User login
Saturday - On Tap
It’s the final day of the Vascular Annual Meeting – and there is plenty on the agenda to keep you busy.
6:30 to 8:00 a.m. – Three Breakfast Sessions: “Beyond the Basics of Hemodialysis Access,” “The Treatment of Chronic Venous Leg Ulcers,” and “How to Write a Paper and Have it Accepted in the JVS or EJVES.”
8:00 to 10:00 a.m. – Plenary 7 and Plenary 8. With so many high-quality abstracts submitted, two plenary sessions are set for Saturday; Plenary 8 includes late-breaking abstracts and the Vascular Quality Initiative. SDCC, Room 6 A/B
9:00 a.m. to 1:00 p.m. – It’s your last chance to visit the Exhibit Hall to see what’s new and improved. Exhibit Hall B.
10:30 a.m. to 12:00 p.m. – Four concurrent sessions, on the modern VA vascular practice and three joint sessions with an alphabet soup of allied societies, on medical management of vascular disease (SVM), collaboration of vascular surgeons and nurses (SVN), and building and managing a vascular laboratory (SVU).
10:30 a.m. to 12:00 p.m. – Top 10 papers relevant to vascular surgery that were NOT published in the Journal of Vascular Surgery. SDCC, Room 6 A/B.
12:00 p.m. – SVS members, see the passing of the gavel and other business issues, as well as award presentations. SDCC, Room 6 D/E.
1:30 to 3:30 p.m. – Sometimes seeing makes more of an impact than listening. The “How I do it” Video Session will feature 11 video abstracts on a variety of topics. SDCC, Room 6C.
1:30 to 5:00 p.m. – RPVI exam preparation, in collaboration with the Society for Vascular Ultrasound. SDCC, Room 4.
1:30 to 5:15 p.m. – Aortic Summit, with the Society of Thoracic Surgeons. SDCC, Room 3.
3:30 to 4:30 p.m. – Poster Runoff: Championship Round. From 120 posters to just 10, with three winners selected by the audience. SDCC, Room 6C.
It’s the final day of the Vascular Annual Meeting – and there is plenty on the agenda to keep you busy.
6:30 to 8:00 a.m. – Three Breakfast Sessions: “Beyond the Basics of Hemodialysis Access,” “The Treatment of Chronic Venous Leg Ulcers,” and “How to Write a Paper and Have it Accepted in the JVS or EJVES.”
8:00 to 10:00 a.m. – Plenary 7 and Plenary 8. With so many high-quality abstracts submitted, two plenary sessions are set for Saturday; Plenary 8 includes late-breaking abstracts and the Vascular Quality Initiative. SDCC, Room 6 A/B
9:00 a.m. to 1:00 p.m. – It’s your last chance to visit the Exhibit Hall to see what’s new and improved. Exhibit Hall B.
10:30 a.m. to 12:00 p.m. – Four concurrent sessions, on the modern VA vascular practice and three joint sessions with an alphabet soup of allied societies, on medical management of vascular disease (SVM), collaboration of vascular surgeons and nurses (SVN), and building and managing a vascular laboratory (SVU).
10:30 a.m. to 12:00 p.m. – Top 10 papers relevant to vascular surgery that were NOT published in the Journal of Vascular Surgery. SDCC, Room 6 A/B.
12:00 p.m. – SVS members, see the passing of the gavel and other business issues, as well as award presentations. SDCC, Room 6 D/E.
1:30 to 3:30 p.m. – Sometimes seeing makes more of an impact than listening. The “How I do it” Video Session will feature 11 video abstracts on a variety of topics. SDCC, Room 6C.
1:30 to 5:00 p.m. – RPVI exam preparation, in collaboration with the Society for Vascular Ultrasound. SDCC, Room 4.
1:30 to 5:15 p.m. – Aortic Summit, with the Society of Thoracic Surgeons. SDCC, Room 3.
3:30 to 4:30 p.m. – Poster Runoff: Championship Round. From 120 posters to just 10, with three winners selected by the audience. SDCC, Room 6C.
It’s the final day of the Vascular Annual Meeting – and there is plenty on the agenda to keep you busy.
6:30 to 8:00 a.m. – Three Breakfast Sessions: “Beyond the Basics of Hemodialysis Access,” “The Treatment of Chronic Venous Leg Ulcers,” and “How to Write a Paper and Have it Accepted in the JVS or EJVES.”
8:00 to 10:00 a.m. – Plenary 7 and Plenary 8. With so many high-quality abstracts submitted, two plenary sessions are set for Saturday; Plenary 8 includes late-breaking abstracts and the Vascular Quality Initiative. SDCC, Room 6 A/B
9:00 a.m. to 1:00 p.m. – It’s your last chance to visit the Exhibit Hall to see what’s new and improved. Exhibit Hall B.
10:30 a.m. to 12:00 p.m. – Four concurrent sessions, on the modern VA vascular practice and three joint sessions with an alphabet soup of allied societies, on medical management of vascular disease (SVM), collaboration of vascular surgeons and nurses (SVN), and building and managing a vascular laboratory (SVU).
10:30 a.m. to 12:00 p.m. – Top 10 papers relevant to vascular surgery that were NOT published in the Journal of Vascular Surgery. SDCC, Room 6 A/B.
12:00 p.m. – SVS members, see the passing of the gavel and other business issues, as well as award presentations. SDCC, Room 6 D/E.
1:30 to 3:30 p.m. – Sometimes seeing makes more of an impact than listening. The “How I do it” Video Session will feature 11 video abstracts on a variety of topics. SDCC, Room 6C.
1:30 to 5:00 p.m. – RPVI exam preparation, in collaboration with the Society for Vascular Ultrasound. SDCC, Room 4.
1:30 to 5:15 p.m. – Aortic Summit, with the Society of Thoracic Surgeons. SDCC, Room 3.
3:30 to 4:30 p.m. – Poster Runoff: Championship Round. From 120 posters to just 10, with three winners selected by the audience. SDCC, Room 6C.
