User login
Broad cross section of clinical topics highlights NAMDRC 2020 Conference
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
NAMDRC will host its Annual Educational Conference at the Scottsdale Resort at McCormick Ranch in Scottsdale, Arizona, March 12-14, 2020, and features a wide cross section of clinical, management, and health policy issues.
The NAMDRC Educational Conference is unlike other medical conferences you have attended. Conference sessions begin early each day and conclude by 12:30 so attendees, spouses, and guests can enjoy the venue, this year in Scottsdale, Arizona. All registrants and their guests enjoy numerous complimentary meals, and speakers and corporate partners invariably linger with the attendees during receptions for those more casual opportunities for conversations and less formal Q&A.
The Program Committee has announced its plans to focus the first day of the 3-day event on lung cancer, severe asthma, and pulmonary hypertension. Speakers include Maxwell Smith, MD from the Mayo Clinic, Arizona; James Herman, MD, Co-Director of the Lung Cancer Program at UPMC, and Colleen Channick, MD, FCCP, Director of Interventional Pulmonary at UCLA Medical Center to address timely updates on lung cancer diagnosis and treatment. The morning sessions also include a presentation on severe asthma by Monica Kraft, MD, FCCP, University of Arizona; and Richard Channick, MD, Geffen School of Medicine, UCLA, examining pulmonary hypertension with a concentration on current approaches to diagnosis and treatment.
On Friday, March 13, the focus shifts from the clinical to the changing landscape in the delivery of medicine, with a concentrated focus on innovation and new tools available to guide physicians in treatment of their patients. Claibe Yarbrough, MD, National Program Director of Pulmonary, Critical Care and Sleep at the VA, University of Texas, will examine the growth of telemedicine in the ICU. Steve Peters, MD, FCCP, a past President of NAMDRC and a current Board member, will look at artificial intelligence and the future of medicine. Dr. Peters will also present a practice management update in partnership with Alan Plummer, MD, FCCP, as he addresses coding changes in the practice of pulmonary, critical care, and sleep medicine effective 2020-21.
Shifting back to a clinical focus, the Walter J. O’Donohue memorial lecture will be given by Gerald Criner, MD, FCCP, Temple University, to examine endobronchial valve therapy for emphysema. Rounding out the presentations will be luncheon speaker Susan Tanski, MD, looking at electronic nicotine delivery systems.
On Saturday, the topics turn to sleep and mechanical ventilation. Insomnia is the subject matter for Jennifer Martin, MD, Geffen School of Medicine at UCLA; Sairam Parthasarathy, MD, at the University of Arizona, will address sleep and noninvasive mechanical ventilation. And, in a corollary presentation, home mechanical ventilation is the topic for John Hansen-Flaschen, MD, FCCP, Hospital of the University of Pennsylvania.
The final morning rounds out with controversies in septic shock, Rodrigo Cartin-Ceba, MD, at the Mayo Clinic in Scottsdale, and palliative care in the ICU, Mark Edwin, also from the Mayo Clinic.
For more information about membership in NAMDRC and conference information, visit its website at www.namdrc.org.
2019 journal CHEST® impact factor update
June 27, 2019
The journal CHEST® has just been awarded an impact factor of 9.657, the highest in its history, which equates to a 26% increase over last year’s record-breaking score. CHEST is ranked 4th out of 33 journals in the Critical Care category and 5th out of 63 journals in the Respiratory System category.
Congratulations to all who contributed to this outstanding achievement.
June 27, 2019
The journal CHEST® has just been awarded an impact factor of 9.657, the highest in its history, which equates to a 26% increase over last year’s record-breaking score. CHEST is ranked 4th out of 33 journals in the Critical Care category and 5th out of 63 journals in the Respiratory System category.
Congratulations to all who contributed to this outstanding achievement.
June 27, 2019
The journal CHEST® has just been awarded an impact factor of 9.657, the highest in its history, which equates to a 26% increase over last year’s record-breaking score. CHEST is ranked 4th out of 33 journals in the Critical Care category and 5th out of 63 journals in the Respiratory System category.
Congratulations to all who contributed to this outstanding achievement.
Bronchoscopy coding and billing tips. HCV+ donors. Women and COPD. Treating penetrating trauma
Practice operations
Basic bronchoscopy coding and billing: Rules of the road
Although complex, reimbursement for bronchoscopy is based on appropriate billing, coding, and precise documentation. It is of utmost importance to have a detailed understanding of the various codes to optimize reimbursement. We understand this is a moving target and beyond the scope of this article to discuss all the specific details, so we will try to focus on “the road less travelled.”
Tip#1: When multiple techniques are performed during a bronchoscopy only one CPT® code is considered primary and fully paid while the rest are partially paid. However, there are certain CPT codes that are considered “add-ons” and, therefore, do not fall under the multiple bronchoscopy rules and are paid in full on top of the other codes.
Tip#2: When separate biopsies are performed on different sites or lesions during the same procedure, be sure to attach the Modifier 59 (distinct procedural service) code.
Tip#3: If the procedure performed was time consuming and/or difficult, attach the Modifier 22 (unusual procedural services) code as it increases the reimbursement by 20% to 25%.
Tip#4: The CPT codes for bronchoscopy with therapeutic aspiration are 31645 (initial) and 31646 (subsequent). These were revised in 2018. They are valued greater than 31622 (airway inspection).
Tip#5: Previously moderate sedation provided by the bronchoscopist was bundled in the CPT codes, but in 2017, CMS reduced the wRVUs of these codes by 0.25. This change was adapted due to the trend of billing for moderate sedation by separate providers and reflects the increased use of anesthetists in the endoscopy suite.
Different insurance companies have varying requirements regarding a lot of codes, particularly the modifiers. Therefore, physicians, hospitals, and the coders need to be aware of all the rules. Please do not hesitate to contact the Practice Operations NetWork for more information.
Salim Surani, MD, MPH, FCCP
Chair
Humayun Anjum, MD, FCCP
Vice-Chair
Additional reading:
Centers for Medicare & Medicaid Services (CMS). Fed Regist. 2017;82:52976.
Liu H, et al. JAMA. 2012;307:1178.
Nelson, ME. Chest. 2017;152:893.
Ninan N, et al. https://doi.org/10.1016/j.chest.2019.02.009
Transplant
Hepatitis C-positive donor organs and lung transplantation: Are we there yet?
The field of lung transplantation continues to be encumbered by the mismatch between organ supply and demand. Only approximately 15% of potential donor lungs are currently being used for transplantation, resulting in unacceptably high wait list mortality (17.2 deaths per 100 wait list years).
To counter this, the transplant community continues to invest in innovations such as ex vivo lung perfusion (EVLP) to increase the availability of suitable lungs for transplantation. At the same time, efforts to modify some of the existing practices are also underway. One area of interest has been the potential use of hepatitis C virus antibody positive (HCV +) donors in solid organ transplantation. Traditionally, the use of HCV + organs, especially when the donor is nucleic acid test (NAT)-positive, which indicates presence of HCV RNA, has been considered a contra-indication for solid organ transplantation. However, this has resulted in the exclusion of a significant number of potential HCV + donors (including young and otherwise healthy donor organs), the increased availability of which has been fueled by the opioid epidemic in the United States.
While kidney transplantation programs have been relatively more liberal with utilizing this subset of donors (due to requiring lesser degree of immunosuppression), heart and lung transplantation programs have shied away from this practice due to concerns for disease transmission and unfavorable outcomes, including reduced survival of the recipient (Englum BR, et al. J Heart Lung Transplant. 2016 Feb;35[2]:228).
Hepatitis C infection is one of the medical conditions for which the treatment of disease has changed substantially in the last decade. The advent of new classes of medications, direct acting antiviral agents (DAA), has ensured that a sustained virologic response (SVR), across all genotypes, is now possible in up to 98% of those who undergo treatment. Further, DAAs have a comparatively favorable pharmacokinetic profile and are well tolerated. Since the initial reports of success in the use of HCV + donor organs for lung transplantation, the results of a recently published trial lend further support to the continued use of these organs (Khan B, et al. Am J Transplant. 2017 Apr;17[4]:1129). One hundred percent of patients (n=35, 28 lung and 7 heart) who received organs from HCV + donors (NAT +) and were treated with DAA for 4 weeks (started immediately after transplantation) had an undetectable viral load and excellent graft function at 6 months posttransplantation (Woolley AE, et al. N Engl J Med. 2019 Apr 25;380[17]:1606). Similar studies with greater power and longer follow-up need to be conducted to instill greater confidence in the use of HCV + organs in potential lung recipients. In addition, ethical issues surrounding the use of HCV + organs should be carefully vetted, as the long-term outcomes regarding use of DAAs are not yet known. It is imperative that transplant centers ensure that patients who consent to receipt of HCV + organs fully comprehend the implications of doing so and have systematic posttransplant surveillance. It is also critical that ready access to the entire planned course of DAA is secured for recipients, since these agents could be cost-prohibitive in nonresearch settings. Willingness to comply with intense surveillance and therapy should also be assessed. While the notion of using HCV + donors has gained ground as a promising strategy, transplant centers have been rightfully cautious in its liberal use, until long-term outcomes are better characterized.
Anupam Kumar, MD
Fellow-in-Training Member
J. W. Awori Hayanga, MD, MPH, FCCP
Steering Committee
Women’s health
Women and COPD
While age-adjusted death rates from COPD declined for men in the US between 1999 and 2014, they did not change significantly for women. There have been increasing numbers of studies that have focused on differences in COPD risk factors and outcomes between men and women.
Health and disease are impacted by both sex and gender. Sex refers to biological differences, including chromosomal differences, sex organs, and endogenous hormone profiles. Gender refers to social and cultural differences and includes socially constructed roles and behaviors that vary across cultures and over time.
The prevalence of COPD is increasing more rapidly in women. Women are more likely to be misdiagnosed or have a delay in diagnosis (Chapman, et al. Chest. 2001;119[6]:1691). Evidence suggests that women with COPD have more exacerbations, worse health status, and greater dyspnea (Roche, et al. Respir Res. 2014;15:20; Celli, et al. Am J Respir Crit Care Med. 2011;183[3]:317). Women diagnosed with COPD are more likely to be nonsmokers, and those who smoke are more susceptible to the harmful effects of tobacco (Vestbo, et al. Am J Respir Crit Care Med. 2013;187[4]:347).
