User login
Nominations for Mary Edwards Walker Inspiring Women in Surgery Award due June 30
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations through Thursday, June 30, for a new annual award, the Mary Edwards Walker Inspiring Women in Surgery Award. The award, which will be presented at Clinical Congress 2016, honors the work of Mary Edwards Walker (1832-1919) the first female surgeon employed by the U.S. Army and the only woman ever to receive the Medal of Honor, the highest U.S. Armed Forces decoration for bravery.
Nominees must be ACS members, either in active practice or retired, who meet the following requirements:
• A demonstrated commitment to the advancement and inspiration of women in surgery.
• Current WiSC members are ineligible for this award.
• The awardee is expected to attend the ACS Clinical Congress 2016 in Washington, DC, to accept the award.
Nominations must include a letter of nomination outlining how the nominee has contributed to the advancement of women in surgery and the nominee’s current curriculum vitae. Self-nominations are acceptable and should include a letter of reference. E-mail all materials to Connie Bura, ACS Associate Director, Division of Member Services, at [email protected]. Contact Ms. Bura for additional information.
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations through Thursday, June 30, for a new annual award, the Mary Edwards Walker Inspiring Women in Surgery Award. The award, which will be presented at Clinical Congress 2016, honors the work of Mary Edwards Walker (1832-1919) the first female surgeon employed by the U.S. Army and the only woman ever to receive the Medal of Honor, the highest U.S. Armed Forces decoration for bravery.
Nominees must be ACS members, either in active practice or retired, who meet the following requirements:
• A demonstrated commitment to the advancement and inspiration of women in surgery.
• Current WiSC members are ineligible for this award.
• The awardee is expected to attend the ACS Clinical Congress 2016 in Washington, DC, to accept the award.
Nominations must include a letter of nomination outlining how the nominee has contributed to the advancement of women in surgery and the nominee’s current curriculum vitae. Self-nominations are acceptable and should include a letter of reference. E-mail all materials to Connie Bura, ACS Associate Director, Division of Member Services, at [email protected]. Contact Ms. Bura for additional information.
The American College of Surgeons (ACS) Women in Surgery Committee (WiSC) is accepting nominations through Thursday, June 30, for a new annual award, the Mary Edwards Walker Inspiring Women in Surgery Award. The award, which will be presented at Clinical Congress 2016, honors the work of Mary Edwards Walker (1832-1919) the first female surgeon employed by the U.S. Army and the only woman ever to receive the Medal of Honor, the highest U.S. Armed Forces decoration for bravery.
Nominees must be ACS members, either in active practice or retired, who meet the following requirements:
• A demonstrated commitment to the advancement and inspiration of women in surgery.
• Current WiSC members are ineligible for this award.
• The awardee is expected to attend the ACS Clinical Congress 2016 in Washington, DC, to accept the award.
Nominations must include a letter of nomination outlining how the nominee has contributed to the advancement of women in surgery and the nominee’s current curriculum vitae. Self-nominations are acceptable and should include a letter of reference. E-mail all materials to Connie Bura, ACS Associate Director, Division of Member Services, at [email protected]. Contact Ms. Bura for additional information.
Health Policy Scholars for 2016 selected
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
Award named in honor of Dr. Clowes available for 2017
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
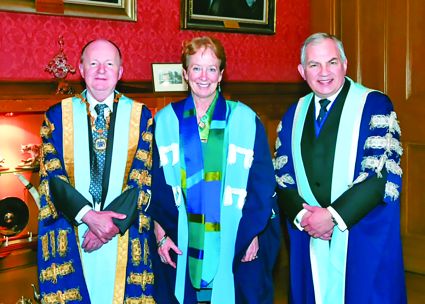
Dr. Julie Ann Freischlag inducted into Royal College of Surgeons of Edinburgh
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Drs. A. Brent Eastman, Michael Sinclair named UCSF Alumni of the Year
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
ACS announces 2016 Oweida Scholarship recipient
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
Register now for ACS NSQIP Conference, July 16−19 in San Diego, CA
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
ACGME announces FIRST trial waiver for 2016−2017
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
2016 Leadership Summit Focuses on Communication and Team Building
The American College of Surgeons (ACS) hosted the fifth annual Leadership & Advocacy Summit, April 9–12, at the JW Marriott in Washington, DC. More than 445 College leaders, residents, and medical students participated in the Leadership portion of the Summit, which featured a full day of sessions on effective leadership building communication and strategic thinking skills for effective leadership in and out of the operating room. The Leadership Summit also provided attendees with ample networking opportunities.