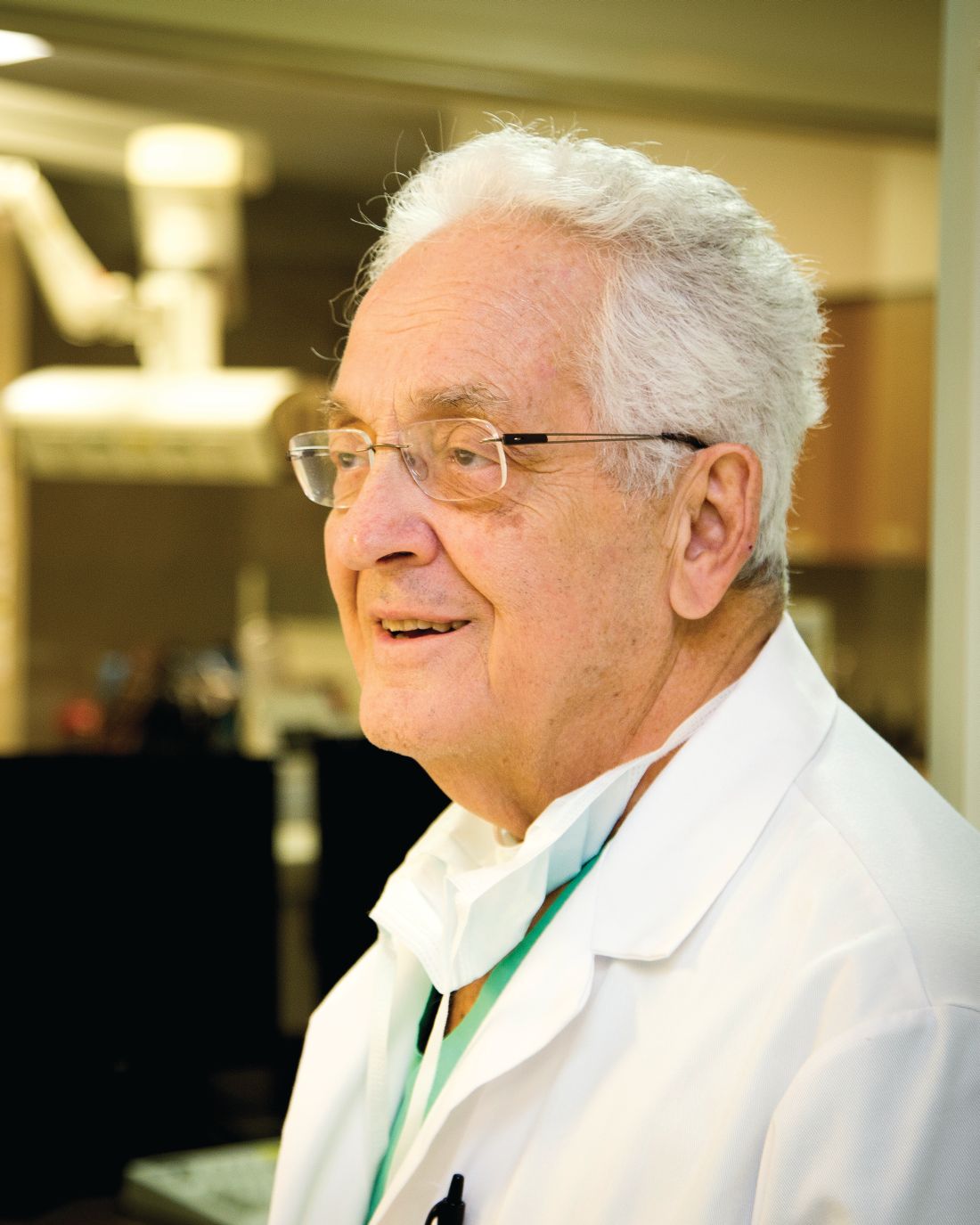
For Dr. Dardik the First, a First-Rate Award
In the early 1950s, an aspiring teen pianist named Herbert Dardik got his big break – a chance to play on the “Ted Mack Amateur Hour.”
Sadly, he didn’t win. He was down but not out until the family’s piano teacher finally told him, “Your brother Irving has talent. You are a hard worker.” That was the last straw.
Happily for vascular surgery, he gave up on a musical career and ended up becoming a surgeon.
But over time, vascular surgery benefited from an explosion of innovation and research. “Today,” Dr. Dardik said, “it’s a different world.”
He built his career and reputation over many years at Englewood Hospital and Medical Center in New Jersey, where he still, at age 82, holds regular office hours, runs student and resident programs, and works in his research lab.
Dr. Dardik has been honored at this year’s Vascular Annual Meeting with the Society’s highest honor, the Lifetime Achievement Award.
According to nominator Richard Lynn, MD, Dr. Dardik is the “first true private practice/community practice individual to win this award. Dr. Dardik is the quintessential complete physician, surgeon, teacher, researcher, clinician, community practitioner/academician, father, husband, brother, and respected colleague.”
The SVS Fellows Council selects the Lifetime Achievement recipient to recognize that member’s outstanding and sustained contributions both to the profession and to the SVS, as well as exemplary professional practice and leadership.
Dr. Dardik is known for his clinical research and his pioneering contributions in lower extremity bypass surgery. His innovative work on the umbilical vein graft, the first bioengineered biologic graft, earned him the Hektoen Gold Medal from the American Medical Association. This work led to his development of the distal arterio-venous fistula as an adjunct to small-vessel bypass in order to enhance patency.
Currently, he is exploring the use of the umbilical cord artery as an aortic interposition graft in the rat. This murine model is also used to enhance resident skills for extremely challenging surgeries. The laboratory also serves as a training site for high school and college students interested in science and medicine. Since 1996, more than 300 high school juniors and seniors have come under the influence of Dr. Dardik.
He is a director and founding member of the Bloodless Program at Englewood and also established one of the earliest wound care centers and approved vascular laboratories. He was an early advocate of completion angiography, completion sonography, and avoidance of radiation in the operating room and has designed and developed vascular tools including clamps, tunnelers, and retractors.
Further contributions include his work on the nationalization of the Society for Clinical Vascular Surgery and as a founding member of the Eastern Vascular Society and the Vascular Society of New Jersey. He served all three as president.
He has given nearly 450 invited lectures and chaired an annual Vascular Symposium for 15 years. His numerous publications have enabled him to mentor his students in writing in addition to how to read the enormous body of literature.
His pioneering work in crural revascularization was recognized in the book Band of Brothers, Creators of Modern Vascular Surgery.
