User login
Associate Fellows: Apply now for ACS Fellowship
Associate Fellows who are interested in pursuing the next level of membership and who meet the criteria for Fellowship are encouraged to start the application process now.
Applications for American College of Surgeons (ACS) Fellowship for induction at the 2018 Clinical Congress in Boston, MA, are due December 1, 2017.
ACS Fellowship is granted to physicians who devote their practice entirely to surgical services and who agree to practice in accordance with the College’s professional and ethical standards.
The College’s Fellowship Pledge and Statements on Principles, found on the ACS website at facs.org, outline the ACS standards of practice. All ACS Fellows and applicants for Fellowship are expected to adhere to these standards.
Surgeons voluntarily submit applications for Fellowship, thereby inviting an evaluation of their practice by their peers. In evaluating the eligibility of Fellowship applicants, the College investigates each applicant’s entire surgical practice. Applicants for Fellowship are required to provide to the appointed committees of the College all information deemed necessary for the investigation and evaluation of their surgical practice.
It is our intention that all Associate Fellows consider applying for Fellowship within the first six years of their surgical practice. To encourage that transition, Associate Fellowship is limited to surgeons who have been in practice less than six years.
Requirements
The basic requirements for Domestic (U.S. and Canada) Fellowship are as follows:
• Certification by an appropriate American Board of Medical Specialties surgical specialty board, an American Osteopathic Association surgical specialty board, or the Royal College of Surgeons in Canada
• One year of surgical practice after the completion of all formal training (including fellowships)
• A current appointment at a primary hospital with no reportable action pending
A full list of the domestic requirements can be accessed at facs.org/member-services/join/fellows. The list of requirements for International Fellowship is online at facs.org/member-services/join/international.
Associate Fellows who are current with their membership dues may apply online for free by visiting facs.org/member-services/join and clicking on the link for either Fellow or International Fellow. You will need your log-in information to access the application. If you do not have your log-in information, contact the College’s Member Services staff at 800-293-9623 or via e-mail at [email protected].
The application requests basic information regarding licensure, certification, education, and hospital affiliations. Applicants also are asked to provide the names of five Fellows of the College, preferably from their current practice location, to serve as references. Applicants do not need to request letters of recommendation; simply list the names in your application, and the College staff will contact your references.
If you need assistance finding ACS Fellows in your area, go to facs.org and click on the “Find a Surgeon” button.
When your application is processed, you will receive an e-mail notification providing details about the application timeline along with a request for your surgical case list.
All Fellowship applicants are required to participate in a personal interview by an ACS committee in their local area. Exceptions are made for military applicants. Following the interview, you will receive notification by July 15 of the action taken on your application. Approved applicants are designated as Initiates to be inducted as Fellows during the Convocation Ceremony at the Clinical Congress.
Contact Member Services with questions at any time throughout the application process. We look forward to you becoming a Fellow of the American College of Surgeons.
Associate Fellows who are interested in pursuing the next level of membership and who meet the criteria for Fellowship are encouraged to start the application process now.
Applications for American College of Surgeons (ACS) Fellowship for induction at the 2018 Clinical Congress in Boston, MA, are due December 1, 2017.
ACS Fellowship is granted to physicians who devote their practice entirely to surgical services and who agree to practice in accordance with the College’s professional and ethical standards.
The College’s Fellowship Pledge and Statements on Principles, found on the ACS website at facs.org, outline the ACS standards of practice. All ACS Fellows and applicants for Fellowship are expected to adhere to these standards.
Surgeons voluntarily submit applications for Fellowship, thereby inviting an evaluation of their practice by their peers. In evaluating the eligibility of Fellowship applicants, the College investigates each applicant’s entire surgical practice. Applicants for Fellowship are required to provide to the appointed committees of the College all information deemed necessary for the investigation and evaluation of their surgical practice.
It is our intention that all Associate Fellows consider applying for Fellowship within the first six years of their surgical practice. To encourage that transition, Associate Fellowship is limited to surgeons who have been in practice less than six years.
Requirements
The basic requirements for Domestic (U.S. and Canada) Fellowship are as follows:
• Certification by an appropriate American Board of Medical Specialties surgical specialty board, an American Osteopathic Association surgical specialty board, or the Royal College of Surgeons in Canada
• One year of surgical practice after the completion of all formal training (including fellowships)
• A current appointment at a primary hospital with no reportable action pending
A full list of the domestic requirements can be accessed at facs.org/member-services/join/fellows. The list of requirements for International Fellowship is online at facs.org/member-services/join/international.
Associate Fellows who are current with their membership dues may apply online for free by visiting facs.org/member-services/join and clicking on the link for either Fellow or International Fellow. You will need your log-in information to access the application. If you do not have your log-in information, contact the College’s Member Services staff at 800-293-9623 or via e-mail at [email protected].
The application requests basic information regarding licensure, certification, education, and hospital affiliations. Applicants also are asked to provide the names of five Fellows of the College, preferably from their current practice location, to serve as references. Applicants do not need to request letters of recommendation; simply list the names in your application, and the College staff will contact your references.
If you need assistance finding ACS Fellows in your area, go to facs.org and click on the “Find a Surgeon” button.
When your application is processed, you will receive an e-mail notification providing details about the application timeline along with a request for your surgical case list.
All Fellowship applicants are required to participate in a personal interview by an ACS committee in their local area. Exceptions are made for military applicants. Following the interview, you will receive notification by July 15 of the action taken on your application. Approved applicants are designated as Initiates to be inducted as Fellows during the Convocation Ceremony at the Clinical Congress.
Contact Member Services with questions at any time throughout the application process. We look forward to you becoming a Fellow of the American College of Surgeons.
Associate Fellows who are interested in pursuing the next level of membership and who meet the criteria for Fellowship are encouraged to start the application process now.
Applications for American College of Surgeons (ACS) Fellowship for induction at the 2018 Clinical Congress in Boston, MA, are due December 1, 2017.
ACS Fellowship is granted to physicians who devote their practice entirely to surgical services and who agree to practice in accordance with the College’s professional and ethical standards.
The College’s Fellowship Pledge and Statements on Principles, found on the ACS website at facs.org, outline the ACS standards of practice. All ACS Fellows and applicants for Fellowship are expected to adhere to these standards.
Surgeons voluntarily submit applications for Fellowship, thereby inviting an evaluation of their practice by their peers. In evaluating the eligibility of Fellowship applicants, the College investigates each applicant’s entire surgical practice. Applicants for Fellowship are required to provide to the appointed committees of the College all information deemed necessary for the investigation and evaluation of their surgical practice.
It is our intention that all Associate Fellows consider applying for Fellowship within the first six years of their surgical practice. To encourage that transition, Associate Fellowship is limited to surgeons who have been in practice less than six years.
Requirements
The basic requirements for Domestic (U.S. and Canada) Fellowship are as follows:
• Certification by an appropriate American Board of Medical Specialties surgical specialty board, an American Osteopathic Association surgical specialty board, or the Royal College of Surgeons in Canada
• One year of surgical practice after the completion of all formal training (including fellowships)
• A current appointment at a primary hospital with no reportable action pending
A full list of the domestic requirements can be accessed at facs.org/member-services/join/fellows. The list of requirements for International Fellowship is online at facs.org/member-services/join/international.
Associate Fellows who are current with their membership dues may apply online for free by visiting facs.org/member-services/join and clicking on the link for either Fellow or International Fellow. You will need your log-in information to access the application. If you do not have your log-in information, contact the College’s Member Services staff at 800-293-9623 or via e-mail at [email protected].
The application requests basic information regarding licensure, certification, education, and hospital affiliations. Applicants also are asked to provide the names of five Fellows of the College, preferably from their current practice location, to serve as references. Applicants do not need to request letters of recommendation; simply list the names in your application, and the College staff will contact your references.
If you need assistance finding ACS Fellows in your area, go to facs.org and click on the “Find a Surgeon” button.