In examining differences in exacerbation risk/severity between men and women, 48% of patients with incident COPD were women. Women were 17% more likely to have a moderate/severe first disease exacerbation and shorter time from diagnosis to exacerbation. During three years of follow-up, women had higher annual rates of moderate to severe exacerbations, most pronounced in ages > 40 years to < 65 years (Stolz et al. Submitted for publication. Chest 2019).
NHLBI convened a workshop of experts to review the current understanding of sex and gender on lung disease. They concluded that sex-specific susceptibility to COPD is poorly understood, and gender-specific approaches to COPD are imperative (Han et al. Am J Respir Crit Care Med. 2018;198[7]:850).
Margaret Pisani, MD, MS, FCCP
Vice-Chair
Disaster response and global health
Treating penetrating trauma
The management of penetrating trauma is an unfortunate but all too common facet of critical care practice. A recent emphasis has been placed on the use of extremity tourniquets for hemorrhage control.
It has been embraced by organizations such as the Hartford Consensus Joint Committee, in which hemorrhage control is viewed as the critical step in eliminating preventable prehospital death, secondary only to neutralizing the threat posed by the shooter (Brinsfield et al. Bull Am Coll Surg. 2015;100(1 Suppl):24). Interestingly, a recent retrospective review of mass shootings incorporating 12 events and 139 fatalities indicated that only 20% of victims sustained an injury to an extremity, while 58% were shot in the head or chest.
Only 7% of deaths occurred in victims with potentially survivable wounds, while the vast majority of fatalities followed wounds to the chest (89%), and there were no reported events of potential survivors exsanguinating from extremity wounds (Smith et al. J Trauma Acute Care Surg. 2016; 81:86). This differs from recent military data, where the use of extremity tourniquets has been widely lauded for improving survival. The majority of military combat injuries has been due to blast injury (62%-74%), with a minority (22%-23%) due to gunshots (Eastridge et al. J Trauma Acute Care Surg. 2012;73:S431; Champion et al. J Trauma. 2003;54:S13). These data suggest that widespread use of pre-hospital extremity tourniquets for hemorrhage control in the treatment of gunshot wounds may not result in the anticipated survival improvement that has led to its widespread advocacy. Basic tenets of trauma care, such as rapid control of the airway and treatment of penetrating trauma to the thorax and abdomen, will continue to be of paramount importance.
Michael Powers, MD
Ryan Maves, MD, FCCP
Michael Tripp, MD, FCCP
Steering Committee Members
Dr. Powers is a United States military service member. This work was prepared as part of his official duties. Title 17 U.S.C. §105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Departments of the Navy, the Department of Defense, nor the U.S. Government.
Practice operations
Basic bronchoscopy coding and billing: Rules of the road
Although complex, reimbursement for bronchoscopy is based on appropriate billing, coding, and precise documentation. It is of utmost importance to have a detailed understanding of the various codes to optimize reimbursement. We understand this is a moving target and beyond the scope of this article to discuss all the specific details, so we will try to focus on “the road less travelled.”
Tip#1: When multiple techniques are performed during a bronchoscopy only one CPT® code is considered primary and fully paid while the rest are partially paid. However, there are certain CPT codes that are considered “add-ons” and, therefore, do not fall under the multiple bronchoscopy rules and are paid in full on top of the other codes.
Tip#2: When separate biopsies are performed on different sites or lesions during the same procedure, be sure to attach the Modifier 59 (distinct procedural service) code.
Tip#3: If the procedure performed was time consuming and/or difficult, attach the Modifier 22 (unusual procedural services) code as it increases the reimbursement by 20% to 25%.
Tip#4: The CPT codes for bronchoscopy with therapeutic aspiration are 31645 (initial) and 31646 (subsequent). These were revised in 2018. They are valued greater than 31622 (airway inspection).
Tip#5: Previously moderate sedation provided by the bronchoscopist was bundled in the CPT codes, but in 2017, CMS reduced the wRVUs of these codes by 0.25. This change was adapted due to the trend of billing for moderate sedation by separate providers and reflects the increased use of anesthetists in the endoscopy suite.
Different insurance companies have varying requirements regarding a lot of codes, particularly the modifiers. Therefore, physicians, hospitals, and the coders need to be aware of all the rules. Please do not hesitate to contact the Practice Operations NetWork for more information.
Salim Surani, MD, MPH, FCCP
Chair
Humayun Anjum, MD, FCCP
Vice-Chair
Additional reading:
Centers for Medicare & Medicaid Services (CMS). Fed Regist. 2017;82:52976.
Liu H, et al. JAMA. 2012;307:1178.
Nelson, ME. Chest. 2017;152:893.
Ninan N, et al. https://doi.org/10.1016/j.chest.2019.02.009
Transplant
Hepatitis C-positive donor organs and lung transplantation: Are we there yet?
The field of lung transplantation continues to be encumbered by the mismatch between organ supply and demand. Only approximately 15% of potential donor lungs are currently being used for transplantation, resulting in unacceptably high wait list mortality (17.2 deaths per 100 wait list years).
To counter this, the transplant community continues to invest in innovations such as ex vivo lung perfusion (EVLP) to increase the availability of suitable lungs for transplantation. At the same time, efforts to modify some of the existing practices are also underway. One area of interest has been the potential use of hepatitis C virus antibody positive (HCV +) donors in solid organ transplantation. Traditionally, the use of HCV + organs, especially when the donor is nucleic acid test (NAT)-positive, which indicates presence of HCV RNA, has been considered a contra-indication for solid organ transplantation. However, this has resulted in the exclusion of a significant number of potential HCV + donors (including young and otherwise healthy donor organs), the increased availability of which has been fueled by the opioid epidemic in the United States.
While kidney transplantation programs have been relatively more liberal with utilizing this subset of donors (due to requiring lesser degree of immunosuppression), heart and lung transplantation programs have shied away from this practice due to concerns for disease transmission and unfavorable outcomes, including reduced survival of the recipient (Englum BR, et al. J Heart Lung Transplant. 2016 Feb;35[2]:228).
Hepatitis C infection is one of the medical conditions for which the treatment of disease has changed substantially in the last decade. The advent of new classes of medications, direct acting antiviral agents (DAA), has ensured that a sustained virologic response (SVR), across all genotypes, is now possible in up to 98% of those who undergo treatment. Further, DAAs have a comparatively favorable pharmacokinetic profile and are well tolerated. Since the initial reports of success in the use of HCV + donor organs for lung transplantation, the results of a recently published trial lend further support to the continued use of these organs (Khan B, et al. Am J Transplant. 2017 Apr;17[4]:1129). One hundred percent of patients (n=35, 28 lung and 7 heart) who received organs from HCV + donors (NAT +) and were treated with DAA for 4 weeks (started immediately after transplantation) had an undetectable viral load and excellent graft function at 6 months posttransplantation (Woolley AE, et al. N Engl J Med. 2019 Apr 25;380[17]:1606). Similar studies with greater power and longer follow-up need to be conducted to instill greater confidence in the use of HCV + organs in potential lung recipients. In addition, ethical issues surrounding the use of HCV + organs should be carefully vetted, as the long-term outcomes regarding use of DAAs are not yet known. It is imperative that transplant centers ensure that patients who consent to receipt of HCV + organs fully comprehend the implications of doing so and have systematic posttransplant surveillance. It is also critical that ready access to the entire planned course of DAA is secured for recipients, since these agents could be cost-prohibitive in nonresearch settings. Willingness to comply with intense surveillance and therapy should also be assessed. While the notion of using HCV + donors has gained ground as a promising strategy, transplant centers have been rightfully cautious in its liberal use, until long-term outcomes are better characterized.
Anupam Kumar, MD
Fellow-in-Training Member
J. W. Awori Hayanga, MD, MPH, FCCP
Steering Committee
Women’s health
Women and COPD
While age-adjusted death rates from COPD declined for men in the US between 1999 and 2014, they did not change significantly for women. There have been increasing numbers of studies that have focused on differences in COPD risk factors and outcomes between men and women.
Health and disease are impacted by both sex and gender. Sex refers to biological differences, including chromosomal differences, sex organs, and endogenous hormone profiles. Gender refers to social and cultural differences and includes socially constructed roles and behaviors that vary across cultures and over time.
The prevalence of COPD is increasing more rapidly in women. Women are more likely to be misdiagnosed or have a delay in diagnosis (Chapman, et al. Chest. 2001;119[6]:1691). Evidence suggests that women with COPD have more exacerbations, worse health status, and greater dyspnea (Roche, et al. Respir Res. 2014;15:20; Celli, et al. Am J Respir Crit Care Med. 2011;183[3]:317). Women diagnosed with COPD are more likely to be nonsmokers, and those who smoke are more susceptible to the harmful effects of tobacco (Vestbo, et al. Am J Respir Crit Care Med. 2013;187[4]:347).
In examining differences in exacerbation risk/severity between men and women, 48% of patients with incident COPD were women. Women were 17% more likely to have a moderate/severe first disease exacerbation and shorter time from diagnosis to exacerbation. During three years of follow-up, women had higher annual rates of moderate to severe exacerbations, most pronounced in ages > 40 years to < 65 years (Stolz et al. Submitted for publication. Chest 2019).
NHLBI convened a workshop of experts to review the current understanding of sex and gender on lung disease. They concluded that sex-specific susceptibility to COPD is poorly understood, and gender-specific approaches to COPD are imperative (Han et al. Am J Respir Crit Care Med. 2018;198[7]:850).
Margaret Pisani, MD, MS, FCCP
Vice-Chair
Disaster response and global health
Treating penetrating trauma
The management of penetrating trauma is an unfortunate but all too common facet of critical care practice. A recent emphasis has been placed on the use of extremity tourniquets for hemorrhage control.
It has been embraced by organizations such as the Hartford Consensus Joint Committee, in which hemorrhage control is viewed as the critical step in eliminating preventable prehospital death, secondary only to neutralizing the threat posed by the shooter (Brinsfield et al. Bull Am Coll Surg. 2015;100(1 Suppl):24). Interestingly, a recent retrospective review of mass shootings incorporating 12 events and 139 fatalities indicated that only 20% of victims sustained an injury to an extremity, while 58% were shot in the head or chest.