Just last year he was awarded the Julius Jacobson Teaching Award at Mt. Sinai Medical Center in New York City as an outstanding mentor. Over the past four decades he trained more than 40 vascular trainees in his vascular fellowship program. To this day, he retains the title of Chief Emeritus of Vascular and General Surgery at Englewood Hospital Medical Center as well as the title of Professor of Surgery.
He has also seen his love of medicine passed on to each of his three children: Alan, a vascular surgeon (and SVS member), Michael, a pathologist, and Sharon, a pediatrician.
If asked about his retirement plans, he’ll demur.
“What’s that word? I’ve never heard that word! It’s so much fun I cannot possibly leave,” he said. “I look forward to coming in, but now I don’t have to put on the alarm clock for 5 a.m. and that has been terrific.”
He maintains there is one other reason he stays on at Englewood. “I have the best office. I can’t give it up!”
In the early 1950s, an aspiring teen pianist named Herbert Dardik got his big break – a chance to play on the “Ted Mack Amateur Hour.”
Sadly, he didn’t win. He was down but not out until the family’s piano teacher finally told him, “Your brother Irving has talent. You are a hard worker.” That was the last straw.
Happily for vascular surgery, he gave up on a musical career and ended up becoming a surgeon.
But over time, vascular surgery benefited from an explosion of innovation and research. “Today,” Dr. Dardik said, “it’s a different world.”
He built his career and reputation over many years at Englewood Hospital and Medical Center in New Jersey, where he still, at age 82, holds regular office hours, runs student and resident programs, and works in his research lab.
Dr. Dardik has been honored at this year’s Vascular Annual Meeting with the Society’s highest honor, the Lifetime Achievement Award.
According to nominator Richard Lynn, MD, Dr. Dardik is the “first true private practice/community practice individual to win this award. Dr. Dardik is the quintessential complete physician, surgeon, teacher, researcher, clinician, community practitioner/academician, father, husband, brother, and respected colleague.”
The SVS Fellows Council selects the Lifetime Achievement recipient to recognize that member’s outstanding and sustained contributions both to the profession and to the SVS, as well as exemplary professional practice and leadership.
Dr. Dardik is known for his clinical research and his pioneering contributions in lower extremity bypass surgery. His innovative work on the umbilical vein graft, the first bioengineered biologic graft, earned him the Hektoen Gold Medal from the American Medical Association. This work led to his development of the distal arterio-venous fistula as an adjunct to small-vessel bypass in order to enhance patency.
Currently, he is exploring the use of the umbilical cord artery as an aortic interposition graft in the rat. This murine model is also used to enhance resident skills for extremely challenging surgeries. The laboratory also serves as a training site for high school and college students interested in science and medicine. Since 1996, more than 300 high school juniors and seniors have come under the influence of Dr. Dardik.
He is a director and founding member of the Bloodless Program at Englewood and also established one of the earliest wound care centers and approved vascular laboratories. He was an early advocate of completion angiography, completion sonography, and avoidance of radiation in the operating room and has designed and developed vascular tools including clamps, tunnelers, and retractors.
Further contributions include his work on the nationalization of the Society for Clinical Vascular Surgery and as a founding member of the Eastern Vascular Society and the Vascular Society of New Jersey. He served all three as president.
He has given nearly 450 invited lectures and chaired an annual Vascular Symposium for 15 years. His numerous publications have enabled him to mentor his students in writing in addition to how to read the enormous body of literature.
His pioneering work in crural revascularization was recognized in the book Band of Brothers, Creators of Modern Vascular Surgery.
Just last year he was awarded the Julius Jacobson Teaching Award at Mt. Sinai Medical Center in New York City as an outstanding mentor. Over the past four decades he trained more than 40 vascular trainees in his vascular fellowship program. To this day, he retains the title of Chief Emeritus of Vascular and General Surgery at Englewood Hospital Medical Center as well as the title of Professor of Surgery.
He has also seen his love of medicine passed on to each of his three children: Alan, a vascular surgeon (and SVS member), Michael, a pathologist, and Sharon, a pediatrician.
If asked about his retirement plans, he’ll demur.
“What’s that word? I’ve never heard that word! It’s so much fun I cannot possibly leave,” he said. “I look forward to coming in, but now I don’t have to put on the alarm clock for 5 a.m. and that has been terrific.”
He maintains there is one other reason he stays on at Englewood. “I have the best office. I can’t give it up!”
In the early 1950s, an aspiring teen pianist named Herbert Dardik got his big break – a chance to play on the “Ted Mack Amateur Hour.”
Sadly, he didn’t win. He was down but not out until the family’s piano teacher finally told him, “Your brother Irving has talent. You are a hard worker.” That was the last straw.
Happily for vascular surgery, he gave up on a musical career and ended up becoming a surgeon.
But over time, vascular surgery benefited from an explosion of innovation and research. “Today,” Dr. Dardik said, “it’s a different world.”
He built his career and reputation over many years at Englewood Hospital and Medical Center in New Jersey, where he still, at age 82, holds regular office hours, runs student and resident programs, and works in his research lab.
Dr. Dardik has been honored at this year’s Vascular Annual Meeting with the Society’s highest honor, the Lifetime Achievement Award.
According to nominator Richard Lynn, MD, Dr. Dardik is the “first true private practice/community practice individual to win this award. Dr. Dardik is the quintessential complete physician, surgeon, teacher, researcher, clinician, community practitioner/academician, father, husband, brother, and respected colleague.”
The SVS Fellows Council selects the Lifetime Achievement recipient to recognize that member’s outstanding and sustained contributions both to the profession and to the SVS, as well as exemplary professional practice and leadership.
Dr. Dardik is known for his clinical research and his pioneering contributions in lower extremity bypass surgery. His innovative work on the umbilical vein graft, the first bioengineered biologic graft, earned him the Hektoen Gold Medal from the American Medical Association. This work led to his development of the distal arterio-venous fistula as an adjunct to small-vessel bypass in order to enhance patency.
Currently, he is exploring the use of the umbilical cord artery as an aortic interposition graft in the rat. This murine model is also used to enhance resident skills for extremely challenging surgeries. The laboratory also serves as a training site for high school and college students interested in science and medicine. Since 1996, more than 300 high school juniors and seniors have come under the influence of Dr. Dardik.
He is a director and founding member of the Bloodless Program at Englewood and also established one of the earliest wound care centers and approved vascular laboratories. He was an early advocate of completion angiography, completion sonography, and avoidance of radiation in the operating room and has designed and developed vascular tools including clamps, tunnelers, and retractors.
