User login
Rethinking Hospital-Associated Disability for Patients With COVID-19
Between February 1 and July 1, 2020, SARS-CoV-2 killed over 120,000 people in the United States alone. Nearly 80% of deaths occurred in those 65 years and older; by contrast, this age group constituted only 65% of deaths from influenza during the same time period.1 Though the reasons for these differences have not been completely elucidated, one thing is abundantly clear: Our nation’s oldest and most frail have been among the most likely to die of COVID-19. With an estimated mortality rate of 4.7% in the United States, we are fortunate that most infected patients survive2,3; however, many survivors require an exceptionally long hospital stay in isolation. Hospitalizations for patients with COVID-19 are distinct and confer a high risk for hospital-associated disability (HAD). HAD, defined as a new loss of ability to complete one or more activities of daily living (ADLs) without assistance after hospital discharge, occurs in approximately one-third of all hospitalized patients.4 In this perspective, we explore why HAD might be worse in patients with COVID-19 and offer new models for delivery of physical and occupational therapy to help them with functional recovery during and after hospitalization.
HOSPITAL-ASSOCIATED DISABILITY BEFORE COVID-19
Functional decline, a life-altering condition that patients experience as part of posthospital syndrome,5 is characterized by loss of mobility, cognitive decline, and HAD. The effects of functional decline can lead to a cascade of readmissions, institutionalization, and even death. During hospitalization, patients spend 87% to 100% of their time in bed. This immobilization is a major contributor to the development of HAD.6,7 The $58.5 billion dollars in yearly Medicare spending that is attributed to post–acute care also highlights the financial toll arising from such disability.8 Early mobilization with physical and occupational therapy is important to prevent HAD. However, even under normal conditions, care teams face innumerable barriers to mobilizing patients: symptomatic patients can be resistant to mobilizing during illness, providers have fears of worsening symptoms or falls, and some providers are unaware of the importance of mobilization. In patients with COVID-19, the barriers are only magnified.
HOSPITAL-ASSOCIATED DISABILITY DURING COVID-19
Given the increasing numbers of COVID-19 survivors discharged from the hospital, it is critical to consider why HAD could be an even larger problem in these patients. Consider their age, symptom burden, and illness severity: Among 5,700 patients who were admitted for COVID-19 in the New York City area, most were elderly (median age, 63 years), many were tachypneic (17%), and many required supplemental oxygen (28%).9 Fourteen percent of these patients required care in the intensive care unit (ICU), most of whom required mechanical ventilation (86%), which independently places them at higher risk of HAD. Given these severe respiratory issues in COVID-19, mobilization may cause significant discomfort. Being symptomatic is, by far, the most common reason hospitalized patients refuse to ambulate.10 As a result, this could make early mobilization for these COVID-19 patients exceptionally difficult.
Patients with COVID-19 also experience prolonged hospitalization. The median hospital length of stay (LOS) is 9.3 days for survivors of SARS-CoV-2 infection compared with the 7-day average LOS for patients with pneumonia requiring ICU admission and 5-day average LOS for patients with influenza.11-13 Complications of COVID, such as cardiac injury, critical illness polyneuropathy or myopathy, or cognitive impairment, also contribute to the significant need for rehabilitation long after recovery from the acute illness.14
Physical and occupational therapy involve prolonged close contact with patients, a known risk factor for contracting SARS-CoV-2.15 For staff, mobilizing a patient with COVID-19 takes longer due to intricate PPE donning and doffing procedures and patients requiring rest breaks because of weakness and respiratory-related recovery time. For patients who are mobilized, their activity is constrained by isolation restrictions that prohibit patients from leaving the confines of their hospital rooms. On March 23, 2020, the World Confederation for Physical Therapy (WCPT) endorsed guidelines created by the Australian Physiotherapy Association (APA) on caring for patients with COVID-19 acknowledging this risk16. The guidelines suggested that personal protective equipment (PPE) required for reducing risk of droplet transmission is appropriate for some scenarios, but they noted that exercising may induce coughing or expectoration, which could make physical therapy an aerosol-generating procedure. Therefore, the guidelines recommended that therapists wear N95 masks and recommend that direct face-to-face physical therapy should be limited to patients with certain functional limitations, including frailty, multiple comorbidities, and advanced age.
Patients with COVID-19 face additional barriers to accessing therapy services following hospital discharge. Post–acute care placement may be difficult due to limited availability of isolation rooms for patients with COVID-19 and the requirement of negative results for recovering patients. For those who manage to secure a bed, PPE shortages in nursing facilities could lead to lower prioritization of therapy interventions among staff and more bedridden days for the patients. Given social distancing restrictions, home health and outpatient therapy may not be possible for similar reasons.
The confluence of often highly symptomatic and even fragile patients, time-consuming visits with high concern for contagion, limited space to freely mobilize, and barriers to post–acute care illustrates why it is likely that COVID-19 admissions will be associated with a higher degree of HAD than admissions for other illnesses.
COVID-19: INNOVATION IN THERAPY SERVICES
The entire healthcare system has had to evolve and innovate rapidly to combat the morbidity and mortality of COVID-19. In the case of HAD, nursing staff, new billing guidelines, hospital redesign, and telemedicine are all facilitating novel ways to mobilize patients during and after hospitalization.
To limit the numbers of staff exposed to patients with COVID-19, the APA recommends engaging nursing staff in initial therapy evaluations and simple exercises that can be performed in a hospital room. Meaningful in-room exercise for some patients may include getting out of bed and walking to the bathroom to brush their teeth or complete other ADLs. Assessment of cognition should be carefully considered for discharge planning given its effects on the patient’s ability to independently participate in exercises and ADLs. For this reason, treatment and prevention of delirium or cognitive changes with interventions targeting environmental modifications, maintenance of healthy sleep-wake cycles, and orientation strategies are vital.
Therapy evaluations can also be administered remotely via phone call or video. To help facilitate telehealth visits, the Centers for Medicaid & Medicare Services has released new guidelines under the Coronavirus Aid, Relief, and Economic Security (CARES) Act. Physical and occupational therapists have been historically excluded from the list of providers able to bill for telehealth services, but the CARES Act allows physical and occupational therapists who accept Medicare part B to bill for telehealth services and e-visits. The new rule applies to patients in healthcare facilities or patients at home.17 Transitioning some physical and occupational therapy to telehealth could prove to be a critical resource for patients with COVID-19 trying to regain strength and independence during and after hospitalization.
Other solutions include converting areas of a hospital into rehabilitation units solely for patients recovering from COVID-19. Alternatively, rural hospitals, which usually run below capacity, or certain post–acute care facilities that are already prepared to manage infectious patients could serve as dedicated COVID-19 rehabilitation facilities, which can offer novel ways to continue therapy services after discharge while decreasing new exposures to COVID-19.18
Given the social isolation patients with COVID-19 experience during hospitalization, virtual group exercise classes may help for overall recovery. Most therapy companies already offer this service, and several include an app that allows therapists to monitor the patient’s exercises and progress. However, when transitioning to telemedicine, it is also important to consider the needs of those who may not be able to navigate technology effectively. For example, some elderly patients can be limited by a range of issues from poor computer skills and “technophobia” to visual and cognitive impairments. Having a friend or family member available to assist with technology should be considered. Additionally, being elderly, having lower income, or having a lower level of education makes it less likely that a patient will have access to internet or smartphones. Therefore, patients with these limitations may be poor candidates for telehealth and require post–acute care for their therapy services.19,20
CONCLUSION
With all the devastation that COVID-19 has created, it might be easy to forget the importance of physical and occupational therapy. But without this focus, the disability resulting from COVID-19 hospitalizations could inflict considerable long-lasting effects on our patients at great cost to an already strained healthcare system. Immediate changes in how we adapt and innovate these services for patients with COVID-19 are critical. It may prove to have enormous impact on patients and the healthcare system long after the worst of the virus is forgotten.
Disclosures
The authors reported having nothing to disclose.
Funding
Dr Arora is funded by National Heart, Lung and Blood Institute (NHLBI Grant K24HL136859).
1. Provisional COVID-19 Death Counts by Sex, Age, and State. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
2. Rajgor DD, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776-777. https://dx.doi.org/10.1016/S1473-3099(20)30244-9
3. Coronavirus Resource Center: Maps & Trends: Mortality Analyses. Johns Hopkins University & Medicine. Accessed April 26, 2020. https://coronavirus.jhu.edu/data/mortality
4. Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc. 2020;21(4):455-461.e5. https://doi.org/10.1016/j.jamda.2019.09.015
5. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. https://doi.org/10.1056/nejmp1212324
6. Summary Health Statistics: National Health Interview Survey, 2017. Tables P10a-P10c; p. 1-9. Centers for Disease Control and Prevention. Accessed April 26,2020. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_P-10.pdf
7. Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? a systematic review and meta-analysis. Appl Nurs Res. 2020;51:151189. https://doi.org/10.1016/j.apnr.2019.151189
8. Fact Sheet: Post-Acute Care. American Hospital Association. July 2019. Accessed April 26, 2020. https://www.aha.org/system/files/media/file/2019/07/fact-sheet-post-acute-care-0719.pdf
9. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059. https://doi.org/10.1001/jama.2020.6775
10. Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. J Hosp Med. 2007;2(5):305-313. https://doi.org/10.1002/jhm.209
11. Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ 2020;369:m1923. https://doi.org/10.1136/bmj.m1923
12. Williams S, Gousen S, DeFrances C. National Hospital Care Survey Demonstration Projects: pneumonia inpatient hospitalizations and emergency department visits. Natl Health Stat Report. 2018;(116):1-11.
13. Milenkovic M, Russo CA, Elixhauser A. Hospital Stays for Influenza, 2004: Statistical Brief #16. 2006 Oct. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed April 26, 2020 https://www.ncbi.nlm.nih.gov/books/NBK63484/
14. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470-474. https://doi.org/10.1097/phm.0000000000001443
15. Coronavirus Disease 2019 (COVID-19): Social Distancing. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
16. Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73-82. https://doi.org/10.1016/j.jphys.2020.03.011
17. COVID1-9 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services. Accessed April 23, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
18. Grabowski DC, Joynt Maddox KE. Postacute care preparedness for COVID-19: thinking ahead. JAMA. 2020;323(20):2007-2008. https://doi.org/10.1001/jama.2020.4686
19. Eung-Hun K, Stolvar A, Lober WB, et al. Challenges to using an electronic health record by a low-income elderly population. J Med Internet Res. 2009;11(4):e44. https://doi.org/10.2196/jmir.1256
20. Rajasekaran K. Access to telemedicine-are we doing all that we can during the COVID-19 pandemic? Otolaryngol Head Neck Surg. 2020;163(1):104-106. https://doi.org/10.1177/0194599820925049
Between February 1 and July 1, 2020, SARS-CoV-2 killed over 120,000 people in the United States alone. Nearly 80% of deaths occurred in those 65 years and older; by contrast, this age group constituted only 65% of deaths from influenza during the same time period.1 Though the reasons for these differences have not been completely elucidated, one thing is abundantly clear: Our nation’s oldest and most frail have been among the most likely to die of COVID-19. With an estimated mortality rate of 4.7% in the United States, we are fortunate that most infected patients survive2,3; however, many survivors require an exceptionally long hospital stay in isolation. Hospitalizations for patients with COVID-19 are distinct and confer a high risk for hospital-associated disability (HAD). HAD, defined as a new loss of ability to complete one or more activities of daily living (ADLs) without assistance after hospital discharge, occurs in approximately one-third of all hospitalized patients.4 In this perspective, we explore why HAD might be worse in patients with COVID-19 and offer new models for delivery of physical and occupational therapy to help them with functional recovery during and after hospitalization.
HOSPITAL-ASSOCIATED DISABILITY BEFORE COVID-19
Functional decline, a life-altering condition that patients experience as part of posthospital syndrome,5 is characterized by loss of mobility, cognitive decline, and HAD. The effects of functional decline can lead to a cascade of readmissions, institutionalization, and even death. During hospitalization, patients spend 87% to 100% of their time in bed. This immobilization is a major contributor to the development of HAD.6,7 The $58.5 billion dollars in yearly Medicare spending that is attributed to post–acute care also highlights the financial toll arising from such disability.8 Early mobilization with physical and occupational therapy is important to prevent HAD. However, even under normal conditions, care teams face innumerable barriers to mobilizing patients: symptomatic patients can be resistant to mobilizing during illness, providers have fears of worsening symptoms or falls, and some providers are unaware of the importance of mobilization. In patients with COVID-19, the barriers are only magnified.
HOSPITAL-ASSOCIATED DISABILITY DURING COVID-19
Given the increasing numbers of COVID-19 survivors discharged from the hospital, it is critical to consider why HAD could be an even larger problem in these patients. Consider their age, symptom burden, and illness severity: Among 5,700 patients who were admitted for COVID-19 in the New York City area, most were elderly (median age, 63 years), many were tachypneic (17%), and many required supplemental oxygen (28%).9 Fourteen percent of these patients required care in the intensive care unit (ICU), most of whom required mechanical ventilation (86%), which independently places them at higher risk of HAD. Given these severe respiratory issues in COVID-19, mobilization may cause significant discomfort. Being symptomatic is, by far, the most common reason hospitalized patients refuse to ambulate.10 As a result, this could make early mobilization for these COVID-19 patients exceptionally difficult.
Patients with COVID-19 also experience prolonged hospitalization. The median hospital length of stay (LOS) is 9.3 days for survivors of SARS-CoV-2 infection compared with the 7-day average LOS for patients with pneumonia requiring ICU admission and 5-day average LOS for patients with influenza.11-13 Complications of COVID, such as cardiac injury, critical illness polyneuropathy or myopathy, or cognitive impairment, also contribute to the significant need for rehabilitation long after recovery from the acute illness.14
Physical and occupational therapy involve prolonged close contact with patients, a known risk factor for contracting SARS-CoV-2.15 For staff, mobilizing a patient with COVID-19 takes longer due to intricate PPE donning and doffing procedures and patients requiring rest breaks because of weakness and respiratory-related recovery time. For patients who are mobilized, their activity is constrained by isolation restrictions that prohibit patients from leaving the confines of their hospital rooms. On March 23, 2020, the World Confederation for Physical Therapy (WCPT) endorsed guidelines created by the Australian Physiotherapy Association (APA) on caring for patients with COVID-19 acknowledging this risk16. The guidelines suggested that personal protective equipment (PPE) required for reducing risk of droplet transmission is appropriate for some scenarios, but they noted that exercising may induce coughing or expectoration, which could make physical therapy an aerosol-generating procedure. Therefore, the guidelines recommended that therapists wear N95 masks and recommend that direct face-to-face physical therapy should be limited to patients with certain functional limitations, including frailty, multiple comorbidities, and advanced age.
Patients with COVID-19 face additional barriers to accessing therapy services following hospital discharge. Post–acute care placement may be difficult due to limited availability of isolation rooms for patients with COVID-19 and the requirement of negative results for recovering patients. For those who manage to secure a bed, PPE shortages in nursing facilities could lead to lower prioritization of therapy interventions among staff and more bedridden days for the patients. Given social distancing restrictions, home health and outpatient therapy may not be possible for similar reasons.
The confluence of often highly symptomatic and even fragile patients, time-consuming visits with high concern for contagion, limited space to freely mobilize, and barriers to post–acute care illustrates why it is likely that COVID-19 admissions will be associated with a higher degree of HAD than admissions for other illnesses.
COVID-19: INNOVATION IN THERAPY SERVICES
The entire healthcare system has had to evolve and innovate rapidly to combat the morbidity and mortality of COVID-19. In the case of HAD, nursing staff, new billing guidelines, hospital redesign, and telemedicine are all facilitating novel ways to mobilize patients during and after hospitalization.
To limit the numbers of staff exposed to patients with COVID-19, the APA recommends engaging nursing staff in initial therapy evaluations and simple exercises that can be performed in a hospital room. Meaningful in-room exercise for some patients may include getting out of bed and walking to the bathroom to brush their teeth or complete other ADLs. Assessment of cognition should be carefully considered for discharge planning given its effects on the patient’s ability to independently participate in exercises and ADLs. For this reason, treatment and prevention of delirium or cognitive changes with interventions targeting environmental modifications, maintenance of healthy sleep-wake cycles, and orientation strategies are vital.
Therapy evaluations can also be administered remotely via phone call or video. To help facilitate telehealth visits, the Centers for Medicaid & Medicare Services has released new guidelines under the Coronavirus Aid, Relief, and Economic Security (CARES) Act. Physical and occupational therapists have been historically excluded from the list of providers able to bill for telehealth services, but the CARES Act allows physical and occupational therapists who accept Medicare part B to bill for telehealth services and e-visits. The new rule applies to patients in healthcare facilities or patients at home.17 Transitioning some physical and occupational therapy to telehealth could prove to be a critical resource for patients with COVID-19 trying to regain strength and independence during and after hospitalization.
Other solutions include converting areas of a hospital into rehabilitation units solely for patients recovering from COVID-19. Alternatively, rural hospitals, which usually run below capacity, or certain post–acute care facilities that are already prepared to manage infectious patients could serve as dedicated COVID-19 rehabilitation facilities, which can offer novel ways to continue therapy services after discharge while decreasing new exposures to COVID-19.18
Given the social isolation patients with COVID-19 experience during hospitalization, virtual group exercise classes may help for overall recovery. Most therapy companies already offer this service, and several include an app that allows therapists to monitor the patient’s exercises and progress. However, when transitioning to telemedicine, it is also important to consider the needs of those who may not be able to navigate technology effectively. For example, some elderly patients can be limited by a range of issues from poor computer skills and “technophobia” to visual and cognitive impairments. Having a friend or family member available to assist with technology should be considered. Additionally, being elderly, having lower income, or having a lower level of education makes it less likely that a patient will have access to internet or smartphones. Therefore, patients with these limitations may be poor candidates for telehealth and require post–acute care for their therapy services.19,20
CONCLUSION
With all the devastation that COVID-19 has created, it might be easy to forget the importance of physical and occupational therapy. But without this focus, the disability resulting from COVID-19 hospitalizations could inflict considerable long-lasting effects on our patients at great cost to an already strained healthcare system. Immediate changes in how we adapt and innovate these services for patients with COVID-19 are critical. It may prove to have enormous impact on patients and the healthcare system long after the worst of the virus is forgotten.
Disclosures
The authors reported having nothing to disclose.
Funding
Dr Arora is funded by National Heart, Lung and Blood Institute (NHLBI Grant K24HL136859).
Between February 1 and July 1, 2020, SARS-CoV-2 killed over 120,000 people in the United States alone. Nearly 80% of deaths occurred in those 65 years and older; by contrast, this age group constituted only 65% of deaths from influenza during the same time period.1 Though the reasons for these differences have not been completely elucidated, one thing is abundantly clear: Our nation’s oldest and most frail have been among the most likely to die of COVID-19. With an estimated mortality rate of 4.7% in the United States, we are fortunate that most infected patients survive2,3; however, many survivors require an exceptionally long hospital stay in isolation. Hospitalizations for patients with COVID-19 are distinct and confer a high risk for hospital-associated disability (HAD). HAD, defined as a new loss of ability to complete one or more activities of daily living (ADLs) without assistance after hospital discharge, occurs in approximately one-third of all hospitalized patients.4 In this perspective, we explore why HAD might be worse in patients with COVID-19 and offer new models for delivery of physical and occupational therapy to help them with functional recovery during and after hospitalization.
HOSPITAL-ASSOCIATED DISABILITY BEFORE COVID-19
Functional decline, a life-altering condition that patients experience as part of posthospital syndrome,5 is characterized by loss of mobility, cognitive decline, and HAD. The effects of functional decline can lead to a cascade of readmissions, institutionalization, and even death. During hospitalization, patients spend 87% to 100% of their time in bed. This immobilization is a major contributor to the development of HAD.6,7 The $58.5 billion dollars in yearly Medicare spending that is attributed to post–acute care also highlights the financial toll arising from such disability.8 Early mobilization with physical and occupational therapy is important to prevent HAD. However, even under normal conditions, care teams face innumerable barriers to mobilizing patients: symptomatic patients can be resistant to mobilizing during illness, providers have fears of worsening symptoms or falls, and some providers are unaware of the importance of mobilization. In patients with COVID-19, the barriers are only magnified.
HOSPITAL-ASSOCIATED DISABILITY DURING COVID-19
Given the increasing numbers of COVID-19 survivors discharged from the hospital, it is critical to consider why HAD could be an even larger problem in these patients. Consider their age, symptom burden, and illness severity: Among 5,700 patients who were admitted for COVID-19 in the New York City area, most were elderly (median age, 63 years), many were tachypneic (17%), and many required supplemental oxygen (28%).9 Fourteen percent of these patients required care in the intensive care unit (ICU), most of whom required mechanical ventilation (86%), which independently places them at higher risk of HAD. Given these severe respiratory issues in COVID-19, mobilization may cause significant discomfort. Being symptomatic is, by far, the most common reason hospitalized patients refuse to ambulate.10 As a result, this could make early mobilization for these COVID-19 patients exceptionally difficult.
Patients with COVID-19 also experience prolonged hospitalization. The median hospital length of stay (LOS) is 9.3 days for survivors of SARS-CoV-2 infection compared with the 7-day average LOS for patients with pneumonia requiring ICU admission and 5-day average LOS for patients with influenza.11-13 Complications of COVID, such as cardiac injury, critical illness polyneuropathy or myopathy, or cognitive impairment, also contribute to the significant need for rehabilitation long after recovery from the acute illness.14
Physical and occupational therapy involve prolonged close contact with patients, a known risk factor for contracting SARS-CoV-2.15 For staff, mobilizing a patient with COVID-19 takes longer due to intricate PPE donning and doffing procedures and patients requiring rest breaks because of weakness and respiratory-related recovery time. For patients who are mobilized, their activity is constrained by isolation restrictions that prohibit patients from leaving the confines of their hospital rooms. On March 23, 2020, the World Confederation for Physical Therapy (WCPT) endorsed guidelines created by the Australian Physiotherapy Association (APA) on caring for patients with COVID-19 acknowledging this risk16. The guidelines suggested that personal protective equipment (PPE) required for reducing risk of droplet transmission is appropriate for some scenarios, but they noted that exercising may induce coughing or expectoration, which could make physical therapy an aerosol-generating procedure. Therefore, the guidelines recommended that therapists wear N95 masks and recommend that direct face-to-face physical therapy should be limited to patients with certain functional limitations, including frailty, multiple comorbidities, and advanced age.
Patients with COVID-19 face additional barriers to accessing therapy services following hospital discharge. Post–acute care placement may be difficult due to limited availability of isolation rooms for patients with COVID-19 and the requirement of negative results for recovering patients. For those who manage to secure a bed, PPE shortages in nursing facilities could lead to lower prioritization of therapy interventions among staff and more bedridden days for the patients. Given social distancing restrictions, home health and outpatient therapy may not be possible for similar reasons.
The confluence of often highly symptomatic and even fragile patients, time-consuming visits with high concern for contagion, limited space to freely mobilize, and barriers to post–acute care illustrates why it is likely that COVID-19 admissions will be associated with a higher degree of HAD than admissions for other illnesses.
COVID-19: INNOVATION IN THERAPY SERVICES
The entire healthcare system has had to evolve and innovate rapidly to combat the morbidity and mortality of COVID-19. In the case of HAD, nursing staff, new billing guidelines, hospital redesign, and telemedicine are all facilitating novel ways to mobilize patients during and after hospitalization.
To limit the numbers of staff exposed to patients with COVID-19, the APA recommends engaging nursing staff in initial therapy evaluations and simple exercises that can be performed in a hospital room. Meaningful in-room exercise for some patients may include getting out of bed and walking to the bathroom to brush their teeth or complete other ADLs. Assessment of cognition should be carefully considered for discharge planning given its effects on the patient’s ability to independently participate in exercises and ADLs. For this reason, treatment and prevention of delirium or cognitive changes with interventions targeting environmental modifications, maintenance of healthy sleep-wake cycles, and orientation strategies are vital.
Therapy evaluations can also be administered remotely via phone call or video. To help facilitate telehealth visits, the Centers for Medicaid & Medicare Services has released new guidelines under the Coronavirus Aid, Relief, and Economic Security (CARES) Act. Physical and occupational therapists have been historically excluded from the list of providers able to bill for telehealth services, but the CARES Act allows physical and occupational therapists who accept Medicare part B to bill for telehealth services and e-visits. The new rule applies to patients in healthcare facilities or patients at home.17 Transitioning some physical and occupational therapy to telehealth could prove to be a critical resource for patients with COVID-19 trying to regain strength and independence during and after hospitalization.
