User login
Survival equivalent in sublobar, lobar resection of NSCLC
MINNEAPOLIS – Sublobar resection and lobectomy resulted in equivalent lung cancer survival and overall recurrence rates in a screen-detected cohort of 348 stage IA non–small cell lung cancer patients.
In all, 7% of patients (4/54) who underwent sublobar resection and 10% of those (29/294) who underwent lobectomy died of lung cancer after a median follow-up of 73 months (P = .64). All-cause mortality was also statistically similar at 17% and 22%, said Dr. Nasser Altorki, professor of cardiothoracic surgery and director of thoracic surgery at New York Presbyterian–Weill Cornell Medical Center in New York.
Although lobectomy has been the standard of care for resection of early-stage non–small cell lung cancer (NSCLC) since 1994, several studies support sublobar resection in patients with small peripheral tumors and the elderly with compromised pulmonary reserve.
The best surgical treatment for younger patients with adequate cardiopulmonary function remains controversial, with two large, ongoing trials in the U.S. and Japan evaluating lobar vs. sublobar resection in this setting. A recent best evidence paper (Interact. CardioVasc. Thorac. Surg. 2012;14:816-20) concluded that lobectomy is still the best surgical option for these patients, citing evidence of lower survival and higher recurrence rates with wedge resections than with anatomic segmentectomies. The two sublobar techniques are often lumped together in comparisons with lobectomy, but are not technically or oncologically the same.
Wedge resection in the current study seemed to be associated with a higher rate of recurrence than segmentectomy, Dr. Altorki said at the annual meeting of the American Association for Thoracic Surgery.
Recurrence occurred in 32 patients after lobectomy and 8 after sublobar resection (11% vs. 15%; P = .40), with all of the sublobar resection recurrences occurring after wedge resection (8/38 or 21% vs. 0%).
"I don’t want to say this is a practice-changing study; however, it is a study that calls for more technical equipoise in our approach to the [surgical] treatment of lung cancer," he said during a discussion of the results. "Clearly, we can apply this operation to patients who would be candidates for both lobectomy and sublobar resection, but it does not extend to those patients, for example, that would have been poor candidates for any surgical resection."
The 348 patients had c1A non–small cell lung cancer that presented as a solid nodule on computed tomography screening and underwent surgery as part of the International Early Lung Cancer Action Program from 1993 to 2011. Comorbidities were similar among the lobectomy and sublobar patients including cardiac disease (6% vs. 11%), chronic obstructive pulmonary disease (15% vs. 26%), and diabetes (9% vs. 7%). Their median age was 63 vs. 65 years, and the median number of pack-years of smoking was 48 vs. 49, respectively.
The lobectomy group had significantly larger tumors (13 mm vs. 11 mm), more frequent sampling of mediastinal nodes (78% vs. 56%), and more resected lymph nodes (mean 8 vs. 5).
The overall rate of hospital mortality in the multicenter study was low at 0.9% (3/348) and "represents what is achievable in screening centers of excellence," Dr. Altorki said.
Ten-year survival was 88% with lobectomy and 90% with sublobar resection (log rank P = .64). There was no difference in patients with tumors less than 2 cm (88% vs. 89%), who represented the majority or 86% of the cohort.
Cox regression analysis, adjusted for the above potential confounders, showed that only age (hazard ratio, 2.9; P less than .0001) and severe emphysema (HR, 4.2; P = .005) significantly predicted survival, whereas sublobar resection did not (HR, 0.8; P = .60), he said.
Invited discussant Dr. Joseph S. Friedberg, chief of thoracic surgery at the University of Pennsylvania Health System-Presbyterian in Philadelphia, expressed surprise that despite undergoing surgery by highly qualified general thoracic surgeons, 70% of sublobar resections were performed as wedge and not segmentectomies, and that more than 40% of sublobar resection patients and nearly a quarter of lobectomy patients did not have one mediastinal node biopsied.
"One would expect, based on the Lung Cancer Study Group analysis and common sense, that some of these patients, especially sublobar resection patients, were understaged and/or undertreated and yet the results are as good as anything in the literature," he said. "How do you reconcile that?"
Dr. Altorki said assessment of the mediastinal field was disappointing and that further education is needed on the prognostic and therapeutic benefits of such assessment, but that the rate far exceeds what is in the published literature. He also speculated that most of the patients were treated by video-assisted thoracic surgery and that mediastinal node assessment may not be as straightforward with VATS as it is with open surgery.
Dr. Altorki said that, going in, many of the surgeons may have thought that a 1- to 1.2-cm tumor may be equally resected with wedge resection and anatomic segmentectomy, and that this "is a job we have to address in ongoing randomized trials."
Dr. Altorki reported no relevant financial disclosures.
MINNEAPOLIS – Sublobar resection and lobectomy resulted in equivalent lung cancer survival and overall recurrence rates in a screen-detected cohort of 348 stage IA non–small cell lung cancer patients.
In all, 7% of patients (4/54) who underwent sublobar resection and 10% of those (29/294) who underwent lobectomy died of lung cancer after a median follow-up of 73 months (P = .64). All-cause mortality was also statistically similar at 17% and 22%, said Dr. Nasser Altorki, professor of cardiothoracic surgery and director of thoracic surgery at New York Presbyterian–Weill Cornell Medical Center in New York.
Although lobectomy has been the standard of care for resection of early-stage non–small cell lung cancer (NSCLC) since 1994, several studies support sublobar resection in patients with small peripheral tumors and the elderly with compromised pulmonary reserve.
The best surgical treatment for younger patients with adequate cardiopulmonary function remains controversial, with two large, ongoing trials in the U.S. and Japan evaluating lobar vs. sublobar resection in this setting. A recent best evidence paper (Interact. CardioVasc. Thorac. Surg. 2012;14:816-20) concluded that lobectomy is still the best surgical option for these patients, citing evidence of lower survival and higher recurrence rates with wedge resections than with anatomic segmentectomies. The two sublobar techniques are often lumped together in comparisons with lobectomy, but are not technically or oncologically the same.
Wedge resection in the current study seemed to be associated with a higher rate of recurrence than segmentectomy, Dr. Altorki said at the annual meeting of the American Association for Thoracic Surgery.
Recurrence occurred in 32 patients after lobectomy and 8 after sublobar resection (11% vs. 15%; P = .40), with all of the sublobar resection recurrences occurring after wedge resection (8/38 or 21% vs. 0%).
"I don’t want to say this is a practice-changing study; however, it is a study that calls for more technical equipoise in our approach to the [surgical] treatment of lung cancer," he said during a discussion of the results. "Clearly, we can apply this operation to patients who would be candidates for both lobectomy and sublobar resection, but it does not extend to those patients, for example, that would have been poor candidates for any surgical resection."
The 348 patients had c1A non–small cell lung cancer that presented as a solid nodule on computed tomography screening and underwent surgery as part of the International Early Lung Cancer Action Program from 1993 to 2011. Comorbidities were similar among the lobectomy and sublobar patients including cardiac disease (6% vs. 11%), chronic obstructive pulmonary disease (15% vs. 26%), and diabetes (9% vs. 7%). Their median age was 63 vs. 65 years, and the median number of pack-years of smoking was 48 vs. 49, respectively.
The lobectomy group had significantly larger tumors (13 mm vs. 11 mm), more frequent sampling of mediastinal nodes (78% vs. 56%), and more resected lymph nodes (mean 8 vs. 5).
The overall rate of hospital mortality in the multicenter study was low at 0.9% (3/348) and "represents what is achievable in screening centers of excellence," Dr. Altorki said.
Ten-year survival was 88% with lobectomy and 90% with sublobar resection (log rank P = .64). There was no difference in patients with tumors less than 2 cm (88% vs. 89%), who represented the majority or 86% of the cohort.
Cox regression analysis, adjusted for the above potential confounders, showed that only age (hazard ratio, 2.9; P less than .0001) and severe emphysema (HR, 4.2; P = .005) significantly predicted survival, whereas sublobar resection did not (HR, 0.8; P = .60), he said.
Invited discussant Dr. Joseph S. Friedberg, chief of thoracic surgery at the University of Pennsylvania Health System-Presbyterian in Philadelphia, expressed surprise that despite undergoing surgery by highly qualified general thoracic surgeons, 70% of sublobar resections were performed as wedge and not segmentectomies, and that more than 40% of sublobar resection patients and nearly a quarter of lobectomy patients did not have one mediastinal node biopsied.
"One would expect, based on the Lung Cancer Study Group analysis and common sense, that some of these patients, especially sublobar resection patients, were understaged and/or undertreated and yet the results are as good as anything in the literature," he said. "How do you reconcile that?"
Dr. Altorki said assessment of the mediastinal field was disappointing and that further education is needed on the prognostic and therapeutic benefits of such assessment, but that the rate far exceeds what is in the published literature. He also speculated that most of the patients were treated by video-assisted thoracic surgery and that mediastinal node assessment may not be as straightforward with VATS as it is with open surgery.
Dr. Altorki said that, going in, many of the surgeons may have thought that a 1- to 1.2-cm tumor may be equally resected with wedge resection and anatomic segmentectomy, and that this "is a job we have to address in ongoing randomized trials."
Dr. Altorki reported no relevant financial disclosures.
MINNEAPOLIS – Sublobar resection and lobectomy resulted in equivalent lung cancer survival and overall recurrence rates in a screen-detected cohort of 348 stage IA non–small cell lung cancer patients.
In all, 7% of patients (4/54) who underwent sublobar resection and 10% of those (29/294) who underwent lobectomy died of lung cancer after a median follow-up of 73 months (P = .64). All-cause mortality was also statistically similar at 17% and 22%, said Dr. Nasser Altorki, professor of cardiothoracic surgery and director of thoracic surgery at New York Presbyterian–Weill Cornell Medical Center in New York.
Although lobectomy has been the standard of care for resection of early-stage non–small cell lung cancer (NSCLC) since 1994, several studies support sublobar resection in patients with small peripheral tumors and the elderly with compromised pulmonary reserve.
The best surgical treatment for younger patients with adequate cardiopulmonary function remains controversial, with two large, ongoing trials in the U.S. and Japan evaluating lobar vs. sublobar resection in this setting. A recent best evidence paper (Interact. CardioVasc. Thorac. Surg. 2012;14:816-20) concluded that lobectomy is still the best surgical option for these patients, citing evidence of lower survival and higher recurrence rates with wedge resections than with anatomic segmentectomies. The two sublobar techniques are often lumped together in comparisons with lobectomy, but are not technically or oncologically the same.