When your application is processed, you will receive an e-mail notification providing details about the application timeline along with a request for your surgical case list.
All Fellowship applicants are required to participate in a personal interview by an ACS committee in their local area. Exceptions are made for military applicants. Following the interview, you will receive notification by July 15 of the action taken on your application. Approved applicants are designated as Initiates to be inducted as Fellows during the Convocation Ceremony at the Clinical Congress.
Contact Member Services with questions at any time throughout the application process. We look forward to you becoming a Fellow of the American College of Surgeons.
Dr. Henri Ford Accorded Honorary Fellowship in RCSEng
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Dr. Thomas Starzl, the “Father of Transplantation,” passes away
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
ACS launches AHRQ Safety Program for ERAS
The American College of Surgeons (ACS), in collaboration with the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD, has launched the AHRQ (Agency for Healthcare Research and Quality) Safety Program for Enhanced Recovery after Surgery (ERAS). This new surgical quality improvement program is funded and guided by AHRQ.
The AHRQ Safety Program for ERAS will support hospitals in implementing perioperative evidence-based protocols to meaningfully improve clinical outcomes, reduce health care utilization, and improve the patient experience. This program aims to enroll at least 750 hospitals throughout the five-year contract. Hospitals within the U.S., Puerto Rico, and the District of Columbia are eligible to participate across five service lines: colorectal, orthopaedic, bariatric, gynecology, and emergency general surgery.
Participating hospitals will have access to the international leaders in ERAS, including representatives of surgery, anesthesiology, and nursing; prototype ERAS protocols developed for five procedures based on up-to-date evidence review; literature to support protocols; tools and educational materials to facilitate implementation; quality improvement specialist support; and coaching calls to support hospital work.
Program enrollment will begin in spring 2017. For more information, contact [email protected].
The American College of Surgeons (ACS), in collaboration with the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD, has launched the AHRQ (Agency for Healthcare Research and Quality) Safety Program for Enhanced Recovery after Surgery (ERAS). This new surgical quality improvement program is funded and guided by AHRQ.
The AHRQ Safety Program for ERAS will support hospitals in implementing perioperative evidence-based protocols to meaningfully improve clinical outcomes, reduce health care utilization, and improve the patient experience. This program aims to enroll at least 750 hospitals throughout the five-year contract. Hospitals within the U.S., Puerto Rico, and the District of Columbia are eligible to participate across five service lines: colorectal, orthopaedic, bariatric, gynecology, and emergency general surgery.
Participating hospitals will have access to the international leaders in ERAS, including representatives of surgery, anesthesiology, and nursing; prototype ERAS protocols developed for five procedures based on up-to-date evidence review; literature to support protocols; tools and educational materials to facilitate implementation; quality improvement specialist support; and coaching calls to support hospital work.
Program enrollment will begin in spring 2017. For more information, contact [email protected].
The American College of Surgeons (ACS), in collaboration with the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, Baltimore, MD, has launched the AHRQ (Agency for Healthcare Research and Quality) Safety Program for Enhanced Recovery after Surgery (ERAS). This new surgical quality improvement program is funded and guided by AHRQ.
The AHRQ Safety Program for ERAS will support hospitals in implementing perioperative evidence-based protocols to meaningfully improve clinical outcomes, reduce health care utilization, and improve the patient experience. This program aims to enroll at least 750 hospitals throughout the five-year contract. Hospitals within the U.S., Puerto Rico, and the District of Columbia are eligible to participate across five service lines: colorectal, orthopaedic, bariatric, gynecology, and emergency general surgery.
Participating hospitals will have access to the international leaders in ERAS, including representatives of surgery, anesthesiology, and nursing; prototype ERAS protocols developed for five procedures based on up-to-date evidence review; literature to support protocols; tools and educational materials to facilitate implementation; quality improvement specialist support; and coaching calls to support hospital work.
Program enrollment will begin in spring 2017. For more information, contact [email protected].
Surgical History Group student and resident papers now available online
The Surgical History Group (SHG) of the American College of Surgeons (ACS) has unveiled the inaugural issue of the Bulletin of the Surgical History Group: Papers from the 2016 Poster Competition. This publication is a compendium of articles based on abstracts that medical students and residents submitted for the SHG’s poster competition at Clinical Congress 2016 in Washington, DC.
The SHG sponsors a poster competition at the annual Clinical Congress, featuring the scholarly work of students and residents. Submissions cover a range of surgical history topics.
More than 40 abstracts were submitted for presentation at Clinical Congress 2016 in Washington, DC. A panel of judges led by J. Patrick O’Leary, MD, FACS, and Patrick Greiffenstein, MD, FACS, Chair and Co-Chair, respectively, of the Poster Competition Committee, selected 21 posters for the program and chose two posters among the high-quality entries for top prizes. The SHG decided that the students’ and residents’ scholarship deserved wider distribution in a more permanent format than posters. All participants were invited to submit their work in written form for this collection of articles available for the study and enjoyment of both Fellows and the public interested in the history of surgery.
The e-bulletin can be accessed on the SHG website at facs.org/about-acs/archives/shg.
The Surgical History Group (SHG) of the American College of Surgeons (ACS) has unveiled the inaugural issue of the Bulletin of the Surgical History Group: Papers from the 2016 Poster Competition. This publication is a compendium of articles based on abstracts that medical students and residents submitted for the SHG’s poster competition at Clinical Congress 2016 in Washington, DC.
The SHG sponsors a poster competition at the annual Clinical Congress, featuring the scholarly work of students and residents. Submissions cover a range of surgical history topics.
More than 40 abstracts were submitted for presentation at Clinical Congress 2016 in Washington, DC. A panel of judges led by J. Patrick O’Leary, MD, FACS, and Patrick Greiffenstein, MD, FACS, Chair and Co-Chair, respectively, of the Poster Competition Committee, selected 21 posters for the program and chose two posters among the high-quality entries for top prizes. The SHG decided that the students’ and residents’ scholarship deserved wider distribution in a more permanent format than posters. All participants were invited to submit their work in written form for this collection of articles available for the study and enjoyment of both Fellows and the public interested in the history of surgery.
The e-bulletin can be accessed on the SHG website at facs.org/about-acs/archives/shg.
The Surgical History Group (SHG) of the American College of Surgeons (ACS) has unveiled the inaugural issue of the Bulletin of the Surgical History Group: Papers from the 2016 Poster Competition. This publication is a compendium of articles based on abstracts that medical students and residents submitted for the SHG’s poster competition at Clinical Congress 2016 in Washington, DC.
The SHG sponsors a poster competition at the annual Clinical Congress, featuring the scholarly work of students and residents. Submissions cover a range of surgical history topics.
More than 40 abstracts were submitted for presentation at Clinical Congress 2016 in Washington, DC. A panel of judges led by J. Patrick O’Leary, MD, FACS, and Patrick Greiffenstein, MD, FACS, Chair and Co-Chair, respectively, of the Poster Competition Committee, selected 21 posters for the program and chose two posters among the high-quality entries for top prizes. The SHG decided that the students’ and residents’ scholarship deserved wider distribution in a more permanent format than posters. All participants were invited to submit their work in written form for this collection of articles available for the study and enjoyment of both Fellows and the public interested in the history of surgery.
The e-bulletin can be accessed on the SHG website at facs.org/about-acs/archives/shg.
ACS NSQIP conference gets new name, expanded focus
To provide a more comprehensive look at the American College of Surgeons (ACS) quality improvement efforts, the College has announced that the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference will now be the 2017 ACS Quality and Safety Conference. The meeting will take place July 21-24 at the New York Hilton Midtown, NY.