Only 7% of deaths occurred in victims with potentially survivable wounds, while the vast majority of fatalities followed wounds to the chest (89%), and there were no reported events of potential survivors exsanguinating from extremity wounds (Smith et al. J Trauma Acute Care Surg. 2016; 81:86). This differs from recent military data, where the use of extremity tourniquets has been widely lauded for improving survival. The majority of military combat injuries has been due to blast injury (62%-74%), with a minority (22%-23%) due to gunshots (Eastridge et al. J Trauma Acute Care Surg. 2012;73:S431; Champion et al. J Trauma. 2003;54:S13). These data suggest that widespread use of pre-hospital extremity tourniquets for hemorrhage control in the treatment of gunshot wounds may not result in the anticipated survival improvement that has led to its widespread advocacy. Basic tenets of trauma care, such as rapid control of the airway and treatment of penetrating trauma to the thorax and abdomen, will continue to be of paramount importance.
Michael Powers, MD
Ryan Maves, MD, FCCP
Michael Tripp, MD, FCCP
Steering Committee Members
Dr. Powers is a United States military service member. This work was prepared as part of his official duties. Title 17 U.S.C. §105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Departments of the Navy, the Department of Defense, nor the U.S. Government.
Practice operations
Basic bronchoscopy coding and billing: Rules of the road
Although complex, reimbursement for bronchoscopy is based on appropriate billing, coding, and precise documentation. It is of utmost importance to have a detailed understanding of the various codes to optimize reimbursement. We understand this is a moving target and beyond the scope of this article to discuss all the specific details, so we will try to focus on “the road less travelled.”
Tip#1: When multiple techniques are performed during a bronchoscopy only one CPT® code is considered primary and fully paid while the rest are partially paid. However, there are certain CPT codes that are considered “add-ons” and, therefore, do not fall under the multiple bronchoscopy rules and are paid in full on top of the other codes.
Tip#2: When separate biopsies are performed on different sites or lesions during the same procedure, be sure to attach the Modifier 59 (distinct procedural service) code.
Tip#3: If the procedure performed was time consuming and/or difficult, attach the Modifier 22 (unusual procedural services) code as it increases the reimbursement by 20% to 25%.
Tip#4: The CPT codes for bronchoscopy with therapeutic aspiration are 31645 (initial) and 31646 (subsequent). These were revised in 2018. They are valued greater than 31622 (airway inspection).
Tip#5: Previously moderate sedation provided by the bronchoscopist was bundled in the CPT codes, but in 2017, CMS reduced the wRVUs of these codes by 0.25. This change was adapted due to the trend of billing for moderate sedation by separate providers and reflects the increased use of anesthetists in the endoscopy suite.
Different insurance companies have varying requirements regarding a lot of codes, particularly the modifiers. Therefore, physicians, hospitals, and the coders need to be aware of all the rules. Please do not hesitate to contact the Practice Operations NetWork for more information.
Salim Surani, MD, MPH, FCCP
Chair
Humayun Anjum, MD, FCCP
Vice-Chair
Additional reading:
Centers for Medicare & Medicaid Services (CMS). Fed Regist. 2017;82:52976.
Liu H, et al. JAMA. 2012;307:1178.
Nelson, ME. Chest. 2017;152:893.
Ninan N, et al. https://doi.org/10.1016/j.chest.2019.02.009
Transplant
Hepatitis C-positive donor organs and lung transplantation: Are we there yet?
The field of lung transplantation continues to be encumbered by the mismatch between organ supply and demand. Only approximately 15% of potential donor lungs are currently being used for transplantation, resulting in unacceptably high wait list mortality (17.2 deaths per 100 wait list years).
To counter this, the transplant community continues to invest in innovations such as ex vivo lung perfusion (EVLP) to increase the availability of suitable lungs for transplantation. At the same time, efforts to modify some of the existing practices are also underway. One area of interest has been the potential use of hepatitis C virus antibody positive (HCV +) donors in solid organ transplantation. Traditionally, the use of HCV + organs, especially when the donor is nucleic acid test (NAT)-positive, which indicates presence of HCV RNA, has been considered a contra-indication for solid organ transplantation. However, this has resulted in the exclusion of a significant number of potential HCV + donors (including young and otherwise healthy donor organs), the increased availability of which has been fueled by the opioid epidemic in the United States.
While kidney transplantation programs have been relatively more liberal with utilizing this subset of donors (due to requiring lesser degree of immunosuppression), heart and lung transplantation programs have shied away from this practice due to concerns for disease transmission and unfavorable outcomes, including reduced survival of the recipient (Englum BR, et al. J Heart Lung Transplant. 2016 Feb;35[2]:228).
Hepatitis C infection is one of the medical conditions for which the treatment of disease has changed substantially in the last decade. The advent of new classes of medications, direct acting antiviral agents (DAA), has ensured that a sustained virologic response (SVR), across all genotypes, is now possible in up to 98% of those who undergo treatment. Further, DAAs have a comparatively favorable pharmacokinetic profile and are well tolerated. Since the initial reports of success in the use of HCV + donor organs for lung transplantation, the results of a recently published trial lend further support to the continued use of these organs (Khan B, et al. Am J Transplant. 2017 Apr;17[4]:1129). One hundred percent of patients (n=35, 28 lung and 7 heart) who received organs from HCV + donors (NAT +) and were treated with DAA for 4 weeks (started immediately after transplantation) had an undetectable viral load and excellent graft function at 6 months posttransplantation (Woolley AE, et al. N Engl J Med. 2019 Apr 25;380[17]:1606). Similar studies with greater power and longer follow-up need to be conducted to instill greater confidence in the use of HCV + organs in potential lung recipients. In addition, ethical issues surrounding the use of HCV + organs should be carefully vetted, as the long-term outcomes regarding use of DAAs are not yet known. It is imperative that transplant centers ensure that patients who consent to receipt of HCV + organs fully comprehend the implications of doing so and have systematic posttransplant surveillance. It is also critical that ready access to the entire planned course of DAA is secured for recipients, since these agents could be cost-prohibitive in nonresearch settings. Willingness to comply with intense surveillance and therapy should also be assessed. While the notion of using HCV + donors has gained ground as a promising strategy, transplant centers have been rightfully cautious in its liberal use, until long-term outcomes are better characterized.
Anupam Kumar, MD
Fellow-in-Training Member
J. W. Awori Hayanga, MD, MPH, FCCP
Steering Committee
Women’s health
Women and COPD
While age-adjusted death rates from COPD declined for men in the US between 1999 and 2014, they did not change significantly for women. There have been increasing numbers of studies that have focused on differences in COPD risk factors and outcomes between men and women.
Health and disease are impacted by both sex and gender. Sex refers to biological differences, including chromosomal differences, sex organs, and endogenous hormone profiles. Gender refers to social and cultural differences and includes socially constructed roles and behaviors that vary across cultures and over time.
The prevalence of COPD is increasing more rapidly in women. Women are more likely to be misdiagnosed or have a delay in diagnosis (Chapman, et al. Chest. 2001;119[6]:1691). Evidence suggests that women with COPD have more exacerbations, worse health status, and greater dyspnea (Roche, et al. Respir Res. 2014;15:20; Celli, et al. Am J Respir Crit Care Med. 2011;183[3]:317). Women diagnosed with COPD are more likely to be nonsmokers, and those who smoke are more susceptible to the harmful effects of tobacco (Vestbo, et al. Am J Respir Crit Care Med. 2013;187[4]:347).
In examining differences in exacerbation risk/severity between men and women, 48% of patients with incident COPD were women. Women were 17% more likely to have a moderate/severe first disease exacerbation and shorter time from diagnosis to exacerbation. During three years of follow-up, women had higher annual rates of moderate to severe exacerbations, most pronounced in ages > 40 years to < 65 years (Stolz et al. Submitted for publication. Chest 2019).
NHLBI convened a workshop of experts to review the current understanding of sex and gender on lung disease. They concluded that sex-specific susceptibility to COPD is poorly understood, and gender-specific approaches to COPD are imperative (Han et al. Am J Respir Crit Care Med. 2018;198[7]:850).
Margaret Pisani, MD, MS, FCCP
Vice-Chair
Disaster response and global health
Treating penetrating trauma
The management of penetrating trauma is an unfortunate but all too common facet of critical care practice. A recent emphasis has been placed on the use of extremity tourniquets for hemorrhage control.
It has been embraced by organizations such as the Hartford Consensus Joint Committee, in which hemorrhage control is viewed as the critical step in eliminating preventable prehospital death, secondary only to neutralizing the threat posed by the shooter (Brinsfield et al. Bull Am Coll Surg. 2015;100(1 Suppl):24). Interestingly, a recent retrospective review of mass shootings incorporating 12 events and 139 fatalities indicated that only 20% of victims sustained an injury to an extremity, while 58% were shot in the head or chest.
Only 7% of deaths occurred in victims with potentially survivable wounds, while the vast majority of fatalities followed wounds to the chest (89%), and there were no reported events of potential survivors exsanguinating from extremity wounds (Smith et al. J Trauma Acute Care Surg. 2016; 81:86). This differs from recent military data, where the use of extremity tourniquets has been widely lauded for improving survival. The majority of military combat injuries has been due to blast injury (62%-74%), with a minority (22%-23%) due to gunshots (Eastridge et al. J Trauma Acute Care Surg. 2012;73:S431; Champion et al. J Trauma. 2003;54:S13). These data suggest that widespread use of pre-hospital extremity tourniquets for hemorrhage control in the treatment of gunshot wounds may not result in the anticipated survival improvement that has led to its widespread advocacy. Basic tenets of trauma care, such as rapid control of the airway and treatment of penetrating trauma to the thorax and abdomen, will continue to be of paramount importance.
Michael Powers, MD
Ryan Maves, MD, FCCP
Michael Tripp, MD, FCCP
Steering Committee Members
Dr. Powers is a United States military service member. This work was prepared as part of his official duties. Title 17 U.S.C. §105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Departments of the Navy, the Department of Defense, nor the U.S. Government.
From the President: IPF—Success or failure?