Other solutions include converting areas of a hospital into rehabilitation units solely for patients recovering from COVID-19. Alternatively, rural hospitals, which usually run below capacity, or certain post–acute care facilities that are already prepared to manage infectious patients could serve as dedicated COVID-19 rehabilitation facilities, which can offer novel ways to continue therapy services after discharge while decreasing new exposures to COVID-19.18
Given the social isolation patients with COVID-19 experience during hospitalization, virtual group exercise classes may help for overall recovery. Most therapy companies already offer this service, and several include an app that allows therapists to monitor the patient’s exercises and progress. However, when transitioning to telemedicine, it is also important to consider the needs of those who may not be able to navigate technology effectively. For example, some elderly patients can be limited by a range of issues from poor computer skills and “technophobia” to visual and cognitive impairments. Having a friend or family member available to assist with technology should be considered. Additionally, being elderly, having lower income, or having a lower level of education makes it less likely that a patient will have access to internet or smartphones. Therefore, patients with these limitations may be poor candidates for telehealth and require post–acute care for their therapy services.19,20
CONCLUSION
With all the devastation that COVID-19 has created, it might be easy to forget the importance of physical and occupational therapy. But without this focus, the disability resulting from COVID-19 hospitalizations could inflict considerable long-lasting effects on our patients at great cost to an already strained healthcare system. Immediate changes in how we adapt and innovate these services for patients with COVID-19 are critical. It may prove to have enormous impact on patients and the healthcare system long after the worst of the virus is forgotten.
Disclosures
The authors reported having nothing to disclose.
Funding
Dr Arora is funded by National Heart, Lung and Blood Institute (NHLBI Grant K24HL136859).
1. Provisional COVID-19 Death Counts by Sex, Age, and State. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
2. Rajgor DD, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776-777. https://dx.doi.org/10.1016/S1473-3099(20)30244-9
3. Coronavirus Resource Center: Maps & Trends: Mortality Analyses. Johns Hopkins University & Medicine. Accessed April 26, 2020. https://coronavirus.jhu.edu/data/mortality
4. Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc. 2020;21(4):455-461.e5. https://doi.org/10.1016/j.jamda.2019.09.015
5. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. https://doi.org/10.1056/nejmp1212324
6. Summary Health Statistics: National Health Interview Survey, 2017. Tables P10a-P10c; p. 1-9. Centers for Disease Control and Prevention. Accessed April 26,2020. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_P-10.pdf
7. Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? a systematic review and meta-analysis. Appl Nurs Res. 2020;51:151189. https://doi.org/10.1016/j.apnr.2019.151189
8. Fact Sheet: Post-Acute Care. American Hospital Association. July 2019. Accessed April 26, 2020. https://www.aha.org/system/files/media/file/2019/07/fact-sheet-post-acute-care-0719.pdf
9. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059. https://doi.org/10.1001/jama.2020.6775
10. Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. J Hosp Med. 2007;2(5):305-313. https://doi.org/10.1002/jhm.209
11. Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ 2020;369:m1923. https://doi.org/10.1136/bmj.m1923
12. Williams S, Gousen S, DeFrances C. National Hospital Care Survey Demonstration Projects: pneumonia inpatient hospitalizations and emergency department visits. Natl Health Stat Report. 2018;(116):1-11.
13. Milenkovic M, Russo CA, Elixhauser A. Hospital Stays for Influenza, 2004: Statistical Brief #16. 2006 Oct. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed April 26, 2020 https://www.ncbi.nlm.nih.gov/books/NBK63484/
14. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470-474. https://doi.org/10.1097/phm.0000000000001443
15. Coronavirus Disease 2019 (COVID-19): Social Distancing. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
16. Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73-82. https://doi.org/10.1016/j.jphys.2020.03.011
17. COVID1-9 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services. Accessed April 23, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
18. Grabowski DC, Joynt Maddox KE. Postacute care preparedness for COVID-19: thinking ahead. JAMA. 2020;323(20):2007-2008. https://doi.org/10.1001/jama.2020.4686
19. Eung-Hun K, Stolvar A, Lober WB, et al. Challenges to using an electronic health record by a low-income elderly population. J Med Internet Res. 2009;11(4):e44. https://doi.org/10.2196/jmir.1256
20. Rajasekaran K. Access to telemedicine-are we doing all that we can during the COVID-19 pandemic? Otolaryngol Head Neck Surg. 2020;163(1):104-106. https://doi.org/10.1177/0194599820925049
1. Provisional COVID-19 Death Counts by Sex, Age, and State. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
2. Rajgor DD, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776-777. https://dx.doi.org/10.1016/S1473-3099(20)30244-9
3. Coronavirus Resource Center: Maps & Trends: Mortality Analyses. Johns Hopkins University & Medicine. Accessed April 26, 2020. https://coronavirus.jhu.edu/data/mortality
4. Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc. 2020;21(4):455-461.e5. https://doi.org/10.1016/j.jamda.2019.09.015
5. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. https://doi.org/10.1056/nejmp1212324
6. Summary Health Statistics: National Health Interview Survey, 2017. Tables P10a-P10c; p. 1-9. Centers for Disease Control and Prevention. Accessed April 26,2020. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_P-10.pdf
7. Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? a systematic review and meta-analysis. Appl Nurs Res. 2020;51:151189. https://doi.org/10.1016/j.apnr.2019.151189
8. Fact Sheet: Post-Acute Care. American Hospital Association. July 2019. Accessed April 26, 2020. https://www.aha.org/system/files/media/file/2019/07/fact-sheet-post-acute-care-0719.pdf
9. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059. https://doi.org/10.1001/jama.2020.6775
10. Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. J Hosp Med. 2007;2(5):305-313. https://doi.org/10.1002/jhm.209
11. Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ 2020;369:m1923. https://doi.org/10.1136/bmj.m1923
12. Williams S, Gousen S, DeFrances C. National Hospital Care Survey Demonstration Projects: pneumonia inpatient hospitalizations and emergency department visits. Natl Health Stat Report. 2018;(116):1-11.
13. Milenkovic M, Russo CA, Elixhauser A. Hospital Stays for Influenza, 2004: Statistical Brief #16. 2006 Oct. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed April 26, 2020 https://www.ncbi.nlm.nih.gov/books/NBK63484/
14. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470-474. https://doi.org/10.1097/phm.0000000000001443
15. Coronavirus Disease 2019 (COVID-19): Social Distancing. Centers for Disease Control and Prevention. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
16. Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73-82. https://doi.org/10.1016/j.jphys.2020.03.011
17. COVID1-9 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services. Accessed April 23, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
18. Grabowski DC, Joynt Maddox KE. Postacute care preparedness for COVID-19: thinking ahead. JAMA. 2020;323(20):2007-2008. https://doi.org/10.1001/jama.2020.4686
19. Eung-Hun K, Stolvar A, Lober WB, et al. Challenges to using an electronic health record by a low-income elderly population. J Med Internet Res. 2009;11(4):e44. https://doi.org/10.2196/jmir.1256
20. Rajasekaran K. Access to telemedicine-are we doing all that we can during the COVID-19 pandemic? Otolaryngol Head Neck Surg. 2020;163(1):104-106. https://doi.org/10.1177/0194599820925049
© 2020 Society of Hospital Medicine
Improving Patient Experience During the COVID-19 Pandemic: One Family’s Reflections
On March 11, 2020, the novel coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization.1 On March 13, 2020, a national emergency was declared in the United States concerning the COVID-19 outbreak.2 Later that week, Mike Kueper, a 52-year-old previously healthy man and resident of the Indianapolis metropolitan area, became sick with what he would eventually learn was COVID-19. Prior to contracting the novel coronavirus, he had never had as much as an Emergency Department (ED) visit. He had never spent a night in a hospital. He and his sister, DeAnn Harvey, describe the events that followed.
DeAnn
As a 20-year veteran clinical child psychologist and mother of two teenagers, my first reaction to the governor’s call for state-wide lockdowns was that they sounded like an opportunity for time at home with my husband and children. I thought we would play games, watch movies, try new recipes, and get a much-needed reprieve from our hectic lives of sports schedules, homework, and social outings. Even a slowdown in my practice sounded good. Maybe I could finally finish those continuing education credits that were due for my upcoming license renewal. My greatest concerns about sheltering in place were about how I was going to structure my children’s online learning while at the same time getting into my office to manage my patients via telehealth. Unfortunately, this relaxed feeling was short-lived.
On March 20, 2020, a few days after the lockdown started, my brother Mike developed high fevers. During a virtual doctor visit, he was told that it could be COVID-19 and to self-quarantine. Our discussions turned to jokes about his lack of taste or smell. We had dropped off soup for him from a new recipe my daughter had tried. My son joked that Mike was lucky that he couldn’t taste it.
On the morning of March 28, my mother called to tell me that Mike needed to go to the ED. Because we needed to figure out which hospital would be the best for him and I didn’t want my children to worry too much, I jumped in my car and drove to our church parking lot. In between calls to area hospitals, I began praying for his health and for guidance and support from God. Mike, concerned about spreading the virus to the rest of the family, refused to let my parents or me drive him to the hospital.
Mike
I thought I had a regular cold, and then, once I had a temperature of 102 °F and night sweats, decided it was the flu. One night, I was so cold that I went to bed wearing winter gloves. After a virtual visit with a nurse, she said my symptoms did not sound like COVID, but recommended self-quarantine, just in case. On March 26, I noticed that my sense of taste and smell had disappeared completely, and it hurt to yawn or take deep breaths. By Saturday, March 28, I was getting sicker and was short of breath and very tired. My elderly parents wanted to drive me to the ED, but if it was COVID-19, I didn’t want them near me. After getting advice from my sister, I called a local hospital and asked if I could come into the ED. The person on the phone said if I got there within an hour, they would be able to take me. When I arrived, an aide came out to my car, put me in a protective gown and mask, and walked me in. Walking even this short distance was tiring, and from this moment, things get fuzzy. I only have glimpses of the next few days. At first, I was put into a negative pressure room. I spent the night in there. I remember talking to a doctor who asked if I had a living will. He recommended that I go on a ventilator. I asked him, “Do you expect me to die?”
I remember him saying, “That is always a possibility.”
DeAnn
Once Mike was admitted to the hospital, we didn’t hear from anyone for about 6 hours, and I started to panic. I called people I knew who worked in the hospital, and my friend who is an intensive care unit (ICU) nurse agreed to track him down. He was indeed admitted to the hospital and was receiving oxygen. When I finally got to talk to him later that night, Mike had difficulty completing sentences because he was so short of breath. I told him not to use his energy, and that if they would let me, I would be there by his side. I promised him that he was going to get through this. Around 1:30
Mike
I don’t remember much from the ICU, but I understand that it was touch and go at times. I knew I was on a ventilator, and I found out later that I was “proned’ for up to 16 hours. Being on the ventilator was horrible, but what was even worse was that, once I was off the vent and alone in my hospital room, I had no idea how I got there. I thought I had been in a plane crash. I wanted to check my phone to see where I was flying in from but couldn’t because I thought my phone had been hacked by terrorists. I had no idea what was real and what was not. It was extremely scary.
DeAnn
When I think about the doctor coming in to tell Mike they had to put him on the ventilator, my heart absolutely breaks. It hurts to think of him all alone, having to make this decision without any of his family there to support him. Neither he nor I wanted to think about it, but we knew there was the possibility that he would never come off the ventilator. We hadn’t had a chance to hug him or even see him for days before his admission. If he didn’t make it, we would never get one of his amazing “Uncle Mike” hugs again.
Our friend, the ICU nurse, made it a point to find out which nurse was assigned to Mike and made it a priority to gather information from that nurse daily, allowing our family to receive updates on Mike’s status 2-3 times a day. In addition, the ICU physician was in daily contact with my parents: however, it was still excruciating not being able to be there. I spent a lot of time pacing the house, not eating or sleeping, checking my phone for texts, fielding texts and calls from friends and family. I was unable to do even simple household tasks, and left laundry, cooking, and my kids’ online schooling to my husband.
Feeling so helpless, I turned to prayer. My close friends organized a daily prayer vigil at 7:30
Then, after 17 days, a miracle: he was taken off the ventilator and moved to the medical unit. Looking back, I think these are really the days that the presence of his family would have sped up his recovery. Mike was experiencing delirium and hallucinations as a result of illness, medications, and the time he spent in an induced coma. I wish I could have been there with him to be the one he asked if what he was experiencing was real or a hallucination. Then we could have laughed about it together; our family has always found that humor helps with healing.
Mike
I understand the purpose of the isolation, but it really did a number on my mind. I remember being in the ICU, having my catheter taken out, not knowing what was happening or how I ended up in the hospital. I was so confused and was seeing people who were not there. One morning, I woke up thinking I was in my house and I had stolen the hospital bed I was in. I was panicking and scheming about how I might get this hospital bed back to the hospital before anyone noticed. As I mentioned earlier, I thought I was on a plane that had been taken over by terrorists who were using us COVID patients as biological weapons. Then I thought agents of the Federal Bureau of Investigation were coming to interrogate me and that they were also looking for my sister. To protect DeAnn, the next time someone asked me the name of my sister, I told them, “Maria” (the name of my sister who passed away in 1991) rather than DeAnn, who is very much alive. Another time, I thought my grandmother and cousin had died in a plane crash. My cousin is a state representative in Illinois, so once I got my phone to work, I checked his Wikipedia page to see if there was a death date listed.
When I was less confused, I found it’s tough spending day after day lying in a hospital bed with no family member or friend to offer companionship, comfort, or clarity. Even though I was extremely weak and could barely walk, I was asking, daily, about when I was expected to be discharged. I had to get out.
One night, our friend the ICU nurse came into my room to sit with me and just talk. She spent about 30 minutes with me around 4:00 in the morning. It was wonderful. All I could think about was what a huge blessing it was. I don’t think she knows just how much that meant to me. More often, I would report some symptom of confusion or insomnia, and a nurse would offer me medications for sleep or pain. I did not want any more drugs in my system. Human contact would have been a far better treatment.
I was reluctant to ask for help when I needed something, like a trip to the bathroom or some ice water. When I did press the call button, I had to wait for the busy nurse or tech to put on all the protective gear, and then, when they left, watch them take all the steps to disinfect and rid themselves of the gear that they had just put on. Even so, I was excited when it came time to take my vital signs or administer medications because that meant human interaction, however brief (and even if it was 4:00 AM). I wanted to bathe or change gowns and/or socks, but I opted to wear the same gown and socks for over three-fourths of the time I was there because I did not want to burden the staff.
Video chat turned out to be one of the best tools for creating connection. I may have sobbed a few times when talking to my parents on FaceTime, but just seeing their faces made all the difference in the world.
Finally, on April 21, 25 days after I was led into the ED, I was discharged. As we reflect on this experience, my family and I have some recommendations for hospitals and health systems trying to make patient experience a priority during this pandemic:
Kueper Family Recommendations to Improve Patient Experience for Those With COVID-19
- Adopt a more systematic approach to communicating with patient families, which would greatly improve the connection between them and healthcare personnel. This is especially important for families when the patient is critically ill, and especially in times when the patient is in isolation. We were fortunate in that we received updates from nurses and physicians several times a day. This was partly due to the relationships or connections with staff members that existed previously or developed over the course of Mike’s stay. Staff members who became invested in Mike’s progress became part of his hospital “family.” Many people who have had a family member with COVID have not had this experience, nor did they have the opportunity to build relationships with the staff, which we felt were important to ensure good care and open and frequent communication with them and the patient. Therefore, we believe a more systematic approach toward communication (eg, “the team will call each day during multidisciplinary rounds at 11 AM,”) would greatly improve the connection between families and healthcare personnel.
- Allow visitation under certain conditions even while the patient is in isolation. Visitation would have been especially helpful once Mike was more awake but isolated and delirious. We know that these policies are difficult to create and navigate but believe that there should be allowance for some visitation when there is a clear clinical benefit (eg, delirium). Because Mike had little human contact the week after he was taken off the ventilator (eg, contact limited to nurses coming in to take vitals, once daily doctor visit), he had to navigate the hallucinations and delirium on his own. Even one family member by his side who could provide frequent feedback on reality would have helped to resolve the feelings of agitation and fear that can accompany delirium.
- Schedule more video chats. Even when Mike was on the ventilator, we found video chats to be an important way to understand his experience and connect with him. Although we know such chats are difficult for clinicians to schedule, it greatly improved the experience for us.
- Reassure patients that caring for them is not a burden and they should not hesitate to ask for help. Being contagious and believing you are a danger to others is a terrible feeling. No one on staff said or even implied that they were afraid to care for him, but Mike felt “dangerous” to the staff and as such hesitated to “burden” the clinicians with requests (eg, going to the bathroom, having a change of clothes). It is time-consuming and difficult to don PPE and the amount of effort it takes to enter the room is immediately obvious to the patient. Because of this, it is very important that the clinicians and staff reassure patients that it is part of the job and not a burden to come in and out of the room.
DeAnn
Having Mike alive and now home is an incredible gift. We are taking every chance we can to make up for the time that we could not see him and are so grateful for the hospital team that saved his life.
Mike
On April 21, I was discharged and sent home. Luckily, for about 2 weeks, I had a best friend, my brother, and DeAnn, separately, stay with me each night. This was a godsend as all made sure I was taking my medicine, eating, and doing my prescribed exercises. I am struggling with a long recovery. I used a walker for a while and had both a physical and occupational therapist visit me two to three times a week. I visit a neurologist for some of my symptoms that have not resolved, such as pain and atrophy in my right shoulder, hand tremors, and some numbness in my thighs. Thankfully, I was able to resume working from home, but even going up stairs causes me to become winded. I know that doctors don’t understand this disease very well, and neither do I. Sometimes I feel discouraged about how much it set me back physically. I wish things could have been different—that I could have avoided this disease altogether or had milder symptoms. But I am so grateful to be alive and so thankful for the doctors and nurses, as well as for my family, who could not be there physically during the hospitalization but did everything they could do to help me. Because of their love and support, I survived.
Disclosures
The authors have nothing to disclose.
1. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID–11 March 2020. Published March 11, 2020. Accessed August 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
2. White House. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Issued March 13, 2020. Accessed August 11, 2020. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
On March 11, 2020, the novel coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization.1 On March 13, 2020, a national emergency was declared in the United States concerning the COVID-19 outbreak.2 Later that week, Mike Kueper, a 52-year-old previously healthy man and resident of the Indianapolis metropolitan area, became sick with what he would eventually learn was COVID-19. Prior to contracting the novel coronavirus, he had never had as much as an Emergency Department (ED) visit. He had never spent a night in a hospital. He and his sister, DeAnn Harvey, describe the events that followed.
DeAnn
As a 20-year veteran clinical child psychologist and mother of two teenagers, my first reaction to the governor’s call for state-wide lockdowns was that they sounded like an opportunity for time at home with my husband and children. I thought we would play games, watch movies, try new recipes, and get a much-needed reprieve from our hectic lives of sports schedules, homework, and social outings. Even a slowdown in my practice sounded good. Maybe I could finally finish those continuing education credits that were due for my upcoming license renewal. My greatest concerns about sheltering in place were about how I was going to structure my children’s online learning while at the same time getting into my office to manage my patients via telehealth. Unfortunately, this relaxed feeling was short-lived.
On March 20, 2020, a few days after the lockdown started, my brother Mike developed high fevers. During a virtual doctor visit, he was told that it could be COVID-19 and to self-quarantine. Our discussions turned to jokes about his lack of taste or smell. We had dropped off soup for him from a new recipe my daughter had tried. My son joked that Mike was lucky that he couldn’t taste it.
On the morning of March 28, my mother called to tell me that Mike needed to go to the ED. Because we needed to figure out which hospital would be the best for him and I didn’t want my children to worry too much, I jumped in my car and drove to our church parking lot. In between calls to area hospitals, I began praying for his health and for guidance and support from God. Mike, concerned about spreading the virus to the rest of the family, refused to let my parents or me drive him to the hospital.
Mike
I thought I had a regular cold, and then, once I had a temperature of 102 °F and night sweats, decided it was the flu. One night, I was so cold that I went to bed wearing winter gloves. After a virtual visit with a nurse, she said my symptoms did not sound like COVID, but recommended self-quarantine, just in case. On March 26, I noticed that my sense of taste and smell had disappeared completely, and it hurt to yawn or take deep breaths. By Saturday, March 28, I was getting sicker and was short of breath and very tired. My elderly parents wanted to drive me to the ED, but if it was COVID-19, I didn’t want them near me. After getting advice from my sister, I called a local hospital and asked if I could come into the ED. The person on the phone said if I got there within an hour, they would be able to take me. When I arrived, an aide came out to my car, put me in a protective gown and mask, and walked me in. Walking even this short distance was tiring, and from this moment, things get fuzzy. I only have glimpses of the next few days. At first, I was put into a negative pressure room. I spent the night in there. I remember talking to a doctor who asked if I had a living will. He recommended that I go on a ventilator. I asked him, “Do you expect me to die?”
I remember him saying, “That is always a possibility.”
DeAnn
Once Mike was admitted to the hospital, we didn’t hear from anyone for about 6 hours, and I started to panic. I called people I knew who worked in the hospital, and my friend who is an intensive care unit (ICU) nurse agreed to track him down. He was indeed admitted to the hospital and was receiving oxygen. When I finally got to talk to him later that night, Mike had difficulty completing sentences because he was so short of breath. I told him not to use his energy, and that if they would let me, I would be there by his side. I promised him that he was going to get through this. Around 1:30
Mike
I don’t remember much from the ICU, but I understand that it was touch and go at times. I knew I was on a ventilator, and I found out later that I was “proned’ for up to 16 hours. Being on the ventilator was horrible, but what was even worse was that, once I was off the vent and alone in my hospital room, I had no idea how I got there. I thought I had been in a plane crash. I wanted to check my phone to see where I was flying in from but couldn’t because I thought my phone had been hacked by terrorists. I had no idea what was real and what was not. It was extremely scary.
DeAnn
When I think about the doctor coming in to tell Mike they had to put him on the ventilator, my heart absolutely breaks. It hurts to think of him all alone, having to make this decision without any of his family there to support him. Neither he nor I wanted to think about it, but we knew there was the possibility that he would never come off the ventilator. We hadn’t had a chance to hug him or even see him for days before his admission. If he didn’t make it, we would never get one of his amazing “Uncle Mike” hugs again.
Our friend, the ICU nurse, made it a point to find out which nurse was assigned to Mike and made it a priority to gather information from that nurse daily, allowing our family to receive updates on Mike’s status 2-3 times a day. In addition, the ICU physician was in daily contact with my parents: however, it was still excruciating not being able to be there. I spent a lot of time pacing the house, not eating or sleeping, checking my phone for texts, fielding texts and calls from friends and family. I was unable to do even simple household tasks, and left laundry, cooking, and my kids’ online schooling to my husband.
Feeling so helpless, I turned to prayer. My close friends organized a daily prayer vigil at 7:30
Then, after 17 days, a miracle: he was taken off the ventilator and moved to the medical unit. Looking back, I think these are really the days that the presence of his family would have sped up his recovery. Mike was experiencing delirium and hallucinations as a result of illness, medications, and the time he spent in an induced coma. I wish I could have been there with him to be the one he asked if what he was experiencing was real or a hallucination. Then we could have laughed about it together; our family has always found that humor helps with healing.
Mike
I understand the purpose of the isolation, but it really did a number on my mind. I remember being in the ICU, having my catheter taken out, not knowing what was happening or how I ended up in the hospital. I was so confused and was seeing people who were not there. One morning, I woke up thinking I was in my house and I had stolen the hospital bed I was in. I was panicking and scheming about how I might get this hospital bed back to the hospital before anyone noticed. As I mentioned earlier, I thought I was on a plane that had been taken over by terrorists who were using us COVID patients as biological weapons. Then I thought agents of the Federal Bureau of Investigation were coming to interrogate me and that they were also looking for my sister. To protect DeAnn, the next time someone asked me the name of my sister, I told them, “Maria” (the name of my sister who passed away in 1991) rather than DeAnn, who is very much alive. Another time, I thought my grandmother and cousin had died in a plane crash. My cousin is a state representative in Illinois, so once I got my phone to work, I checked his Wikipedia page to see if there was a death date listed.
When I was less confused, I found it’s tough spending day after day lying in a hospital bed with no family member or friend to offer companionship, comfort, or clarity. Even though I was extremely weak and could barely walk, I was asking, daily, about when I was expected to be discharged. I had to get out.
