User login
Student Hospitalist Scholars: Preventing unplanned PICU transfers
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Pediatric hospital medicine marches toward subspecialty recognition
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
The role of NPs and PAs in hospital medicine programs
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
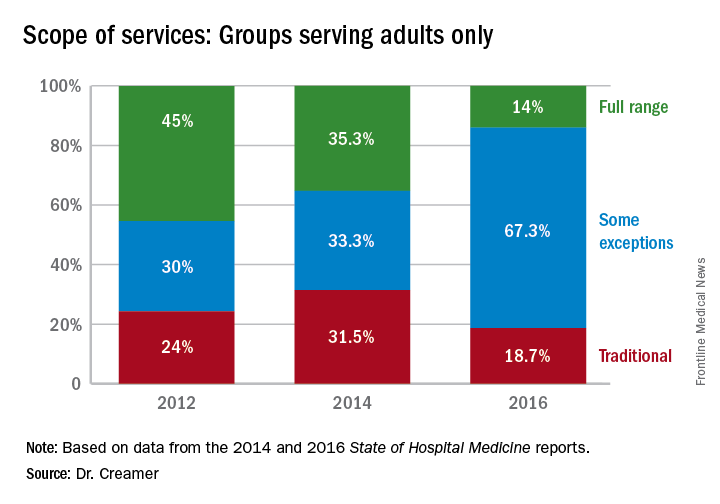
Hospitalists’ scope of services continues to evolve
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
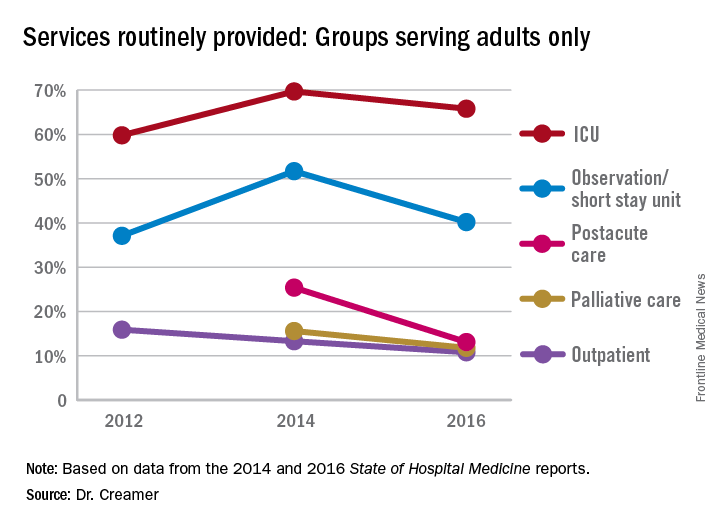
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
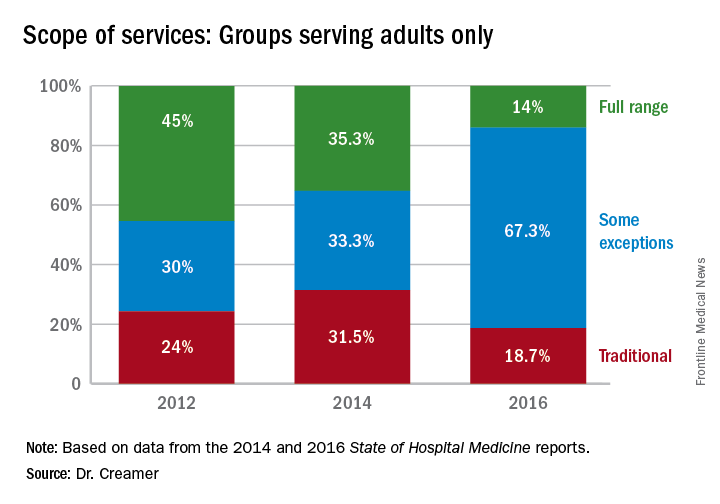
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
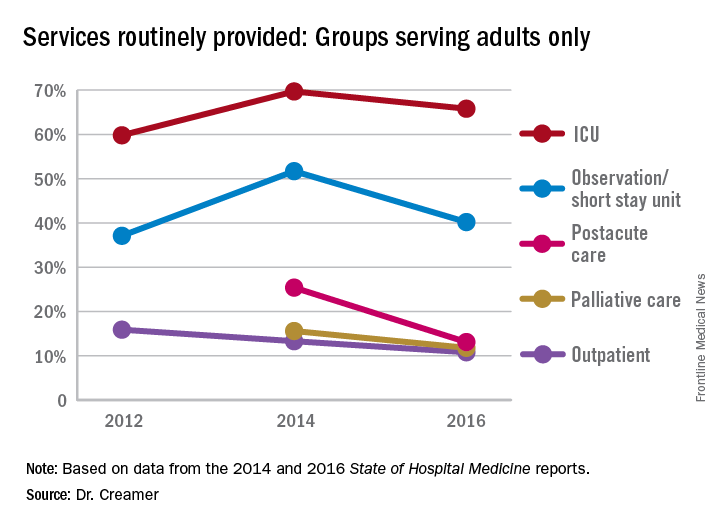
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
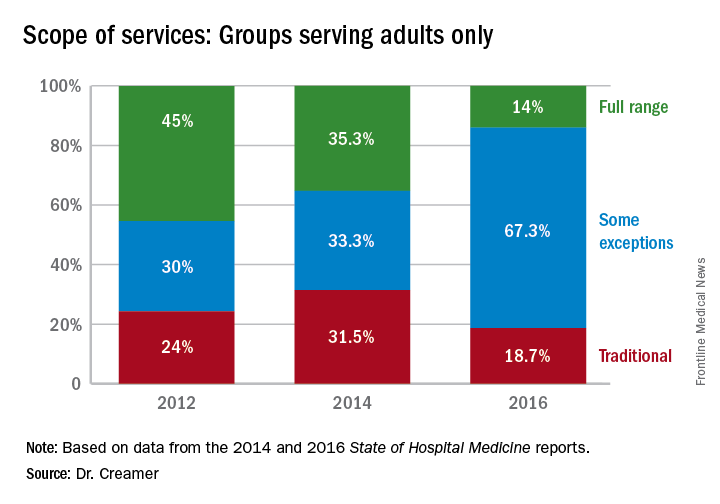
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
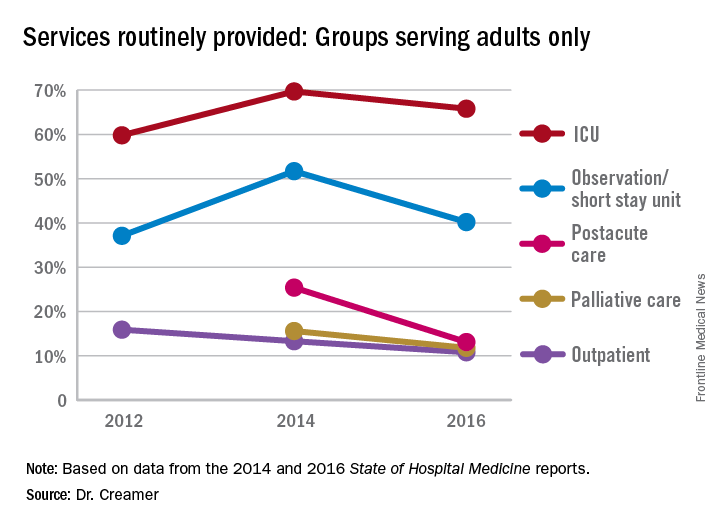
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Pediatrics Committee’s role amplified with subspecialty’s evolution
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. For more information on how you can lend your expertise to help SHM improve the care of hospitalized patients, log on to www.hospitalmedicine.org/getinvolved.
This month, The Hospitalist spotlights Sandra Gage, MD, PhD, SFHM, associate professor of pediatrics in the section of hospital medicine at the Medical College of Wisconsin, newly appointed chair of SHM’s Pediatrics Committee, and SHM member of almost 20 years.
Why did you choose a career in pediatric hospital medicine, and how did you become an SHM member?
I would say that pediatric hospital medicine chose me. After obtaining a degree in physical therapy and spending five years treating children with a variety of neurological and neurodevelopmental disorders, I went back to school to get my MD and a PhD in neurobiology, thinking that I would specialize in either pediatric neurology or pediatric physical medicine and rehabilitation.
I always had an interest in treating children but never considered general pediatrics because spending my time in the outpatient clinic setting had little appeal for me. This was before the concept of being a “hospitalist” was widespread – and even before the phrase was coined – but there were a few providers in my academic pediatric group who focused on inpatient care. The pace, variety and challenge of treating hospitalized children was exactly what I was looking for, and, following completion of my pediatric residency, I slowly became a full-time hospitalist.
What is the Pediatrics Committee currently working on, and what do you hope to accomplish during your term as Committee Chair?
