User login
Antiplatelet Use
Tthe other major message from the revised CABG guidelines is a new approach to dealing with antiplatelet therapies in the days leading up to cardiac surgery, said Dr. Peter K. Smith, vice-chairman of the CABG guidelines committee.
"There is a growing body of evidence that patients benefit from these agents," the P2Y12-receptor binding drug class of clopidogrel (Plavix), prasugrel (Effient), and ticagrelor (Brilinta). "Our guidelines emphasize that surgery can be safely done in the presence of some of these platelet inhibitors when necessary," he said in an interview. "There is reluctance against doing surgery in the presence of these drugs that is to the disadvantage of patients."
Specifically, the new guidelines say that in patients referred for urgent CABG, clopidogrel and ticagrelor should be discontinued to at least 24 hours to reduce major bleeding complications. Stoppage scheduled 1 day before surgery is a significant scaling down from the prior recommendation that clopidogrel be halted at least 5 days before surgery, he said. "Surgeons need to be more permissive about having this [antiplatelet] environment in place when surgery is performed."
The new guidelines add that for patients undergoing elective CABG, clopidogrel or ticagrelor treatment should stop at least 5 days before surgery, and prasugrel treatment should stop for at least 7 days. This more conservative approach makes sense when patients are not unstable and in a prothrombotic state, Dr. Smith said.
The guidelines also update the presurgical approach to aspirin treatment. Aspirin should be administered preoperatively, at 100-325 mg/day, right up to surgery. Prior guidelines called for stopping aspirin several days before. The new guidelines recommend if aspirin was not administered preoperatively, it should be initiated within 6 hours after surgery and then continued indefinitely. Clopidogrel should be used in patients allergic to or intolerant of aspirin.
–Mitchel L. Zoler
Tthe other major message from the revised CABG guidelines is a new approach to dealing with antiplatelet therapies in the days leading up to cardiac surgery, said Dr. Peter K. Smith, vice-chairman of the CABG guidelines committee.
"There is a growing body of evidence that patients benefit from these agents," the P2Y12-receptor binding drug class of clopidogrel (Plavix), prasugrel (Effient), and ticagrelor (Brilinta). "Our guidelines emphasize that surgery can be safely done in the presence of some of these platelet inhibitors when necessary," he said in an interview. "There is reluctance against doing surgery in the presence of these drugs that is to the disadvantage of patients."
Specifically, the new guidelines say that in patients referred for urgent CABG, clopidogrel and ticagrelor should be discontinued to at least 24 hours to reduce major bleeding complications. Stoppage scheduled 1 day before surgery is a significant scaling down from the prior recommendation that clopidogrel be halted at least 5 days before surgery, he said. "Surgeons need to be more permissive about having this [antiplatelet] environment in place when surgery is performed."
The new guidelines add that for patients undergoing elective CABG, clopidogrel or ticagrelor treatment should stop at least 5 days before surgery, and prasugrel treatment should stop for at least 7 days. This more conservative approach makes sense when patients are not unstable and in a prothrombotic state, Dr. Smith said.
The guidelines also update the presurgical approach to aspirin treatment. Aspirin should be administered preoperatively, at 100-325 mg/day, right up to surgery. Prior guidelines called for stopping aspirin several days before. The new guidelines recommend if aspirin was not administered preoperatively, it should be initiated within 6 hours after surgery and then continued indefinitely. Clopidogrel should be used in patients allergic to or intolerant of aspirin.
–Mitchel L. Zoler
Tthe other major message from the revised CABG guidelines is a new approach to dealing with antiplatelet therapies in the days leading up to cardiac surgery, said Dr. Peter K. Smith, vice-chairman of the CABG guidelines committee.
"There is a growing body of evidence that patients benefit from these agents," the P2Y12-receptor binding drug class of clopidogrel (Plavix), prasugrel (Effient), and ticagrelor (Brilinta). "Our guidelines emphasize that surgery can be safely done in the presence of some of these platelet inhibitors when necessary," he said in an interview. "There is reluctance against doing surgery in the presence of these drugs that is to the disadvantage of patients."
Specifically, the new guidelines say that in patients referred for urgent CABG, clopidogrel and ticagrelor should be discontinued to at least 24 hours to reduce major bleeding complications. Stoppage scheduled 1 day before surgery is a significant scaling down from the prior recommendation that clopidogrel be halted at least 5 days before surgery, he said. "Surgeons need to be more permissive about having this [antiplatelet] environment in place when surgery is performed."
The new guidelines add that for patients undergoing elective CABG, clopidogrel or ticagrelor treatment should stop at least 5 days before surgery, and prasugrel treatment should stop for at least 7 days. This more conservative approach makes sense when patients are not unstable and in a prothrombotic state, Dr. Smith said.
The guidelines also update the presurgical approach to aspirin treatment. Aspirin should be administered preoperatively, at 100-325 mg/day, right up to surgery. Prior guidelines called for stopping aspirin several days before. The new guidelines recommend if aspirin was not administered preoperatively, it should be initiated within 6 hours after surgery and then continued indefinitely. Clopidogrel should be used in patients allergic to or intolerant of aspirin.
–Mitchel L. Zoler
New PCI, CABG Guidelines Support The Heart Team
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
New PCI, CABG Guidelines Support The Heart Team
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.☐
New PCI, CABG Guidelines Support The Heart Team
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.
The Heart Team is now officially the home team for selecting the best revascularization approach for patients with challenging coronary artery disease.
Two expert panels organized by the American College of Cardiology and American Heart Association each simultaneously released a revised set of guidelines – for Percutaneous Coronary Intervention (PCI) and for Coronary Artery Bypass Grafting (CABG). Both documents firmly recommended that physicians rely on Heart Teams to determine the best way to revascularize each patient who presents with either unprotected left main or "complex" coronary artery disease. The new revisions were also notable for the congruence of their recommendations, down to identical tables in both documents, and the collaboration between the two guideline-writing committees in coming up with their core revascularization sections (J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.007; J. Am. Coll. Cardiol. 2011;58:doi:10.1016/j.jacc.2011.08.009).
"The 2011 guideline includes an unprecedented degree of collaboration [among cardiologists and cardiothoracic surgeons] in generating revascularization recommendations for patients with CAD [coronary artery disease]," said Dr. Glenn N. Levine, professor of medicine and director of the cardiac care unit at Baylor College of Medicine in Houston, and chairman of the PCI guidelines panel, in a written statement.
"It’s a breakthrough, the complete concordance of the revascularization sections" of the PCI and CABG guidelines, said Dr. Peter K. Smith, professor of surgery and chief of cardiovascular and thoracic surgery at Duke University in Durham, N.C., and vice-chairman of the CABG panel. The revascularization recommendations contained in both documents "were made with complete unanimity between the two groups," he said in an interview.
The new PCI guidelines also received endorsement from the Society for Cardiovascular Angiography and Interventions, while the new CABG recommendations carried imprimaturs from the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery, and the Society of Cardiovascular Anesthesiologists.
The concept of relying on a Heart Team, a collaboration between at least one cardiologist and cardiac surgeon, to determine the best management strategy for a patient with coronary disease who could be managed by either an endovascular or surgical approach, first came to prominence in the mid-2000s during the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial, the most recent large study to compare the safety and efficacy of PCI and CABG (N. Engl. J. Med. 2009;360:961-72). More recently, the PARTNER (Placement of Aortic Transcatheter Valves) trial for assessing the safety and efficacy of transcatheter aortic valve replacement, served as another high-profile setting for Heart Teams (N. Engl. J. Med. 2011;364:2187-98). The new guidelines for both PCI and CABG, which each gave the Heart Team approach a class 1 recommendation for managing patients with unprotected left main or complex CAD, represent the first time the Heart Team strategy received official endorsement from a health-policy setting group.