One night, our friend the ICU nurse came into my room to sit with me and just talk. She spent about 30 minutes with me around 4:00 in the morning. It was wonderful. All I could think about was what a huge blessing it was. I don’t think she knows just how much that meant to me. More often, I would report some symptom of confusion or insomnia, and a nurse would offer me medications for sleep or pain. I did not want any more drugs in my system. Human contact would have been a far better treatment.
I was reluctant to ask for help when I needed something, like a trip to the bathroom or some ice water. When I did press the call button, I had to wait for the busy nurse or tech to put on all the protective gear, and then, when they left, watch them take all the steps to disinfect and rid themselves of the gear that they had just put on. Even so, I was excited when it came time to take my vital signs or administer medications because that meant human interaction, however brief (and even if it was 4:00 AM). I wanted to bathe or change gowns and/or socks, but I opted to wear the same gown and socks for over three-fourths of the time I was there because I did not want to burden the staff.
Video chat turned out to be one of the best tools for creating connection. I may have sobbed a few times when talking to my parents on FaceTime, but just seeing their faces made all the difference in the world.
Finally, on April 21, 25 days after I was led into the ED, I was discharged. As we reflect on this experience, my family and I have some recommendations for hospitals and health systems trying to make patient experience a priority during this pandemic:
Kueper Family Recommendations to Improve Patient Experience for Those With COVID-19
- Adopt a more systematic approach to communicating with patient families, which would greatly improve the connection between them and healthcare personnel. This is especially important for families when the patient is critically ill, and especially in times when the patient is in isolation. We were fortunate in that we received updates from nurses and physicians several times a day. This was partly due to the relationships or connections with staff members that existed previously or developed over the course of Mike’s stay. Staff members who became invested in Mike’s progress became part of his hospital “family.” Many people who have had a family member with COVID have not had this experience, nor did they have the opportunity to build relationships with the staff, which we felt were important to ensure good care and open and frequent communication with them and the patient. Therefore, we believe a more systematic approach toward communication (eg, “the team will call each day during multidisciplinary rounds at 11 AM,”) would greatly improve the connection between families and healthcare personnel.
- Allow visitation under certain conditions even while the patient is in isolation. Visitation would have been especially helpful once Mike was more awake but isolated and delirious. We know that these policies are difficult to create and navigate but believe that there should be allowance for some visitation when there is a clear clinical benefit (eg, delirium). Because Mike had little human contact the week after he was taken off the ventilator (eg, contact limited to nurses coming in to take vitals, once daily doctor visit), he had to navigate the hallucinations and delirium on his own. Even one family member by his side who could provide frequent feedback on reality would have helped to resolve the feelings of agitation and fear that can accompany delirium.
- Schedule more video chats. Even when Mike was on the ventilator, we found video chats to be an important way to understand his experience and connect with him. Although we know such chats are difficult for clinicians to schedule, it greatly improved the experience for us.
- Reassure patients that caring for them is not a burden and they should not hesitate to ask for help. Being contagious and believing you are a danger to others is a terrible feeling. No one on staff said or even implied that they were afraid to care for him, but Mike felt “dangerous” to the staff and as such hesitated to “burden” the clinicians with requests (eg, going to the bathroom, having a change of clothes). It is time-consuming and difficult to don PPE and the amount of effort it takes to enter the room is immediately obvious to the patient. Because of this, it is very important that the clinicians and staff reassure patients that it is part of the job and not a burden to come in and out of the room.
DeAnn
Having Mike alive and now home is an incredible gift. We are taking every chance we can to make up for the time that we could not see him and are so grateful for the hospital team that saved his life.
Mike
On April 21, I was discharged and sent home. Luckily, for about 2 weeks, I had a best friend, my brother, and DeAnn, separately, stay with me each night. This was a godsend as all made sure I was taking my medicine, eating, and doing my prescribed exercises. I am struggling with a long recovery. I used a walker for a while and had both a physical and occupational therapist visit me two to three times a week. I visit a neurologist for some of my symptoms that have not resolved, such as pain and atrophy in my right shoulder, hand tremors, and some numbness in my thighs. Thankfully, I was able to resume working from home, but even going up stairs causes me to become winded. I know that doctors don’t understand this disease very well, and neither do I. Sometimes I feel discouraged about how much it set me back physically. I wish things could have been different—that I could have avoided this disease altogether or had milder symptoms. But I am so grateful to be alive and so thankful for the doctors and nurses, as well as for my family, who could not be there physically during the hospitalization but did everything they could do to help me. Because of their love and support, I survived.
Disclosures
The authors have nothing to disclose.
On March 11, 2020, the novel coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization.1 On March 13, 2020, a national emergency was declared in the United States concerning the COVID-19 outbreak.2 Later that week, Mike Kueper, a 52-year-old previously healthy man and resident of the Indianapolis metropolitan area, became sick with what he would eventually learn was COVID-19. Prior to contracting the novel coronavirus, he had never had as much as an Emergency Department (ED) visit. He had never spent a night in a hospital. He and his sister, DeAnn Harvey, describe the events that followed.
DeAnn
As a 20-year veteran clinical child psychologist and mother of two teenagers, my first reaction to the governor’s call for state-wide lockdowns was that they sounded like an opportunity for time at home with my husband and children. I thought we would play games, watch movies, try new recipes, and get a much-needed reprieve from our hectic lives of sports schedules, homework, and social outings. Even a slowdown in my practice sounded good. Maybe I could finally finish those continuing education credits that were due for my upcoming license renewal. My greatest concerns about sheltering in place were about how I was going to structure my children’s online learning while at the same time getting into my office to manage my patients via telehealth. Unfortunately, this relaxed feeling was short-lived.
On March 20, 2020, a few days after the lockdown started, my brother Mike developed high fevers. During a virtual doctor visit, he was told that it could be COVID-19 and to self-quarantine. Our discussions turned to jokes about his lack of taste or smell. We had dropped off soup for him from a new recipe my daughter had tried. My son joked that Mike was lucky that he couldn’t taste it.
On the morning of March 28, my mother called to tell me that Mike needed to go to the ED. Because we needed to figure out which hospital would be the best for him and I didn’t want my children to worry too much, I jumped in my car and drove to our church parking lot. In between calls to area hospitals, I began praying for his health and for guidance and support from God. Mike, concerned about spreading the virus to the rest of the family, refused to let my parents or me drive him to the hospital.
Mike
I thought I had a regular cold, and then, once I had a temperature of 102 °F and night sweats, decided it was the flu. One night, I was so cold that I went to bed wearing winter gloves. After a virtual visit with a nurse, she said my symptoms did not sound like COVID, but recommended self-quarantine, just in case. On March 26, I noticed that my sense of taste and smell had disappeared completely, and it hurt to yawn or take deep breaths. By Saturday, March 28, I was getting sicker and was short of breath and very tired. My elderly parents wanted to drive me to the ED, but if it was COVID-19, I didn’t want them near me. After getting advice from my sister, I called a local hospital and asked if I could come into the ED. The person on the phone said if I got there within an hour, they would be able to take me. When I arrived, an aide came out to my car, put me in a protective gown and mask, and walked me in. Walking even this short distance was tiring, and from this moment, things get fuzzy. I only have glimpses of the next few days. At first, I was put into a negative pressure room. I spent the night in there. I remember talking to a doctor who asked if I had a living will. He recommended that I go on a ventilator. I asked him, “Do you expect me to die?”
I remember him saying, “That is always a possibility.”
DeAnn
Once Mike was admitted to the hospital, we didn’t hear from anyone for about 6 hours, and I started to panic. I called people I knew who worked in the hospital, and my friend who is an intensive care unit (ICU) nurse agreed to track him down. He was indeed admitted to the hospital and was receiving oxygen. When I finally got to talk to him later that night, Mike had difficulty completing sentences because he was so short of breath. I told him not to use his energy, and that if they would let me, I would be there by his side. I promised him that he was going to get through this. Around 1:30
Mike
I don’t remember much from the ICU, but I understand that it was touch and go at times. I knew I was on a ventilator, and I found out later that I was “proned’ for up to 16 hours. Being on the ventilator was horrible, but what was even worse was that, once I was off the vent and alone in my hospital room, I had no idea how I got there. I thought I had been in a plane crash. I wanted to check my phone to see where I was flying in from but couldn’t because I thought my phone had been hacked by terrorists. I had no idea what was real and what was not. It was extremely scary.
DeAnn
When I think about the doctor coming in to tell Mike they had to put him on the ventilator, my heart absolutely breaks. It hurts to think of him all alone, having to make this decision without any of his family there to support him. Neither he nor I wanted to think about it, but we knew there was the possibility that he would never come off the ventilator. We hadn’t had a chance to hug him or even see him for days before his admission. If he didn’t make it, we would never get one of his amazing “Uncle Mike” hugs again.
Our friend, the ICU nurse, made it a point to find out which nurse was assigned to Mike and made it a priority to gather information from that nurse daily, allowing our family to receive updates on Mike’s status 2-3 times a day. In addition, the ICU physician was in daily contact with my parents: however, it was still excruciating not being able to be there. I spent a lot of time pacing the house, not eating or sleeping, checking my phone for texts, fielding texts and calls from friends and family. I was unable to do even simple household tasks, and left laundry, cooking, and my kids’ online schooling to my husband.
Feeling so helpless, I turned to prayer. My close friends organized a daily prayer vigil at 7:30
Then, after 17 days, a miracle: he was taken off the ventilator and moved to the medical unit. Looking back, I think these are really the days that the presence of his family would have sped up his recovery. Mike was experiencing delirium and hallucinations as a result of illness, medications, and the time he spent in an induced coma. I wish I could have been there with him to be the one he asked if what he was experiencing was real or a hallucination. Then we could have laughed about it together; our family has always found that humor helps with healing.
Mike
I understand the purpose of the isolation, but it really did a number on my mind. I remember being in the ICU, having my catheter taken out, not knowing what was happening or how I ended up in the hospital. I was so confused and was seeing people who were not there. One morning, I woke up thinking I was in my house and I had stolen the hospital bed I was in. I was panicking and scheming about how I might get this hospital bed back to the hospital before anyone noticed. As I mentioned earlier, I thought I was on a plane that had been taken over by terrorists who were using us COVID patients as biological weapons. Then I thought agents of the Federal Bureau of Investigation were coming to interrogate me and that they were also looking for my sister. To protect DeAnn, the next time someone asked me the name of my sister, I told them, “Maria” (the name of my sister who passed away in 1991) rather than DeAnn, who is very much alive. Another time, I thought my grandmother and cousin had died in a plane crash. My cousin is a state representative in Illinois, so once I got my phone to work, I checked his Wikipedia page to see if there was a death date listed.
When I was less confused, I found it’s tough spending day after day lying in a hospital bed with no family member or friend to offer companionship, comfort, or clarity. Even though I was extremely weak and could barely walk, I was asking, daily, about when I was expected to be discharged. I had to get out.
One night, our friend the ICU nurse came into my room to sit with me and just talk. She spent about 30 minutes with me around 4:00 in the morning. It was wonderful. All I could think about was what a huge blessing it was. I don’t think she knows just how much that meant to me. More often, I would report some symptom of confusion or insomnia, and a nurse would offer me medications for sleep or pain. I did not want any more drugs in my system. Human contact would have been a far better treatment.
I was reluctant to ask for help when I needed something, like a trip to the bathroom or some ice water. When I did press the call button, I had to wait for the busy nurse or tech to put on all the protective gear, and then, when they left, watch them take all the steps to disinfect and rid themselves of the gear that they had just put on. Even so, I was excited when it came time to take my vital signs or administer medications because that meant human interaction, however brief (and even if it was 4:00 AM). I wanted to bathe or change gowns and/or socks, but I opted to wear the same gown and socks for over three-fourths of the time I was there because I did not want to burden the staff.
Video chat turned out to be one of the best tools for creating connection. I may have sobbed a few times when talking to my parents on FaceTime, but just seeing their faces made all the difference in the world.
Finally, on April 21, 25 days after I was led into the ED, I was discharged. As we reflect on this experience, my family and I have some recommendations for hospitals and health systems trying to make patient experience a priority during this pandemic:
Kueper Family Recommendations to Improve Patient Experience for Those With COVID-19
- Adopt a more systematic approach to communicating with patient families, which would greatly improve the connection between them and healthcare personnel. This is especially important for families when the patient is critically ill, and especially in times when the patient is in isolation. We were fortunate in that we received updates from nurses and physicians several times a day. This was partly due to the relationships or connections with staff members that existed previously or developed over the course of Mike’s stay. Staff members who became invested in Mike’s progress became part of his hospital “family.” Many people who have had a family member with COVID have not had this experience, nor did they have the opportunity to build relationships with the staff, which we felt were important to ensure good care and open and frequent communication with them and the patient. Therefore, we believe a more systematic approach toward communication (eg, “the team will call each day during multidisciplinary rounds at 11 AM,”) would greatly improve the connection between families and healthcare personnel.
- Allow visitation under certain conditions even while the patient is in isolation. Visitation would have been especially helpful once Mike was more awake but isolated and delirious. We know that these policies are difficult to create and navigate but believe that there should be allowance for some visitation when there is a clear clinical benefit (eg, delirium). Because Mike had little human contact the week after he was taken off the ventilator (eg, contact limited to nurses coming in to take vitals, once daily doctor visit), he had to navigate the hallucinations and delirium on his own. Even one family member by his side who could provide frequent feedback on reality would have helped to resolve the feelings of agitation and fear that can accompany delirium.
- Schedule more video chats. Even when Mike was on the ventilator, we found video chats to be an important way to understand his experience and connect with him. Although we know such chats are difficult for clinicians to schedule, it greatly improved the experience for us.
- Reassure patients that caring for them is not a burden and they should not hesitate to ask for help. Being contagious and believing you are a danger to others is a terrible feeling. No one on staff said or even implied that they were afraid to care for him, but Mike felt “dangerous” to the staff and as such hesitated to “burden” the clinicians with requests (eg, going to the bathroom, having a change of clothes). It is time-consuming and difficult to don PPE and the amount of effort it takes to enter the room is immediately obvious to the patient. Because of this, it is very important that the clinicians and staff reassure patients that it is part of the job and not a burden to come in and out of the room.
DeAnn
Having Mike alive and now home is an incredible gift. We are taking every chance we can to make up for the time that we could not see him and are so grateful for the hospital team that saved his life.
Mike
On April 21, I was discharged and sent home. Luckily, for about 2 weeks, I had a best friend, my brother, and DeAnn, separately, stay with me each night. This was a godsend as all made sure I was taking my medicine, eating, and doing my prescribed exercises. I am struggling with a long recovery. I used a walker for a while and had both a physical and occupational therapist visit me two to three times a week. I visit a neurologist for some of my symptoms that have not resolved, such as pain and atrophy in my right shoulder, hand tremors, and some numbness in my thighs. Thankfully, I was able to resume working from home, but even going up stairs causes me to become winded. I know that doctors don’t understand this disease very well, and neither do I. Sometimes I feel discouraged about how much it set me back physically. I wish things could have been different—that I could have avoided this disease altogether or had milder symptoms. But I am so grateful to be alive and so thankful for the doctors and nurses, as well as for my family, who could not be there physically during the hospitalization but did everything they could do to help me. Because of their love and support, I survived.
Disclosures
The authors have nothing to disclose.
1. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID–11 March 2020. Published March 11, 2020. Accessed August 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
2. White House. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Issued March 13, 2020. Accessed August 11, 2020. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
1. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID–11 March 2020. Published March 11, 2020. Accessed August 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
2. White House. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Issued March 13, 2020. Accessed August 11, 2020. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
© 2020 Society of Hospital Medicine
Deployed: Pediatric Residents Caring for Adults During COVID-19’s First Wave in New York City
Stepping onto a busy coronavirus disease (COVID-19) unit for the first time can elicit trepidation for any medical provider. For a group of deployed pediatric residents at a New York City hospital in the spring of 2020, it was also the first time caring for adults since medical school. Imagine a pediatrician receiving this handoff: “77-year-old female with a history of diabetes, peripheral vascular disease, and COPD admitted with COVID-19 pneumonia, now intubated and proned with O2 saturations in the 80s. To do: DNR discussion.” General anxiety around COVID-19 was compounded by the discomfort of being thrust into adult medicine. But the doctoring instinct we have been honing throughout training kicked in, and we acted.
A NEW ORDER
As the COVID-19 crisis escalated in New York City, it became evident that staff from other specialties would be essential to manage the surge of patients. Hospital administrators selected a group of trainees for deployment based on their clinical experiences and willingness to volunteer. Almost overnight, a group of senior pediatric residents became adult providers, honoring the oath we each took to “remain a member of society with special obligations to all . . . fellow human beings.”¹
This health crisis brought different clinical disciplines together like never before. Entire wings of the hospital were converted into new COVID-19–dedicated wards and intensive care units (ICUs), and teams were built to optimize providers’ skills and capabilities. For example, one third-year pediatric resident was grouped with an outpatient endocrinologist—who had not practiced inpatient medicine in a decade—and a medicine intern. Hospitalists provided crucial support and guidance to these ward teams of deployed providers who were eager and willing to work but often not very knowledgeable about inpatient adult medicine.² In new ad hoc COVID-19 ICUs housed in other ICUs, where most pediatric residents were deployed, critical care attendings and neurointensivists led teams that also included anesthesiology, radiology, and neurosurgery residents, as well as nurses and advanced practice providers trained in various subspecialties of adult medicine.
PEDIATRICIANS IN AN ADULT WORLD
Although we wanted to help in any way we could, the prospect of entering this new world was incredibly daunting. We had not treated adults in several years, and during that time, our clinical experience with pediatric medicine greatly surpassed our adult training from medical school. We dug out materials on adult diseases, watched impromptu lectures on COVID-19 given by our critical care attendings, taught ourselves ventilator management in adults, and reviewed advanced cardiac life support (ACLS) protocols. But putting this all into practice was entirely different. Nothing can truly prepare you for arriving at the bedside of a hemodynamically unstable patient suffering from a virus that no one really understands.
When we arrived and introduced ourselves, we occasionally encountered surprise and curiosity from other providers. We felt that there was a perception that pediatricians do not often take care of critically ill or complex patients. Some of us were reluctant to disclose our specialty, lest it cloud perceptions of our capabilities. However, sick patients awaited us, so we got to work.
There was a steep learning curve over the first few days, from adjusting insulin for type 2 diabetes to troubleshooting renal replacement therapy issues. Accustomed to pediatric weight-based dosing, we were very anxious about ordering medications. The adult providers on our teams oriented us and helped us with many of these concerns. But the mystery of COVID-19 was a great equalizing force, leaving providers of every background with questions: Should we anticoagulate? How about steroids? Could this clinical change be another effect of the virus or a new infection?
We were pleasantly surprised that many aspects of our pediatric training proved beneficial in caring for adults. The focus on family-centered rounds and shared decision-making in pediatrics had imprinted on us the paramount importance of good communication. We were very cognizant of involving loved ones in discussions, now conducted by telephone or video call because infection-prevention guidelines precluded visitors. Family members were thankful for frequent updates, and as a result, largely embraced us as the doctors treating their loved ones. On one occasion, an internist, whose mother was a patient, was delighted to learn that the provider was a pediatric resident, saying, “I know you’ll take such good care of her.”
With the hospital inundated with sick adults, colleagues were grateful for our help. More so, they seemed appreciative of our compassion and ability to maintain a sense of humanity during the pandemonium of the pandemic despite feeling vulnerable, scared, and often powerless against COVID-19. In pediatrics, we do our best to truly engage with patients, from playing games with a 6-year-old with perforated appendicitis to holding and soothing a newborn in the neonatal ICU. We carried those skills over to the adult side. The team appreciated when a pediatric resident, with the help of an occupational therapist, used a letter board to communicate and receive assent for a tracheostomy from a nonsedated, intubated patient, directly answering the patient’s questions and addressing concerns rather than relying solely on a family member’s consent. And, though we had not previously led end-of-life discussions, we found that we were capable of doing so with the compassion instilled in us from our pediatric training. It had prepared us to face the universal challenge of communication in times of grief.
COVID-19 CHALLENGES
Besides grappling with our insecurity in treating adults, we, like all medical providers, had to balance our desire to provide care while keeping ourselves safe from COVID-19. To reduce our risk of exposure and preserve the dwindling supply of personal protective equipment (PPE), the flow of rounding, bedside care, and interventions was adapted to better cluster examinations, blood draws, and bedside tasks. Although efficient, this meant we did not enter rooms as frequently, creating an unfamiliar distance between provider and patient.³ We feared missing moments of clinical decompensation, and for pediatricians who value close patient contact, this made for a deeply uncomfortable reality.
We considered every plausible treatment for critically ill patients, sometimes unsure if they were beneficial or instead complicating the course further. Was lack of improvement a treatment failure or just the natural progression of this new illness? Unfortunately, most of the time, treatments were to no avail. Watching the respiratory, cardiovascular, renal, and neurologic devastation of COVID-19 on so many patients was horrifying. Seeing patients die without their loved ones beside them and at an alarmingly fast rate was simply crushing, as other trainees have similarly described.4 It was unlike anything we had ever experienced in pediatrics. Though we had begun to see a few pediatric COVID-19 patients in the hospital, their disease course was less severe. And, in the rare cases when pediatric patients die, they are almost invariably surrounded by family. One pediatric resident, who had never performed a single death examination before, did three in 1 week. It was emotionally trying, yet we had little time to mourn, as deathbeds were only briefly empty before the next gravely ill patients filled them.
Deployment took a toll on our bodies as well. We padded our faces to alleviate skin breakdown from 12-hour shifts spent entirely in N95 masks. We sanitized and washed our hands constantly, developing cracked skin and dermatitis, and showered meticulously after every shift. We isolated ourselves from our families and loved ones to protect them from the virus.
MOMENTS OF POSITIVITY
Despite these challenges, positive moments emerged. We worked with many wonderful colleagues from different disciplines we likely never would have met, let alone work alongside. We valued each other’s skills, talents, and knowledge. On an overnight shift in one of the ICUs, among the “ragtag team of deployees,” as one pediatric resident phrased it, each presented a topic from his or her respective specialty that might interest others. The pediatrician presented Kawasaki disease, as adult colleagues were beginning to ask questions about its cousin, the emerging multisystem inflammatory syndrome in children (MIS-C). This collegiality promoted a culture of collaboration and respect for other specialties that will hopefully continue.
A strong drive toward teamwork and shared responsibility flourished during deployment. No one was above any task. Residents and even fellows performed typical frontline tasks, such as ordering laboratory work and coordinating imaging. We all helped the proning team turn patients. Everyone shared insights, perspectives, and information gleaned from friends in different wards and hospitals and the ever-evolving literature. As we grappled with unpredictable disease courses, the traditional hierarchical roles of medicine—attending, fellow, resident—often blurred. We felt like we were all in this together.
Patient triumphs were celebrated. We danced with an 80-year-old patient admitted for almost 2 weeks when she was informed of her discharge and gave a standing ovation for a 91-year-old woman as she headed home. Music played over the hospital loudspeaker for every patient discharge. We also tried to create moments of lightheartedness. In the ICUs, we ate donated meals together and posed for pictures to express our gratitude to restaurants. Camaraderie blossomed during deployment.
ADVICE FOR THE FUTURE
Answering the call to help during the COVID-19 surge in New York City indelibly shaped our experiences as trainees and physicians. We will carry with us the lessons that we learned, both in the short term for the possible resurgence of cases and in the long term for ongoing patient care for the rest of our careers. For those residents who may be called upon next, the experience will be challenging, but rewarding. Each trainee has a foundation of knowledge, abilities, and instincts that will be useful, so trust in your training. Do not be afraid to ask questions or for help. You may be leaving your comfort zone, but you will not be alone, and families and other clinicians will be grateful to have you there. You are resilient, and you will make a difference.
Disclosures
The authors have nothing to disclose.
1. Lasagna L. Hippocratic oath—modern version. Published 1964. Accessed September 14, 2020. http://www.pbs.org/wgbh/nova/doctors/oath_modern.html
2. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314-315.https://doi.org/10.12788/jhm.3426
3. Cunningham CO, Diaz C, Slawek DE. COVID-19: the worst days of our careers. Ann Intern Med. 2020;172(11):764-765. https://doi.org/10.7326/M20-1715
4. Gallagher TH, Schleyer AM. “We signed up for this!”—student and trainee responses to the COVID-19 pandemic. N Engl J Med. 2020;382(25):e96. https://doi.org/10.1056/NEJMp2005234
Stepping onto a busy coronavirus disease (COVID-19) unit for the first time can elicit trepidation for any medical provider. For a group of deployed pediatric residents at a New York City hospital in the spring of 2020, it was also the first time caring for adults since medical school. Imagine a pediatrician receiving this handoff: “77-year-old female with a history of diabetes, peripheral vascular disease, and COPD admitted with COVID-19 pneumonia, now intubated and proned with O2 saturations in the 80s. To do: DNR discussion.” General anxiety around COVID-19 was compounded by the discomfort of being thrust into adult medicine. But the doctoring instinct we have been honing throughout training kicked in, and we acted.