With subspecialty status coming soon, rapidly expanding interest in the profession and the introduction of hospitalists into more areas of care, the landscape of pediatric hospital medicine is ever-changing. This amplifies the importance of the Pediatrics Committee’s role. The overall goals of the committee are to promote the growth and development of pediatric hospital medicine as a field and to provide educational and practical resources for individual practitioners.
The 2017-2018 committee comprises enthusiastic members from a wide variety of practice settings. At our first meeting in May, we formulated many exciting and innovative ideas to achieve our goals. As we continue to narrow down our approach and finalize our tasks for the year, we are also beginning to determine the content for the pediatric track at HM18. An example of a project the committee has executed in the past is the development of hospitalist-specific American Board of Pediatrics Maintenance of Certification modules for the SHM Learning Portal. In addition, the 2017 Pediatric Hospital Medicine (PHM) meeting is hosted by SHM this July in Nashville, and many Pediatrics Committee members are hard at work on finalizing those plans.
How has the PHM meeting evolved since its inception, and what value do you find in attending?
I have been an attendee of PHM many times over the years. The meeting has grown from a small group of no more than 100 individuals in a few hotel meeting rooms to more than 1,000 attendees and a wide variety of tracks and offerings. The growth of this meeting is truly reflective of the growth of our subspecialty, and the meeting brings together practitioners, both old and new, in an atmosphere full of innovations and ideas. Like SHM’s annual meeting, the PHM meeting is a great place for learning, sharing, and networking.
What advice do you have for fellow pediatric hospitalists during this transformational time in health care?
The direction of health care has provided fodder for lively discussion since I started my career 20 years ago. The nature of the practice of medicine is evolving, and, as physicians, we must be adept at navigating the changing climate while maintaining our goal of providing excellent care for our patients. As hospitalists, we have the opportunity to be in the forefront of the changes that will impact hospital care and utilization.
Whether our work is done at a local or a national level, as a group or as individuals, I believe that hospitalists will have an active role in directing the course of the future of medicine. We spend much of our clinical time advocating for our patients, but your experience is important and your voice can make an important contribution to the direction of health care for one child or for all children. Whether it is in the hospital hallway or on the Hill, continue to strive to do what you already do best.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. For more information on how you can lend your expertise to help SHM improve the care of hospitalized patients, log on to www.hospitalmedicine.org/getinvolved.