Further contributions include his work on the nationalization of the Society for Clinical Vascular Surgery and as a founding member of the Eastern Vascular Society and the Vascular Society of New Jersey. He served all three as president.
He has given nearly 450 invited lectures and chaired an annual Vascular Symposium for 15 years. His numerous publications have enabled him to mentor his students in writing in addition to how to read the enormous body of literature.
His pioneering work in crural revascularization was recognized in the book Band of Brothers, Creators of Modern Vascular Surgery.
Just last year he was awarded the Julius Jacobson Teaching Award at Mt. Sinai Medical Center in New York City as an outstanding mentor. Over the past four decades he trained more than 40 vascular trainees in his vascular fellowship program. To this day, he retains the title of Chief Emeritus of Vascular and General Surgery at Englewood Hospital Medical Center as well as the title of Professor of Surgery.
He has also seen his love of medicine passed on to each of his three children: Alan, a vascular surgeon (and SVS member), Michael, a pathologist, and Sharon, a pediatrician.
If asked about his retirement plans, he’ll demur.
“What’s that word? I’ve never heard that word! It’s so much fun I cannot possibly leave,” he said. “I look forward to coming in, but now I don’t have to put on the alarm clock for 5 a.m. and that has been terrific.”
He maintains there is one other reason he stays on at Englewood. “I have the best office. I can’t give it up!”
Highlights from new guidelines, and a chance to weigh in
Though the Society for Vascular Surgery has long published clinical practice guidelines, its 2017 annual meeting marks the first seminar dedicated to guidelines in progress, allowing for more interaction, debate, and feedback across the vascular community before these guidelines become final.
At Friday afternoon’s update on SVS clinical practice guidelines, speakers will present on four that are in advanced development, including new global vascular guidelines.
All too often, Dr. Forbes said, the guideline process can seem opaque, or top-town or cumbersome in soliciting and incorporating feedback – problems that this kind of interactive seminar can help rectify. “We don’t want to be Moses with the tablet from the mountain, handing them down and asking everybody to follow them without question,” he said.
Keith D. Calligaro, MD, who practices in Philadelphia, starts the seminar off with highlights from new guidelines on hospital privileges across practice settings, an update of SVS guidelines from 2008. The new guidelines “describe specific procedure-related training requirements that would then lead to privileges in a hospital setting. This is especially relevant in some of the practice environments in the U.S.,” Dr. Forbes said.
R. Eugene Zierler, MD, of the University of Washington in Seattle, will present broad-reaching new advice on the follow-up of patients after vascular procedures. These guidelines cover patients who’ve undergone a wide variety of procedures, “all the way from carotid to abdominal aortic aneurysm repairs to venous surgery – and offers specific, evidence-based recommendations for how patients should be followed up, how often they should undergo imaging, bloodwork, and other follow-up modalities,” Dr. Forbes said.
And Elliot Chaikof, MD, of Beth Israel Deaconess Medical Center in Boston, will discuss new guidelines on the care of patients with abdominal aortic aneurysms that incorporates “what we know today about the different therapeutic options: from medical management to endovascular and open repair to different treatment strategies for men and women – all this based on advances from the last couple years,” Dr. Forbes said.
Finally, in separate talks, two presenters will describe different elements of a new global vascular guideline developed jointly by the SVS, the European Society for Vascular Surgery, and the World Federation of Vascular Societies.
Andrew W. Bradbury, MD, of the University of Birmingham in the U.K. and Michael S. Conte of the University of California San Francisco will speak on some issues the guidelines are tackling, all with an aim to reflect a more inclusive, worldwide picture of vascular practice.
“This is the first time we’re going to hear what these recommendations are,” Dr. Forbes said. One highlight is likely to be a new global classification system for peripheral arterial disease. “This is a new and novel concept in vascular disease, and that is similar to the classification systems used for cancer,” Dr. Forbes said.
Dr. Forbes said that he hopes that a seminar focused on guidelines in progress will become a regular feature of the annual meeting, and that this year’s seminar will help shape the society’s approach to future guidelines as well.
“Members may know of areas of vascular surgery where there’s a real need for guidelines, or some evidence-based recommendations that we don’t have, and we’d love them to come forward and propose those topics,” he said. “We need practitioners in academic centers and community practitioners alike, to represent the breath of the work being done out there.”
Friday, June 2
3:30 p.m. - 5:00 p.m., SDCC, Room 4
C9: Update on Society for Vascular Surgery Clinical Practice Guidelines
Though the Society for Vascular Surgery has long published clinical practice guidelines, its 2017 annual meeting marks the first seminar dedicated to guidelines in progress, allowing for more interaction, debate, and feedback across the vascular community before these guidelines become final.
At Friday afternoon’s update on SVS clinical practice guidelines, speakers will present on four that are in advanced development, including new global vascular guidelines.
All too often, Dr. Forbes said, the guideline process can seem opaque, or top-town or cumbersome in soliciting and incorporating feedback – problems that this kind of interactive seminar can help rectify. “We don’t want to be Moses with the tablet from the mountain, handing them down and asking everybody to follow them without question,” he said.
Keith D. Calligaro, MD, who practices in Philadelphia, starts the seminar off with highlights from new guidelines on hospital privileges across practice settings, an update of SVS guidelines from 2008. The new guidelines “describe specific procedure-related training requirements that would then lead to privileges in a hospital setting. This is especially relevant in some of the practice environments in the U.S.,” Dr. Forbes said.
R. Eugene Zierler, MD, of the University of Washington in Seattle, will present broad-reaching new advice on the follow-up of patients after vascular procedures. These guidelines cover patients who’ve undergone a wide variety of procedures, “all the way from carotid to abdominal aortic aneurysm repairs to venous surgery – and offers specific, evidence-based recommendations for how patients should be followed up, how often they should undergo imaging, bloodwork, and other follow-up modalities,” Dr. Forbes said.
And Elliot Chaikof, MD, of Beth Israel Deaconess Medical Center in Boston, will discuss new guidelines on the care of patients with abdominal aortic aneurysms that incorporates “what we know today about the different therapeutic options: from medical management to endovascular and open repair to different treatment strategies for men and women – all this based on advances from the last couple years,” Dr. Forbes said.