"The Heart Team concept evolved from these randomized trials, where patients could get either treatment. If that was how the trials led to their results, they are best replicated by using the same design," said Dr. Smith. When the guidelines refer to "complex" CAD, they mean triple vessel disease, as well as patients with two-vessel CAD that involves the proximal left anterior descending coronary artery, he noted. In such patients, as well as those with unprotected left main disease, the goal of revascularization is reduced mortality. Both sets of guidelines suggest assessing CAD complexity by calculating each patient’s SYNTAX score, a formula for quantifying CAD complexity originally developed for the SYNTAX trial. A score of 23 or higher defines more complex CAD, according to the new guidelines.
Results from "SYNTAX and other trials showed that [patients can] do as well with PCI or CABG for their longevity benefit," As a consequence, it is important for a cardiologist and surgeon to determine the suitability of each of these patients for the two options, Dr. Smith said.
The guidelines suggest physicians assess patients’ risk for surgery by quantifying their cardiac health and comorbidity severity by calculation of a STS score, as well as taking into account any other comorbidities not included in the STS score. "When the surgical risk is low, CABG is preferred even when PCI is possible, but if the surgery risk is high then patients should undergo PCI," he said. "Cardiac surgeons need to refer some patients with left main disease to PCI" because their clinical status makes them poor surgical candidates. "This is a big change [for cardiac surgeons], compared with 5 years ago," Dr. Smith said. "But only about 25% of left main patients fall into this category," where PCI is the better option.
While a Heart Team is important for deciding the best treatment for patients with life-threatening CAD, this subgroup probably represents about a quarter of all patients who need revascularization treatment, Dr. Smith said. The remaining three-quarters need revascularization for symptom relief, and while CABG also works well for this purpose, most patients in this category would also benefit from PCI, which may be the preferred choice, he added.
This new approach will probably not have a big impact on the volume of U.S. PCIs performed, predicted Dr. James C. Blankenship, vice-chairman of the PCI guidelines committee and an interventional cardiologist practicing in Danville, Pa. "On the complex end, I doubt that many PCIs today are done in super complex patients. On the low end, there has been a big shift in recognizing coronary lesions that need PCI," using tools that identify ischemia-causing lesions such as intravascular ultrasound and measuring fractional flow reserve. "Most interventionalists have shifted to this paradigm. For any who haven’t, the guidelines emphasize the importance of this approach," Dr. Blankenship said in an interview.
The call for Heart Teams by the new guidelines raises the issue whether enough U.S. teams exist to handle the volume of appropriate patients. Dr. Smith said there are, although they may not have a formal Heart Team designation.
"I think surgeons and cardiologists collaborate on this more than people think. They may not even realize they are doing it. To a large extent today it is not a formal process, but cardiologists and surgeons have multiple encounters with each other over their patients and they develop a sense of where to go, and when it is a close call [on how to manage a patient] they get together," Dr. Smith said
"It may not be a Heart Team as defined in the SYNTAX study. It can be any cardiac surgeon, and any interventional cardiologist," said Dr. Blankenship.
But, Dr. Smith noted, "the average cardiologist doesn’t calculate a SYNTAX score. We hope [the new guidelines] will lead to a resetting of the thought process."
And there are undoubtedly cardiologists today who do not consult with surgeons as often as they should, said Dr. Blankenship. "For many cardiologists it’s routine, but some cardiologists may be more aggressive about using PCI and less aggressive about getting surgical input." The new guidelines "set it forth as standard, and codify it by making the SYNTAX score a surrogate for disease complexity."
Dr. Levine said that he had no disclosures. Dr. Smith said that he has been a consultant to Eli Lilly and Baxter BioSurgery. Dr. Blankenship said that he has received research support from Abiomed, AstraZeneca, Boston Scientific, Conor Medsystems, Kai Pharmaceuticals, and Schering-Plough.
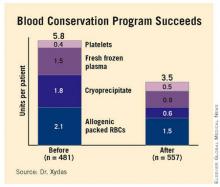
Blood Conservation Program Successful
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
Major Finding: Use of a blood conservation algorithm reduced total blood product usage from an average of 5.8 U per patient at baseline to 3.5 U per patient, without compromising safety.
Data Source: Prospective study of 1,038 patients undergoing isolated coronary artery bypass grafting.
Disclosures: Dr. Xydas said he had no relevant financial disclosures.
CABG Beats PCI Regardless of SYNTAX Score
PARIS – Coronary artery bypass grafting was found to surpass percutaneous coronary intervention in a "real-world" registry of patients with three-vessel coronary disease, largely confirming the findings of the SYNTAX trial in patients with high SYNTAX scores and in those with low scores.
However, because the new data – obtained at 26 Japanese centers during 2005-2007 and involving nearly 3,000 patients – came from a nonrandomized registry, it may have been flawed by selection biases that skewed which patients underwent bypass surgery and which ones had percutaneous revascularization.
Coronary artery bypass grafting (CABG) "remains the standard treatment option for patients with triple-vessel disease, even when their SYNTAX scores are high," Dr. Hiroki Shiomi said at the annual congress of the European society of Cardiology.
"Use of PCI [percutaneous coronary intervention] in patients with high SYNTAX scores should be seriously discouraged unless their operative risk is prohibitively high," said Dr. Shiomi, a cardiologist at Kyoto University Hospital, Japan.
The registry results "suggested that the clinical outcome of PCI is not comparable with CABG even in patients with low syntax scores."
But the study’s findings also suggested that a selection bias occurred that even the risk-adjusted analysis used by Dr. Shiomi and his associates failed to adequately control, commented Dr. Uwe Zeymer, an interventional cardiologist and professor at the Institute for Myocardial Infarction Research in Ludwigshafen, Germany.
A major clue that selection bias came into play was that all-cause death during the 3-year follow-up of the study was 62% higher among the patients who underwent PCI, compared with those who underwent CABG, a statistically significant difference; in contrast, the rate of cardiac death was not significantly different between the CABG and PCI patients.
This discrepancy "says there was selection bias. Physicians had to decide what to do with patients who had a lot of comorbidities," and most of those patients probably underwent PCI, Dr. Zeymer said in an interview.
"If the patients [undergoing PCI and CABG] were the same clinically, you’d expect that with PCI you would at least have the same result" for all-cause mortality. "There seems to have been a selection bias toward using PCI in patients with more comorbidities.
"What we can say is that in this real-world situation, cardiac mortality was the same" with both revascularization methods, "which is reassuring for the use of PCI," he added.
CREDO-Kyoto (Coronary Revascularization Demonstrating Outcome Study in Kyoto) enrolled more than 13,000 patients who underwent coronary revascularization at any of 26 Japanese centers during 2005-2007, a period when all PCIs used a drug-eluting coronary stent.
The current analysis focused on 2,981 patients with triple-vessel disease and no left main coronary disease or acute MI, and included 1,825 who were treated with CABG and 1,156 treated by PCI. The average age of the PCI patients was 70 years; the CABG patients averaged 68 years old.
After 1 year of follow-up, the combined rate of death, MI, or stroke was 23% higher in the patients treated with PCI, compared with those treated with CABG, a statistically significant difference in an unadjusted analysis for the study’s primary end point.
