.
Addressing advance care planning in patients with COPD. By Dr. E. Rose, et al.
The cost of ARDS: A systematic review. By Dr. P. Boucher, et al.
Acute management of high- and intermediate-risk pulmonary embolism in children: A review. By Dr. C. Ross, et al.
Surgical outcomes for early-stage non-small cell lung cancer at facilities with stereotactic body radiation therapy programs. By Dr. Y. Syed, et al.
Bronchial thermoplasty in severe asthmatics at 5 years: The PAS2 study. By Dr. G. Chupp, et al.
Significant spirometric transitions and preserved ratio-impaired spirometry (PRISm) among ever-smokers. By Dr. E. Wan, et al.
Addressing advance care planning in patients with COPD. By Dr. E. Rose, et al.
The cost of ARDS: A systematic review. By Dr. P. Boucher, et al.
Acute management of high- and intermediate-risk pulmonary embolism in children: A review. By Dr. C. Ross, et al.
Surgical outcomes for early-stage non-small cell lung cancer at facilities with stereotactic body radiation therapy programs. By Dr. Y. Syed, et al.
Nonphysician practitioner (NPP) billing for evaluation and management (E/M) and critical care services: A sea change now in effect!
In the 2022 Medicare Physician Fee Schedule, the Centers for Medicare and Medicaid Services (CMS) further refined E/M billing by addressing split/shared visits between nonphysician practitioners (such as nurse practitioners and physician assistants) (see https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf, pp. 65150-9).
A split/shared visit is “an E/M visit in the facility setting that is performed in part by both a physician and an NPP who are in the same group, in accordance with applicable laws and regulations.” CMS recognized team-based care increased utilization of NPPs in the inpatient setting, typically under physician supervision rather than completely independent NPP practice. NPP-physician team-based care is widely prevalent on critical care, hospitalist, and specialty consultation services.
These new changes from CMS went into effect January 1, 2022. CMS now mandates the practitioner providing the “substantive portion” of the service must bill for the service. For the past 20 years, the substantive portion was largely defined by medical decision making (MDM): the physician often spent less face-to-face and/or non-face-to-face time than the NPP, but the physician could bill for the service based on MDM including a nuanced synthesis of data, and final approvals or revisions to decisions on additional evaluation and treatment. Beginning January 1, 2023, CMS will no longer define MDM as the substantive portion of the visit “because MDM is not necessarily quantifiable and can depend on patient characteristics (for example, risk).” Thus, CMS will define the “substantive portion” of the visit as the practitioner who spent >50% of the total of both face-to-face and non-face-to-face time, on the calendar day. 2022 is a transitional year allowing “the practitioner who spends more than half of the total time, or performs the history, exam, or MDM to be considered to have performed the substantive portion and can bill for the split (or shared) E/M visit.” During 2022, the visit level can be chosen based on MDM or time. In 2023, the visit level can still be chosen based upon MDM, but the billing provider is determined by who performed the “substantive portion” of the visit, which will be exclusively based upon which provider spent the most amount of time.
During 2022, when billing based on time, the practitioner spending the most time (the NPP or the physician) dictates who will be the billing provider. Alternatively, billing based on the substantive portion of the visit allows billing by the provider (NPP or physician) who completely performs the key component (history, physical examination, or medical decision making) that determines the level of the visit. With the new documentation guidelines, MDM is the only key component that can determine the visit level in the office setting. In 2023, only time-based billing will be in effect for choosing the billing provider in the inpatient hospital setting. Most importantly, time-based billing is already the only method for determining the billing provider for billing critical care services, based on the provider (NPP or physician) with the greater individual total of time.
This change represents a major shift in reimbursement for physician-NPP teams. Many physician compensation plans are based on a work relative value unit (wRVU) system. This time-based billing may shift attribution to the NPP and, thereby, disadvantage the physicians working with NPPs as they will no longer receive wRVU credit for team-based care delivery. This shift demands we all reexamine our compensation models, and how organizations attribute work value across their providers (both NPPs and physicians), with special consideration for how to credit physicians for their essential supervision of team-based care delivered and now billed by NPPs. Ideally, options for revising compensation models without changing the care delivery model would preserve the essential partnership between physicians and NPPs.
*The CHEST Health Policy and Advocacy Work Group includes Nikki Augustyn, Geoffrey D. Bass, MD, Jamie Cummings, Ian Nathanson, MD, FCCP, Emily Petraglia, Gulshan Sharma, MD, FCCP, Kelly Shriner, and John E. Studdard, MD, FCCP.
In the 2022 Medicare Physician Fee Schedule, the Centers for Medicare and Medicaid Services (CMS) further refined E/M billing by addressing split/shared visits between nonphysician practitioners (such as nurse practitioners and physician assistants) (see https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf, pp. 65150-9).
A split/shared visit is “an E/M visit in the facility setting that is performed in part by both a physician and an NPP who are in the same group, in accordance with applicable laws and regulations.” CMS recognized team-based care increased utilization of NPPs in the inpatient setting, typically under physician supervision rather than completely independent NPP practice. NPP-physician team-based care is widely prevalent on critical care, hospitalist, and specialty consultation services.