This month, The Hospitalist spotlights Sandra Gage, MD, PhD, SFHM, associate professor of pediatrics in the section of hospital medicine at the Medical College of Wisconsin, newly appointed chair of SHM’s Pediatrics Committee, and SHM member of almost 20 years.
Why did you choose a career in pediatric hospital medicine, and how did you become an SHM member?
I would say that pediatric hospital medicine chose me. After obtaining a degree in physical therapy and spending five years treating children with a variety of neurological and neurodevelopmental disorders, I went back to school to get my MD and a PhD in neurobiology, thinking that I would specialize in either pediatric neurology or pediatric physical medicine and rehabilitation.
I always had an interest in treating children but never considered general pediatrics because spending my time in the outpatient clinic setting had little appeal for me. This was before the concept of being a “hospitalist” was widespread – and even before the phrase was coined – but there were a few providers in my academic pediatric group who focused on inpatient care. The pace, variety and challenge of treating hospitalized children was exactly what I was looking for, and, following completion of my pediatric residency, I slowly became a full-time hospitalist.
What is the Pediatrics Committee currently working on, and what do you hope to accomplish during your term as Committee Chair?
With subspecialty status coming soon, rapidly expanding interest in the profession and the introduction of hospitalists into more areas of care, the landscape of pediatric hospital medicine is ever-changing. This amplifies the importance of the Pediatrics Committee’s role. The overall goals of the committee are to promote the growth and development of pediatric hospital medicine as a field and to provide educational and practical resources for individual practitioners.
The 2017-2018 committee comprises enthusiastic members from a wide variety of practice settings. At our first meeting in May, we formulated many exciting and innovative ideas to achieve our goals. As we continue to narrow down our approach and finalize our tasks for the year, we are also beginning to determine the content for the pediatric track at HM18. An example of a project the committee has executed in the past is the development of hospitalist-specific American Board of Pediatrics Maintenance of Certification modules for the SHM Learning Portal. In addition, the 2017 Pediatric Hospital Medicine (PHM) meeting is hosted by SHM this July in Nashville, and many Pediatrics Committee members are hard at work on finalizing those plans.
How has the PHM meeting evolved since its inception, and what value do you find in attending?
I have been an attendee of PHM many times over the years. The meeting has grown from a small group of no more than 100 individuals in a few hotel meeting rooms to more than 1,000 attendees and a wide variety of tracks and offerings. The growth of this meeting is truly reflective of the growth of our subspecialty, and the meeting brings together practitioners, both old and new, in an atmosphere full of innovations and ideas. Like SHM’s annual meeting, the PHM meeting is a great place for learning, sharing, and networking.
What advice do you have for fellow pediatric hospitalists during this transformational time in health care?
The direction of health care has provided fodder for lively discussion since I started my career 20 years ago. The nature of the practice of medicine is evolving, and, as physicians, we must be adept at navigating the changing climate while maintaining our goal of providing excellent care for our patients. As hospitalists, we have the opportunity to be in the forefront of the changes that will impact hospital care and utilization.
Whether our work is done at a local or a national level, as a group or as individuals, I believe that hospitalists will have an active role in directing the course of the future of medicine. We spend much of our clinical time advocating for our patients, but your experience is important and your voice can make an important contribution to the direction of health care for one child or for all children. Whether it is in the hospital hallway or on the Hill, continue to strive to do what you already do best.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. For more information on how you can lend your expertise to help SHM improve the care of hospitalized patients, log on to www.hospitalmedicine.org/getinvolved.
This month, The Hospitalist spotlights Sandra Gage, MD, PhD, SFHM, associate professor of pediatrics in the section of hospital medicine at the Medical College of Wisconsin, newly appointed chair of SHM’s Pediatrics Committee, and SHM member of almost 20 years.
Why did you choose a career in pediatric hospital medicine, and how did you become an SHM member?
I would say that pediatric hospital medicine chose me. After obtaining a degree in physical therapy and spending five years treating children with a variety of neurological and neurodevelopmental disorders, I went back to school to get my MD and a PhD in neurobiology, thinking that I would specialize in either pediatric neurology or pediatric physical medicine and rehabilitation.
I always had an interest in treating children but never considered general pediatrics because spending my time in the outpatient clinic setting had little appeal for me. This was before the concept of being a “hospitalist” was widespread – and even before the phrase was coined – but there were a few providers in my academic pediatric group who focused on inpatient care. The pace, variety and challenge of treating hospitalized children was exactly what I was looking for, and, following completion of my pediatric residency, I slowly became a full-time hospitalist.
What is the Pediatrics Committee currently working on, and what do you hope to accomplish during your term as Committee Chair?
With subspecialty status coming soon, rapidly expanding interest in the profession and the introduction of hospitalists into more areas of care, the landscape of pediatric hospital medicine is ever-changing. This amplifies the importance of the Pediatrics Committee’s role. The overall goals of the committee are to promote the growth and development of pediatric hospital medicine as a field and to provide educational and practical resources for individual practitioners.
The 2017-2018 committee comprises enthusiastic members from a wide variety of practice settings. At our first meeting in May, we formulated many exciting and innovative ideas to achieve our goals. As we continue to narrow down our approach and finalize our tasks for the year, we are also beginning to determine the content for the pediatric track at HM18. An example of a project the committee has executed in the past is the development of hospitalist-specific American Board of Pediatrics Maintenance of Certification modules for the SHM Learning Portal. In addition, the 2017 Pediatric Hospital Medicine (PHM) meeting is hosted by SHM this July in Nashville, and many Pediatrics Committee members are hard at work on finalizing those plans.