Finally, in separate talks, two presenters will describe different elements of a new global vascular guideline developed jointly by the SVS, the European Society for Vascular Surgery, and the World Federation of Vascular Societies.
Andrew W. Bradbury, MD, of the University of Birmingham in the U.K. and Michael S. Conte of the University of California San Francisco will speak on some issues the guidelines are tackling, all with an aim to reflect a more inclusive, worldwide picture of vascular practice.
“This is the first time we’re going to hear what these recommendations are,” Dr. Forbes said. One highlight is likely to be a new global classification system for peripheral arterial disease. “This is a new and novel concept in vascular disease, and that is similar to the classification systems used for cancer,” Dr. Forbes said.
Dr. Forbes said that he hopes that a seminar focused on guidelines in progress will become a regular feature of the annual meeting, and that this year’s seminar will help shape the society’s approach to future guidelines as well.
“Members may know of areas of vascular surgery where there’s a real need for guidelines, or some evidence-based recommendations that we don’t have, and we’d love them to come forward and propose those topics,” he said. “We need practitioners in academic centers and community practitioners alike, to represent the breath of the work being done out there.”
Friday, June 2
3:30 p.m. - 5:00 p.m., SDCC, Room 4
C9: Update on Society for Vascular Surgery Clinical Practice Guidelines
Though the Society for Vascular Surgery has long published clinical practice guidelines, its 2017 annual meeting marks the first seminar dedicated to guidelines in progress, allowing for more interaction, debate, and feedback across the vascular community before these guidelines become final.
At Friday afternoon’s update on SVS clinical practice guidelines, speakers will present on four that are in advanced development, including new global vascular guidelines.
All too often, Dr. Forbes said, the guideline process can seem opaque, or top-town or cumbersome in soliciting and incorporating feedback – problems that this kind of interactive seminar can help rectify. “We don’t want to be Moses with the tablet from the mountain, handing them down and asking everybody to follow them without question,” he said.
Keith D. Calligaro, MD, who practices in Philadelphia, starts the seminar off with highlights from new guidelines on hospital privileges across practice settings, an update of SVS guidelines from 2008. The new guidelines “describe specific procedure-related training requirements that would then lead to privileges in a hospital setting. This is especially relevant in some of the practice environments in the U.S.,” Dr. Forbes said.
R. Eugene Zierler, MD, of the University of Washington in Seattle, will present broad-reaching new advice on the follow-up of patients after vascular procedures. These guidelines cover patients who’ve undergone a wide variety of procedures, “all the way from carotid to abdominal aortic aneurysm repairs to venous surgery – and offers specific, evidence-based recommendations for how patients should be followed up, how often they should undergo imaging, bloodwork, and other follow-up modalities,” Dr. Forbes said.
And Elliot Chaikof, MD, of Beth Israel Deaconess Medical Center in Boston, will discuss new guidelines on the care of patients with abdominal aortic aneurysms that incorporates “what we know today about the different therapeutic options: from medical management to endovascular and open repair to different treatment strategies for men and women – all this based on advances from the last couple years,” Dr. Forbes said.
Finally, in separate talks, two presenters will describe different elements of a new global vascular guideline developed jointly by the SVS, the European Society for Vascular Surgery, and the World Federation of Vascular Societies.
Andrew W. Bradbury, MD, of the University of Birmingham in the U.K. and Michael S. Conte of the University of California San Francisco will speak on some issues the guidelines are tackling, all with an aim to reflect a more inclusive, worldwide picture of vascular practice.
“This is the first time we’re going to hear what these recommendations are,” Dr. Forbes said. One highlight is likely to be a new global classification system for peripheral arterial disease. “This is a new and novel concept in vascular disease, and that is similar to the classification systems used for cancer,” Dr. Forbes said.
Dr. Forbes said that he hopes that a seminar focused on guidelines in progress will become a regular feature of the annual meeting, and that this year’s seminar will help shape the society’s approach to future guidelines as well.
“Members may know of areas of vascular surgery where there’s a real need for guidelines, or some evidence-based recommendations that we don’t have, and we’d love them to come forward and propose those topics,” he said. “We need practitioners in academic centers and community practitioners alike, to represent the breath of the work being done out there.”
Friday, June 2
3:30 p.m. - 5:00 p.m., SDCC, Room 4
C9: Update on Society for Vascular Surgery Clinical Practice Guidelines
How to get published in JVS and EJVES: Editors disclose secrets of success
Over the past year, the Journal of Vascular Surgery and its two affiliated journals have undergone a number of important changes.
Editorial boards have been revamped, disadvantageous limits on the number of contributing authors and on references have been scrapped, and editors’ videos accompany every new issue. New short abstracts, take-home messages, and extended tables of contents allow even the most time-crunched clinicians to get up to speed.
Even the look of the journals has changed – with a red color scheme for JVS, a blue one for JVS-VL, the venous and lymphatic disorders journal, and a mixed red and blue one for the open-access publication dedicated to cases and techniques.
On Saturday morning, Dr. Gloviczki, the editor in chief of JVS, and senior editor Peter F. Lawrence helm a seminar that describes not only what they’ve been doing since taking over the journals’ leadership in July 2016, but how more SVS members can take part by producing quality papers or reviewing for the journals.
Dr. Gloviczki and Dr. Lawrence have also invited Dr. Philip Kolh if the University of Liege in Liege, Belgium, to co-lead the seminar. Dr. Kolh, who is editor in chief of the European Journal of Vascular and Endovascular Surgery, will advise on what the EJVES is looking for in its reviews and submissions.
“We believe it is important for JVS and EJVES to work together, to develop joint guidelines, to avoid repetition and redundancy, and double-publish papers that are important for both readerships,” Dr. Gloviczki said.
Dr. Gloviczki will start the seminar off by discussing the sweeping changes aimed at raising the quality of all three JVS journals and, he hopes, will also affect their impact factor, currently at 3.45 for JVS.
In addition to increasing the scrutiny of the peer review and the number of statistical reviews performed by master statisticians, the editors are looking for systematic reviews, meta-analyses, practice guidelines, and reporting standards – and will publish paper types not previously accepted, such as study protocols.
The journal will retain many initiatives of the previous editors, including the international debates, and will continue recruiting international authors and reviewers. Having the best reviewers, Dr. Gloviczki noted, “is an important parallel to having top-quality studies.”