After adjustment for baseline differences between the CABG and PCI patients, the rate of this combined end point was 47% higher among the PCI patients, also a statistically significant difference.
Analysis of several secondary end points showed a mixed pattern of differences between the two treatment groups in the adjusted analyses.
A statistically significant difference in favor of fewer events with CABG occurred in the end point of all-cause death, which was found to be 62% higher with PCI, as well as in the end point of MI, which was 2.39-fold higher in the PCI group.
The protection against MI by CABG, compared with PCI, was "particularly remarkable," Dr. Shiomi said.
But the end points of cardiac death and stroke showed no statistically significant differences between the two treatment groups in either the unadjusted or adjusted analyses.
Dr. Shiomi said that baseline SYNTAX scores were available for 94% of the patients. The mean score was 24 in the PCI patients and 30 for the CABG patients.
For the primary end point of death, MI, or stroke, treatment with PCI linked with a statistically significant 59% higher rate of the combined, primary end point, compared with CABG, in the adjusted analysis of patients with the highest SYNTAX scores (33 or greater); among patients with the lowest scores (22 or less), the adjusted analysis showed a significant, 66% higher rate of the combined outcome end point with PCI, compared with CABG.
For patients with SYNTAX scores of 23-32, the two treatment strategies led to similar adverse event rates in the two treatment groups.
Dr. Shiomi said he had no disclosures. Dr. Zeymer said that the Institute of MI Research in Germany, where he works, has received research grant support from multiple cardiac-device companies.
Cardiologists devised the SYNTAX score (EuroIntervention 2005;1:219-27) as a tool for quantifying the complexity of coronary anatomy in patients enrolled in the landmark SYNTAX trial (N. Engl. J. Med. 2009;360:961-72).
The SYNTAX investigators recently published the 3-year outcomes results from SYNTAX (Eur. Heart J. 2011;32:2125-34). Those results showed that patients treated with CABG had significantly fewer major adverse coronary and cerebrovascular events (MACCE) than did those who underwent PCI among patients with a high SYNTAX score (greater than 33), including the analysis with all patients, in patients with triple-vessel disease, and in patients with left main coronary disease. Among patients with intermediate SYNTAX scores (23-32), the MACCE rate was significantly lower with CABG than with PCI among all patients and in the subgroup with triple-vessel disease; in those with left main coronary disease, the MACCE rate was similar among patients treated with CABG and those treated with PCI. In patients with low SYNTAX scores (22 or less), the MACCE rates were similar among all CABG and PCI patients, as well as those in the subgroups who had either triple-vessel disease or left main coronary disease.
Given this background, it is a big surprise to learn that the Japanese study found a statistically significant advantage for CABG in the 3-year incidence of death, MI, and stroke among patients with a low SYNTAX score who were treated with CABG, compared with those who underwent PCI. This finding needs further examination in future randomized studies.
The CREDO-Kyoto study differed from SYNTAX by being nonrandomized. The current analysis focused exclusively on patients with triple-vessel coronary disease and excluded those with left main coronary disease.
The new Japanese results confirmed the key findings from the SYNTAX study in a large, real-world population. The new results show the usefulness of the SYNTAX score when it is used in clinical practice; however, in this study, the score calculation and the analysis of its relevance to outcomes occurred retrospectively. The ability of the SYNTAX score to help assign patients to optimal treatment with either CABG or PCI needs testing prospectively.
Frans Van de Werf, M.D., is professor and chairman of the department of cardiovascular medicine at University Hospitals Leuven (Belgium). He said that he had no relevant disclosures. This is adapted from the comments he made as the discussant for the study.
Cardiologists devised the SYNTAX score (EuroIntervention 2005;1:219-27) as a tool for quantifying the complexity of coronary anatomy in patients enrolled in the landmark SYNTAX trial (N. Engl. J. Med. 2009;360:961-72).
The SYNTAX investigators recently published the 3-year outcomes results from SYNTAX (Eur. Heart J. 2011;32:2125-34). Those results showed that patients treated with CABG had significantly fewer major adverse coronary and cerebrovascular events (MACCE) than did those who underwent PCI among patients with a high SYNTAX score (greater than 33), including the analysis with all patients, in patients with triple-vessel disease, and in patients with left main coronary disease. Among patients with intermediate SYNTAX scores (23-32), the MACCE rate was significantly lower with CABG than with PCI among all patients and in the subgroup with triple-vessel disease; in those with left main coronary disease, the MACCE rate was similar among patients treated with CABG and those treated with PCI. In patients with low SYNTAX scores (22 or less), the MACCE rates were similar among all CABG and PCI patients, as well as those in the subgroups who had either triple-vessel disease or left main coronary disease.
Given this background, it is a big surprise to learn that the Japanese study found a statistically significant advantage for CABG in the 3-year incidence of death, MI, and stroke among patients with a low SYNTAX score who were treated with CABG, compared with those who underwent PCI. This finding needs further examination in future randomized studies.
The CREDO-Kyoto study differed from SYNTAX by being nonrandomized. The current analysis focused exclusively on patients with triple-vessel coronary disease and excluded those with left main coronary disease.
The new Japanese results confirmed the key findings from the SYNTAX study in a large, real-world population. The new results show the usefulness of the SYNTAX score when it is used in clinical practice; however, in this study, the score calculation and the analysis of its relevance to outcomes occurred retrospectively. The ability of the SYNTAX score to help assign patients to optimal treatment with either CABG or PCI needs testing prospectively.
Frans Van de Werf, M.D., is professor and chairman of the department of cardiovascular medicine at University Hospitals Leuven (Belgium). He said that he had no relevant disclosures. This is adapted from the comments he made as the discussant for the study.
Cardiologists devised the SYNTAX score (EuroIntervention 2005;1:219-27) as a tool for quantifying the complexity of coronary anatomy in patients enrolled in the landmark SYNTAX trial (N. Engl. J. Med. 2009;360:961-72).
The SYNTAX investigators recently published the 3-year outcomes results from SYNTAX (Eur. Heart J. 2011;32:2125-34). Those results showed that patients treated with CABG had significantly fewer major adverse coronary and cerebrovascular events (MACCE) than did those who underwent PCI among patients with a high SYNTAX score (greater than 33), including the analysis with all patients, in patients with triple-vessel disease, and in patients with left main coronary disease. Among patients with intermediate SYNTAX scores (23-32), the MACCE rate was significantly lower with CABG than with PCI among all patients and in the subgroup with triple-vessel disease; in those with left main coronary disease, the MACCE rate was similar among patients treated with CABG and those treated with PCI. In patients with low SYNTAX scores (22 or less), the MACCE rates were similar among all CABG and PCI patients, as well as those in the subgroups who had either triple-vessel disease or left main coronary disease.
Given this background, it is a big surprise to learn that the Japanese study found a statistically significant advantage for CABG in the 3-year incidence of death, MI, and stroke among patients with a low SYNTAX score who were treated with CABG, compared with those who underwent PCI. This finding needs further examination in future randomized studies.
The CREDO-Kyoto study differed from SYNTAX by being nonrandomized. The current analysis focused exclusively on patients with triple-vessel coronary disease and excluded those with left main coronary disease.
The new Japanese results confirmed the key findings from the SYNTAX study in a large, real-world population. The new results show the usefulness of the SYNTAX score when it is used in clinical practice; however, in this study, the score calculation and the analysis of its relevance to outcomes occurred retrospectively. The ability of the SYNTAX score to help assign patients to optimal treatment with either CABG or PCI needs testing prospectively.