How has the PHM meeting evolved since its inception, and what value do you find in attending?
I have been an attendee of PHM many times over the years. The meeting has grown from a small group of no more than 100 individuals in a few hotel meeting rooms to more than 1,000 attendees and a wide variety of tracks and offerings. The growth of this meeting is truly reflective of the growth of our subspecialty, and the meeting brings together practitioners, both old and new, in an atmosphere full of innovations and ideas. Like SHM’s annual meeting, the PHM meeting is a great place for learning, sharing, and networking.
What advice do you have for fellow pediatric hospitalists during this transformational time in health care?
The direction of health care has provided fodder for lively discussion since I started my career 20 years ago. The nature of the practice of medicine is evolving, and, as physicians, we must be adept at navigating the changing climate while maintaining our goal of providing excellent care for our patients. As hospitalists, we have the opportunity to be in the forefront of the changes that will impact hospital care and utilization.
Whether our work is done at a local or a national level, as a group or as individuals, I believe that hospitalists will have an active role in directing the course of the future of medicine. We spend much of our clinical time advocating for our patients, but your experience is important and your voice can make an important contribution to the direction of health care for one child or for all children. Whether it is in the hospital hallway or on the Hill, continue to strive to do what you already do best.
Felicia Steele is SHM’s communications coordinator.
QI enthusiast to QI leader: John Bulger, DO
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of John Bulger, DO, chief medical officer for Geisinger Health Plan.
As chief medical officer for Geisinger Health Plan, John Bulger, DO, MBA, is intimately acquainted with the daily challenges that intersect with the delivery of safe, quality-driven care in the hospital system.
He’s also very familiar with the intricacies of carving out a professional road map. When Dr. Bulger began practicing as an internist at Geisinger Health System in the late 1990s, there wasn’t a formal hospitalist designation. He created one and became director of the hospital medicine program. Years later, when the opportunity arose to become chief quality officer, Dr. Bulger was a natural fit for the position, having led many improvement-centered committees and projects while running the hospital medicine group.
Early in his QI immersion, Dr. Bulger sought training where available from sources such as ACP and SHM, while familiarizing himself with methodologies such as PDSA and Lean. There are far more QI training opportunities available to hospitalists today than when Dr. Bulger began his journey, but the fundamentals of success come back to finding the right mentors, team building, and implementing projects built around SMART goals.
Getting started, Dr. Bulger suggests to “pick something within your scope, like medical reconciliation for every patient, or ensuring that every patient who leaves the hospital gets an appointment with their primary physician within 7 days. Early on, we were working on issues like pneumonia core measures and providing discharge instructions.”
He cautions those starting out in QI against viewing unintended outcomes or project setbacks as failure. “If your goal is to take a (scenario) from bad to perfect, you’ll end up getting discouraged. Any effort toward making things better is helpful. If it doesn’t work you try something else.”
While Dr. Bulger is fully supportive of the impact that quality improvement projects make at the institutional level, he encourages clinicians and researchers to always keep the Institute for Healthcare Improvement Triple Aim in sight.
“We need better measures and more discussion about what is best for patients,” Dr. Bulger said. “The things we talk about in (health care) – readmission rates, glycemic control – have a minimal impact on people’s health, but the social determinants of health – the patient’s housing and economic situation – play a bigger role than anything else. As we move from provider- to patient-centric communities by fixing the Triple Aim, the experience will be better for both providers and patients.”
Claudia Stahl is content manager for the Society of Hospital Medicine.
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of John Bulger, DO, chief medical officer for Geisinger Health Plan.
As chief medical officer for Geisinger Health Plan, John Bulger, DO, MBA, is intimately acquainted with the daily challenges that intersect with the delivery of safe, quality-driven care in the hospital system.
He’s also very familiar with the intricacies of carving out a professional road map. When Dr. Bulger began practicing as an internist at Geisinger Health System in the late 1990s, there wasn’t a formal hospitalist designation. He created one and became director of the hospital medicine program. Years later, when the opportunity arose to become chief quality officer, Dr. Bulger was a natural fit for the position, having led many improvement-centered committees and projects while running the hospital medicine group.
Early in his QI immersion, Dr. Bulger sought training where available from sources such as ACP and SHM, while familiarizing himself with methodologies such as PDSA and Lean. There are far more QI training opportunities available to hospitalists today than when Dr. Bulger began his journey, but the fundamentals of success come back to finding the right mentors, team building, and implementing projects built around SMART goals.
Getting started, Dr. Bulger suggests to “pick something within your scope, like medical reconciliation for every patient, or ensuring that every patient who leaves the hospital gets an appointment with their primary physician within 7 days. Early on, we were working on issues like pneumonia core measures and providing discharge instructions.”
He cautions those starting out in QI against viewing unintended outcomes or project setbacks as failure. “If your goal is to take a (scenario) from bad to perfect, you’ll end up getting discouraged. Any effort toward making things better is helpful. If it doesn’t work you try something else.”
While Dr. Bulger is fully supportive of the impact that quality improvement projects make at the institutional level, he encourages clinicians and researchers to always keep the Institute for Healthcare Improvement Triple Aim in sight.
“We need better measures and more discussion about what is best for patients,” Dr. Bulger said. “The things we talk about in (health care) – readmission rates, glycemic control – have a minimal impact on people’s health, but the social determinants of health – the patient’s housing and economic situation – play a bigger role than anything else. As we move from provider- to patient-centric communities by fixing the Triple Aim, the experience will be better for both providers and patients.”
Claudia Stahl is content manager for the Society of Hospital Medicine.
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of John Bulger, DO, chief medical officer for Geisinger Health Plan.