Dr. Lawrence, of the University of California Los Angeles, will discuss what makes a clinical research paper successful. “We want papers that are highly cited – and the highly cited papers are prospective studies, whether randomized controlled trials or single-arm cohort studies,” Dr. Gloviczki said. “We also favor large retrospective reviews of prospectively collected national or international registries.”
Peter Henke, MD, of the University of Michigan in Ann Arbor, Mich., will talk about what the JVS editors and reviewers want in basic science papers – which Dr. Gloviczki called an important and sometimes overlooked counterpart to the clinical studies. “We believe that our profession must be in charge of basic research, that whoever owns basic research in our field owns the disease,” he said.
“To understand vascular disease you have to start at the basics of anatomy, pathophysiology, etiology, prevention, presentation and finally treatment,” he said, noting that vascular surgeons at many academic centers are conducting experimental studies and other basic research, efforts often supported by SVS grants.
Last year the JVS editors re-named the journal’s basic science section and called it “From Bench to Bedside” to try and capture the importance of preclinical vascular studies. “It’s a relatively small section of our journal but it’s important,” Dr. Gloviczki said. “And now we are really pushing to get commentaries that emphasize the potential clinical application of the basic science research.”
Richard L. Amdur, MD, of George Washington University in Washington, DC, will talk about what the JVS journal editors want to see in terms of statistics, while Marc L. Schermerhorn, MD, of Beth Israel Deaconess Medical Center in Boston and Martin Bjorck, MD, PhD, of Uppsala University, Uppsala, Sweden, will both discuss mining the large vascular registries from the United States and Europe for studies attractive to JVS or EJVES.
“There are so many papers where real-world experience is given to us by analyzing these registries,” Dr. Gloviczki said. Studies from the SVS Vascular Quality Initiatives database, the American College of Surgeons’ National Surgical Quality Improvement Program, the National Inpatient Sample, the Swedish Vascular registry, VADUNET and the International Consortium of Vascular Registries, “have changed the way we practice vascular surgery, and we publish multiple papers from these in every issue.”
Saturday, June 3
6:30 a.m. - 8:00 a.m.
Breakfast Session B9: How to Write a Paper and Have it Accepted in the JVS or EJVES
Over the past year, the Journal of Vascular Surgery and its two affiliated journals have undergone a number of important changes.
Editorial boards have been revamped, disadvantageous limits on the number of contributing authors and on references have been scrapped, and editors’ videos accompany every new issue. New short abstracts, take-home messages, and extended tables of contents allow even the most time-crunched clinicians to get up to speed.
Even the look of the journals has changed – with a red color scheme for JVS, a blue one for JVS-VL, the venous and lymphatic disorders journal, and a mixed red and blue one for the open-access publication dedicated to cases and techniques.
On Saturday morning, Dr. Gloviczki, the editor in chief of JVS, and senior editor Peter F. Lawrence helm a seminar that describes not only what they’ve been doing since taking over the journals’ leadership in July 2016, but how more SVS members can take part by producing quality papers or reviewing for the journals.
Dr. Gloviczki and Dr. Lawrence have also invited Dr. Philip Kolh if the University of Liege in Liege, Belgium, to co-lead the seminar. Dr. Kolh, who is editor in chief of the European Journal of Vascular and Endovascular Surgery, will advise on what the EJVES is looking for in its reviews and submissions.
“We believe it is important for JVS and EJVES to work together, to develop joint guidelines, to avoid repetition and redundancy, and double-publish papers that are important for both readerships,” Dr. Gloviczki said.
Dr. Gloviczki will start the seminar off by discussing the sweeping changes aimed at raising the quality of all three JVS journals and, he hopes, will also affect their impact factor, currently at 3.45 for JVS.
In addition to increasing the scrutiny of the peer review and the number of statistical reviews performed by master statisticians, the editors are looking for systematic reviews, meta-analyses, practice guidelines, and reporting standards – and will publish paper types not previously accepted, such as study protocols.
The journal will retain many initiatives of the previous editors, including the international debates, and will continue recruiting international authors and reviewers. Having the best reviewers, Dr. Gloviczki noted, “is an important parallel to having top-quality studies.”
Dr. Lawrence, of the University of California Los Angeles, will discuss what makes a clinical research paper successful. “We want papers that are highly cited – and the highly cited papers are prospective studies, whether randomized controlled trials or single-arm cohort studies,” Dr. Gloviczki said. “We also favor large retrospective reviews of prospectively collected national or international registries.”
Peter Henke, MD, of the University of Michigan in Ann Arbor, Mich., will talk about what the JVS editors and reviewers want in basic science papers – which Dr. Gloviczki called an important and sometimes overlooked counterpart to the clinical studies. “We believe that our profession must be in charge of basic research, that whoever owns basic research in our field owns the disease,” he said.
“To understand vascular disease you have to start at the basics of anatomy, pathophysiology, etiology, prevention, presentation and finally treatment,” he said, noting that vascular surgeons at many academic centers are conducting experimental studies and other basic research, efforts often supported by SVS grants.
Last year the JVS editors re-named the journal’s basic science section and called it “From Bench to Bedside” to try and capture the importance of preclinical vascular studies. “It’s a relatively small section of our journal but it’s important,” Dr. Gloviczki said. “And now we are really pushing to get commentaries that emphasize the potential clinical application of the basic science research.”
Richard L. Amdur, MD, of George Washington University in Washington, DC, will talk about what the JVS journal editors want to see in terms of statistics, while Marc L. Schermerhorn, MD, of Beth Israel Deaconess Medical Center in Boston and Martin Bjorck, MD, PhD, of Uppsala University, Uppsala, Sweden, will both discuss mining the large vascular registries from the United States and Europe for studies attractive to JVS or EJVES.
“There are so many papers where real-world experience is given to us by analyzing these registries,” Dr. Gloviczki said. Studies from the SVS Vascular Quality Initiatives database, the American College of Surgeons’ National Surgical Quality Improvement Program, the National Inpatient Sample, the Swedish Vascular registry, VADUNET and the International Consortium of Vascular Registries, “have changed the way we practice vascular surgery, and we publish multiple papers from these in every issue.”
Saturday, June 3
6:30 a.m. - 8:00 a.m.