These new changes from CMS went into effect January 1, 2022. CMS now mandates the practitioner providing the “substantive portion” of the service must bill for the service. For the past 20 years, the substantive portion was largely defined by medical decision making (MDM): the physician often spent less face-to-face and/or non-face-to-face time than the NPP, but the physician could bill for the service based on MDM including a nuanced synthesis of data, and final approvals or revisions to decisions on additional evaluation and treatment. Beginning January 1, 2023, CMS will no longer define MDM as the substantive portion of the visit “because MDM is not necessarily quantifiable and can depend on patient characteristics (for example, risk).” Thus, CMS will define the “substantive portion” of the visit as the practitioner who spent >50% of the total of both face-to-face and non-face-to-face time, on the calendar day. 2022 is a transitional year allowing “the practitioner who spends more than half of the total time, or performs the history, exam, or MDM to be considered to have performed the substantive portion and can bill for the split (or shared) E/M visit.” During 2022, the visit level can be chosen based on MDM or time. In 2023, the visit level can still be chosen based upon MDM, but the billing provider is determined by who performed the “substantive portion” of the visit, which will be exclusively based upon which provider spent the most amount of time.
During 2022, when billing based on time, the practitioner spending the most time (the NPP or the physician) dictates who will be the billing provider. Alternatively, billing based on the substantive portion of the visit allows billing by the provider (NPP or physician) who completely performs the key component (history, physical examination, or medical decision making) that determines the level of the visit. With the new documentation guidelines, MDM is the only key component that can determine the visit level in the office setting. In 2023, only time-based billing will be in effect for choosing the billing provider in the inpatient hospital setting. Most importantly, time-based billing is already the only method for determining the billing provider for billing critical care services, based on the provider (NPP or physician) with the greater individual total of time.
This change represents a major shift in reimbursement for physician-NPP teams. Many physician compensation plans are based on a work relative value unit (wRVU) system. This time-based billing may shift attribution to the NPP and, thereby, disadvantage the physicians working with NPPs as they will no longer receive wRVU credit for team-based care delivery. This shift demands we all reexamine our compensation models, and how organizations attribute work value across their providers (both NPPs and physicians), with special consideration for how to credit physicians for their essential supervision of team-based care delivered and now billed by NPPs. Ideally, options for revising compensation models without changing the care delivery model would preserve the essential partnership between physicians and NPPs.
*The CHEST Health Policy and Advocacy Work Group includes Nikki Augustyn, Geoffrey D. Bass, MD, Jamie Cummings, Ian Nathanson, MD, FCCP, Emily Petraglia, Gulshan Sharma, MD, FCCP, Kelly Shriner, and John E. Studdard, MD, FCCP.
In the 2022 Medicare Physician Fee Schedule, the Centers for Medicare and Medicaid Services (CMS) further refined E/M billing by addressing split/shared visits between nonphysician practitioners (such as nurse practitioners and physician assistants) (see https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf, pp. 65150-9).
A split/shared visit is “an E/M visit in the facility setting that is performed in part by both a physician and an NPP who are in the same group, in accordance with applicable laws and regulations.” CMS recognized team-based care increased utilization of NPPs in the inpatient setting, typically under physician supervision rather than completely independent NPP practice. NPP-physician team-based care is widely prevalent on critical care, hospitalist, and specialty consultation services.
These new changes from CMS went into effect January 1, 2022. CMS now mandates the practitioner providing the “substantive portion” of the service must bill for the service. For the past 20 years, the substantive portion was largely defined by medical decision making (MDM): the physician often spent less face-to-face and/or non-face-to-face time than the NPP, but the physician could bill for the service based on MDM including a nuanced synthesis of data, and final approvals or revisions to decisions on additional evaluation and treatment. Beginning January 1, 2023, CMS will no longer define MDM as the substantive portion of the visit “because MDM is not necessarily quantifiable and can depend on patient characteristics (for example, risk).” Thus, CMS will define the “substantive portion” of the visit as the practitioner who spent >50% of the total of both face-to-face and non-face-to-face time, on the calendar day. 2022 is a transitional year allowing “the practitioner who spends more than half of the total time, or performs the history, exam, or MDM to be considered to have performed the substantive portion and can bill for the split (or shared) E/M visit.” During 2022, the visit level can be chosen based on MDM or time. In 2023, the visit level can still be chosen based upon MDM, but the billing provider is determined by who performed the “substantive portion” of the visit, which will be exclusively based upon which provider spent the most amount of time.
During 2022, when billing based on time, the practitioner spending the most time (the NPP or the physician) dictates who will be the billing provider. Alternatively, billing based on the substantive portion of the visit allows billing by the provider (NPP or physician) who completely performs the key component (history, physical examination, or medical decision making) that determines the level of the visit. With the new documentation guidelines, MDM is the only key component that can determine the visit level in the office setting. In 2023, only time-based billing will be in effect for choosing the billing provider in the inpatient hospital setting. Most importantly, time-based billing is already the only method for determining the billing provider for billing critical care services, based on the provider (NPP or physician) with the greater individual total of time.
This change represents a major shift in reimbursement for physician-NPP teams. Many physician compensation plans are based on a work relative value unit (wRVU) system. This time-based billing may shift attribution to the NPP and, thereby, disadvantage the physicians working with NPPs as they will no longer receive wRVU credit for team-based care delivery. This shift demands we all reexamine our compensation models, and how organizations attribute work value across their providers (both NPPs and physicians), with special consideration for how to credit physicians for their essential supervision of team-based care delivered and now billed by NPPs. Ideally, options for revising compensation models without changing the care delivery model would preserve the essential partnership between physicians and NPPs.
*The CHEST Health Policy and Advocacy Work Group includes Nikki Augustyn, Geoffrey D. Bass, MD, Jamie Cummings, Ian Nathanson, MD, FCCP, Emily Petraglia, Gulshan Sharma, MD, FCCP, Kelly Shriner, and John E. Studdard, MD, FCCP.