The Leadership Summit began with a well-attended Welcome Reception on Saturday evening. Sunday’s program featured nine presentations on such topics as preparing for difficult conversations, best practices for social networking, improving team emotional intelligence, leading teams through conflict situations, and sharpening strategic thinking skills. Leaders from the Georgia, North Texas, and West Virginia Chapters of the ACS presented their chapter’s success stories from the past year. Leadership Summit attendees also convened over lunch by state/region to identify new areas for collaboration in the coming year.
Details regarding the Leadership Summit will be published in the July Bulletin of the American College of Surgeons at http://bulletin.facs.org/. The sixth annual Leadership & Advocacy Summit will take place May 6−9, 2017 at the Renaissance Washington, DC Downtown Hotel. For more information on the Leadership Summit, contact Donna Tieberg, ACS International Chapter Services Manager, at [email protected].
The American College of Surgeons (ACS) hosted the fifth annual Leadership & Advocacy Summit, April 9–12, at the JW Marriott in Washington, DC. More than 445 College leaders, residents, and medical students participated in the Leadership portion of the Summit, which featured a full day of sessions on effective leadership building communication and strategic thinking skills for effective leadership in and out of the operating room. The Leadership Summit also provided attendees with ample networking opportunities.
The Leadership Summit began with a well-attended Welcome Reception on Saturday evening. Sunday’s program featured nine presentations on such topics as preparing for difficult conversations, best practices for social networking, improving team emotional intelligence, leading teams through conflict situations, and sharpening strategic thinking skills. Leaders from the Georgia, North Texas, and West Virginia Chapters of the ACS presented their chapter’s success stories from the past year. Leadership Summit attendees also convened over lunch by state/region to identify new areas for collaboration in the coming year.
Details regarding the Leadership Summit will be published in the July Bulletin of the American College of Surgeons at http://bulletin.facs.org/. The sixth annual Leadership & Advocacy Summit will take place May 6−9, 2017 at the Renaissance Washington, DC Downtown Hotel. For more information on the Leadership Summit, contact Donna Tieberg, ACS International Chapter Services Manager, at [email protected].
The American College of Surgeons (ACS) hosted the fifth annual Leadership & Advocacy Summit, April 9–12, at the JW Marriott in Washington, DC. More than 445 College leaders, residents, and medical students participated in the Leadership portion of the Summit, which featured a full day of sessions on effective leadership building communication and strategic thinking skills for effective leadership in and out of the operating room. The Leadership Summit also provided attendees with ample networking opportunities.
The Leadership Summit began with a well-attended Welcome Reception on Saturday evening. Sunday’s program featured nine presentations on such topics as preparing for difficult conversations, best practices for social networking, improving team emotional intelligence, leading teams through conflict situations, and sharpening strategic thinking skills. Leaders from the Georgia, North Texas, and West Virginia Chapters of the ACS presented their chapter’s success stories from the past year. Leadership Summit attendees also convened over lunch by state/region to identify new areas for collaboration in the coming year.
Details regarding the Leadership Summit will be published in the July Bulletin of the American College of Surgeons at http://bulletin.facs.org/. The sixth annual Leadership & Advocacy Summit will take place May 6−9, 2017 at the Renaissance Washington, DC Downtown Hotel. For more information on the Leadership Summit, contact Donna Tieberg, ACS International Chapter Services Manager, at [email protected].
Survey: Civilians support wider access to education on how to help victims of mass casualty events
Many civilians have expressed interest in taking a bleeding control training course that would empower them to immediately assist victims of active shooter and other intentional mass casualty events at the point of wounding, according to the results of a national poll published in the Journal of the American College of Surgeons (JACS). Furthermore, most civilians support training and equipping police officers to perform severe bleeding control on victims as soon as possible, rather than wait for emergency medical services (EMS) personnel to arrive on the scene. Survey respondents also supported the placement of bleeding control kits in public places where large crowds gather, similar to the way that automatic external defibrillators are now found in airports and shopping malls.
Working to save lives
The Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass Casualty and Active Shooter Events, convened by the American College of Surgeons, recommends careful consideration of these study results. The committee’s deliberations are known as the Hartford Consensus™. The Hartford Consensus reports have been published in the Bulletin and JACS since the group’s formation in 2013 and promote the group’s core principle that “no one should die from uncontrolled bleeding.”