Breakfast Session B9: How to Write a Paper and Have it Accepted in the JVS or EJVES
Over the past year, the Journal of Vascular Surgery and its two affiliated journals have undergone a number of important changes.
Editorial boards have been revamped, disadvantageous limits on the number of contributing authors and on references have been scrapped, and editors’ videos accompany every new issue. New short abstracts, take-home messages, and extended tables of contents allow even the most time-crunched clinicians to get up to speed.
Even the look of the journals has changed – with a red color scheme for JVS, a blue one for JVS-VL, the venous and lymphatic disorders journal, and a mixed red and blue one for the open-access publication dedicated to cases and techniques.
On Saturday morning, Dr. Gloviczki, the editor in chief of JVS, and senior editor Peter F. Lawrence helm a seminar that describes not only what they’ve been doing since taking over the journals’ leadership in July 2016, but how more SVS members can take part by producing quality papers or reviewing for the journals.
Dr. Gloviczki and Dr. Lawrence have also invited Dr. Philip Kolh if the University of Liege in Liege, Belgium, to co-lead the seminar. Dr. Kolh, who is editor in chief of the European Journal of Vascular and Endovascular Surgery, will advise on what the EJVES is looking for in its reviews and submissions.
“We believe it is important for JVS and EJVES to work together, to develop joint guidelines, to avoid repetition and redundancy, and double-publish papers that are important for both readerships,” Dr. Gloviczki said.
Dr. Gloviczki will start the seminar off by discussing the sweeping changes aimed at raising the quality of all three JVS journals and, he hopes, will also affect their impact factor, currently at 3.45 for JVS.
In addition to increasing the scrutiny of the peer review and the number of statistical reviews performed by master statisticians, the editors are looking for systematic reviews, meta-analyses, practice guidelines, and reporting standards – and will publish paper types not previously accepted, such as study protocols.
The journal will retain many initiatives of the previous editors, including the international debates, and will continue recruiting international authors and reviewers. Having the best reviewers, Dr. Gloviczki noted, “is an important parallel to having top-quality studies.”
Dr. Lawrence, of the University of California Los Angeles, will discuss what makes a clinical research paper successful. “We want papers that are highly cited – and the highly cited papers are prospective studies, whether randomized controlled trials or single-arm cohort studies,” Dr. Gloviczki said. “We also favor large retrospective reviews of prospectively collected national or international registries.”
Peter Henke, MD, of the University of Michigan in Ann Arbor, Mich., will talk about what the JVS editors and reviewers want in basic science papers – which Dr. Gloviczki called an important and sometimes overlooked counterpart to the clinical studies. “We believe that our profession must be in charge of basic research, that whoever owns basic research in our field owns the disease,” he said.
“To understand vascular disease you have to start at the basics of anatomy, pathophysiology, etiology, prevention, presentation and finally treatment,” he said, noting that vascular surgeons at many academic centers are conducting experimental studies and other basic research, efforts often supported by SVS grants.
Last year the JVS editors re-named the journal’s basic science section and called it “From Bench to Bedside” to try and capture the importance of preclinical vascular studies. “It’s a relatively small section of our journal but it’s important,” Dr. Gloviczki said. “And now we are really pushing to get commentaries that emphasize the potential clinical application of the basic science research.”
Richard L. Amdur, MD, of George Washington University in Washington, DC, will talk about what the JVS journal editors want to see in terms of statistics, while Marc L. Schermerhorn, MD, of Beth Israel Deaconess Medical Center in Boston and Martin Bjorck, MD, PhD, of Uppsala University, Uppsala, Sweden, will both discuss mining the large vascular registries from the United States and Europe for studies attractive to JVS or EJVES.
“There are so many papers where real-world experience is given to us by analyzing these registries,” Dr. Gloviczki said. Studies from the SVS Vascular Quality Initiatives database, the American College of Surgeons’ National Surgical Quality Improvement Program, the National Inpatient Sample, the Swedish Vascular registry, VADUNET and the International Consortium of Vascular Registries, “have changed the way we practice vascular surgery, and we publish multiple papers from these in every issue.”
Saturday, June 3
6:30 a.m. - 8:00 a.m.
Breakfast Session B9: How to Write a Paper and Have it Accepted in the JVS or EJVES
Friday - On Tap
What will happen Friday that people will be talking about Saturday? All of the below, and much more:
• 6:30 to 8:00 a.m. Breakfast Sessions: Pushing the boundaries in managing PAD, managing arterial infections and the aging of vascular surgeons. See Mobile App for room locations.
• 8:00 - 11:00 a.m.Plenary Sessions 4 through 6. Room 6 A/B. See Mobile App for abstracts and times.
• 11:00 a.m. Presidential address from Dr. Ronald M. Fairman. President-Elect Dr. R. Clement Darling, III, will introduce Dr. Fairman. Room 6 A/B.
• 3:30 to 5:00 p.m. Six Concurrent Sessions: the SVS/ESVS debate, joint sessions with the STS and AVF, an update on clinical practice guidelines and introduction of global vascular guidelines, and the Poster Competition. See Mobile App for details and room locations.
• 12:15 to 1:30 p.m. The Vascular Surgery Trainee Luncheon, Room 6C. Topics include how to find a job and “day in the life” stories from recent 5+2 and 0+5 graduates. Register at the Registration Counter.
• 5:00 to 6:30 p.m. Residency Fair. Exhibit Hall A.
What will happen Friday that people will be talking about Saturday? All of the below, and much more:
• 6:30 to 8:00 a.m. Breakfast Sessions: Pushing the boundaries in managing PAD, managing arterial infections and the aging of vascular surgeons. See Mobile App for room locations.
• 8:00 - 11:00 a.m.Plenary Sessions 4 through 6. Room 6 A/B. See Mobile App for abstracts and times.
• 11:00 a.m. Presidential address from Dr. Ronald M. Fairman. President-Elect Dr. R. Clement Darling, III, will introduce Dr. Fairman. Room 6 A/B.
• 3:30 to 5:00 p.m. Six Concurrent Sessions: the SVS/ESVS debate, joint sessions with the STS and AVF, an update on clinical practice guidelines and introduction of global vascular guidelines, and the Poster Competition. See Mobile App for details and room locations.
• 12:15 to 1:30 p.m. The Vascular Surgery Trainee Luncheon, Room 6C. Topics include how to find a job and “day in the life” stories from recent 5+2 and 0+5 graduates. Register at the Registration Counter.