As chief medical officer for Geisinger Health Plan, John Bulger, DO, MBA, is intimately acquainted with the daily challenges that intersect with the delivery of safe, quality-driven care in the hospital system.
He’s also very familiar with the intricacies of carving out a professional road map. When Dr. Bulger began practicing as an internist at Geisinger Health System in the late 1990s, there wasn’t a formal hospitalist designation. He created one and became director of the hospital medicine program. Years later, when the opportunity arose to become chief quality officer, Dr. Bulger was a natural fit for the position, having led many improvement-centered committees and projects while running the hospital medicine group.
Early in his QI immersion, Dr. Bulger sought training where available from sources such as ACP and SHM, while familiarizing himself with methodologies such as PDSA and Lean. There are far more QI training opportunities available to hospitalists today than when Dr. Bulger began his journey, but the fundamentals of success come back to finding the right mentors, team building, and implementing projects built around SMART goals.
Getting started, Dr. Bulger suggests to “pick something within your scope, like medical reconciliation for every patient, or ensuring that every patient who leaves the hospital gets an appointment with their primary physician within 7 days. Early on, we were working on issues like pneumonia core measures and providing discharge instructions.”
He cautions those starting out in QI against viewing unintended outcomes or project setbacks as failure. “If your goal is to take a (scenario) from bad to perfect, you’ll end up getting discouraged. Any effort toward making things better is helpful. If it doesn’t work you try something else.”
While Dr. Bulger is fully supportive of the impact that quality improvement projects make at the institutional level, he encourages clinicians and researchers to always keep the Institute for Healthcare Improvement Triple Aim in sight.
“We need better measures and more discussion about what is best for patients,” Dr. Bulger said. “The things we talk about in (health care) – readmission rates, glycemic control – have a minimal impact on people’s health, but the social determinants of health – the patient’s housing and economic situation – play a bigger role than anything else. As we move from provider- to patient-centric communities by fixing the Triple Aim, the experience will be better for both providers and patients.”
Claudia Stahl is content manager for the Society of Hospital Medicine.
Here’s what’s trending at SHM: July 2017
Updated Clinical Documentation & Coding resources now available
SHM’s Clinical Documentation & Coding for Hospitalists, formerly CODE-H, has been updated for 2017.
“[It’s] an exciting program that offers valuable insight into the coding and billing challenges of hospitalist services. Whether you are a new or seasoned physician, SHM’s Clinical Documentation & Coding for Hospitalists provides you with a solid foundation for documentation, identifies common problems, and offers strategies for success.” – Carol Pohlig, BSN, RN, CPC, ASC Senior Coding and Compliance Specialist
For more information, visit hospitalmedicine.org/codeh.
Registration now open for NP/PA Bootcamp
Whether you’re new to hospital medicine or need a refresher on the latest topics, this course from the AAPA and SHM is perfect for you and offers up to 34.75 AAPA Category 1 CME credits.
At the Adult Hospital Medicine Bootcamp, you will cover commonly encountered diagnoses and diseases of adult hospitalized patients while networking with other hospital-based practitioners. Plus, attend optional pre-courses on reimbursement, hands-on ultrasound or hospital medicine basics.
Join us at the ninth annual Adult Hospital Medicine Boot Camp, September 27 – October 1, 2017, in San Diego. To register and learn more visit: aapa.org/bootcamp.
Learn how your HMG stacks up with the State of Hospital Medicine report
Did you know that hospitalist compensation typically consists of 80% base pay and 20% supplemental income based on production and performance? SHM’s State of Hospital Medicine Report continues to be your best source of information about how hospital medicine groups (HMGs) operate.
Don’t miss the new additions to the report for the 2016 version, including:
• Percentage of the hospital’s total patient volume the HMG was responsible for caring for.
• Presence of medical hospitalists within the HMG focusing their practice in a specific medical subspecialty.
• Value of CME allowances for hospitalists.
• Utilization of prolonged service codes by hospitalists.
• Charge capture methodologies being used by HMGs.
• For academic HMGs, the dollar amount of financial support provided for non-clinical work.
Order your print or digital copy at hospitalmedicine.org/sohm.
Enhance your leadership skills at SHM’s Leadership Academy
SHM’s Leadership Academy is the only leadership program designed specifically for hospitalists. The 2017 meeting will be held October 23 – 26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
Course highlight: Leadership mastering teamwork
Developed in response to high demand from previous Leadership Academy attendees, this course focuses on strengthening teams and institutions. Participants learn how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and develop effective communication strategies.
Upon completion of this course, participants will be able to apply communication strategies that allow others to fully experience their message, lead teams in complex environments to achieve the best results, invest in themselves as leaders to optimize their professional growth and career path, and critically assess program growth opportunities and implement the necessary infrastructure for success.
To view the course schedule, faculty and more visit shmleadershipacademy.org/masteringteamwork.
Improve glycemic control efforts in your hospital with online resources & mentorship
SHM offers a variety of resources to improve glycemic control in your hospital. Glycemic Control Electronic Quality Improvement Programs (eQUIPS) are designed to enhance the efficiency and reliability of your quality improvement efforts to close the gap between best practices and methods for caring for the inpatient with hyperglycemia.
Benefits of SHM’s eQUIPS include:
• Data and performance tracking tools.
• Step-by-step instructions for improving glycemic control, preventing hypoglycemia, and optimizing care of inpatients with hyperglycemia and diabetes.
• An online community and library of tools and documents, including sample order sets and protocols, awareness campaigns, patient educational materials, and supplemental articles.
• Toolkit of clinical tools and interventions, research materials, literature reviews, case studies, teaching slide sets, and more.