Frans Van de Werf, M.D., is professor and chairman of the department of cardiovascular medicine at University Hospitals Leuven (Belgium). He said that he had no relevant disclosures. This is adapted from the comments he made as the discussant for the study.
PARIS – Coronary artery bypass grafting was found to surpass percutaneous coronary intervention in a "real-world" registry of patients with three-vessel coronary disease, largely confirming the findings of the SYNTAX trial in patients with high SYNTAX scores and in those with low scores.
However, because the new data – obtained at 26 Japanese centers during 2005-2007 and involving nearly 3,000 patients – came from a nonrandomized registry, it may have been flawed by selection biases that skewed which patients underwent bypass surgery and which ones had percutaneous revascularization.
Coronary artery bypass grafting (CABG) "remains the standard treatment option for patients with triple-vessel disease, even when their SYNTAX scores are high," Dr. Hiroki Shiomi said at the annual congress of the European society of Cardiology.
"Use of PCI [percutaneous coronary intervention] in patients with high SYNTAX scores should be seriously discouraged unless their operative risk is prohibitively high," said Dr. Shiomi, a cardiologist at Kyoto University Hospital, Japan.
The registry results "suggested that the clinical outcome of PCI is not comparable with CABG even in patients with low syntax scores."
But the study’s findings also suggested that a selection bias occurred that even the risk-adjusted analysis used by Dr. Shiomi and his associates failed to adequately control, commented Dr. Uwe Zeymer, an interventional cardiologist and professor at the Institute for Myocardial Infarction Research in Ludwigshafen, Germany.
A major clue that selection bias came into play was that all-cause death during the 3-year follow-up of the study was 62% higher among the patients who underwent PCI, compared with those who underwent CABG, a statistically significant difference; in contrast, the rate of cardiac death was not significantly different between the CABG and PCI patients.
This discrepancy "says there was selection bias. Physicians had to decide what to do with patients who had a lot of comorbidities," and most of those patients probably underwent PCI, Dr. Zeymer said in an interview.
"If the patients [undergoing PCI and CABG] were the same clinically, you’d expect that with PCI you would at least have the same result" for all-cause mortality. "There seems to have been a selection bias toward using PCI in patients with more comorbidities.
"What we can say is that in this real-world situation, cardiac mortality was the same" with both revascularization methods, "which is reassuring for the use of PCI," he added.
CREDO-Kyoto (Coronary Revascularization Demonstrating Outcome Study in Kyoto) enrolled more than 13,000 patients who underwent coronary revascularization at any of 26 Japanese centers during 2005-2007, a period when all PCIs used a drug-eluting coronary stent.
The current analysis focused on 2,981 patients with triple-vessel disease and no left main coronary disease or acute MI, and included 1,825 who were treated with CABG and 1,156 treated by PCI. The average age of the PCI patients was 70 years; the CABG patients averaged 68 years old.
After 1 year of follow-up, the combined rate of death, MI, or stroke was 23% higher in the patients treated with PCI, compared with those treated with CABG, a statistically significant difference in an unadjusted analysis for the study’s primary end point.
After adjustment for baseline differences between the CABG and PCI patients, the rate of this combined end point was 47% higher among the PCI patients, also a statistically significant difference.
Analysis of several secondary end points showed a mixed pattern of differences between the two treatment groups in the adjusted analyses.
A statistically significant difference in favor of fewer events with CABG occurred in the end point of all-cause death, which was found to be 62% higher with PCI, as well as in the end point of MI, which was 2.39-fold higher in the PCI group.
The protection against MI by CABG, compared with PCI, was "particularly remarkable," Dr. Shiomi said.
But the end points of cardiac death and stroke showed no statistically significant differences between the two treatment groups in either the unadjusted or adjusted analyses.
Dr. Shiomi said that baseline SYNTAX scores were available for 94% of the patients. The mean score was 24 in the PCI patients and 30 for the CABG patients.
For the primary end point of death, MI, or stroke, treatment with PCI linked with a statistically significant 59% higher rate of the combined, primary end point, compared with CABG, in the adjusted analysis of patients with the highest SYNTAX scores (33 or greater); among patients with the lowest scores (22 or less), the adjusted analysis showed a significant, 66% higher rate of the combined outcome end point with PCI, compared with CABG.
For patients with SYNTAX scores of 23-32, the two treatment strategies led to similar adverse event rates in the two treatment groups.
Dr. Shiomi said he had no disclosures. Dr. Zeymer said that the Institute of MI Research in Germany, where he works, has received research grant support from multiple cardiac-device companies.
PARIS – Coronary artery bypass grafting was found to surpass percutaneous coronary intervention in a "real-world" registry of patients with three-vessel coronary disease, largely confirming the findings of the SYNTAX trial in patients with high SYNTAX scores and in those with low scores.
However, because the new data – obtained at 26 Japanese centers during 2005-2007 and involving nearly 3,000 patients – came from a nonrandomized registry, it may have been flawed by selection biases that skewed which patients underwent bypass surgery and which ones had percutaneous revascularization.
Coronary artery bypass grafting (CABG) "remains the standard treatment option for patients with triple-vessel disease, even when their SYNTAX scores are high," Dr. Hiroki Shiomi said at the annual congress of the European society of Cardiology.
"Use of PCI [percutaneous coronary intervention] in patients with high SYNTAX scores should be seriously discouraged unless their operative risk is prohibitively high," said Dr. Shiomi, a cardiologist at Kyoto University Hospital, Japan.
The registry results "suggested that the clinical outcome of PCI is not comparable with CABG even in patients with low syntax scores."
But the study’s findings also suggested that a selection bias occurred that even the risk-adjusted analysis used by Dr. Shiomi and his associates failed to adequately control, commented Dr. Uwe Zeymer, an interventional cardiologist and professor at the Institute for Myocardial Infarction Research in Ludwigshafen, Germany.
A major clue that selection bias came into play was that all-cause death during the 3-year follow-up of the study was 62% higher among the patients who underwent PCI, compared with those who underwent CABG, a statistically significant difference; in contrast, the rate of cardiac death was not significantly different between the CABG and PCI patients.
This discrepancy "says there was selection bias. Physicians had to decide what to do with patients who had a lot of comorbidities," and most of those patients probably underwent PCI, Dr. Zeymer said in an interview.
"If the patients [undergoing PCI and CABG] were the same clinically, you’d expect that with PCI you would at least have the same result" for all-cause mortality. "There seems to have been a selection bias toward using PCI in patients with more comorbidities.
"What we can say is that in this real-world situation, cardiac mortality was the same" with both revascularization methods, "which is reassuring for the use of PCI," he added.
CREDO-Kyoto (Coronary Revascularization Demonstrating Outcome Study in Kyoto) enrolled more than 13,000 patients who underwent coronary revascularization at any of 26 Japanese centers during 2005-2007, a period when all PCIs used a drug-eluting coronary stent.
The current analysis focused on 2,981 patients with triple-vessel disease and no left main coronary disease or acute MI, and included 1,825 who were treated with CABG and 1,156 treated by PCI. The average age of the PCI patients was 70 years; the CABG patients averaged 68 years old.
After 1 year of follow-up, the combined rate of death, MI, or stroke was 23% higher in the patients treated with PCI, compared with those treated with CABG, a statistically significant difference in an unadjusted analysis for the study’s primary end point.
After adjustment for baseline differences between the CABG and PCI patients, the rate of this combined end point was 47% higher among the PCI patients, also a statistically significant difference.
Analysis of several secondary end points showed a mixed pattern of differences between the two treatment groups in the adjusted analyses.