Past President’s perspective
It’s January 1, 2022, as I write, and my CHEST presidency came to an end last night as the fireworks lit up the sky. With COVID-19 waxing and waning across the United States and around the world, I have been a wartime president. CHEST has not been able to do a number of the things that we would normally have done in person, including that there has not been an in-person CHEST annual meeting during my entire presidency. We have, nonetheless, achieved some important things that I will share with you.
If you’re a typical CHEST member, you probably don’t spend a lot of time wondering about CHEST’s finances, nor should you. Nevertheless, CHEST – your organization – does have to be fiscally responsible if we desire to continue our educational and research missions, and that is the job of your Board of Regents, your presidents, and your professional staff at the CHEST headquarters. I’m happy to tell you that your organization is in healthy financial condition, in spite of a challenging economic environment and, being forced into remote, online annual meetings and board reviews for 2 years. What that means to us and to you is that we get to maintain and improve our full array of educational activities, including our annual meeting, our journal, our board reviews, our hands-on courses at the CHEST headquarters, and our web content. And, we get to accelerate our advocacy activities for our patients and for the clinical folks who care for them (us!). CHEST is primed for emerging from this pandemic stronger, because we have had to make the most of every dollar we have, and more innovative, because that’s how we have done it. We are ready for new ways of interacting and for innovative new ways of delivering education, sponsoring research, fostering networking, and leading in the clinical arena of chest medicine.
During my time as CHEST President, many of us have become progressively more aware of the blatant inequities that continue in society – and, yes, even in medicine. Perhaps more than anything, it both saddens and angers me when anyone values or devalues someone else’s life because of the color of their skin, who they feel attracted to or love, the sex they were born with or their knowledge that nature gave them the wrong physical characteristics for their gender, what physical impairments they have, where they were born, where they were educated - or not, what language is their first language, or what opportunities they were presented with in their lives. Everyone deserves the opportunity to be who and what they are and to be respected for who they are, and everyone deserves the opportunity to excel. The strongest collaborations have diverse constituents with unified goals, and I want for CHEST to be among the strongest of professional collaborations. It has been deeply important to me during my presidency to champion these values, and we have worked hard to make CHEST an inclusive and diverse organization. Much remains to be done, but we did make some good progress this year.
We established a spirometry working group to look at the science around race-based adjustments for normal values, to call out if there are mistakes or omissions in that approach, and to propose the work that needs to be done to correct them. We invited the American Thoracic Society and the Canadian Thoracic Society to join us in this effort. Race is a social construct, not a physiologic principle, and some data suggest that apparent differences in physiology could actually reflect differences in socioeconomic status of study participants. In similar work, our nephrology colleagues demonstrated that apparent differences in normal glomerular filtration rate (GFR) are related to socio-economic and health care access issues; they called for labs to no longer report race-based norms for creatinine and GFR values. Our colleagues believe that race-based GFR norms have harmed patients by promoting delay in treatments aimed at preventing dialysis or by causing delays in the initiation of dialysis. In our world, asbestos companies have argued that African American and other populations of color should receive lower asbestosis settlements on the basis that they began with lower predicted lung function and, therefore, had been less damaged by exposure to asbestos. I am very interested to see our working group’s output. I think it could result in landmark changes in our evaluation and treatment of patients with lung diseases.
A very important undertaking for us this year was a top to bottom analysis of our own practices around diversity, equity, and inclusion. We started by taking lessons from the CHEST Foundation-sponsored listening tour across the nation. Many of our patients of color lack adequate access to the care they need, which informs our efforts in advocacy and health policy. We also learned that, as a profession, we have not earned the trust of our patients of color, and we must take steps to remedy that. CHEST began this effort by developing the First 5 Minutes program, which teaches all of us how to take the first moments of our interactions with patients to enhance our empathy and to establish trusting relationships with them. You will hear more about this program in the months to come.
CHEST is dedicated to ensuring that all of our members have equitable opportunities to take part in our learning activities, both as participants and as developers. Likewise, we want any member who desires to advance in our organization to have wide open opportunity to develop and use their skills. We hired a consulting firm who specializes in aiding nonprofits with their diversity, equity, and inclusion goals to help us find our weaknesses in that area. They spent several months interviewing members at all stages of their careers and in a variety of job types, with the goal of determining what it is like to be a CHEST member of color, a woman, a member of the LGBTQIA community, or a member of any group that has been made to feel “other.” We are currently working to turn their findings into concrete steps to make CHEST the most diverse and inclusive medical society possible. Finally, our consultants are helping us to ensure that the people we hire to work for our organization full time have equitable opportunities in their workplace, and that CHEST headquarters feels inclusive and is diverse for them.
COVID-19 rages on. In fact, daily case numbers at this writing are skyrocketing, higher than at any time during the pandemic, and hospitalization rates, while lower than with some of the previous waves, are following. Many of us are stressed, and in many of our ICUs, we have fewer nurses than we did at the outset of the pandemic. The CHEST COVID-19 task force continues on the job, though, with fresh content to match the current circumstances. These dedicated individuals, who I recognized with a Presidential Citation for 2021, have worked since the early days of the pandemic to scour the literature and the landscape to find the right data and the right experts to inform the topical infographics, reviews, webinars, and podcasts that are freely available to all and are posted on the CHEST website. I hope that you have availed yourself of the material there, and, if not, you have missed some valuable learning opportunities. Missed them in real time, that is; they are all on the site for you to use at will. We are optimistic that someday soon, there will be less of a need for the COVID-19 task force, but the members are all ready to continue their work until that time comes..