SHM’s Glycemic Control Mentored Implementation program sites receive 1 year of individualized mentoring including:
• On-site mentoring and training for the entire care team to help members interpret needs and resource assessments, map system processes, and develop site-specific action and intervention plans.
• Monthly coaching calls with the mentor to develop, modify, and implement interventions, establish evaluation processes, and monitor performance over time.
• SHM-facilitated calls with live webinars with other sites in the collaborative to share success stories and experiences.
• Access to the online community to share ideas, documents, and other resources.
• Data collection and analysis tools to generate on-demand reports and benchmark against other program participants.
Learn more about all of SHM’s Glycemic Control offerings by watching the recorded webinar from June 28, 2017, at hospitalmedicine.org/gc.
Earn CME with SHM’s Learning Portal
SHM’s Learning Portal is the online learning destination for hospitalists, featuring all of SHM’s eLearning initiatives in one place. Members can access over 85 CME credits for free in the Learning Portal.
Featured topics currently include perioperative medicine, anticoagulation, quality improvement, cardiac arrhythmia, and antimicrobial stewardship.
Try out the most popular modules:
• The Role of the Medical Consultant.
• Pulmonary Risk Management in the Perioperative Setting.
• Perioperative Medication Management.
• Venous Thromboembolism Prophylaxis in Surgical Patients.
• Perioperative Cardiac Risk Assessment.
Not a member? Join today or pay a small fee per module. Visit shmlearningportal.org to learn more and earn CME credits today.
Brett Radler is communications specialist at the Society of Hospital Medicine.
Updated Clinical Documentation & Coding resources now available
SHM’s Clinical Documentation & Coding for Hospitalists, formerly CODE-H, has been updated for 2017.
“[It’s] an exciting program that offers valuable insight into the coding and billing challenges of hospitalist services. Whether you are a new or seasoned physician, SHM’s Clinical Documentation & Coding for Hospitalists provides you with a solid foundation for documentation, identifies common problems, and offers strategies for success.” – Carol Pohlig, BSN, RN, CPC, ASC Senior Coding and Compliance Specialist
For more information, visit hospitalmedicine.org/codeh.
Registration now open for NP/PA Bootcamp
Whether you’re new to hospital medicine or need a refresher on the latest topics, this course from the AAPA and SHM is perfect for you and offers up to 34.75 AAPA Category 1 CME credits.
At the Adult Hospital Medicine Bootcamp, you will cover commonly encountered diagnoses and diseases of adult hospitalized patients while networking with other hospital-based practitioners. Plus, attend optional pre-courses on reimbursement, hands-on ultrasound or hospital medicine basics.
Join us at the ninth annual Adult Hospital Medicine Boot Camp, September 27 – October 1, 2017, in San Diego. To register and learn more visit: aapa.org/bootcamp.
Learn how your HMG stacks up with the State of Hospital Medicine report
Did you know that hospitalist compensation typically consists of 80% base pay and 20% supplemental income based on production and performance? SHM’s State of Hospital Medicine Report continues to be your best source of information about how hospital medicine groups (HMGs) operate.
Don’t miss the new additions to the report for the 2016 version, including:
• Percentage of the hospital’s total patient volume the HMG was responsible for caring for.
• Presence of medical hospitalists within the HMG focusing their practice in a specific medical subspecialty.
• Value of CME allowances for hospitalists.
• Utilization of prolonged service codes by hospitalists.
• Charge capture methodologies being used by HMGs.
• For academic HMGs, the dollar amount of financial support provided for non-clinical work.
Order your print or digital copy at hospitalmedicine.org/sohm.
Enhance your leadership skills at SHM’s Leadership Academy
SHM’s Leadership Academy is the only leadership program designed specifically for hospitalists. The 2017 meeting will be held October 23 – 26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
Course highlight: Leadership mastering teamwork
Developed in response to high demand from previous Leadership Academy attendees, this course focuses on strengthening teams and institutions. Participants learn how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and develop effective communication strategies.
Upon completion of this course, participants will be able to apply communication strategies that allow others to fully experience their message, lead teams in complex environments to achieve the best results, invest in themselves as leaders to optimize their professional growth and career path, and critically assess program growth opportunities and implement the necessary infrastructure for success.
To view the course schedule, faculty and more visit shmleadershipacademy.org/masteringteamwork.
Improve glycemic control efforts in your hospital with online resources & mentorship
SHM offers a variety of resources to improve glycemic control in your hospital. Glycemic Control Electronic Quality Improvement Programs (eQUIPS) are designed to enhance the efficiency and reliability of your quality improvement efforts to close the gap between best practices and methods for caring for the inpatient with hyperglycemia.
Benefits of SHM’s eQUIPS include:
• Data and performance tracking tools.
• Step-by-step instructions for improving glycemic control, preventing hypoglycemia, and optimizing care of inpatients with hyperglycemia and diabetes.
• An online community and library of tools and documents, including sample order sets and protocols, awareness campaigns, patient educational materials, and supplemental articles.
• Toolkit of clinical tools and interventions, research materials, literature reviews, case studies, teaching slide sets, and more.
SHM’s Glycemic Control Mentored Implementation program sites receive 1 year of individualized mentoring including:
• On-site mentoring and training for the entire care team to help members interpret needs and resource assessments, map system processes, and develop site-specific action and intervention plans.
• Monthly coaching calls with the mentor to develop, modify, and implement interventions, establish evaluation processes, and monitor performance over time.
• SHM-facilitated calls with live webinars with other sites in the collaborative to share success stories and experiences.
• Access to the online community to share ideas, documents, and other resources.