A statistically significant difference in favor of fewer events with CABG occurred in the end point of all-cause death, which was found to be 62% higher with PCI, as well as in the end point of MI, which was 2.39-fold higher in the PCI group.
The protection against MI by CABG, compared with PCI, was "particularly remarkable," Dr. Shiomi said.
But the end points of cardiac death and stroke showed no statistically significant differences between the two treatment groups in either the unadjusted or adjusted analyses.
Dr. Shiomi said that baseline SYNTAX scores were available for 94% of the patients. The mean score was 24 in the PCI patients and 30 for the CABG patients.
For the primary end point of death, MI, or stroke, treatment with PCI linked with a statistically significant 59% higher rate of the combined, primary end point, compared with CABG, in the adjusted analysis of patients with the highest SYNTAX scores (33 or greater); among patients with the lowest scores (22 or less), the adjusted analysis showed a significant, 66% higher rate of the combined outcome end point with PCI, compared with CABG.
For patients with SYNTAX scores of 23-32, the two treatment strategies led to similar adverse event rates in the two treatment groups.
Dr. Shiomi said he had no disclosures. Dr. Zeymer said that the Institute of MI Research in Germany, where he works, has received research grant support from multiple cardiac-device companies.
In Coronary Artery Bypass, BIMA May Be Best
COLORADO SPRINGS ? Using bilateral internal mammary artery grafts provided a significant long-term survival advantage over single mammary artery grafts for coronary artery bypass surgery patients with normal or moderately impaired left ventricular function, according to a large retrospective study with lengthy follow-up. But when preoperative left ventricular ejection fraction (EF) was less than 30%, the procedure choice showed no difference in survival.
"BIMA grafting is the operation of choice in patients with a life expectancy beyond 1-2 decades," Dr. David Galbut said at the annual meeting of the Western Thoracic Surgical Association. He reported on 4,537 consecutive patients who had CABG with internal mammary artery grafting during 1972-1994 at three Florida hospitals. BIMA grafts were performed in 48% of the patients, an exceptionally high BIMA rate. In contrast, the Society of Thoracic Surgeons database shows that 4% of patients undergoing CABG nationally receive BIMA grafts. The reason for the 12-fold higher BIMA rate in the Florida study is that Dr. Galbut and colleagues had a decades-long conviction that BIMA has major clinical advantages.
In the Florida study, 233 patients had an EF below 30%, another 1,256 had an EF of 30%-50%, and 3,048 had a normal EF. In the low EF group, 87 BIMA patients were matched to an equal number of SIMA patients on the basis of 14 preoperative variables. In like manner, propensity scores were used to match 448 BIMA patients in the moderately impaired EF group and 1,137 BIMA patients with a normal EF to similar SIMA patients.
Many surgeons are reluctant to use BIMA grafting because of a concern that it will result in increased complications. This wasn?t the case in the Florida series. Indeed, operative morbidity ? including sternal wound infection rates ? were similar between BIMA and SIMA, according to Dr. Galbut of the Aventura (Fla.) Medical Center.
The 20-year survival rate in BIMA patients with moderately impaired EF was 33.1%, significantly better than the 19% survival in matched SIMA patients. In the normal EF group, the 20-year survival rate was 38.1% with BIMA and 35.8% with SIMA.
The general strategy the surgeons followed in BIMA grafting was to run the left internal mammary artery (LIMA) graft to the left anterior descending coronary artery. The LIMA is the dominant vessel in most patients and would therefore be the most durable conduit. The right internal mammary artery graft was placed wherever it fit best.
Discussant Dr. Anthony P. Furnary observed that retrospective studies can?t prove causality, not even when they?re large, painstakingly performed, and feature more than 2 decades of follow-up. Limitations in propensity score matching may account for much or all of the long-term survival advantage observed with BIMA grafting seen. Although patients were extensively matched in 14 preoperative variables, the year of surgery wasn?t among them.
The 22-year study period saw the introduction of many myocardial protection techniques. If more SIMA patients were operated on in earlier years, they might well have missed out on these therapies, said Dr. Furnary of the Providence Heart and Vascular Institute, Portland, Ore.
Dr. Galbut had no disclosures.
COLORADO SPRINGS ? Using bilateral internal mammary artery grafts provided a significant long-term survival advantage over single mammary artery grafts for coronary artery bypass surgery patients with normal or moderately impaired left ventricular function, according to a large retrospective study with lengthy follow-up. But when preoperative left ventricular ejection fraction (EF) was less than 30%, the procedure choice showed no difference in survival.
"BIMA grafting is the operation of choice in patients with a life expectancy beyond 1-2 decades," Dr. David Galbut said at the annual meeting of the Western Thoracic Surgical Association. He reported on 4,537 consecutive patients who had CABG with internal mammary artery grafting during 1972-1994 at three Florida hospitals. BIMA grafts were performed in 48% of the patients, an exceptionally high BIMA rate. In contrast, the Society of Thoracic Surgeons database shows that 4% of patients undergoing CABG nationally receive BIMA grafts. The reason for the 12-fold higher BIMA rate in the Florida study is that Dr. Galbut and colleagues had a decades-long conviction that BIMA has major clinical advantages.
In the Florida study, 233 patients had an EF below 30%, another 1,256 had an EF of 30%-50%, and 3,048 had a normal EF. In the low EF group, 87 BIMA patients were matched to an equal number of SIMA patients on the basis of 14 preoperative variables. In like manner, propensity scores were used to match 448 BIMA patients in the moderately impaired EF group and 1,137 BIMA patients with a normal EF to similar SIMA patients.
Many surgeons are reluctant to use BIMA grafting because of a concern that it will result in increased complications. This wasn?t the case in the Florida series. Indeed, operative morbidity ? including sternal wound infection rates ? were similar between BIMA and SIMA, according to Dr. Galbut of the Aventura (Fla.) Medical Center.
The 20-year survival rate in BIMA patients with moderately impaired EF was 33.1%, significantly better than the 19% survival in matched SIMA patients. In the normal EF group, the 20-year survival rate was 38.1% with BIMA and 35.8% with SIMA.
The general strategy the surgeons followed in BIMA grafting was to run the left internal mammary artery (LIMA) graft to the left anterior descending coronary artery. The LIMA is the dominant vessel in most patients and would therefore be the most durable conduit. The right internal mammary artery graft was placed wherever it fit best.
Discussant Dr. Anthony P. Furnary observed that retrospective studies can?t prove causality, not even when they?re large, painstakingly performed, and feature more than 2 decades of follow-up. Limitations in propensity score matching may account for much or all of the long-term survival advantage observed with BIMA grafting seen. Although patients were extensively matched in 14 preoperative variables, the year of surgery wasn?t among them.
The 22-year study period saw the introduction of many myocardial protection techniques. If more SIMA patients were operated on in earlier years, they might well have missed out on these therapies, said Dr. Furnary of the Providence Heart and Vascular Institute, Portland, Ore.
Dr. Galbut had no disclosures.
COLORADO SPRINGS ? Using bilateral internal mammary artery grafts provided a significant long-term survival advantage over single mammary artery grafts for coronary artery bypass surgery patients with normal or moderately impaired left ventricular function, according to a large retrospective study with lengthy follow-up. But when preoperative left ventricular ejection fraction (EF) was less than 30%, the procedure choice showed no difference in survival.