Wedge resection in the current study seemed to be associated with a higher rate of recurrence than segmentectomy, Dr. Altorki said at the annual meeting of the American Association for Thoracic Surgery.
Recurrence occurred in 32 patients after lobectomy and 8 after sublobar resection (11% vs. 15%; P = .40), with all of the sublobar resection recurrences occurring after wedge resection (8/38 or 21% vs. 0%).
"I don’t want to say this is a practice-changing study; however, it is a study that calls for more technical equipoise in our approach to the [surgical] treatment of lung cancer," he said during a discussion of the results. "Clearly, we can apply this operation to patients who would be candidates for both lobectomy and sublobar resection, but it does not extend to those patients, for example, that would have been poor candidates for any surgical resection."
The 348 patients had c1A non–small cell lung cancer that presented as a solid nodule on computed tomography screening and underwent surgery as part of the International Early Lung Cancer Action Program from 1993 to 2011. Comorbidities were similar among the lobectomy and sublobar patients including cardiac disease (6% vs. 11%), chronic obstructive pulmonary disease (15% vs. 26%), and diabetes (9% vs. 7%). Their median age was 63 vs. 65 years, and the median number of pack-years of smoking was 48 vs. 49, respectively.
The lobectomy group had significantly larger tumors (13 mm vs. 11 mm), more frequent sampling of mediastinal nodes (78% vs. 56%), and more resected lymph nodes (mean 8 vs. 5).
The overall rate of hospital mortality in the multicenter study was low at 0.9% (3/348) and "represents what is achievable in screening centers of excellence," Dr. Altorki said.
Ten-year survival was 88% with lobectomy and 90% with sublobar resection (log rank P = .64). There was no difference in patients with tumors less than 2 cm (88% vs. 89%), who represented the majority or 86% of the cohort.
Cox regression analysis, adjusted for the above potential confounders, showed that only age (hazard ratio, 2.9; P less than .0001) and severe emphysema (HR, 4.2; P = .005) significantly predicted survival, whereas sublobar resection did not (HR, 0.8; P = .60), he said.
Invited discussant Dr. Joseph S. Friedberg, chief of thoracic surgery at the University of Pennsylvania Health System-Presbyterian in Philadelphia, expressed surprise that despite undergoing surgery by highly qualified general thoracic surgeons, 70% of sublobar resections were performed as wedge and not segmentectomies, and that more than 40% of sublobar resection patients and nearly a quarter of lobectomy patients did not have one mediastinal node biopsied.
"One would expect, based on the Lung Cancer Study Group analysis and common sense, that some of these patients, especially sublobar resection patients, were understaged and/or undertreated and yet the results are as good as anything in the literature," he said. "How do you reconcile that?"
Dr. Altorki said assessment of the mediastinal field was disappointing and that further education is needed on the prognostic and therapeutic benefits of such assessment, but that the rate far exceeds what is in the published literature. He also speculated that most of the patients were treated by video-assisted thoracic surgery and that mediastinal node assessment may not be as straightforward with VATS as it is with open surgery.
Dr. Altorki said that, going in, many of the surgeons may have thought that a 1- to 1.2-cm tumor may be equally resected with wedge resection and anatomic segmentectomy, and that this "is a job we have to address in ongoing randomized trials."
Dr. Altorki reported no relevant financial disclosures.
AT THE AATS ANNUAL MEETING
Major finding: Lung cancer–specific mortality was 7% with sublobar resection and 10% with lobar resection.
Data source: Retrospective analysis of 348 patients with stage IA non–small-cell lung cancer in the prospective International Early Lung Cancer Action Program.
Disclosures: Dr. Altorki reported no relevant financial disclosures.
Esophagectomy cases have been rising steadily
INDIANAPOLIS - Transthoracic esophagectomy for esophageal cancer provides significantly lower in-hospital mortality and major morbidity rates than does transhiatal esophagectomy, according to an analysis of a large multiyear national database.
Further, in-hospital outcomes of esophagectomy didn?t differ significantly between high-volume centers ? in this study, defined as those doing 10 or more cases per year ? and low-volume centers, Dr. Mehraneh D. Jafari reported at the annual meeting of the American Surgical Association.
That finding was met with skepticism, and discussants were quick to argue that study limitations make it difficult to draw any meaningful conclusions from the data. For one thing, speakers contended that defining a high-volume center based upon an institutional threshold of 10 or more cases per year sets the bar far too low given that a single dedicated esophageal surgery specialist might easily perform 50 or more esophagectomies annually.
Dr. Jafari presented an analysis of 11,473 transthoracic and 3,717 transhiatal esophagectomies performed for esophageal cancer. The data came from the Nationwide Inpatient Sample (NIS) during 2001-2010. The NIS records data on in-hospital outcomes for a nationally representative sample composed of roughly 20% of the country?s hospital discharges each year.
The number of esophagectomies rose steadily by an average of 4% annually during the study years, reflecting the substantial national increase in cases of esophageal cancer. The growing case count, expected to reach an estimated 18,000 cases of esophageal cancer nationwide in 2013, has been attributed to rising rates of gastroesophageal reflux disease, Barrett?s esophagus, and obesity. Transthoracic esophagectomy, used in 76% of cases, remained the preferred operative strategy throughout the study years.
In-hospital outcomes were markedly better in patients who had transthoracic esophagectomy. After adjustment for potential confounding variables in a multivariate analysis, transhiatal esophagectomy recipients had a 67% increased risk of in-hospital mortality and a 39% greater risk of serious complications, including a 37% increased risk of pulmonary complications. However, anastomotic leak rates were similar with both operations, according to Dr. Jafari of the University of California, Irvine.
The referral rate to high-volume esophagectomy centers climbed steadily over time, rising from 22% of all cases in 2001 to 58% in 2010.
The 35 high-volume centers performed an average of 16 cases per year. In contrast, the 484 low-volume centers averaged 2 cases per year. In-hospital mortality among the 9,386 patients treated in low-volume centers averaged 7.6% compared with 4.3% for patients in high-volume centers. Overall in-hospital serious morbidity rates were greater in the low-volume centers as well: 47% versus 41%. While these raw differences were statistically significant, a risk-adjusted multivariate analysis found no significant outcome differences between low- and high-volume centers.
Discussant Dr. Michael J. Zinner noted that in an earlier study he and his coworkers showed that an institutional threshold of roughly 30 esophagectomies per year is required to discriminate between low- and high-volume centers in terms of in-hospital mortality. So why define high-volume centers as those doing a mere 10 cases per year? asked Dr. Zinner, chairman of the department of surgery at Brigham and Women?s Hospital and professor of surgery at Harvard Medical School, Boston.
"The problem here is if you establish 30 cases per year as the threshold for a high-volume center, I can tell you there are probably less than 20 centers in the whole U.S. capable of doing that volume. That?s a real issue, because then how are patients who live in a remote region going to get care at one of those centers?" replied Dr. Jafari?s senior coauthor Dr. Ninh T. Nguyen, professor and vice-chair of surgery at UC Irvine.
"I think instead we should try to lift all boats: Develop a national esophageal center network to identify the qualities reflective of better outcomes in the high-volume centers and introduce those factors at low-volume centers. This way we?re not impeding access to care for our patients," he continued.
Dr. Nguyen said that in-hospital surgical morbidity rates in the NIS need to be taken with a grain of salt, as the accuracy of coding for complications is "rather low." The development of minimally invasive techniques for intrathoracic anastomosis has transformed transthoracic esophagectomy into a procedure with an improved complication profile.
"I switched to transthoracic esophagectomy 5 years ago. One reason was development of the minimally invasive approach. As a result, we?re not scared of a chest anastomosis like we used to be. When patients undergoing transthoracic esophagectomy with thoracotomy had a leak in the chest they had a very high risk for mortality. That?s not the case anymore. We have not observed any mortality associated with a leak in the chest for many, many years now," he said.
The investigators reported having no conflicts of interest.
I have major problems with this study, stemming from inherent limitations in the Nationwide Inpatient Sample. It?s an administrative database set up chiefly to track costs, utilization, and length of stay. It contains no information at all on key clinical outcomes such as 30- and 90-day mortality, discharge disposition, or 30-day readmission rates.
| Dr. Luketich |
In addition, the accuracy of the quoted in-hospital morbidity rates is suspect, probably because data entry isn?t performed by trained researchers. For example, the 8% incidence of renal failure in esophagectomy patients cited in this study sounds too high to be right.
And there?s another major problem with this database: The superior outcomes reported for transthoracic esophagectomy recipients in this study fly in the face of earlier, well-conducted meta-analyses that reached the opposite conclusion. The most likely explanation for the discordant findings lies in the fact that the NIS doesn?t show whether a transthoracic esophagectomy was performed via open thoracotomy in the old-school manner or with an intrathoracic anastomosis created using contemporary minimally invasive techniques which, while complex, have been associated with better outcomes.
Dr. James D. Luketich is professor of surgery and chief of the Heart, Lung, and Esophageal Surgery Institute at the University of Pittsburgh. He was a designated discussant of the study at the meeting.
I have major problems with this study, stemming from inherent limitations in the Nationwide Inpatient Sample. It?s an administrative database set up chiefly to track costs, utilization, and length of stay. It contains no information at all on key clinical outcomes such as 30- and 90-day mortality, discharge disposition, or 30-day readmission rates.
| Dr. Luketich |
In addition, the accuracy of the quoted in-hospital morbidity rates is suspect, probably because data entry isn?t performed by trained researchers. For example, the 8% incidence of renal failure in esophagectomy patients cited in this study sounds too high to be right.
And there?s another major problem with this database: The superior outcomes reported for transthoracic esophagectomy recipients in this study fly in the face of earlier, well-conducted meta-analyses that reached the opposite conclusion. The most likely explanation for the discordant findings lies in the fact that the NIS doesn?t show whether a transthoracic esophagectomy was performed via open thoracotomy in the old-school manner or with an intrathoracic anastomosis created using contemporary minimally invasive techniques which, while complex, have been associated with better outcomes.
Dr. James D. Luketich is professor of surgery and chief of the Heart, Lung, and Esophageal Surgery Institute at the University of Pittsburgh. He was a designated discussant of the study at the meeting.
I have major problems with this study, stemming from inherent limitations in the Nationwide Inpatient Sample. It?s an administrative database set up chiefly to track costs, utilization, and length of stay. It contains no information at all on key clinical outcomes such as 30- and 90-day mortality, discharge disposition, or 30-day readmission rates.
| Dr. Luketich |
In addition, the accuracy of the quoted in-hospital morbidity rates is suspect, probably because data entry isn?t performed by trained researchers. For example, the 8% incidence of renal failure in esophagectomy patients cited in this study sounds too high to be right.