Last month, I attended the funeral of my uncle who died at age 88 from pulmonary fibrosis, a condition that he battled for more than a decade. Having the honor of delivering a tribute to his life during the ceremony, I included an explanation of the basics of the disease to the audience that had packed the church located in an upscale neighborhood in the Chicago suburbs.
Afterward, I wondered if medical science and we as medical providers are making any real progress in fighting this relentless fibrotic interstitial lung disease. After all, I had watched him gradually decline, first plagued by an endless nonproductive cough, then exertional dyspnea, exertional hypoxia, and followed by hypoxia at rest. Eventually, he was short of breath with moving from his bed to the bathroom – even on high flow supplemental oxygen. It was a slow, gradual process of asphyxiation.
He had every resource available to him. He was seen by the best subspecialty providers in his community and saw experts in major medical centers across the country. He had been given the seemingly usual trial of corticosteroids initially, and then for unclear reasons, several inhalers. Maybe because his doctors didn’t have much else to offer. He was then treated with pirfenidone, and later switched to nintedanib when the side effects were too much for him to handle. Lung transplant was considered and then ruled out. With more respiratory symptoms, and despite my caution against it, he even tried experimental therapy with stem cells – an unproven treatment with additional potential for untoward consequences. At that point, he considered my suggestion to hold off, shrugged, and indicated that if he had the wherewithal and means to try it, why not?
Besides watching the desperation of finding that elusive therapy that will somehow erase the progressive symptoms of shortness of breath and cough, what I realized from being on the “other side of the gurney” with a family member is that sometimes obtaining basic treatments like supplemental oxygen can be more challenging than obtaining the more expensive pharmacologic therapies. And, that having to use supplemental oxygen is like being tethered, especially if your portable oxygen delivery device is unreliable or battery power is questionable. I’ve thought about folks with lung disease who do not have a “best practice” resource that includes unlimited medical direction and access to care. What about the people who can’t afford experimental therapies, who cannot easily navigate the medical maze, or who do not have someone to phone and call to help them when their portable oxygen concentrator develops a fatal hardware error?
I pondered the reality of his illness. Yes, at some point all of us will die. But in the end, were his treatments a success? What exactly does success look like when it comes to treatment of idiopathic pulmonary fibrosis? Did we as a medical community slow down his inevitable decline in lung function? Did we make a meaningful difference? Ultimately, does it matter if someone has a better FEV1, or trek 30 feet farther on a 6-minute walk for a few more months? Maybe. Then, as I traveled with my uncle on his medical journey, I realized that, yes, even the small things really do matter, retrospectively.
I think in my uncle’s case, his eventual demise came, but only after great successes by the medical community. The inevitable was delayed for several years at a minimum. He remained comfortable. He was able to do things on his “bucket list” that he would not likely have been able to enjoy without treatment. It allowed him to take an Honor Flight to Washington, DC, to be remembered for his heroic service in the Korean War. It allowed him to attend the 150th annual convention of the American Legion last summer, as he completed his service as the Commander of his local post. On a personal and maybe more selfish level, it allowed me to be able to enjoy dinner with him on two or three occasions while visiting Chicago during CHEST business meetings at the headquarters location. How much value do we place on being able to hear a few more family stories, to watch someone who you know is going to die smile and laugh, and share memories together for what could be the final time?
Through this experience, I have been reminded to recognize that there are many small, silent victories for our medical community in the war against devastating disease. We need to celebrate even the tiny advances. The medical community did not let him down. It rallied to give him the best we could offer with the tools we had at hand. And, keeping in mind those yet to develop this condition, it’s time to keep working hard to make a difference. Whether doing basic research, creating the medications of the future to treat respiratory illness, diagnosing conditions earlier and more accurately, or providing compassionate, patient-centered care, let’s keep our focus on crushing lung disease -- a little bit at a time.
Last month, I attended the funeral of my uncle who died at age 88 from pulmonary fibrosis, a condition that he battled for more than a decade. Having the honor of delivering a tribute to his life during the ceremony, I included an explanation of the basics of the disease to the audience that had packed the church located in an upscale neighborhood in the Chicago suburbs.
Afterward, I wondered if medical science and we as medical providers are making any real progress in fighting this relentless fibrotic interstitial lung disease. After all, I had watched him gradually decline, first plagued by an endless nonproductive cough, then exertional dyspnea, exertional hypoxia, and followed by hypoxia at rest. Eventually, he was short of breath with moving from his bed to the bathroom – even on high flow supplemental oxygen. It was a slow, gradual process of asphyxiation.
He had every resource available to him. He was seen by the best subspecialty providers in his community and saw experts in major medical centers across the country. He had been given the seemingly usual trial of corticosteroids initially, and then for unclear reasons, several inhalers. Maybe because his doctors didn’t have much else to offer. He was then treated with pirfenidone, and later switched to nintedanib when the side effects were too much for him to handle. Lung transplant was considered and then ruled out. With more respiratory symptoms, and despite my caution against it, he even tried experimental therapy with stem cells – an unproven treatment with additional potential for untoward consequences. At that point, he considered my suggestion to hold off, shrugged, and indicated that if he had the wherewithal and means to try it, why not?
Besides watching the desperation of finding that elusive therapy that will somehow erase the progressive symptoms of shortness of breath and cough, what I realized from being on the “other side of the gurney” with a family member is that sometimes obtaining basic treatments like supplemental oxygen can be more challenging than obtaining the more expensive pharmacologic therapies. And, that having to use supplemental oxygen is like being tethered, especially if your portable oxygen delivery device is unreliable or battery power is questionable. I’ve thought about folks with lung disease who do not have a “best practice” resource that includes unlimited medical direction and access to care. What about the people who can’t afford experimental therapies, who cannot easily navigate the medical maze, or who do not have someone to phone and call to help them when their portable oxygen concentrator develops a fatal hardware error?
I pondered the reality of his illness. Yes, at some point all of us will die. But in the end, were his treatments a success? What exactly does success look like when it comes to treatment of idiopathic pulmonary fibrosis? Did we as a medical community slow down his inevitable decline in lung function? Did we make a meaningful difference? Ultimately, does it matter if someone has a better FEV1, or trek 30 feet farther on a 6-minute walk for a few more months? Maybe. Then, as I traveled with my uncle on his medical journey, I realized that, yes, even the small things really do matter, retrospectively.
I think in my uncle’s case, his eventual demise came, but only after great successes by the medical community. The inevitable was delayed for several years at a minimum. He remained comfortable. He was able to do things on his “bucket list” that he would not likely have been able to enjoy without treatment. It allowed him to take an Honor Flight to Washington, DC, to be remembered for his heroic service in the Korean War. It allowed him to attend the 150th annual convention of the American Legion last summer, as he completed his service as the Commander of his local post. On a personal and maybe more selfish level, it allowed me to be able to enjoy dinner with him on two or three occasions while visiting Chicago during CHEST business meetings at the headquarters location. How much value do we place on being able to hear a few more family stories, to watch someone who you know is going to die smile and laugh, and share memories together for what could be the final time?
Through this experience, I have been reminded to recognize that there are many small, silent victories for our medical community in the war against devastating disease. We need to celebrate even the tiny advances. The medical community did not let him down. It rallied to give him the best we could offer with the tools we had at hand. And, keeping in mind those yet to develop this condition, it’s time to keep working hard to make a difference. Whether doing basic research, creating the medications of the future to treat respiratory illness, diagnosing conditions earlier and more accurately, or providing compassionate, patient-centered care, let’s keep our focus on crushing lung disease -- a little bit at a time.
Last month, I attended the funeral of my uncle who died at age 88 from pulmonary fibrosis, a condition that he battled for more than a decade. Having the honor of delivering a tribute to his life during the ceremony, I included an explanation of the basics of the disease to the audience that had packed the church located in an upscale neighborhood in the Chicago suburbs.
Afterward, I wondered if medical science and we as medical providers are making any real progress in fighting this relentless fibrotic interstitial lung disease. After all, I had watched him gradually decline, first plagued by an endless nonproductive cough, then exertional dyspnea, exertional hypoxia, and followed by hypoxia at rest. Eventually, he was short of breath with moving from his bed to the bathroom – even on high flow supplemental oxygen. It was a slow, gradual process of asphyxiation.
He had every resource available to him. He was seen by the best subspecialty providers in his community and saw experts in major medical centers across the country. He had been given the seemingly usual trial of corticosteroids initially, and then for unclear reasons, several inhalers. Maybe because his doctors didn’t have much else to offer. He was then treated with pirfenidone, and later switched to nintedanib when the side effects were too much for him to handle. Lung transplant was considered and then ruled out. With more respiratory symptoms, and despite my caution against it, he even tried experimental therapy with stem cells – an unproven treatment with additional potential for untoward consequences. At that point, he considered my suggestion to hold off, shrugged, and indicated that if he had the wherewithal and means to try it, why not?
Besides watching the desperation of finding that elusive therapy that will somehow erase the progressive symptoms of shortness of breath and cough, what I realized from being on the “other side of the gurney” with a family member is that sometimes obtaining basic treatments like supplemental oxygen can be more challenging than obtaining the more expensive pharmacologic therapies. And, that having to use supplemental oxygen is like being tethered, especially if your portable oxygen delivery device is unreliable or battery power is questionable. I’ve thought about folks with lung disease who do not have a “best practice” resource that includes unlimited medical direction and access to care. What about the people who can’t afford experimental therapies, who cannot easily navigate the medical maze, or who do not have someone to phone and call to help them when their portable oxygen concentrator develops a fatal hardware error?
I pondered the reality of his illness. Yes, at some point all of us will die. But in the end, were his treatments a success? What exactly does success look like when it comes to treatment of idiopathic pulmonary fibrosis? Did we as a medical community slow down his inevitable decline in lung function? Did we make a meaningful difference? Ultimately, does it matter if someone has a better FEV1, or trek 30 feet farther on a 6-minute walk for a few more months? Maybe. Then, as I traveled with my uncle on his medical journey, I realized that, yes, even the small things really do matter, retrospectively.
I think in my uncle’s case, his eventual demise came, but only after great successes by the medical community. The inevitable was delayed for several years at a minimum. He remained comfortable. He was able to do things on his “bucket list” that he would not likely have been able to enjoy without treatment. It allowed him to take an Honor Flight to Washington, DC, to be remembered for his heroic service in the Korean War. It allowed him to attend the 150th annual convention of the American Legion last summer, as he completed his service as the Commander of his local post. On a personal and maybe more selfish level, it allowed me to be able to enjoy dinner with him on two or three occasions while visiting Chicago during CHEST business meetings at the headquarters location. How much value do we place on being able to hear a few more family stories, to watch someone who you know is going to die smile and laugh, and share memories together for what could be the final time?