I’ve highlighted just a few of the higher profile things that CHEST achieved in 2021. It would be impossible for me to cover all that CHEST has accomplished this past year. My sources tell me that during my presidency, we generated, signed on, or declined to join nearly 100 advocacy statements on topics ranging from recall of home CPAP machines to access to appropriate supplemental oxygen for patients with interstitial lung disease, to the acquisition of a nebulizer company by a tobacco company. We held successful board review sessions and repeated our all online, yet interactive, version of the CHEST annual meeting, with more than 4,000 total attendees– not as large as an in-person meeting, but not terribly far off, either. I will add that our program chairs and their committee pivoted from a meeting in Vancouver to a meeting in Orlando to, with only 6 weeks’ notice, a meeting in the ether. We are fortunate to have worked with such talented and dedicated individuals, and all of us owe them a lot for their efforts.
If, as I say, I have been a wartime president, then the worldwide viral pandemic that directly affects those of us in chest medicine has been the war. In spite of the current tsunami of cases, I am optimistic that the war ends relatively soon. CHEST will not simply return to normalcy, though. Dr. David Schulman, a brilliant and innovative educator, has taken the leadership reins of the organization, and I foresee exhilarating times ahead.
We are making it through a challenging environment, and CHEST is stronger for it. I will look forward to seeing all of you in Nashville, when we, at long last, can look one another in the eye, shake one another’s hand, and enjoy the experience of the CHEST annual meeting together. And if you don’t mind me asking, when you see me in Nashville, will you please do exactly that?
It’s January 1, 2022, as I write, and my CHEST presidency came to an end last night as the fireworks lit up the sky. With COVID-19 waxing and waning across the United States and around the world, I have been a wartime president. CHEST has not been able to do a number of the things that we would normally have done in person, including that there has not been an in-person CHEST annual meeting during my entire presidency. We have, nonetheless, achieved some important things that I will share with you.
If you’re a typical CHEST member, you probably don’t spend a lot of time wondering about CHEST’s finances, nor should you. Nevertheless, CHEST – your organization – does have to be fiscally responsible if we desire to continue our educational and research missions, and that is the job of your Board of Regents, your presidents, and your professional staff at the CHEST headquarters. I’m happy to tell you that your organization is in healthy financial condition, in spite of a challenging economic environment and, being forced into remote, online annual meetings and board reviews for 2 years. What that means to us and to you is that we get to maintain and improve our full array of educational activities, including our annual meeting, our journal, our board reviews, our hands-on courses at the CHEST headquarters, and our web content. And, we get to accelerate our advocacy activities for our patients and for the clinical folks who care for them (us!). CHEST is primed for emerging from this pandemic stronger, because we have had to make the most of every dollar we have, and more innovative, because that’s how we have done it. We are ready for new ways of interacting and for innovative new ways of delivering education, sponsoring research, fostering networking, and leading in the clinical arena of chest medicine.
During my time as CHEST President, many of us have become progressively more aware of the blatant inequities that continue in society – and, yes, even in medicine. Perhaps more than anything, it both saddens and angers me when anyone values or devalues someone else’s life because of the color of their skin, who they feel attracted to or love, the sex they were born with or their knowledge that nature gave them the wrong physical characteristics for their gender, what physical impairments they have, where they were born, where they were educated - or not, what language is their first language, or what opportunities they were presented with in their lives. Everyone deserves the opportunity to be who and what they are and to be respected for who they are, and everyone deserves the opportunity to excel. The strongest collaborations have diverse constituents with unified goals, and I want for CHEST to be among the strongest of professional collaborations. It has been deeply important to me during my presidency to champion these values, and we have worked hard to make CHEST an inclusive and diverse organization. Much remains to be done, but we did make some good progress this year.
We established a spirometry working group to look at the science around race-based adjustments for normal values, to call out if there are mistakes or omissions in that approach, and to propose the work that needs to be done to correct them. We invited the American Thoracic Society and the Canadian Thoracic Society to join us in this effort. Race is a social construct, not a physiologic principle, and some data suggest that apparent differences in physiology could actually reflect differences in socioeconomic status of study participants. In similar work, our nephrology colleagues demonstrated that apparent differences in normal glomerular filtration rate (GFR) are related to socio-economic and health care access issues; they called for labs to no longer report race-based norms for creatinine and GFR values. Our colleagues believe that race-based GFR norms have harmed patients by promoting delay in treatments aimed at preventing dialysis or by causing delays in the initiation of dialysis. In our world, asbestos companies have argued that African American and other populations of color should receive lower asbestosis settlements on the basis that they began with lower predicted lung function and, therefore, had been less damaged by exposure to asbestos. I am very interested to see our working group’s output. I think it could result in landmark changes in our evaluation and treatment of patients with lung diseases.
A very important undertaking for us this year was a top to bottom analysis of our own practices around diversity, equity, and inclusion. We started by taking lessons from the CHEST Foundation-sponsored listening tour across the nation. Many of our patients of color lack adequate access to the care they need, which informs our efforts in advocacy and health policy. We also learned that, as a profession, we have not earned the trust of our patients of color, and we must take steps to remedy that. CHEST began this effort by developing the First 5 Minutes program, which teaches all of us how to take the first moments of our interactions with patients to enhance our empathy and to establish trusting relationships with them. You will hear more about this program in the months to come.
CHEST is dedicated to ensuring that all of our members have equitable opportunities to take part in our learning activities, both as participants and as developers. Likewise, we want any member who desires to advance in our organization to have wide open opportunity to develop and use their skills. We hired a consulting firm who specializes in aiding nonprofits with their diversity, equity, and inclusion goals to help us find our weaknesses in that area. They spent several months interviewing members at all stages of their careers and in a variety of job types, with the goal of determining what it is like to be a CHEST member of color, a woman, a member of the LGBTQIA community, or a member of any group that has been made to feel “other.” We are currently working to turn their findings into concrete steps to make CHEST the most diverse and inclusive medical society possible. Finally, our consultants are helping us to ensure that the people we hire to work for our organization full time have equitable opportunities in their workplace, and that CHEST headquarters feels inclusive and is diverse for them.