And there?s another major problem with this database: The superior outcomes reported for transthoracic esophagectomy recipients in this study fly in the face of earlier, well-conducted meta-analyses that reached the opposite conclusion. The most likely explanation for the discordant findings lies in the fact that the NIS doesn?t show whether a transthoracic esophagectomy was performed via open thoracotomy in the old-school manner or with an intrathoracic anastomosis created using contemporary minimally invasive techniques which, while complex, have been associated with better outcomes.
Dr. James D. Luketich is professor of surgery and chief of the Heart, Lung, and Esophageal Surgery Institute at the University of Pittsburgh. He was a designated discussant of the study at the meeting.
INDIANAPOLIS - Transthoracic esophagectomy for esophageal cancer provides significantly lower in-hospital mortality and major morbidity rates than does transhiatal esophagectomy, according to an analysis of a large multiyear national database.
Further, in-hospital outcomes of esophagectomy didn?t differ significantly between high-volume centers ? in this study, defined as those doing 10 or more cases per year ? and low-volume centers, Dr. Mehraneh D. Jafari reported at the annual meeting of the American Surgical Association.
That finding was met with skepticism, and discussants were quick to argue that study limitations make it difficult to draw any meaningful conclusions from the data. For one thing, speakers contended that defining a high-volume center based upon an institutional threshold of 10 or more cases per year sets the bar far too low given that a single dedicated esophageal surgery specialist might easily perform 50 or more esophagectomies annually.
Dr. Jafari presented an analysis of 11,473 transthoracic and 3,717 transhiatal esophagectomies performed for esophageal cancer. The data came from the Nationwide Inpatient Sample (NIS) during 2001-2010. The NIS records data on in-hospital outcomes for a nationally representative sample composed of roughly 20% of the country?s hospital discharges each year.
The number of esophagectomies rose steadily by an average of 4% annually during the study years, reflecting the substantial national increase in cases of esophageal cancer. The growing case count, expected to reach an estimated 18,000 cases of esophageal cancer nationwide in 2013, has been attributed to rising rates of gastroesophageal reflux disease, Barrett?s esophagus, and obesity. Transthoracic esophagectomy, used in 76% of cases, remained the preferred operative strategy throughout the study years.
In-hospital outcomes were markedly better in patients who had transthoracic esophagectomy. After adjustment for potential confounding variables in a multivariate analysis, transhiatal esophagectomy recipients had a 67% increased risk of in-hospital mortality and a 39% greater risk of serious complications, including a 37% increased risk of pulmonary complications. However, anastomotic leak rates were similar with both operations, according to Dr. Jafari of the University of California, Irvine.
The referral rate to high-volume esophagectomy centers climbed steadily over time, rising from 22% of all cases in 2001 to 58% in 2010.
The 35 high-volume centers performed an average of 16 cases per year. In contrast, the 484 low-volume centers averaged 2 cases per year. In-hospital mortality among the 9,386 patients treated in low-volume centers averaged 7.6% compared with 4.3% for patients in high-volume centers. Overall in-hospital serious morbidity rates were greater in the low-volume centers as well: 47% versus 41%. While these raw differences were statistically significant, a risk-adjusted multivariate analysis found no significant outcome differences between low- and high-volume centers.
Discussant Dr. Michael J. Zinner noted that in an earlier study he and his coworkers showed that an institutional threshold of roughly 30 esophagectomies per year is required to discriminate between low- and high-volume centers in terms of in-hospital mortality. So why define high-volume centers as those doing a mere 10 cases per year? asked Dr. Zinner, chairman of the department of surgery at Brigham and Women?s Hospital and professor of surgery at Harvard Medical School, Boston.
"The problem here is if you establish 30 cases per year as the threshold for a high-volume center, I can tell you there are probably less than 20 centers in the whole U.S. capable of doing that volume. That?s a real issue, because then how are patients who live in a remote region going to get care at one of those centers?" replied Dr. Jafari?s senior coauthor Dr. Ninh T. Nguyen, professor and vice-chair of surgery at UC Irvine.
"I think instead we should try to lift all boats: Develop a national esophageal center network to identify the qualities reflective of better outcomes in the high-volume centers and introduce those factors at low-volume centers. This way we?re not impeding access to care for our patients," he continued.
Dr. Nguyen said that in-hospital surgical morbidity rates in the NIS need to be taken with a grain of salt, as the accuracy of coding for complications is "rather low." The development of minimally invasive techniques for intrathoracic anastomosis has transformed transthoracic esophagectomy into a procedure with an improved complication profile.
"I switched to transthoracic esophagectomy 5 years ago. One reason was development of the minimally invasive approach. As a result, we?re not scared of a chest anastomosis like we used to be. When patients undergoing transthoracic esophagectomy with thoracotomy had a leak in the chest they had a very high risk for mortality. That?s not the case anymore. We have not observed any mortality associated with a leak in the chest for many, many years now," he said.
The investigators reported having no conflicts of interest.
INDIANAPOLIS - Transthoracic esophagectomy for esophageal cancer provides significantly lower in-hospital mortality and major morbidity rates than does transhiatal esophagectomy, according to an analysis of a large multiyear national database.
Further, in-hospital outcomes of esophagectomy didn?t differ significantly between high-volume centers ? in this study, defined as those doing 10 or more cases per year ? and low-volume centers, Dr. Mehraneh D. Jafari reported at the annual meeting of the American Surgical Association.
That finding was met with skepticism, and discussants were quick to argue that study limitations make it difficult to draw any meaningful conclusions from the data. For one thing, speakers contended that defining a high-volume center based upon an institutional threshold of 10 or more cases per year sets the bar far too low given that a single dedicated esophageal surgery specialist might easily perform 50 or more esophagectomies annually.
Dr. Jafari presented an analysis of 11,473 transthoracic and 3,717 transhiatal esophagectomies performed for esophageal cancer. The data came from the Nationwide Inpatient Sample (NIS) during 2001-2010. The NIS records data on in-hospital outcomes for a nationally representative sample composed of roughly 20% of the country?s hospital discharges each year.
The number of esophagectomies rose steadily by an average of 4% annually during the study years, reflecting the substantial national increase in cases of esophageal cancer. The growing case count, expected to reach an estimated 18,000 cases of esophageal cancer nationwide in 2013, has been attributed to rising rates of gastroesophageal reflux disease, Barrett?s esophagus, and obesity. Transthoracic esophagectomy, used in 76% of cases, remained the preferred operative strategy throughout the study years.
In-hospital outcomes were markedly better in patients who had transthoracic esophagectomy. After adjustment for potential confounding variables in a multivariate analysis, transhiatal esophagectomy recipients had a 67% increased risk of in-hospital mortality and a 39% greater risk of serious complications, including a 37% increased risk of pulmonary complications. However, anastomotic leak rates were similar with both operations, according to Dr. Jafari of the University of California, Irvine.
The referral rate to high-volume esophagectomy centers climbed steadily over time, rising from 22% of all cases in 2001 to 58% in 2010.
The 35 high-volume centers performed an average of 16 cases per year. In contrast, the 484 low-volume centers averaged 2 cases per year. In-hospital mortality among the 9,386 patients treated in low-volume centers averaged 7.6% compared with 4.3% for patients in high-volume centers. Overall in-hospital serious morbidity rates were greater in the low-volume centers as well: 47% versus 41%. While these raw differences were statistically significant, a risk-adjusted multivariate analysis found no significant outcome differences between low- and high-volume centers.
Discussant Dr. Michael J. Zinner noted that in an earlier study he and his coworkers showed that an institutional threshold of roughly 30 esophagectomies per year is required to discriminate between low- and high-volume centers in terms of in-hospital mortality. So why define high-volume centers as those doing a mere 10 cases per year? asked Dr. Zinner, chairman of the department of surgery at Brigham and Women?s Hospital and professor of surgery at Harvard Medical School, Boston.
"The problem here is if you establish 30 cases per year as the threshold for a high-volume center, I can tell you there are probably less than 20 centers in the whole U.S. capable of doing that volume. That?s a real issue, because then how are patients who live in a remote region going to get care at one of those centers?" replied Dr. Jafari?s senior coauthor Dr. Ninh T. Nguyen, professor and vice-chair of surgery at UC Irvine.
"I think instead we should try to lift all boats: Develop a national esophageal center network to identify the qualities reflective of better outcomes in the high-volume centers and introduce those factors at low-volume centers. This way we?re not impeding access to care for our patients," he continued.
Dr. Nguyen said that in-hospital surgical morbidity rates in the NIS need to be taken with a grain of salt, as the accuracy of coding for complications is "rather low." The development of minimally invasive techniques for intrathoracic anastomosis has transformed transthoracic esophagectomy into a procedure with an improved complication profile.
"I switched to transthoracic esophagectomy 5 years ago. One reason was development of the minimally invasive approach. As a result, we?re not scared of a chest anastomosis like we used to be. When patients undergoing transthoracic esophagectomy with thoracotomy had a leak in the chest they had a very high risk for mortality. That?s not the case anymore. We have not observed any mortality associated with a leak in the chest for many, many years now," he said.
The investigators reported having no conflicts of interest.
At the ASA Annual Meeting
Major finding: In-hospital mortality occurred nationally in 5.8% of esophageal cancer patients who underwent transthoracic esophagectomy compared with 8.3% of transhiatal esophagectomy recipients.
Data source: A retrospective study of more than 15,000 patients who underwent esophagectomy for esophageal cancer during 2001-2010 and were Included in the Nationwide Inpatient Sample, a database sponsored by the Agency for Healthcare Research and Quality.
Disclosures: The study presenters reported having no financial conflicts.
FDA okays PCC for warfarin-induced bleeding
The Food and Drug Administration has approved a new agent for the urgent reversal of vitamin K antagonist anticoagulation in adults with acute major bleeding.
Kcentra (Prothrombin Complex Concentrate, Human), manufactured by CSL Behring of King of Prussia, Pa., is a nonactivated 4-factor prothrombin complex concentrate (PCC). It contains the coagulation factors that are low in warfarin-treated patients: factors II (prothrombin), VII, IX, and X. The product also contains antithrombotic proteins C and S. Fresh frozen plasma is the only FDA-approved product for reversing warfarin-induced acute bleeding.Like plasma, Kcentra is used with administration of vitamin K to reverse the anticoagulation effect and stop bleeding. Unlike plasma, Kcentra can be given quickly because it does not require thawing or determination of blood type.