A NEW ORDER
As the COVID-19 crisis escalated in New York City, it became evident that staff from other specialties would be essential to manage the surge of patients. Hospital administrators selected a group of trainees for deployment based on their clinical experiences and willingness to volunteer. Almost overnight, a group of senior pediatric residents became adult providers, honoring the oath we each took to “remain a member of society with special obligations to all . . . fellow human beings.”¹
This health crisis brought different clinical disciplines together like never before. Entire wings of the hospital were converted into new COVID-19–dedicated wards and intensive care units (ICUs), and teams were built to optimize providers’ skills and capabilities. For example, one third-year pediatric resident was grouped with an outpatient endocrinologist—who had not practiced inpatient medicine in a decade—and a medicine intern. Hospitalists provided crucial support and guidance to these ward teams of deployed providers who were eager and willing to work but often not very knowledgeable about inpatient adult medicine.² In new ad hoc COVID-19 ICUs housed in other ICUs, where most pediatric residents were deployed, critical care attendings and neurointensivists led teams that also included anesthesiology, radiology, and neurosurgery residents, as well as nurses and advanced practice providers trained in various subspecialties of adult medicine.
PEDIATRICIANS IN AN ADULT WORLD
Although we wanted to help in any way we could, the prospect of entering this new world was incredibly daunting. We had not treated adults in several years, and during that time, our clinical experience with pediatric medicine greatly surpassed our adult training from medical school. We dug out materials on adult diseases, watched impromptu lectures on COVID-19 given by our critical care attendings, taught ourselves ventilator management in adults, and reviewed advanced cardiac life support (ACLS) protocols. But putting this all into practice was entirely different. Nothing can truly prepare you for arriving at the bedside of a hemodynamically unstable patient suffering from a virus that no one really understands.
When we arrived and introduced ourselves, we occasionally encountered surprise and curiosity from other providers. We felt that there was a perception that pediatricians do not often take care of critically ill or complex patients. Some of us were reluctant to disclose our specialty, lest it cloud perceptions of our capabilities. However, sick patients awaited us, so we got to work.
There was a steep learning curve over the first few days, from adjusting insulin for type 2 diabetes to troubleshooting renal replacement therapy issues. Accustomed to pediatric weight-based dosing, we were very anxious about ordering medications. The adult providers on our teams oriented us and helped us with many of these concerns. But the mystery of COVID-19 was a great equalizing force, leaving providers of every background with questions: Should we anticoagulate? How about steroids? Could this clinical change be another effect of the virus or a new infection?
We were pleasantly surprised that many aspects of our pediatric training proved beneficial in caring for adults. The focus on family-centered rounds and shared decision-making in pediatrics had imprinted on us the paramount importance of good communication. We were very cognizant of involving loved ones in discussions, now conducted by telephone or video call because infection-prevention guidelines precluded visitors. Family members were thankful for frequent updates, and as a result, largely embraced us as the doctors treating their loved ones. On one occasion, an internist, whose mother was a patient, was delighted to learn that the provider was a pediatric resident, saying, “I know you’ll take such good care of her.”
With the hospital inundated with sick adults, colleagues were grateful for our help. More so, they seemed appreciative of our compassion and ability to maintain a sense of humanity during the pandemonium of the pandemic despite feeling vulnerable, scared, and often powerless against COVID-19. In pediatrics, we do our best to truly engage with patients, from playing games with a 6-year-old with perforated appendicitis to holding and soothing a newborn in the neonatal ICU. We carried those skills over to the adult side. The team appreciated when a pediatric resident, with the help of an occupational therapist, used a letter board to communicate and receive assent for a tracheostomy from a nonsedated, intubated patient, directly answering the patient’s questions and addressing concerns rather than relying solely on a family member’s consent. And, though we had not previously led end-of-life discussions, we found that we were capable of doing so with the compassion instilled in us from our pediatric training. It had prepared us to face the universal challenge of communication in times of grief.
COVID-19 CHALLENGES
Besides grappling with our insecurity in treating adults, we, like all medical providers, had to balance our desire to provide care while keeping ourselves safe from COVID-19. To reduce our risk of exposure and preserve the dwindling supply of personal protective equipment (PPE), the flow of rounding, bedside care, and interventions was adapted to better cluster examinations, blood draws, and bedside tasks. Although efficient, this meant we did not enter rooms as frequently, creating an unfamiliar distance between provider and patient.³ We feared missing moments of clinical decompensation, and for pediatricians who value close patient contact, this made for a deeply uncomfortable reality.
We considered every plausible treatment for critically ill patients, sometimes unsure if they were beneficial or instead complicating the course further. Was lack of improvement a treatment failure or just the natural progression of this new illness? Unfortunately, most of the time, treatments were to no avail. Watching the respiratory, cardiovascular, renal, and neurologic devastation of COVID-19 on so many patients was horrifying. Seeing patients die without their loved ones beside them and at an alarmingly fast rate was simply crushing, as other trainees have similarly described.4 It was unlike anything we had ever experienced in pediatrics. Though we had begun to see a few pediatric COVID-19 patients in the hospital, their disease course was less severe. And, in the rare cases when pediatric patients die, they are almost invariably surrounded by family. One pediatric resident, who had never performed a single death examination before, did three in 1 week. It was emotionally trying, yet we had little time to mourn, as deathbeds were only briefly empty before the next gravely ill patients filled them.
Deployment took a toll on our bodies as well. We padded our faces to alleviate skin breakdown from 12-hour shifts spent entirely in N95 masks. We sanitized and washed our hands constantly, developing cracked skin and dermatitis, and showered meticulously after every shift. We isolated ourselves from our families and loved ones to protect them from the virus.
MOMENTS OF POSITIVITY
Despite these challenges, positive moments emerged. We worked with many wonderful colleagues from different disciplines we likely never would have met, let alone work alongside. We valued each other’s skills, talents, and knowledge. On an overnight shift in one of the ICUs, among the “ragtag team of deployees,” as one pediatric resident phrased it, each presented a topic from his or her respective specialty that might interest others. The pediatrician presented Kawasaki disease, as adult colleagues were beginning to ask questions about its cousin, the emerging multisystem inflammatory syndrome in children (MIS-C). This collegiality promoted a culture of collaboration and respect for other specialties that will hopefully continue.
A strong drive toward teamwork and shared responsibility flourished during deployment. No one was above any task. Residents and even fellows performed typical frontline tasks, such as ordering laboratory work and coordinating imaging. We all helped the proning team turn patients. Everyone shared insights, perspectives, and information gleaned from friends in different wards and hospitals and the ever-evolving literature. As we grappled with unpredictable disease courses, the traditional hierarchical roles of medicine—attending, fellow, resident—often blurred. We felt like we were all in this together.
Patient triumphs were celebrated. We danced with an 80-year-old patient admitted for almost 2 weeks when she was informed of her discharge and gave a standing ovation for a 91-year-old woman as she headed home. Music played over the hospital loudspeaker for every patient discharge. We also tried to create moments of lightheartedness. In the ICUs, we ate donated meals together and posed for pictures to express our gratitude to restaurants. Camaraderie blossomed during deployment.
ADVICE FOR THE FUTURE
Answering the call to help during the COVID-19 surge in New York City indelibly shaped our experiences as trainees and physicians. We will carry with us the lessons that we learned, both in the short term for the possible resurgence of cases and in the long term for ongoing patient care for the rest of our careers. For those residents who may be called upon next, the experience will be challenging, but rewarding. Each trainee has a foundation of knowledge, abilities, and instincts that will be useful, so trust in your training. Do not be afraid to ask questions or for help. You may be leaving your comfort zone, but you will not be alone, and families and other clinicians will be grateful to have you there. You are resilient, and you will make a difference.
Disclosures
The authors have nothing to disclose.
Stepping onto a busy coronavirus disease (COVID-19) unit for the first time can elicit trepidation for any medical provider. For a group of deployed pediatric residents at a New York City hospital in the spring of 2020, it was also the first time caring for adults since medical school. Imagine a pediatrician receiving this handoff: “77-year-old female with a history of diabetes, peripheral vascular disease, and COPD admitted with COVID-19 pneumonia, now intubated and proned with O2 saturations in the 80s. To do: DNR discussion.” General anxiety around COVID-19 was compounded by the discomfort of being thrust into adult medicine. But the doctoring instinct we have been honing throughout training kicked in, and we acted.
A NEW ORDER
As the COVID-19 crisis escalated in New York City, it became evident that staff from other specialties would be essential to manage the surge of patients. Hospital administrators selected a group of trainees for deployment based on their clinical experiences and willingness to volunteer. Almost overnight, a group of senior pediatric residents became adult providers, honoring the oath we each took to “remain a member of society with special obligations to all . . . fellow human beings.”¹
This health crisis brought different clinical disciplines together like never before. Entire wings of the hospital were converted into new COVID-19–dedicated wards and intensive care units (ICUs), and teams were built to optimize providers’ skills and capabilities. For example, one third-year pediatric resident was grouped with an outpatient endocrinologist—who had not practiced inpatient medicine in a decade—and a medicine intern. Hospitalists provided crucial support and guidance to these ward teams of deployed providers who were eager and willing to work but often not very knowledgeable about inpatient adult medicine.² In new ad hoc COVID-19 ICUs housed in other ICUs, where most pediatric residents were deployed, critical care attendings and neurointensivists led teams that also included anesthesiology, radiology, and neurosurgery residents, as well as nurses and advanced practice providers trained in various subspecialties of adult medicine.
PEDIATRICIANS IN AN ADULT WORLD
Although we wanted to help in any way we could, the prospect of entering this new world was incredibly daunting. We had not treated adults in several years, and during that time, our clinical experience with pediatric medicine greatly surpassed our adult training from medical school. We dug out materials on adult diseases, watched impromptu lectures on COVID-19 given by our critical care attendings, taught ourselves ventilator management in adults, and reviewed advanced cardiac life support (ACLS) protocols. But putting this all into practice was entirely different. Nothing can truly prepare you for arriving at the bedside of a hemodynamically unstable patient suffering from a virus that no one really understands.
When we arrived and introduced ourselves, we occasionally encountered surprise and curiosity from other providers. We felt that there was a perception that pediatricians do not often take care of critically ill or complex patients. Some of us were reluctant to disclose our specialty, lest it cloud perceptions of our capabilities. However, sick patients awaited us, so we got to work.
There was a steep learning curve over the first few days, from adjusting insulin for type 2 diabetes to troubleshooting renal replacement therapy issues. Accustomed to pediatric weight-based dosing, we were very anxious about ordering medications. The adult providers on our teams oriented us and helped us with many of these concerns. But the mystery of COVID-19 was a great equalizing force, leaving providers of every background with questions: Should we anticoagulate? How about steroids? Could this clinical change be another effect of the virus or a new infection?
We were pleasantly surprised that many aspects of our pediatric training proved beneficial in caring for adults. The focus on family-centered rounds and shared decision-making in pediatrics had imprinted on us the paramount importance of good communication. We were very cognizant of involving loved ones in discussions, now conducted by telephone or video call because infection-prevention guidelines precluded visitors. Family members were thankful for frequent updates, and as a result, largely embraced us as the doctors treating their loved ones. On one occasion, an internist, whose mother was a patient, was delighted to learn that the provider was a pediatric resident, saying, “I know you’ll take such good care of her.”
With the hospital inundated with sick adults, colleagues were grateful for our help. More so, they seemed appreciative of our compassion and ability to maintain a sense of humanity during the pandemonium of the pandemic despite feeling vulnerable, scared, and often powerless against COVID-19. In pediatrics, we do our best to truly engage with patients, from playing games with a 6-year-old with perforated appendicitis to holding and soothing a newborn in the neonatal ICU. We carried those skills over to the adult side. The team appreciated when a pediatric resident, with the help of an occupational therapist, used a letter board to communicate and receive assent for a tracheostomy from a nonsedated, intubated patient, directly answering the patient’s questions and addressing concerns rather than relying solely on a family member’s consent. And, though we had not previously led end-of-life discussions, we found that we were capable of doing so with the compassion instilled in us from our pediatric training. It had prepared us to face the universal challenge of communication in times of grief.
COVID-19 CHALLENGES
Besides grappling with our insecurity in treating adults, we, like all medical providers, had to balance our desire to provide care while keeping ourselves safe from COVID-19. To reduce our risk of exposure and preserve the dwindling supply of personal protective equipment (PPE), the flow of rounding, bedside care, and interventions was adapted to better cluster examinations, blood draws, and bedside tasks. Although efficient, this meant we did not enter rooms as frequently, creating an unfamiliar distance between provider and patient.³ We feared missing moments of clinical decompensation, and for pediatricians who value close patient contact, this made for a deeply uncomfortable reality.
We considered every plausible treatment for critically ill patients, sometimes unsure if they were beneficial or instead complicating the course further. Was lack of improvement a treatment failure or just the natural progression of this new illness? Unfortunately, most of the time, treatments were to no avail. Watching the respiratory, cardiovascular, renal, and neurologic devastation of COVID-19 on so many patients was horrifying. Seeing patients die without their loved ones beside them and at an alarmingly fast rate was simply crushing, as other trainees have similarly described.4 It was unlike anything we had ever experienced in pediatrics. Though we had begun to see a few pediatric COVID-19 patients in the hospital, their disease course was less severe. And, in the rare cases when pediatric patients die, they are almost invariably surrounded by family. One pediatric resident, who had never performed a single death examination before, did three in 1 week. It was emotionally trying, yet we had little time to mourn, as deathbeds were only briefly empty before the next gravely ill patients filled them.
Deployment took a toll on our bodies as well. We padded our faces to alleviate skin breakdown from 12-hour shifts spent entirely in N95 masks. We sanitized and washed our hands constantly, developing cracked skin and dermatitis, and showered meticulously after every shift. We isolated ourselves from our families and loved ones to protect them from the virus.
MOMENTS OF POSITIVITY
Despite these challenges, positive moments emerged. We worked with many wonderful colleagues from different disciplines we likely never would have met, let alone work alongside. We valued each other’s skills, talents, and knowledge. On an overnight shift in one of the ICUs, among the “ragtag team of deployees,” as one pediatric resident phrased it, each presented a topic from his or her respective specialty that might interest others. The pediatrician presented Kawasaki disease, as adult colleagues were beginning to ask questions about its cousin, the emerging multisystem inflammatory syndrome in children (MIS-C). This collegiality promoted a culture of collaboration and respect for other specialties that will hopefully continue.
A strong drive toward teamwork and shared responsibility flourished during deployment. No one was above any task. Residents and even fellows performed typical frontline tasks, such as ordering laboratory work and coordinating imaging. We all helped the proning team turn patients. Everyone shared insights, perspectives, and information gleaned from friends in different wards and hospitals and the ever-evolving literature. As we grappled with unpredictable disease courses, the traditional hierarchical roles of medicine—attending, fellow, resident—often blurred. We felt like we were all in this together.
Patient triumphs were celebrated. We danced with an 80-year-old patient admitted for almost 2 weeks when she was informed of her discharge and gave a standing ovation for a 91-year-old woman as she headed home. Music played over the hospital loudspeaker for every patient discharge. We also tried to create moments of lightheartedness. In the ICUs, we ate donated meals together and posed for pictures to express our gratitude to restaurants. Camaraderie blossomed during deployment.
ADVICE FOR THE FUTURE
Answering the call to help during the COVID-19 surge in New York City indelibly shaped our experiences as trainees and physicians. We will carry with us the lessons that we learned, both in the short term for the possible resurgence of cases and in the long term for ongoing patient care for the rest of our careers. For those residents who may be called upon next, the experience will be challenging, but rewarding. Each trainee has a foundation of knowledge, abilities, and instincts that will be useful, so trust in your training. Do not be afraid to ask questions or for help. You may be leaving your comfort zone, but you will not be alone, and families and other clinicians will be grateful to have you there. You are resilient, and you will make a difference.
Disclosures
The authors have nothing to disclose.
1. Lasagna L. Hippocratic oath—modern version. Published 1964. Accessed September 14, 2020. http://www.pbs.org/wgbh/nova/doctors/oath_modern.html
2. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314-315.https://doi.org/10.12788/jhm.3426
3. Cunningham CO, Diaz C, Slawek DE. COVID-19: the worst days of our careers. Ann Intern Med. 2020;172(11):764-765. https://doi.org/10.7326/M20-1715
4. Gallagher TH, Schleyer AM. “We signed up for this!”—student and trainee responses to the COVID-19 pandemic. N Engl J Med. 2020;382(25):e96. https://doi.org/10.1056/NEJMp2005234
1. Lasagna L. Hippocratic oath—modern version. Published 1964. Accessed September 14, 2020. http://www.pbs.org/wgbh/nova/doctors/oath_modern.html
2. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314-315.https://doi.org/10.12788/jhm.3426
3. Cunningham CO, Diaz C, Slawek DE. COVID-19: the worst days of our careers. Ann Intern Med. 2020;172(11):764-765. https://doi.org/10.7326/M20-1715
4. Gallagher TH, Schleyer AM. “We signed up for this!”—student and trainee responses to the COVID-19 pandemic. N Engl J Med. 2020;382(25):e96. https://doi.org/10.1056/NEJMp2005234
© 2020 Society of Hospital Medicine
Professional Identity Formation During the COVID-19 Pandemic
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
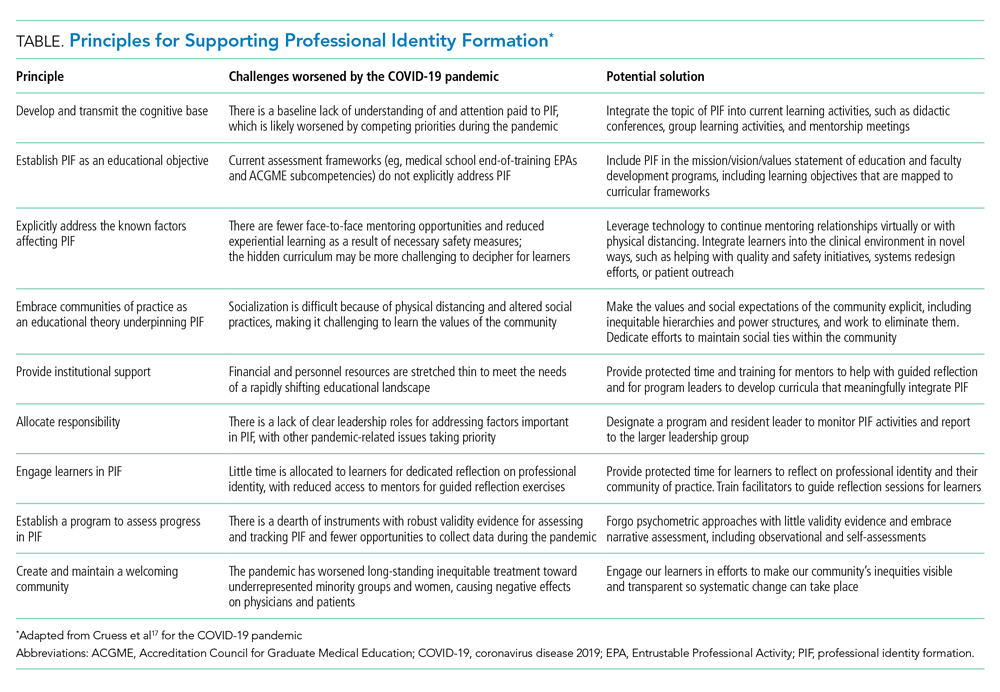
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
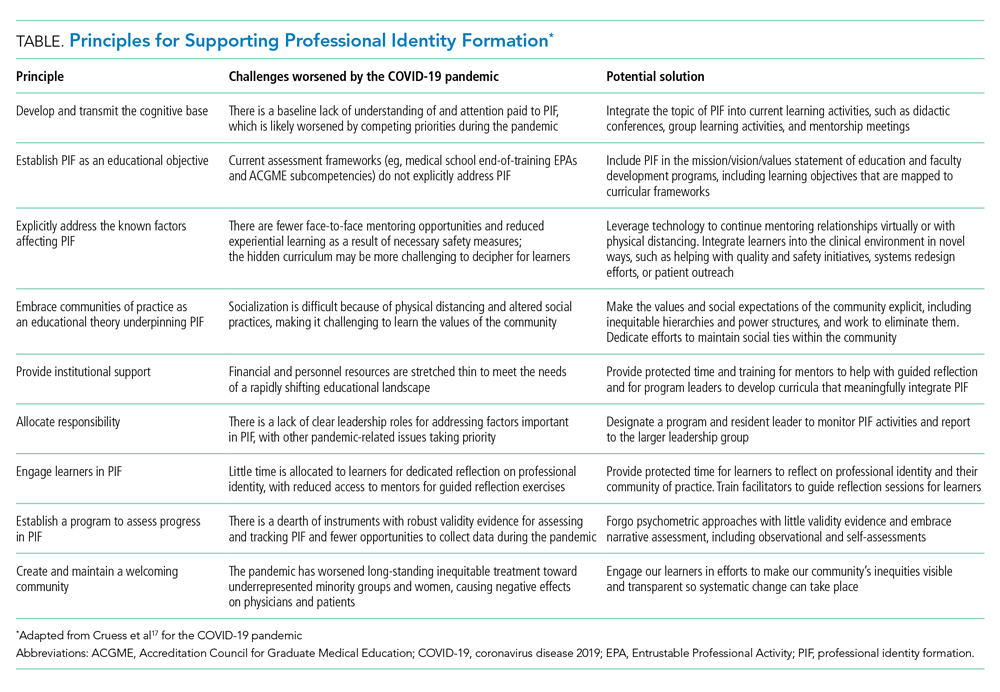
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
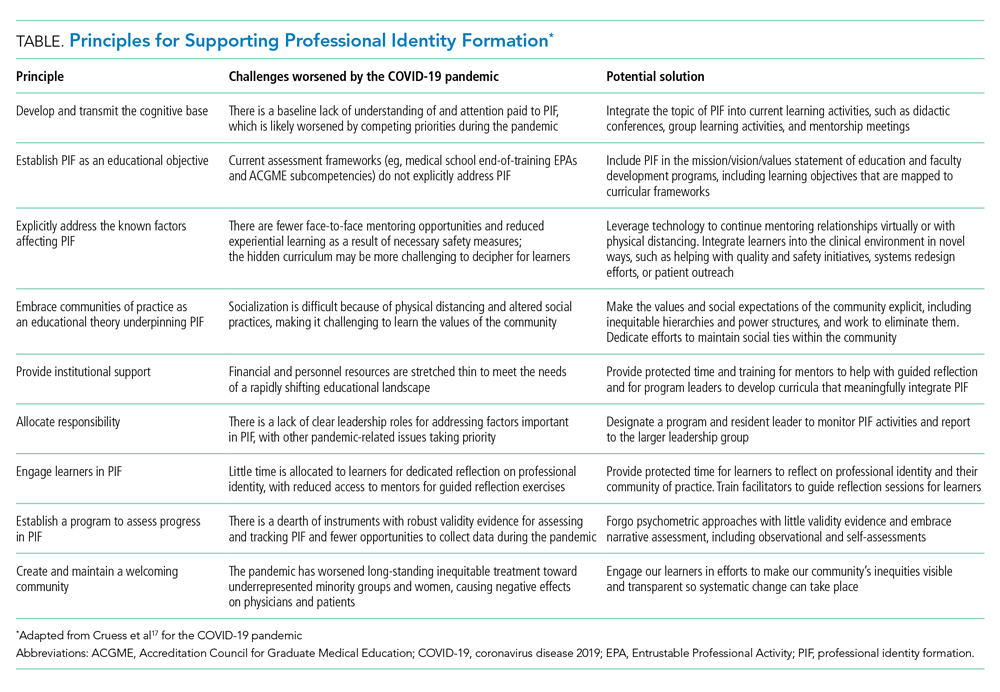
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
© 2021 Society of Hospital Medicine
Creating Psychological Safety on Medical Teams in Times of Crisis
Hospitalized patients receive care via a team-based approach. Because of frequent turnover and constant changes in team members, medical teams require rapid establishment of psychological safety. Psychological safety, or “being able to show and employ one’s self without fear of negative consequences of self-image, status or career,”1 is at the core of successful team functioning. Google studied successful teams and found diverse personalities and skillsets work together most productively if they incorporate certain team dynamics; chief among these are focusing on shared values and psychological safety.2 Times of acute crisis, especially those in which clinicians are working in unfamiliar settings and with new teams, increase the need for psychological safety. During the first wave of the coronavirus disease 2019 (COVID-19) pandemic, many hospitals responded by forming ad hoc teams of non-hospitalist clinicians, including redeployed outpatient physicians and subspecialists.3 Because this situation was an acute crisis in which strangers (some new to the field) were suddenly working side by side, it was an excellent example of a moment that required rapid establishment of psychological safety. As subsequent waves of COVID-19 arrive, this will likely occur again. In this perspective, we identify strategies that help to establish psychological safety on medical teams, aiming to increase the effectiveness of teams caring for hospitalized patients, enhance leaders’ abilities to improve team function, and allow for delivery of high-quality patient care.