COVID-19 rages on. In fact, daily case numbers at this writing are skyrocketing, higher than at any time during the pandemic, and hospitalization rates, while lower than with some of the previous waves, are following. Many of us are stressed, and in many of our ICUs, we have fewer nurses than we did at the outset of the pandemic. The CHEST COVID-19 task force continues on the job, though, with fresh content to match the current circumstances. These dedicated individuals, who I recognized with a Presidential Citation for 2021, have worked since the early days of the pandemic to scour the literature and the landscape to find the right data and the right experts to inform the topical infographics, reviews, webinars, and podcasts that are freely available to all and are posted on the CHEST website. I hope that you have availed yourself of the material there, and, if not, you have missed some valuable learning opportunities. Missed them in real time, that is; they are all on the site for you to use at will. We are optimistic that someday soon, there will be less of a need for the COVID-19 task force, but the members are all ready to continue their work until that time comes..
I’ve highlighted just a few of the higher profile things that CHEST achieved in 2021. It would be impossible for me to cover all that CHEST has accomplished this past year. My sources tell me that during my presidency, we generated, signed on, or declined to join nearly 100 advocacy statements on topics ranging from recall of home CPAP machines to access to appropriate supplemental oxygen for patients with interstitial lung disease, to the acquisition of a nebulizer company by a tobacco company. We held successful board review sessions and repeated our all online, yet interactive, version of the CHEST annual meeting, with more than 4,000 total attendees– not as large as an in-person meeting, but not terribly far off, either. I will add that our program chairs and their committee pivoted from a meeting in Vancouver to a meeting in Orlando to, with only 6 weeks’ notice, a meeting in the ether. We are fortunate to have worked with such talented and dedicated individuals, and all of us owe them a lot for their efforts.
If, as I say, I have been a wartime president, then the worldwide viral pandemic that directly affects those of us in chest medicine has been the war. In spite of the current tsunami of cases, I am optimistic that the war ends relatively soon. CHEST will not simply return to normalcy, though. Dr. David Schulman, a brilliant and innovative educator, has taken the leadership reins of the organization, and I foresee exhilarating times ahead.
We are making it through a challenging environment, and CHEST is stronger for it. I will look forward to seeing all of you in Nashville, when we, at long last, can look one another in the eye, shake one another’s hand, and enjoy the experience of the CHEST annual meeting together. And if you don’t mind me asking, when you see me in Nashville, will you please do exactly that?
It’s January 1, 2022, as I write, and my CHEST presidency came to an end last night as the fireworks lit up the sky. With COVID-19 waxing and waning across the United States and around the world, I have been a wartime president. CHEST has not been able to do a number of the things that we would normally have done in person, including that there has not been an in-person CHEST annual meeting during my entire presidency. We have, nonetheless, achieved some important things that I will share with you.
If you’re a typical CHEST member, you probably don’t spend a lot of time wondering about CHEST’s finances, nor should you. Nevertheless, CHEST – your organization – does have to be fiscally responsible if we desire to continue our educational and research missions, and that is the job of your Board of Regents, your presidents, and your professional staff at the CHEST headquarters. I’m happy to tell you that your organization is in healthy financial condition, in spite of a challenging economic environment and, being forced into remote, online annual meetings and board reviews for 2 years. What that means to us and to you is that we get to maintain and improve our full array of educational activities, including our annual meeting, our journal, our board reviews, our hands-on courses at the CHEST headquarters, and our web content. And, we get to accelerate our advocacy activities for our patients and for the clinical folks who care for them (us!). CHEST is primed for emerging from this pandemic stronger, because we have had to make the most of every dollar we have, and more innovative, because that’s how we have done it. We are ready for new ways of interacting and for innovative new ways of delivering education, sponsoring research, fostering networking, and leading in the clinical arena of chest medicine.
During my time as CHEST President, many of us have become progressively more aware of the blatant inequities that continue in society – and, yes, even in medicine. Perhaps more than anything, it both saddens and angers me when anyone values or devalues someone else’s life because of the color of their skin, who they feel attracted to or love, the sex they were born with or their knowledge that nature gave them the wrong physical characteristics for their gender, what physical impairments they have, where they were born, where they were educated - or not, what language is their first language, or what opportunities they were presented with in their lives. Everyone deserves the opportunity to be who and what they are and to be respected for who they are, and everyone deserves the opportunity to excel. The strongest collaborations have diverse constituents with unified goals, and I want for CHEST to be among the strongest of professional collaborations. It has been deeply important to me during my presidency to champion these values, and we have worked hard to make CHEST an inclusive and diverse organization. Much remains to be done, but we did make some good progress this year.
We established a spirometry working group to look at the science around race-based adjustments for normal values, to call out if there are mistakes or omissions in that approach, and to propose the work that needs to be done to correct them. We invited the American Thoracic Society and the Canadian Thoracic Society to join us in this effort. Race is a social construct, not a physiologic principle, and some data suggest that apparent differences in physiology could actually reflect differences in socioeconomic status of study participants. In similar work, our nephrology colleagues demonstrated that apparent differences in normal glomerular filtration rate (GFR) are related to socio-economic and health care access issues; they called for labs to no longer report race-based norms for creatinine and GFR values. Our colleagues believe that race-based GFR norms have harmed patients by promoting delay in treatments aimed at preventing dialysis or by causing delays in the initiation of dialysis. In our world, asbestos companies have argued that African American and other populations of color should receive lower asbestosis settlements on the basis that they began with lower predicted lung function and, therefore, had been less damaged by exposure to asbestos. I am very interested to see our working group’s output. I think it could result in landmark changes in our evaluation and treatment of patients with lung diseases.