To that end, the Hartford Consensus calls for providing law enforcement officers with the training and equipment needed to act before EMS personnel arrive, providing EMS professionals with quicker access to the wounded, and training civilian bystanders to act as immediate responders. This element from the Hartford Consensus is at the heart of the “Stop the Bleed” campaign launched by the U.S. Department of Homeland Security through the National Security Council.
“We know that to save life and limb, you need to stop the bleeding very early—within five to 10 minutes—or victims can lose their lives,” said ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, Chair of the Hartford Consensus and director of the Trauma Institute at Hartford Hospital, CT. “However, until now, there has been no clear indication of how well trained the general public is in bleeding control and how willing they might be to participate as immediate responders until professionals arrive on the scene.”
Public ready and willing to act
Langer Research Associates, New York, NY, conducted a national telephone survey of the general public, November 6−11, 2015, concluding just two days before the terrorist attacks in Paris. A total of 1,051 telephone interviews were conducted—528 via cellphone and 523 via landline. Respondents were asked whether they had ever participated in first aid training, and, if so, when and whether it included bleeding control instruction. Nearly half of all respondents (47 percent) said that they had received first aid training at some point. Of that number, 13 percent had trained in first aid in the last two years and 52 percent had first aid training in the last five years.
Respondents also were asked about their willingness to provide aid to bleeding victims in two different scenarios: a car crash and a mass shooting.
Within the context of the two scenarios, the study authors reported that:
Of the 941 respondents able to provide first aid, 98 percent indicated they would be “very likely” or “somewhat likely” to attempt bleeding control on a family member with a leg wound. Within this subgroup, 62 percent indicated they would apply pressure or compression to the wound, 36 percent would apply a tourniquet, 6 percent would cover or wrap the wound in a bandage, and 2 percent would elevate the injured leg.
When presented with a scenario of trying to stop severe bleeding in a car crash victim who is unknown to them, 92 percent of a random half sample of respondents indicated they would be very likely (61 percent) or somewhat likely (31 percent) to act.
In a mass shooting scenario, 75 percent of the other random half sample responded that they would attempt to give first aid if it seemed safe to act, 16 percent responded that they would wait to see what happens, and 8 percent said they would leave the area. In terms of assisting if the situation seemed safe, 94 percent responded that they would be very likely (62 percent) or somewhat likely (32 percent) to try to help a stranger.
Many respondents reported having major or some concern about several issues related to trying to stop severe bleeding in someone whom they did not know. Specifically, respondents expressed concern about seeing someone bleeding heavily (30 percent), becoming contaminated with a disease (61 percent), endangering personal safety (43 percent), causing a victim additional pain or injury (65 percent), and being responsible for a bad outcome (61 percent). Within the context of rendering assistance in the shooting scenario, 71 percent expressed concern about “putting themselves in physical danger from additional violence.”
Respondents also were asked about their interest in taking a bleeding control class and their support for requiring bleeding control kits in public places. Among the respondents who were physically able to provide first aid, 82 percent said they would be “very interested” or “somewhat interested” in attending a two-hour bleeding control course.
In addition, 93 percent supported the public placement of bleeding control kits (containing gloves, tourniquets, and compression dressings).
The authors also noted strong public approval (91 percent of all surveyed) for training and equipping police officers for severe bleeding control to act as soon as possible before the arrival of EMS personnel, with 65 percent also supporting “faster access of EMS to victims in areas that may not be totally secure.”
“It takes internal fortitude to want to get involved as an immediate responder. We were overwhelmed to learn that the public is prepared to accept this responsibility,” Dr. Jacobs said. “Moving forward, we plan to use these new insights to develop a training program for the public, not just health care professionals, so civilians can learn how to act as immediate responders. We want to steer interested people toward getting the right training and to understand when victims are experiencing the signs of massive bleeding so they can ‘stop the bleed’ and save lives.”
Many civilians have expressed interest in taking a bleeding control training course that would empower them to immediately assist victims of active shooter and other intentional mass casualty events at the point of wounding, according to the results of a national poll published in the Journal of the American College of Surgeons (JACS). Furthermore, most civilians support training and equipping police officers to perform severe bleeding control on victims as soon as possible, rather than wait for emergency medical services (EMS) personnel to arrive on the scene. Survey respondents also supported the placement of bleeding control kits in public places where large crowds gather, similar to the way that automatic external defibrillators are now found in airports and shopping malls.