WHY IS PSYCHOLOGICAL SAFETY IMPORTANT?
Psychological safety creates a nonthreatening team environment in which clinicians can ask questions and seek help with unfamiliar clinical scenarios. When psychological safety is present, the team dynamic encourages interpersonal risk-taking, improves learning, and increases the likelihood that team members will suggest new ideas.4 A culture of openness where people feel accepted and respected plays a vital role in helping people thrive in challenging and high-stakes work environments.5 In healthcare, team members who do not fear punishment for mistakes are more likely to disclose errors.6 Psychological safety has been associated with decreased anxiety in stressful situations, thereby freeing learners’ mental capacity to explore, innovate, and absorb new information.6
STRATEGIES TO IMPLEMENT PSYCHOLOGICAL SAFETY
Through a thorough literature review, we identified strategies that can increase psychological safety on clinical teams. We focused on strategies applicable to acute crises, like COVID-19, when dynamic teams and uncertainty are rife. These strategies primarily focus on “team leaders,” generally the attendings or senior residents, who influence the team’s culture.
Discuss Mistakes
Creating a culture in which openly discussing mistakes is normalized and learning is fostered is especially important for healthcare providers redeployed to COVID-19 wards. Acknowledging errors can be challenging, especially in medicine, because success is often celebrated.7 Creating an environment where discussing mistakes in a nonjudgmental manner is the norm helps people disclose and learn from errors. By modeling fallibility, team leaders can create an environment where learning from mistakes seems less threatening.8 Leaders can say, “I may miss something. I encourage all members of the team to share what they know.”9
Provide Frequent Updates and Seek Feedback
Information and guidelines are changing frequently as we learn more about the novel coronavirus. The barrage of new information and periodic policy changes can be disconcerting. Leaders can dispel some of the team’s anxiety by providing a unified message that distills new information into clear and essential updates.9 They can reassure the team that updates will be provided frequently, be honest about what is known, and offer some predictability by providing updates at set times via consistent forms of communication during times of crisis. They can show empathy by inquiring about individual worries and responding to concerns about changes that are being made in response to COVID-19.10 Leaders should routinely seek feedback. They can ask, “How are things going for you? What can we improve? What should we do differently? How can I make you feel more comfortable or help you learn more effectively?” Inviting input communicates that everyone’s opinion is respected and creates a climate where everyone feels comfortable asking questions or respectfully expressing diverging opinions.9
Foster Creativity and Seek New Ideas
Curiosity and creativity are associated with better group outcomes.11 Curiosity, or the motivation to learn and seek new ideas, improves individual and group dynamics by stimulating better job performance, inspiring leaders to discover more creative solutions, and encouraging employees to develop more trusting relationships, which makes them less likely to stereotype coworkers and patients as they ask questions and learn about others.12 People who approach situations with a more creative perspective are less likely to react defensively. Curious people tend to try to learn about and understand different points of view.13 For example, if an order is not placed for a patient, a curious team leader might think about why—was there disagreement on the order, confusion on how to place it, or was it inadvertently forgotten?—and be able help avoid similar scenarios in the future. This ability to see things from another person’s point of view helps individuals with diverse clinical, social, and ethnic backgrounds function as a harmonious team. An attitude of curiosity and interest in learning about what each person can contribute based on their unique training and personality will help well-functioning teams form in response to COVID-19. Openness to new ideas allows for more innovative solutions, which are important in times of crisis. To promote curiosity, team members should discuss differences and varied opinions openly. This open dialogue provides individuals opportunities to learn from each other.5
Build Connection and Trust
A culture of trust—the belief that others will act for the good of the team—helps create psychological safety.10 Leaders can build trust by making expectations clear, being consistent, being inclusive, and modeling behaviors they wish to encourage.6 Predictability reduces anxiety and promotes psychological safety.9 Defining goals and expectations helps people relax, ask questions, and focus on learning.14 In times of crisis, leaders can tell teams what changes to expect, spell out new priorities, and assign specific tasks to give people a way to contribute.15
Activities that create connection also build trust, enhancing the team’s sense of psychological safety. Shared experiences foster connections.2 Leaders can encourage team bonding by setting aside time to share stories and coping strategies.10 Chief residents in the early days of the pandemic found defining social distancing only as physical separation and focusing on emotional bonds helped maintain a sense of community. Debriefing about emotional patient encounters and discussing interesting clinical cases during video calls were ways to implement this strategy.10 Team members feel connected to each other and dedicated to their work if they focus on the meaning of the work to them, as well as its impact on society.2 This shared belief that what they are doing matters to their community helps bond them.2 Currently, the shared experience of treating a novel illness during the COVID-19 pandemic and the common goal of patient well-being unites healthcare providers across the globe. Leaders can create solidarity by emphasizing the shared identity of fighting COVID-19 and reminding teams of the impact of their work. Leaders can say, “Remember, we are here to improve patients’ health and form emotional bonds with people and their families.” These reminders have been shown to promote psychological safety and connection.16
Make Team Members Feel Valued
As many healthcare providers work harder or in unfamiliar environments during this pandemic, recognition of their efforts by leaders can be especially motivating and meaningful. When individuals on a team feel their work is valued, it helps create a sense of psychological safety.17 Employees feel valued when they believe their leaders care, they are in socially supportive environments, and are given resources for professional growth.17 Diversity and inclusion are also associated with feeling valued.17 During the height of the initial COVID-19 surge at our hospital, the chief of the Department of Medicine regularly sent messages and photographs of trainees and faculty, showing teams coming together during these unprecedented times. This boosted morale and created comradery and is an excellent example of a leader modeling inclusion.
Gratitude strengthens relationships and motivates people, especially when its expression is thoughtful and unique to individuals.18 Sincere compliments, acknowledgement of hard work, inclusiveness, and gratitude all contribute to team members feeling at ease and are key to leading, especially in times of crisis.17 Leaders can provide motivation by affirming the team’s ability to work together. Leaders can say, “I believe in each and every one of your capabilities—and I believe even more so in our joint capabilities. We can do this together.”19
CONCLUSION
Psychological safety is a powerful predictor of team performance, increased engagement, and satisfaction. It is critical for creating teams that can deal with uncertainty in high-risk situations, promoting a culture that is safe to acknowledge mistakes and take chances, which is important for optimal team functioning. Crises like the COVID-19 pandemic emphasize the need for psychologically safe team climates to promote learning, safe patient care, and team support. Hospitalists often care for patients when they are at their most vulnerable. Respecting and connecting with patients, through good and efficient teamwork, is important to providing effective care. The strategies suggested in this article strive to help hospitalists create a respectful culture to strengthen relationships with patients and colleagues in order to create an inclusive environment in times of crisis.
1. Kahn WA. Psychological conditions of personal engagement and disengagement at work. Acad Manage J. 1990;33(4):692-724. https://doi.org/10.5465/256287
2. Rozovsky J. The five keys to a successful Google team. re:Work. Posted November 17, 2015. Accessed October 11, 2020. https://rework.withgoogle.com/blog/five-keys-to-a-successful-google-team/
3. Hettle D, Sutherland K, Miles E, et al. Cross-skilling training to support medical redeployment in the COVID-19 pandemic. Future Healthc J. 2020:fhj.2020-0049. https://doi.org/10.7861/fhj.2020-0049
4. Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23-43. https://doi.org/10.1146/annurev-orgpsych-031413-091305
5. Edmondson A. Psychological safety and learning behavior in work teams. Admin Sci Quart.1999;44(2):350-383. https://doi.org/10.2307/2666999
6. Turner S, Harder N. Psychological safe environment: a concept analysis. Clin Simul Nurs. 2018;18:47-55. https://doi.org/10.1016/j.ecns.2018.02.004
7. Jug R, Jiang XS, Bean SM. Giving and receiving effective feedback: a review article and how-to guide. Arch Pathol Lab Med. 2019;143(2):244-250. https://doi.org/10.5858/arpa.2018-0058-RA
8. Ende J. Feedback in clinical medical education. JAMA. 1983;250(6):777-781. https://doi.org/10.1001/jama.1983.03340060055026
9. Edmondson AC, Woolley AW. Understanding outcomes of organizational learning interventions. In: Easterby-Smith M, Lyles M, eds. Blackwell Handbook of Organizational Learning and Knowledge Management. Blackwell Publishing; 2003.
10. Rakowsky S, Flashner BM, Doolin J, et al. Five questions for residency leadership in the time of COVID-19: reflections of chief medical residents from an internal medicine program. Acad Med. 2020;95(8):1152-1154. https://doi.org/10.1097/ACM.0000000000003419
11. Armstrong K. If you can’t beat it, join it: uncertainty and trust in medicine. Ann Intern Med. 2018;168(11):818-819. https://doi.org/10.7326/M18-0445
12. Gino F. The business case for curiosity. Harvard Bus Rev. 2018;96(5):48-57.
13. Kashdan TB, DeWall CN, Pond RS, et al. Curiosity protects against interpersonal aggression: cross-sectional, daily process, and behavioral evidence. J Pers. 2013;81(1):87-102. https://doi.org/10.1111/j.1467-6494.2012.00783.x
14. Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301-303. https://doi.org/10.1097/ACM.0b013e318280cff0
15. Petriglieri G. The psychology behind effective crisis leadership. Harvard Bus Rev. Published April 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/the-psychology-behind-effective-crisis-leadership
16. Edmondson A. Building a psychologically safe workplace: TEDx Talk. May 4, 2014. Accessed October 11, 2020. https://youtube.com/watch?v=LhoLuui9gX8
17. Simpkin AL, Chang Y, Yu L, Campbell EG, Armstrong K, Walensky RP. Assessment of job satisfaction and feeling valued in academic medicine. JAMA Intern Med. 2019;179(7):992-994. https://doi.org/10.1001/jamainternmed.2019.0377
18. Nawaz S. In times of crisis, a little thanks goes a long way. Harvard Bus Rev. Published May 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/05/in-times-of-crisis-a-little-thanks-goes-a-long-way
19. Knight R. How to talk to your team when the future is uncertain. Harvard Bus Rev. Published April 20, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/how-to-talk-to-your-team-when-the-future-is-uncertain
Hospitalized patients receive care via a team-based approach. Because of frequent turnover and constant changes in team members, medical teams require rapid establishment of psychological safety. Psychological safety, or “being able to show and employ one’s self without fear of negative consequences of self-image, status or career,”1 is at the core of successful team functioning. Google studied successful teams and found diverse personalities and skillsets work together most productively if they incorporate certain team dynamics; chief among these are focusing on shared values and psychological safety.2 Times of acute crisis, especially those in which clinicians are working in unfamiliar settings and with new teams, increase the need for psychological safety. During the first wave of the coronavirus disease 2019 (COVID-19) pandemic, many hospitals responded by forming ad hoc teams of non-hospitalist clinicians, including redeployed outpatient physicians and subspecialists.3 Because this situation was an acute crisis in which strangers (some new to the field) were suddenly working side by side, it was an excellent example of a moment that required rapid establishment of psychological safety. As subsequent waves of COVID-19 arrive, this will likely occur again. In this perspective, we identify strategies that help to establish psychological safety on medical teams, aiming to increase the effectiveness of teams caring for hospitalized patients, enhance leaders’ abilities to improve team function, and allow for delivery of high-quality patient care.
WHY IS PSYCHOLOGICAL SAFETY IMPORTANT?
Psychological safety creates a nonthreatening team environment in which clinicians can ask questions and seek help with unfamiliar clinical scenarios. When psychological safety is present, the team dynamic encourages interpersonal risk-taking, improves learning, and increases the likelihood that team members will suggest new ideas.4 A culture of openness where people feel accepted and respected plays a vital role in helping people thrive in challenging and high-stakes work environments.5 In healthcare, team members who do not fear punishment for mistakes are more likely to disclose errors.6 Psychological safety has been associated with decreased anxiety in stressful situations, thereby freeing learners’ mental capacity to explore, innovate, and absorb new information.6
STRATEGIES TO IMPLEMENT PSYCHOLOGICAL SAFETY
Through a thorough literature review, we identified strategies that can increase psychological safety on clinical teams. We focused on strategies applicable to acute crises, like COVID-19, when dynamic teams and uncertainty are rife. These strategies primarily focus on “team leaders,” generally the attendings or senior residents, who influence the team’s culture.
Discuss Mistakes
Creating a culture in which openly discussing mistakes is normalized and learning is fostered is especially important for healthcare providers redeployed to COVID-19 wards. Acknowledging errors can be challenging, especially in medicine, because success is often celebrated.7 Creating an environment where discussing mistakes in a nonjudgmental manner is the norm helps people disclose and learn from errors. By modeling fallibility, team leaders can create an environment where learning from mistakes seems less threatening.8 Leaders can say, “I may miss something. I encourage all members of the team to share what they know.”9
Provide Frequent Updates and Seek Feedback
Information and guidelines are changing frequently as we learn more about the novel coronavirus. The barrage of new information and periodic policy changes can be disconcerting. Leaders can dispel some of the team’s anxiety by providing a unified message that distills new information into clear and essential updates.9 They can reassure the team that updates will be provided frequently, be honest about what is known, and offer some predictability by providing updates at set times via consistent forms of communication during times of crisis. They can show empathy by inquiring about individual worries and responding to concerns about changes that are being made in response to COVID-19.10 Leaders should routinely seek feedback. They can ask, “How are things going for you? What can we improve? What should we do differently? How can I make you feel more comfortable or help you learn more effectively?” Inviting input communicates that everyone’s opinion is respected and creates a climate where everyone feels comfortable asking questions or respectfully expressing diverging opinions.9
Foster Creativity and Seek New Ideas
Curiosity and creativity are associated with better group outcomes.11 Curiosity, or the motivation to learn and seek new ideas, improves individual and group dynamics by stimulating better job performance, inspiring leaders to discover more creative solutions, and encouraging employees to develop more trusting relationships, which makes them less likely to stereotype coworkers and patients as they ask questions and learn about others.12 People who approach situations with a more creative perspective are less likely to react defensively. Curious people tend to try to learn about and understand different points of view.13 For example, if an order is not placed for a patient, a curious team leader might think about why—was there disagreement on the order, confusion on how to place it, or was it inadvertently forgotten?—and be able help avoid similar scenarios in the future. This ability to see things from another person’s point of view helps individuals with diverse clinical, social, and ethnic backgrounds function as a harmonious team. An attitude of curiosity and interest in learning about what each person can contribute based on their unique training and personality will help well-functioning teams form in response to COVID-19. Openness to new ideas allows for more innovative solutions, which are important in times of crisis. To promote curiosity, team members should discuss differences and varied opinions openly. This open dialogue provides individuals opportunities to learn from each other.5
Build Connection and Trust
A culture of trust—the belief that others will act for the good of the team—helps create psychological safety.10 Leaders can build trust by making expectations clear, being consistent, being inclusive, and modeling behaviors they wish to encourage.6 Predictability reduces anxiety and promotes psychological safety.9 Defining goals and expectations helps people relax, ask questions, and focus on learning.14 In times of crisis, leaders can tell teams what changes to expect, spell out new priorities, and assign specific tasks to give people a way to contribute.15
Activities that create connection also build trust, enhancing the team’s sense of psychological safety. Shared experiences foster connections.2 Leaders can encourage team bonding by setting aside time to share stories and coping strategies.10 Chief residents in the early days of the pandemic found defining social distancing only as physical separation and focusing on emotional bonds helped maintain a sense of community. Debriefing about emotional patient encounters and discussing interesting clinical cases during video calls were ways to implement this strategy.10 Team members feel connected to each other and dedicated to their work if they focus on the meaning of the work to them, as well as its impact on society.2 This shared belief that what they are doing matters to their community helps bond them.2 Currently, the shared experience of treating a novel illness during the COVID-19 pandemic and the common goal of patient well-being unites healthcare providers across the globe. Leaders can create solidarity by emphasizing the shared identity of fighting COVID-19 and reminding teams of the impact of their work. Leaders can say, “Remember, we are here to improve patients’ health and form emotional bonds with people and their families.” These reminders have been shown to promote psychological safety and connection.16
Make Team Members Feel Valued
As many healthcare providers work harder or in unfamiliar environments during this pandemic, recognition of their efforts by leaders can be especially motivating and meaningful. When individuals on a team feel their work is valued, it helps create a sense of psychological safety.17 Employees feel valued when they believe their leaders care, they are in socially supportive environments, and are given resources for professional growth.17 Diversity and inclusion are also associated with feeling valued.17 During the height of the initial COVID-19 surge at our hospital, the chief of the Department of Medicine regularly sent messages and photographs of trainees and faculty, showing teams coming together during these unprecedented times. This boosted morale and created comradery and is an excellent example of a leader modeling inclusion.
Gratitude strengthens relationships and motivates people, especially when its expression is thoughtful and unique to individuals.18 Sincere compliments, acknowledgement of hard work, inclusiveness, and gratitude all contribute to team members feeling at ease and are key to leading, especially in times of crisis.17 Leaders can provide motivation by affirming the team’s ability to work together. Leaders can say, “I believe in each and every one of your capabilities—and I believe even more so in our joint capabilities. We can do this together.”19
CONCLUSION
Psychological safety is a powerful predictor of team performance, increased engagement, and satisfaction. It is critical for creating teams that can deal with uncertainty in high-risk situations, promoting a culture that is safe to acknowledge mistakes and take chances, which is important for optimal team functioning. Crises like the COVID-19 pandemic emphasize the need for psychologically safe team climates to promote learning, safe patient care, and team support. Hospitalists often care for patients when they are at their most vulnerable. Respecting and connecting with patients, through good and efficient teamwork, is important to providing effective care. The strategies suggested in this article strive to help hospitalists create a respectful culture to strengthen relationships with patients and colleagues in order to create an inclusive environment in times of crisis.
Hospitalized patients receive care via a team-based approach. Because of frequent turnover and constant changes in team members, medical teams require rapid establishment of psychological safety. Psychological safety, or “being able to show and employ one’s self without fear of negative consequences of self-image, status or career,”1 is at the core of successful team functioning. Google studied successful teams and found diverse personalities and skillsets work together most productively if they incorporate certain team dynamics; chief among these are focusing on shared values and psychological safety.2 Times of acute crisis, especially those in which clinicians are working in unfamiliar settings and with new teams, increase the need for psychological safety. During the first wave of the coronavirus disease 2019 (COVID-19) pandemic, many hospitals responded by forming ad hoc teams of non-hospitalist clinicians, including redeployed outpatient physicians and subspecialists.3 Because this situation was an acute crisis in which strangers (some new to the field) were suddenly working side by side, it was an excellent example of a moment that required rapid establishment of psychological safety. As subsequent waves of COVID-19 arrive, this will likely occur again. In this perspective, we identify strategies that help to establish psychological safety on medical teams, aiming to increase the effectiveness of teams caring for hospitalized patients, enhance leaders’ abilities to improve team function, and allow for delivery of high-quality patient care.
WHY IS PSYCHOLOGICAL SAFETY IMPORTANT?
Psychological safety creates a nonthreatening team environment in which clinicians can ask questions and seek help with unfamiliar clinical scenarios. When psychological safety is present, the team dynamic encourages interpersonal risk-taking, improves learning, and increases the likelihood that team members will suggest new ideas.4 A culture of openness where people feel accepted and respected plays a vital role in helping people thrive in challenging and high-stakes work environments.5 In healthcare, team members who do not fear punishment for mistakes are more likely to disclose errors.6 Psychological safety has been associated with decreased anxiety in stressful situations, thereby freeing learners’ mental capacity to explore, innovate, and absorb new information.6
STRATEGIES TO IMPLEMENT PSYCHOLOGICAL SAFETY
Through a thorough literature review, we identified strategies that can increase psychological safety on clinical teams. We focused on strategies applicable to acute crises, like COVID-19, when dynamic teams and uncertainty are rife. These strategies primarily focus on “team leaders,” generally the attendings or senior residents, who influence the team’s culture.
Discuss Mistakes
Creating a culture in which openly discussing mistakes is normalized and learning is fostered is especially important for healthcare providers redeployed to COVID-19 wards. Acknowledging errors can be challenging, especially in medicine, because success is often celebrated.7 Creating an environment where discussing mistakes in a nonjudgmental manner is the norm helps people disclose and learn from errors. By modeling fallibility, team leaders can create an environment where learning from mistakes seems less threatening.8 Leaders can say, “I may miss something. I encourage all members of the team to share what they know.”9
Provide Frequent Updates and Seek Feedback
Information and guidelines are changing frequently as we learn more about the novel coronavirus. The barrage of new information and periodic policy changes can be disconcerting. Leaders can dispel some of the team’s anxiety by providing a unified message that distills new information into clear and essential updates.9 They can reassure the team that updates will be provided frequently, be honest about what is known, and offer some predictability by providing updates at set times via consistent forms of communication during times of crisis. They can show empathy by inquiring about individual worries and responding to concerns about changes that are being made in response to COVID-19.10 Leaders should routinely seek feedback. They can ask, “How are things going for you? What can we improve? What should we do differently? How can I make you feel more comfortable or help you learn more effectively?” Inviting input communicates that everyone’s opinion is respected and creates a climate where everyone feels comfortable asking questions or respectfully expressing diverging opinions.9
Foster Creativity and Seek New Ideas
Curiosity and creativity are associated with better group outcomes.11 Curiosity, or the motivation to learn and seek new ideas, improves individual and group dynamics by stimulating better job performance, inspiring leaders to discover more creative solutions, and encouraging employees to develop more trusting relationships, which makes them less likely to stereotype coworkers and patients as they ask questions and learn about others.12 People who approach situations with a more creative perspective are less likely to react defensively. Curious people tend to try to learn about and understand different points of view.13 For example, if an order is not placed for a patient, a curious team leader might think about why—was there disagreement on the order, confusion on how to place it, or was it inadvertently forgotten?—and be able help avoid similar scenarios in the future. This ability to see things from another person’s point of view helps individuals with diverse clinical, social, and ethnic backgrounds function as a harmonious team. An attitude of curiosity and interest in learning about what each person can contribute based on their unique training and personality will help well-functioning teams form in response to COVID-19. Openness to new ideas allows for more innovative solutions, which are important in times of crisis. To promote curiosity, team members should discuss differences and varied opinions openly. This open dialogue provides individuals opportunities to learn from each other.5
Build Connection and Trust
A culture of trust—the belief that others will act for the good of the team—helps create psychological safety.10 Leaders can build trust by making expectations clear, being consistent, being inclusive, and modeling behaviors they wish to encourage.6 Predictability reduces anxiety and promotes psychological safety.9 Defining goals and expectations helps people relax, ask questions, and focus on learning.14 In times of crisis, leaders can tell teams what changes to expect, spell out new priorities, and assign specific tasks to give people a way to contribute.15
Activities that create connection also build trust, enhancing the team’s sense of psychological safety. Shared experiences foster connections.2 Leaders can encourage team bonding by setting aside time to share stories and coping strategies.10 Chief residents in the early days of the pandemic found defining social distancing only as physical separation and focusing on emotional bonds helped maintain a sense of community. Debriefing about emotional patient encounters and discussing interesting clinical cases during video calls were ways to implement this strategy.10 Team members feel connected to each other and dedicated to their work if they focus on the meaning of the work to them, as well as its impact on society.2 This shared belief that what they are doing matters to their community helps bond them.2 Currently, the shared experience of treating a novel illness during the COVID-19 pandemic and the common goal of patient well-being unites healthcare providers across the globe. Leaders can create solidarity by emphasizing the shared identity of fighting COVID-19 and reminding teams of the impact of their work. Leaders can say, “Remember, we are here to improve patients’ health and form emotional bonds with people and their families.” These reminders have been shown to promote psychological safety and connection.16
Make Team Members Feel Valued
As many healthcare providers work harder or in unfamiliar environments during this pandemic, recognition of their efforts by leaders can be especially motivating and meaningful. When individuals on a team feel their work is valued, it helps create a sense of psychological safety.17 Employees feel valued when they believe their leaders care, they are in socially supportive environments, and are given resources for professional growth.17 Diversity and inclusion are also associated with feeling valued.17 During the height of the initial COVID-19 surge at our hospital, the chief of the Department of Medicine regularly sent messages and photographs of trainees and faculty, showing teams coming together during these unprecedented times. This boosted morale and created comradery and is an excellent example of a leader modeling inclusion.