• 5:00 to 6:30 p.m. Residency Fair. Exhibit Hall A.
What will happen Friday that people will be talking about Saturday? All of the below, and much more:
• 6:30 to 8:00 a.m. Breakfast Sessions: Pushing the boundaries in managing PAD, managing arterial infections and the aging of vascular surgeons. See Mobile App for room locations.
• 8:00 - 11:00 a.m.Plenary Sessions 4 through 6. Room 6 A/B. See Mobile App for abstracts and times.
• 11:00 a.m. Presidential address from Dr. Ronald M. Fairman. President-Elect Dr. R. Clement Darling, III, will introduce Dr. Fairman. Room 6 A/B.
• 3:30 to 5:00 p.m. Six Concurrent Sessions: the SVS/ESVS debate, joint sessions with the STS and AVF, an update on clinical practice guidelines and introduction of global vascular guidelines, and the Poster Competition. See Mobile App for details and room locations.
• 12:15 to 1:30 p.m. The Vascular Surgery Trainee Luncheon, Room 6C. Topics include how to find a job and “day in the life” stories from recent 5+2 and 0+5 graduates. Register at the Registration Counter.
• 5:00 to 6:30 p.m. Residency Fair. Exhibit Hall A.
Stop By, Say Hi! 6 Great Reasons to Visit the Membership Booth
While you’re in the neighborhood, why not stop by the SVS Membership Booth, located just outside the plenary doors?
Whether you are a member of SVS or not, we’d love to see you. Here are some reasons you’ll be glad you did:
Enter to win a $500 gift card if you update your SVS member profile or fill out a membership form.
Pick up a memento – SVS pens, notebooks, even saltwater taffy – of your visit (while supplies last).
Members are encouraged to update their personal information – emails, addresses, and even names can change. Don’t let yourself fall off the contact lists!
Inquire about membership options; learn about the benefits of belonging.
Get help with your mobile app.
Bonus: If you update your member details AND make a donation to the SVS Foundation (adjoining booth), you can enter the contest twice.
While you’re in the neighborhood, why not stop by the SVS Membership Booth, located just outside the plenary doors?
Whether you are a member of SVS or not, we’d love to see you. Here are some reasons you’ll be glad you did:
Enter to win a $500 gift card if you update your SVS member profile or fill out a membership form.
Pick up a memento – SVS pens, notebooks, even saltwater taffy – of your visit (while supplies last).
Members are encouraged to update their personal information – emails, addresses, and even names can change. Don’t let yourself fall off the contact lists!
Inquire about membership options; learn about the benefits of belonging.
Get help with your mobile app.
Bonus: If you update your member details AND make a donation to the SVS Foundation (adjoining booth), you can enter the contest twice.
While you’re in the neighborhood, why not stop by the SVS Membership Booth, located just outside the plenary doors?
Whether you are a member of SVS or not, we’d love to see you. Here are some reasons you’ll be glad you did:
Enter to win a $500 gift card if you update your SVS member profile or fill out a membership form.
Pick up a memento – SVS pens, notebooks, even saltwater taffy – of your visit (while supplies last).
Members are encouraged to update their personal information – emails, addresses, and even names can change. Don’t let yourself fall off the contact lists!
Inquire about membership options; learn about the benefits of belonging.
Get help with your mobile app.
Bonus: If you update your member details AND make a donation to the SVS Foundation (adjoining booth), you can enter the contest twice.
At Opening Reception: Vendors, Posters, Raffle
Meet up with friends, visit vendor booths to see the latest and greatest in all things vascular, peruse the posters.
And enter a high-tech raffle to win a high-flying prize: two airline tickets to anywhere in the continental United States AND complimentary registration for the 2018 Vascular Annual Meeting. While traversing the Exhibit Hall, be sure to look for placards with QR codes in select exhibitor booths; scan the QR code and be automatically entered into the raffle. No pens, no paper required, just a smart phone and the QR code.
Industry support is vital to VAM, permitting registration fees considerably lower than those assessed at comparable annual meetings. Please show your support by visiting our vendors.
The reception coincides with the end of the Interactive Poster Session, set for 5:00 to 6:30 p.m. in the same location.
Thursday, June 1
5:00 – 6:30 p.m.
Exhibit Hall B
Interactive Poster Session
5:30 – 6:30 p.m.
Exhibit Hall B
Opening Reception
Meet up with friends, visit vendor booths to see the latest and greatest in all things vascular, peruse the posters.
And enter a high-tech raffle to win a high-flying prize: two airline tickets to anywhere in the continental United States AND complimentary registration for the 2018 Vascular Annual Meeting. While traversing the Exhibit Hall, be sure to look for placards with QR codes in select exhibitor booths; scan the QR code and be automatically entered into the raffle. No pens, no paper required, just a smart phone and the QR code.
Industry support is vital to VAM, permitting registration fees considerably lower than those assessed at comparable annual meetings. Please show your support by visiting our vendors.
The reception coincides with the end of the Interactive Poster Session, set for 5:00 to 6:30 p.m. in the same location.
Thursday, June 1
5:00 – 6:30 p.m.
Exhibit Hall B
Interactive Poster Session
5:30 – 6:30 p.m.
Exhibit Hall B
Opening Reception
Meet up with friends, visit vendor booths to see the latest and greatest in all things vascular, peruse the posters.
And enter a high-tech raffle to win a high-flying prize: two airline tickets to anywhere in the continental United States AND complimentary registration for the 2018 Vascular Annual Meeting. While traversing the Exhibit Hall, be sure to look for placards with QR codes in select exhibitor booths; scan the QR code and be automatically entered into the raffle. No pens, no paper required, just a smart phone and the QR code.
Industry support is vital to VAM, permitting registration fees considerably lower than those assessed at comparable annual meetings. Please show your support by visiting our vendors.
The reception coincides with the end of the Interactive Poster Session, set for 5:00 to 6:30 p.m. in the same location.
Thursday, June 1
5:00 – 6:30 p.m.
Exhibit Hall B
Interactive Poster Session
5:30 – 6:30 p.m.
Exhibit Hall B
Opening Reception
How to Welcome a Patient Advisor to Your Research Team
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
On Tap – Thursday
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
2017 Resident Research Award: Epigenetic Mechanisms in Type 2 Diabetic Wound Healing
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award