"The FDA’s approval of this new product gives physicians a choice when deciding how to treat patients requiring urgent reversal of VKA [vitamin K antagonist] anticoagulation," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. "Kcentra is administered in a significantly lower volume than plasma at recommended doses, providing an alternative for those patients who may not tolerate the volume of plasma required to reverse VKA anticoagulation."
The American College of Chest Physicians endorsed use of PCC for rapid reversal of VKA-associated bleeding in its 2012 consensus guidelines on anticoagulant therapy (CHEST 2012;141(Suppl):e152S- e184S).
"Kcentra has been shown to restore the decreased vitamin K–dependent clotting factors significantly faster than plasma in patients on warfarin," Dr. Ravi Sarode, the coordinating investigator for the pivotal Kcentra trial and director of transfusion medicine and hemostasis reference laboratory at the University of Texas Southwestern Medical Center, said in a statement issued by CSL Behring.
According to the company, 3-4 million people in the United States each year receive warfarin to prevent clots after a stroke, heart attack, heart valve surgery, or deep vein thrombosis/pulmonary embolism, or for atrial fibrillation. Severe bleeding is possible, however, because of the warfarin-induced clotting factor deficiency. CSL Behring said that some 29,000 emergency department visits annually are for warfarin-associated bleeding.
The FDA said that Kcentra will carry a boxed warning on the risk of blood clots. Patients should be monitored for signs and symptoms of thromboembolic events. "Both fatal and nonfatal arterial and venous thromboembolic complications have been reported in clinical trials and postmarketing surveillance," said the FDA. The warning further states that Kcentra was not studied in subjects who had a thromboembolic event, myocardial infarction, disseminated intravascular coagulation, cerebral vascular accident, transient ischemic attack, unstable angina pectoris, or severe peripheral vascular disease within the prior 3 months, and as such might not be suitable in patients who had any of those events in the 3 months before starting therapy.
Kcentra, made from pooled plasma of healthy donors, is processed to minimize risk of transmitting viral and other diseases, the agency said. It is marketed as Beriplex or Confidex in 25 countries.
Dr. Sarode received compensation as coordinating principal investigator of the study.
The Food and Drug Administration has approved a new agent for the urgent reversal of vitamin K antagonist anticoagulation in adults with acute major bleeding.
Kcentra (Prothrombin Complex Concentrate, Human), manufactured by CSL Behring of King of Prussia, Pa., is a nonactivated 4-factor prothrombin complex concentrate (PCC). It contains the coagulation factors that are low in warfarin-treated patients: factors II (prothrombin), VII, IX, and X. The product also contains antithrombotic proteins C and S. Fresh frozen plasma is the only FDA-approved product for reversing warfarin-induced acute bleeding.Like plasma, Kcentra is used with administration of vitamin K to reverse the anticoagulation effect and stop bleeding. Unlike plasma, Kcentra can be given quickly because it does not require thawing or determination of blood type.
"The FDA’s approval of this new product gives physicians a choice when deciding how to treat patients requiring urgent reversal of VKA [vitamin K antagonist] anticoagulation," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. "Kcentra is administered in a significantly lower volume than plasma at recommended doses, providing an alternative for those patients who may not tolerate the volume of plasma required to reverse VKA anticoagulation."
The American College of Chest Physicians endorsed use of PCC for rapid reversal of VKA-associated bleeding in its 2012 consensus guidelines on anticoagulant therapy (CHEST 2012;141(Suppl):e152S- e184S).
"Kcentra has been shown to restore the decreased vitamin K–dependent clotting factors significantly faster than plasma in patients on warfarin," Dr. Ravi Sarode, the coordinating investigator for the pivotal Kcentra trial and director of transfusion medicine and hemostasis reference laboratory at the University of Texas Southwestern Medical Center, said in a statement issued by CSL Behring.
According to the company, 3-4 million people in the United States each year receive warfarin to prevent clots after a stroke, heart attack, heart valve surgery, or deep vein thrombosis/pulmonary embolism, or for atrial fibrillation. Severe bleeding is possible, however, because of the warfarin-induced clotting factor deficiency. CSL Behring said that some 29,000 emergency department visits annually are for warfarin-associated bleeding.
The FDA said that Kcentra will carry a boxed warning on the risk of blood clots. Patients should be monitored for signs and symptoms of thromboembolic events. "Both fatal and nonfatal arterial and venous thromboembolic complications have been reported in clinical trials and postmarketing surveillance," said the FDA. The warning further states that Kcentra was not studied in subjects who had a thromboembolic event, myocardial infarction, disseminated intravascular coagulation, cerebral vascular accident, transient ischemic attack, unstable angina pectoris, or severe peripheral vascular disease within the prior 3 months, and as such might not be suitable in patients who had any of those events in the 3 months before starting therapy.
Kcentra, made from pooled plasma of healthy donors, is processed to minimize risk of transmitting viral and other diseases, the agency said. It is marketed as Beriplex or Confidex in 25 countries.
Dr. Sarode received compensation as coordinating principal investigator of the study.
The Food and Drug Administration has approved a new agent for the urgent reversal of vitamin K antagonist anticoagulation in adults with acute major bleeding.
Kcentra (Prothrombin Complex Concentrate, Human), manufactured by CSL Behring of King of Prussia, Pa., is a nonactivated 4-factor prothrombin complex concentrate (PCC). It contains the coagulation factors that are low in warfarin-treated patients: factors II (prothrombin), VII, IX, and X. The product also contains antithrombotic proteins C and S. Fresh frozen plasma is the only FDA-approved product for reversing warfarin-induced acute bleeding.Like plasma, Kcentra is used with administration of vitamin K to reverse the anticoagulation effect and stop bleeding. Unlike plasma, Kcentra can be given quickly because it does not require thawing or determination of blood type.
"The FDA’s approval of this new product gives physicians a choice when deciding how to treat patients requiring urgent reversal of VKA [vitamin K antagonist] anticoagulation," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in a statement. "Kcentra is administered in a significantly lower volume than plasma at recommended doses, providing an alternative for those patients who may not tolerate the volume of plasma required to reverse VKA anticoagulation."
The American College of Chest Physicians endorsed use of PCC for rapid reversal of VKA-associated bleeding in its 2012 consensus guidelines on anticoagulant therapy (CHEST 2012;141(Suppl):e152S- e184S).
"Kcentra has been shown to restore the decreased vitamin K–dependent clotting factors significantly faster than plasma in patients on warfarin," Dr. Ravi Sarode, the coordinating investigator for the pivotal Kcentra trial and director of transfusion medicine and hemostasis reference laboratory at the University of Texas Southwestern Medical Center, said in a statement issued by CSL Behring.
According to the company, 3-4 million people in the United States each year receive warfarin to prevent clots after a stroke, heart attack, heart valve surgery, or deep vein thrombosis/pulmonary embolism, or for atrial fibrillation. Severe bleeding is possible, however, because of the warfarin-induced clotting factor deficiency. CSL Behring said that some 29,000 emergency department visits annually are for warfarin-associated bleeding.
The FDA said that Kcentra will carry a boxed warning on the risk of blood clots. Patients should be monitored for signs and symptoms of thromboembolic events. "Both fatal and nonfatal arterial and venous thromboembolic complications have been reported in clinical trials and postmarketing surveillance," said the FDA. The warning further states that Kcentra was not studied in subjects who had a thromboembolic event, myocardial infarction, disseminated intravascular coagulation, cerebral vascular accident, transient ischemic attack, unstable angina pectoris, or severe peripheral vascular disease within the prior 3 months, and as such might not be suitable in patients who had any of those events in the 3 months before starting therapy.
Kcentra, made from pooled plasma of healthy donors, is processed to minimize risk of transmitting viral and other diseases, the agency said. It is marketed as Beriplex or Confidex in 25 countries.
Dr. Sarode received compensation as coordinating principal investigator of the study.
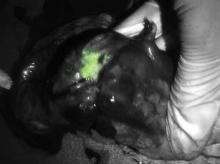
Green glow locates tumors during surgery
NATIONAL HARBOR, MD. - Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the United States and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors -- including noncontiguous pockets of malignancy -- during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, an ACS Fellow of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within 2 centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the NIR portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam" which consists of a light source and NIR camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5-cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal and Dr. Brouwer both reported that they had no disclosures.
NATIONAL HARBOR, MD. - Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the United States and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors -- including noncontiguous pockets of malignancy -- during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, an ACS Fellow of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within 2 centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the NIR portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam" which consists of a light source and NIR camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5-cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal and Dr. Brouwer both reported that they had no disclosures.
NATIONAL HARBOR, MD. - Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the United States and the Netherlands reported in oral and poster sessions.
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors -- including noncontiguous pockets of malignancy -- during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, an ACS Fellow of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within 2 centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the NIR portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam" which consists of a light source and NIR camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5-cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal and Dr. Brouwer both reported that they had no disclosures.
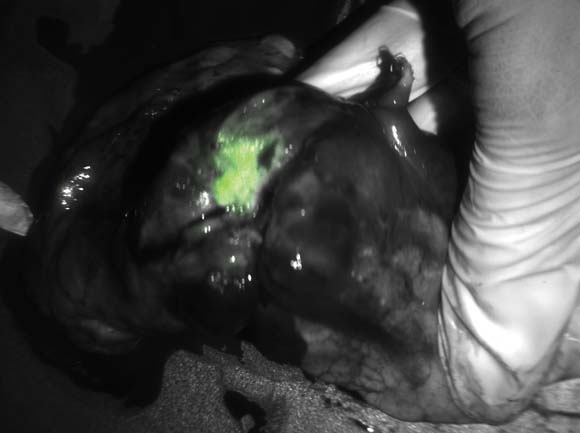
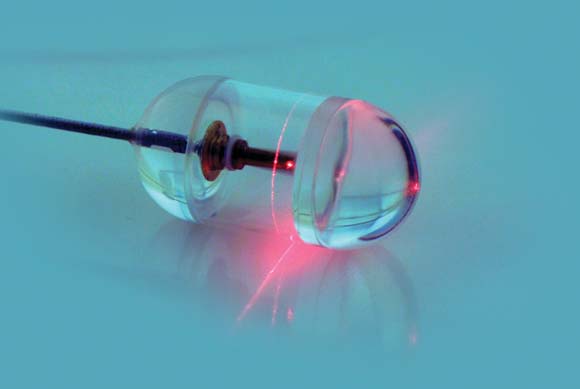
Laser pill shows potential benefits over upper GI endoscopy
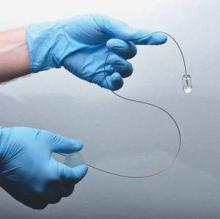
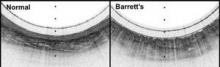
A small, swallowed, laser imaging capsule provides full-thickness imaging of the upper gastro- intestinal tract without biopsy, and is quicker and less invasive than traditional endoscopy, according to the Harvard University research-ers who are developing it.