Gratitude strengthens relationships and motivates people, especially when its expression is thoughtful and unique to individuals.18 Sincere compliments, acknowledgement of hard work, inclusiveness, and gratitude all contribute to team members feeling at ease and are key to leading, especially in times of crisis.17 Leaders can provide motivation by affirming the team’s ability to work together. Leaders can say, “I believe in each and every one of your capabilities—and I believe even more so in our joint capabilities. We can do this together.”19
CONCLUSION
Psychological safety is a powerful predictor of team performance, increased engagement, and satisfaction. It is critical for creating teams that can deal with uncertainty in high-risk situations, promoting a culture that is safe to acknowledge mistakes and take chances, which is important for optimal team functioning. Crises like the COVID-19 pandemic emphasize the need for psychologically safe team climates to promote learning, safe patient care, and team support. Hospitalists often care for patients when they are at their most vulnerable. Respecting and connecting with patients, through good and efficient teamwork, is important to providing effective care. The strategies suggested in this article strive to help hospitalists create a respectful culture to strengthen relationships with patients and colleagues in order to create an inclusive environment in times of crisis.
1. Kahn WA. Psychological conditions of personal engagement and disengagement at work. Acad Manage J. 1990;33(4):692-724. https://doi.org/10.5465/256287
2. Rozovsky J. The five keys to a successful Google team. re:Work. Posted November 17, 2015. Accessed October 11, 2020. https://rework.withgoogle.com/blog/five-keys-to-a-successful-google-team/
3. Hettle D, Sutherland K, Miles E, et al. Cross-skilling training to support medical redeployment in the COVID-19 pandemic. Future Healthc J. 2020:fhj.2020-0049. https://doi.org/10.7861/fhj.2020-0049
4. Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23-43. https://doi.org/10.1146/annurev-orgpsych-031413-091305
5. Edmondson A. Psychological safety and learning behavior in work teams. Admin Sci Quart.1999;44(2):350-383. https://doi.org/10.2307/2666999
6. Turner S, Harder N. Psychological safe environment: a concept analysis. Clin Simul Nurs. 2018;18:47-55. https://doi.org/10.1016/j.ecns.2018.02.004
7. Jug R, Jiang XS, Bean SM. Giving and receiving effective feedback: a review article and how-to guide. Arch Pathol Lab Med. 2019;143(2):244-250. https://doi.org/10.5858/arpa.2018-0058-RA
8. Ende J. Feedback in clinical medical education. JAMA. 1983;250(6):777-781. https://doi.org/10.1001/jama.1983.03340060055026
9. Edmondson AC, Woolley AW. Understanding outcomes of organizational learning interventions. In: Easterby-Smith M, Lyles M, eds. Blackwell Handbook of Organizational Learning and Knowledge Management. Blackwell Publishing; 2003.
10. Rakowsky S, Flashner BM, Doolin J, et al. Five questions for residency leadership in the time of COVID-19: reflections of chief medical residents from an internal medicine program. Acad Med. 2020;95(8):1152-1154. https://doi.org/10.1097/ACM.0000000000003419
11. Armstrong K. If you can’t beat it, join it: uncertainty and trust in medicine. Ann Intern Med. 2018;168(11):818-819. https://doi.org/10.7326/M18-0445
12. Gino F. The business case for curiosity. Harvard Bus Rev. 2018;96(5):48-57.
13. Kashdan TB, DeWall CN, Pond RS, et al. Curiosity protects against interpersonal aggression: cross-sectional, daily process, and behavioral evidence. J Pers. 2013;81(1):87-102. https://doi.org/10.1111/j.1467-6494.2012.00783.x
14. Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301-303. https://doi.org/10.1097/ACM.0b013e318280cff0
15. Petriglieri G. The psychology behind effective crisis leadership. Harvard Bus Rev. Published April 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/the-psychology-behind-effective-crisis-leadership
16. Edmondson A. Building a psychologically safe workplace: TEDx Talk. May 4, 2014. Accessed October 11, 2020. https://youtube.com/watch?v=LhoLuui9gX8
17. Simpkin AL, Chang Y, Yu L, Campbell EG, Armstrong K, Walensky RP. Assessment of job satisfaction and feeling valued in academic medicine. JAMA Intern Med. 2019;179(7):992-994. https://doi.org/10.1001/jamainternmed.2019.0377
18. Nawaz S. In times of crisis, a little thanks goes a long way. Harvard Bus Rev. Published May 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/05/in-times-of-crisis-a-little-thanks-goes-a-long-way
19. Knight R. How to talk to your team when the future is uncertain. Harvard Bus Rev. Published April 20, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/how-to-talk-to-your-team-when-the-future-is-uncertain
1. Kahn WA. Psychological conditions of personal engagement and disengagement at work. Acad Manage J. 1990;33(4):692-724. https://doi.org/10.5465/256287
2. Rozovsky J. The five keys to a successful Google team. re:Work. Posted November 17, 2015. Accessed October 11, 2020. https://rework.withgoogle.com/blog/five-keys-to-a-successful-google-team/
3. Hettle D, Sutherland K, Miles E, et al. Cross-skilling training to support medical redeployment in the COVID-19 pandemic. Future Healthc J. 2020:fhj.2020-0049. https://doi.org/10.7861/fhj.2020-0049
4. Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23-43. https://doi.org/10.1146/annurev-orgpsych-031413-091305
5. Edmondson A. Psychological safety and learning behavior in work teams. Admin Sci Quart.1999;44(2):350-383. https://doi.org/10.2307/2666999
6. Turner S, Harder N. Psychological safe environment: a concept analysis. Clin Simul Nurs. 2018;18:47-55. https://doi.org/10.1016/j.ecns.2018.02.004
7. Jug R, Jiang XS, Bean SM. Giving and receiving effective feedback: a review article and how-to guide. Arch Pathol Lab Med. 2019;143(2):244-250. https://doi.org/10.5858/arpa.2018-0058-RA
8. Ende J. Feedback in clinical medical education. JAMA. 1983;250(6):777-781. https://doi.org/10.1001/jama.1983.03340060055026
9. Edmondson AC, Woolley AW. Understanding outcomes of organizational learning interventions. In: Easterby-Smith M, Lyles M, eds. Blackwell Handbook of Organizational Learning and Knowledge Management. Blackwell Publishing; 2003.
10. Rakowsky S, Flashner BM, Doolin J, et al. Five questions for residency leadership in the time of COVID-19: reflections of chief medical residents from an internal medicine program. Acad Med. 2020;95(8):1152-1154. https://doi.org/10.1097/ACM.0000000000003419
11. Armstrong K. If you can’t beat it, join it: uncertainty and trust in medicine. Ann Intern Med. 2018;168(11):818-819. https://doi.org/10.7326/M18-0445
12. Gino F. The business case for curiosity. Harvard Bus Rev. 2018;96(5):48-57.
13. Kashdan TB, DeWall CN, Pond RS, et al. Curiosity protects against interpersonal aggression: cross-sectional, daily process, and behavioral evidence. J Pers. 2013;81(1):87-102. https://doi.org/10.1111/j.1467-6494.2012.00783.x
14. Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301-303. https://doi.org/10.1097/ACM.0b013e318280cff0
15. Petriglieri G. The psychology behind effective crisis leadership. Harvard Bus Rev. Published April 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/the-psychology-behind-effective-crisis-leadership
16. Edmondson A. Building a psychologically safe workplace: TEDx Talk. May 4, 2014. Accessed October 11, 2020. https://youtube.com/watch?v=LhoLuui9gX8
17. Simpkin AL, Chang Y, Yu L, Campbell EG, Armstrong K, Walensky RP. Assessment of job satisfaction and feeling valued in academic medicine. JAMA Intern Med. 2019;179(7):992-994. https://doi.org/10.1001/jamainternmed.2019.0377
18. Nawaz S. In times of crisis, a little thanks goes a long way. Harvard Bus Rev. Published May 22, 2020. Accessed October 11, 2020. https://hbr.org/2020/05/in-times-of-crisis-a-little-thanks-goes-a-long-way
19. Knight R. How to talk to your team when the future is uncertain. Harvard Bus Rev. Published April 20, 2020. Accessed October 11, 2020. https://hbr.org/2020/04/how-to-talk-to-your-team-when-the-future-is-uncertain
© 2021 Society of Hospital Medicine
Masks, Seat Belts, and the Politicization of Public Health
At the time this piece was written, 54 Florida hospitals reported no available intensive care unit (ICU) beds1; hospitals in Miami-Dade County even started sending patients to neighboring Broward County for care despite Broward County also reporting a hospital bed shortage. Patients might even have needed to be transferred further north to Palm Beach County.2 Miami-Dade County was diagnosing over 100 cases with SARS-CoV-2 per 100,000 residents per day at one point, with a test positivity rate of over 25% that suggests testing is inadequate and many more would-be positive tests are being missed.3 While certain parts of the United States seem to have gained some semblance of control over the novel coronavirus, Florida appears to be in a downward spiral of high infection rates and increasing hospitalizations.
It didn’t have to go this way.
According to Robert Redfield, MD, Director of the Centers for Disease Control and Prevention, wearing a mask significantly reduces SARS-CoV-2 transmission. If community masking were increased only modestly, disease transmission could be curtailed enough to prevent many stay-at-home orders and reduce losses of an estimated $1 trillion in gross domestic product4 while also providing incalculable improvements in morbidity and mortality. Some experts believe that, while wearing a mask can protect others, it can also protect the wearer.5
That masking should be universal has become the accepted public health sentiment during this pandemic. Yet at the time of writing this article, there was still no law mandating masks in Florida, perhaps due to a significant but vocal minority—those who have personal concerns about wearing a mask and little concern about transmitting the virus to other, more vulnerable populations. This was the reason that one of the authors (M.B.) campaigned tirelessly for mandatory masking at Palm Beach County Commission meetings, one of which made the international news because of the outrageous and seemingly heart-felt statements made by several antimask advocates.6
AN ORGANIZED AND OUTSPOKEN MINORITY
At the Palm Beach County Commission, organized antimask advocates arrived hours before the start of the meeting, coming in two buses. Because of social distancing guidelines and seating limitations, they were able to fill many of the open seats at the meeting, making it appear that the antimask advocates far outnumbered those in favor of mask laws. Despite their tactics of screaming and intimidation, a law mandating masks in the county passed unanimously, though medical exemptions for those with chronic obstructive pulmonary disease, asthma, or “other conditions that reduce breathing” and religious exemptions for “persons for whom wearing a facial covering conflicts with their religious beliefs or practices” were included.7 After the meeting, police escorts were required by those in favor of masks, while the county commissioners had to lock themselves behind chamber doors.
The antimask campaigners were already known to M.B., a teacher, from previous gatherings she had attended in support of firearm legislation aimed at reducing gun violence. The same antimask advocates at the County Commission meeting had previously gathered as counter-protesters at this prior event, heckling and threatening those advocating for improving gun safety through legislation such as background checks. While it should not be, mask wearing and the laws mandating it have become a question of politics rather than one based in scientific evidence.
POLITICIZATION OF PUBLIC HEALTH IN FLORIDA AND ITS CONSEQUENCES
The absence of mandatory masking laws in populations hesitant to wear them, combined with the rush to reopen businesses, resulted in increasing death rates in Florida, with 7-day averages continuing in an upward trajectory and over 7,000 deaths being reported as of August 3, 2020.8 A small glimmer of hope was raised on that day, when fewer than 100 deaths for the previous day were reported, although one wonders if the weekend’s Hurricane Isaias preparations may have delayed some reporting.
In the face of mounting death counts and increasingly stressed hospitals, Florida’s governor, Ron DeSantis, has not heeded calls to institute new regulations, instead deferring to localities. This is perhaps good news considering Georgia’s governor, Brian Kemp, has spoken out against local mask laws and has said that mandating wearing them, even at the local level, would be a “bridge too far.”9 Several Georgia municipalities defied the governor, passing mandatory masking for their populations anyway, prompting Governor Kemp to file a lawsuit against the city of Atlanta, which he subsequently dropped after a judge ordered the state and city into mediation.10
The idea that the state should create laws to regulate the health and safety of the population has been met with resistance in the past where there is a greater degree of libertarian and antipaternalistic thinking.11 Campaigning against public health laws is not a new phenomenon. In the 1970s and 1980s, mandatory seat belt laws were met with significant resistance by a vocal minority, with the most common predictors for opposing these laws noted as holding beliefs that seat belts were ineffective, inconvenient, or uncomfortable12—the same arguments that have been made against masks. Additionally, having lower educational attainment, less income, and younger age were predictors of being against mandatory seat belt laws.12
THE IMPORTANCE OF COMMUNITY ENGAGEMENT
In response to a vociferous and somewhat organized minority, which has, in many cases, intimidated state and local politicians into inaction, community organizers have put out the call for many more citizens to make their voices heard. This seemed to have had an impact on the Palm Beach County commissioners, one of whom tried to demonstrate that there was broad support for passing a mandatory masking law during the commission meeting by bringing a stack of printed-out communications he had received in favor of it. Community organizers and public health advocates generally have an easier time reaching local officials, whereas it can be more difficult to engage other government officials farther away in state capitals, especially in larger states such as Florida. The organizers can also appeal to the fact that the local officials must live in the communities they represent and do not want to suffer from the spread of SARS-CoV-2 and overflowing hospitals. While local officials may be ill equipped to handle a global pandemic, appealing to the community has been somewhat effective in putting pressure on these officials to get a patchwork of local laws, which hopefully will have an impact on Florida’s surge numbers.
In the absence of a statewide mandatory masking law in Florida, several municipalities have instituted their own restrictions. Counties with some of the largest cities, such as Miami, Fort Lauderdale, Tampa, and Orlando, have required that masks be worn in public since June or early July.13 These restrictions, however, were implemented later than states in the northeastern United States, which have required masks since April or May and before significant reopening of businesses took place, in contrast to the sequence observed in Florida.
In the absence of political leadership, Florida businesses are increasingly taking up the charge and mandating that employees work from home, while others are requiring that employees and customers wear masks. Following New York–based grocer Key Foods and national chains like Whole Foods, both of which have long required that Florida customers wear masks, Florida’s ubiquitous Publix Supermarkets mandated masks in over 800 of their stores beginning July 21.14
While individual businesses and localities should be commended for their efforts, unfortunately, this may not be enough to dampen the surge. A tool developed by Harvard-based researchers, has labeled Florida and several other neighboring states as having severe spread, necessitating the need for stay-at-home orders to be reinstated.15
CONCLUSION
Florida is currently a global epicenter for COVID-19 diagnoses, with the state reporting nearly 600,000 cases as of August 17,8 more than most countries with larger populations. Florida faces many barriers to gaining control over the virus, including a vocal and organized minority which has opposed public health measures, an unwilling state government and ill-equipped local officials, and an underfunded safety net if stay-at-home orders were to be issued. Appealing to the public and elected officials with science, sanity, and support for those who want to prevent the spread of COVID-19 may provide one solution for gaining some control over the pandemic.
Disclosures
The authors have nothing to disclose.
1. Hospital ICU Beds Census and Staffed Availability as Reported in ESS. My Florida. Accessed July 30, 2020. https://bi.ahca.myflorida.com/t/ABICC/views/Public/ICUBedsHospital
2. Goodman CK. Broward hospitals nearing capacity with overflow patients from Miami-Dade. South Florida Sun Sentinel. July 28, 2020. Accessed August 3, 2020. https://www.sun-sentinel.com/coronavirus/fl-ne-broward-hospitals-getting-overflow-20200728-akz7k5wmubb2billpnofsqtqdy-story.html
3. Miami-Dade County, FL. Covid Act Now. Accessed August 3, 2020. https://covidactnow.org/us/fl/county/miami_dade_county?s=790144
4. Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission—the time is now. JAMA. Published online July 14, 2020. https://doi.org/10.1001/jama.2020.13107
5. Gandhi M, Beyrer C, Goosby E. Masks do more than protect others during COVID-19: reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;1-4. https://doi.org/10.1007/s11606-020-06067-8
6. ‘They want to throw God’s wonderful breathing system out.’ BBC News. June 25, 2020. Accessed August 3, 2020. https://www.bbc.com/news/av/world-us-canada-53174415/they-want-to-throw-god-s-wonderful-breathing-system-out
7. Palm Beach County Facial Coverings Frequently Asked Questions. Palm Beach County: Discover the Palm Beaches…the Best of Everything. Updated June 26, 2020. Accessed July 30, 2020. https://discover.pbcgov.org/PDF/COVID19/PBC-Facial-Coverings-FAQs.pdf
8. Florida COVID-19 Response. Accessed August 17, 2020. https://floridahealthcovid19.gov/
9. Flynn M, Iati M. Georgia Gov. Brian Kemp sues Atlanta over mask requirement as coronavirus surges in the state. Washington Post. July 16, 2020. Accessed August 3, 2020. https://www.washingtonpost.com/nation/2020/07/16/kemp-georgia-mask-mandates/
10. Jamerson J. Georgia Gov. Kemp drops lawsuit against Atlanta mayor over coronavirus restrictions. Wall Street Journal. August 13, 2020. Accessed August 17, 2020. https://www.wsj.com/articles/georgia-gov-kemp-drops-lawsuit-against-atlanta-mayor-over-coronavirus-restrictions-11597347685
11. Giubilini A, Savulescu J. Vaccination, risks, and freedom: the seat belt analogy. Public Health Ethics. 2019;12(3):237-249. https://doi.org/10.1093/phe/phz014
12. Morelock S, Hingson RW, Smith RA, Lederman RI. Mandatory seatbelt law support and opposition in New England—a survey. Public Health Rep. 1985;100(4):357-363.
13. Muller B. Most major Florida cities now require wearing face masks in public. News4Jax. June 19, 2020. Updated June 19, 2020. Accessed August 3, 2020. https://www.news4jax.com/news/local/2020/06/19/major-florida-cities-now-require-use-of-face-mask-in-public-places/
14. Ward B. Publix to mandate face masks for all stores starting next week. Tampa Bay Business Journal. July 16, 2020. Updated July 16, 2020. Accessed August 3, 2020. https://www.bizjournals.com/tampabay/news/2020/07/16/publix-to-mandate-face-masks-for-all-stores-starti.html
15. COVID Risk Levels Dashboard. Pandemics explained: unlocking evidence for better decision making. Accessed August 3, 2020. https://globalepidemics.org/key-metrics-for-covid-suppression/
At the time this piece was written, 54 Florida hospitals reported no available intensive care unit (ICU) beds1; hospitals in Miami-Dade County even started sending patients to neighboring Broward County for care despite Broward County also reporting a hospital bed shortage. Patients might even have needed to be transferred further north to Palm Beach County.2 Miami-Dade County was diagnosing over 100 cases with SARS-CoV-2 per 100,000 residents per day at one point, with a test positivity rate of over 25% that suggests testing is inadequate and many more would-be positive tests are being missed.3 While certain parts of the United States seem to have gained some semblance of control over the novel coronavirus, Florida appears to be in a downward spiral of high infection rates and increasing hospitalizations.
It didn’t have to go this way.
According to Robert Redfield, MD, Director of the Centers for Disease Control and Prevention, wearing a mask significantly reduces SARS-CoV-2 transmission. If community masking were increased only modestly, disease transmission could be curtailed enough to prevent many stay-at-home orders and reduce losses of an estimated $1 trillion in gross domestic product4 while also providing incalculable improvements in morbidity and mortality. Some experts believe that, while wearing a mask can protect others, it can also protect the wearer.5
That masking should be universal has become the accepted public health sentiment during this pandemic. Yet at the time of writing this article, there was still no law mandating masks in Florida, perhaps due to a significant but vocal minority—those who have personal concerns about wearing a mask and little concern about transmitting the virus to other, more vulnerable populations. This was the reason that one of the authors (M.B.) campaigned tirelessly for mandatory masking at Palm Beach County Commission meetings, one of which made the international news because of the outrageous and seemingly heart-felt statements made by several antimask advocates.6
AN ORGANIZED AND OUTSPOKEN MINORITY
At the Palm Beach County Commission, organized antimask advocates arrived hours before the start of the meeting, coming in two buses. Because of social distancing guidelines and seating limitations, they were able to fill many of the open seats at the meeting, making it appear that the antimask advocates far outnumbered those in favor of mask laws. Despite their tactics of screaming and intimidation, a law mandating masks in the county passed unanimously, though medical exemptions for those with chronic obstructive pulmonary disease, asthma, or “other conditions that reduce breathing” and religious exemptions for “persons for whom wearing a facial covering conflicts with their religious beliefs or practices” were included.7 After the meeting, police escorts were required by those in favor of masks, while the county commissioners had to lock themselves behind chamber doors.
The antimask campaigners were already known to M.B., a teacher, from previous gatherings she had attended in support of firearm legislation aimed at reducing gun violence. The same antimask advocates at the County Commission meeting had previously gathered as counter-protesters at this prior event, heckling and threatening those advocating for improving gun safety through legislation such as background checks. While it should not be, mask wearing and the laws mandating it have become a question of politics rather than one based in scientific evidence.
POLITICIZATION OF PUBLIC HEALTH IN FLORIDA AND ITS CONSEQUENCES
The absence of mandatory masking laws in populations hesitant to wear them, combined with the rush to reopen businesses, resulted in increasing death rates in Florida, with 7-day averages continuing in an upward trajectory and over 7,000 deaths being reported as of August 3, 2020.8 A small glimmer of hope was raised on that day, when fewer than 100 deaths for the previous day were reported, although one wonders if the weekend’s Hurricane Isaias preparations may have delayed some reporting.
In the face of mounting death counts and increasingly stressed hospitals, Florida’s governor, Ron DeSantis, has not heeded calls to institute new regulations, instead deferring to localities. This is perhaps good news considering Georgia’s governor, Brian Kemp, has spoken out against local mask laws and has said that mandating wearing them, even at the local level, would be a “bridge too far.”9 Several Georgia municipalities defied the governor, passing mandatory masking for their populations anyway, prompting Governor Kemp to file a lawsuit against the city of Atlanta, which he subsequently dropped after a judge ordered the state and city into mediation.10
The idea that the state should create laws to regulate the health and safety of the population has been met with resistance in the past where there is a greater degree of libertarian and antipaternalistic thinking.11 Campaigning against public health laws is not a new phenomenon. In the 1970s and 1980s, mandatory seat belt laws were met with significant resistance by a vocal minority, with the most common predictors for opposing these laws noted as holding beliefs that seat belts were ineffective, inconvenient, or uncomfortable12—the same arguments that have been made against masks. Additionally, having lower educational attainment, less income, and younger age were predictors of being against mandatory seat belt laws.12
THE IMPORTANCE OF COMMUNITY ENGAGEMENT
In response to a vociferous and somewhat organized minority, which has, in many cases, intimidated state and local politicians into inaction, community organizers have put out the call for many more citizens to make their voices heard. This seemed to have had an impact on the Palm Beach County commissioners, one of whom tried to demonstrate that there was broad support for passing a mandatory masking law during the commission meeting by bringing a stack of printed-out communications he had received in favor of it. Community organizers and public health advocates generally have an easier time reaching local officials, whereas it can be more difficult to engage other government officials farther away in state capitals, especially in larger states such as Florida. The organizers can also appeal to the fact that the local officials must live in the communities they represent and do not want to suffer from the spread of SARS-CoV-2 and overflowing hospitals. While local officials may be ill equipped to handle a global pandemic, appealing to the community has been somewhat effective in putting pressure on these officials to get a patchwork of local laws, which hopefully will have an impact on Florida’s surge numbers.
In the absence of a statewide mandatory masking law in Florida, several municipalities have instituted their own restrictions. Counties with some of the largest cities, such as Miami, Fort Lauderdale, Tampa, and Orlando, have required that masks be worn in public since June or early July.13 These restrictions, however, were implemented later than states in the northeastern United States, which have required masks since April or May and before significant reopening of businesses took place, in contrast to the sequence observed in Florida.