• Data collection and analysis tools to generate on-demand reports and benchmark against other program participants.
Learn more about all of SHM’s Glycemic Control offerings by watching the recorded webinar from June 28, 2017, at hospitalmedicine.org/gc.
Earn CME with SHM’s Learning Portal
SHM’s Learning Portal is the online learning destination for hospitalists, featuring all of SHM’s eLearning initiatives in one place. Members can access over 85 CME credits for free in the Learning Portal.
Featured topics currently include perioperative medicine, anticoagulation, quality improvement, cardiac arrhythmia, and antimicrobial stewardship.
Try out the most popular modules:
• The Role of the Medical Consultant.
• Pulmonary Risk Management in the Perioperative Setting.
• Perioperative Medication Management.
• Venous Thromboembolism Prophylaxis in Surgical Patients.
• Perioperative Cardiac Risk Assessment.
Not a member? Join today or pay a small fee per module. Visit shmlearningportal.org to learn more and earn CME credits today.
Brett Radler is communications specialist at the Society of Hospital Medicine.
Updated Clinical Documentation & Coding resources now available
SHM’s Clinical Documentation & Coding for Hospitalists, formerly CODE-H, has been updated for 2017.
“[It’s] an exciting program that offers valuable insight into the coding and billing challenges of hospitalist services. Whether you are a new or seasoned physician, SHM’s Clinical Documentation & Coding for Hospitalists provides you with a solid foundation for documentation, identifies common problems, and offers strategies for success.” – Carol Pohlig, BSN, RN, CPC, ASC Senior Coding and Compliance Specialist
For more information, visit hospitalmedicine.org/codeh.
Registration now open for NP/PA Bootcamp
Whether you’re new to hospital medicine or need a refresher on the latest topics, this course from the AAPA and SHM is perfect for you and offers up to 34.75 AAPA Category 1 CME credits.
At the Adult Hospital Medicine Bootcamp, you will cover commonly encountered diagnoses and diseases of adult hospitalized patients while networking with other hospital-based practitioners. Plus, attend optional pre-courses on reimbursement, hands-on ultrasound or hospital medicine basics.
Join us at the ninth annual Adult Hospital Medicine Boot Camp, September 27 – October 1, 2017, in San Diego. To register and learn more visit: aapa.org/bootcamp.
Learn how your HMG stacks up with the State of Hospital Medicine report
Did you know that hospitalist compensation typically consists of 80% base pay and 20% supplemental income based on production and performance? SHM’s State of Hospital Medicine Report continues to be your best source of information about how hospital medicine groups (HMGs) operate.
Don’t miss the new additions to the report for the 2016 version, including:
• Percentage of the hospital’s total patient volume the HMG was responsible for caring for.
• Presence of medical hospitalists within the HMG focusing their practice in a specific medical subspecialty.
• Value of CME allowances for hospitalists.
• Utilization of prolonged service codes by hospitalists.
• Charge capture methodologies being used by HMGs.
• For academic HMGs, the dollar amount of financial support provided for non-clinical work.
Order your print or digital copy at hospitalmedicine.org/sohm.
Enhance your leadership skills at SHM’s Leadership Academy
SHM’s Leadership Academy is the only leadership program designed specifically for hospitalists. The 2017 meeting will be held October 23 – 26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
Course highlight: Leadership mastering teamwork
Developed in response to high demand from previous Leadership Academy attendees, this course focuses on strengthening teams and institutions. Participants learn how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and develop effective communication strategies.
Upon completion of this course, participants will be able to apply communication strategies that allow others to fully experience their message, lead teams in complex environments to achieve the best results, invest in themselves as leaders to optimize their professional growth and career path, and critically assess program growth opportunities and implement the necessary infrastructure for success.
To view the course schedule, faculty and more visit shmleadershipacademy.org/masteringteamwork.
Improve glycemic control efforts in your hospital with online resources & mentorship
SHM offers a variety of resources to improve glycemic control in your hospital. Glycemic Control Electronic Quality Improvement Programs (eQUIPS) are designed to enhance the efficiency and reliability of your quality improvement efforts to close the gap between best practices and methods for caring for the inpatient with hyperglycemia.
Benefits of SHM’s eQUIPS include:
• Data and performance tracking tools.
• Step-by-step instructions for improving glycemic control, preventing hypoglycemia, and optimizing care of inpatients with hyperglycemia and diabetes.
• An online community and library of tools and documents, including sample order sets and protocols, awareness campaigns, patient educational materials, and supplemental articles.
• Toolkit of clinical tools and interventions, research materials, literature reviews, case studies, teaching slide sets, and more.
SHM’s Glycemic Control Mentored Implementation program sites receive 1 year of individualized mentoring including:
• On-site mentoring and training for the entire care team to help members interpret needs and resource assessments, map system processes, and develop site-specific action and intervention plans.
• Monthly coaching calls with the mentor to develop, modify, and implement interventions, establish evaluation processes, and monitor performance over time.
• SHM-facilitated calls with live webinars with other sites in the collaborative to share success stories and experiences.
• Access to the online community to share ideas, documents, and other resources.
• Data collection and analysis tools to generate on-demand reports and benchmark against other program participants.
Learn more about all of SHM’s Glycemic Control offerings by watching the recorded webinar from June 28, 2017, at hospitalmedicine.org/gc.
Earn CME with SHM’s Learning Portal
SHM’s Learning Portal is the online learning destination for hospitalists, featuring all of SHM’s eLearning initiatives in one place. Members can access over 85 CME credits for free in the Learning Portal.