About the size of a large multivitamin pill, the transparent capsule generates a near-infrared beam that spins rapidly about its circumference during transit. Changes in the reflected light allow cross-sectional imaging of the esophagus in a few minutes. Sequential cross-sections can be compiled into three-dimensional models of the entire lumen (Nat. Med. 2013 Jan. 13 [doi: 10.1038/nm.3052]).
"This system gives us a convenient way to screen for Barrett?s [esophagus] that doesn?t require patient sedation, a specialized setting and equipment, or a physician who has been trained in endoscopy. By showing the three-dimensional, microscopic structure of the esophageal lining, it reveals much more detail than can be seen with even high-resolution endoscopy. The images produced have been some of the best we have seen of the esophagus," investigator Dr. Guillermo Tearney, a Harvard Medical School pathology professor and the associate director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said in a statement.
The capsule is on a tether, which carries its fiber optic line and laser driveshaft and helps with positioning. The capsule is pulled up and out after use, and disinfected for the next patient.
In early testing, 15 cm of esophagus in seven healthy and six Barrett?s esophagus patients was imaged in a mean of 58 seconds; it took about 6 minutes to make two down- and two up-transits. The technique, dubbed tethered capsule endomicroscopy, clearly distinguished the cellular abnormalities of Barrett?s. Standard upper GI endoscopy takes about 90 minutes.
"We originally were concerned that we might miss a lot of data because of the small size of the capsule, but we were surprised to find that, once the pill has been swallowed, it is firmly grasped by the esophagus, allowing complete microscopic imaging of the entire wall," Dr. Tearney said.
There were no complications, and 12 of the 13 subjects said they preferred the capsule to previous endoscopies.
"Because the tethered endomicroscopy pill traverses the gastrointestinal tract without visual guidance, the training required to conduct the procedure is minimal. This fact, combined with the brevity and ease with which the procedure is performed, will enable internal microscopic imaging in almost any health care setting, including in the office of the primary care physician," Dr. Tearney and his colleagues wrote in their paper.
The research was supported by grants from the National Institutes of Health. The researchers said they had no disclosures.
A small, swallowed, laser imaging capsule provides full-thickness imaging of the upper gastro- intestinal tract without biopsy, and is quicker and less invasive than traditional endoscopy, according to the Harvard University research-ers who are developing it.
About the size of a large multivitamin pill, the transparent capsule generates a near-infrared beam that spins rapidly about its circumference during transit. Changes in the reflected light allow cross-sectional imaging of the esophagus in a few minutes. Sequential cross-sections can be compiled into three-dimensional models of the entire lumen (Nat. Med. 2013 Jan. 13 [doi: 10.1038/nm.3052]).
"This system gives us a convenient way to screen for Barrett?s [esophagus] that doesn?t require patient sedation, a specialized setting and equipment, or a physician who has been trained in endoscopy. By showing the three-dimensional, microscopic structure of the esophageal lining, it reveals much more detail than can be seen with even high-resolution endoscopy. The images produced have been some of the best we have seen of the esophagus," investigator Dr. Guillermo Tearney, a Harvard Medical School pathology professor and the associate director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said in a statement.
The capsule is on a tether, which carries its fiber optic line and laser driveshaft and helps with positioning. The capsule is pulled up and out after use, and disinfected for the next patient.
In early testing, 15 cm of esophagus in seven healthy and six Barrett?s esophagus patients was imaged in a mean of 58 seconds; it took about 6 minutes to make two down- and two up-transits. The technique, dubbed tethered capsule endomicroscopy, clearly distinguished the cellular abnormalities of Barrett?s. Standard upper GI endoscopy takes about 90 minutes.
"We originally were concerned that we might miss a lot of data because of the small size of the capsule, but we were surprised to find that, once the pill has been swallowed, it is firmly grasped by the esophagus, allowing complete microscopic imaging of the entire wall," Dr. Tearney said.
There were no complications, and 12 of the 13 subjects said they preferred the capsule to previous endoscopies.
"Because the tethered endomicroscopy pill traverses the gastrointestinal tract without visual guidance, the training required to conduct the procedure is minimal. This fact, combined with the brevity and ease with which the procedure is performed, will enable internal microscopic imaging in almost any health care setting, including in the office of the primary care physician," Dr. Tearney and his colleagues wrote in their paper.
The research was supported by grants from the National Institutes of Health. The researchers said they had no disclosures.
A small, swallowed, laser imaging capsule provides full-thickness imaging of the upper gastro- intestinal tract without biopsy, and is quicker and less invasive than traditional endoscopy, according to the Harvard University research-ers who are developing it.
About the size of a large multivitamin pill, the transparent capsule generates a near-infrared beam that spins rapidly about its circumference during transit. Changes in the reflected light allow cross-sectional imaging of the esophagus in a few minutes. Sequential cross-sections can be compiled into three-dimensional models of the entire lumen (Nat. Med. 2013 Jan. 13 [doi: 10.1038/nm.3052]).
"This system gives us a convenient way to screen for Barrett?s [esophagus] that doesn?t require patient sedation, a specialized setting and equipment, or a physician who has been trained in endoscopy. By showing the three-dimensional, microscopic structure of the esophageal lining, it reveals much more detail than can be seen with even high-resolution endoscopy. The images produced have been some of the best we have seen of the esophagus," investigator Dr. Guillermo Tearney, a Harvard Medical School pathology professor and the associate director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said in a statement.
The capsule is on a tether, which carries its fiber optic line and laser driveshaft and helps with positioning. The capsule is pulled up and out after use, and disinfected for the next patient.
In early testing, 15 cm of esophagus in seven healthy and six Barrett?s esophagus patients was imaged in a mean of 58 seconds; it took about 6 minutes to make two down- and two up-transits. The technique, dubbed tethered capsule endomicroscopy, clearly distinguished the cellular abnormalities of Barrett?s. Standard upper GI endoscopy takes about 90 minutes.
"We originally were concerned that we might miss a lot of data because of the small size of the capsule, but we were surprised to find that, once the pill has been swallowed, it is firmly grasped by the esophagus, allowing complete microscopic imaging of the entire wall," Dr. Tearney said.
There were no complications, and 12 of the 13 subjects said they preferred the capsule to previous endoscopies.
"Because the tethered endomicroscopy pill traverses the gastrointestinal tract without visual guidance, the training required to conduct the procedure is minimal. This fact, combined with the brevity and ease with which the procedure is performed, will enable internal microscopic imaging in almost any health care setting, including in the office of the primary care physician," Dr. Tearney and his colleagues wrote in their paper.
The research was supported by grants from the National Institutes of Health. The researchers said they had no disclosures.
Major Finding: In early testing, 15 cm of esophagus was imaged in a mean of 58 seconds and clearly distinguished the cellular abnormalities of Barrett?s esophagus; it took about 6 minutes to make two down- and two up-transits.
Data Source: A pilot study to image the esophagus in seven healthy patients and six with Barrett?s esophagus.
Disclosures: The research was supported by grants from the National Institutes of Health. The investigators said they had no disclosures.
Study: Early esophageal cancer staging suspect
LOS ANGELES – Clinical staging of T2N0 esophageal cancer remains unreliable, despite advances in staging techniques, a study has shown.
The addition of endoscopic ultrasound and PET/CT has improved the ability to clinically stage esophageal cancer overall, but clinical staging of T2N0 disease has generally been less reliable than staging of more advanced disease. The subset of patients with T2N0 disease, which accounts for only a small portion of esophageal resections, has been a difficult group to study because single-center investigations involve a limited number of patients, Dr. Traves D. Crabtree said at the annual meeting of the Society of Thoracic Surgeons in the prestigious Richard E. Clark Paper for General Thoracic Surgery.
Dr. Crabtree of Washington University, St. Louis, and his colleagues examined the adequacy of clinical staging of T2N0 disease using the Society of Thoracic Surgeons (STS) General Thoracic Surgery Database.
The researchers identified 810 patients clinically staged as T2N0 from 2002 to 2011 and excluded 58 because of inadequate pathologic staging data. Clinical stage, pathologic stage, and preoperative characteristics were recorded for each patient and multivariable analysis was used to identify factors associated with upstaging at the time of surgery.
Among 752 patients with clinically staged T2N0, the investigators found that 482 went directly to surgery. Of these, 27.4% (132) were confirmed as pathologic T2N0. A total of 25.9% (125) were downstaged (T1N0), while 46.7% (225) were upstaged (T3-4N0 or TanyN1-3).
Tumor depth (pT3-4) accounted for 18.2% of upstaging while nodal upstaging occurred in approximately 82%. When logistic regression was used, male sex was associated with upstaging (odds ratio = 1.85, P = .024). By analyzing the part of the database that included tumor grade (between the years 2009 and 2011), the investigators found that a higher histologic grade was significantly associated with upstaging (P = .004).
"Over one-third of surgeons have opted to treat T2N0 disease with induction therapy, despite the fact that one-quarter of these patients will be pT1N0," he said.
"This is the first large-scale multi-institutional study of clinical T2N0 patients using the STS General Thoracic Surgery Database. These data highlight the inaccuracy associated with clinical staging of T2N0 esophageal cancer and may influence the surgeon’s decision-making process in choosing a treatment regimen for these patients," Dr. Crabtree added in an interview.
"Given the current limitations of clinical staging of T2N0 patients, the incidence of occult nodal disease, and the similar perioperative outcomes among patients treated with and without induction therapy, these patients may more likely be treated with induction therapy in the future. Additional studies are needed to compare long-term outcomes between patients receiving induction therapy, vs. those clinical T2N0 patients going directly to surgery, before a definitive recommendation can be made," he concluded.
Dr. Crabtree reported that he had no relevant financial disclosures.
LOS ANGELES – Clinical staging of T2N0 esophageal cancer remains unreliable, despite advances in staging techniques, a study has shown.