In the absence of political leadership, Florida businesses are increasingly taking up the charge and mandating that employees work from home, while others are requiring that employees and customers wear masks. Following New York–based grocer Key Foods and national chains like Whole Foods, both of which have long required that Florida customers wear masks, Florida’s ubiquitous Publix Supermarkets mandated masks in over 800 of their stores beginning July 21.14
While individual businesses and localities should be commended for their efforts, unfortunately, this may not be enough to dampen the surge. A tool developed by Harvard-based researchers, has labeled Florida and several other neighboring states as having severe spread, necessitating the need for stay-at-home orders to be reinstated.15
CONCLUSION
Florida is currently a global epicenter for COVID-19 diagnoses, with the state reporting nearly 600,000 cases as of August 17,8 more than most countries with larger populations. Florida faces many barriers to gaining control over the virus, including a vocal and organized minority which has opposed public health measures, an unwilling state government and ill-equipped local officials, and an underfunded safety net if stay-at-home orders were to be issued. Appealing to the public and elected officials with science, sanity, and support for those who want to prevent the spread of COVID-19 may provide one solution for gaining some control over the pandemic.
Disclosures
The authors have nothing to disclose.
At the time this piece was written, 54 Florida hospitals reported no available intensive care unit (ICU) beds1; hospitals in Miami-Dade County even started sending patients to neighboring Broward County for care despite Broward County also reporting a hospital bed shortage. Patients might even have needed to be transferred further north to Palm Beach County.2 Miami-Dade County was diagnosing over 100 cases with SARS-CoV-2 per 100,000 residents per day at one point, with a test positivity rate of over 25% that suggests testing is inadequate and many more would-be positive tests are being missed.3 While certain parts of the United States seem to have gained some semblance of control over the novel coronavirus, Florida appears to be in a downward spiral of high infection rates and increasing hospitalizations.
It didn’t have to go this way.
According to Robert Redfield, MD, Director of the Centers for Disease Control and Prevention, wearing a mask significantly reduces SARS-CoV-2 transmission. If community masking were increased only modestly, disease transmission could be curtailed enough to prevent many stay-at-home orders and reduce losses of an estimated $1 trillion in gross domestic product4 while also providing incalculable improvements in morbidity and mortality. Some experts believe that, while wearing a mask can protect others, it can also protect the wearer.5
That masking should be universal has become the accepted public health sentiment during this pandemic. Yet at the time of writing this article, there was still no law mandating masks in Florida, perhaps due to a significant but vocal minority—those who have personal concerns about wearing a mask and little concern about transmitting the virus to other, more vulnerable populations. This was the reason that one of the authors (M.B.) campaigned tirelessly for mandatory masking at Palm Beach County Commission meetings, one of which made the international news because of the outrageous and seemingly heart-felt statements made by several antimask advocates.6
AN ORGANIZED AND OUTSPOKEN MINORITY
At the Palm Beach County Commission, organized antimask advocates arrived hours before the start of the meeting, coming in two buses. Because of social distancing guidelines and seating limitations, they were able to fill many of the open seats at the meeting, making it appear that the antimask advocates far outnumbered those in favor of mask laws. Despite their tactics of screaming and intimidation, a law mandating masks in the county passed unanimously, though medical exemptions for those with chronic obstructive pulmonary disease, asthma, or “other conditions that reduce breathing” and religious exemptions for “persons for whom wearing a facial covering conflicts with their religious beliefs or practices” were included.7 After the meeting, police escorts were required by those in favor of masks, while the county commissioners had to lock themselves behind chamber doors.
The antimask campaigners were already known to M.B., a teacher, from previous gatherings she had attended in support of firearm legislation aimed at reducing gun violence. The same antimask advocates at the County Commission meeting had previously gathered as counter-protesters at this prior event, heckling and threatening those advocating for improving gun safety through legislation such as background checks. While it should not be, mask wearing and the laws mandating it have become a question of politics rather than one based in scientific evidence.
POLITICIZATION OF PUBLIC HEALTH IN FLORIDA AND ITS CONSEQUENCES
The absence of mandatory masking laws in populations hesitant to wear them, combined with the rush to reopen businesses, resulted in increasing death rates in Florida, with 7-day averages continuing in an upward trajectory and over 7,000 deaths being reported as of August 3, 2020.8 A small glimmer of hope was raised on that day, when fewer than 100 deaths for the previous day were reported, although one wonders if the weekend’s Hurricane Isaias preparations may have delayed some reporting.
In the face of mounting death counts and increasingly stressed hospitals, Florida’s governor, Ron DeSantis, has not heeded calls to institute new regulations, instead deferring to localities. This is perhaps good news considering Georgia’s governor, Brian Kemp, has spoken out against local mask laws and has said that mandating wearing them, even at the local level, would be a “bridge too far.”9 Several Georgia municipalities defied the governor, passing mandatory masking for their populations anyway, prompting Governor Kemp to file a lawsuit against the city of Atlanta, which he subsequently dropped after a judge ordered the state and city into mediation.10
The idea that the state should create laws to regulate the health and safety of the population has been met with resistance in the past where there is a greater degree of libertarian and antipaternalistic thinking.11 Campaigning against public health laws is not a new phenomenon. In the 1970s and 1980s, mandatory seat belt laws were met with significant resistance by a vocal minority, with the most common predictors for opposing these laws noted as holding beliefs that seat belts were ineffective, inconvenient, or uncomfortable12—the same arguments that have been made against masks. Additionally, having lower educational attainment, less income, and younger age were predictors of being against mandatory seat belt laws.12
THE IMPORTANCE OF COMMUNITY ENGAGEMENT
In response to a vociferous and somewhat organized minority, which has, in many cases, intimidated state and local politicians into inaction, community organizers have put out the call for many more citizens to make their voices heard. This seemed to have had an impact on the Palm Beach County commissioners, one of whom tried to demonstrate that there was broad support for passing a mandatory masking law during the commission meeting by bringing a stack of printed-out communications he had received in favor of it. Community organizers and public health advocates generally have an easier time reaching local officials, whereas it can be more difficult to engage other government officials farther away in state capitals, especially in larger states such as Florida. The organizers can also appeal to the fact that the local officials must live in the communities they represent and do not want to suffer from the spread of SARS-CoV-2 and overflowing hospitals. While local officials may be ill equipped to handle a global pandemic, appealing to the community has been somewhat effective in putting pressure on these officials to get a patchwork of local laws, which hopefully will have an impact on Florida’s surge numbers.
In the absence of a statewide mandatory masking law in Florida, several municipalities have instituted their own restrictions. Counties with some of the largest cities, such as Miami, Fort Lauderdale, Tampa, and Orlando, have required that masks be worn in public since June or early July.13 These restrictions, however, were implemented later than states in the northeastern United States, which have required masks since April or May and before significant reopening of businesses took place, in contrast to the sequence observed in Florida.
In the absence of political leadership, Florida businesses are increasingly taking up the charge and mandating that employees work from home, while others are requiring that employees and customers wear masks. Following New York–based grocer Key Foods and national chains like Whole Foods, both of which have long required that Florida customers wear masks, Florida’s ubiquitous Publix Supermarkets mandated masks in over 800 of their stores beginning July 21.14
While individual businesses and localities should be commended for their efforts, unfortunately, this may not be enough to dampen the surge. A tool developed by Harvard-based researchers, has labeled Florida and several other neighboring states as having severe spread, necessitating the need for stay-at-home orders to be reinstated.15
CONCLUSION
Florida is currently a global epicenter for COVID-19 diagnoses, with the state reporting nearly 600,000 cases as of August 17,8 more than most countries with larger populations. Florida faces many barriers to gaining control over the virus, including a vocal and organized minority which has opposed public health measures, an unwilling state government and ill-equipped local officials, and an underfunded safety net if stay-at-home orders were to be issued. Appealing to the public and elected officials with science, sanity, and support for those who want to prevent the spread of COVID-19 may provide one solution for gaining some control over the pandemic.
Disclosures
The authors have nothing to disclose.
1. Hospital ICU Beds Census and Staffed Availability as Reported in ESS. My Florida. Accessed July 30, 2020. https://bi.ahca.myflorida.com/t/ABICC/views/Public/ICUBedsHospital
2. Goodman CK. Broward hospitals nearing capacity with overflow patients from Miami-Dade. South Florida Sun Sentinel. July 28, 2020. Accessed August 3, 2020. https://www.sun-sentinel.com/coronavirus/fl-ne-broward-hospitals-getting-overflow-20200728-akz7k5wmubb2billpnofsqtqdy-story.html
3. Miami-Dade County, FL. Covid Act Now. Accessed August 3, 2020. https://covidactnow.org/us/fl/county/miami_dade_county?s=790144
4. Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission—the time is now. JAMA. Published online July 14, 2020. https://doi.org/10.1001/jama.2020.13107
5. Gandhi M, Beyrer C, Goosby E. Masks do more than protect others during COVID-19: reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;1-4. https://doi.org/10.1007/s11606-020-06067-8
6. ‘They want to throw God’s wonderful breathing system out.’ BBC News. June 25, 2020. Accessed August 3, 2020. https://www.bbc.com/news/av/world-us-canada-53174415/they-want-to-throw-god-s-wonderful-breathing-system-out
7. Palm Beach County Facial Coverings Frequently Asked Questions. Palm Beach County: Discover the Palm Beaches…the Best of Everything. Updated June 26, 2020. Accessed July 30, 2020. https://discover.pbcgov.org/PDF/COVID19/PBC-Facial-Coverings-FAQs.pdf
8. Florida COVID-19 Response. Accessed August 17, 2020. https://floridahealthcovid19.gov/
9. Flynn M, Iati M. Georgia Gov. Brian Kemp sues Atlanta over mask requirement as coronavirus surges in the state. Washington Post. July 16, 2020. Accessed August 3, 2020. https://www.washingtonpost.com/nation/2020/07/16/kemp-georgia-mask-mandates/
10. Jamerson J. Georgia Gov. Kemp drops lawsuit against Atlanta mayor over coronavirus restrictions. Wall Street Journal. August 13, 2020. Accessed August 17, 2020. https://www.wsj.com/articles/georgia-gov-kemp-drops-lawsuit-against-atlanta-mayor-over-coronavirus-restrictions-11597347685
11. Giubilini A, Savulescu J. Vaccination, risks, and freedom: the seat belt analogy. Public Health Ethics. 2019;12(3):237-249. https://doi.org/10.1093/phe/phz014
12. Morelock S, Hingson RW, Smith RA, Lederman RI. Mandatory seatbelt law support and opposition in New England—a survey. Public Health Rep. 1985;100(4):357-363.
13. Muller B. Most major Florida cities now require wearing face masks in public. News4Jax. June 19, 2020. Updated June 19, 2020. Accessed August 3, 2020. https://www.news4jax.com/news/local/2020/06/19/major-florida-cities-now-require-use-of-face-mask-in-public-places/
14. Ward B. Publix to mandate face masks for all stores starting next week. Tampa Bay Business Journal. July 16, 2020. Updated July 16, 2020. Accessed August 3, 2020. https://www.bizjournals.com/tampabay/news/2020/07/16/publix-to-mandate-face-masks-for-all-stores-starti.html
15. COVID Risk Levels Dashboard. Pandemics explained: unlocking evidence for better decision making. Accessed August 3, 2020. https://globalepidemics.org/key-metrics-for-covid-suppression/
1. Hospital ICU Beds Census and Staffed Availability as Reported in ESS. My Florida. Accessed July 30, 2020. https://bi.ahca.myflorida.com/t/ABICC/views/Public/ICUBedsHospital
2. Goodman CK. Broward hospitals nearing capacity with overflow patients from Miami-Dade. South Florida Sun Sentinel. July 28, 2020. Accessed August 3, 2020. https://www.sun-sentinel.com/coronavirus/fl-ne-broward-hospitals-getting-overflow-20200728-akz7k5wmubb2billpnofsqtqdy-story.html
3. Miami-Dade County, FL. Covid Act Now. Accessed August 3, 2020. https://covidactnow.org/us/fl/county/miami_dade_county?s=790144
4. Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission—the time is now. JAMA. Published online July 14, 2020. https://doi.org/10.1001/jama.2020.13107
5. Gandhi M, Beyrer C, Goosby E. Masks do more than protect others during COVID-19: reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;1-4. https://doi.org/10.1007/s11606-020-06067-8
6. ‘They want to throw God’s wonderful breathing system out.’ BBC News. June 25, 2020. Accessed August 3, 2020. https://www.bbc.com/news/av/world-us-canada-53174415/they-want-to-throw-god-s-wonderful-breathing-system-out
7. Palm Beach County Facial Coverings Frequently Asked Questions. Palm Beach County: Discover the Palm Beaches…the Best of Everything. Updated June 26, 2020. Accessed July 30, 2020. https://discover.pbcgov.org/PDF/COVID19/PBC-Facial-Coverings-FAQs.pdf
8. Florida COVID-19 Response. Accessed August 17, 2020. https://floridahealthcovid19.gov/
9. Flynn M, Iati M. Georgia Gov. Brian Kemp sues Atlanta over mask requirement as coronavirus surges in the state. Washington Post. July 16, 2020. Accessed August 3, 2020. https://www.washingtonpost.com/nation/2020/07/16/kemp-georgia-mask-mandates/
10. Jamerson J. Georgia Gov. Kemp drops lawsuit against Atlanta mayor over coronavirus restrictions. Wall Street Journal. August 13, 2020. Accessed August 17, 2020. https://www.wsj.com/articles/georgia-gov-kemp-drops-lawsuit-against-atlanta-mayor-over-coronavirus-restrictions-11597347685
11. Giubilini A, Savulescu J. Vaccination, risks, and freedom: the seat belt analogy. Public Health Ethics. 2019;12(3):237-249. https://doi.org/10.1093/phe/phz014
12. Morelock S, Hingson RW, Smith RA, Lederman RI. Mandatory seatbelt law support and opposition in New England—a survey. Public Health Rep. 1985;100(4):357-363.
13. Muller B. Most major Florida cities now require wearing face masks in public. News4Jax. June 19, 2020. Updated June 19, 2020. Accessed August 3, 2020. https://www.news4jax.com/news/local/2020/06/19/major-florida-cities-now-require-use-of-face-mask-in-public-places/
14. Ward B. Publix to mandate face masks for all stores starting next week. Tampa Bay Business Journal. July 16, 2020. Updated July 16, 2020. Accessed August 3, 2020. https://www.bizjournals.com/tampabay/news/2020/07/16/publix-to-mandate-face-masks-for-all-stores-starti.html
15. COVID Risk Levels Dashboard. Pandemics explained: unlocking evidence for better decision making. Accessed August 3, 2020. https://globalepidemics.org/key-metrics-for-covid-suppression/
© 2020 Society of Hospital Medicine
Grieving and Hospital-Based Bereavement Care During the COVID-19 Pandemic
As of July 25, 2020, there had been 146,073 deaths from COVID-19 in the United States and 641,273 worldwide, with a disproportionate number of deaths occurring in historically disadvantaged minority groups, specifically African Americans.1,2 The number of decedents will continue to increase over the coming months, even as the number of new COVID-19 cases decreases. Given that, for each death, five persons are believed to be significantly affected,3 the number of bereaved individuals whose loved ones died during the pandemic in the United States alone is likely to be in the millions.
COVID-19–related mortality has become a pressing public health issue, and as a result, support for bereaved family members, especially for minority populations, is also an important public health issue.4 It is likely that bereaved individuals are at greater risk of poor bereavement outcomes during the pandemic—irrespective of whether the death was a result of COVID-19—because of social isolation. This is particularly true if loved ones died in the hospital and, due to visitor restrictions, faced limited or no visitation. For many, bereavement will be affected by stay-at-home orders and social distancing restrictions that reduce access to emotional support and rituals, such as funerals, that usually provide comfort.5
Urgent attention is needed to support bereaved individuals, to flatten the curve of mental health disorders associated with the death of loved ones during the pandemic. Within a preventive model of care, we offer guidelines for how hospitals, longitudinal providers, and mental health clinicians can provide bereavement outreach to all individuals whose loved ones died during the COVID-19 pandemic.
PUBLIC HEALTH MODEL OF BEREAVEMENT SUPPORT
The provision of bereavement care, including the assessment of risk for poor bereavement outcomes, is an essential component of high-quality end-of-life care endorsed by the hospice and palliative care movement.6 However, the development of standardized bereavement services has lagged behind that of other components of palliative care, varying greatly by institution and provider.7 Approximately 10% to 20% of bereaved individuals experience psychiatric difficulties following the death of a loved one, including prolonged grief disorder, posttraumatic stress disorder, and major depressive disorder.8 Risk factors include a hospital-based death, death in an intensive care unit (ICU), sudden death, not being able to say goodbye, and a history of psychiatric disorders.8,9
One of the biggest barriers in providing standardized bereavement services is the lack of a systematic process to identify individuals at risk of poor bereavement outcomes.10 Aoun et al developed a public health model of bereavement support that comprises a three-tiered approach to risk and the corresponding need for support.11 They propose that the low-risk group, approximately 60% of bereaved individuals, would primarily need support from family and friends, the moderate-risk group (30%) would need support from the wider community, and the high-risk group (10%) would need support from mental health providers.
It is reasonable to assume that many individuals whose loved ones died during the pandemic will fall into a high-risk group for poor bereavement outcomes, as identified by Aoun et al.11 Given a higher than usual inpatient mortality due to COVID-19 for certain populations and that bereavement care is already underrecognized within healthcare systems, hospitals and other healthcare facilities and their providers need to fill this void.
EDUCATION, GUIDANCE, AND SUPPORT MODEL
We adopted an education, guidance, and support model of bereavement support in 2019.7 This model has been shown to positively affect the experience of bereaved individuals, especially because of condolences from providers and psycho-educational information about coping with grief.7 Each month, a list of deceased patients and family contacts is generated from a mortality review database,12 and bereavement packets are mailed to family members; the packet includes a condolence letter from senior management, a psycho-educational grief guide, and a list of community-based resources. A social worker is also available to provide telephone support and to assist with mental health referrals. For patients who died in the COVID-19–specific units, social work also provides support and outreach to families.
Psycho-Education
During the early weeks of the pandemic, a tip sheet—”Grieving during a pandemic”13— was created to include in the bereavement packet and for distribution to community organizations within the hospital’s geographical area. This tip sheet offers strategies to facilitate coping based on the psychological model of cognitive-behavioral therapy (CBT).14 Topics addressed include understanding the nature of grief, self-care, adapting bereavement rituals in light of social distancing, challenging unhelpful thinking patterns that might lead to feelings of guilt especially regarding the death of the patient, and ways to obtain support during the pandemic. The tip sheet was made available in Spanish, French, Chinese, Haitian Creole, Portuguese, Arabic, and Russian given that our mortality data, consistent with preliminary findings from New York State, suggested higher death rates among Black/African American and Hispanic/Latino groups, compared with historical mortality statistics.15
Virtual Support
As part of our bereavement response during the COVID-19 crisis, we have launched virtual bereavement support for families impacted by the pandemic. It is challenging to identify the optimal type of support and timing, given the reliance on virtual outreach without in-person screening. With the increased distress and trauma associated with deaths during the pandemic, one clinical challenge is managing emotions in a virtual group without access to the usual tools that clinicians rely on, such as reading body language. Following a graded exposure approach, a form of behavioral therapy,14 we recommend offering a psycho-educational seminar first in which facilitators can control the content and limit exposure of sharing stories from participants. For support groups (eg, 6 to 8 sessions), we recommend that participants be screened prior to assess their risk factors and readiness and provide individual therapist referrals as needed.10
Community Outreach
Many diverse communities have been affected significantly by COVID-19 and faced high mortality rates.16 We recognized that proactive bereavement outreach to these communities was essential. Grief guides and tip sheets in various languages were made available as part of our community outreach programs, which included vans traveling to severely affected communities and providing testing, masks, alcohol-based hand sanitizer, and written materials.
Education About Bereavement
Many clinicians and staff express feelings of inadequacy about providing bereavement outreach. Such feelings are not uncommon, especially because clinicians tend to receive little training in dealing with the emotional toll of patient deaths and bereavement care.17,18 These feelings are likely to be heightened during this pandemic given the increased exposure to patient deaths, concern for personal safety, and changed practices in providing care, including the need to socially distance. Providing support for clinicians to process their feelings about the death of patients is crucial.19 In addition to our Employee Assistance Program, psychosocial clinicians are facilitating weekly virtual support groups for providers to discuss the effects of the pandemic on their personal and professional lives.
Bereaved family members report they benefit from hearing from the clinical team and receiving condolences, which is seen as humanizing the physician-family relationship. This personal outreach is likely more important during this time because many providers will have interacted with family members virtually.7,20,21 To help facilitate offers of condolences, we developed the TEARS acronym to describe the components of a condolence call that can also be adapted for writing condolence cards (Table).
GUIDELINES
We recommend that hospitals and other healthcare facilities that might not have well-established bereavement programs consider adopting a building block approach to provide basic outreach to families of their deceased patients.7 Tapping into existing resources, the major components are as follows: (1) a letter of condolence from leadership, (2) psycho-educational information about grief, (3) a list of community/online resources, including information about local hospice bereavement programs and bereavement camps or programs for children, (4) offers of condolences from individual providers/teams, and (5) mental health outreach as indicated.
CONCLUSION
The COVID-19–related mortality, particularly among already vulnerable populations, coupled with the existing underrecognition of bereavement has created an urgent public health issue that needs to be addressed. Given that few institutions offer standardized bereavement follow-up, we believe that hospital providers and mental health clinicians need to take a proactive approach to providing bereavement outreach to families affected by death during the pandemic.
Acknowledgments
The authors would like to acknowledge the Brigham Health Bereavement Committee and the staff of Care Continuum Management and the Department of Community Outreach at Brigham and Women’s Hospital.
Disclosures
No competing financial interests relevant to this article exist for Dr Morris, Ms Paterson, and Dr Mendu. Dr Morris receives royalties for two self-help books about grief published by Robinson and Dr Mendu provides consulting services for Bayer AG unrelated to the content of this article.
1. Coronavirus Resource Center Covid-19: Case Tracker. Johns Hopkins University. Accessed July 25, 2020. https://coronavirus.jhu.edu/
2. Tappe A. America’s black and Hispanic communities are bearing the brunt of the coronavirus. CNN. April 21, 2020. Accessed June 7, 2020. https://www.cnn.com/2020/04/21/economy/coronavirus-burden-black-hispanic-workers/index.html
3. Shear K, Frank E, Houck PR, Reynolds CF 3rd. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608. https://doi.org/10.1001/jama.293.21.2601
4. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med. 2020;382(26):2534-2543. https://doi.org/10.1056/nejmsa2011686
5. Morris SE, Moment A, Thomas JD. Caring for bereaved family members during the COVID-19 pandemic: before and after the death of a patient. J Pain Symptom Manage. Published online May 7, 2020. https://doi.org/10.1016/j.jpainsymman.2020.05.002
6. National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 4th ed. National Coalition for Hospice and Palliative Care; 2018. Accessed June 7, 2020. https://www.nationalcoalitionhpc.org/ncp
7. Morris SE, Block SD. Adding value to palliative care services: the development of an institutional bereavement program. J Palliat Med. 2015;18(11):915-922. https://doi.org/10.1089/jpm.2015.0080
8. Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960-1973. https://doi.org/10.1016/s0140-6736(07)61816-9
9. Kentish-Barnes N, Chaize M, Seegers V, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J. 2015;45(5):1341-1352. https://doi.org/10.1183/09031936.00160014
10. Morris SE, Anderson CM, Tarquini SJ, Block SD. A standardized approach to bereavement risk-screening: a quality improvement project. J Psychosoc Oncol. 2020;38(4):406-417. https://doi.org/10.1080/07347332.2019.1703065
11. Aoun SM, Breen LJ, Howting DA, Rumbold B, McNamara B, Hegney D. Who needs bereavement support? a population based survey of bereavement risk and support need. PLoS One. 2015;10(3):e0121101. https://doi.org/10.1371/journal.pone.0121101
12. Mendu ML, Lu Y, Petersen A, et al. Reflections on implementing a hospital-wide provider-based electronic inpatient mortality review system: lessons learnt. BMJ Qual Saf. 2020;29(4):304‐312. https://doi.org/10.1136/bmjqs-2019-009864
13. Morris SE. Grieving during a pandemic. Brigham and Women’s Hospital. Accessed July 25, 2020. https://www.brighamandwomens.org/covid-19/grieving-during-a-pandemic
14. Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed. Guilford Press; 2011.