Featured topics currently include perioperative medicine, anticoagulation, quality improvement, cardiac arrhythmia, and antimicrobial stewardship.
Try out the most popular modules:
• The Role of the Medical Consultant.
• Pulmonary Risk Management in the Perioperative Setting.
• Perioperative Medication Management.
• Venous Thromboembolism Prophylaxis in Surgical Patients.
• Perioperative Cardiac Risk Assessment.
Not a member? Join today or pay a small fee per module. Visit shmlearningportal.org to learn more and earn CME credits today.
Brett Radler is communications specialist at the Society of Hospital Medicine.
Sneak Peek: The Hospital Leader blog - July 2017
“We Are Not Done Changing”
Recently, the online version of JAMA published an original investigation titled, “Patient Mortality During Unannounced Accreditation Surveys at US Hospitals.” The purpose of this investigation was to determine the effect of heightened vigilance during unannounced accreditation surveys on safety and quality of inpatient care.
The authors found that there was a significant reduction in mortality in patients admitted during the week of surveys by The Joint Commission. The change was more significant in major teaching hospitals, where mortality fell from 6.41% to 5.93% during survey weeks, a 5.9% relative decrease. The positive effects of being monitored have been well documented in all kinds of arenas, such as hand washing and antibiotic stewardship. But mortality?
Overall, I feel like I’m a reasonable person, but the clear lack of interest – or willingness to consider that this might not be a good idea on the part of the hospitalist in charge – incited a certain amount of anger and disbelief in me. She also received an antibiotic that she had a documented allergy to – a clear medical error. I instructed my sis-in-law to refuse access to the line; it was removed, and she ultimately recovered to discharge.
This brings me back to the JAMA study. It’s easy to perceive unannounced inspections as merely an inconvenience, where things are locked up that normally aren’t, or where that coveted cup of coffee you normally bring on rounds to get you through your day is summarily yanked out of your hand.
Read the full text of this blog post at hospitalleader.org.
Also on The Hospital Leader…
• How Often Do You Ask This (Ineffective) Question? by Brad Flansbaum, DO, MPH, MHM• Building a Practice that People Want to Be a Part Of by Leslie Flores, MHA• A Need for Medicare Appeals Process Reform in Hospital Observation Care by Anne Sheehy, MD, MS, FHM
“We Are Not Done Changing”
Recently, the online version of JAMA published an original investigation titled, “Patient Mortality During Unannounced Accreditation Surveys at US Hospitals.” The purpose of this investigation was to determine the effect of heightened vigilance during unannounced accreditation surveys on safety and quality of inpatient care.
The authors found that there was a significant reduction in mortality in patients admitted during the week of surveys by The Joint Commission. The change was more significant in major teaching hospitals, where mortality fell from 6.41% to 5.93% during survey weeks, a 5.9% relative decrease. The positive effects of being monitored have been well documented in all kinds of arenas, such as hand washing and antibiotic stewardship. But mortality?
Overall, I feel like I’m a reasonable person, but the clear lack of interest – or willingness to consider that this might not be a good idea on the part of the hospitalist in charge – incited a certain amount of anger and disbelief in me. She also received an antibiotic that she had a documented allergy to – a clear medical error. I instructed my sis-in-law to refuse access to the line; it was removed, and she ultimately recovered to discharge.
This brings me back to the JAMA study. It’s easy to perceive unannounced inspections as merely an inconvenience, where things are locked up that normally aren’t, or where that coveted cup of coffee you normally bring on rounds to get you through your day is summarily yanked out of your hand.
Read the full text of this blog post at hospitalleader.org.
Also on The Hospital Leader…
• How Often Do You Ask This (Ineffective) Question? by Brad Flansbaum, DO, MPH, MHM• Building a Practice that People Want to Be a Part Of by Leslie Flores, MHA• A Need for Medicare Appeals Process Reform in Hospital Observation Care by Anne Sheehy, MD, MS, FHM
“We Are Not Done Changing”
Recently, the online version of JAMA published an original investigation titled, “Patient Mortality During Unannounced Accreditation Surveys at US Hospitals.” The purpose of this investigation was to determine the effect of heightened vigilance during unannounced accreditation surveys on safety and quality of inpatient care.
The authors found that there was a significant reduction in mortality in patients admitted during the week of surveys by The Joint Commission. The change was more significant in major teaching hospitals, where mortality fell from 6.41% to 5.93% during survey weeks, a 5.9% relative decrease. The positive effects of being monitored have been well documented in all kinds of arenas, such as hand washing and antibiotic stewardship. But mortality?
Overall, I feel like I’m a reasonable person, but the clear lack of interest – or willingness to consider that this might not be a good idea on the part of the hospitalist in charge – incited a certain amount of anger and disbelief in me. She also received an antibiotic that she had a documented allergy to – a clear medical error. I instructed my sis-in-law to refuse access to the line; it was removed, and she ultimately recovered to discharge.
This brings me back to the JAMA study. It’s easy to perceive unannounced inspections as merely an inconvenience, where things are locked up that normally aren’t, or where that coveted cup of coffee you normally bring on rounds to get you through your day is summarily yanked out of your hand.
Read the full text of this blog post at hospitalleader.org.
Also on The Hospital Leader…
• How Often Do You Ask This (Ineffective) Question? by Brad Flansbaum, DO, MPH, MHM• Building a Practice that People Want to Be a Part Of by Leslie Flores, MHA• A Need for Medicare Appeals Process Reform in Hospital Observation Care by Anne Sheehy, MD, MS, FHM
Everything We Say and Do: Take time to leave a good impression
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
Meet the two newest SHM board members
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.




