Through this experience, I have been reminded to recognize that there are many small, silent victories for our medical community in the war against devastating disease. We need to celebrate even the tiny advances. The medical community did not let him down. It rallied to give him the best we could offer with the tools we had at hand. And, keeping in mind those yet to develop this condition, it’s time to keep working hard to make a difference. Whether doing basic research, creating the medications of the future to treat respiratory illness, diagnosing conditions earlier and more accurately, or providing compassionate, patient-centered care, let’s keep our focus on crushing lung disease -- a little bit at a time.
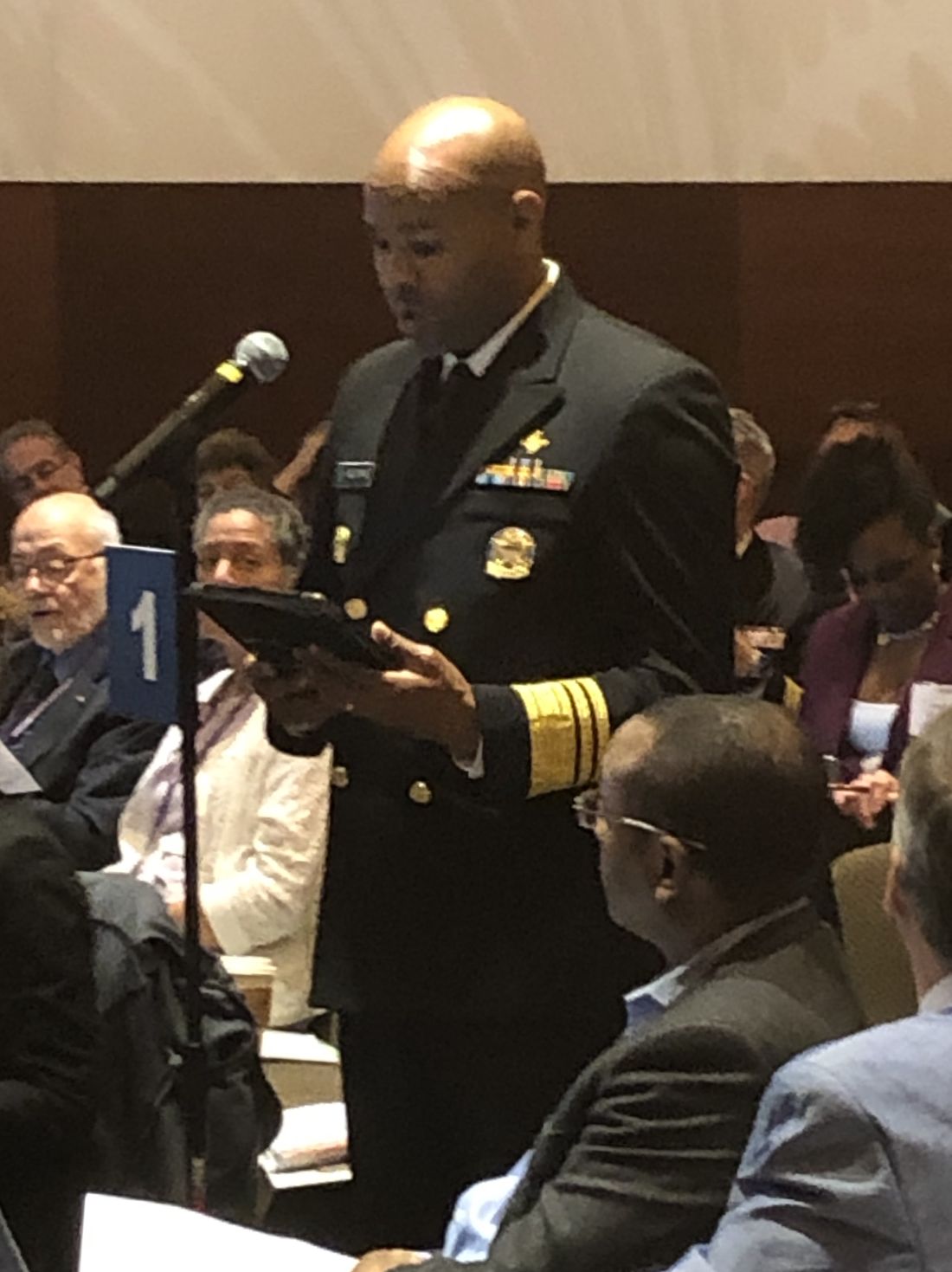
Update from AMA Annual Meeting 2019
The American Medical Association (AMA) conducted the Annual Meeting of the AMA House of Delegates from June 8-12 in Chicago. The House of Delegates (HOD) is the principal policymaking body of the AMA, consisting of more than 600 delegates and accompanying alternate delegates who represent the medical specialty societies (including CHEST); the state and territorial medical associations; the uniformed services; and other stakeholder organizations. Leading policymakers including Centers for Medicare & Medicaid Services (CMS) Administrator Seema Verma and the Surgeon General of the United States, Vice Admiral Jerome M. Adams, MD, also participated in the meeting.
This year, the delegates (CHEST has three delegate positions) considered more than 200 policy proposals (resolutions and reports) in a multi-step process: caucuses, Reference Committees, and hearings before the full House of Delegates.
The caucuses are an important first step in the HOD process. The Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met the day before the Reference Committee hearings to:
• Decide what resolutions and reports are most important to the chest diseases, critical care medicine, sleep medicine, and allergy communities;
• Determine (if possible) a unified position (support/oppose);
• Develop talking points; and
• Identify who will speak for the caucus (or as individuals if there were differing positions) at the various Reference Committee meetings.
Under the leadership of Tina Shah, MD, MPH, from the Society of Critical Care Medicine, the caucus decided to focus on 16 reports and resolutions that were slated for discussion at 7 different Reference Committees. The caucus used the GroupMe mobile, a group messaging app, to stay in touch during the meeting to ensure that someone from the caucus would be at all pertinent sessions and to communicate progress and results in real time.
The topics of the reports and resolutions selected by the Caucus for involvement included:
• Returning Liquid Oxygen to the Medicare Fee Schedule
• COPD National Action Plan
• Low Nicotine Product Standard
• Addressing the Vaping Crisis
• Regulating Liquid Nicotine and E-Cigarettes
• Put Over-the-Counter Inhaled Epinephrine Behind Pharmacy Counter
• Change in Marijuana Classification to Allow Research
• Promotion of Early Recognition and Treatment of Sepsis by Out-of-Hospital Healthcare Providers
• The Climate Change Lecture for US Medical Schools
• Physician-Assisted Suicide
• End-of-Life Care
The Reference Committees, where both AMA members and nonmembers (with permission) may testify, are organized by topic:
• Medical Service
• Legislation, Legal, and Regulatory Issues
• Medical Education
• Public Health
• Science and Technology
• AMA Governance and Finance
• Medical Practice
• Constitution and Bylaws
The Reference Committees hear testimony on each resolution, adjourn, and then meet privately (often into the wee hours) to develop recommendations to the full House. Their options include:
• Recommend Adoption
• Recommend Adoption With Amendment
• Recommend Referral (further study by one of several Councils)
• Recommend Referral for Decision (by the Board of Trustees after further study)
• Recommend for Non-Adoption
During the following 3 days, the full House of Delegates considers the Reference Committee recommendations. Any delegate may object to any recommendation and cause it to be debated and voted on by the full House of Delegates. Details about the outcomes of the 200+ resolutions are available at the AMA website (ama-assn.org).
The compendium of policies covers the entire range of topics impacting the practice of medicine – ethics, legislation, regulation, public health, individual health, and medical education among them. The full range of policies may be found in the AMA’s Policy Manual available on the AMA website (ama-assn.org).
CHEST members with an interest in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills with no cost at scores of educational sessions and will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at [email protected] for details.
Dr. Desai is with the Chicago Chest Center and Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates. Mr. Newman is the Senior Director of Strategy, Product, & Global Development at CHEST.
The American Medical Association (AMA) conducted the Annual Meeting of the AMA House of Delegates from June 8-12 in Chicago. The House of Delegates (HOD) is the principal policymaking body of the AMA, consisting of more than 600 delegates and accompanying alternate delegates who represent the medical specialty societies (including CHEST); the state and territorial medical associations; the uniformed services; and other stakeholder organizations. Leading policymakers including Centers for Medicare & Medicaid Services (CMS) Administrator Seema Verma and the Surgeon General of the United States, Vice Admiral Jerome M. Adams, MD, also participated in the meeting.
This year, the delegates (CHEST has three delegate positions) considered more than 200 policy proposals (resolutions and reports) in a multi-step process: caucuses, Reference Committees, and hearings before the full House of Delegates.
The caucuses are an important first step in the HOD process. The Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met the day before the Reference Committee hearings to:
• Decide what resolutions and reports are most important to the chest diseases, critical care medicine, sleep medicine, and allergy communities;
• Determine (if possible) a unified position (support/oppose);
• Develop talking points; and
• Identify who will speak for the caucus (or as individuals if there were differing positions) at the various Reference Committee meetings.
Under the leadership of Tina Shah, MD, MPH, from the Society of Critical Care Medicine, the caucus decided to focus on 16 reports and resolutions that were slated for discussion at 7 different Reference Committees. The caucus used the GroupMe mobile, a group messaging app, to stay in touch during the meeting to ensure that someone from the caucus would be at all pertinent sessions and to communicate progress and results in real time.