Working to save lives
The Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass Casualty and Active Shooter Events, convened by the American College of Surgeons, recommends careful consideration of these study results. The committee’s deliberations are known as the Hartford Consensus™. The Hartford Consensus reports have been published in the Bulletin and JACS since the group’s formation in 2013 and promote the group’s core principle that “no one should die from uncontrolled bleeding.”
To that end, the Hartford Consensus calls for providing law enforcement officers with the training and equipment needed to act before EMS personnel arrive, providing EMS professionals with quicker access to the wounded, and training civilian bystanders to act as immediate responders. This element from the Hartford Consensus is at the heart of the “Stop the Bleed” campaign launched by the U.S. Department of Homeland Security through the National Security Council.
“We know that to save life and limb, you need to stop the bleeding very early—within five to 10 minutes—or victims can lose their lives,” said ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, Chair of the Hartford Consensus and director of the Trauma Institute at Hartford Hospital, CT. “However, until now, there has been no clear indication of how well trained the general public is in bleeding control and how willing they might be to participate as immediate responders until professionals arrive on the scene.”
Public ready and willing to act
Langer Research Associates, New York, NY, conducted a national telephone survey of the general public, November 6−11, 2015, concluding just two days before the terrorist attacks in Paris. A total of 1,051 telephone interviews were conducted—528 via cellphone and 523 via landline. Respondents were asked whether they had ever participated in first aid training, and, if so, when and whether it included bleeding control instruction. Nearly half of all respondents (47 percent) said that they had received first aid training at some point. Of that number, 13 percent had trained in first aid in the last two years and 52 percent had first aid training in the last five years.
Respondents also were asked about their willingness to provide aid to bleeding victims in two different scenarios: a car crash and a mass shooting.
Within the context of the two scenarios, the study authors reported that:
Of the 941 respondents able to provide first aid, 98 percent indicated they would be “very likely” or “somewhat likely” to attempt bleeding control on a family member with a leg wound. Within this subgroup, 62 percent indicated they would apply pressure or compression to the wound, 36 percent would apply a tourniquet, 6 percent would cover or wrap the wound in a bandage, and 2 percent would elevate the injured leg.
When presented with a scenario of trying to stop severe bleeding in a car crash victim who is unknown to them, 92 percent of a random half sample of respondents indicated they would be very likely (61 percent) or somewhat likely (31 percent) to act.
In a mass shooting scenario, 75 percent of the other random half sample responded that they would attempt to give first aid if it seemed safe to act, 16 percent responded that they would wait to see what happens, and 8 percent said they would leave the area. In terms of assisting if the situation seemed safe, 94 percent responded that they would be very likely (62 percent) or somewhat likely (32 percent) to try to help a stranger.
Many respondents reported having major or some concern about several issues related to trying to stop severe bleeding in someone whom they did not know. Specifically, respondents expressed concern about seeing someone bleeding heavily (30 percent), becoming contaminated with a disease (61 percent), endangering personal safety (43 percent), causing a victim additional pain or injury (65 percent), and being responsible for a bad outcome (61 percent). Within the context of rendering assistance in the shooting scenario, 71 percent expressed concern about “putting themselves in physical danger from additional violence.”
Respondents also were asked about their interest in taking a bleeding control class and their support for requiring bleeding control kits in public places. Among the respondents who were physically able to provide first aid, 82 percent said they would be “very interested” or “somewhat interested” in attending a two-hour bleeding control course.
In addition, 93 percent supported the public placement of bleeding control kits (containing gloves, tourniquets, and compression dressings).
The authors also noted strong public approval (91 percent of all surveyed) for training and equipping police officers for severe bleeding control to act as soon as possible before the arrival of EMS personnel, with 65 percent also supporting “faster access of EMS to victims in areas that may not be totally secure.”
“It takes internal fortitude to want to get involved as an immediate responder. We were overwhelmed to learn that the public is prepared to accept this responsibility,” Dr. Jacobs said. “Moving forward, we plan to use these new insights to develop a training program for the public, not just health care professionals, so civilians can learn how to act as immediate responders. We want to steer interested people toward getting the right training and to understand when victims are experiencing the signs of massive bleeding so they can ‘stop the bleed’ and save lives.”
Many civilians have expressed interest in taking a bleeding control training course that would empower them to immediately assist victims of active shooter and other intentional mass casualty events at the point of wounding, according to the results of a national poll published in the Journal of the American College of Surgeons (JACS). Furthermore, most civilians support training and equipping police officers to perform severe bleeding control on victims as soon as possible, rather than wait for emergency medical services (EMS) personnel to arrive on the scene. Survey respondents also supported the placement of bleeding control kits in public places where large crowds gather, similar to the way that automatic external defibrillators are now found in airports and shopping malls.