"BIMA grafting is the operation of choice in patients with a life expectancy beyond 1-2 decades," Dr. David Galbut said at the annual meeting of the Western Thoracic Surgical Association. He reported on 4,537 consecutive patients who had CABG with internal mammary artery grafting during 1972-1994 at three Florida hospitals. BIMA grafts were performed in 48% of the patients, an exceptionally high BIMA rate. In contrast, the Society of Thoracic Surgeons database shows that 4% of patients undergoing CABG nationally receive BIMA grafts. The reason for the 12-fold higher BIMA rate in the Florida study is that Dr. Galbut and colleagues had a decades-long conviction that BIMA has major clinical advantages.
In the Florida study, 233 patients had an EF below 30%, another 1,256 had an EF of 30%-50%, and 3,048 had a normal EF. In the low EF group, 87 BIMA patients were matched to an equal number of SIMA patients on the basis of 14 preoperative variables. In like manner, propensity scores were used to match 448 BIMA patients in the moderately impaired EF group and 1,137 BIMA patients with a normal EF to similar SIMA patients.
Many surgeons are reluctant to use BIMA grafting because of a concern that it will result in increased complications. This wasn?t the case in the Florida series. Indeed, operative morbidity ? including sternal wound infection rates ? were similar between BIMA and SIMA, according to Dr. Galbut of the Aventura (Fla.) Medical Center.
The 20-year survival rate in BIMA patients with moderately impaired EF was 33.1%, significantly better than the 19% survival in matched SIMA patients. In the normal EF group, the 20-year survival rate was 38.1% with BIMA and 35.8% with SIMA.
The general strategy the surgeons followed in BIMA grafting was to run the left internal mammary artery (LIMA) graft to the left anterior descending coronary artery. The LIMA is the dominant vessel in most patients and would therefore be the most durable conduit. The right internal mammary artery graft was placed wherever it fit best.
Discussant Dr. Anthony P. Furnary observed that retrospective studies can?t prove causality, not even when they?re large, painstakingly performed, and feature more than 2 decades of follow-up. Limitations in propensity score matching may account for much or all of the long-term survival advantage observed with BIMA grafting seen. Although patients were extensively matched in 14 preoperative variables, the year of surgery wasn?t among them.
The 22-year study period saw the introduction of many myocardial protection techniques. If more SIMA patients were operated on in earlier years, they might well have missed out on these therapies, said Dr. Furnary of the Providence Heart and Vascular Institute, Portland, Ore.
Dr. Galbut had no disclosures.
Major Finding: The 20-year survival rate in BIMA patients in the moderately impaired EF group was 33.1%, significantly better than the 19% in matched SIMA patients. In the normal EF group, the 20-year survival rate was 38.1% with BIMA and 35.8% with SIMA.
Data Source: A retrospective study of 4,537 consecutive patients who underwent CABG with internal mammary artery grafting during 1972-1994 at three Florida hospitals.
Disclosures: Dr. Galbut declared having no financial conflicts.
Cardiothoracic Clinical Trails Move Forward
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
CABG, PCI Trends Suggest Many Not Treated Optimally
The rate of coronary artery bypass grafting performed in U.S. hospitals declined by approximately one-third between 2001 and 2008, according to an analysis of the Agency for Healthcare Research and Quality database.
During the same period, the rate of percutaneous coronary interventions (PCIs) showed a far more modest decrease.
"Our data imply a sizeable shift in cardiovascular clinical practice patterns away from surgical treatment toward percutaneous, catheter-based interventions," said Andrew J. Epstein, Ph.D., of the Philadelphia Veterans Affairs? Center for Health Equity Research and Promotion and the University of Pennsylvania, and his associates.
Given that coronary artery bypass grafting remains the better choice for patients with previously untreated three-vessel or left main coronary artery disease, according to the results of the SYNTAX trial (N. Engl. J. Med. 2009;360:961-72), it appears that CABG is being underused, the authors wrote.
It seems likely that in recent years, "patients who would have been optimally treated with CABG surgery were instead treated with PCI," they noted.
To assess temporal trends in coronary revascularization procedures, the investigators examined a nationally representative sample of hospitalization claims using an Agency for Healthcare Research and Quality database.
The database includes discharge data from approximately 1,000 nonfederal hospitals in 42 states, which covers 20% of U.S. hospitals and allows accurate estimates for the entire population of hospitalized patients, regardless of payer or insurance status.
Between 2001 and 2008, the total number of coronary revascularizations decreased "modestly," by approximately 15%.
There was a "substantial," statistically significant, 38% decrease in the annual rate of CABG surgery, from 1,742 per million adults in the first year of the study period to 1,081 per million in the final year.
This decline was roughly linear throughout the 8-year study period, suggesting that it "was not triggered by any single event occurring during the past decade, such as the introduction of competing technologies, advances in CABG surgical techniques, publication of clinical trials, or issuance of clinical guidelines."
CABG procedures decreased across all sex, age, racial, and regional subgroups.
In contrast, the PCI rate remained fairly constant, showing a "modest" 4% decrease from 3,827 per million adults per year in the first year of the study to 3,667 in the final year.
"Projected to the entire U.S. population, these rate changes implied that 130,000 fewer CABG surgeries were performed in 2008 compared to 2001," Dr. Epstein and his colleagues noted (JAMA 2011;305:1769-76).
The data did not allow the researchers to distinguish which patients may have been more appropriate candidates for CABG than for PCI, so "it cannot be known with certainty whether physicians were increasingly substituting PCI for CABG surgery during the past decade. ... [But] our findings suggest the possibility that several thousand patients who underwent PCI in 2008 would have undergone CABG surgery had patterns of care not changed markedly," they said.
The preferences of patients were also not discernible from the data, lead investigator Dr. Peter W. Groeneveld said in an interview. "However, if patient preference [for PCI vs. CABG] was the driving factor, there would have to be some reason that PCI was even more preferable to patients in 2008 than it was in 2001.
This scenario seems unlikely since the procedures haven?t changed that much," said Dr. Groeneveld, assistant professor of medicine at the University of Pennsylvania and staff physician at the Philadelphia Veterans Affairs Medical Center.
Another important finding was that during this interval, the number of hospitals providing CABG increased. Combined with the drop in the number of CABG surgeries, this resulted in a 28% decline in the median caseload per hospital, "and a substantial increase in the number of hospitals that provided fewer than 100 CABG surgeries per year."
Whether or not low-volume centers inherently have worse CABG outcomes can be debated, but either way "our findings highlight the increasing role of low-volume hospitals in the provision of CABG surgery," Dr. Epstein and his associates said.
The final trend in coronary revascularizations revealed in these data was the marked surge in PCI procedures using drug-eluting stents soon after two devices were approved by the Food and Drug Administration in 2003.
By mid-2005, 90% of PCI procedures involved drug-eluting stents, reflecting "a high level of clinician enthusiasm" for the devices.
This peak was soon followed by a marked decline after the publication of safety concerns such as late in-stent thrombosis, "as well as increasing clinician awareness of the imperative for ... adherence to long-duration antiplatelet therapy."
By the beginning of 2008, only 61% of PCI procedures involved placement of drug-eluting stents, but that rate increased steadily during that year, which also saw the adoption of second-generation stents that carried lower restenosis rates.
"An important implication of this volatility is that thousands of patients may have received drug-eluting stents during the peak years who would have received bare-metal stents [in later years].
"Whether these patients were appropriately treated ... during these years of ?high enthusiasm? for drug-eluting stents is uncertain," the investigators noted.
This study was supported by the National Heart, Lung, and Blood Institute; the Agency for Healthcare Research and Quality; and the Pennsylvania Department of Health. ☐
The rate of coronary artery bypass grafting performed in U.S. hospitals declined by approximately one-third between 2001 and 2008, according to an analysis of the Agency for Healthcare Research and Quality database.