The addition of endoscopic ultrasound and PET/CT has improved the ability to clinically stage esophageal cancer overall, but clinical staging of T2N0 disease has generally been less reliable than staging of more advanced disease. The subset of patients with T2N0 disease, which accounts for only a small portion of esophageal resections, has been a difficult group to study because single-center investigations involve a limited number of patients, Dr. Traves D. Crabtree said at the annual meeting of the Society of Thoracic Surgeons in the prestigious Richard E. Clark Paper for General Thoracic Surgery.
Dr. Crabtree of Washington University, St. Louis, and his colleagues examined the adequacy of clinical staging of T2N0 disease using the Society of Thoracic Surgeons (STS) General Thoracic Surgery Database.
The researchers identified 810 patients clinically staged as T2N0 from 2002 to 2011 and excluded 58 because of inadequate pathologic staging data. Clinical stage, pathologic stage, and preoperative characteristics were recorded for each patient and multivariable analysis was used to identify factors associated with upstaging at the time of surgery.
Among 752 patients with clinically staged T2N0, the investigators found that 482 went directly to surgery. Of these, 27.4% (132) were confirmed as pathologic T2N0. A total of 25.9% (125) were downstaged (T1N0), while 46.7% (225) were upstaged (T3-4N0 or TanyN1-3).
Tumor depth (pT3-4) accounted for 18.2% of upstaging while nodal upstaging occurred in approximately 82%. When logistic regression was used, male sex was associated with upstaging (odds ratio = 1.85, P = .024). By analyzing the part of the database that included tumor grade (between the years 2009 and 2011), the investigators found that a higher histologic grade was significantly associated with upstaging (P = .004).
"Over one-third of surgeons have opted to treat T2N0 disease with induction therapy, despite the fact that one-quarter of these patients will be pT1N0," he said.
"This is the first large-scale multi-institutional study of clinical T2N0 patients using the STS General Thoracic Surgery Database. These data highlight the inaccuracy associated with clinical staging of T2N0 esophageal cancer and may influence the surgeon’s decision-making process in choosing a treatment regimen for these patients," Dr. Crabtree added in an interview.
"Given the current limitations of clinical staging of T2N0 patients, the incidence of occult nodal disease, and the similar perioperative outcomes among patients treated with and without induction therapy, these patients may more likely be treated with induction therapy in the future. Additional studies are needed to compare long-term outcomes between patients receiving induction therapy, vs. those clinical T2N0 patients going directly to surgery, before a definitive recommendation can be made," he concluded.
Dr. Crabtree reported that he had no relevant financial disclosures.
LOS ANGELES – Clinical staging of T2N0 esophageal cancer remains unreliable, despite advances in staging techniques, a study has shown.
The addition of endoscopic ultrasound and PET/CT has improved the ability to clinically stage esophageal cancer overall, but clinical staging of T2N0 disease has generally been less reliable than staging of more advanced disease. The subset of patients with T2N0 disease, which accounts for only a small portion of esophageal resections, has been a difficult group to study because single-center investigations involve a limited number of patients, Dr. Traves D. Crabtree said at the annual meeting of the Society of Thoracic Surgeons in the prestigious Richard E. Clark Paper for General Thoracic Surgery.
Dr. Crabtree of Washington University, St. Louis, and his colleagues examined the adequacy of clinical staging of T2N0 disease using the Society of Thoracic Surgeons (STS) General Thoracic Surgery Database.
The researchers identified 810 patients clinically staged as T2N0 from 2002 to 2011 and excluded 58 because of inadequate pathologic staging data. Clinical stage, pathologic stage, and preoperative characteristics were recorded for each patient and multivariable analysis was used to identify factors associated with upstaging at the time of surgery.
Among 752 patients with clinically staged T2N0, the investigators found that 482 went directly to surgery. Of these, 27.4% (132) were confirmed as pathologic T2N0. A total of 25.9% (125) were downstaged (T1N0), while 46.7% (225) were upstaged (T3-4N0 or TanyN1-3).
Tumor depth (pT3-4) accounted for 18.2% of upstaging while nodal upstaging occurred in approximately 82%. When logistic regression was used, male sex was associated with upstaging (odds ratio = 1.85, P = .024). By analyzing the part of the database that included tumor grade (between the years 2009 and 2011), the investigators found that a higher histologic grade was significantly associated with upstaging (P = .004).
"Over one-third of surgeons have opted to treat T2N0 disease with induction therapy, despite the fact that one-quarter of these patients will be pT1N0," he said.
"This is the first large-scale multi-institutional study of clinical T2N0 patients using the STS General Thoracic Surgery Database. These data highlight the inaccuracy associated with clinical staging of T2N0 esophageal cancer and may influence the surgeon’s decision-making process in choosing a treatment regimen for these patients," Dr. Crabtree added in an interview.
"Given the current limitations of clinical staging of T2N0 patients, the incidence of occult nodal disease, and the similar perioperative outcomes among patients treated with and without induction therapy, these patients may more likely be treated with induction therapy in the future. Additional studies are needed to compare long-term outcomes between patients receiving induction therapy, vs. those clinical T2N0 patients going directly to surgery, before a definitive recommendation can be made," he concluded.
Dr. Crabtree reported that he had no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE SOCIETY OF THORACIC SURGEONS
Major Finding: Of 482 patients who went directly to surgery, 26% were downstaged, while 47% were upstaged.
Data Source: A retrospective, database analysis of 810 patients clinically staged as T2N0 from 2002 to 2011.
Disclosures: Dr. Crabtree reported that he had no relevant financial disclosures.
Targeted CT follow-up for incidental lung nodules?
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional x-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York–Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex.
Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported grants from several imaging companies.
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional x-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York–Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex.
Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported grants from several imaging companies.
CHICAGO – Limiting CT follow-up of incidental pulmonary nodules to a small area around the suspicious nodule may help resolve a common clinical dilemma and an Achilles heel of lung cancer screening, researchers suggest.
It could also reduce the radiation dose by more than 80%.
"Why should we radiate the entire thorax on follow-up?" Dr. Gregory D. Pearson asked rhetorically at the annual meeting of the Radiological Society of North America.
In the pivotal National Lung Cancer Screening Trial, annual low-dose CT reduced lung cancer deaths by 20% and all-cause mortality by 6.7% among heavy smokers, compared with traditional x-rays. Approximately 40% of the CT group, however, had findings of small, indeterminate pulmonary nodules considered suspicious for lung cancer on at least one scan, with 1.4% experiencing a complication as a result of additional testing (N. Engl. J. Med. 2011;365:395-409).
Several societies are working to devise the best protocol for further workup of detected nodules, but none have come up with the solution. The Fleischner Society, an international society for thoracic radiology, previously proposed serial follow-up imaging at intervals of less than 1 year for solid nodules smaller than 8 mm detected incidentally at nonscreening CT (Radiology 2005;237:395-400). For all semisolid nodules and ground-glass nodules at least 5 mm in size, researchers recommended a 3-month follow-up (Radiology 2005;237:395-400).
Follow-up CT scans, however, add costs and contribute to a patient’s cumulative radiation burden, said Dr. Pearson, a thoracic radiologist at New York–Presbyterian Hospital/Columbia University in New York City.
In an effort to develop a more practical solution, Dr. Pearson and his colleagues analyzed the variability in nodule location among 50 patients with subcentimeter nodules identified on CT screening for lung cancer and emphysema, and then devised a protocol for targeted CT follow-up that was validated in 50 additional patients.
Two experts and one novice reader, a medical student, independently measured the distances of the nodules from two anatomical landmarks, the lung apex and carina, on baseline and follow-up scans by cross-referencing the axial images with the CT scanogram on a PACS (picture archiving and communication system) workstation.
The interobserver variability was quite low, with mean differences of just 2-3 mm when the two experts were paired together or individually paired with the novice reader, Dr. Pearson said. Results were significantly better measuring from the apex than from the carina for two of the three reader pairings (P = .005 and .03), although the absolute difference was just 1 mm.
To allow for a greater margin of error, measurements in the validation phase of the study were only from the ipsilateral lung apex and covered a 60-mm range. At baseline, the expert identified the nodule and placed a cut line on the scan to measure the distance from the apex.
Medical students then measured the distance of the nodule from the apex on the follow-up scan, and reviewed a region of about 6 cm to determine whether the nodule would have been included in its entirety if the range of the CT scan had been narrowed to just 60 mm.
"The results here are pretty simple; 100% of the nodules in follow-up were scanned in their entirety," Dr. Pearson said.
The average craniocaudal coverage on follow-up CT was 363 mm.
By using a targeted 60-mm range, the average craniocaudal coverage and radiation dose would be reduced by 83%, although the actual dose reduction will depend on the location of the nodules, he added.
Still, the technique needs to be validated prospectively in larger groups, and would require buy-in from radiologists, medical societies, and Medicare and private insurers, Dr. Pearson said.
Session comoderator Dr. H. Page McAdams, division chief of cardiac and thoracic imaging at Duke University in Durham, N.C., said in an interview that the concept is intriguing, but raises a number of potential societal, reimbursement, and medical-legal issues.
Roughly 75% of the 100 consecutive patients in the study had a single nodule, Dr. Pearson told this publication.
Dr. McAdams reported grants from several imaging companies.
Major Finding: By using a targeted 60-mm range during CT follow-up of suspicious nodules, the average craniocaudal coverage and radiation dose would be reduced by 83%.
Data Source: Two-phase validation study in 100 consecutive patients with incidental subcentimeter lung nodules.
Disclosures: Dr. McAdams reported a research grant from General Electric, serving as a consultant for American College of Radiology Image Metrix, and working as an author for Reed Elsevier and UpToDate Inc.
COPD varies by state, peaks above 9%
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The prevalence of chronic obstructive pulmonary disease is 6% nationwide, but varies from less than 4% in Washington and Minnesota to more than 9% in Alabama and Kentucky, according to data from the Centers for Disease Control and Prevention. The findings were published in the CDC’s Morbidity and Mortality Weekly Report.
A total of 13,306 adults who reported having chronic obstructive pulmonary disease (COPD) in the national survey also responded to the COPD module. Of these, 76% reported undergoing a diagnostic breathing test, 64% reported that COPD symptoms (specifically shortness of breath) had an adverse effect on their quality of life, and 51% reported taking at least one COPD medication (MMWR 2012;61:938-43).
In age-adjusted comparisons, women were more likely to report COPD compared with men (7% vs. 5%, respectively). COPD prevalence decreased from an average of 10% among individuals making less than $25,000 per year to 3% in those making more than $75,000 per year, and the prevalence was lower among employed individuals, homemakers, and students compared with those who were unemployed, retired, or otherwise unable to work. The prevalence of COPD was highest in current smokers (13%) compared with former smokers (7%) and never smokers (3%).