A very important undertaking for us this year was a top to bottom analysis of our own practices around diversity, equity, and inclusion. We started by taking lessons from the CHEST Foundation-sponsored listening tour across the nation. Many of our patients of color lack adequate access to the care they need, which informs our efforts in advocacy and health policy. We also learned that, as a profession, we have not earned the trust of our patients of color, and we must take steps to remedy that. CHEST began this effort by developing the First 5 Minutes program, which teaches all of us how to take the first moments of our interactions with patients to enhance our empathy and to establish trusting relationships with them. You will hear more about this program in the months to come.
CHEST is dedicated to ensuring that all of our members have equitable opportunities to take part in our learning activities, both as participants and as developers. Likewise, we want any member who desires to advance in our organization to have wide open opportunity to develop and use their skills. We hired a consulting firm who specializes in aiding nonprofits with their diversity, equity, and inclusion goals to help us find our weaknesses in that area. They spent several months interviewing members at all stages of their careers and in a variety of job types, with the goal of determining what it is like to be a CHEST member of color, a woman, a member of the LGBTQIA community, or a member of any group that has been made to feel “other.” We are currently working to turn their findings into concrete steps to make CHEST the most diverse and inclusive medical society possible. Finally, our consultants are helping us to ensure that the people we hire to work for our organization full time have equitable opportunities in their workplace, and that CHEST headquarters feels inclusive and is diverse for them.
COVID-19 rages on. In fact, daily case numbers at this writing are skyrocketing, higher than at any time during the pandemic, and hospitalization rates, while lower than with some of the previous waves, are following. Many of us are stressed, and in many of our ICUs, we have fewer nurses than we did at the outset of the pandemic. The CHEST COVID-19 task force continues on the job, though, with fresh content to match the current circumstances. These dedicated individuals, who I recognized with a Presidential Citation for 2021, have worked since the early days of the pandemic to scour the literature and the landscape to find the right data and the right experts to inform the topical infographics, reviews, webinars, and podcasts that are freely available to all and are posted on the CHEST website. I hope that you have availed yourself of the material there, and, if not, you have missed some valuable learning opportunities. Missed them in real time, that is; they are all on the site for you to use at will. We are optimistic that someday soon, there will be less of a need for the COVID-19 task force, but the members are all ready to continue their work until that time comes..
I’ve highlighted just a few of the higher profile things that CHEST achieved in 2021. It would be impossible for me to cover all that CHEST has accomplished this past year. My sources tell me that during my presidency, we generated, signed on, or declined to join nearly 100 advocacy statements on topics ranging from recall of home CPAP machines to access to appropriate supplemental oxygen for patients with interstitial lung disease, to the acquisition of a nebulizer company by a tobacco company. We held successful board review sessions and repeated our all online, yet interactive, version of the CHEST annual meeting, with more than 4,000 total attendees– not as large as an in-person meeting, but not terribly far off, either. I will add that our program chairs and their committee pivoted from a meeting in Vancouver to a meeting in Orlando to, with only 6 weeks’ notice, a meeting in the ether. We are fortunate to have worked with such talented and dedicated individuals, and all of us owe them a lot for their efforts.
If, as I say, I have been a wartime president, then the worldwide viral pandemic that directly affects those of us in chest medicine has been the war. In spite of the current tsunami of cases, I am optimistic that the war ends relatively soon. CHEST will not simply return to normalcy, though. Dr. David Schulman, a brilliant and innovative educator, has taken the leadership reins of the organization, and I foresee exhilarating times ahead.
We are making it through a challenging environment, and CHEST is stronger for it. I will look forward to seeing all of you in Nashville, when we, at long last, can look one another in the eye, shake one another’s hand, and enjoy the experience of the CHEST annual meeting together. And if you don’t mind me asking, when you see me in Nashville, will you please do exactly that?
Optimal NIV Medicare access promotion – a hopeful way forward for users of NIV
Use of positive airway pressure (PAP) devices for treatment of sleep apnea was first described in 1981. Subsequent use of PAP devices expanded to treat patients with respiratory failure. While the treatment in this population has rapidly gained widespread use and undoubtedly has reduced morbidity and mortality in these populations, policies governing these prescriptions have not really kept up with the burgeoning need.
In 2020, Drs. Peter Gay and Robert Owens brought together a technical expert panel (TEP) to systematically review the CMS policies with an eye to remove “regulatory barriers” to improve access for these patients with the mantra: “the right device gets to the right patient at the right time.”
The panel focused on “Optimal NIV Medicare Access Promotion (ONMAP),” and members with specific expertise were recruited for five patient groups: Thoracic Restrictive Disorders (TRD), COPD, Central Sleep Apnea (CSA), Hypoventilation Syndromes (HVS), and Obstructive Sleep Apnea (OSA). Each group reviewed the current coverage, outlined the deficiencies, and suggested revisions. Herein, I will briefly highlight each group’s most important points.
TRD: The goal for this group was to bring the US standards of care closer to the rest of the world. This group advocates that the start of noninvasive ventilation (NIV) should be substantially earlier, to provide the largest improvement in disease outcome and stability. Other prominent features submitted included arterial blood gases (ABG) to not be the only form of CO2 measurement allowed; paying for a second device if patients are using NIV continuously; qualification for a BiPAP to include if vital capacity is ≤ 80%; and, to obtain a home mechanical ventilator, a patient must either fail BiPAP or have extreme loss of function, high pressure requirements, or need mouthpiece ventilation.