The annual ACS NSQIP conference has grown rapidly in recent years – the 2016 conference in San Diego, CA, drew nearly 1,500 surgeon champions, surgical clinical reviewers (SCRs), and other quality improvement professionals. The ACS Quality and Safety Conference will build on that success, featuring leaders in surgery as speakers and various presentations focused on ACS NSQIP, while offering expanded content on the following ACS Quality Programs:
• ACS NSQIP Pediatric
• Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program
• Children’s Surgery Verification™ Quality Improvement Program
• Surgeon Specific Registry
Achieving quality
The theme of the expanded conference, Achieving Quality: Present and Future, will serve as the basis of the meeting’s proceedings. To achieve the goal of improving quality, presenters and organizers are striving to accomplish the following objectives:
Provide a forum to share the most up-to-date knowledge pertaining to local, national, and international quality improvement initiatives in surgery.
Present methods used to analyze clinical registry data and demonstrate practical ways to use the data.
Assist hospitals in analyzing, managing, and interpreting data by providing education on proven methods that will empower hospitals to make a positive impact on patient care.
Enhance the learning experience by offering breakout sessions that educate attendees on topic areas of interest to them, with consideration of their level of experience in ACS quality improvement programs.
Conference highlights
In addition to talks from surgical leaders, the 2017 ACS Quality and Safety Conference will offer other notable events.
Keynote speaker Blake Haxton, a member of the 2016 U.S. Paralympic Team in rowing, will share his unique insight with attendees. Mr. Haxton contracted necrotizing fasciitis in March 2009, in his senior year of high school. The infection led to heart, lung, kidney, and liver failure, as well as the loss of both legs; however, after an intensive rehabilitation regimen, he was able to attend and graduate from college and law school.
Another conference highlight will be abstract competitions in four categories: Medical Student and Surgical Resident Abstract Competition, SCR Abstract Competition, Clinical Abstract Competition, and Abstract Poster Competition.
Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Director, ACS Division of Research and Optimal Patient Care, which oversees all ACS Quality Programs, is enthusiastic about the newly expanded ACS Quality and Safety Conference. “We are excited to have multiple quality programs of the American College of Surgeons coming together for this conference so that we can all learn how to get better, become more efficient, and provide high-value care in all types of settings,” Dr. Ko said. “This is the first time we’ve put together a conference like this, which we hope will be the first of many.”
More information about the 2017 ACS Quality and Safety Conference can be found at facs.org/quality-programs/quality-safety-conference.
To provide a more comprehensive look at the American College of Surgeons (ACS) quality improvement efforts, the College has announced that the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference will now be the 2017 ACS Quality and Safety Conference. The meeting will take place July 21-24 at the New York Hilton Midtown, NY.
The annual ACS NSQIP conference has grown rapidly in recent years – the 2016 conference in San Diego, CA, drew nearly 1,500 surgeon champions, surgical clinical reviewers (SCRs), and other quality improvement professionals. The ACS Quality and Safety Conference will build on that success, featuring leaders in surgery as speakers and various presentations focused on ACS NSQIP, while offering expanded content on the following ACS Quality Programs:
• ACS NSQIP Pediatric
• Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program
• Children’s Surgery Verification™ Quality Improvement Program
• Surgeon Specific Registry
Achieving quality
The theme of the expanded conference, Achieving Quality: Present and Future, will serve as the basis of the meeting’s proceedings. To achieve the goal of improving quality, presenters and organizers are striving to accomplish the following objectives:
Provide a forum to share the most up-to-date knowledge pertaining to local, national, and international quality improvement initiatives in surgery.
Present methods used to analyze clinical registry data and demonstrate practical ways to use the data.
Assist hospitals in analyzing, managing, and interpreting data by providing education on proven methods that will empower hospitals to make a positive impact on patient care.
Enhance the learning experience by offering breakout sessions that educate attendees on topic areas of interest to them, with consideration of their level of experience in ACS quality improvement programs.
Conference highlights
In addition to talks from surgical leaders, the 2017 ACS Quality and Safety Conference will offer other notable events.
Keynote speaker Blake Haxton, a member of the 2016 U.S. Paralympic Team in rowing, will share his unique insight with attendees. Mr. Haxton contracted necrotizing fasciitis in March 2009, in his senior year of high school. The infection led to heart, lung, kidney, and liver failure, as well as the loss of both legs; however, after an intensive rehabilitation regimen, he was able to attend and graduate from college and law school.
Another conference highlight will be abstract competitions in four categories: Medical Student and Surgical Resident Abstract Competition, SCR Abstract Competition, Clinical Abstract Competition, and Abstract Poster Competition.
Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Director, ACS Division of Research and Optimal Patient Care, which oversees all ACS Quality Programs, is enthusiastic about the newly expanded ACS Quality and Safety Conference. “We are excited to have multiple quality programs of the American College of Surgeons coming together for this conference so that we can all learn how to get better, become more efficient, and provide high-value care in all types of settings,” Dr. Ko said. “This is the first time we’ve put together a conference like this, which we hope will be the first of many.”
More information about the 2017 ACS Quality and Safety Conference can be found at facs.org/quality-programs/quality-safety-conference.
To provide a more comprehensive look at the American College of Surgeons (ACS) quality improvement efforts, the College has announced that the ACS National Surgical Quality Improvement Program (ACS NSQIP®) Annual Conference will now be the 2017 ACS Quality and Safety Conference. The meeting will take place July 21-24 at the New York Hilton Midtown, NY.
The annual ACS NSQIP conference has grown rapidly in recent years – the 2016 conference in San Diego, CA, drew nearly 1,500 surgeon champions, surgical clinical reviewers (SCRs), and other quality improvement professionals. The ACS Quality and Safety Conference will build on that success, featuring leaders in surgery as speakers and various presentations focused on ACS NSQIP, while offering expanded content on the following ACS Quality Programs:
• ACS NSQIP Pediatric
• Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program
• Children’s Surgery Verification™ Quality Improvement Program
• Surgeon Specific Registry
Achieving quality
The theme of the expanded conference, Achieving Quality: Present and Future, will serve as the basis of the meeting’s proceedings. To achieve the goal of improving quality, presenters and organizers are striving to accomplish the following objectives:
Provide a forum to share the most up-to-date knowledge pertaining to local, national, and international quality improvement initiatives in surgery.
Present methods used to analyze clinical registry data and demonstrate practical ways to use the data.
Assist hospitals in analyzing, managing, and interpreting data by providing education on proven methods that will empower hospitals to make a positive impact on patient care.
Enhance the learning experience by offering breakout sessions that educate attendees on topic areas of interest to them, with consideration of their level of experience in ACS quality improvement programs.
Conference highlights
In addition to talks from surgical leaders, the 2017 ACS Quality and Safety Conference will offer other notable events.
Keynote speaker Blake Haxton, a member of the 2016 U.S. Paralympic Team in rowing, will share his unique insight with attendees. Mr. Haxton contracted necrotizing fasciitis in March 2009, in his senior year of high school. The infection led to heart, lung, kidney, and liver failure, as well as the loss of both legs; however, after an intensive rehabilitation regimen, he was able to attend and graduate from college and law school.
Another conference highlight will be abstract competitions in four categories: Medical Student and Surgical Resident Abstract Competition, SCR Abstract Competition, Clinical Abstract Competition, and Abstract Poster Competition.
Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Director, ACS Division of Research and Optimal Patient Care, which oversees all ACS Quality Programs, is enthusiastic about the newly expanded ACS Quality and Safety Conference. “We are excited to have multiple quality programs of the American College of Surgeons coming together for this conference so that we can all learn how to get better, become more efficient, and provide high-value care in all types of settings,” Dr. Ko said. “This is the first time we’ve put together a conference like this, which we hope will be the first of many.”
More information about the 2017 ACS Quality and Safety Conference can be found at facs.org/quality-programs/quality-safety-conference.
Post-election health policy takes center stage at AMA HOD meeting
The American Medical Association (AMA) Interim House of Delegates (HOD) meeting took place November 12–15, 2016, in Orlando, FL. A total of 530 state medical society and specialty society delegates, including the six members of the American College of Surgeons’ (ACS) delegation, debated the policy implications of 32 reports and 101 resolutions. Occurring within a week of the national elections, a central focus of the meeting was the uncertainty about the future of the Affordable Care Act (ACA). On the other hand, the Stop the Bleed® program received an enthusiastic reception.