Data were taken from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey. Additional COPD data were collected in an optional COPD module about COPD diagnosis and quality of life. This module was part of the BRFSS in 21 states, the District of Columbia, and Puerto Rico.
The 2011 BRFSS was conducted via telephone, either landline or mobile. The survey population included adults aged 18 years and older throughout the United States.
The findings were limited by several factors including the absence of data on individuals in institutions or nursing homes and by the use of self-reports for COPD diagnosis, the researchers said. However, the report is the first to analyze data on COPD prevalence in all 50 states, the District of Columbia, and Puerto Rico, they noted. State-level health officials should focus surveillance efforts, educational campaigns, and interventions on areas of highest COPD prevalence, they added.
The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Major Finding: The overall prevalence of chronic obstructive pulmonary disease in the United States is approximately 6%.
Data Source: The data come from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) survey.
Disclosures: The study was supported by the CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Stereotactic body radiation boosts NSCLC survival
BOSTON – Delivering stereotactic body radiation for early-stage, inoperable non–small cell lung cancer doubled overall survival rates achieved in historical series with conventional radiation, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 3-year overall survival rate reached 59.9% for 100 patients whose stage IA non–small cell lung cancer (NSCLC) was treated with stereotactic body radiation therapy (SBRT), said Dr. Yasushi Nagata. He compared results of the nonrandomized phase II trial with 31%-39% in historical series with conventional radiation.
The 5-year overall survival rate was 40.8%, compared with 13%-22.2% historically, added Dr. Nagata from Hiroshima University, Japan.
He described SBRT as well tolerated with only mild toxicities, making it a suitable alternative to other therapies, particularly in older patients. "Patients with early inoperable lung cancer should consider this treatment," Dr. Nagata advised in a briefing.
The investigators concluded that the treatment should be the new standard, replacing conventional radiotherapy in this population.
Similar in concept to stereotactic radiosurgery with a cyberknife, SBRT is a technique for precise high-dose targeting of tissues from multiple angles and planes, allowing delivery of much larger doses by fraction than conformal 3-dimensional or intensity-modulated radiation therapy. With SBRT, radiation therapy sessions can often be compressed into as little as 4-6 fractions delivered over 2 to 2.5 weeks, compared with 8 to 9 weeks of daily fractions for other techniques.
The phase II Japanese Clinical Oncology Group trial, JCOG-0403, is said to be the first to evaluate SBRT in both operable and nonoperable NSCLC. At the 2010 ASTRO annual meeting, the investigators reported 3-year survival rates for 64 patients with surgically resectable NSCLC: overall survival was 76%; progression-free survival, 54.5%; local progression-free survival, 68.5%; and event-free survival, 51.4%.
In the current study, 77 men and 27 women with a median age of 78 years (range 59-90 years) were enrolled; four patients were later excluded from the study, three because they developed a second primary cancer.
The median tumor size was 21 mm (range 9-30 mm). Fifty patients had adenocarcinomas, 40 had squamous cell carcinomas, and 14 had other tumor histologies. All patients had histologically or cytologically proven NSCLC, clinical T1N0M0 disease, and were determined by thoracic surgeons to be inoperable.
All patients completed the treatment protocol, consisting of a dose of 48 Gy at the isocenter divided into 4 fractions over 4-8 days.
The progression-free survival rate at 3 years was 49.8%; the local progression-free survival rate was 52.8%, and event-free survival, 46.8%.
Dr. Nagata and Dr. Chang disclosed no relevant conflicts.
BOSTON – Delivering stereotactic body radiation for early-stage, inoperable non–small cell lung cancer doubled overall survival rates achieved in historical series with conventional radiation, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 3-year overall survival rate reached 59.9% for 100 patients whose stage IA non–small cell lung cancer (NSCLC) was treated with stereotactic body radiation therapy (SBRT), said Dr. Yasushi Nagata. He compared results of the nonrandomized phase II trial with 31%-39% in historical series with conventional radiation.
The 5-year overall survival rate was 40.8%, compared with 13%-22.2% historically, added Dr. Nagata from Hiroshima University, Japan.
He described SBRT as well tolerated with only mild toxicities, making it a suitable alternative to other therapies, particularly in older patients. "Patients with early inoperable lung cancer should consider this treatment," Dr. Nagata advised in a briefing.
The investigators concluded that the treatment should be the new standard, replacing conventional radiotherapy in this population.
Similar in concept to stereotactic radiosurgery with a cyberknife, SBRT is a technique for precise high-dose targeting of tissues from multiple angles and planes, allowing delivery of much larger doses by fraction than conformal 3-dimensional or intensity-modulated radiation therapy. With SBRT, radiation therapy sessions can often be compressed into as little as 4-6 fractions delivered over 2 to 2.5 weeks, compared with 8 to 9 weeks of daily fractions for other techniques.
The phase II Japanese Clinical Oncology Group trial, JCOG-0403, is said to be the first to evaluate SBRT in both operable and nonoperable NSCLC. At the 2010 ASTRO annual meeting, the investigators reported 3-year survival rates for 64 patients with surgically resectable NSCLC: overall survival was 76%; progression-free survival, 54.5%; local progression-free survival, 68.5%; and event-free survival, 51.4%.
In the current study, 77 men and 27 women with a median age of 78 years (range 59-90 years) were enrolled; four patients were later excluded from the study, three because they developed a second primary cancer.
The median tumor size was 21 mm (range 9-30 mm). Fifty patients had adenocarcinomas, 40 had squamous cell carcinomas, and 14 had other tumor histologies. All patients had histologically or cytologically proven NSCLC, clinical T1N0M0 disease, and were determined by thoracic surgeons to be inoperable.
All patients completed the treatment protocol, consisting of a dose of 48 Gy at the isocenter divided into 4 fractions over 4-8 days.
The progression-free survival rate at 3 years was 49.8%; the local progression-free survival rate was 52.8%, and event-free survival, 46.8%.
Dr. Nagata and Dr. Chang disclosed no relevant conflicts.
BOSTON – Delivering stereotactic body radiation for early-stage, inoperable non–small cell lung cancer doubled overall survival rates achieved in historical series with conventional radiation, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 3-year overall survival rate reached 59.9% for 100 patients whose stage IA non–small cell lung cancer (NSCLC) was treated with stereotactic body radiation therapy (SBRT), said Dr. Yasushi Nagata. He compared results of the nonrandomized phase II trial with 31%-39% in historical series with conventional radiation.
The 5-year overall survival rate was 40.8%, compared with 13%-22.2% historically, added Dr. Nagata from Hiroshima University, Japan.
He described SBRT as well tolerated with only mild toxicities, making it a suitable alternative to other therapies, particularly in older patients. "Patients with early inoperable lung cancer should consider this treatment," Dr. Nagata advised in a briefing.
The investigators concluded that the treatment should be the new standard, replacing conventional radiotherapy in this population.
Similar in concept to stereotactic radiosurgery with a cyberknife, SBRT is a technique for precise high-dose targeting of tissues from multiple angles and planes, allowing delivery of much larger doses by fraction than conformal 3-dimensional or intensity-modulated radiation therapy. With SBRT, radiation therapy sessions can often be compressed into as little as 4-6 fractions delivered over 2 to 2.5 weeks, compared with 8 to 9 weeks of daily fractions for other techniques.
The phase II Japanese Clinical Oncology Group trial, JCOG-0403, is said to be the first to evaluate SBRT in both operable and nonoperable NSCLC. At the 2010 ASTRO annual meeting, the investigators reported 3-year survival rates for 64 patients with surgically resectable NSCLC: overall survival was 76%; progression-free survival, 54.5%; local progression-free survival, 68.5%; and event-free survival, 51.4%.
In the current study, 77 men and 27 women with a median age of 78 years (range 59-90 years) were enrolled; four patients were later excluded from the study, three because they developed a second primary cancer.
The median tumor size was 21 mm (range 9-30 mm). Fifty patients had adenocarcinomas, 40 had squamous cell carcinomas, and 14 had other tumor histologies. All patients had histologically or cytologically proven NSCLC, clinical T1N0M0 disease, and were determined by thoracic surgeons to be inoperable.
All patients completed the treatment protocol, consisting of a dose of 48 Gy at the isocenter divided into 4 fractions over 4-8 days.
The progression-free survival rate at 3 years was 49.8%; the local progression-free survival rate was 52.8%, and event-free survival, 46.8%.
Dr. Nagata and Dr. Chang disclosed no relevant conflicts.
Major Finding: The 3-year overall survival rate for 100 patients with stage IA NSCLC treated with stereotactic body radiation therapy was 59.9%, compared with 31%-39% for conventional radiation.
Data Source: This was a nonrandomized phase II trial.
Disclosures: The study was supported by Japan’s Ministry of Health. Dr. Nagata and Dr. Chang disclosed no relevant conflicts of interest.
Crizotinib changes practice for ALK-positive NSCLC
VIENNA – Long-awaited data from the phase III PROFILE 1007 confirm that crizotinib provides superior progression-free survival and responses, compared with second-line chemo-therapy in advanced anaplastic lymphoma kinase–positive non–small cell lung cancer.
Median progression-free survival more than doubled from 3.0 months with single-agent chemotherapy to 7.7 months with crizotinib, according to an independent radiologic review (P value less than .0001; hazard ratio, 0.49). Crizotinib (Xalkori) remained superior regardless of whether chemotherapy contained docetaxel (Taxotere) (7.7 vs. 2.6 months; P less than .0001) or pemetrexed (Alimta) (7.7 vs. 4.2; P = .0004), an agent previously shown to be effective against ALK-positive NSCLC.
The overall response rate was 65.3% for crizotinib and 19.5% for chemotherapy in the intent to treat population of 347 patients (overall response rate ratio 3.4; P less than .0001).
Crizotinib was also associated with significantly greater improvement in lung cancer symptoms and quality of life, Dr. Alice Shaw said at the European Society for Medical Oncology Congress. "Taken together, these results establish crizotinib as the standard of care for patients with advanced, previously treated ALK-positive non–small cell lung cancer."
ALK rearrangements are present in about 5% of lung cancers, typically in younger, never smokers.
Overall survival in the study was 22.8 months for chemotherapy and 20.3 months for crizotinib (P = .5394; HR, 1.02). The interim survival analysis was immature with just 40% of expected deaths reported and likely confounded by the high number (87%) of chemotherapy patients who crossed over to crizotinib after progression, she noted. After adjusting for crossover, the hazard ratio suggests a survival advantage with crizotinib (HR, 0.83).