CSA: The big challenges with this diagnosis related to qualifying coverage language in the current policies, which are confusing for many providers. Additionally, these policies often deny certain PAP devices and/or oxygen therapy. The group proposed: a single definition of CSA; eliminate discussion of hypoventilation; mirror qualifying symptoms, and, continuing coverage, to the same as that for OSA treatment; and remove need for a prior failure of BiPAP without a backup rate (BUR). The group also had specific recommendations for when oxygen therapy should be covered in patients with CSA.
COPD: This group also focused on the oxygen therapy and promoting use of devices with a BUR. Two problematic areas included the requirement that nocturnal oxygen saturation must drop to ≤ 88% for at least 5 cumulative minutes, and, that patients must begin with an S mode device (no BUR) for at least 2 months and can only then be prescribed a device with a BUR if CO2 fails to drop. The group advocates for the removal of both, the need for a nocturnal oximetry test, and, to “try” an S mode device. The panel advocated giving the prescribing physician discretion in making this determination. The panel also provided recommendations on when a home mechanical ventilator (HMV) should be considered instead of BiPAP therapy.
HVS: Hypoventilation syndromes are a heterogeneous group of disorders with hypercapnia, defined as a Paco2 ≥45 mm Hg. This panel noted that the current coverage criteria are outdated and fail to recognize the spectrum of disease severity and advances in technology, which often leads to circumvention by prescribing more costly home mechanical ventilators (HMV). Consistent with the TRD group, this panel recommended acceptance of surrogate noninvasive end tidal and transcutaneous Pco2 and venous blood gases in lieu of arterial blood gases. Additionally, they suggested no longer requiring CO2 measures while using prescribed oxygen; eliminating the need for a sleep study to avoid delays in care for patients being discharged from the hospital; removing spirometry as a requirement; and no longer a failure of BiPAP without a BUR.
OSA: The initial purpose of examining OSA in this process was to examine when BiPAP should be utilized for treatment; however, it necessitated examination of the entire policy for PAP. The areas that were identified as needing revision included: expansion of the symptom list for patients with OSA; revising the “4 hour rule,” suggesting that 2 hours has been proven to provide benefit; eliminating the need for another sleep study to re-qualify for PAP or supplemental oxygen; and embracing telehealth as a way to improve accessibility for follow-up visits.
For details, please review the papers published in the November 2021 issue of the journal CHEST® (2021; 160[5]:1579-1990, e377-e543).
We now await what CMS will do with our recommendations and work for “the right device to the right patient at the right time.”
Acknowledgment: Drs. Gerald Criner, Nicholas Hill, Babak Mohklesi, Timothy Morgenthaler, and Lisa Wolfe assisted with the content.
Use of positive airway pressure (PAP) devices for treatment of sleep apnea was first described in 1981. Subsequent use of PAP devices expanded to treat patients with respiratory failure. While the treatment in this population has rapidly gained widespread use and undoubtedly has reduced morbidity and mortality in these populations, policies governing these prescriptions have not really kept up with the burgeoning need.
In 2020, Drs. Peter Gay and Robert Owens brought together a technical expert panel (TEP) to systematically review the CMS policies with an eye to remove “regulatory barriers” to improve access for these patients with the mantra: “the right device gets to the right patient at the right time.”
The panel focused on “Optimal NIV Medicare Access Promotion (ONMAP),” and members with specific expertise were recruited for five patient groups: Thoracic Restrictive Disorders (TRD), COPD, Central Sleep Apnea (CSA), Hypoventilation Syndromes (HVS), and Obstructive Sleep Apnea (OSA). Each group reviewed the current coverage, outlined the deficiencies, and suggested revisions. Herein, I will briefly highlight each group’s most important points.
TRD: The goal for this group was to bring the US standards of care closer to the rest of the world. This group advocates that the start of noninvasive ventilation (NIV) should be substantially earlier, to provide the largest improvement in disease outcome and stability. Other prominent features submitted included arterial blood gases (ABG) to not be the only form of CO2 measurement allowed; paying for a second device if patients are using NIV continuously; qualification for a BiPAP to include if vital capacity is ≤ 80%; and, to obtain a home mechanical ventilator, a patient must either fail BiPAP or have extreme loss of function, high pressure requirements, or need mouthpiece ventilation.
CSA: The big challenges with this diagnosis related to qualifying coverage language in the current policies, which are confusing for many providers. Additionally, these policies often deny certain PAP devices and/or oxygen therapy. The group proposed: a single definition of CSA; eliminate discussion of hypoventilation; mirror qualifying symptoms, and, continuing coverage, to the same as that for OSA treatment; and remove need for a prior failure of BiPAP without a backup rate (BUR). The group also had specific recommendations for when oxygen therapy should be covered in patients with CSA.
COPD: This group also focused on the oxygen therapy and promoting use of devices with a BUR. Two problematic areas included the requirement that nocturnal oxygen saturation must drop to ≤ 88% for at least 5 cumulative minutes, and, that patients must begin with an S mode device (no BUR) for at least 2 months and can only then be prescribed a device with a BUR if CO2 fails to drop. The group advocates for the removal of both, the need for a nocturnal oximetry test, and, to “try” an S mode device. The panel advocated giving the prescribing physician discretion in making this determination. The panel also provided recommendations on when a home mechanical ventilator (HMV) should be considered instead of BiPAP therapy.