ACS delegation sponsors Stop the Bleed skills course
AMA meetings provide an opportunity for the ACS delegates to share College initiatives with physician leaders from a breadth of geographic locations, specialties, and career stages. In this spirit, ACS delegates, all of whom are Stop the Bleed instructors, along with Leonard J. Weireter, MD, FACS, Vice-Chair, ACS Committee on Trauma, presented the skills course to 125 practicing physicians, residents, and medical student delegates. Through four half-hour sessions, participants refreshed their hands-on skills in bleeding control and became advocates for bringing the course back to their communities. Course success was recognized before the entire HOD.
Surgical Caucus focuses on mass casualty readiness
The Surgical Caucus sponsored a one-hour educational session, The Hartford Consensus: Strategies to Enhance Survival in Active Shooter and Intentional Mass Casualty Events. Dr. Weireter shared an overview of the Hartford Consensus recommendations for effective response to active shooter and mass casualty events and highlighted the value of the Stop the Bleed course in improving survival of casualties from these events.
Orlando trauma surgeon Michael Cheatham, MD, FACS, gave a synopsis of the Orlando Regional Medical Center response to the Pulse nightclub shooting in June 2016. In addition to conducting relevant readiness drills, he emphasized the importance of including casualty family assistance and post-event hospital staff counseling in mass casualty plans.
At this meeting, the AMA endorsed recommendations from a 2015 call to action by eight health professional organizations and the American Bar Association to reduce the public health consequences of firearm-related injury.
U.S. elections put health care system in spotlight
Five resolutions covering a spectrum of opinions about AMA engagement in ACA reform were discussed. The five proposals were consolidated into one adopted resolution, which calls for the AMA, in collaboration with state and specialty medical societies, to actively discuss the future of health care reform with the new presidential administration and Congress. AMA executive vice-president James Madera, MD, sent a letter to congressional leaders on January 3 emphasizing the AMA’s interest in proposals that “make coverage more affordable, provide greater choice, and increase the number of those insured.”
The ACS delegation focused on the ACS Health Care Reform General Principles, which promote a systems-based approach to health care quality and safety, patient access to surgical care, reduction of health care costs, and medical liability reform.
Maintenance of Certification
General disaffection with Maintenance of Certification (MOC) requirements persists in multiple specialties, with particular concerns related to its use in credentialing and privileging decisions. The HOD adopted a policy that directs the AMA to increase efforts to ensure that MOC does not become a requirement for insurance panel participation, state medical licensure, and medical staff membership (initial and ongoing).
Medical student and resident training
Delegates agreed with a need for formal leadership training during medical school. The AMA now advocates for the creation of leadership programs that emphasize experiential learning of skills necessary to lead inter-professional teams. Delegates also recognized the importance of having training program policies that support residents who are breastfeeding. As a result, the AMA will now work with appropriate professional regulatory organizations to put policies for protected times and locations for breastfeeding into program requirements.
Surgeon management of patients with perioperative pain
A resolution intended to reduce perioperative opioid consumption was introduced, calling for hospitals to adopt practices for perioperative pain management, which include services dedicated to acute pain management. This proposal generated a great deal of concern among surgical and anesthesiology delegates. The HOD appreciated that surgeons are trained to manage the perioperative pain of their patients and may consult for additional services as needed. Thus, existing AMA efforts to promote appropriate clinical use of opioid analgesics were reaffirmed in lieu of the resolution.
Next meeting
The next meeting of the AMA HOD is scheduled for June 10–14 in Chicago. This meeting will be the first since the inauguration of President Donald Trump, and the ACS delegates anticipate that national health care policy will again dominate the discussion. ACS members with suggestions for potential resolutions should forward them to Jon Sutton at [email protected].
ACS Delegation at the AMA HOD
• John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Ocala, FL
• Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
• Jacob Moalem, MD, FACS (also Young Physicians Section delegate), general surgery, Rochester, NY
• Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Vice-Chair, ACS Board of Regents
• Naveen F. Sangji, MD, general surgery resident, Boston, MA
• Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; Chair, AMA Council on Medical Education
Dr. Armstrong is a member of the American College of Surgeons (ACS) Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy, Washington, DC.
The American Medical Association (AMA) Interim House of Delegates (HOD) meeting took place November 12–15, 2016, in Orlando, FL. A total of 530 state medical society and specialty society delegates, including the six members of the American College of Surgeons’ (ACS) delegation, debated the policy implications of 32 reports and 101 resolutions. Occurring within a week of the national elections, a central focus of the meeting was the uncertainty about the future of the Affordable Care Act (ACA). On the other hand, the Stop the Bleed® program received an enthusiastic reception.
ACS delegation sponsors Stop the Bleed skills course
AMA meetings provide an opportunity for the ACS delegates to share College initiatives with physician leaders from a breadth of geographic locations, specialties, and career stages. In this spirit, ACS delegates, all of whom are Stop the Bleed instructors, along with Leonard J. Weireter, MD, FACS, Vice-Chair, ACS Committee on Trauma, presented the skills course to 125 practicing physicians, residents, and medical student delegates. Through four half-hour sessions, participants refreshed their hands-on skills in bleeding control and became advocates for bringing the course back to their communities. Course success was recognized before the entire HOD.
Surgical Caucus focuses on mass casualty readiness
The Surgical Caucus sponsored a one-hour educational session, The Hartford Consensus: Strategies to Enhance Survival in Active Shooter and Intentional Mass Casualty Events. Dr. Weireter shared an overview of the Hartford Consensus recommendations for effective response to active shooter and mass casualty events and highlighted the value of the Stop the Bleed course in improving survival of casualties from these events.
Orlando trauma surgeon Michael Cheatham, MD, FACS, gave a synopsis of the Orlando Regional Medical Center response to the Pulse nightclub shooting in June 2016. In addition to conducting relevant readiness drills, he emphasized the importance of including casualty family assistance and post-event hospital staff counseling in mass casualty plans.
At this meeting, the AMA endorsed recommendations from a 2015 call to action by eight health professional organizations and the American Bar Association to reduce the public health consequences of firearm-related injury.
U.S. elections put health care system in spotlight
Five resolutions covering a spectrum of opinions about AMA engagement in ACA reform were discussed. The five proposals were consolidated into one adopted resolution, which calls for the AMA, in collaboration with state and specialty medical societies, to actively discuss the future of health care reform with the new presidential administration and Congress. AMA executive vice-president James Madera, MD, sent a letter to congressional leaders on January 3 emphasizing the AMA’s interest in proposals that “make coverage more affordable, provide greater choice, and increase the number of those insured.”
The ACS delegation focused on the ACS Health Care Reform General Principles, which promote a systems-based approach to health care quality and safety, patient access to surgical care, reduction of health care costs, and medical liability reform.
Maintenance of Certification
General disaffection with Maintenance of Certification (MOC) requirements persists in multiple specialties, with particular concerns related to its use in credentialing and privileging decisions. The HOD adopted a policy that directs the AMA to increase efforts to ensure that MOC does not become a requirement for insurance panel participation, state medical licensure, and medical staff membership (initial and ongoing).
Medical student and resident training
Delegates agreed with a need for formal leadership training during medical school. The AMA now advocates for the creation of leadership programs that emphasize experiential learning of skills necessary to lead inter-professional teams. Delegates also recognized the importance of having training program policies that support residents who are breastfeeding. As a result, the AMA will now work with appropriate professional regulatory organizations to put policies for protected times and locations for breastfeeding into program requirements.
Surgeon management of patients with perioperative pain
A resolution intended to reduce perioperative opioid consumption was introduced, calling for hospitals to adopt practices for perioperative pain management, which include services dedicated to acute pain management. This proposal generated a great deal of concern among surgical and anesthesiology delegates. The HOD appreciated that surgeons are trained to manage the perioperative pain of their patients and may consult for additional services as needed. Thus, existing AMA efforts to promote appropriate clinical use of opioid analgesics were reaffirmed in lieu of the resolution.