During the same period, the rate of percutaneous coronary interventions (PCIs) showed a far more modest decrease.
"Our data imply a sizeable shift in cardiovascular clinical practice patterns away from surgical treatment toward percutaneous, catheter-based interventions," said Andrew J. Epstein, Ph.D., of the Philadelphia Veterans Affairs? Center for Health Equity Research and Promotion and the University of Pennsylvania, and his associates.
Given that coronary artery bypass grafting remains the better choice for patients with previously untreated three-vessel or left main coronary artery disease, according to the results of the SYNTAX trial (N. Engl. J. Med. 2009;360:961-72), it appears that CABG is being underused, the authors wrote.
It seems likely that in recent years, "patients who would have been optimally treated with CABG surgery were instead treated with PCI," they noted.
To assess temporal trends in coronary revascularization procedures, the investigators examined a nationally representative sample of hospitalization claims using an Agency for Healthcare Research and Quality database.
The database includes discharge data from approximately 1,000 nonfederal hospitals in 42 states, which covers 20% of U.S. hospitals and allows accurate estimates for the entire population of hospitalized patients, regardless of payer or insurance status.
Between 2001 and 2008, the total number of coronary revascularizations decreased "modestly," by approximately 15%.
There was a "substantial," statistically significant, 38% decrease in the annual rate of CABG surgery, from 1,742 per million adults in the first year of the study period to 1,081 per million in the final year.
This decline was roughly linear throughout the 8-year study period, suggesting that it "was not triggered by any single event occurring during the past decade, such as the introduction of competing technologies, advances in CABG surgical techniques, publication of clinical trials, or issuance of clinical guidelines."
CABG procedures decreased across all sex, age, racial, and regional subgroups.
In contrast, the PCI rate remained fairly constant, showing a "modest" 4% decrease from 3,827 per million adults per year in the first year of the study to 3,667 in the final year.
"Projected to the entire U.S. population, these rate changes implied that 130,000 fewer CABG surgeries were performed in 2008 compared to 2001," Dr. Epstein and his colleagues noted (JAMA 2011;305:1769-76).
The data did not allow the researchers to distinguish which patients may have been more appropriate candidates for CABG than for PCI, so "it cannot be known with certainty whether physicians were increasingly substituting PCI for CABG surgery during the past decade. ... [But] our findings suggest the possibility that several thousand patients who underwent PCI in 2008 would have undergone CABG surgery had patterns of care not changed markedly," they said.
The preferences of patients were also not discernible from the data, lead investigator Dr. Peter W. Groeneveld said in an interview. "However, if patient preference [for PCI vs. CABG] was the driving factor, there would have to be some reason that PCI was even more preferable to patients in 2008 than it was in 2001.
This scenario seems unlikely since the procedures haven?t changed that much," said Dr. Groeneveld, assistant professor of medicine at the University of Pennsylvania and staff physician at the Philadelphia Veterans Affairs Medical Center.
Another important finding was that during this interval, the number of hospitals providing CABG increased. Combined with the drop in the number of CABG surgeries, this resulted in a 28% decline in the median caseload per hospital, "and a substantial increase in the number of hospitals that provided fewer than 100 CABG surgeries per year."
Whether or not low-volume centers inherently have worse CABG outcomes can be debated, but either way "our findings highlight the increasing role of low-volume hospitals in the provision of CABG surgery," Dr. Epstein and his associates said.
The final trend in coronary revascularizations revealed in these data was the marked surge in PCI procedures using drug-eluting stents soon after two devices were approved by the Food and Drug Administration in 2003.
By mid-2005, 90% of PCI procedures involved drug-eluting stents, reflecting "a high level of clinician enthusiasm" for the devices.
This peak was soon followed by a marked decline after the publication of safety concerns such as late in-stent thrombosis, "as well as increasing clinician awareness of the imperative for ... adherence to long-duration antiplatelet therapy."
By the beginning of 2008, only 61% of PCI procedures involved placement of drug-eluting stents, but that rate increased steadily during that year, which also saw the adoption of second-generation stents that carried lower restenosis rates.
"An important implication of this volatility is that thousands of patients may have received drug-eluting stents during the peak years who would have received bare-metal stents [in later years].
"Whether these patients were appropriately treated ... during these years of ?high enthusiasm? for drug-eluting stents is uncertain," the investigators noted.
This study was supported by the National Heart, Lung, and Blood Institute; the Agency for Healthcare Research and Quality; and the Pennsylvania Department of Health. ☐
The rate of coronary artery bypass grafting performed in U.S. hospitals declined by approximately one-third between 2001 and 2008, according to an analysis of the Agency for Healthcare Research and Quality database.
During the same period, the rate of percutaneous coronary interventions (PCIs) showed a far more modest decrease.
"Our data imply a sizeable shift in cardiovascular clinical practice patterns away from surgical treatment toward percutaneous, catheter-based interventions," said Andrew J. Epstein, Ph.D., of the Philadelphia Veterans Affairs? Center for Health Equity Research and Promotion and the University of Pennsylvania, and his associates.
Given that coronary artery bypass grafting remains the better choice for patients with previously untreated three-vessel or left main coronary artery disease, according to the results of the SYNTAX trial (N. Engl. J. Med. 2009;360:961-72), it appears that CABG is being underused, the authors wrote.
It seems likely that in recent years, "patients who would have been optimally treated with CABG surgery were instead treated with PCI," they noted.
To assess temporal trends in coronary revascularization procedures, the investigators examined a nationally representative sample of hospitalization claims using an Agency for Healthcare Research and Quality database.
The database includes discharge data from approximately 1,000 nonfederal hospitals in 42 states, which covers 20% of U.S. hospitals and allows accurate estimates for the entire population of hospitalized patients, regardless of payer or insurance status.
Between 2001 and 2008, the total number of coronary revascularizations decreased "modestly," by approximately 15%.
There was a "substantial," statistically significant, 38% decrease in the annual rate of CABG surgery, from 1,742 per million adults in the first year of the study period to 1,081 per million in the final year.
This decline was roughly linear throughout the 8-year study period, suggesting that it "was not triggered by any single event occurring during the past decade, such as the introduction of competing technologies, advances in CABG surgical techniques, publication of clinical trials, or issuance of clinical guidelines."
CABG procedures decreased across all sex, age, racial, and regional subgroups.
In contrast, the PCI rate remained fairly constant, showing a "modest" 4% decrease from 3,827 per million adults per year in the first year of the study to 3,667 in the final year.
"Projected to the entire U.S. population, these rate changes implied that 130,000 fewer CABG surgeries were performed in 2008 compared to 2001," Dr. Epstein and his colleagues noted (JAMA 2011;305:1769-76).
The data did not allow the researchers to distinguish which patients may have been more appropriate candidates for CABG than for PCI, so "it cannot be known with certainty whether physicians were increasingly substituting PCI for CABG surgery during the past decade. ... [But] our findings suggest the possibility that several thousand patients who underwent PCI in 2008 would have undergone CABG surgery had patterns of care not changed markedly," they said.
The preferences of patients were also not discernible from the data, lead investigator Dr. Peter W. Groeneveld said in an interview. "However, if patient preference [for PCI vs. CABG] was the driving factor, there would have to be some reason that PCI was even more preferable to patients in 2008 than it was in 2001.
This scenario seems unlikely since the procedures haven?t changed that much," said Dr. Groeneveld, assistant professor of medicine at the University of Pennsylvania and staff physician at the Philadelphia Veterans Affairs Medical Center.