The topics of the reports and resolutions selected by the Caucus for involvement included:
• Returning Liquid Oxygen to the Medicare Fee Schedule
• COPD National Action Plan
• Low Nicotine Product Standard
• Addressing the Vaping Crisis
• Regulating Liquid Nicotine and E-Cigarettes
• Put Over-the-Counter Inhaled Epinephrine Behind Pharmacy Counter
• Change in Marijuana Classification to Allow Research
• Promotion of Early Recognition and Treatment of Sepsis by Out-of-Hospital Healthcare Providers
• The Climate Change Lecture for US Medical Schools
• Physician-Assisted Suicide
• End-of-Life Care
The Reference Committees, where both AMA members and nonmembers (with permission) may testify, are organized by topic:
• Medical Service
• Legislation, Legal, and Regulatory Issues
• Medical Education
• Public Health
• Science and Technology
• AMA Governance and Finance
• Medical Practice
• Constitution and Bylaws
The Reference Committees hear testimony on each resolution, adjourn, and then meet privately (often into the wee hours) to develop recommendations to the full House. Their options include:
• Recommend Adoption
• Recommend Adoption With Amendment
• Recommend Referral (further study by one of several Councils)
• Recommend Referral for Decision (by the Board of Trustees after further study)
• Recommend for Non-Adoption
During the following 3 days, the full House of Delegates considers the Reference Committee recommendations. Any delegate may object to any recommendation and cause it to be debated and voted on by the full House of Delegates. Details about the outcomes of the 200+ resolutions are available at the AMA website (ama-assn.org).
The compendium of policies covers the entire range of topics impacting the practice of medicine – ethics, legislation, regulation, public health, individual health, and medical education among them. The full range of policies may be found in the AMA’s Policy Manual available on the AMA website (ama-assn.org).
CHEST members with an interest in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills with no cost at scores of educational sessions and will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at [email protected] for details.
Dr. Desai is with the Chicago Chest Center and Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates. Mr. Newman is the Senior Director of Strategy, Product, & Global Development at CHEST.
The American Medical Association (AMA) conducted the Annual Meeting of the AMA House of Delegates from June 8-12 in Chicago. The House of Delegates (HOD) is the principal policymaking body of the AMA, consisting of more than 600 delegates and accompanying alternate delegates who represent the medical specialty societies (including CHEST); the state and territorial medical associations; the uniformed services; and other stakeholder organizations. Leading policymakers including Centers for Medicare & Medicaid Services (CMS) Administrator Seema Verma and the Surgeon General of the United States, Vice Admiral Jerome M. Adams, MD, also participated in the meeting.
This year, the delegates (CHEST has three delegate positions) considered more than 200 policy proposals (resolutions and reports) in a multi-step process: caucuses, Reference Committees, and hearings before the full House of Delegates.
The caucuses are an important first step in the HOD process. The Chest/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met the day before the Reference Committee hearings to:
• Decide what resolutions and reports are most important to the chest diseases, critical care medicine, sleep medicine, and allergy communities;
• Determine (if possible) a unified position (support/oppose);
• Develop talking points; and
• Identify who will speak for the caucus (or as individuals if there were differing positions) at the various Reference Committee meetings.
Under the leadership of Tina Shah, MD, MPH, from the Society of Critical Care Medicine, the caucus decided to focus on 16 reports and resolutions that were slated for discussion at 7 different Reference Committees. The caucus used the GroupMe mobile, a group messaging app, to stay in touch during the meeting to ensure that someone from the caucus would be at all pertinent sessions and to communicate progress and results in real time.
The topics of the reports and resolutions selected by the Caucus for involvement included:
• Returning Liquid Oxygen to the Medicare Fee Schedule
• COPD National Action Plan
• Low Nicotine Product Standard
• Addressing the Vaping Crisis
• Regulating Liquid Nicotine and E-Cigarettes
• Put Over-the-Counter Inhaled Epinephrine Behind Pharmacy Counter
• Change in Marijuana Classification to Allow Research
• Promotion of Early Recognition and Treatment of Sepsis by Out-of-Hospital Healthcare Providers
• The Climate Change Lecture for US Medical Schools
• Physician-Assisted Suicide
• End-of-Life Care
The Reference Committees, where both AMA members and nonmembers (with permission) may testify, are organized by topic:
• Medical Service
• Legislation, Legal, and Regulatory Issues
• Medical Education
• Public Health
• Science and Technology
• AMA Governance and Finance
• Medical Practice
• Constitution and Bylaws
The Reference Committees hear testimony on each resolution, adjourn, and then meet privately (often into the wee hours) to develop recommendations to the full House. Their options include:
• Recommend Adoption
• Recommend Adoption With Amendment
• Recommend Referral (further study by one of several Councils)
• Recommend Referral for Decision (by the Board of Trustees after further study)
• Recommend for Non-Adoption
During the following 3 days, the full House of Delegates considers the Reference Committee recommendations. Any delegate may object to any recommendation and cause it to be debated and voted on by the full House of Delegates. Details about the outcomes of the 200+ resolutions are available at the AMA website (ama-assn.org).
The compendium of policies covers the entire range of topics impacting the practice of medicine – ethics, legislation, regulation, public health, individual health, and medical education among them. The full range of policies may be found in the AMA’s Policy Manual available on the AMA website (ama-assn.org).
CHEST members with an interest in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills with no cost at scores of educational sessions and will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at [email protected] for details.
Dr. Desai is with the Chicago Chest Center and Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates. Mr. Newman is the Senior Director of Strategy, Product, & Global Development at CHEST.
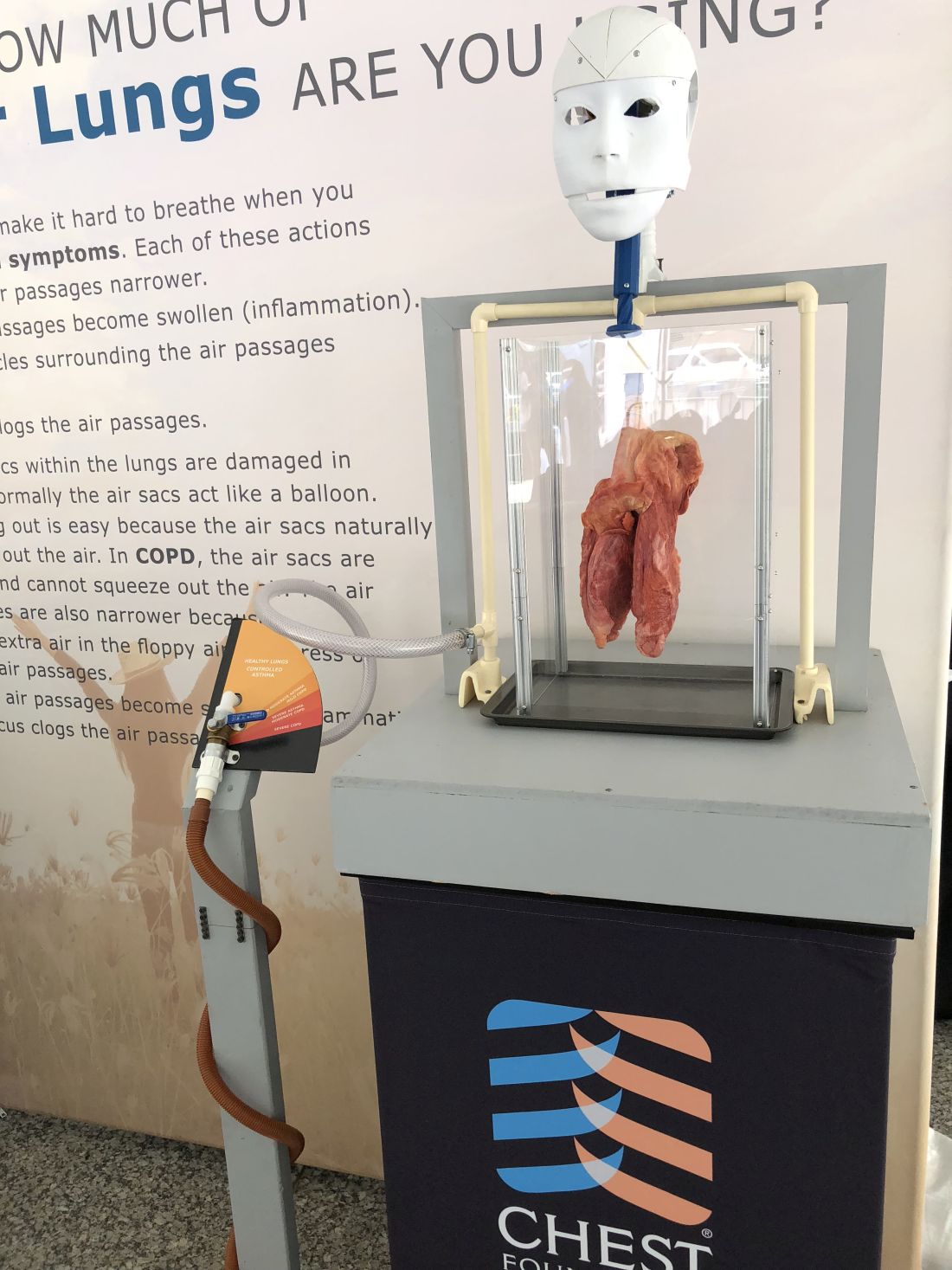
The robots are coming: How artificial intelligence will shape the future of chest medicine (and CHEST)*
The robots are coming – at least according to a report,1 which states that Google created an artificial intelligence model that was able to detect lung cancer and cut back on false-positives at a rate that beat experienced radiologists.
As a fan of Star Wars, sci-fi, and innovation, in general – I say, bring it on! It’s an exciting trend in medicine to see technology that has already changed the way we work and live enter into the world of health care. And, this is not about replacing humans either (like what occurs in a lot of sci-fi ); this technology will potentially provide clinicians with the tools they can use to improve outcomes for their patients.
The researchers for this study used a system called convolutional neural networks to study patterns in 3D CT scans. One advantage computers has over humans is that a computer can process the entire scan all at once while trained radiologists need to review individual slices of each scan to make their diagnosis.
While this technology will need more testing and large-scale trials before being used to diagnose patients’ disorders, the early results are encouraging. The researchers also picked a cancer that impacts so many of CHEST’s members and their patients. Lung cancer kills more Americans than any type of cancer while accounting for more than 25% of all cancer deaths annually.2 In a statistic that many people find shocking, lung cancer actually kills more women than breast, ovarian, and uterine cancers combined.3 Given the devastation of this disease, we can use all of the help we can get. Another positive from this study that might be overlooked is the rate of improvement for false-positive results. This could be a major benefit of both saving the time and preventing invasive treatments or attempts to confirm a diagnosis.