15. Coronavirus Disease 2019 (COVID-19). Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Updated July 24, 2020. Accessed July 25, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
16. Death rates in Mass. surged in areas already hard hit. Boston Globe. May 17, 2020. Accessed June 8, 2020. https://www.bostonglobe.com/2020/05/17/opinion/death-rate-mass-surged-areas-already-hard-hit/
17. Jackson VA, Sullivan AM, Gadmer NM, et al. “It was haunting…”: physicians’ descriptions of emotionally powerful patient deaths. Acad Med. 2005;80(7):648-656. https://doi.org/10.1097/00001888-200507000-00007
18. Morris S, Schaefer K, Rosowsky E. Primary care for the elderly bereaved: recommendations for medical education. J Clin Psychol Med Settings. 2018;25(4):463‐470. https://doi.org/10.1007/s10880-018-9556-9
19. Morris SE, Kearns JP, Moment A, Lee KA, deLima Thomas J. “Remembrance”: a self-care tool for clinicians. J Palliat Med. 2019;22(3):316-318. https://doi.org/10.1089/jpm.2018.0395
20. Morris SE, Nayak MM, Block SD. Insights from bereaved family members about end-of-life care and bereavement. J Palliat Med. Published online February 10, 2020. https://doi.org/10.1089/jpm.2019.0467
21. Kentish-Barnes N, Cohen-Solal Z, Souppart V, et al. “It was the only thing I could hold onto, but…”: receiving a letter of condolence after loss of a loved one in the ICU: a qualitative study of bereaved relatives’ experience. Crit Care Med. 2017;45(12):1965-1971. https://doi.org/10.1097/ccm.0000000000002687
As of July 25, 2020, there had been 146,073 deaths from COVID-19 in the United States and 641,273 worldwide, with a disproportionate number of deaths occurring in historically disadvantaged minority groups, specifically African Americans.1,2 The number of decedents will continue to increase over the coming months, even as the number of new COVID-19 cases decreases. Given that, for each death, five persons are believed to be significantly affected,3 the number of bereaved individuals whose loved ones died during the pandemic in the United States alone is likely to be in the millions.
COVID-19–related mortality has become a pressing public health issue, and as a result, support for bereaved family members, especially for minority populations, is also an important public health issue.4 It is likely that bereaved individuals are at greater risk of poor bereavement outcomes during the pandemic—irrespective of whether the death was a result of COVID-19—because of social isolation. This is particularly true if loved ones died in the hospital and, due to visitor restrictions, faced limited or no visitation. For many, bereavement will be affected by stay-at-home orders and social distancing restrictions that reduce access to emotional support and rituals, such as funerals, that usually provide comfort.5
Urgent attention is needed to support bereaved individuals, to flatten the curve of mental health disorders associated with the death of loved ones during the pandemic. Within a preventive model of care, we offer guidelines for how hospitals, longitudinal providers, and mental health clinicians can provide bereavement outreach to all individuals whose loved ones died during the COVID-19 pandemic.
PUBLIC HEALTH MODEL OF BEREAVEMENT SUPPORT
The provision of bereavement care, including the assessment of risk for poor bereavement outcomes, is an essential component of high-quality end-of-life care endorsed by the hospice and palliative care movement.6 However, the development of standardized bereavement services has lagged behind that of other components of palliative care, varying greatly by institution and provider.7 Approximately 10% to 20% of bereaved individuals experience psychiatric difficulties following the death of a loved one, including prolonged grief disorder, posttraumatic stress disorder, and major depressive disorder.8 Risk factors include a hospital-based death, death in an intensive care unit (ICU), sudden death, not being able to say goodbye, and a history of psychiatric disorders.8,9
One of the biggest barriers in providing standardized bereavement services is the lack of a systematic process to identify individuals at risk of poor bereavement outcomes.10 Aoun et al developed a public health model of bereavement support that comprises a three-tiered approach to risk and the corresponding need for support.11 They propose that the low-risk group, approximately 60% of bereaved individuals, would primarily need support from family and friends, the moderate-risk group (30%) would need support from the wider community, and the high-risk group (10%) would need support from mental health providers.
It is reasonable to assume that many individuals whose loved ones died during the pandemic will fall into a high-risk group for poor bereavement outcomes, as identified by Aoun et al.11 Given a higher than usual inpatient mortality due to COVID-19 for certain populations and that bereavement care is already underrecognized within healthcare systems, hospitals and other healthcare facilities and their providers need to fill this void.
EDUCATION, GUIDANCE, AND SUPPORT MODEL
We adopted an education, guidance, and support model of bereavement support in 2019.7 This model has been shown to positively affect the experience of bereaved individuals, especially because of condolences from providers and psycho-educational information about coping with grief.7 Each month, a list of deceased patients and family contacts is generated from a mortality review database,12 and bereavement packets are mailed to family members; the packet includes a condolence letter from senior management, a psycho-educational grief guide, and a list of community-based resources. A social worker is also available to provide telephone support and to assist with mental health referrals. For patients who died in the COVID-19–specific units, social work also provides support and outreach to families.
Psycho-Education
During the early weeks of the pandemic, a tip sheet—”Grieving during a pandemic”13— was created to include in the bereavement packet and for distribution to community organizations within the hospital’s geographical area. This tip sheet offers strategies to facilitate coping based on the psychological model of cognitive-behavioral therapy (CBT).14 Topics addressed include understanding the nature of grief, self-care, adapting bereavement rituals in light of social distancing, challenging unhelpful thinking patterns that might lead to feelings of guilt especially regarding the death of the patient, and ways to obtain support during the pandemic. The tip sheet was made available in Spanish, French, Chinese, Haitian Creole, Portuguese, Arabic, and Russian given that our mortality data, consistent with preliminary findings from New York State, suggested higher death rates among Black/African American and Hispanic/Latino groups, compared with historical mortality statistics.15
Virtual Support
As part of our bereavement response during the COVID-19 crisis, we have launched virtual bereavement support for families impacted by the pandemic. It is challenging to identify the optimal type of support and timing, given the reliance on virtual outreach without in-person screening. With the increased distress and trauma associated with deaths during the pandemic, one clinical challenge is managing emotions in a virtual group without access to the usual tools that clinicians rely on, such as reading body language. Following a graded exposure approach, a form of behavioral therapy,14 we recommend offering a psycho-educational seminar first in which facilitators can control the content and limit exposure of sharing stories from participants. For support groups (eg, 6 to 8 sessions), we recommend that participants be screened prior to assess their risk factors and readiness and provide individual therapist referrals as needed.10
Community Outreach
Many diverse communities have been affected significantly by COVID-19 and faced high mortality rates.16 We recognized that proactive bereavement outreach to these communities was essential. Grief guides and tip sheets in various languages were made available as part of our community outreach programs, which included vans traveling to severely affected communities and providing testing, masks, alcohol-based hand sanitizer, and written materials.
Education About Bereavement
Many clinicians and staff express feelings of inadequacy about providing bereavement outreach. Such feelings are not uncommon, especially because clinicians tend to receive little training in dealing with the emotional toll of patient deaths and bereavement care.17,18 These feelings are likely to be heightened during this pandemic given the increased exposure to patient deaths, concern for personal safety, and changed practices in providing care, including the need to socially distance. Providing support for clinicians to process their feelings about the death of patients is crucial.19 In addition to our Employee Assistance Program, psychosocial clinicians are facilitating weekly virtual support groups for providers to discuss the effects of the pandemic on their personal and professional lives.
Bereaved family members report they benefit from hearing from the clinical team and receiving condolences, which is seen as humanizing the physician-family relationship. This personal outreach is likely more important during this time because many providers will have interacted with family members virtually.7,20,21 To help facilitate offers of condolences, we developed the TEARS acronym to describe the components of a condolence call that can also be adapted for writing condolence cards (Table).
GUIDELINES
We recommend that hospitals and other healthcare facilities that might not have well-established bereavement programs consider adopting a building block approach to provide basic outreach to families of their deceased patients.7 Tapping into existing resources, the major components are as follows: (1) a letter of condolence from leadership, (2) psycho-educational information about grief, (3) a list of community/online resources, including information about local hospice bereavement programs and bereavement camps or programs for children, (4) offers of condolences from individual providers/teams, and (5) mental health outreach as indicated.
CONCLUSION
The COVID-19–related mortality, particularly among already vulnerable populations, coupled with the existing underrecognition of bereavement has created an urgent public health issue that needs to be addressed. Given that few institutions offer standardized bereavement follow-up, we believe that hospital providers and mental health clinicians need to take a proactive approach to providing bereavement outreach to families affected by death during the pandemic.
Acknowledgments
The authors would like to acknowledge the Brigham Health Bereavement Committee and the staff of Care Continuum Management and the Department of Community Outreach at Brigham and Women’s Hospital.
Disclosures
No competing financial interests relevant to this article exist for Dr Morris, Ms Paterson, and Dr Mendu. Dr Morris receives royalties for two self-help books about grief published by Robinson and Dr Mendu provides consulting services for Bayer AG unrelated to the content of this article.
As of July 25, 2020, there had been 146,073 deaths from COVID-19 in the United States and 641,273 worldwide, with a disproportionate number of deaths occurring in historically disadvantaged minority groups, specifically African Americans.1,2 The number of decedents will continue to increase over the coming months, even as the number of new COVID-19 cases decreases. Given that, for each death, five persons are believed to be significantly affected,3 the number of bereaved individuals whose loved ones died during the pandemic in the United States alone is likely to be in the millions.
COVID-19–related mortality has become a pressing public health issue, and as a result, support for bereaved family members, especially for minority populations, is also an important public health issue.4 It is likely that bereaved individuals are at greater risk of poor bereavement outcomes during the pandemic—irrespective of whether the death was a result of COVID-19—because of social isolation. This is particularly true if loved ones died in the hospital and, due to visitor restrictions, faced limited or no visitation. For many, bereavement will be affected by stay-at-home orders and social distancing restrictions that reduce access to emotional support and rituals, such as funerals, that usually provide comfort.5
Urgent attention is needed to support bereaved individuals, to flatten the curve of mental health disorders associated with the death of loved ones during the pandemic. Within a preventive model of care, we offer guidelines for how hospitals, longitudinal providers, and mental health clinicians can provide bereavement outreach to all individuals whose loved ones died during the COVID-19 pandemic.
PUBLIC HEALTH MODEL OF BEREAVEMENT SUPPORT
The provision of bereavement care, including the assessment of risk for poor bereavement outcomes, is an essential component of high-quality end-of-life care endorsed by the hospice and palliative care movement.6 However, the development of standardized bereavement services has lagged behind that of other components of palliative care, varying greatly by institution and provider.7 Approximately 10% to 20% of bereaved individuals experience psychiatric difficulties following the death of a loved one, including prolonged grief disorder, posttraumatic stress disorder, and major depressive disorder.8 Risk factors include a hospital-based death, death in an intensive care unit (ICU), sudden death, not being able to say goodbye, and a history of psychiatric disorders.8,9
One of the biggest barriers in providing standardized bereavement services is the lack of a systematic process to identify individuals at risk of poor bereavement outcomes.10 Aoun et al developed a public health model of bereavement support that comprises a three-tiered approach to risk and the corresponding need for support.11 They propose that the low-risk group, approximately 60% of bereaved individuals, would primarily need support from family and friends, the moderate-risk group (30%) would need support from the wider community, and the high-risk group (10%) would need support from mental health providers.
It is reasonable to assume that many individuals whose loved ones died during the pandemic will fall into a high-risk group for poor bereavement outcomes, as identified by Aoun et al.11 Given a higher than usual inpatient mortality due to COVID-19 for certain populations and that bereavement care is already underrecognized within healthcare systems, hospitals and other healthcare facilities and their providers need to fill this void.
EDUCATION, GUIDANCE, AND SUPPORT MODEL
We adopted an education, guidance, and support model of bereavement support in 2019.7 This model has been shown to positively affect the experience of bereaved individuals, especially because of condolences from providers and psycho-educational information about coping with grief.7 Each month, a list of deceased patients and family contacts is generated from a mortality review database,12 and bereavement packets are mailed to family members; the packet includes a condolence letter from senior management, a psycho-educational grief guide, and a list of community-based resources. A social worker is also available to provide telephone support and to assist with mental health referrals. For patients who died in the COVID-19–specific units, social work also provides support and outreach to families.
Psycho-Education
During the early weeks of the pandemic, a tip sheet—”Grieving during a pandemic”13— was created to include in the bereavement packet and for distribution to community organizations within the hospital’s geographical area. This tip sheet offers strategies to facilitate coping based on the psychological model of cognitive-behavioral therapy (CBT).14 Topics addressed include understanding the nature of grief, self-care, adapting bereavement rituals in light of social distancing, challenging unhelpful thinking patterns that might lead to feelings of guilt especially regarding the death of the patient, and ways to obtain support during the pandemic. The tip sheet was made available in Spanish, French, Chinese, Haitian Creole, Portuguese, Arabic, and Russian given that our mortality data, consistent with preliminary findings from New York State, suggested higher death rates among Black/African American and Hispanic/Latino groups, compared with historical mortality statistics.15
Virtual Support
As part of our bereavement response during the COVID-19 crisis, we have launched virtual bereavement support for families impacted by the pandemic. It is challenging to identify the optimal type of support and timing, given the reliance on virtual outreach without in-person screening. With the increased distress and trauma associated with deaths during the pandemic, one clinical challenge is managing emotions in a virtual group without access to the usual tools that clinicians rely on, such as reading body language. Following a graded exposure approach, a form of behavioral therapy,14 we recommend offering a psycho-educational seminar first in which facilitators can control the content and limit exposure of sharing stories from participants. For support groups (eg, 6 to 8 sessions), we recommend that participants be screened prior to assess their risk factors and readiness and provide individual therapist referrals as needed.10
Community Outreach
Many diverse communities have been affected significantly by COVID-19 and faced high mortality rates.16 We recognized that proactive bereavement outreach to these communities was essential. Grief guides and tip sheets in various languages were made available as part of our community outreach programs, which included vans traveling to severely affected communities and providing testing, masks, alcohol-based hand sanitizer, and written materials.
Education About Bereavement
Many clinicians and staff express feelings of inadequacy about providing bereavement outreach. Such feelings are not uncommon, especially because clinicians tend to receive little training in dealing with the emotional toll of patient deaths and bereavement care.17,18 These feelings are likely to be heightened during this pandemic given the increased exposure to patient deaths, concern for personal safety, and changed practices in providing care, including the need to socially distance. Providing support for clinicians to process their feelings about the death of patients is crucial.19 In addition to our Employee Assistance Program, psychosocial clinicians are facilitating weekly virtual support groups for providers to discuss the effects of the pandemic on their personal and professional lives.
Bereaved family members report they benefit from hearing from the clinical team and receiving condolences, which is seen as humanizing the physician-family relationship. This personal outreach is likely more important during this time because many providers will have interacted with family members virtually.7,20,21 To help facilitate offers of condolences, we developed the TEARS acronym to describe the components of a condolence call that can also be adapted for writing condolence cards (Table).
GUIDELINES
We recommend that hospitals and other healthcare facilities that might not have well-established bereavement programs consider adopting a building block approach to provide basic outreach to families of their deceased patients.7 Tapping into existing resources, the major components are as follows: (1) a letter of condolence from leadership, (2) psycho-educational information about grief, (3) a list of community/online resources, including information about local hospice bereavement programs and bereavement camps or programs for children, (4) offers of condolences from individual providers/teams, and (5) mental health outreach as indicated.
CONCLUSION
The COVID-19–related mortality, particularly among already vulnerable populations, coupled with the existing underrecognition of bereavement has created an urgent public health issue that needs to be addressed. Given that few institutions offer standardized bereavement follow-up, we believe that hospital providers and mental health clinicians need to take a proactive approach to providing bereavement outreach to families affected by death during the pandemic.
Acknowledgments
The authors would like to acknowledge the Brigham Health Bereavement Committee and the staff of Care Continuum Management and the Department of Community Outreach at Brigham and Women’s Hospital.
Disclosures
No competing financial interests relevant to this article exist for Dr Morris, Ms Paterson, and Dr Mendu. Dr Morris receives royalties for two self-help books about grief published by Robinson and Dr Mendu provides consulting services for Bayer AG unrelated to the content of this article.
1. Coronavirus Resource Center Covid-19: Case Tracker. Johns Hopkins University. Accessed July 25, 2020. https://coronavirus.jhu.edu/
2. Tappe A. America’s black and Hispanic communities are bearing the brunt of the coronavirus. CNN. April 21, 2020. Accessed June 7, 2020. https://www.cnn.com/2020/04/21/economy/coronavirus-burden-black-hispanic-workers/index.html
3. Shear K, Frank E, Houck PR, Reynolds CF 3rd. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608. https://doi.org/10.1001/jama.293.21.2601
4. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med. 2020;382(26):2534-2543. https://doi.org/10.1056/nejmsa2011686
5. Morris SE, Moment A, Thomas JD. Caring for bereaved family members during the COVID-19 pandemic: before and after the death of a patient. J Pain Symptom Manage. Published online May 7, 2020. https://doi.org/10.1016/j.jpainsymman.2020.05.002
6. National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 4th ed. National Coalition for Hospice and Palliative Care; 2018. Accessed June 7, 2020. https://www.nationalcoalitionhpc.org/ncp
7. Morris SE, Block SD. Adding value to palliative care services: the development of an institutional bereavement program. J Palliat Med. 2015;18(11):915-922. https://doi.org/10.1089/jpm.2015.0080
8. Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960-1973. https://doi.org/10.1016/s0140-6736(07)61816-9
9. Kentish-Barnes N, Chaize M, Seegers V, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J. 2015;45(5):1341-1352. https://doi.org/10.1183/09031936.00160014
10. Morris SE, Anderson CM, Tarquini SJ, Block SD. A standardized approach to bereavement risk-screening: a quality improvement project. J Psychosoc Oncol. 2020;38(4):406-417. https://doi.org/10.1080/07347332.2019.1703065
11. Aoun SM, Breen LJ, Howting DA, Rumbold B, McNamara B, Hegney D. Who needs bereavement support? a population based survey of bereavement risk and support need. PLoS One. 2015;10(3):e0121101. https://doi.org/10.1371/journal.pone.0121101
12. Mendu ML, Lu Y, Petersen A, et al. Reflections on implementing a hospital-wide provider-based electronic inpatient mortality review system: lessons learnt. BMJ Qual Saf. 2020;29(4):304‐312. https://doi.org/10.1136/bmjqs-2019-009864
13. Morris SE. Grieving during a pandemic. Brigham and Women’s Hospital. Accessed July 25, 2020. https://www.brighamandwomens.org/covid-19/grieving-during-a-pandemic
14. Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed. Guilford Press; 2011.
15. Coronavirus Disease 2019 (COVID-19). Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Updated July 24, 2020. Accessed July 25, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
16. Death rates in Mass. surged in areas already hard hit. Boston Globe. May 17, 2020. Accessed June 8, 2020. https://www.bostonglobe.com/2020/05/17/opinion/death-rate-mass-surged-areas-already-hard-hit/
17. Jackson VA, Sullivan AM, Gadmer NM, et al. “It was haunting…”: physicians’ descriptions of emotionally powerful patient deaths. Acad Med. 2005;80(7):648-656. https://doi.org/10.1097/00001888-200507000-00007
18. Morris S, Schaefer K, Rosowsky E. Primary care for the elderly bereaved: recommendations for medical education. J Clin Psychol Med Settings. 2018;25(4):463‐470. https://doi.org/10.1007/s10880-018-9556-9
19. Morris SE, Kearns JP, Moment A, Lee KA, deLima Thomas J. “Remembrance”: a self-care tool for clinicians. J Palliat Med. 2019;22(3):316-318. https://doi.org/10.1089/jpm.2018.0395
20. Morris SE, Nayak MM, Block SD. Insights from bereaved family members about end-of-life care and bereavement. J Palliat Med. Published online February 10, 2020. https://doi.org/10.1089/jpm.2019.0467
21. Kentish-Barnes N, Cohen-Solal Z, Souppart V, et al. “It was the only thing I could hold onto, but…”: receiving a letter of condolence after loss of a loved one in the ICU: a qualitative study of bereaved relatives’ experience. Crit Care Med. 2017;45(12):1965-1971. https://doi.org/10.1097/ccm.0000000000002687
1. Coronavirus Resource Center Covid-19: Case Tracker. Johns Hopkins University. Accessed July 25, 2020. https://coronavirus.jhu.edu/
2. Tappe A. America’s black and Hispanic communities are bearing the brunt of the coronavirus. CNN. April 21, 2020. Accessed June 7, 2020. https://www.cnn.com/2020/04/21/economy/coronavirus-burden-black-hispanic-workers/index.html
3. Shear K, Frank E, Houck PR, Reynolds CF 3rd. Treatment of complicated grief: a randomized controlled trial. JAMA. 2005;293(21):2601-2608. https://doi.org/10.1001/jama.293.21.2601
4. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med. 2020;382(26):2534-2543. https://doi.org/10.1056/nejmsa2011686
5. Morris SE, Moment A, Thomas JD. Caring for bereaved family members during the COVID-19 pandemic: before and after the death of a patient. J Pain Symptom Manage. Published online May 7, 2020. https://doi.org/10.1016/j.jpainsymman.2020.05.002
6. National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 4th ed. National Coalition for Hospice and Palliative Care; 2018. Accessed June 7, 2020. https://www.nationalcoalitionhpc.org/ncp
7. Morris SE, Block SD. Adding value to palliative care services: the development of an institutional bereavement program. J Palliat Med. 2015;18(11):915-922. https://doi.org/10.1089/jpm.2015.0080
8. Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960-1973. https://doi.org/10.1016/s0140-6736(07)61816-9
9. Kentish-Barnes N, Chaize M, Seegers V, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J. 2015;45(5):1341-1352. https://doi.org/10.1183/09031936.00160014
10. Morris SE, Anderson CM, Tarquini SJ, Block SD. A standardized approach to bereavement risk-screening: a quality improvement project. J Psychosoc Oncol. 2020;38(4):406-417. https://doi.org/10.1080/07347332.2019.1703065
11. Aoun SM, Breen LJ, Howting DA, Rumbold B, McNamara B, Hegney D. Who needs bereavement support? a population based survey of bereavement risk and support need. PLoS One. 2015;10(3):e0121101. https://doi.org/10.1371/journal.pone.0121101
12. Mendu ML, Lu Y, Petersen A, et al. Reflections on implementing a hospital-wide provider-based electronic inpatient mortality review system: lessons learnt. BMJ Qual Saf. 2020;29(4):304‐312. https://doi.org/10.1136/bmjqs-2019-009864
13. Morris SE. Grieving during a pandemic. Brigham and Women’s Hospital. Accessed July 25, 2020. https://www.brighamandwomens.org/covid-19/grieving-during-a-pandemic
14. Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed. Guilford Press; 2011.
15. Coronavirus Disease 2019 (COVID-19). Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Updated July 24, 2020. Accessed July 25, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
16. Death rates in Mass. surged in areas already hard hit. Boston Globe. May 17, 2020. Accessed June 8, 2020. https://www.bostonglobe.com/2020/05/17/opinion/death-rate-mass-surged-areas-already-hard-hit/
17. Jackson VA, Sullivan AM, Gadmer NM, et al. “It was haunting…”: physicians’ descriptions of emotionally powerful patient deaths. Acad Med. 2005;80(7):648-656. https://doi.org/10.1097/00001888-200507000-00007
18. Morris S, Schaefer K, Rosowsky E. Primary care for the elderly bereaved: recommendations for medical education. J Clin Psychol Med Settings. 2018;25(4):463‐470. https://doi.org/10.1007/s10880-018-9556-9
19. Morris SE, Kearns JP, Moment A, Lee KA, deLima Thomas J. “Remembrance”: a self-care tool for clinicians. J Palliat Med. 2019;22(3):316-318. https://doi.org/10.1089/jpm.2018.0395
20. Morris SE, Nayak MM, Block SD. Insights from bereaved family members about end-of-life care and bereavement. J Palliat Med. Published online February 10, 2020. https://doi.org/10.1089/jpm.2019.0467
21. Kentish-Barnes N, Cohen-Solal Z, Souppart V, et al. “It was the only thing I could hold onto, but…”: receiving a letter of condolence after loss of a loved one in the ICU: a qualitative study of bereaved relatives’ experience. Crit Care Med. 2017;45(12):1965-1971. https://doi.org/10.1097/ccm.0000000000002687
© 2020 Society of Hospital Medicine