Another important finding was that during this interval, the number of hospitals providing CABG increased. Combined with the drop in the number of CABG surgeries, this resulted in a 28% decline in the median caseload per hospital, "and a substantial increase in the number of hospitals that provided fewer than 100 CABG surgeries per year."
Whether or not low-volume centers inherently have worse CABG outcomes can be debated, but either way "our findings highlight the increasing role of low-volume hospitals in the provision of CABG surgery," Dr. Epstein and his associates said.
The final trend in coronary revascularizations revealed in these data was the marked surge in PCI procedures using drug-eluting stents soon after two devices were approved by the Food and Drug Administration in 2003.
By mid-2005, 90% of PCI procedures involved drug-eluting stents, reflecting "a high level of clinician enthusiasm" for the devices.
This peak was soon followed by a marked decline after the publication of safety concerns such as late in-stent thrombosis, "as well as increasing clinician awareness of the imperative for ... adherence to long-duration antiplatelet therapy."
By the beginning of 2008, only 61% of PCI procedures involved placement of drug-eluting stents, but that rate increased steadily during that year, which also saw the adoption of second-generation stents that carried lower restenosis rates.
"An important implication of this volatility is that thousands of patients may have received drug-eluting stents during the peak years who would have received bare-metal stents [in later years].
"Whether these patients were appropriately treated ... during these years of ?high enthusiasm? for drug-eluting stents is uncertain," the investigators noted.
This study was supported by the National Heart, Lung, and Blood Institute; the Agency for Healthcare Research and Quality; and the Pennsylvania Department of Health. ☐
Major Finding: The rate of CABG surgeries declined by approximately one-third and that of PCI procedures fell by 4% between 2001 and 2008, while the number of hospitals providing CABG increased by 12% and the number providing PCI rose by 26% during the same period.
Data Source: A nationwide serial cross-sectional study of time trends in coronary revascularization procedures.
Disclosures: This study was supported by the National Heart, Lung, and Blood Institute; the Agency for Healthcare Research and Quality; and the Pennsylvania Department of Health.
Most Stable CAD Goes Right to PCI
Contrary to clinical practice guidelines and simple logic, most patients who have stable coronary artery disease are not given optimal medical therapy before undergoing percutaneous coronary intervention, according to a recent study reported in JAMA.
In March 2007, "the most definitive randomized trial" comparing percutaneous coronary intervention (PCI) to optimal medical therapy, determined that PCI is no more effective than drug treatment at preventing MI or death in stable CAD. But even with this evidence, there was little change in the pattern of stable CAD patients going straight to PCI, said Dr. William B. Borden of Weill Cornell Medical College in New York, and his associates.
Dr. Borden and his colleagues assessed the practice patterns regarding the use of optimal medical therapy before and after PCI using data obtained from the national CathPCI Registry.
The researchers examined a 19-month interval occurring before publication of the trial results of Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) (N. Engl. J. Med. 2007;356:1503-16) and a 24-month period occuring afterward, to determine whether physicians had been inspired to transfer those findings into clinical practice.
The study population comprised 467,211 patients treated at 1,013 U.S. hospitals, which constituted about 28% of the total CathPCI population during the study period.
Optimal medical therapy was defined as being prescribed aspirin, a beta-blocker, and a statin before PCI and being prescribed aspirin or thienopyridine, a beta-blocker, a statin, and an ACE inhibitor or angiotensin receptor blocker after PCI, or having specific contraindications to these medications.
Overall, fewer than half of PCI patients ? 45% ? received optimal medical therapy before undergoing PCI. Current guidelines recommend maximizing medical therapy because that often relieves symptoms, obviating the need for PCI.
The rates of optimal medical therapy increased only slightly after publication of the COURAGE results, from 43% to 45%. This increase "was of little clinical significance," the investigators said (JAMA 2011:305:1882-9).
Dr. Borden disclosed ties to the pharmaceutical Kowa Company.
Contrary to clinical practice guidelines and simple logic, most patients who have stable coronary artery disease are not given optimal medical therapy before undergoing percutaneous coronary intervention, according to a recent study reported in JAMA.
In March 2007, "the most definitive randomized trial" comparing percutaneous coronary intervention (PCI) to optimal medical therapy, determined that PCI is no more effective than drug treatment at preventing MI or death in stable CAD. But even with this evidence, there was little change in the pattern of stable CAD patients going straight to PCI, said Dr. William B. Borden of Weill Cornell Medical College in New York, and his associates.
Dr. Borden and his colleagues assessed the practice patterns regarding the use of optimal medical therapy before and after PCI using data obtained from the national CathPCI Registry.
The researchers examined a 19-month interval occurring before publication of the trial results of Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) (N. Engl. J. Med. 2007;356:1503-16) and a 24-month period occuring afterward, to determine whether physicians had been inspired to transfer those findings into clinical practice.
The study population comprised 467,211 patients treated at 1,013 U.S. hospitals, which constituted about 28% of the total CathPCI population during the study period.
Optimal medical therapy was defined as being prescribed aspirin, a beta-blocker, and a statin before PCI and being prescribed aspirin or thienopyridine, a beta-blocker, a statin, and an ACE inhibitor or angiotensin receptor blocker after PCI, or having specific contraindications to these medications.
Overall, fewer than half of PCI patients ? 45% ? received optimal medical therapy before undergoing PCI. Current guidelines recommend maximizing medical therapy because that often relieves symptoms, obviating the need for PCI.
The rates of optimal medical therapy increased only slightly after publication of the COURAGE results, from 43% to 45%. This increase "was of little clinical significance," the investigators said (JAMA 2011:305:1882-9).
Dr. Borden disclosed ties to the pharmaceutical Kowa Company.
Contrary to clinical practice guidelines and simple logic, most patients who have stable coronary artery disease are not given optimal medical therapy before undergoing percutaneous coronary intervention, according to a recent study reported in JAMA.
In March 2007, "the most definitive randomized trial" comparing percutaneous coronary intervention (PCI) to optimal medical therapy, determined that PCI is no more effective than drug treatment at preventing MI or death in stable CAD. But even with this evidence, there was little change in the pattern of stable CAD patients going straight to PCI, said Dr. William B. Borden of Weill Cornell Medical College in New York, and his associates.
Dr. Borden and his colleagues assessed the practice patterns regarding the use of optimal medical therapy before and after PCI using data obtained from the national CathPCI Registry.
The researchers examined a 19-month interval occurring before publication of the trial results of Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) (N. Engl. J. Med. 2007;356:1503-16) and a 24-month period occuring afterward, to determine whether physicians had been inspired to transfer those findings into clinical practice.
The study population comprised 467,211 patients treated at 1,013 U.S. hospitals, which constituted about 28% of the total CathPCI population during the study period.
Optimal medical therapy was defined as being prescribed aspirin, a beta-blocker, and a statin before PCI and being prescribed aspirin or thienopyridine, a beta-blocker, a statin, and an ACE inhibitor or angiotensin receptor blocker after PCI, or having specific contraindications to these medications.
Overall, fewer than half of PCI patients ? 45% ? received optimal medical therapy before undergoing PCI. Current guidelines recommend maximizing medical therapy because that often relieves symptoms, obviating the need for PCI.
The rates of optimal medical therapy increased only slightly after publication of the COURAGE results, from 43% to 45%. This increase "was of little clinical significance," the investigators said (JAMA 2011:305:1882-9).
Dr. Borden disclosed ties to the pharmaceutical Kowa Company.