This news is exciting for everyone trying to (as we say at CHEST) crush lung disease, but seeing AI in medicine is not surprising, because we are already using it at CHEST. The AI projects at CHEST include analyzing the types of activities that are most beneficial to members and building predictive analytics models for a project. These were only initial forays into using this new technology. One of the even more mind-blowing developments has been rolling out natural language processing4 for our internal data reporting.
This is a new development, and much like the Google lung cancer study, we cannot tell you what the end result will be. What we can say is that it’s likely to change the way we work and provide new opportunities to create analytics solutions for our partners.
CHEST is not “just” a medical association: we are also an innovative group using the latest tools to create a better future for members, partners, and ,ultimately, patients and their families.
Mr. Jackson is CHEST Chief Innovation Officer & Vice President of Market Growth and Innovation.
References
1. https://www.statnews.com/2019/05/20/googles-ai-improves-accuracy-of-lung-cancer-diagnosis-study-shows/. Accessed July 17, 2019.
2. https://foundation.chestnet.org/patient-education-resources/lung-cancer/. Accessed July 17, 2019.
3. https://foundation.chestnet.org/wp-content/uploads/2017/01/15110313_10154723685773104_3710772562030977299_o-1.png. Accessed July 17, 2019.
4. https://www.tableau.com/products/new-features/ask-data. Accessed July 17, 2019.
*This article originally appeared as a blog July 1, 2019, on https://insights.chestnet.org/.
The robots are coming – at least according to a report,1 which states that Google created an artificial intelligence model that was able to detect lung cancer and cut back on false-positives at a rate that beat experienced radiologists.
As a fan of Star Wars, sci-fi, and innovation, in general – I say, bring it on! It’s an exciting trend in medicine to see technology that has already changed the way we work and live enter into the world of health care. And, this is not about replacing humans either (like what occurs in a lot of sci-fi ); this technology will potentially provide clinicians with the tools they can use to improve outcomes for their patients.
The researchers for this study used a system called convolutional neural networks to study patterns in 3D CT scans. One advantage computers has over humans is that a computer can process the entire scan all at once while trained radiologists need to review individual slices of each scan to make their diagnosis.
While this technology will need more testing and large-scale trials before being used to diagnose patients’ disorders, the early results are encouraging. The researchers also picked a cancer that impacts so many of CHEST’s members and their patients. Lung cancer kills more Americans than any type of cancer while accounting for more than 25% of all cancer deaths annually.2 In a statistic that many people find shocking, lung cancer actually kills more women than breast, ovarian, and uterine cancers combined.3 Given the devastation of this disease, we can use all of the help we can get. Another positive from this study that might be overlooked is the rate of improvement for false-positive results. This could be a major benefit of both saving the time and preventing invasive treatments or attempts to confirm a diagnosis.
This news is exciting for everyone trying to (as we say at CHEST) crush lung disease, but seeing AI in medicine is not surprising, because we are already using it at CHEST. The AI projects at CHEST include analyzing the types of activities that are most beneficial to members and building predictive analytics models for a project. These were only initial forays into using this new technology. One of the even more mind-blowing developments has been rolling out natural language processing4 for our internal data reporting.
This is a new development, and much like the Google lung cancer study, we cannot tell you what the end result will be. What we can say is that it’s likely to change the way we work and provide new opportunities to create analytics solutions for our partners.
CHEST is not “just” a medical association: we are also an innovative group using the latest tools to create a better future for members, partners, and ,ultimately, patients and their families.
Mr. Jackson is CHEST Chief Innovation Officer & Vice President of Market Growth and Innovation.
References
1. https://www.statnews.com/2019/05/20/googles-ai-improves-accuracy-of-lung-cancer-diagnosis-study-shows/. Accessed July 17, 2019.
2. https://foundation.chestnet.org/patient-education-resources/lung-cancer/. Accessed July 17, 2019.
3. https://foundation.chestnet.org/wp-content/uploads/2017/01/15110313_10154723685773104_3710772562030977299_o-1.png. Accessed July 17, 2019.
4. https://www.tableau.com/products/new-features/ask-data. Accessed July 17, 2019.
*This article originally appeared as a blog July 1, 2019, on https://insights.chestnet.org/.
The robots are coming – at least according to a report,1 which states that Google created an artificial intelligence model that was able to detect lung cancer and cut back on false-positives at a rate that beat experienced radiologists.
As a fan of Star Wars, sci-fi, and innovation, in general – I say, bring it on! It’s an exciting trend in medicine to see technology that has already changed the way we work and live enter into the world of health care. And, this is not about replacing humans either (like what occurs in a lot of sci-fi ); this technology will potentially provide clinicians with the tools they can use to improve outcomes for their patients.
The researchers for this study used a system called convolutional neural networks to study patterns in 3D CT scans. One advantage computers has over humans is that a computer can process the entire scan all at once while trained radiologists need to review individual slices of each scan to make their diagnosis.
While this technology will need more testing and large-scale trials before being used to diagnose patients’ disorders, the early results are encouraging. The researchers also picked a cancer that impacts so many of CHEST’s members and their patients. Lung cancer kills more Americans than any type of cancer while accounting for more than 25% of all cancer deaths annually.2 In a statistic that many people find shocking, lung cancer actually kills more women than breast, ovarian, and uterine cancers combined.3 Given the devastation of this disease, we can use all of the help we can get. Another positive from this study that might be overlooked is the rate of improvement for false-positive results. This could be a major benefit of both saving the time and preventing invasive treatments or attempts to confirm a diagnosis.
This news is exciting for everyone trying to (as we say at CHEST) crush lung disease, but seeing AI in medicine is not surprising, because we are already using it at CHEST. The AI projects at CHEST include analyzing the types of activities that are most beneficial to members and building predictive analytics models for a project. These were only initial forays into using this new technology. One of the even more mind-blowing developments has been rolling out natural language processing4 for our internal data reporting.
This is a new development, and much like the Google lung cancer study, we cannot tell you what the end result will be. What we can say is that it’s likely to change the way we work and provide new opportunities to create analytics solutions for our partners.
CHEST is not “just” a medical association: we are also an innovative group using the latest tools to create a better future for members, partners, and ,ultimately, patients and their families.
Mr. Jackson is CHEST Chief Innovation Officer & Vice President of Market Growth and Innovation.
References
1. https://www.statnews.com/2019/05/20/googles-ai-improves-accuracy-of-lung-cancer-diagnosis-study-shows/. Accessed July 17, 2019.
2. https://foundation.chestnet.org/patient-education-resources/lung-cancer/. Accessed July 17, 2019.
3. https://foundation.chestnet.org/wp-content/uploads/2017/01/15110313_10154723685773104_3710772562030977299_o-1.png. Accessed July 17, 2019.
4. https://www.tableau.com/products/new-features/ask-data. Accessed July 17, 2019.
*This article originally appeared as a blog July 1, 2019, on https://insights.chestnet.org/.
This month in the journal CHEST®
Editor’s Picks
COMMENTARY
Imaging of Pulmonary Hypertension: Pictorial Essay
By Dr. E. Altschul, et al.
ORIGINAL RESEARCH
Epidemiology of Quick Sequential Organ Failure Assessment Criteria in Undifferentiated Patients and Association With Suspected Infection and Sepsis
By Dr. V. Anand, et al.
Infectious Disease Hospitalizations: United States, 2001 to 2014
By Dr. J. L. Kennedy, et al.
Overdiagnosis of COPD in Subjects With Unobstructed Spirometry: A BOLD Analysis
By Dr. L. Sator, et al.
TRANSLATING BASIC RESEARCH INTO CLINICAL PRACTICE
Common Pathogenic Mechanisms Between Idiopathic Pulmonary Fibrosis and Lung Cancer
By Dr. A. Tzouvelekis, et al.
Editor’s Picks
Editor’s Picks
COMMENTARY
Imaging of Pulmonary Hypertension: Pictorial Essay
By Dr. E. Altschul, et al.
ORIGINAL RESEARCH
Epidemiology of Quick Sequential Organ Failure Assessment Criteria in Undifferentiated Patients and Association With Suspected Infection and Sepsis
By Dr. V. Anand, et al.
Infectious Disease Hospitalizations: United States, 2001 to 2014
By Dr. J. L. Kennedy, et al.
Overdiagnosis of COPD in Subjects With Unobstructed Spirometry: A BOLD Analysis
By Dr. L. Sator, et al.
TRANSLATING BASIC RESEARCH INTO CLINICAL PRACTICE
Common Pathogenic Mechanisms Between Idiopathic Pulmonary Fibrosis and Lung Cancer
By Dr. A. Tzouvelekis, et al.
COMMENTARY
Imaging of Pulmonary Hypertension: Pictorial Essay
By Dr. E. Altschul, et al.
ORIGINAL RESEARCH
Epidemiology of Quick Sequential Organ Failure Assessment Criteria in Undifferentiated Patients and Association With Suspected Infection and Sepsis
By Dr. V. Anand, et al.
Infectious Disease Hospitalizations: United States, 2001 to 2014
By Dr. J. L. Kennedy, et al.
Overdiagnosis of COPD in Subjects With Unobstructed Spirometry: A BOLD Analysis
By Dr. L. Sator, et al.
TRANSLATING BASIC RESEARCH INTO CLINICAL PRACTICE
Common Pathogenic Mechanisms Between Idiopathic Pulmonary Fibrosis and Lung Cancer
By Dr. A. Tzouvelekis, et al.
Your CHEST board working for you
The CHEST Board of Regents (BOR) held their summer meeting for 3 days starting June 20 in Coeur D’Alene, Idaho. The key drivers of the BOR are to continuously assess and adjust our strategic plan to further CHEST’s mission and to be good fiducial stewards in allocating resources. At this meeting, the BOR continued its efforts in both of these areas.
CHEST’s mission is to champion the prevention, diagnosis, and treatment of chest diseases through education, communication, and research. The budget for fiscal year 2019-2020 facilitates the expansion of this mission by allocating more resources for e-learning and for the improving engagement and member experience.