Next meeting
The next meeting of the AMA HOD is scheduled for June 10–14 in Chicago. This meeting will be the first since the inauguration of President Donald Trump, and the ACS delegates anticipate that national health care policy will again dominate the discussion. ACS members with suggestions for potential resolutions should forward them to Jon Sutton at [email protected].
ACS Delegation at the AMA HOD
• John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Ocala, FL
• Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
• Jacob Moalem, MD, FACS (also Young Physicians Section delegate), general surgery, Rochester, NY
• Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Vice-Chair, ACS Board of Regents
• Naveen F. Sangji, MD, general surgery resident, Boston, MA
• Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; Chair, AMA Council on Medical Education
Dr. Armstrong is a member of the American College of Surgeons (ACS) Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy, Washington, DC.
The American Medical Association (AMA) Interim House of Delegates (HOD) meeting took place November 12–15, 2016, in Orlando, FL. A total of 530 state medical society and specialty society delegates, including the six members of the American College of Surgeons’ (ACS) delegation, debated the policy implications of 32 reports and 101 resolutions. Occurring within a week of the national elections, a central focus of the meeting was the uncertainty about the future of the Affordable Care Act (ACA). On the other hand, the Stop the Bleed® program received an enthusiastic reception.
ACS delegation sponsors Stop the Bleed skills course
AMA meetings provide an opportunity for the ACS delegates to share College initiatives with physician leaders from a breadth of geographic locations, specialties, and career stages. In this spirit, ACS delegates, all of whom are Stop the Bleed instructors, along with Leonard J. Weireter, MD, FACS, Vice-Chair, ACS Committee on Trauma, presented the skills course to 125 practicing physicians, residents, and medical student delegates. Through four half-hour sessions, participants refreshed their hands-on skills in bleeding control and became advocates for bringing the course back to their communities. Course success was recognized before the entire HOD.
Surgical Caucus focuses on mass casualty readiness
The Surgical Caucus sponsored a one-hour educational session, The Hartford Consensus: Strategies to Enhance Survival in Active Shooter and Intentional Mass Casualty Events. Dr. Weireter shared an overview of the Hartford Consensus recommendations for effective response to active shooter and mass casualty events and highlighted the value of the Stop the Bleed course in improving survival of casualties from these events.
Orlando trauma surgeon Michael Cheatham, MD, FACS, gave a synopsis of the Orlando Regional Medical Center response to the Pulse nightclub shooting in June 2016. In addition to conducting relevant readiness drills, he emphasized the importance of including casualty family assistance and post-event hospital staff counseling in mass casualty plans.
At this meeting, the AMA endorsed recommendations from a 2015 call to action by eight health professional organizations and the American Bar Association to reduce the public health consequences of firearm-related injury.
U.S. elections put health care system in spotlight
Five resolutions covering a spectrum of opinions about AMA engagement in ACA reform were discussed. The five proposals were consolidated into one adopted resolution, which calls for the AMA, in collaboration with state and specialty medical societies, to actively discuss the future of health care reform with the new presidential administration and Congress. AMA executive vice-president James Madera, MD, sent a letter to congressional leaders on January 3 emphasizing the AMA’s interest in proposals that “make coverage more affordable, provide greater choice, and increase the number of those insured.”
The ACS delegation focused on the ACS Health Care Reform General Principles, which promote a systems-based approach to health care quality and safety, patient access to surgical care, reduction of health care costs, and medical liability reform.
Maintenance of Certification
General disaffection with Maintenance of Certification (MOC) requirements persists in multiple specialties, with particular concerns related to its use in credentialing and privileging decisions. The HOD adopted a policy that directs the AMA to increase efforts to ensure that MOC does not become a requirement for insurance panel participation, state medical licensure, and medical staff membership (initial and ongoing).
Medical student and resident training
Delegates agreed with a need for formal leadership training during medical school. The AMA now advocates for the creation of leadership programs that emphasize experiential learning of skills necessary to lead inter-professional teams. Delegates also recognized the importance of having training program policies that support residents who are breastfeeding. As a result, the AMA will now work with appropriate professional regulatory organizations to put policies for protected times and locations for breastfeeding into program requirements.
Surgeon management of patients with perioperative pain
A resolution intended to reduce perioperative opioid consumption was introduced, calling for hospitals to adopt practices for perioperative pain management, which include services dedicated to acute pain management. This proposal generated a great deal of concern among surgical and anesthesiology delegates. The HOD appreciated that surgeons are trained to manage the perioperative pain of their patients and may consult for additional services as needed. Thus, existing AMA efforts to promote appropriate clinical use of opioid analgesics were reaffirmed in lieu of the resolution.
Next meeting
The next meeting of the AMA HOD is scheduled for June 10–14 in Chicago. This meeting will be the first since the inauguration of President Donald Trump, and the ACS delegates anticipate that national health care policy will again dominate the discussion. ACS members with suggestions for potential resolutions should forward them to Jon Sutton at [email protected].
ACS Delegation at the AMA HOD
• John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Ocala, FL
• Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
• Jacob Moalem, MD, FACS (also Young Physicians Section delegate), general surgery, Rochester, NY
• Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Vice-Chair, ACS Board of Regents
• Naveen F. Sangji, MD, general surgery resident, Boston, MA
• Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; Chair, AMA Council on Medical Education
Dr. Armstrong is a member of the American College of Surgeons (ACS) Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy, Washington, DC.
Initiating a surgical society within the ACS: The renewed Excelsior Surgical Society
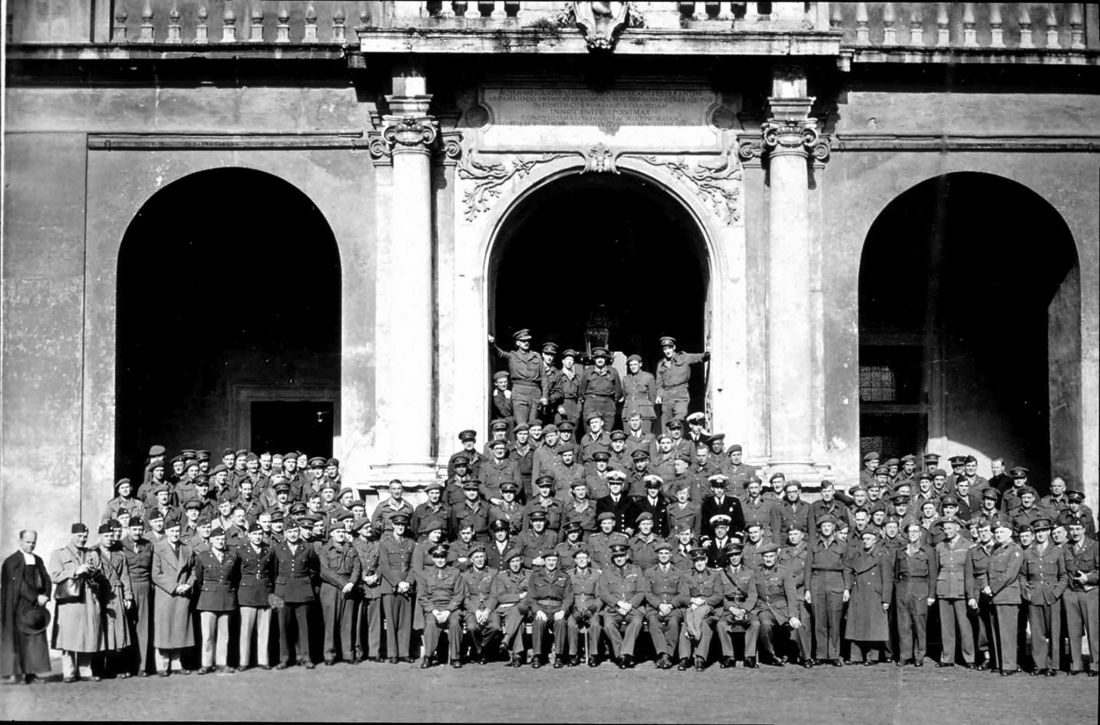
At the end of World War II, surgeons who had served during the conflict gathered at the Excelsior Hotel in Rome, Italy, to discuss their experiences. This meeting was the first of what would be called the Excelsior Surgical Society. These meetings continued annually until the death of the last World War II member, Michael E. DeBakey, MD, FACS.