Discussant Jean-Charles Soria of Institut Gustave Roussy, Villejuif, France, agreed and said the survival times in either arm were impressive, observing that just 2 years ago survival in second-line ALK-positive NSCLC was just 9 months.
Crizotinib, an oral, first in class ALK inhibitor, was given accelerated approval in 2011 in the United States to treat advanced ALK-positive NSCLC but is not approved in Europe, where regulatory agencies have required data from the randomized trial.
Dr. Soria said that worldwide use of crizotinib will require that several financial and practical issues surrounding implementation of molecular testing in daily practice be addressed including the optimal technique, type of sample, and tissue availability.
Testing for epidermal growth factor receptor, another molecular alteration that directs targeted therapy in lung cancer, "should not compete with ALK," he said, adding that multiplexing test strategies "are key."
Investigators at 105 sites across 21 countries randomized 173 patients to crizotinib 250 mg twice-daily in a 21-day cycle and 174 patients to chemotherapy containing pemetrexed 500 mg/m2 or docetaxel 75 mg/m2 given intravenously on day 1 of a 21-day cycle.
Treatment duration varied significantly, with patients receiving a median of 11 cycles of crizotinib vs. 4 cycles of chemotherapy. This may have influenced the higher number of all-cause deaths among crizotinib patients (25 deaths vs. 7 deaths), said Dr. Shaw, a thoracic oncologist at Massachusetts General Hospital Cancer Center in Boston.
Crizotinib patients were more likely than chemotherapy patients to experience visual disturbances (any grade 60% vs. 9%), as well as diarrhea, nausea, elevated transaminases (16% grade 3/4 ), edema, upper respiratory infection, dysgeusia, and dizziness. In contrast, fatigue, alopecia, dyspnea, and rash were more common with chemotherapy.
Despite the fact that patients on crizotinib experienced more nausea and vomiting, antiemetic use was significantly higher in the chemotherapy arm (67% vs. 20%). Based on the EORTC Quality of Life Questionnaire (QLQ C-30) and QLQ-LC 13, crizotinib patients had greater improvement from baseline in cough, dyspnea, fatigue, alopecia, insomnia, and pain as well as global quality of life (both P less than .0001).
Dr. Soria reported financial relationshisps with several firms including Pfizer, the study sponsor.
VIENNA – Long-awaited data from the phase III PROFILE 1007 confirm that crizotinib provides superior progression-free survival and responses, compared with second-line chemo-therapy in advanced anaplastic lymphoma kinase–positive non–small cell lung cancer.
Median progression-free survival more than doubled from 3.0 months with single-agent chemotherapy to 7.7 months with crizotinib, according to an independent radiologic review (P value less than .0001; hazard ratio, 0.49). Crizotinib (Xalkori) remained superior regardless of whether chemotherapy contained docetaxel (Taxotere) (7.7 vs. 2.6 months; P less than .0001) or pemetrexed (Alimta) (7.7 vs. 4.2; P = .0004), an agent previously shown to be effective against ALK-positive NSCLC.
The overall response rate was 65.3% for crizotinib and 19.5% for chemotherapy in the intent to treat population of 347 patients (overall response rate ratio 3.4; P less than .0001).
Crizotinib was also associated with significantly greater improvement in lung cancer symptoms and quality of life, Dr. Alice Shaw said at the European Society for Medical Oncology Congress. "Taken together, these results establish crizotinib as the standard of care for patients with advanced, previously treated ALK-positive non–small cell lung cancer."
ALK rearrangements are present in about 5% of lung cancers, typically in younger, never smokers.
Overall survival in the study was 22.8 months for chemotherapy and 20.3 months for crizotinib (P = .5394; HR, 1.02). The interim survival analysis was immature with just 40% of expected deaths reported and likely confounded by the high number (87%) of chemotherapy patients who crossed over to crizotinib after progression, she noted. After adjusting for crossover, the hazard ratio suggests a survival advantage with crizotinib (HR, 0.83).
Discussant Jean-Charles Soria of Institut Gustave Roussy, Villejuif, France, agreed and said the survival times in either arm were impressive, observing that just 2 years ago survival in second-line ALK-positive NSCLC was just 9 months.
Crizotinib, an oral, first in class ALK inhibitor, was given accelerated approval in 2011 in the United States to treat advanced ALK-positive NSCLC but is not approved in Europe, where regulatory agencies have required data from the randomized trial.
Dr. Soria said that worldwide use of crizotinib will require that several financial and practical issues surrounding implementation of molecular testing in daily practice be addressed including the optimal technique, type of sample, and tissue availability.
Testing for epidermal growth factor receptor, another molecular alteration that directs targeted therapy in lung cancer, "should not compete with ALK," he said, adding that multiplexing test strategies "are key."
Investigators at 105 sites across 21 countries randomized 173 patients to crizotinib 250 mg twice-daily in a 21-day cycle and 174 patients to chemotherapy containing pemetrexed 500 mg/m2 or docetaxel 75 mg/m2 given intravenously on day 1 of a 21-day cycle.
Treatment duration varied significantly, with patients receiving a median of 11 cycles of crizotinib vs. 4 cycles of chemotherapy. This may have influenced the higher number of all-cause deaths among crizotinib patients (25 deaths vs. 7 deaths), said Dr. Shaw, a thoracic oncologist at Massachusetts General Hospital Cancer Center in Boston.
Crizotinib patients were more likely than chemotherapy patients to experience visual disturbances (any grade 60% vs. 9%), as well as diarrhea, nausea, elevated transaminases (16% grade 3/4 ), edema, upper respiratory infection, dysgeusia, and dizziness. In contrast, fatigue, alopecia, dyspnea, and rash were more common with chemotherapy.
Despite the fact that patients on crizotinib experienced more nausea and vomiting, antiemetic use was significantly higher in the chemotherapy arm (67% vs. 20%). Based on the EORTC Quality of Life Questionnaire (QLQ C-30) and QLQ-LC 13, crizotinib patients had greater improvement from baseline in cough, dyspnea, fatigue, alopecia, insomnia, and pain as well as global quality of life (both P less than .0001).
Dr. Soria reported financial relationshisps with several firms including Pfizer, the study sponsor.
VIENNA – Long-awaited data from the phase III PROFILE 1007 confirm that crizotinib provides superior progression-free survival and responses, compared with second-line chemo-therapy in advanced anaplastic lymphoma kinase–positive non–small cell lung cancer.
Median progression-free survival more than doubled from 3.0 months with single-agent chemotherapy to 7.7 months with crizotinib, according to an independent radiologic review (P value less than .0001; hazard ratio, 0.49). Crizotinib (Xalkori) remained superior regardless of whether chemotherapy contained docetaxel (Taxotere) (7.7 vs. 2.6 months; P less than .0001) or pemetrexed (Alimta) (7.7 vs. 4.2; P = .0004), an agent previously shown to be effective against ALK-positive NSCLC.
The overall response rate was 65.3% for crizotinib and 19.5% for chemotherapy in the intent to treat population of 347 patients (overall response rate ratio 3.4; P less than .0001).
Crizotinib was also associated with significantly greater improvement in lung cancer symptoms and quality of life, Dr. Alice Shaw said at the European Society for Medical Oncology Congress. "Taken together, these results establish crizotinib as the standard of care for patients with advanced, previously treated ALK-positive non–small cell lung cancer."
ALK rearrangements are present in about 5% of lung cancers, typically in younger, never smokers.
Overall survival in the study was 22.8 months for chemotherapy and 20.3 months for crizotinib (P = .5394; HR, 1.02). The interim survival analysis was immature with just 40% of expected deaths reported and likely confounded by the high number (87%) of chemotherapy patients who crossed over to crizotinib after progression, she noted. After adjusting for crossover, the hazard ratio suggests a survival advantage with crizotinib (HR, 0.83).
Discussant Jean-Charles Soria of Institut Gustave Roussy, Villejuif, France, agreed and said the survival times in either arm were impressive, observing that just 2 years ago survival in second-line ALK-positive NSCLC was just 9 months.
Crizotinib, an oral, first in class ALK inhibitor, was given accelerated approval in 2011 in the United States to treat advanced ALK-positive NSCLC but is not approved in Europe, where regulatory agencies have required data from the randomized trial.
Dr. Soria said that worldwide use of crizotinib will require that several financial and practical issues surrounding implementation of molecular testing in daily practice be addressed including the optimal technique, type of sample, and tissue availability.
Testing for epidermal growth factor receptor, another molecular alteration that directs targeted therapy in lung cancer, "should not compete with ALK," he said, adding that multiplexing test strategies "are key."
Investigators at 105 sites across 21 countries randomized 173 patients to crizotinib 250 mg twice-daily in a 21-day cycle and 174 patients to chemotherapy containing pemetrexed 500 mg/m2 or docetaxel 75 mg/m2 given intravenously on day 1 of a 21-day cycle.
Treatment duration varied significantly, with patients receiving a median of 11 cycles of crizotinib vs. 4 cycles of chemotherapy. This may have influenced the higher number of all-cause deaths among crizotinib patients (25 deaths vs. 7 deaths), said Dr. Shaw, a thoracic oncologist at Massachusetts General Hospital Cancer Center in Boston.
Crizotinib patients were more likely than chemotherapy patients to experience visual disturbances (any grade 60% vs. 9%), as well as diarrhea, nausea, elevated transaminases (16% grade 3/4 ), edema, upper respiratory infection, dysgeusia, and dizziness. In contrast, fatigue, alopecia, dyspnea, and rash were more common with chemotherapy.
Despite the fact that patients on crizotinib experienced more nausea and vomiting, antiemetic use was significantly higher in the chemotherapy arm (67% vs. 20%). Based on the EORTC Quality of Life Questionnaire (QLQ C-30) and QLQ-LC 13, crizotinib patients had greater improvement from baseline in cough, dyspnea, fatigue, alopecia, insomnia, and pain as well as global quality of life (both P less than .0001).
Dr. Soria reported financial relationshisps with several firms including Pfizer, the study sponsor.
Major Finding: Median progression-free survival was 3.0 months with chemotherapy and 7.7 months with crizotinib (P less than .0001; hazard ratio 0.49).
Data Source: Results came from a phase III study involving 318 patients with advanced ALK-positive non–small cell lung cancer.
Disclosures: Dr. Shaw reported an advisory relationship with Pfizer, Ariad, Chugai, Novartis, and Daiichi-Sankyo and research funding from AstraZeneca and Novartis.