Specifically, the Board is placing significant emphasis for more content to be digital, downloadable, digestible, and (hopefully) addictive. Aside from allocating capital for updates of existing equipment, Board Designated Funds were made available for an aggressive redesign of content delivery. Over the next 2 years, CHEST will achieve single sign on for all our learning platforms; enhance mobile access; and deploy mobile apps for gaming, personalized learning, and just-in-time education. The effort also aims to streamline journal and topic workflows and launch personalized content recommendations for our members.
Our formal strategic planning continued with an external review of our recent environmental scan and 5- year plan by a select group of entrepreneurs and innovators. Board members engaged in a rich debate about ways to better focus the organization. The group noted that the best time for strategic initiatives is now, while the association is doing well and highly functioning, rather than waiting for difficult times to initiate a potentially more painful course correction.
Education is the base for our entire enterprise. The BOR had a vigorous discussion about the development of a clinician educator track with certification and was introduced to CHEST’s new Chief Learning Officer. The CHEST staff plans a deeper dive into needs assessment and developing a business plan around this program.
Communication is also a core part of our mission. The BOR recognizes that more needs to be done to support the NetWorks. For this year’s annual meeting, plans have been made to move the NetWork meetings into two time slots, unopposed by other scientific content, and to rename these meetings “NetWork Featured Lecture and Open Forum.” The rationale for the name change is to make the meetings more inviting by referring to them as “open forums.” CHEST 2019 will feature improved signage in common areas to highlight the NetWork meetings, providing times and locations. The goal is to at least double attendance. Dr. Stephanie Levine, President-Elect of CHEST, is forming a task force to explore other ways of enhancing NetWork engagement.
In order to expand CHEST educational impact, the Board launched a new global events strategy. These global educational programs were another focus of the Board of Regents. Staff provided updates on the CHEST Congress Thailand 2019 in collaboration with the Thoracic Society of Thailand. There were more than 1,000 delegates representing 57 countries. The meeting was supported by our partner, Kenes, which will also be helping with smaller regional meetings, including the June meeting in Athens in collaboration with the Hellenic Thoracic Society. CHEST is in the advanced stages of planning a CHEST Congress in Bologna, Italy, in summer 2020 in conjunction with our colleagues in that country. CHEST is putting together a 5-year plan for regional meetings with a variety of local medical societies throughout the world. To support this, the Governance Committee recommended augmenting the Council of Global Governors with an Executive Committee. This group will serve as a small, strategic set of individuals, appointed by the Governance Committee, to assist in furthering the global strategy and efforts of the organization. Going forward, the Chair of the Executive Committee will serve as a member of the Board of Regents for a 2-year term, to better represent international concerns at a board level.
The BOR addressed additional items, including reviewing the process for selecting Master FCCPs and a very positive update on our CHEST 2019 meeting in New Orleans. They also enhanced coordination with the CHEST Foundation Board of Trustees (BOT) via joint meetings. The CHEST Foundation BOT celebrated success in matching funds for the one million dollar grant to establish the Erin Popovich Endowment. Additional fundraising plans include holding five separate events in the next year, including a repeat of last year’s Feldman Family Foundation Poker Night.
The CHEST Board of Regents (BOR) held their summer meeting for 3 days starting June 20 in Coeur D’Alene, Idaho. The key drivers of the BOR are to continuously assess and adjust our strategic plan to further CHEST’s mission and to be good fiducial stewards in allocating resources. At this meeting, the BOR continued its efforts in both of these areas.
CHEST’s mission is to champion the prevention, diagnosis, and treatment of chest diseases through education, communication, and research. The budget for fiscal year 2019-2020 facilitates the expansion of this mission by allocating more resources for e-learning and for the improving engagement and member experience.
Specifically, the Board is placing significant emphasis for more content to be digital, downloadable, digestible, and (hopefully) addictive. Aside from allocating capital for updates of existing equipment, Board Designated Funds were made available for an aggressive redesign of content delivery. Over the next 2 years, CHEST will achieve single sign on for all our learning platforms; enhance mobile access; and deploy mobile apps for gaming, personalized learning, and just-in-time education. The effort also aims to streamline journal and topic workflows and launch personalized content recommendations for our members.
Our formal strategic planning continued with an external review of our recent environmental scan and 5- year plan by a select group of entrepreneurs and innovators. Board members engaged in a rich debate about ways to better focus the organization. The group noted that the best time for strategic initiatives is now, while the association is doing well and highly functioning, rather than waiting for difficult times to initiate a potentially more painful course correction.
Education is the base for our entire enterprise. The BOR had a vigorous discussion about the development of a clinician educator track with certification and was introduced to CHEST’s new Chief Learning Officer. The CHEST staff plans a deeper dive into needs assessment and developing a business plan around this program.
Communication is also a core part of our mission. The BOR recognizes that more needs to be done to support the NetWorks. For this year’s annual meeting, plans have been made to move the NetWork meetings into two time slots, unopposed by other scientific content, and to rename these meetings “NetWork Featured Lecture and Open Forum.” The rationale for the name change is to make the meetings more inviting by referring to them as “open forums.” CHEST 2019 will feature improved signage in common areas to highlight the NetWork meetings, providing times and locations. The goal is to at least double attendance. Dr. Stephanie Levine, President-Elect of CHEST, is forming a task force to explore other ways of enhancing NetWork engagement.
In order to expand CHEST educational impact, the Board launched a new global events strategy. These global educational programs were another focus of the Board of Regents. Staff provided updates on the CHEST Congress Thailand 2019 in collaboration with the Thoracic Society of Thailand. There were more than 1,000 delegates representing 57 countries. The meeting was supported by our partner, Kenes, which will also be helping with smaller regional meetings, including the June meeting in Athens in collaboration with the Hellenic Thoracic Society. CHEST is in the advanced stages of planning a CHEST Congress in Bologna, Italy, in summer 2020 in conjunction with our colleagues in that country. CHEST is putting together a 5-year plan for regional meetings with a variety of local medical societies throughout the world. To support this, the Governance Committee recommended augmenting the Council of Global Governors with an Executive Committee. This group will serve as a small, strategic set of individuals, appointed by the Governance Committee, to assist in furthering the global strategy and efforts of the organization. Going forward, the Chair of the Executive Committee will serve as a member of the Board of Regents for a 2-year term, to better represent international concerns at a board level.
The BOR addressed additional items, including reviewing the process for selecting Master FCCPs and a very positive update on our CHEST 2019 meeting in New Orleans. They also enhanced coordination with the CHEST Foundation Board of Trustees (BOT) via joint meetings. The CHEST Foundation BOT celebrated success in matching funds for the one million dollar grant to establish the Erin Popovich Endowment. Additional fundraising plans include holding five separate events in the next year, including a repeat of last year’s Feldman Family Foundation Poker Night.
The CHEST Board of Regents (BOR) held their summer meeting for 3 days starting June 20 in Coeur D’Alene, Idaho. The key drivers of the BOR are to continuously assess and adjust our strategic plan to further CHEST’s mission and to be good fiducial stewards in allocating resources. At this meeting, the BOR continued its efforts in both of these areas.
CHEST’s mission is to champion the prevention, diagnosis, and treatment of chest diseases through education, communication, and research. The budget for fiscal year 2019-2020 facilitates the expansion of this mission by allocating more resources for e-learning and for the improving engagement and member experience.
Specifically, the Board is placing significant emphasis for more content to be digital, downloadable, digestible, and (hopefully) addictive. Aside from allocating capital for updates of existing equipment, Board Designated Funds were made available for an aggressive redesign of content delivery. Over the next 2 years, CHEST will achieve single sign on for all our learning platforms; enhance mobile access; and deploy mobile apps for gaming, personalized learning, and just-in-time education. The effort also aims to streamline journal and topic workflows and launch personalized content recommendations for our members.
Our formal strategic planning continued with an external review of our recent environmental scan and 5- year plan by a select group of entrepreneurs and innovators. Board members engaged in a rich debate about ways to better focus the organization. The group noted that the best time for strategic initiatives is now, while the association is doing well and highly functioning, rather than waiting for difficult times to initiate a potentially more painful course correction.
Education is the base for our entire enterprise. The BOR had a vigorous discussion about the development of a clinician educator track with certification and was introduced to CHEST’s new Chief Learning Officer. The CHEST staff plans a deeper dive into needs assessment and developing a business plan around this program.
Communication is also a core part of our mission. The BOR recognizes that more needs to be done to support the NetWorks. For this year’s annual meeting, plans have been made to move the NetWork meetings into two time slots, unopposed by other scientific content, and to rename these meetings “NetWork Featured Lecture and Open Forum.” The rationale for the name change is to make the meetings more inviting by referring to them as “open forums.” CHEST 2019 will feature improved signage in common areas to highlight the NetWork meetings, providing times and locations. The goal is to at least double attendance. Dr. Stephanie Levine, President-Elect of CHEST, is forming a task force to explore other ways of enhancing NetWork engagement.
In order to expand CHEST educational impact, the Board launched a new global events strategy. These global educational programs were another focus of the Board of Regents. Staff provided updates on the CHEST Congress Thailand 2019 in collaboration with the Thoracic Society of Thailand. There were more than 1,000 delegates representing 57 countries. The meeting was supported by our partner, Kenes, which will also be helping with smaller regional meetings, including the June meeting in Athens in collaboration with the Hellenic Thoracic Society. CHEST is in the advanced stages of planning a CHEST Congress in Bologna, Italy, in summer 2020 in conjunction with our colleagues in that country. CHEST is putting together a 5-year plan for regional meetings with a variety of local medical societies throughout the world. To support this, the Governance Committee recommended augmenting the Council of Global Governors with an Executive Committee. This group will serve as a small, strategic set of individuals, appointed by the Governance Committee, to assist in furthering the global strategy and efforts of the organization. Going forward, the Chair of the Executive Committee will serve as a member of the Board of Regents for a 2-year term, to better represent international concerns at a board level.
The BOR addressed additional items, including reviewing the process for selecting Master FCCPs and a very positive update on our CHEST 2019 meeting in New Orleans. They also enhanced coordination with the CHEST Foundation Board of Trustees (BOT) via joint meetings. The CHEST Foundation BOT celebrated success in matching funds for the one million dollar grant to establish the Erin Popovich Endowment. Additional fundraising plans include holding five separate events in the next year, including a repeat of last year’s Feldman Family Foundation Poker Night.
What’s new for CHEST 2019?
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
CHEST Foundation at Board Review
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!