Visit the society’s web page for more information and to apply for membership.
Day-long meeting
In conjunction with Clinical Congress 2016, the Excelsior Surgical Society held a day-long meeting, with nearly 200 active and retired military surgeons, residents, and students in attendance. The meeting included discussion of the following topics:
• State of the Service addresses by the three General Surgery Consultants to the Army, Navy, and Air Force Surgeon Generals:
o COL Mary Edwards, MD, FACS (Army).
o CAPT Craig Shepps, MD, FACS (Navy).
o COL Gregory York, MD, FACS (Air Force).
• The John Pryor Annual Lectureship, delivered by retired Army COL Norman M. Rich, MD, FACS, department of surgery, Uniformed Services University of the Health Sciences (USUHS) and the Walter Reed National Military Medical Center (WRNMMC), Bethesda, Md.
• The Committee on Trauma Region 13 (Military Region) annual resident paper competition.
• Abstracts on various surgical topics submitted by surgeons from multiple military health care facilities across the country.
• Panel discussions on training and sustainment for surgeons in the military.
Election of Officers
At the business meeting, the following Excelsior Surgical Society Officers were elected:
• President: CAPT Eric Elster, MD, FACS, U.S. Navy, professor and chairman, department of surgery at USUHS and WRNMMC.
• Vice-President: COL Stacy Shackelford, MD, FACS, U.S. Air Force, deputy commander for clinical services/chief of the medical staff 455th Expeditionary Medical Dental Group, Craig Joint Theater Hospital Bagram Airfield, Afghanistan.
• Secretary: COL Robert B. Lim, MD, FACS, U.S. Army, chief, metabolic and advanced laparoscopic surgery, Tripler Army Medical Center, Honolulu, Hawaii.
• Treasurer: COL Kirby R. Gross, MD, FACS, U.S. Army, director, Army Trauma Training Center, University of Miami, Fla.
• Councilperson at Large, U.S. Army: COL Matthew Martin, MD, FACS, FASMBS, trauma medical director, Madigan Army Medical Center, Tacoma, Wash.
• Councilperson at Large, U.S. Navy: CPT Gordon Wisbach, MD, FACS, staff surgeon, department of general surgery, Naval Medical Center San Diego, Calif.
• Councilperson at Large, U.S. Air Force: Col Joe DuBose, MD, FACS, vascular and trauma surgeon, Travis Air Force Base, Calif.
• Councilperson at Large, Reserve/National Guard: COL Jay A. Johannigman, MD, FACS, director of the division of trauma and surgical critical care and professor of surgery at the University of Cincinnati, Ohio.
• Honorary Member: Dr. Rich, Leonard Heaton & David Packard Professor, founding chairman, department of surgery, USUHS and WRNMMC.
At the end of World War II, surgeons who had served during the conflict gathered at the Excelsior Hotel in Rome, Italy, to discuss their experiences. This meeting was the first of what would be called the Excelsior Surgical Society. These meetings continued annually until the death of the last World War II member, Michael E. DeBakey, MD, FACS.
Visit the society’s web page for more information and to apply for membership.
Day-long meeting
In conjunction with Clinical Congress 2016, the Excelsior Surgical Society held a day-long meeting, with nearly 200 active and retired military surgeons, residents, and students in attendance. The meeting included discussion of the following topics:
• State of the Service addresses by the three General Surgery Consultants to the Army, Navy, and Air Force Surgeon Generals:
o COL Mary Edwards, MD, FACS (Army).
o CAPT Craig Shepps, MD, FACS (Navy).
o COL Gregory York, MD, FACS (Air Force).
• The John Pryor Annual Lectureship, delivered by retired Army COL Norman M. Rich, MD, FACS, department of surgery, Uniformed Services University of the Health Sciences (USUHS) and the Walter Reed National Military Medical Center (WRNMMC), Bethesda, Md.
• The Committee on Trauma Region 13 (Military Region) annual resident paper competition.
• Abstracts on various surgical topics submitted by surgeons from multiple military health care facilities across the country.
• Panel discussions on training and sustainment for surgeons in the military.
Election of Officers
At the business meeting, the following Excelsior Surgical Society Officers were elected:
• President: CAPT Eric Elster, MD, FACS, U.S. Navy, professor and chairman, department of surgery at USUHS and WRNMMC.
• Vice-President: COL Stacy Shackelford, MD, FACS, U.S. Air Force, deputy commander for clinical services/chief of the medical staff 455th Expeditionary Medical Dental Group, Craig Joint Theater Hospital Bagram Airfield, Afghanistan.
• Secretary: COL Robert B. Lim, MD, FACS, U.S. Army, chief, metabolic and advanced laparoscopic surgery, Tripler Army Medical Center, Honolulu, Hawaii.
• Treasurer: COL Kirby R. Gross, MD, FACS, U.S. Army, director, Army Trauma Training Center, University of Miami, Fla.
• Councilperson at Large, U.S. Army: COL Matthew Martin, MD, FACS, FASMBS, trauma medical director, Madigan Army Medical Center, Tacoma, Wash.
• Councilperson at Large, U.S. Navy: CPT Gordon Wisbach, MD, FACS, staff surgeon, department of general surgery, Naval Medical Center San Diego, Calif.
• Councilperson at Large, U.S. Air Force: Col Joe DuBose, MD, FACS, vascular and trauma surgeon, Travis Air Force Base, Calif.
• Councilperson at Large, Reserve/National Guard: COL Jay A. Johannigman, MD, FACS, director of the division of trauma and surgical critical care and professor of surgery at the University of Cincinnati, Ohio.
• Honorary Member: Dr. Rich, Leonard Heaton & David Packard Professor, founding chairman, department of surgery, USUHS and WRNMMC.
At the end of World War II, surgeons who had served during the conflict gathered at the Excelsior Hotel in Rome, Italy, to discuss their experiences. This meeting was the first of what would be called the Excelsior Surgical Society. These meetings continued annually until the death of the last World War II member, Michael E. DeBakey, MD, FACS.
Visit the society’s web page for more information and to apply for membership.
Day-long meeting
In conjunction with Clinical Congress 2016, the Excelsior Surgical Society held a day-long meeting, with nearly 200 active and retired military surgeons, residents, and students in attendance. The meeting included discussion of the following topics:
• State of the Service addresses by the three General Surgery Consultants to the Army, Navy, and Air Force Surgeon Generals:
o COL Mary Edwards, MD, FACS (Army).
o CAPT Craig Shepps, MD, FACS (Navy).
o COL Gregory York, MD, FACS (Air Force).
• The John Pryor Annual Lectureship, delivered by retired Army COL Norman M. Rich, MD, FACS, department of surgery, Uniformed Services University of the Health Sciences (USUHS) and the Walter Reed National Military Medical Center (WRNMMC), Bethesda, Md.
• The Committee on Trauma Region 13 (Military Region) annual resident paper competition.
• Abstracts on various surgical topics submitted by surgeons from multiple military health care facilities across the country.
• Panel discussions on training and sustainment for surgeons in the military.
Election of Officers
At the business meeting, the following Excelsior Surgical Society Officers were elected:
• President: CAPT Eric Elster, MD, FACS, U.S. Navy, professor and chairman, department of surgery at USUHS and WRNMMC.
• Vice-President: COL Stacy Shackelford, MD, FACS, U.S. Air Force, deputy commander for clinical services/chief of the medical staff 455th Expeditionary Medical Dental Group, Craig Joint Theater Hospital Bagram Airfield, Afghanistan.