HVS: Hypoventilation syndromes are a heterogeneous group of disorders with hypercapnia, defined as a Paco2 ≥45 mm Hg. This panel noted that the current coverage criteria are outdated and fail to recognize the spectrum of disease severity and advances in technology, which often leads to circumvention by prescribing more costly home mechanical ventilators (HMV). Consistent with the TRD group, this panel recommended acceptance of surrogate noninvasive end tidal and transcutaneous Pco2 and venous blood gases in lieu of arterial blood gases. Additionally, they suggested no longer requiring CO2 measures while using prescribed oxygen; eliminating the need for a sleep study to avoid delays in care for patients being discharged from the hospital; removing spirometry as a requirement; and no longer a failure of BiPAP without a BUR.
OSA: The initial purpose of examining OSA in this process was to examine when BiPAP should be utilized for treatment; however, it necessitated examination of the entire policy for PAP. The areas that were identified as needing revision included: expansion of the symptom list for patients with OSA; revising the “4 hour rule,” suggesting that 2 hours has been proven to provide benefit; eliminating the need for another sleep study to re-qualify for PAP or supplemental oxygen; and embracing telehealth as a way to improve accessibility for follow-up visits.
For details, please review the papers published in the November 2021 issue of the journal CHEST® (2021; 160[5]:1579-1990, e377-e543).
We now await what CMS will do with our recommendations and work for “the right device to the right patient at the right time.”
Acknowledgment: Drs. Gerald Criner, Nicholas Hill, Babak Mohklesi, Timothy Morgenthaler, and Lisa Wolfe assisted with the content.
Use of positive airway pressure (PAP) devices for treatment of sleep apnea was first described in 1981. Subsequent use of PAP devices expanded to treat patients with respiratory failure. While the treatment in this population has rapidly gained widespread use and undoubtedly has reduced morbidity and mortality in these populations, policies governing these prescriptions have not really kept up with the burgeoning need.
In 2020, Drs. Peter Gay and Robert Owens brought together a technical expert panel (TEP) to systematically review the CMS policies with an eye to remove “regulatory barriers” to improve access for these patients with the mantra: “the right device gets to the right patient at the right time.”
The panel focused on “Optimal NIV Medicare Access Promotion (ONMAP),” and members with specific expertise were recruited for five patient groups: Thoracic Restrictive Disorders (TRD), COPD, Central Sleep Apnea (CSA), Hypoventilation Syndromes (HVS), and Obstructive Sleep Apnea (OSA). Each group reviewed the current coverage, outlined the deficiencies, and suggested revisions. Herein, I will briefly highlight each group’s most important points.
TRD: The goal for this group was to bring the US standards of care closer to the rest of the world. This group advocates that the start of noninvasive ventilation (NIV) should be substantially earlier, to provide the largest improvement in disease outcome and stability. Other prominent features submitted included arterial blood gases (ABG) to not be the only form of CO2 measurement allowed; paying for a second device if patients are using NIV continuously; qualification for a BiPAP to include if vital capacity is ≤ 80%; and, to obtain a home mechanical ventilator, a patient must either fail BiPAP or have extreme loss of function, high pressure requirements, or need mouthpiece ventilation.
CSA: The big challenges with this diagnosis related to qualifying coverage language in the current policies, which are confusing for many providers. Additionally, these policies often deny certain PAP devices and/or oxygen therapy. The group proposed: a single definition of CSA; eliminate discussion of hypoventilation; mirror qualifying symptoms, and, continuing coverage, to the same as that for OSA treatment; and remove need for a prior failure of BiPAP without a backup rate (BUR). The group also had specific recommendations for when oxygen therapy should be covered in patients with CSA.
COPD: This group also focused on the oxygen therapy and promoting use of devices with a BUR. Two problematic areas included the requirement that nocturnal oxygen saturation must drop to ≤ 88% for at least 5 cumulative minutes, and, that patients must begin with an S mode device (no BUR) for at least 2 months and can only then be prescribed a device with a BUR if CO2 fails to drop. The group advocates for the removal of both, the need for a nocturnal oximetry test, and, to “try” an S mode device. The panel advocated giving the prescribing physician discretion in making this determination. The panel also provided recommendations on when a home mechanical ventilator (HMV) should be considered instead of BiPAP therapy.
HVS: Hypoventilation syndromes are a heterogeneous group of disorders with hypercapnia, defined as a Paco2 ≥45 mm Hg. This panel noted that the current coverage criteria are outdated and fail to recognize the spectrum of disease severity and advances in technology, which often leads to circumvention by prescribing more costly home mechanical ventilators (HMV). Consistent with the TRD group, this panel recommended acceptance of surrogate noninvasive end tidal and transcutaneous Pco2 and venous blood gases in lieu of arterial blood gases. Additionally, they suggested no longer requiring CO2 measures while using prescribed oxygen; eliminating the need for a sleep study to avoid delays in care for patients being discharged from the hospital; removing spirometry as a requirement; and no longer a failure of BiPAP without a BUR.
OSA: The initial purpose of examining OSA in this process was to examine when BiPAP should be utilized for treatment; however, it necessitated examination of the entire policy for PAP. The areas that were identified as needing revision included: expansion of the symptom list for patients with OSA; revising the “4 hour rule,” suggesting that 2 hours has been proven to provide benefit; eliminating the need for another sleep study to re-qualify for PAP or supplemental oxygen; and embracing telehealth as a way to improve accessibility for follow-up visits.
For details, please review the papers published in the November 2021 issue of the journal CHEST® (2021; 160[5]:1579-1990, e377-e543).
We now await what CMS will do with our recommendations and work for “the right device to the right patient at the right time.”
Acknowledgment: Drs. Gerald Criner, Nicholas Hill, Babak Mohklesi, Timothy Morgenthaler, and Lisa Wolfe assisted with the content.
Meet the new CHEST Physician Editor in Chief
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.