Working to save lives
The Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass Casualty and Active Shooter Events, convened by the American College of Surgeons, recommends careful consideration of these study results. The committee’s deliberations are known as the Hartford Consensus™. The Hartford Consensus reports have been published in the Bulletin and JACS since the group’s formation in 2013 and promote the group’s core principle that “no one should die from uncontrolled bleeding.”
To that end, the Hartford Consensus calls for providing law enforcement officers with the training and equipment needed to act before EMS personnel arrive, providing EMS professionals with quicker access to the wounded, and training civilian bystanders to act as immediate responders. This element from the Hartford Consensus is at the heart of the “Stop the Bleed” campaign launched by the U.S. Department of Homeland Security through the National Security Council.
“We know that to save life and limb, you need to stop the bleeding very early—within five to 10 minutes—or victims can lose their lives,” said ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, Chair of the Hartford Consensus and director of the Trauma Institute at Hartford Hospital, CT. “However, until now, there has been no clear indication of how well trained the general public is in bleeding control and how willing they might be to participate as immediate responders until professionals arrive on the scene.”
Public ready and willing to act
Langer Research Associates, New York, NY, conducted a national telephone survey of the general public, November 6−11, 2015, concluding just two days before the terrorist attacks in Paris. A total of 1,051 telephone interviews were conducted—528 via cellphone and 523 via landline. Respondents were asked whether they had ever participated in first aid training, and, if so, when and whether it included bleeding control instruction. Nearly half of all respondents (47 percent) said that they had received first aid training at some point. Of that number, 13 percent had trained in first aid in the last two years and 52 percent had first aid training in the last five years.
Respondents also were asked about their willingness to provide aid to bleeding victims in two different scenarios: a car crash and a mass shooting.
Within the context of the two scenarios, the study authors reported that:
Of the 941 respondents able to provide first aid, 98 percent indicated they would be “very likely” or “somewhat likely” to attempt bleeding control on a family member with a leg wound. Within this subgroup, 62 percent indicated they would apply pressure or compression to the wound, 36 percent would apply a tourniquet, 6 percent would cover or wrap the wound in a bandage, and 2 percent would elevate the injured leg.
When presented with a scenario of trying to stop severe bleeding in a car crash victim who is unknown to them, 92 percent of a random half sample of respondents indicated they would be very likely (61 percent) or somewhat likely (31 percent) to act.
In a mass shooting scenario, 75 percent of the other random half sample responded that they would attempt to give first aid if it seemed safe to act, 16 percent responded that they would wait to see what happens, and 8 percent said they would leave the area. In terms of assisting if the situation seemed safe, 94 percent responded that they would be very likely (62 percent) or somewhat likely (32 percent) to try to help a stranger.
Many respondents reported having major or some concern about several issues related to trying to stop severe bleeding in someone whom they did not know. Specifically, respondents expressed concern about seeing someone bleeding heavily (30 percent), becoming contaminated with a disease (61 percent), endangering personal safety (43 percent), causing a victim additional pain or injury (65 percent), and being responsible for a bad outcome (61 percent). Within the context of rendering assistance in the shooting scenario, 71 percent expressed concern about “putting themselves in physical danger from additional violence.”
Respondents also were asked about their interest in taking a bleeding control class and their support for requiring bleeding control kits in public places. Among the respondents who were physically able to provide first aid, 82 percent said they would be “very interested” or “somewhat interested” in attending a two-hour bleeding control course.
In addition, 93 percent supported the public placement of bleeding control kits (containing gloves, tourniquets, and compression dressings).
The authors also noted strong public approval (91 percent of all surveyed) for training and equipping police officers for severe bleeding control to act as soon as possible before the arrival of EMS personnel, with 65 percent also supporting “faster access of EMS to victims in areas that may not be totally secure.”
“It takes internal fortitude to want to get involved as an immediate responder. We were overwhelmed to learn that the public is prepared to accept this responsibility,” Dr. Jacobs said. “Moving forward, we plan to use these new insights to develop a training program for the public, not just health care professionals, so civilians can learn how to act as immediate responders. We want to steer interested people toward getting the right training and to understand when victims are experiencing the signs of massive bleeding so they can ‘stop the bleed’ and save lives.”