• Secretary: COL Robert B. Lim, MD, FACS, U.S. Army, chief, metabolic and advanced laparoscopic surgery, Tripler Army Medical Center, Honolulu, Hawaii.
• Treasurer: COL Kirby R. Gross, MD, FACS, U.S. Army, director, Army Trauma Training Center, University of Miami, Fla.
• Councilperson at Large, U.S. Army: COL Matthew Martin, MD, FACS, FASMBS, trauma medical director, Madigan Army Medical Center, Tacoma, Wash.
• Councilperson at Large, U.S. Navy: CPT Gordon Wisbach, MD, FACS, staff surgeon, department of general surgery, Naval Medical Center San Diego, Calif.
• Councilperson at Large, U.S. Air Force: Col Joe DuBose, MD, FACS, vascular and trauma surgeon, Travis Air Force Base, Calif.
• Councilperson at Large, Reserve/National Guard: COL Jay A. Johannigman, MD, FACS, director of the division of trauma and surgical critical care and professor of surgery at the University of Cincinnati, Ohio.
• Honorary Member: Dr. Rich, Leonard Heaton & David Packard Professor, founding chairman, department of surgery, USUHS and WRNMMC.
Register now to participate in ACS Leadership & Advocacy Summit 2017
The American College of Surgeons (ACS) will host its sixth annual Leadership & Advocacy Summit, May 6-9 at the Renaissance Washington, DC, Downtown Hotel. The summit is a dual meeting that offers comprehensive and specialized sessions that provide volunteer leaders and advocates with the skills and tools they need to be effective in those roles. Registration for the event is now open at facs.org/summit.
Leadership Summit
The Leadership Summit provides a venue for members to connect with ACS leaders, and to participate in discussions about innovative ways to face challenges and enhance leadership skills. It begins Saturday, May 6, with an initial reception open to all registrants, followed by a full day of programming on Sunday, May 7.
More than 400 ACS leaders, members, residents, and medical students participate in the Leadership portion of the summit. Topics will focus on honing the communication and strategic thinking skills necessary for effective leadership in and out of the operating room. Speakers will address topics such as leadership strategies, ethics in leadership, common mistakes in leadership, team building, managing critical situations, and domestic volunteerism. In addition, a portion of the meeting will be dedicated to sharing ACS chapter success stories and working to identify strategies to enhance and strengthen chapters.
Advocacy Summit
The Advocacy Summit provides the best opportunity to attain the skills and knowledge needed to become a seasoned surgeon advocate. With a new presidential administration and Congress, it is vital that surgeons make the trip to Washington to observe and participate in the evolving political environment.
Since last year’s summit, many details about physician payment under the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015 have been set. At the Advocacy Summit, surgeons will be briefed on the steps they must now take to start complying with MACRA, and ACS staff will help members navigate the many additional legislative changes that are likely to occur.
The Advocacy Summit will begin Sunday, May 7, with a dinner and keynote address. Past speakers have included political commentator Chris Matthews, U.S. Army Gen. (Retired) Stanley A. McChrystal, author Thomas Goetz, and journalists Bob Woodward and George Will.
Sessions planned for the following day will focus on the political climate in Washington, and speakers will provide updates on important health care issues, including Medicare physician payment, graduate medical education, and ensuring patient access to the highest quality surgical care. Tuesday morning, attendees will apply what they have learned at the summit in face-to-face meetings with their senators and representatives and/or congressional staffs. This portion of the program provides an opportunity to rally surgery’s collective grassroots on issues such as physician payment, professional liability, and physician workforce.
Fellows attending the Advocacy Summit will have the opportunity to make an early impression on a new Congress. During this three-day conference, participants can expect to receive comprehensive advocacy training and learn how to use these skills throughout the year, not just when in Washington. The Advocacy Summit is the place to confer with other surgeon advocates to share ideas and meet face-to-face with key health care policymakers and legislators. Perhaps more importantly, the Advocacy Summit gives surgeons an opportunity to become the constituent their legislators know and trust to offer advice on surgical issues.
The ACS Professional Association political action committee (ACSPA-SurgeonsPAC) will host various events for members and SurgeonsPAC contributors. These events provide contributors with unique networking opportunities, advanced educational sessions aimed at helping College members become more effective surgeon-advocates, and an insider’s perspective on how to remain engaged in the political process.
In addition to raising funds to elect and/or re-elect congressional candidates who support a pro-surgeon, pro-patient agenda, SurgeonsPAC will host a reception at which PAC contributors will be recognized for their commitment to surgery and the surgical patient. Other SurgeonsPAC-sponsored events include the annual raffle, a political luncheon featuring a special guest speaker, and presentation of the 2016 PAC awards. Resident engagement opportunities will be provided as well. In addition, the SurgeonsPAC booth provides attendees with a venue to interact with ACS Division of Advocacy and Health Policy staff to learn more about the PAC and ACS advocacy efforts.
For more information about the Leadership Summit, e-mail [email protected]. For more information about the Advocacy Summit and ACSPA-SurgeonsPAC activities, e-mail [email protected] or call 202-672-1520.
The American College of Surgeons (ACS) will host its sixth annual Leadership & Advocacy Summit, May 6-9 at the Renaissance Washington, DC, Downtown Hotel. The summit is a dual meeting that offers comprehensive and specialized sessions that provide volunteer leaders and advocates with the skills and tools they need to be effective in those roles. Registration for the event is now open at facs.org/summit.
Leadership Summit
The Leadership Summit provides a venue for members to connect with ACS leaders, and to participate in discussions about innovative ways to face challenges and enhance leadership skills. It begins Saturday, May 6, with an initial reception open to all registrants, followed by a full day of programming on Sunday, May 7.
More than 400 ACS leaders, members, residents, and medical students participate in the Leadership portion of the summit. Topics will focus on honing the communication and strategic thinking skills necessary for effective leadership in and out of the operating room. Speakers will address topics such as leadership strategies, ethics in leadership, common mistakes in leadership, team building, managing critical situations, and domestic volunteerism. In addition, a portion of the meeting will be dedicated to sharing ACS chapter success stories and working to identify strategies to enhance and strengthen chapters.
Advocacy Summit
The Advocacy Summit provides the best opportunity to attain the skills and knowledge needed to become a seasoned surgeon advocate. With a new presidential administration and Congress, it is vital that surgeons make the trip to Washington to observe and participate in the evolving political environment.
Since last year’s summit, many details about physician payment under the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015 have been set. At the Advocacy Summit, surgeons will be briefed on the steps they must now take to start complying with MACRA, and ACS staff will help members navigate the many additional legislative changes that are likely to occur.
The Advocacy Summit will begin Sunday, May 7, with a dinner and keynote address. Past speakers have included political commentator Chris Matthews, U.S. Army Gen. (Retired) Stanley A. McChrystal, author Thomas Goetz, and journalists Bob Woodward and George Will.
Sessions planned for the following day will focus on the political climate in Washington, and speakers will provide updates on important health care issues, including Medicare physician payment, graduate medical education, and ensuring patient access to the highest quality surgical care. Tuesday morning, attendees will apply what they have learned at the summit in face-to-face meetings with their senators and representatives and/or congressional staffs. This portion of the program provides an opportunity to rally surgery’s collective grassroots on issues such as physician payment, professional liability, and physician workforce.
Fellows attending the Advocacy Summit will have the opportunity to make an early impression on a new Congress. During this three-day conference, participants can expect to receive comprehensive advocacy training and learn how to use these skills throughout the year, not just when in Washington. The Advocacy Summit is the place to confer with other surgeon advocates to share ideas and meet face-to-face with key health care policymakers and legislators. Perhaps more importantly, the Advocacy Summit gives surgeons an opportunity to become the constituent their legislators know and trust to offer advice on surgical issues.
The ACS Professional Association political action committee (ACSPA-SurgeonsPAC) will host various events for members and SurgeonsPAC contributors. These events provide contributors with unique networking opportunities, advanced educational sessions aimed at helping College members become more effective surgeon-advocates, and an insider’s perspective on how to remain engaged in the political process.
In addition to raising funds to elect and/or re-elect congressional candidates who support a pro-surgeon, pro-patient agenda, SurgeonsPAC will host a reception at which PAC contributors will be recognized for their commitment to surgery and the surgical patient. Other SurgeonsPAC-sponsored events include the annual raffle, a political luncheon featuring a special guest speaker, and presentation of the 2016 PAC awards. Resident engagement opportunities will be provided as well. In addition, the SurgeonsPAC booth provides attendees with a venue to interact with ACS Division of Advocacy and Health Policy staff to learn more about the PAC and ACS advocacy efforts.
For more information about the Leadership Summit, e-mail [email protected]. For more information about the Advocacy Summit and ACSPA-SurgeonsPAC activities, e-mail [email protected] or call 202-672-1520.
The American College of Surgeons (ACS) will host its sixth annual Leadership & Advocacy Summit, May 6-9 at the Renaissance Washington, DC, Downtown Hotel. The summit is a dual meeting that offers comprehensive and specialized sessions that provide volunteer leaders and advocates with the skills and tools they need to be effective in those roles. Registration for the event is now open at facs.org/summit.
Leadership Summit
The Leadership Summit provides a venue for members to connect with ACS leaders, and to participate in discussions about innovative ways to face challenges and enhance leadership skills. It begins Saturday, May 6, with an initial reception open to all registrants, followed by a full day of programming on Sunday, May 7.
More than 400 ACS leaders, members, residents, and medical students participate in the Leadership portion of the summit. Topics will focus on honing the communication and strategic thinking skills necessary for effective leadership in and out of the operating room. Speakers will address topics such as leadership strategies, ethics in leadership, common mistakes in leadership, team building, managing critical situations, and domestic volunteerism. In addition, a portion of the meeting will be dedicated to sharing ACS chapter success stories and working to identify strategies to enhance and strengthen chapters.
Advocacy Summit
The Advocacy Summit provides the best opportunity to attain the skills and knowledge needed to become a seasoned surgeon advocate. With a new presidential administration and Congress, it is vital that surgeons make the trip to Washington to observe and participate in the evolving political environment.
Since last year’s summit, many details about physician payment under the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act (MACRA) of 2015 have been set. At the Advocacy Summit, surgeons will be briefed on the steps they must now take to start complying with MACRA, and ACS staff will help members navigate the many additional legislative changes that are likely to occur.
The Advocacy Summit will begin Sunday, May 7, with a dinner and keynote address. Past speakers have included political commentator Chris Matthews, U.S. Army Gen. (Retired) Stanley A. McChrystal, author Thomas Goetz, and journalists Bob Woodward and George Will.
Sessions planned for the following day will focus on the political climate in Washington, and speakers will provide updates on important health care issues, including Medicare physician payment, graduate medical education, and ensuring patient access to the highest quality surgical care. Tuesday morning, attendees will apply what they have learned at the summit in face-to-face meetings with their senators and representatives and/or congressional staffs. This portion of the program provides an opportunity to rally surgery’s collective grassroots on issues such as physician payment, professional liability, and physician workforce.
Fellows attending the Advocacy Summit will have the opportunity to make an early impression on a new Congress. During this three-day conference, participants can expect to receive comprehensive advocacy training and learn how to use these skills throughout the year, not just when in Washington. The Advocacy Summit is the place to confer with other surgeon advocates to share ideas and meet face-to-face with key health care policymakers and legislators. Perhaps more importantly, the Advocacy Summit gives surgeons an opportunity to become the constituent their legislators know and trust to offer advice on surgical issues.
The ACS Professional Association political action committee (ACSPA-SurgeonsPAC) will host various events for members and SurgeonsPAC contributors. These events provide contributors with unique networking opportunities, advanced educational sessions aimed at helping College members become more effective surgeon-advocates, and an insider’s perspective on how to remain engaged in the political process.
In addition to raising funds to elect and/or re-elect congressional candidates who support a pro-surgeon, pro-patient agenda, SurgeonsPAC will host a reception at which PAC contributors will be recognized for their commitment to surgery and the surgical patient. Other SurgeonsPAC-sponsored events include the annual raffle, a political luncheon featuring a special guest speaker, and presentation of the 2016 PAC awards. Resident engagement opportunities will be provided as well. In addition, the SurgeonsPAC booth provides attendees with a venue to interact with ACS Division of Advocacy and Health Policy staff to learn more about the PAC and ACS advocacy efforts.
For more information about the Leadership Summit, e-mail [email protected]. For more information about the Advocacy Summit and ACSPA-SurgeonsPAC activities, e-mail [email protected] or call 202-672-1520.
Dr. Frank Lewis, ABS executive director, announces retirement
Frank R. Lewis, MD, FACS, executive director of the American Board of Surgery (ABS), announced that he will retire from the organization at the end of 2017. The ABS will conduct a national recruitment process to identify his successor, with the goal of having that individual in place in late June.
Dr. Lewis, who joined the ABS as executive director in 2002, guided the society through many significant initiatives and changes, including the creation of the Surgical Council on Resident Education (SCORE), development of a primary certificate in vascular surgery, establishment of flexible rotations in residency training, and the subsequent design and implementation of the Flexibility In duty hour Requirements for Surgical Trainees (FIRST) Trial, among others.
In addition, Dr. Lewis is past chair of the ABS and the Residency Review Committee for Surgery of the Accreditation Council for Graduate Medical Education. Dr. Lewis also served as 1995-1996 First Vice-President of the American College of Surgeons (ACS) and as the 1991-1993 Chair of the ACS Board of Governors. Read more about Dr. Lewis’ retirement and accomplishments on the ABS website at www.absurgery.org/default.jsp?news_lewis0117.
Frank R. Lewis, MD, FACS, executive director of the American Board of Surgery (ABS), announced that he will retire from the organization at the end of 2017. The ABS will conduct a national recruitment process to identify his successor, with the goal of having that individual in place in late June.
Dr. Lewis, who joined the ABS as executive director in 2002, guided the society through many significant initiatives and changes, including the creation of the Surgical Council on Resident Education (SCORE), development of a primary certificate in vascular surgery, establishment of flexible rotations in residency training, and the subsequent design and implementation of the Flexibility In duty hour Requirements for Surgical Trainees (FIRST) Trial, among others.
In addition, Dr. Lewis is past chair of the ABS and the Residency Review Committee for Surgery of the Accreditation Council for Graduate Medical Education. Dr. Lewis also served as 1995-1996 First Vice-President of the American College of Surgeons (ACS) and as the 1991-1993 Chair of the ACS Board of Governors. Read more about Dr. Lewis’ retirement and accomplishments on the ABS website at www.absurgery.org/default.jsp?news_lewis0117.
Frank R. Lewis, MD, FACS, executive director of the American Board of Surgery (ABS), announced that he will retire from the organization at the end of 2017. The ABS will conduct a national recruitment process to identify his successor, with the goal of having that individual in place in late June.
Dr. Lewis, who joined the ABS as executive director in 2002, guided the society through many significant initiatives and changes, including the creation of the Surgical Council on Resident Education (SCORE), development of a primary certificate in vascular surgery, establishment of flexible rotations in residency training, and the subsequent design and implementation of the Flexibility In duty hour Requirements for Surgical Trainees (FIRST) Trial, among others.
In addition, Dr. Lewis is past chair of the ABS and the Residency Review Committee for Surgery of the Accreditation Council for Graduate Medical Education. Dr. Lewis also served as 1995-1996 First Vice-President of the American College of Surgeons (ACS) and as the 1991-1993 Chair of the ACS Board of Governors. Read more about Dr. Lewis’ retirement and accomplishments on the ABS website at www.absurgery.org/default.jsp?news_lewis0117.